Prevalence and Management of Pressure Ulcers in Acute Care Wards: A Systematic Review
VerifiedAdded on 2023/06/09
|78
|24275
|382
AI Summary
This systematic review focuses on the prevalence and management of pressure ulcers in acute care wards. The study adopts interpretivism research philosophy and analyses 12 English scholarly articles published from 2008 to 2018. The findings suggest that pressure ulcers are prevalent among most patients admitted to acute care wards across hospitals and nursing homes in different countries. The study identifies the major barriers that prevent the proper implementation of prevention strategies and recommends nursing education and training for increasing clinical knowledge and attitude towards PU prevention.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: MSC NURSING
Dissertation
Name of the Student
Name of the University
Author Note
Dissertation
Name of the Student
Name of the University
Author Note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1MSC NURSING
Abstract
Background- Pressure ulcers occur when a strong pressure is applied over the soft tissues
that underlie the skin, thus resulting in complete or partial obstruction of blood flow to the
regions of soft tissue. Also referred to as bed sores, the condition usually occurs over a region
of bony prominence and is found widely prevalent, on a global scale.
Methodology- The research philosophy of interpretivism was adopted to conduct an
extensive systematic review of English scholarly articles that were published from 2008 to
2018, followed by organisation of the data findings on the basis of themes or data patterns.
Results- 12 articles provided an exhaustive detail on the prevalence of pressure ulcer among
most patients admitted to the acute wards across hospitals and nursing homes in different
countries. Most of the studies graded PU into 4 different categories, based on the NPUAP and
EPUAP classification guidelines. PUs were found to affect most people in the sacral region,
heels and the hips, and is more found among older adults, females, people who are under
affected with malnutrition and diabetics. Most common impacts of PU were identified as a
restriction in mobility of the patients, lack of participation in activities of daily living,
increased stay at hospitals, and economic burden on the patient and family members. Poor
knowledge among nursing assistants, inadequate staff, lack of time, and huge workload were
recognised as the major barriers that prevented the proper implementation of prevention
strategies.
Conclusion- Efforts must be taken by nursing staff to explain the management process to all
patients. Provisions for nursing education and training are imperative for increasing their
clinical knowledge and attitude towards PU prevention. Skin grafting surgery can prove
effective in management of the condition.
Keywords: pressure, ulcer, prevalence, acute, management, nursing
Abstract
Background- Pressure ulcers occur when a strong pressure is applied over the soft tissues
that underlie the skin, thus resulting in complete or partial obstruction of blood flow to the
regions of soft tissue. Also referred to as bed sores, the condition usually occurs over a region
of bony prominence and is found widely prevalent, on a global scale.
Methodology- The research philosophy of interpretivism was adopted to conduct an
extensive systematic review of English scholarly articles that were published from 2008 to
2018, followed by organisation of the data findings on the basis of themes or data patterns.
Results- 12 articles provided an exhaustive detail on the prevalence of pressure ulcer among
most patients admitted to the acute wards across hospitals and nursing homes in different
countries. Most of the studies graded PU into 4 different categories, based on the NPUAP and
EPUAP classification guidelines. PUs were found to affect most people in the sacral region,
heels and the hips, and is more found among older adults, females, people who are under
affected with malnutrition and diabetics. Most common impacts of PU were identified as a
restriction in mobility of the patients, lack of participation in activities of daily living,
increased stay at hospitals, and economic burden on the patient and family members. Poor
knowledge among nursing assistants, inadequate staff, lack of time, and huge workload were
recognised as the major barriers that prevented the proper implementation of prevention
strategies.
Conclusion- Efforts must be taken by nursing staff to explain the management process to all
patients. Provisions for nursing education and training are imperative for increasing their
clinical knowledge and attitude towards PU prevention. Skin grafting surgery can prove
effective in management of the condition.
Keywords: pressure, ulcer, prevalence, acute, management, nursing
2MSC NURSING
Table of Contents
Chapter 1:...................................................................................................................................4
Introduction............................................................................................................................4
Problem statement..................................................................................................................6
Rationale................................................................................................................................9
Research question.................................................................................................................12
Research aim........................................................................................................................12
Research objective...............................................................................................................12
Chapter 2:.................................................................................................................................13
Introduction..........................................................................................................................13
Qualitative research..............................................................................................................13
Research philosophy............................................................................................................14
Research approach...............................................................................................................14
Research design....................................................................................................................14
Literature search...................................................................................................................14
Keywords.............................................................................................................................15
Bibliographic Aids...............................................................................................................16
Inclusion and Exclusion Criteria..........................................................................................17
Justification between inclusion and exclusion criteria.........................................................18
Revised inclusion and inclusion criteria..............................................................................18
Search Strategy.....................................................................................................................19
Search Outcomes..................................................................................................................19
Table of Contents
Chapter 1:...................................................................................................................................4
Introduction............................................................................................................................4
Problem statement..................................................................................................................6
Rationale................................................................................................................................9
Research question.................................................................................................................12
Research aim........................................................................................................................12
Research objective...............................................................................................................12
Chapter 2:.................................................................................................................................13
Introduction..........................................................................................................................13
Qualitative research..............................................................................................................13
Research philosophy............................................................................................................14
Research approach...............................................................................................................14
Research design....................................................................................................................14
Literature search...................................................................................................................14
Keywords.............................................................................................................................15
Bibliographic Aids...............................................................................................................16
Inclusion and Exclusion Criteria..........................................................................................17
Justification between inclusion and exclusion criteria.........................................................18
Revised inclusion and inclusion criteria..............................................................................18
Search Strategy.....................................................................................................................19
Search Outcomes..................................................................................................................19
3MSC NURSING
Snowball Technique.............................................................................................................21
Quality Assessment..............................................................................................................23
Conclusion............................................................................................................................24
Chapter 3:.................................................................................................................................25
Chapter 4:.................................................................................................................................39
Results..................................................................................................................................39
Theme 1: Following NPUAP and EPUAP classification pattern....................................39
Theme 2: Methodological quality of the studies..............................................................41
Theme 3: Location of the PU...........................................................................................44
Discussion............................................................................................................................45
Impacts of pressure ulcer.................................................................................................45
Nursing knowledge and attitude on pressure ulcer..........................................................48
Nursing implications and preventive strategies in pressure ulcer....................................50
Limitations...........................................................................................................................53
Chapter 5:.................................................................................................................................54
Conclusion............................................................................................................................54
Recommendation..................................................................................................................56
References................................................................................................................................59
Appendix..................................................................................................................................70
Snowball Technique.............................................................................................................21
Quality Assessment..............................................................................................................23
Conclusion............................................................................................................................24
Chapter 3:.................................................................................................................................25
Chapter 4:.................................................................................................................................39
Results..................................................................................................................................39
Theme 1: Following NPUAP and EPUAP classification pattern....................................39
Theme 2: Methodological quality of the studies..............................................................41
Theme 3: Location of the PU...........................................................................................44
Discussion............................................................................................................................45
Impacts of pressure ulcer.................................................................................................45
Nursing knowledge and attitude on pressure ulcer..........................................................48
Nursing implications and preventive strategies in pressure ulcer....................................50
Limitations...........................................................................................................................53
Chapter 5:.................................................................................................................................54
Conclusion............................................................................................................................54
Recommendation..................................................................................................................56
References................................................................................................................................59
Appendix..................................................................................................................................70
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4MSC NURSING
Chapter 1:
Introduction
Pressure ulcers (PU) are most commonly defined as localized injuries to the skin
and/or tissues that underlie the skin, usually present over a bony prominence. The ulcer most
commonly occurs due to pressure, often in combination with friction and/or shear. Some of
the most common sites that get affected due to pressure ulcer are the skin regions that overlie
the coccyx, sacrum, hips and the heels (McGinnis et al. 2014). However, some other sites that
might also be affected include the elbows, ankles, knees, and the back of shoulder.Pressure
ulcers usually occur due to burden that is applied to the different soft tissues of the body,
thereby causing completeand/or partial obstruction to the blood flow in soft tissues. Shear is
considered as a major cause for the physiological condition owing to the fact that shear forces
pull on different blood vessels that are responsible for feeding the skin. Pressure ulcers have
been found to most commonly develop in persons who follow a sedentary lifestyle and
generally do not move about much, such as patients or disabled individuals who are confined
to wheelchairs or are bedridden. Researchers and healthcare professionals hold the strong
belief that a plethora of other factors are also responsible for influencing theforbearance of
the skin for shear and pressure, thusgrowing the risks of development of pressure ulcer
(Edwards et al. 2014).
Some of these factors are associated with microclimate(wetness of the skin that is
caused due to incontinence or sweating), protein-calorie malnutrition, diseases that play a role
in reducing the flow of blood to the skin, such as, arteriosclerosis, and other illnessesthat
directly lower the perceptionpower in the skin, such as, neuropathy or paralysis. The time that
is taken by an affected individual for the healing of PUoften gets slowed down with an
increase in age of the patients, in addition to a range of concomitant factors such as, diabetes,
Chapter 1:
Introduction
Pressure ulcers (PU) are most commonly defined as localized injuries to the skin
and/or tissues that underlie the skin, usually present over a bony prominence. The ulcer most
commonly occurs due to pressure, often in combination with friction and/or shear. Some of
the most common sites that get affected due to pressure ulcer are the skin regions that overlie
the coccyx, sacrum, hips and the heels (McGinnis et al. 2014). However, some other sites that
might also be affected include the elbows, ankles, knees, and the back of shoulder.Pressure
ulcers usually occur due to burden that is applied to the different soft tissues of the body,
thereby causing completeand/or partial obstruction to the blood flow in soft tissues. Shear is
considered as a major cause for the physiological condition owing to the fact that shear forces
pull on different blood vessels that are responsible for feeding the skin. Pressure ulcers have
been found to most commonly develop in persons who follow a sedentary lifestyle and
generally do not move about much, such as patients or disabled individuals who are confined
to wheelchairs or are bedridden. Researchers and healthcare professionals hold the strong
belief that a plethora of other factors are also responsible for influencing theforbearance of
the skin for shear and pressure, thusgrowing the risks of development of pressure ulcer
(Edwards et al. 2014).
Some of these factors are associated with microclimate(wetness of the skin that is
caused due to incontinence or sweating), protein-calorie malnutrition, diseases that play a role
in reducing the flow of blood to the skin, such as, arteriosclerosis, and other illnessesthat
directly lower the perceptionpower in the skin, such as, neuropathy or paralysis. The time that
is taken by an affected individual for the healing of PUoften gets slowed down with an
increase in age of the patients, in addition to a range of concomitant factors such as, diabetes,
5MSC NURSING
smoking, infection, and/or medications namely, anti-inflammatory drugs. PU has been
identified as a grave safety matter in healthcare systems in recent years (Kasuya, Sakabe and
Tokura 2014). This can be attributed to the fact that the condition has been found to create an
adverse impact on all patients, owing to the pain that it results in, and the time that is required
for healing of the injury or wound. These ulcers are also responsible for greatly increasing the
workload of healthcare professionals, due to which the costs of healthcare
servicesincreaseradically. These ulcers have also been found responsible for death, under
extreme situations (Fu Shaw et al. 2014). The period of compression that is tolerated by the
skin, until there occurs a breakdown differs from one person to another, and tissue damage as
a result of pressure ulcer are most commonly found to occur within less than two hours
among patients who are incapable. Pressure ulcers are primarily caused due to inadequate
supply of blood that leads to a reperfusion injury, upon re-entry of the blood into the tissues
(Manorama et al. 2013).
One common example of mild pressure related soresare often experienced by healthy
persons while they sit in same position for long periods of time. They report experiences of a
dull ache that is generally indicative of an obstructing in the blood flow to the regions that are
mostly affected. Within few hours of this condition, blood supply shortage, referred to as
ischemia, leads to damage of tissues and/or cell death. The sores usually beginin the form of a
red and painful sensation. Other events that have been found responsible for pressure ulcer
development are instances when pressure is large enough to result in damage of the cell
membrane of the muscle cells. This leads to subsequent death of the muscle cells, in addition
to death of the skin that is fed through blood vessels that originate from the muscles
(Coleman et al. 2014). This is usually categorised as a deep tissue injury type of pressure
ulcer and appears in the form of a purple intact skin.According to data estimates provided by
the NHS Safety Thermometer, 25,000 new patients had been identified to develop symptoms
smoking, infection, and/or medications namely, anti-inflammatory drugs. PU has been
identified as a grave safety matter in healthcare systems in recent years (Kasuya, Sakabe and
Tokura 2014). This can be attributed to the fact that the condition has been found to create an
adverse impact on all patients, owing to the pain that it results in, and the time that is required
for healing of the injury or wound. These ulcers are also responsible for greatly increasing the
workload of healthcare professionals, due to which the costs of healthcare
servicesincreaseradically. These ulcers have also been found responsible for death, under
extreme situations (Fu Shaw et al. 2014). The period of compression that is tolerated by the
skin, until there occurs a breakdown differs from one person to another, and tissue damage as
a result of pressure ulcer are most commonly found to occur within less than two hours
among patients who are incapable. Pressure ulcers are primarily caused due to inadequate
supply of blood that leads to a reperfusion injury, upon re-entry of the blood into the tissues
(Manorama et al. 2013).
One common example of mild pressure related soresare often experienced by healthy
persons while they sit in same position for long periods of time. They report experiences of a
dull ache that is generally indicative of an obstructing in the blood flow to the regions that are
mostly affected. Within few hours of this condition, blood supply shortage, referred to as
ischemia, leads to damage of tissues and/or cell death. The sores usually beginin the form of a
red and painful sensation. Other events that have been found responsible for pressure ulcer
development are instances when pressure is large enough to result in damage of the cell
membrane of the muscle cells. This leads to subsequent death of the muscle cells, in addition
to death of the skin that is fed through blood vessels that originate from the muscles
(Coleman et al. 2014). This is usually categorised as a deep tissue injury type of pressure
ulcer and appears in the form of a purple intact skin.According to data estimates provided by
the NHS Safety Thermometer, 25,000 new patients had been identified to develop symptoms
6MSC NURSING
of pressure ulcer from April 2014 to March 2015. On average, an estimated 2,000 newly
acquired instances of pressure ulcers are encountered every month withinNHS, in England.
Aged population is more likely to suffer from pressure ulcer, especially people aged more
than 70 years, and those who have been operated for a hip fracture. People having spinal cord
injuries are another major group where the prevalence of PU is as high as 20-30%, following
one or five years after the injury has occurred (GOV.UK 2018). Hence, healthcare
professionals should have an understanding of the needs and demands of the community,
individual, and population, in addition to thinking about the resources that are easily available
in the healthcare facility. Obtaining relevant data regarding the prevalence of pressure ulcer
in acute wards will help in identifying the specific quality standards that need to be
implemented and coordinated across the acute care units, in order to encompass the complete
pressure ulcer pathway. This research will further facilitate identifying the ways by which an
appropriate system-based method can be utilised, with the aim of conducting investigation on
the prevention measures and interventions, to reduce the prevalence.
Problem statement
The National Pressure Ulcer Advisory Panel (NPUAP) has divided pressure ulcer into
four stages, depending on the severity of the condition. While stage 1 represents a condition
where there occurs a reddened spot that is not blanched by pressuring and is often
accompanied by edema, damage of the skin surface layers occur in stage 2. The epidermis
and dermis usually get affected in the second stage (Edsberg et al. 2016). Thickness of the
skin gets lost completely in stage 3 where the damage of the subcutaneous tissue often gets
extended deep into the muscular tissues. This stage encompasses a clinical observation of the
ulcer in the form of a deep cavity that generally gets extended to the adjacent tissues and
requires a longer healing time. Complete skin loss, in addition to skin destruction and
of pressure ulcer from April 2014 to March 2015. On average, an estimated 2,000 newly
acquired instances of pressure ulcers are encountered every month withinNHS, in England.
Aged population is more likely to suffer from pressure ulcer, especially people aged more
than 70 years, and those who have been operated for a hip fracture. People having spinal cord
injuries are another major group where the prevalence of PU is as high as 20-30%, following
one or five years after the injury has occurred (GOV.UK 2018). Hence, healthcare
professionals should have an understanding of the needs and demands of the community,
individual, and population, in addition to thinking about the resources that are easily available
in the healthcare facility. Obtaining relevant data regarding the prevalence of pressure ulcer
in acute wards will help in identifying the specific quality standards that need to be
implemented and coordinated across the acute care units, in order to encompass the complete
pressure ulcer pathway. This research will further facilitate identifying the ways by which an
appropriate system-based method can be utilised, with the aim of conducting investigation on
the prevention measures and interventions, to reduce the prevalence.
Problem statement
The National Pressure Ulcer Advisory Panel (NPUAP) has divided pressure ulcer into
four stages, depending on the severity of the condition. While stage 1 represents a condition
where there occurs a reddened spot that is not blanched by pressuring and is often
accompanied by edema, damage of the skin surface layers occur in stage 2. The epidermis
and dermis usually get affected in the second stage (Edsberg et al. 2016). Thickness of the
skin gets lost completely in stage 3 where the damage of the subcutaneous tissue often gets
extended deep into the muscular tissues. This stage encompasses a clinical observation of the
ulcer in the form of a deep cavity that generally gets extended to the adjacent tissues and
requires a longer healing time. Complete skin loss, in addition to skin destruction and
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7MSC NURSING
necrosis are the characteristic features of stage 4. This stage also comprises of secretory
sinuses (Biglari et al. 2014).
Thus, the rate of infection that are associated with pressure ulcers are of prime
concern due to the fact that staying in a fixed position for a prolonged time increases the
likelihood of the condition getting aggravated (Cooper 2013). Shearing of skin most
commonly refer to its separation from the tissues present beneath it. In instances when a
patient is found to partially sit up on the bed, the skin gets stuck to the sheet or mattress,
thereby making it susceptible to shearing forces. This generally happens when the underlying
tissues go downwards along with the entire body, towards the bed foot. Friction is also
damaging to the blood vessels that are superficial on the skin and is experienced when the
two surfaces get rubbed against each other. Friction most commonly occurs an injury to the
skin present over the elbows (Brienza et al. 2015). It also injures the back when the patients
are slid or pulled over the bed sheets, while they are transferred from the bed to stretchers or
wheelchairs. Upon exertion of pressure over a specific area of the body, primarily the bony
prominences, the blood capillaries get obstructed as a result of which the tissues are deprived
of their oxygen content and nutrients. This leads to the development of ischemia, edema,
hypoxia, or inflammation, followed by ulcer. Patients are also subjected to development of
PU due to moisture (Solovyev et al. 2013). Urine, sweat, fecal matter, and excess wound
drainage often exacerbate the damage that pressure, friction and shearing forces create on the
skin and its tissues. This directly contributes to a maceration of the skin surrounding the
affected point, thereby potentially aggravating the deleterious impacts of ulcers.
PUs have also been associated with morbidity and infection caused due to Methicillin-
resistant Staphylococcus aureus (MRSA), which in turn are directly responsiblefor increasing
the length of stay at hospitals. Research evidences have established the fact that PUs ensue in
patients, admitted across different healthcare units, which most commonly includes acute
necrosis are the characteristic features of stage 4. This stage also comprises of secretory
sinuses (Biglari et al. 2014).
Thus, the rate of infection that are associated with pressure ulcers are of prime
concern due to the fact that staying in a fixed position for a prolonged time increases the
likelihood of the condition getting aggravated (Cooper 2013). Shearing of skin most
commonly refer to its separation from the tissues present beneath it. In instances when a
patient is found to partially sit up on the bed, the skin gets stuck to the sheet or mattress,
thereby making it susceptible to shearing forces. This generally happens when the underlying
tissues go downwards along with the entire body, towards the bed foot. Friction is also
damaging to the blood vessels that are superficial on the skin and is experienced when the
two surfaces get rubbed against each other. Friction most commonly occurs an injury to the
skin present over the elbows (Brienza et al. 2015). It also injures the back when the patients
are slid or pulled over the bed sheets, while they are transferred from the bed to stretchers or
wheelchairs. Upon exertion of pressure over a specific area of the body, primarily the bony
prominences, the blood capillaries get obstructed as a result of which the tissues are deprived
of their oxygen content and nutrients. This leads to the development of ischemia, edema,
hypoxia, or inflammation, followed by ulcer. Patients are also subjected to development of
PU due to moisture (Solovyev et al. 2013). Urine, sweat, fecal matter, and excess wound
drainage often exacerbate the damage that pressure, friction and shearing forces create on the
skin and its tissues. This directly contributes to a maceration of the skin surrounding the
affected point, thereby potentially aggravating the deleterious impacts of ulcers.
PUs have also been associated with morbidity and infection caused due to Methicillin-
resistant Staphylococcus aureus (MRSA), which in turn are directly responsiblefor increasing
the length of stay at hospitals. Research evidences have established the fact that PUs ensue in
patients, admitted across different healthcare units, which most commonly includes acute
8MSC NURSING
care wards. Acute care units generally comprise of surgical, medical, orthopedics, critical
care, and elderly care wards. Placing focus on a specific healthcare setting such as, acute care
ward, will facilitate the process of investigating the prevalence of pressure ulcer, through
epidemiology (Beeckman et al. 2014). Acute care wards refer to those settingsin healthcare
institutions where patients are provided medical care facilities, while they are recovering
from any surgery or illness. Furthermore, due to the fact that acute care wards generally
comprise of patients who are severely ill, and have restricted mobility or activity, they are
more prone to be bedridden and develop pressure ulcers. These patients also report a loss of
their sensory perception and circulatory/metabolic changes due to anesthesia and surgery.
Pressure ulcers are largely responsible for several economic challenges to the allocation of
resources in any healthcare system. The high costs of treating pressure ulcer patients every
day have been found to vary from 1.71€ to 470.5€, across different healthcare settings
(Demarré et al. 2015). Similar results have also been retrieved from the United Kingdom,
where PU treatment costs were found to range from £1,214 for stage 1 patients to £14,108 for
stage 4 patients (Dealey, Posnett and Walker 2012).
Use of biofilms are cited as one of the primary reasons that contribute to a delay in the
healing of PU. Biofilm stall the wound healing process by maintaining an inflammation at the
site of injury. Antimicrobial dressings and frequent debridement are essential for controlling
the biofilms (Seth et al. 2012). This infection creates an impairment in the process of healing
of pressure ulcers. Certain signs and symptoms that help in the detection of a pressure wound
are presence of erythema, fever, edema, drainage and odor (Delmore et al. 2015). Erythema
around a wound or injury results in the form of normal response of the body to the traumatic
injury (Chan et al. 2013). However, presence of a poorly defined of erythema indicates
infection. PU is also accompanied with systemic fever along with concomitant complaints of
malaise. This in turn indicates the presence of infection, and an increase in local temperature,
care wards. Acute care units generally comprise of surgical, medical, orthopedics, critical
care, and elderly care wards. Placing focus on a specific healthcare setting such as, acute care
ward, will facilitate the process of investigating the prevalence of pressure ulcer, through
epidemiology (Beeckman et al. 2014). Acute care wards refer to those settingsin healthcare
institutions where patients are provided medical care facilities, while they are recovering
from any surgery or illness. Furthermore, due to the fact that acute care wards generally
comprise of patients who are severely ill, and have restricted mobility or activity, they are
more prone to be bedridden and develop pressure ulcers. These patients also report a loss of
their sensory perception and circulatory/metabolic changes due to anesthesia and surgery.
Pressure ulcers are largely responsible for several economic challenges to the allocation of
resources in any healthcare system. The high costs of treating pressure ulcer patients every
day have been found to vary from 1.71€ to 470.5€, across different healthcare settings
(Demarré et al. 2015). Similar results have also been retrieved from the United Kingdom,
where PU treatment costs were found to range from £1,214 for stage 1 patients to £14,108 for
stage 4 patients (Dealey, Posnett and Walker 2012).
Use of biofilms are cited as one of the primary reasons that contribute to a delay in the
healing of PU. Biofilm stall the wound healing process by maintaining an inflammation at the
site of injury. Antimicrobial dressings and frequent debridement are essential for controlling
the biofilms (Seth et al. 2012). This infection creates an impairment in the process of healing
of pressure ulcers. Certain signs and symptoms that help in the detection of a pressure wound
are presence of erythema, fever, edema, drainage and odor (Delmore et al. 2015). Erythema
around a wound or injury results in the form of normal response of the body to the traumatic
injury (Chan et al. 2013). However, presence of a poorly defined of erythema indicates
infection. PU is also accompanied with systemic fever along with concomitant complaints of
malaise. This in turn indicates the presence of infection, and an increase in local temperature,
9MSC NURSING
which is a direct result of inflammation. Presence of a sweet smell from the site of the skin
that has been injured provides evidence for the presence of infection due to Pseudomonas.
Proteus infection leads to a smell of ammonia gas.
Rationale
Some of the intrinsic factors that contribute to the incidence of pressure ulcer are
illnesses that affect the mobility of a person. These mobility issues are commonly faced by
people who have suffered from a spinal cord injury that have resulted in paralysis of the
limbs Brain damage due to stroke or severe head injury or other conditions such as, multiple
sclerosis, fractured bones, or a coma state make it difficult for a person to move freely.Poor
nutrition that occurs due to dehydration and anorexia nervosa is another major contributor to
the condition (Posthauer et al. 2015). Normal blood flow to the skin and underlying tissues
are a direct manifestation of type 1 and 2 diabetes, and peripheral artery disease. The latter
condition has been found responsible for restricting blood flow due to an accumulation of
fatty substances in the major blood vessels (arteries) present in the legs. Furthermore, renal
failure also leads to loss of all or most functions of the kidney that results in an accumulation
of poison or toxin in the blood, thereby causing damage to the tissues. Some of the primary
reasons that make an aeging skin more vulnerable to development of pressure ulcer is that the
skin generally loses the property of stretching and elasticity, with an increase in age that
makes it prone to get damaged (Qaddumi and Khawaldeh 2014). Direct effects of ageing are
also associated with a reduction in blood flow and a lowering in the amount of fat that is
present under the skin.However, there are a plethora of extrinsic factors that also increase the
likelihood of a person of acquiring pressure ulcer. Pressure exerted by a hard surface such as,
a wheelchair or bed that the patient has been using for a prolonged period of time in acute
wards, is one major factor. Pressure on the skin is also exerted through several involuntary
movements like muscle spasms (Anderson et al. 2014). Thus, the time that PU takes to
which is a direct result of inflammation. Presence of a sweet smell from the site of the skin
that has been injured provides evidence for the presence of infection due to Pseudomonas.
Proteus infection leads to a smell of ammonia gas.
Rationale
Some of the intrinsic factors that contribute to the incidence of pressure ulcer are
illnesses that affect the mobility of a person. These mobility issues are commonly faced by
people who have suffered from a spinal cord injury that have resulted in paralysis of the
limbs Brain damage due to stroke or severe head injury or other conditions such as, multiple
sclerosis, fractured bones, or a coma state make it difficult for a person to move freely.Poor
nutrition that occurs due to dehydration and anorexia nervosa is another major contributor to
the condition (Posthauer et al. 2015). Normal blood flow to the skin and underlying tissues
are a direct manifestation of type 1 and 2 diabetes, and peripheral artery disease. The latter
condition has been found responsible for restricting blood flow due to an accumulation of
fatty substances in the major blood vessels (arteries) present in the legs. Furthermore, renal
failure also leads to loss of all or most functions of the kidney that results in an accumulation
of poison or toxin in the blood, thereby causing damage to the tissues. Some of the primary
reasons that make an aeging skin more vulnerable to development of pressure ulcer is that the
skin generally loses the property of stretching and elasticity, with an increase in age that
makes it prone to get damaged (Qaddumi and Khawaldeh 2014). Direct effects of ageing are
also associated with a reduction in blood flow and a lowering in the amount of fat that is
present under the skin.However, there are a plethora of extrinsic factors that also increase the
likelihood of a person of acquiring pressure ulcer. Pressure exerted by a hard surface such as,
a wheelchair or bed that the patient has been using for a prolonged period of time in acute
wards, is one major factor. Pressure on the skin is also exerted through several involuntary
movements like muscle spasms (Anderson et al. 2014). Thus, the time that PU takes to
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10MSC NURSING
develop in patients depends on the amount of pressure that is applied, and the vulnerability of
the patient skin to the damage.
The development of PU can lead to several health complications. One of the most
serious complication is onset of sepsis. Presence of a PU is most often accompanied with
aerobic and/or anaerobic bacteremia, owing to the fact that these kinds of ulcers are one of
the most common source of the infection. Further health complications of Pus also include
cellulitis, localized infection, and osteomyelitis. Fair often, development of a non-healing
PUprovides an indication underlying osteomyelitis. Several studies have been conducted that
have successfully established a correlation between development of PU and patient mortality
in both nursing home and hospital settings (Girard et al. 2014). Furthermore, mortality rates
have been found to be as large as 60%, for the aged population, who generally develop an
ulcer within a year of discharge from a hospital. Hence, it is imperative to conduct a careful
assessment of PU among patients. Some other complications related with PU include
depression and pain, both of which have largely been connected with reduced wound healing
(McInnes et al. 2015).Long term non-healing PUs have also been found to result in the
development of squamous cell carcinoma. This calls for the need of healthcare professionals
providing care in the acute medical wards to try shifting the weight of the patients who use a
wheelchair, or are bedridden, every 15-20 minutes, and reposition them after every hour to
prevent the hard surface of the chair of bed from exerting a pressure on their skin (Gillespie
et al. 2014).
Under conditions, when the patients admitted to acute wards are found in possession
of upper body strength, they should also be provided an assistance in wheelchair push-ups.
Use of appropriate cushions and special pressure relieving mattresses that reduce pressure
and ensure well-positioning of the entire body. In addition, adjusting the bed elevation at less
than 30 degrees are another essential step that can be taken in acute wards. However, there
develop in patients depends on the amount of pressure that is applied, and the vulnerability of
the patient skin to the damage.
The development of PU can lead to several health complications. One of the most
serious complication is onset of sepsis. Presence of a PU is most often accompanied with
aerobic and/or anaerobic bacteremia, owing to the fact that these kinds of ulcers are one of
the most common source of the infection. Further health complications of Pus also include
cellulitis, localized infection, and osteomyelitis. Fair often, development of a non-healing
PUprovides an indication underlying osteomyelitis. Several studies have been conducted that
have successfully established a correlation between development of PU and patient mortality
in both nursing home and hospital settings (Girard et al. 2014). Furthermore, mortality rates
have been found to be as large as 60%, for the aged population, who generally develop an
ulcer within a year of discharge from a hospital. Hence, it is imperative to conduct a careful
assessment of PU among patients. Some other complications related with PU include
depression and pain, both of which have largely been connected with reduced wound healing
(McInnes et al. 2015).Long term non-healing PUs have also been found to result in the
development of squamous cell carcinoma. This calls for the need of healthcare professionals
providing care in the acute medical wards to try shifting the weight of the patients who use a
wheelchair, or are bedridden, every 15-20 minutes, and reposition them after every hour to
prevent the hard surface of the chair of bed from exerting a pressure on their skin (Gillespie
et al. 2014).
Under conditions, when the patients admitted to acute wards are found in possession
of upper body strength, they should also be provided an assistance in wheelchair push-ups.
Use of appropriate cushions and special pressure relieving mattresses that reduce pressure
and ensure well-positioning of the entire body. In addition, adjusting the bed elevation at less
than 30 degrees are another essential step that can be taken in acute wards. However, there
11MSC NURSING
exist several gaps in the theory and practice of pressure ulcer. Time and again researchers
have identified presence of an inconsistency between the guidelines of PU prevention and
management that are taught and those that are implemented by nurses, across a range of
healthcare settings (Padula et al. 2014). These gaps are directly related to the clinical
expertise and education that nurses have on prevention of PU and its elimination from acute
medical wards. The fact that nursing colleges across the globe differ in the education and
training they provide to the nursing professionals on the condition, significantly contributes
to a major difference in the ways the prevalence of PU is perceived across the different
countries. New graduate nurses often lack an empowerment and are not able to take
necessary clinical decisions such as, adding a pressure relieving surface or preventing shear
or friction forces in the affected people. Further gaps in research on pressure ulcer can be
attributed to the risk factors that make a person susceptible to the condition. In addition, the
range of risk factors such as, nutrition, moisture, shear, friction varies among people based on
their geographical location, socio-economic condition, and employment status (Cremasco et
al. 2013). People belonging to poor economic households most often resort to occupational
roles that requires them perform manual handling tasks that increases risks of shear, in
addition to inadequate nutritional intake (Bain et al. 2013). Furthermore, the risk assessment
tools that are used in acute care units of developed nations often do not encompass all aspects
that are necessary for long-term care of PU patients. Another major gap lies in the fact that
developing countries have medical departments that are devoid of such risk assessment tools,
or even if present, the nursing professionals do not have adequate knowledge on utilising
them (Chou et al. 2013). This prevents detailed analysis of the skin of the affected people.
Further gaps that established the need of conducting this research lie in the fact that there are
discrepancies in the guidelines that are most often followed by clinicians and interventions
that are supported by scientific evidences. Hence, identifying the prevalence of pressure ulcer
exist several gaps in the theory and practice of pressure ulcer. Time and again researchers
have identified presence of an inconsistency between the guidelines of PU prevention and
management that are taught and those that are implemented by nurses, across a range of
healthcare settings (Padula et al. 2014). These gaps are directly related to the clinical
expertise and education that nurses have on prevention of PU and its elimination from acute
medical wards. The fact that nursing colleges across the globe differ in the education and
training they provide to the nursing professionals on the condition, significantly contributes
to a major difference in the ways the prevalence of PU is perceived across the different
countries. New graduate nurses often lack an empowerment and are not able to take
necessary clinical decisions such as, adding a pressure relieving surface or preventing shear
or friction forces in the affected people. Further gaps in research on pressure ulcer can be
attributed to the risk factors that make a person susceptible to the condition. In addition, the
range of risk factors such as, nutrition, moisture, shear, friction varies among people based on
their geographical location, socio-economic condition, and employment status (Cremasco et
al. 2013). People belonging to poor economic households most often resort to occupational
roles that requires them perform manual handling tasks that increases risks of shear, in
addition to inadequate nutritional intake (Bain et al. 2013). Furthermore, the risk assessment
tools that are used in acute care units of developed nations often do not encompass all aspects
that are necessary for long-term care of PU patients. Another major gap lies in the fact that
developing countries have medical departments that are devoid of such risk assessment tools,
or even if present, the nursing professionals do not have adequate knowledge on utilising
them (Chou et al. 2013). This prevents detailed analysis of the skin of the affected people.
Further gaps that established the need of conducting this research lie in the fact that there are
discrepancies in the guidelines that are most often followed by clinicians and interventions
that are supported by scientific evidences. Hence, identifying the prevalence of pressure ulcer
12MSC NURSING
across acute wards in different countries, followed by dissemination of the findings would
help healthcare professionals to effectively manage the condition.
Research question
A research question is most commonly formulated in the form of an answerable
inquiry of a specific issue or concern that acts as the preliminary step for a research project.
The research question formulated for this systematic review is as follows:
What is the prevalence of pressure ulcer among patients admitted to the acute ward?
Research aim
The main aim of the research is to determine the rates of prevalence of PU in acute
care units, by conducting a thorough and exhaustive search of available literature that are
relevant to the research question. This would help to explore the size of the health problem in
acute wards in hospitals and nursing homes, while taking into consideration the major
contributing factors of its development, specifically in the target population.
Research objective
Determine the prevalence of pressure ulcer in acute ward patients
Investigate the impacts of pressure ulcers in acute ward patients
Recognise the instruments that are used to classify PU status
across acute wards in different countries, followed by dissemination of the findings would
help healthcare professionals to effectively manage the condition.
Research question
A research question is most commonly formulated in the form of an answerable
inquiry of a specific issue or concern that acts as the preliminary step for a research project.
The research question formulated for this systematic review is as follows:
What is the prevalence of pressure ulcer among patients admitted to the acute ward?
Research aim
The main aim of the research is to determine the rates of prevalence of PU in acute
care units, by conducting a thorough and exhaustive search of available literature that are
relevant to the research question. This would help to explore the size of the health problem in
acute wards in hospitals and nursing homes, while taking into consideration the major
contributing factors of its development, specifically in the target population.
Research objective
Determine the prevalence of pressure ulcer in acute ward patients
Investigate the impacts of pressure ulcers in acute ward patients
Recognise the instruments that are used to classify PU status
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13MSC NURSING
Chapter 2:
Introduction
Methodology is a crucial chapter of dissertation. It helps the author to select the
optimal ways or the steps which will be important in conducting the research towards the
achievement of the research aims and objectives. According to Saunders and Rojon (2014),
research methodology mainly highlights the philosophy underlying specific research
approach. Chapter mainly aims to highlight the steps that the author will be using while
conducting thematic analysis of the systematic review of the qualitative research. The
approaches and the steps which are selected will be critically evaluated with detailed
justification behind the reason for selection and the strengths of that specific approach in
comparison to other research approaches.
The methodology of the systematic review will be based mainly be based on the
research question and the type and design of the overall study will be reflected throughput the
body of the systematic review and its methodology (Gough et al. 2017). As stated earlier in
the Introduction chapter, the main aim is to determine the rates of prevalence of PU in acute
care units. Therefore, in order to achieve the aim of the research, the author will follow
objective rather than highlighting subjective realities.
Qualitative research
The main mode of the study selected by the author for this systematic review was
qualitative research. Qualitative research deals with the study and understanding of the
complex phenomenon via thematic analysis. It initiates via observation and then collection of
data and thus helping to recognize the pattern of data (via themes) and thereby generating
new theories about the present phenomenon (Ross, 2012).
Chapter 2:
Introduction
Methodology is a crucial chapter of dissertation. It helps the author to select the
optimal ways or the steps which will be important in conducting the research towards the
achievement of the research aims and objectives. According to Saunders and Rojon (2014),
research methodology mainly highlights the philosophy underlying specific research
approach. Chapter mainly aims to highlight the steps that the author will be using while
conducting thematic analysis of the systematic review of the qualitative research. The
approaches and the steps which are selected will be critically evaluated with detailed
justification behind the reason for selection and the strengths of that specific approach in
comparison to other research approaches.
The methodology of the systematic review will be based mainly be based on the
research question and the type and design of the overall study will be reflected throughput the
body of the systematic review and its methodology (Gough et al. 2017). As stated earlier in
the Introduction chapter, the main aim is to determine the rates of prevalence of PU in acute
care units. Therefore, in order to achieve the aim of the research, the author will follow
objective rather than highlighting subjective realities.
Qualitative research
The main mode of the study selected by the author for this systematic review was
qualitative research. Qualitative research deals with the study and understanding of the
complex phenomenon via thematic analysis. It initiates via observation and then collection of
data and thus helping to recognize the pattern of data (via themes) and thereby generating
new theories about the present phenomenon (Ross, 2012).
14MSC NURSING
Research philosophy
The main research philosophy selected for the qualitative research is interpretivisim.
According to Bergh and Ketchen (2011), intrepretivism research philosophy is selected over
positivism research philosophy in qualitative research because it helps to provide in-depth
analysis of the small data via the use of themes.
Research approach
The research approach selected for this qualitative research is inductive research
approach. Inductive research approach helps in the generation of new theory from the
emerging information in comparison to deductive research approach which is based on the
existing theory (Crowther and Lancaster 2012). Inductive research approach will help the
research to compare the prevalence rate in pressure ulcers and this will help to generate new
theory on the occurrence of pressure ulcers in different body parts.
Research design
The researcher selected descriptive type research design for this qualitative research.
According to Ellis and Levy (2012), descriptive type research design helps in research to
describe the relationship between the cause and effect. This is best suited in comparison
explanatory and exploratory research design as these two research design do no provide
scope of comparative analysis.
Literature search
The first step of the qualitative methodology for systematic review is the search of the
literary articles in the electronic databases in an organised and in a methodological manner.
Searching article in an organised manner will help the researcher to highlight relevant yet
authentic studies which are already published online in esteemed scientific journals. The
search of the articles was conducted in the electronic databases via the use of keywords.
Research philosophy
The main research philosophy selected for the qualitative research is interpretivisim.
According to Bergh and Ketchen (2011), intrepretivism research philosophy is selected over
positivism research philosophy in qualitative research because it helps to provide in-depth
analysis of the small data via the use of themes.
Research approach
The research approach selected for this qualitative research is inductive research
approach. Inductive research approach helps in the generation of new theory from the
emerging information in comparison to deductive research approach which is based on the
existing theory (Crowther and Lancaster 2012). Inductive research approach will help the
research to compare the prevalence rate in pressure ulcers and this will help to generate new
theory on the occurrence of pressure ulcers in different body parts.
Research design
The researcher selected descriptive type research design for this qualitative research.
According to Ellis and Levy (2012), descriptive type research design helps in research to
describe the relationship between the cause and effect. This is best suited in comparison
explanatory and exploratory research design as these two research design do no provide
scope of comparative analysis.
Literature search
The first step of the qualitative methodology for systematic review is the search of the
literary articles in the electronic databases in an organised and in a methodological manner.
Searching article in an organised manner will help the researcher to highlight relevant yet
authentic studies which are already published online in esteemed scientific journals. The
search of the articles was conducted in the electronic databases via the use of keywords.
15MSC NURSING
Keywords
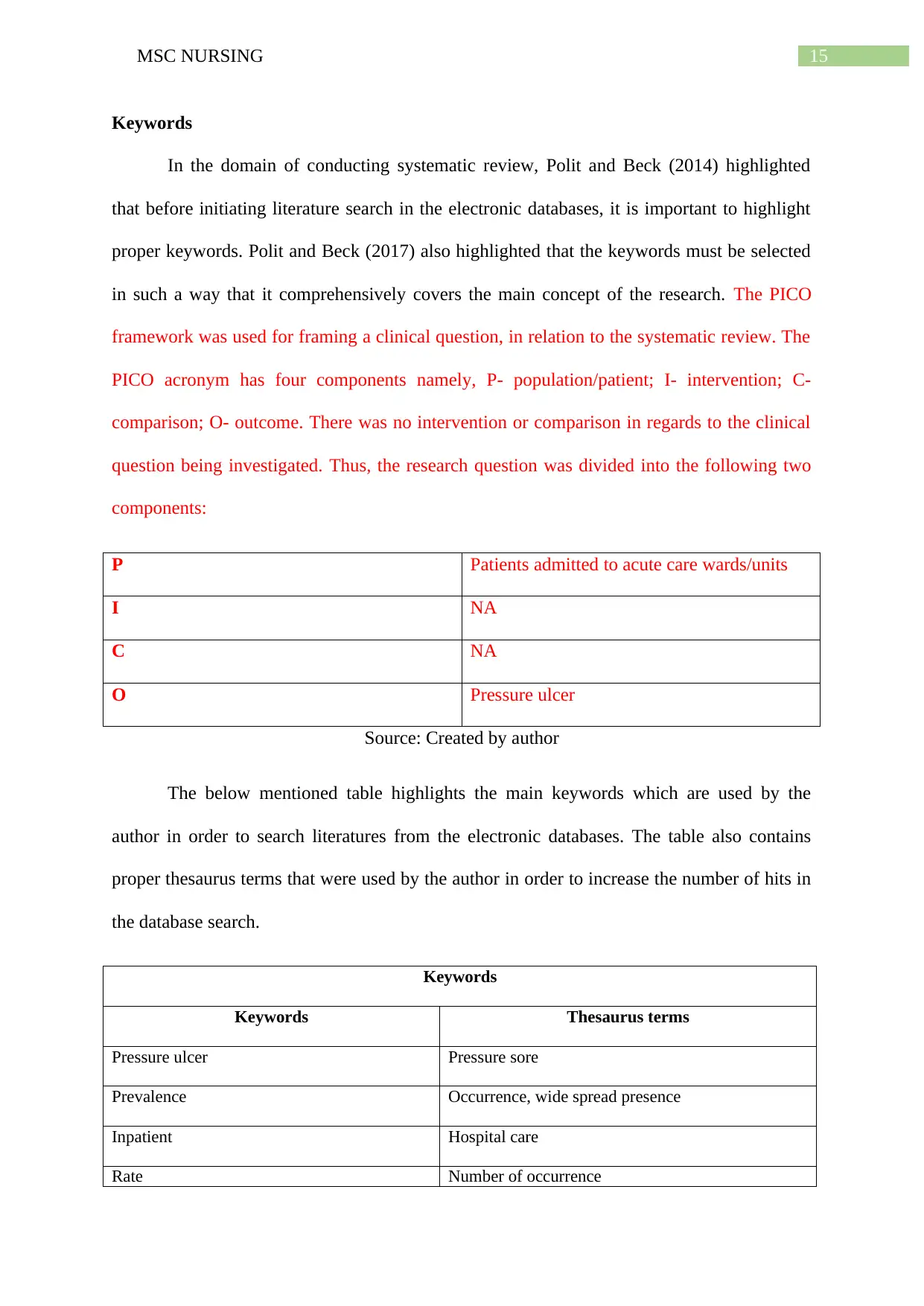
In the domain of conducting systematic review, Polit and Beck (2014) highlighted
that before initiating literature search in the electronic databases, it is important to highlight
proper keywords. Polit and Beck (2017) also highlighted that the keywords must be selected
in such a way that it comprehensively covers the main concept of the research. The PICO
framework was used for framing a clinical question, in relation to the systematic review. The
PICO acronym has four components namely, P- population/patient; I- intervention; C-
comparison; O- outcome. There was no intervention or comparison in regards to the clinical
question being investigated. Thus, the research question was divided into the following two
components:
P Patients admitted to acute care wards/units
I NA
C NA
O Pressure ulcer
Source: Created by author
The below mentioned table highlights the main keywords which are used by the
author in order to search literatures from the electronic databases. The table also contains
proper thesaurus terms that were used by the author in order to increase the number of hits in
the database search.
Keywords
Keywords Thesaurus terms
Pressure ulcer Pressure sore
Prevalence Occurrence, wide spread presence
Inpatient Hospital care
Rate Number of occurrence
Keywords
In the domain of conducting systematic review, Polit and Beck (2014) highlighted
that before initiating literature search in the electronic databases, it is important to highlight
proper keywords. Polit and Beck (2017) also highlighted that the keywords must be selected
in such a way that it comprehensively covers the main concept of the research. The PICO
framework was used for framing a clinical question, in relation to the systematic review. The
PICO acronym has four components namely, P- population/patient; I- intervention; C-
comparison; O- outcome. There was no intervention or comparison in regards to the clinical
question being investigated. Thus, the research question was divided into the following two
components:
P Patients admitted to acute care wards/units
I NA
C NA
O Pressure ulcer
Source: Created by author
The below mentioned table highlights the main keywords which are used by the
author in order to search literatures from the electronic databases. The table also contains
proper thesaurus terms that were used by the author in order to increase the number of hits in
the database search.
Keywords
Keywords Thesaurus terms
Pressure ulcer Pressure sore
Prevalence Occurrence, wide spread presence
Inpatient Hospital care
Rate Number of occurrence
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
16MSC NURSING
Hospital Clinic, nursing home
Source: Created by author
Bibliographic Aids
According to Parahoo (2014), search of the literature is important in order to avail
quick access to the information related to the research questions which are available online.
The main medium selected for the collection of data includes online databases. Preliminary
search of the relevant research articles were done via the use of the electronic databases like
PubMed, MEDLINE, Cochrane and Ovid Full Text Nursing Plus and Cinhal. These specific
electronic databases were selected for the search of the literary articles because the articles
presented in these databases are mostly associated with the scope of the systematic review.
According to Parahoo (2014), before initiating a systematic review of literature, it is crucial
important to conduct a detailed search of the literary articles which are available online as
reviews or meta-analysis or narrative review. This helps to mitigate the chances of getting
duplicate work and thereby helping to make a novel research question. By taking this concept
into consideration, the author conducted the search of literary articles in Cochrane Database
for Systematic Review with the keywords which are highlighted in the above mentioned
table. The search of the articles provided negative or zero hits. This signifies that there are no
other reviews based on the presence of pressure ulcers which are published online in the form
of systematic review. According to Holloway and Wheeler (2010) conducting a preliminary
search in the Cochrane databases helps to highlight the research gap and thereby helping to
figure out a novel research questions with an unique research approach.
Hospital Clinic, nursing home
Source: Created by author
Bibliographic Aids
According to Parahoo (2014), search of the literature is important in order to avail
quick access to the information related to the research questions which are available online.
The main medium selected for the collection of data includes online databases. Preliminary
search of the relevant research articles were done via the use of the electronic databases like
PubMed, MEDLINE, Cochrane and Ovid Full Text Nursing Plus and Cinhal. These specific
electronic databases were selected for the search of the literary articles because the articles
presented in these databases are mostly associated with the scope of the systematic review.
According to Parahoo (2014), before initiating a systematic review of literature, it is crucial
important to conduct a detailed search of the literary articles which are available online as
reviews or meta-analysis or narrative review. This helps to mitigate the chances of getting
duplicate work and thereby helping to make a novel research question. By taking this concept
into consideration, the author conducted the search of literary articles in Cochrane Database
for Systematic Review with the keywords which are highlighted in the above mentioned
table. The search of the articles provided negative or zero hits. This signifies that there are no
other reviews based on the presence of pressure ulcers which are published online in the form
of systematic review. According to Holloway and Wheeler (2010) conducting a preliminary
search in the Cochrane databases helps to highlight the research gap and thereby helping to
figure out a novel research questions with an unique research approach.
17MSC NURSING
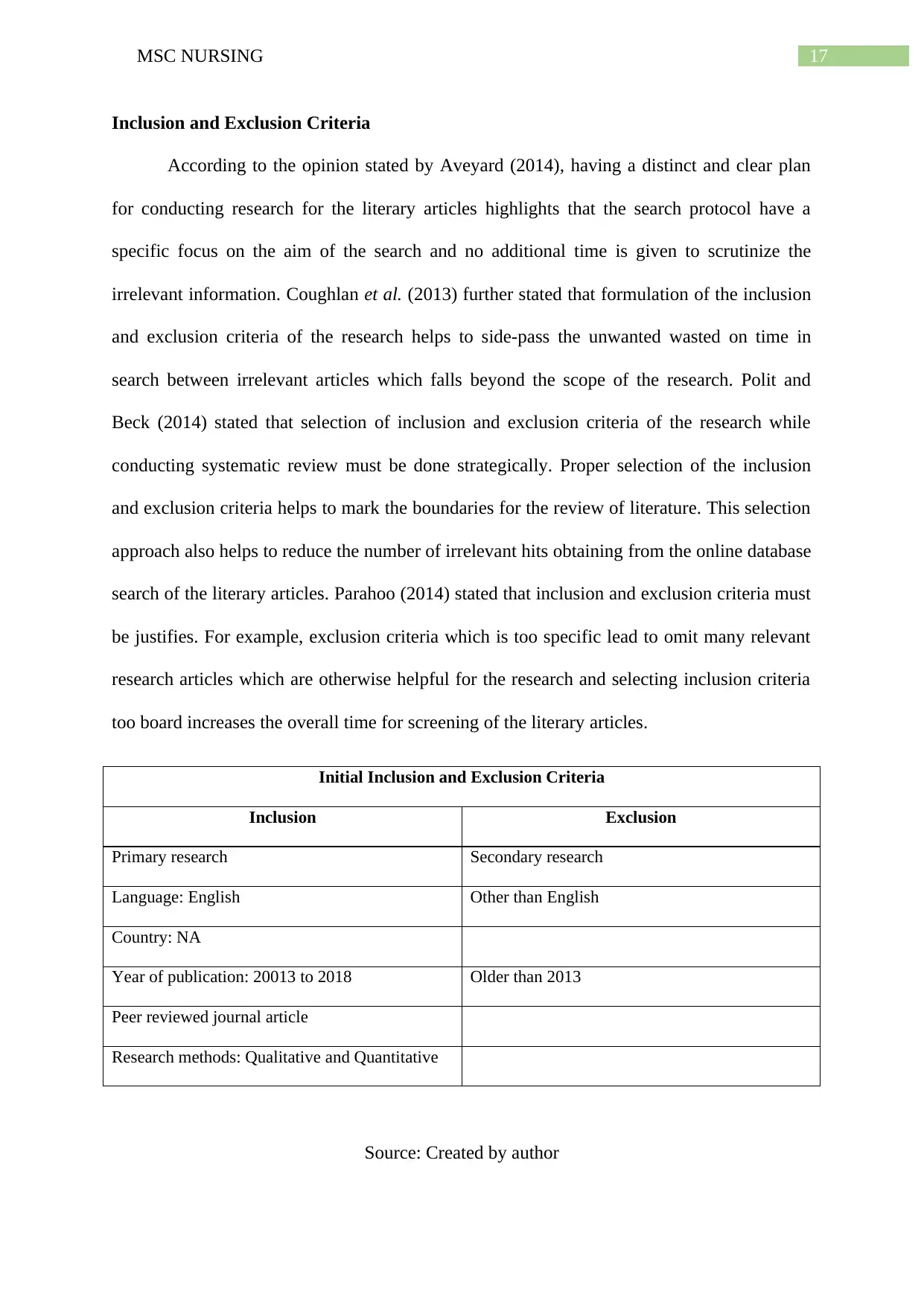
Inclusion and Exclusion Criteria
According to the opinion stated by Aveyard (2014), having a distinct and clear plan
for conducting research for the literary articles highlights that the search protocol have a
specific focus on the aim of the search and no additional time is given to scrutinize the
irrelevant information. Coughlan et al. (2013) further stated that formulation of the inclusion
and exclusion criteria of the research helps to side-pass the unwanted wasted on time in
search between irrelevant articles which falls beyond the scope of the research. Polit and
Beck (2014) stated that selection of inclusion and exclusion criteria of the research while
conducting systematic review must be done strategically. Proper selection of the inclusion
and exclusion criteria helps to mark the boundaries for the review of literature. This selection
approach also helps to reduce the number of irrelevant hits obtaining from the online database
search of the literary articles. Parahoo (2014) stated that inclusion and exclusion criteria must
be justifies. For example, exclusion criteria which is too specific lead to omit many relevant
research articles which are otherwise helpful for the research and selecting inclusion criteria
too board increases the overall time for screening of the literary articles.
Initial Inclusion and Exclusion Criteria
Inclusion Exclusion
Primary research Secondary research
Language: English Other than English
Country: NA
Year of publication: 20013 to 2018 Older than 2013
Peer reviewed journal article
Research methods: Qualitative and Quantitative
Source: Created by author
Inclusion and Exclusion Criteria
According to the opinion stated by Aveyard (2014), having a distinct and clear plan
for conducting research for the literary articles highlights that the search protocol have a
specific focus on the aim of the search and no additional time is given to scrutinize the
irrelevant information. Coughlan et al. (2013) further stated that formulation of the inclusion
and exclusion criteria of the research helps to side-pass the unwanted wasted on time in
search between irrelevant articles which falls beyond the scope of the research. Polit and
Beck (2014) stated that selection of inclusion and exclusion criteria of the research while
conducting systematic review must be done strategically. Proper selection of the inclusion
and exclusion criteria helps to mark the boundaries for the review of literature. This selection
approach also helps to reduce the number of irrelevant hits obtaining from the online database
search of the literary articles. Parahoo (2014) stated that inclusion and exclusion criteria must
be justifies. For example, exclusion criteria which is too specific lead to omit many relevant
research articles which are otherwise helpful for the research and selecting inclusion criteria
too board increases the overall time for screening of the literary articles.
Initial Inclusion and Exclusion Criteria
Inclusion Exclusion
Primary research Secondary research
Language: English Other than English
Country: NA
Year of publication: 20013 to 2018 Older than 2013
Peer reviewed journal article
Research methods: Qualitative and Quantitative
Source: Created by author
18MSC NURSING
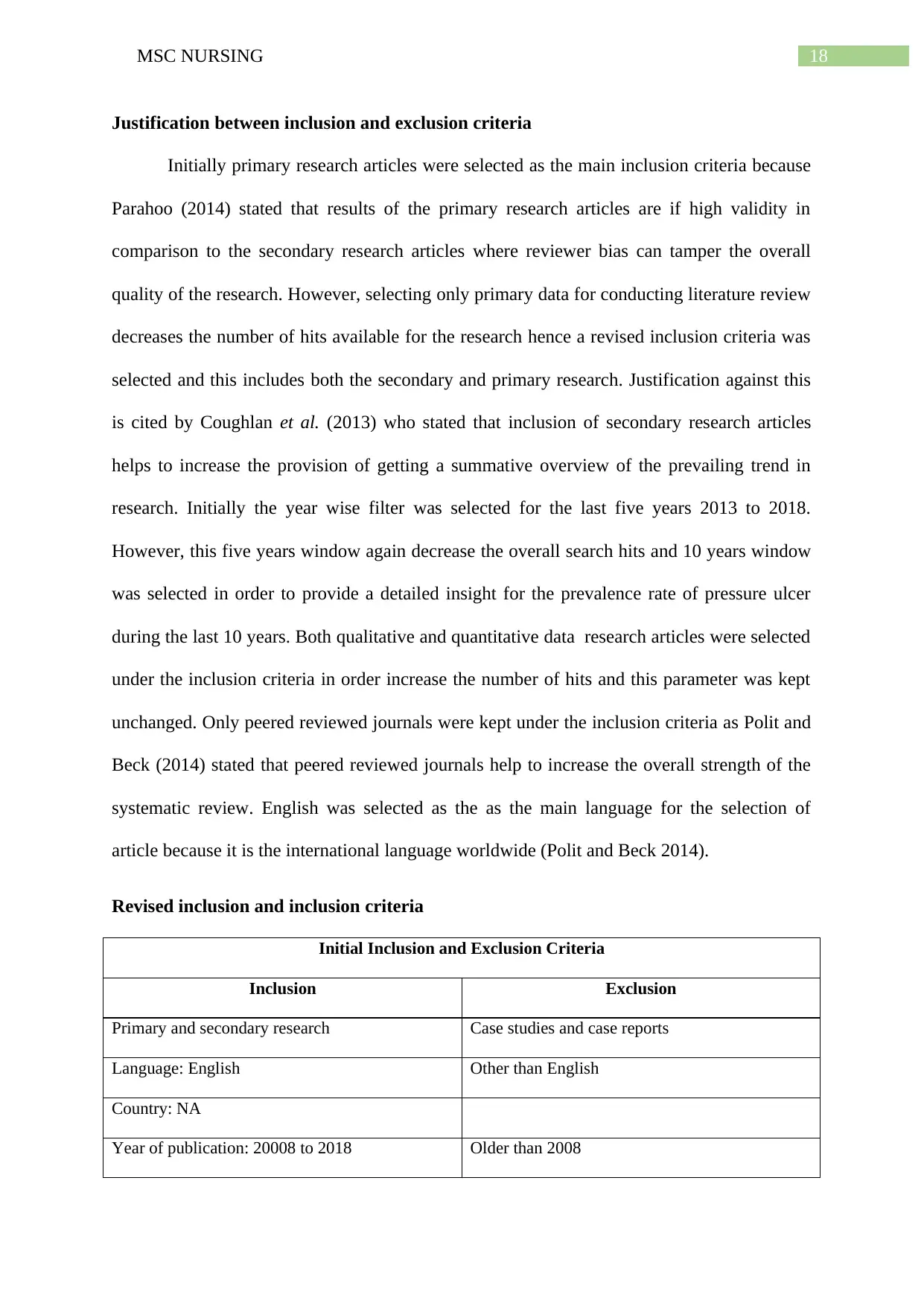
Justification between inclusion and exclusion criteria
Initially primary research articles were selected as the main inclusion criteria because
Parahoo (2014) stated that results of the primary research articles are if high validity in
comparison to the secondary research articles where reviewer bias can tamper the overall
quality of the research. However, selecting only primary data for conducting literature review
decreases the number of hits available for the research hence a revised inclusion criteria was
selected and this includes both the secondary and primary research. Justification against this
is cited by Coughlan et al. (2013) who stated that inclusion of secondary research articles
helps to increase the provision of getting a summative overview of the prevailing trend in
research. Initially the year wise filter was selected for the last five years 2013 to 2018.
However, this five years window again decrease the overall search hits and 10 years window
was selected in order to provide a detailed insight for the prevalence rate of pressure ulcer
during the last 10 years. Both qualitative and quantitative data research articles were selected
under the inclusion criteria in order increase the number of hits and this parameter was kept
unchanged. Only peered reviewed journals were kept under the inclusion criteria as Polit and
Beck (2014) stated that peered reviewed journals help to increase the overall strength of the
systematic review. English was selected as the as the main language for the selection of
article because it is the international language worldwide (Polit and Beck 2014).
Revised inclusion and inclusion criteria
Initial Inclusion and Exclusion Criteria
Inclusion Exclusion
Primary and secondary research Case studies and case reports
Language: English Other than English
Country: NA
Year of publication: 20008 to 2018 Older than 2008
Justification between inclusion and exclusion criteria
Initially primary research articles were selected as the main inclusion criteria because
Parahoo (2014) stated that results of the primary research articles are if high validity in
comparison to the secondary research articles where reviewer bias can tamper the overall
quality of the research. However, selecting only primary data for conducting literature review
decreases the number of hits available for the research hence a revised inclusion criteria was
selected and this includes both the secondary and primary research. Justification against this
is cited by Coughlan et al. (2013) who stated that inclusion of secondary research articles
helps to increase the provision of getting a summative overview of the prevailing trend in
research. Initially the year wise filter was selected for the last five years 2013 to 2018.
However, this five years window again decrease the overall search hits and 10 years window
was selected in order to provide a detailed insight for the prevalence rate of pressure ulcer
during the last 10 years. Both qualitative and quantitative data research articles were selected
under the inclusion criteria in order increase the number of hits and this parameter was kept
unchanged. Only peered reviewed journals were kept under the inclusion criteria as Polit and
Beck (2014) stated that peered reviewed journals help to increase the overall strength of the
systematic review. English was selected as the as the main language for the selection of
article because it is the international language worldwide (Polit and Beck 2014).
Revised inclusion and inclusion criteria
Initial Inclusion and Exclusion Criteria
Inclusion Exclusion
Primary and secondary research Case studies and case reports
Language: English Other than English
Country: NA
Year of publication: 20008 to 2018 Older than 2008
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
19MSC NURSING
Peer reviewed journal article
Research methods: Qualitative and Quantitative
Source: Created by author
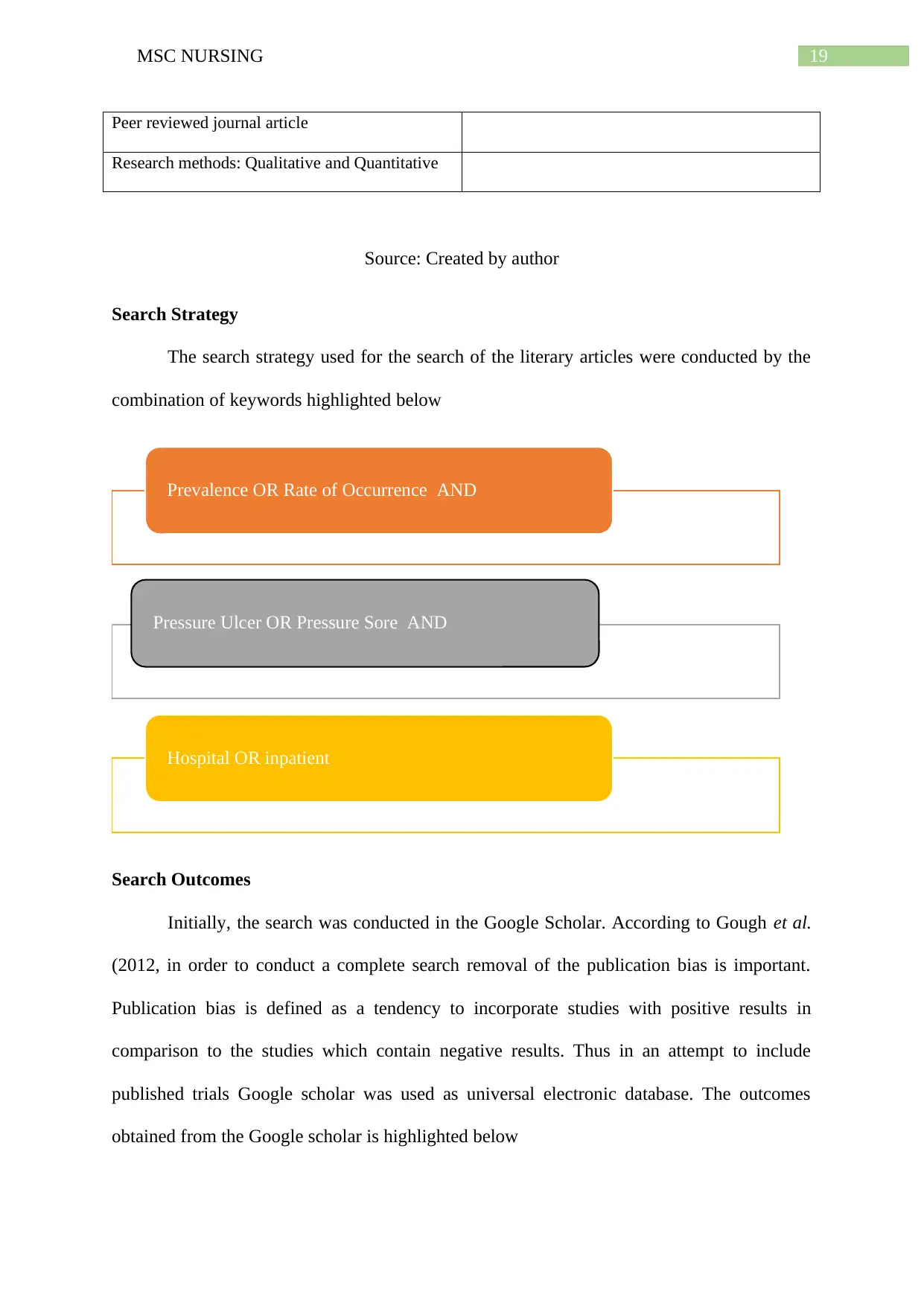
Search Strategy
The search strategy used for the search of the literary articles were conducted by the
combination of keywords highlighted below
Search Outcomes
Initially, the search was conducted in the Google Scholar. According to Gough et al.
(2012, in order to conduct a complete search removal of the publication bias is important.
Publication bias is defined as a tendency to incorporate studies with positive results in
comparison to the studies which contain negative results. Thus in an attempt to include
published trials Google scholar was used as universal electronic database. The outcomes
obtained from the Google scholar is highlighted below
Prevalence OR Rate of Occurrence AND
Pressure Ulcer OR Pressure Sore AND
Hospital OR inpatient
Peer reviewed journal article
Research methods: Qualitative and Quantitative
Source: Created by author
Search Strategy
The search strategy used for the search of the literary articles were conducted by the
combination of keywords highlighted below
Search Outcomes
Initially, the search was conducted in the Google Scholar. According to Gough et al.
(2012, in order to conduct a complete search removal of the publication bias is important.
Publication bias is defined as a tendency to incorporate studies with positive results in
comparison to the studies which contain negative results. Thus in an attempt to include
published trials Google scholar was used as universal electronic database. The outcomes
obtained from the Google scholar is highlighted below
Prevalence OR Rate of Occurrence AND
Pressure Ulcer OR Pressure Sore AND
Hospital OR inpatient
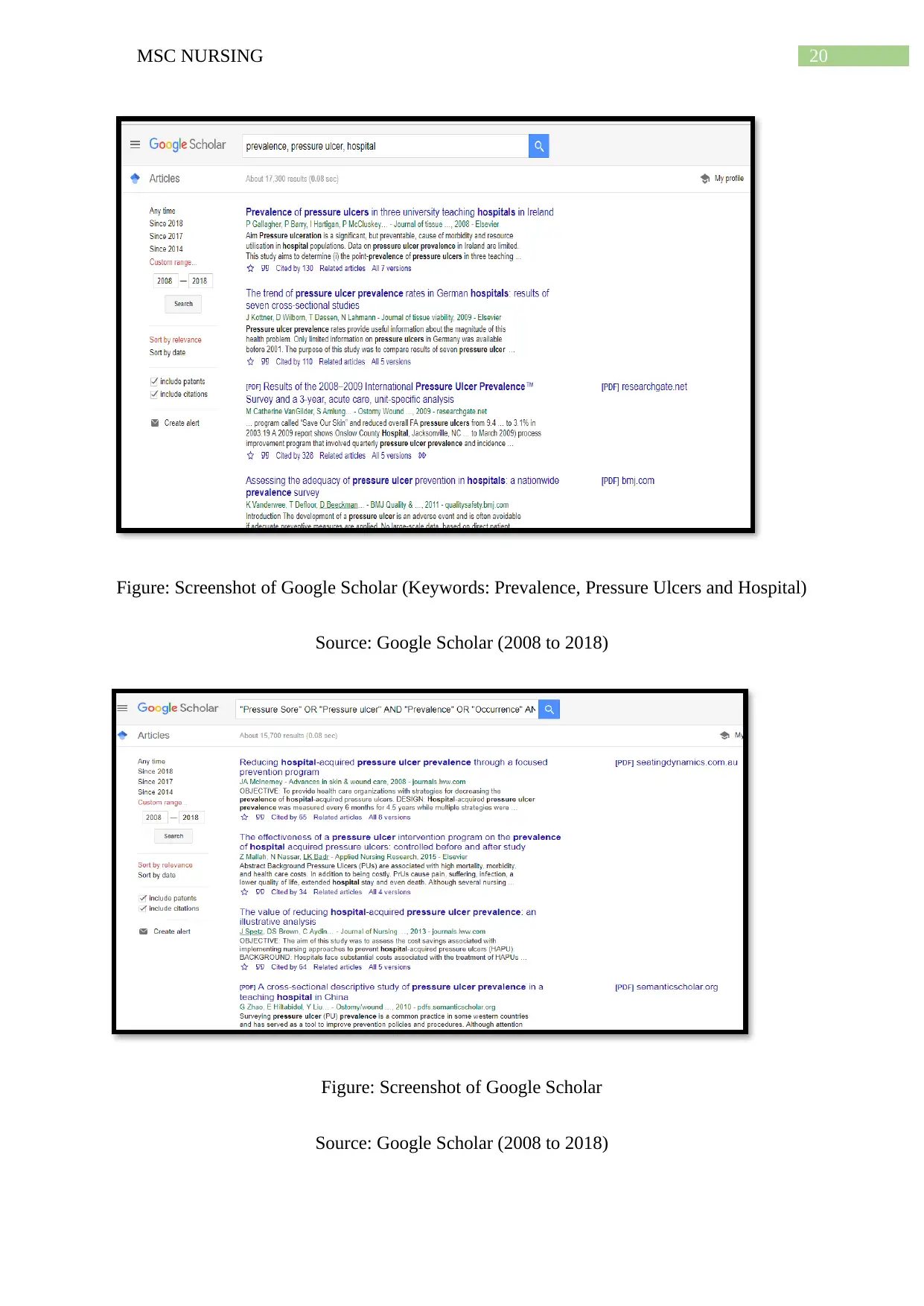
20MSC NURSING
Figure: Screenshot of Google Scholar (Keywords: Prevalence, Pressure Ulcers and Hospital)
Source: Google Scholar (2008 to 2018)
Figure: Screenshot of Google Scholar
Source: Google Scholar (2008 to 2018)
Figure: Screenshot of Google Scholar (Keywords: Prevalence, Pressure Ulcers and Hospital)
Source: Google Scholar (2008 to 2018)
Figure: Screenshot of Google Scholar
Source: Google Scholar (2008 to 2018)
21MSC NURSING
The number of hits obtained from the broad keyword search (Keywords: Prevalence,
Pressure Ulcers and Hospital) were 17,300 hits. The number of hits obtained via specific
search results with quotes (“”) and via the use of Boolean search indicators (Keywords
combination: "Pressure Sore" OR "Pressure ulcer" AND "Prevalence" OR "Occurrence"
AND "Hospital" OR "inpatient" were 15,700 (time frame 2008 to 2018). Thus it can be said
that the outcome obtained from Google Scholar was huge and this indicated that there were
gamut literature published online which coincided with the scope of the research question
drafted from the systematic review. However, accessing gamut data manually was not
feasible. So in order to stringent the search further electronic databases were used. Betanny-
Saltikiv (2012) highlighted that this kind of approach promotes further refinement in the
literature search. Use of the limiters as indicated by the inclusion and exclusion criteria and
the use of Boolean operators helped to obtained specific search.
According to Robband Shellenbarger (2014), use of Boolean operators is important in
order to establish relationship with the keywords. In this systematic review, two types of
Boolean operators were used by the researcher and these are AND/PR. The use of Boolean
operators like AND/OR helps to obtain combination of different keywords (Polit and Beck
2014). Moreover, use of Boolean operators also assisted the researcher to save potential time
via reducing the number of obtained hits. The search results obtained via Boolean operators
are limited and this assisted the author to scrutinise the relevancy of the search results
obtained manually.
Snowball Technique
The hits obtained via search of the articles in the electronic databases are
comprehensive as they are updated regularly. However, while conductive systematic review
of literature, it is important to use numerous other alternative methods for the search of the
literary articles. Aveyard (2014) highlighted that using electronic databases for the search of
The number of hits obtained from the broad keyword search (Keywords: Prevalence,
Pressure Ulcers and Hospital) were 17,300 hits. The number of hits obtained via specific
search results with quotes (“”) and via the use of Boolean search indicators (Keywords
combination: "Pressure Sore" OR "Pressure ulcer" AND "Prevalence" OR "Occurrence"
AND "Hospital" OR "inpatient" were 15,700 (time frame 2008 to 2018). Thus it can be said
that the outcome obtained from Google Scholar was huge and this indicated that there were
gamut literature published online which coincided with the scope of the research question
drafted from the systematic review. However, accessing gamut data manually was not
feasible. So in order to stringent the search further electronic databases were used. Betanny-
Saltikiv (2012) highlighted that this kind of approach promotes further refinement in the
literature search. Use of the limiters as indicated by the inclusion and exclusion criteria and
the use of Boolean operators helped to obtained specific search.
According to Robband Shellenbarger (2014), use of Boolean operators is important in
order to establish relationship with the keywords. In this systematic review, two types of
Boolean operators were used by the researcher and these are AND/PR. The use of Boolean
operators like AND/OR helps to obtain combination of different keywords (Polit and Beck
2014). Moreover, use of Boolean operators also assisted the researcher to save potential time
via reducing the number of obtained hits. The search results obtained via Boolean operators
are limited and this assisted the author to scrutinise the relevancy of the search results
obtained manually.
Snowball Technique
The hits obtained via search of the articles in the electronic databases are
comprehensive as they are updated regularly. However, while conductive systematic review
of literature, it is important to use numerous other alternative methods for the search of the
literary articles. Aveyard (2014) highlighted that using electronic databases for the search of
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
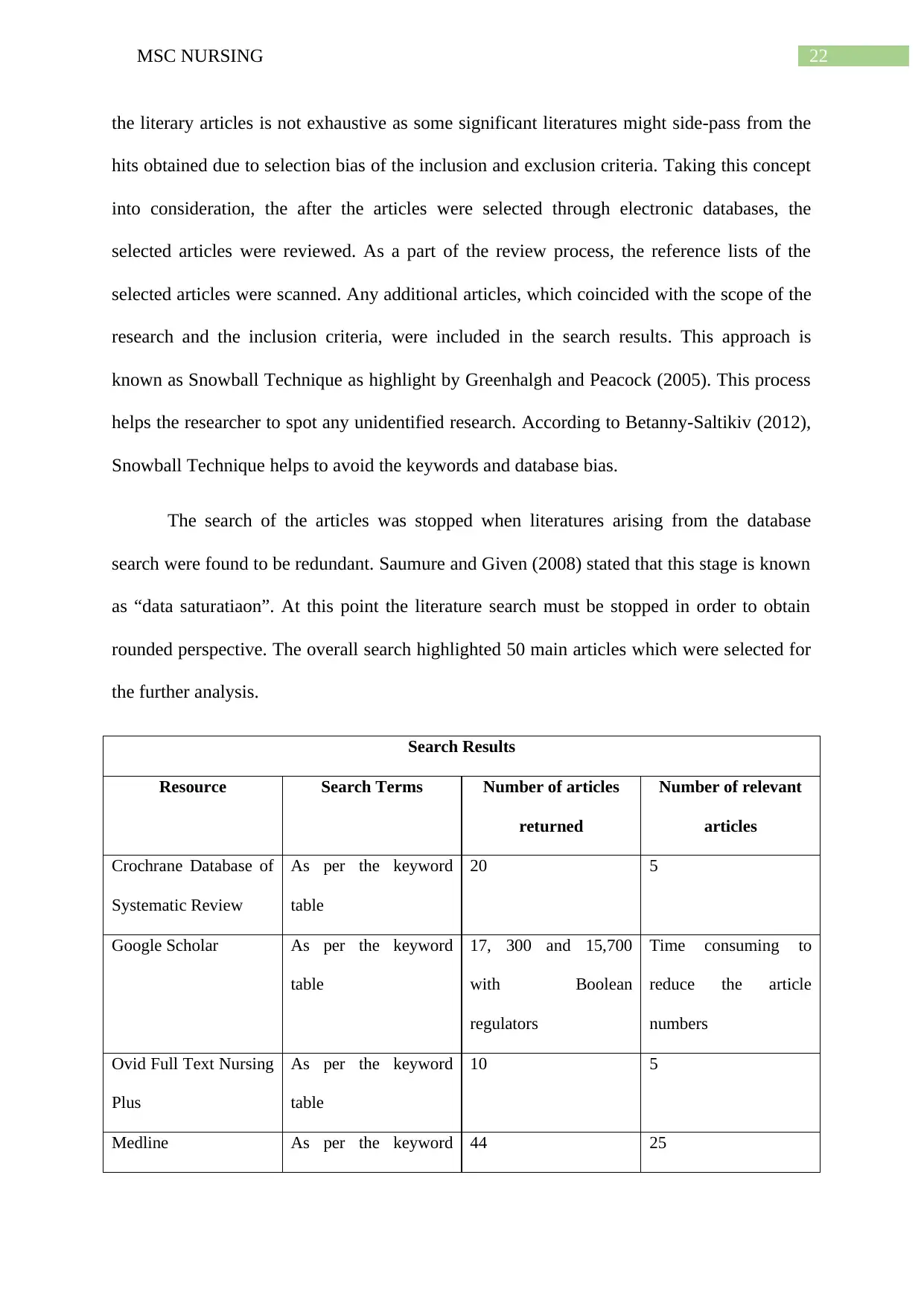
22MSC NURSING
the literary articles is not exhaustive as some significant literatures might side-pass from the
hits obtained due to selection bias of the inclusion and exclusion criteria. Taking this concept
into consideration, the after the articles were selected through electronic databases, the
selected articles were reviewed. As a part of the review process, the reference lists of the
selected articles were scanned. Any additional articles, which coincided with the scope of the
research and the inclusion criteria, were included in the search results. This approach is
known as Snowball Technique as highlight by Greenhalgh and Peacock (2005). This process
helps the researcher to spot any unidentified research. According to Betanny-Saltikiv (2012),
Snowball Technique helps to avoid the keywords and database bias.
The search of the articles was stopped when literatures arising from the database
search were found to be redundant. Saumure and Given (2008) stated that this stage is known
as “data saturatiaon”. At this point the literature search must be stopped in order to obtain
rounded perspective. The overall search highlighted 50 main articles which were selected for
the further analysis.
Search Results
Resource Search Terms Number of articles
returned
Number of relevant
articles
Crochrane Database of
Systematic Review
As per the keyword
table
20 5
Google Scholar As per the keyword
table
17, 300 and 15,700
with Boolean
regulators
Time consuming to
reduce the article
numbers
Ovid Full Text Nursing
Plus
As per the keyword
table
10 5
Medline As per the keyword 44 25
the literary articles is not exhaustive as some significant literatures might side-pass from the
hits obtained due to selection bias of the inclusion and exclusion criteria. Taking this concept
into consideration, the after the articles were selected through electronic databases, the
selected articles were reviewed. As a part of the review process, the reference lists of the
selected articles were scanned. Any additional articles, which coincided with the scope of the
research and the inclusion criteria, were included in the search results. This approach is
known as Snowball Technique as highlight by Greenhalgh and Peacock (2005). This process
helps the researcher to spot any unidentified research. According to Betanny-Saltikiv (2012),
Snowball Technique helps to avoid the keywords and database bias.
The search of the articles was stopped when literatures arising from the database
search were found to be redundant. Saumure and Given (2008) stated that this stage is known
as “data saturatiaon”. At this point the literature search must be stopped in order to obtain
rounded perspective. The overall search highlighted 50 main articles which were selected for
the further analysis.
Search Results
Resource Search Terms Number of articles
returned
Number of relevant
articles
Crochrane Database of
Systematic Review
As per the keyword
table
20 5
Google Scholar As per the keyword
table
17, 300 and 15,700
with Boolean
regulators
Time consuming to
reduce the article
numbers
Ovid Full Text Nursing
Plus
As per the keyword
table
10 5
Medline As per the keyword 44 25
23MSC NURSING
table
Cinhal As per the keyword
table
30 10
Snowballing 10
Quality Assessment
Quality Assessment was done in an ordered manner. The quality assessment was
initiated via the removal of the duplicates from the search results. After
removal of the duplicates, selected 50 articles were reviewed on the basis of their title.
Parahoo (2014) highlighted that title of the literature should be considered perfect if it clearly
describes aim to the study and study approach. The title of the articles which failed to satisfy
these criteria was excluded from the research. The total number of articles which are obtained
after the title scrutiny was 30. These 30 articles were scanned on the basis of their abstract
and filtered out 17 odd articles. The rest articles were analysed full-text. In the full-text
analysis, the selection bias, confounding bias, allocation bias and reporting bias along with
sample size were taken into detailed notice. Of them confounding bias is of prime
importance. Confounding bias generates when the nature of the participants both
experimental and placebo or the control and the intervention groups are not identical at the
time of selection. Confounding generally rise when another factor produces observed
outcome rather than the investigated scope of the study. According to Parahoo (2014), poor
sample size results in generating biased results. The full-text analysis highlighted 12 articles
which were included in the final systematic review. Quality assessment however,
fails to in-corporate source bias. It mainly analysed whether the design of
the study aligns with the purpose of the study purpose and whether the
table
Cinhal As per the keyword
table
30 10
Snowballing 10
Quality Assessment
Quality Assessment was done in an ordered manner. The quality assessment was
initiated via the removal of the duplicates from the search results. After
removal of the duplicates, selected 50 articles were reviewed on the basis of their title.
Parahoo (2014) highlighted that title of the literature should be considered perfect if it clearly
describes aim to the study and study approach. The title of the articles which failed to satisfy
these criteria was excluded from the research. The total number of articles which are obtained
after the title scrutiny was 30. These 30 articles were scanned on the basis of their abstract
and filtered out 17 odd articles. The rest articles were analysed full-text. In the full-text
analysis, the selection bias, confounding bias, allocation bias and reporting bias along with
sample size were taken into detailed notice. Of them confounding bias is of prime
importance. Confounding bias generates when the nature of the participants both
experimental and placebo or the control and the intervention groups are not identical at the
time of selection. Confounding generally rise when another factor produces observed
outcome rather than the investigated scope of the study. According to Parahoo (2014), poor
sample size results in generating biased results. The full-text analysis highlighted 12 articles
which were included in the final systematic review. Quality assessment however,
fails to in-corporate source bias. It mainly analysed whether the design of
the study aligns with the purpose of the study purpose and whether the
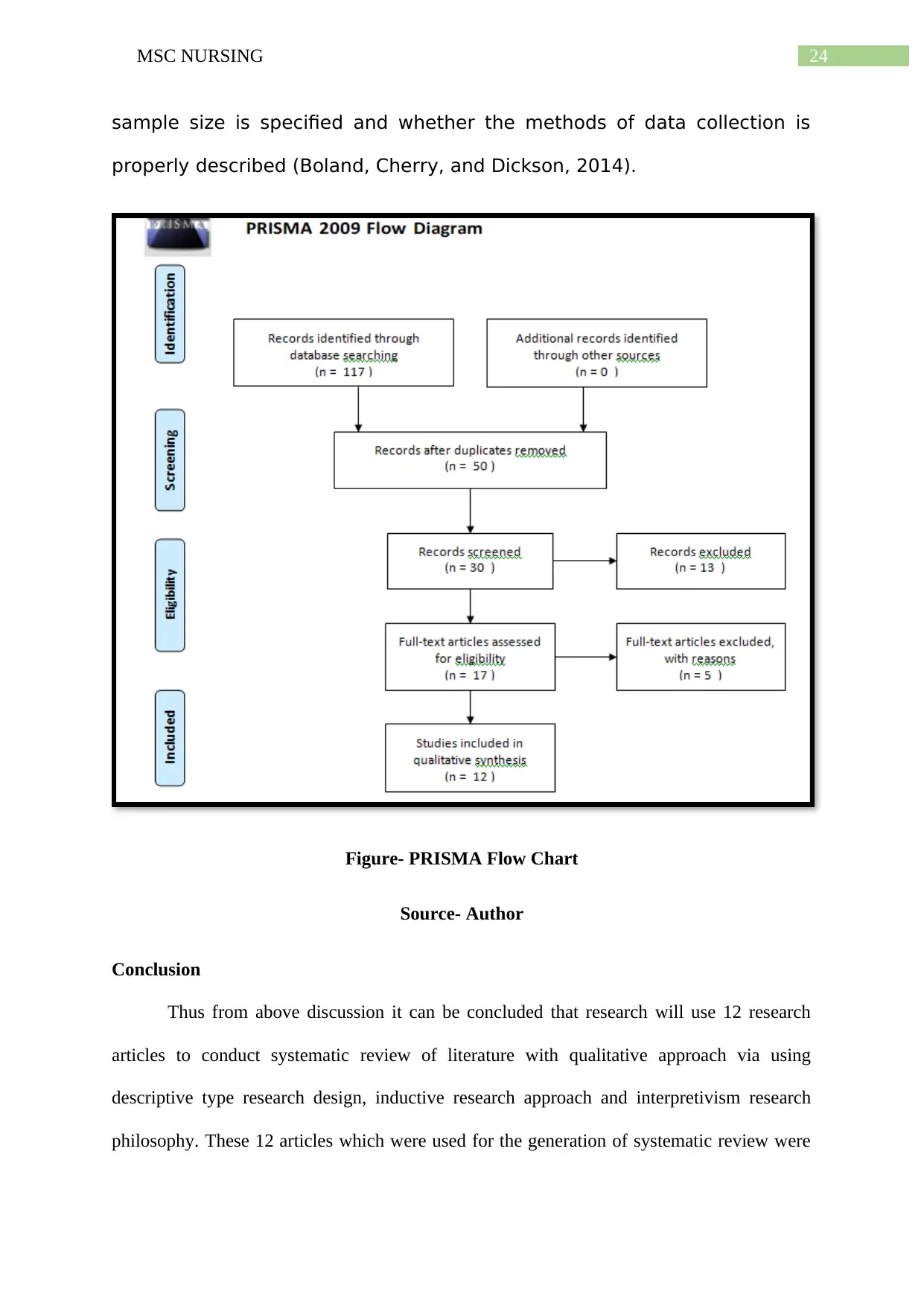
24MSC NURSING
sample size is specified and whether the methods of data collection is
properly described (Boland, Cherry, and Dickson, 2014).
Figure- PRISMA Flow Chart
Source- Author
Conclusion
Thus from above discussion it can be concluded that research will use 12 research
articles to conduct systematic review of literature with qualitative approach via using
descriptive type research design, inductive research approach and interpretivism research
philosophy. These 12 articles which were used for the generation of systematic review were
sample size is specified and whether the methods of data collection is
properly described (Boland, Cherry, and Dickson, 2014).
Figure- PRISMA Flow Chart
Source- Author
Conclusion
Thus from above discussion it can be concluded that research will use 12 research
articles to conduct systematic review of literature with qualitative approach via using
descriptive type research design, inductive research approach and interpretivism research
philosophy. These 12 articles which were used for the generation of systematic review were
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

25MSC NURSING
selected from the esteemed electronic databases via the use of proper keywords along with
inclusion and exclusion criteria.
selected from the esteemed electronic databases via the use of proper keywords along with
inclusion and exclusion criteria.
26MSC NURSING
Chapter 3:
Despite the mounting evidence of literature which have investigated the underlying
factors that contribute to pressure ulcer (PU) among patients, admitted to acute wards and
significance of PU, the health event is a matter of major concern. This chapter on literature
review aims to scrutinize all the available evidences that represent substantial data on the
prevalence of PU in critical care units, across different hospitals. The prime objective of the
literature review is to recognise, evaluate and combine accessible knowledge that is produced
by rigorous scientific research. Literature review is often termed as ‘research done on
research’, with the aim of providing an overview and drawing conclusions from the
obtainable findings.Hence, conduction of a literature review serves an essential platform for
future research prospects. This literature review was conducted in the form of a systematic
review. The procedure refers to the rapid collection of literature in relation to a certain
clinical area (pressure ulcer prevalence), or a given policy. The primary aim of the review
was to accumulate as much data as possible, and map results related to prevalence of the
condition accordingly. This review was conducted based on a methodological
framework(Treadwell et al. 2011).
Such a review comprises of different stages of data collection and assimilation. While
the primary aim of stage 1 is to clarify the objective and purpose, thus linking the research
question with them, stage 2 helps in balancing feasibility of the study with the richness and
breadth of the entire process. An iterative technique was employed in stage 3 for selecting
studies that were appropriate to the research question. This was conducted in a way that any
other person undertaking the same selection would possibly end up with similar results.
Stage4 comprised of data collection,followed by thematic analysis in stage 5. This was
followed by taking into consideration the implications of the research findings to medicine
practice and health care policies. The search process was entirely based on the research
Chapter 3:
Despite the mounting evidence of literature which have investigated the underlying
factors that contribute to pressure ulcer (PU) among patients, admitted to acute wards and
significance of PU, the health event is a matter of major concern. This chapter on literature
review aims to scrutinize all the available evidences that represent substantial data on the
prevalence of PU in critical care units, across different hospitals. The prime objective of the
literature review is to recognise, evaluate and combine accessible knowledge that is produced
by rigorous scientific research. Literature review is often termed as ‘research done on
research’, with the aim of providing an overview and drawing conclusions from the
obtainable findings.Hence, conduction of a literature review serves an essential platform for
future research prospects. This literature review was conducted in the form of a systematic
review. The procedure refers to the rapid collection of literature in relation to a certain
clinical area (pressure ulcer prevalence), or a given policy. The primary aim of the review
was to accumulate as much data as possible, and map results related to prevalence of the
condition accordingly. This review was conducted based on a methodological
framework(Treadwell et al. 2011).
Such a review comprises of different stages of data collection and assimilation. While
the primary aim of stage 1 is to clarify the objective and purpose, thus linking the research
question with them, stage 2 helps in balancing feasibility of the study with the richness and
breadth of the entire process. An iterative technique was employed in stage 3 for selecting
studies that were appropriate to the research question. This was conducted in a way that any
other person undertaking the same selection would possibly end up with similar results.
Stage4 comprised of data collection,followed by thematic analysis in stage 5. This was
followed by taking into consideration the implications of the research findings to medicine
practice and health care policies. The search process was entirely based on the research
27MSC NURSING
question and was plannedin careful manner. The essential problem of subject that was
intended to be investigated was defined initially, followed by identification of the key
concepts such as,‘pressure ulcer’,‘prevalence’,‘incidence’, ‘rate’, ‘hospital’. This was
followed by selection of suitable electronic databases and performing the search process.
Below given are the initial results of the studies that were evaluated based on their quality,
reliability, and relevance to the research question:
A retrospective study had been conducted to investigate the prevalence of PU across
Dutch general hospitals, since the year 2001. The primary objective of the researchers was to
investigate the impact of different factors such as, prevention strategies of PU, patient
characteristics, and structural quality indicators that were implemented by hospital wards and
institutions for an apparent reduction in the prevalence rate of the condition from 2001-2008.
The researchers collected data from the Dutch National Prevalence Survey of Care Problems
(Also referred to as the LPZ database) from the year 2001 to 2008, with the aim of exploring
the existing variations in characteristics of patients, the prevention strategies and the
indicators. Health indicators wereassessedduring two different time periods namely 2005-
2008, wherePU was evaluated as an external health quality indicator and during 2001-2004,
where it functioned as an internal indicator. Upon comparing the results from 2001-2004, the
authors found that there were fewer participants who reported hemiparesis/CVA (OR 0.485),
surgery that lasted more than 2 hours (OR 0.637), infectious or contagious diseases (OR
0.861), and those who were at risk for Braden scale scores (OR 0.844). However, high
prevalence was found for patients who reported diabetes mellitus (OR 1.693), corresponding
to the 2005-2008 group. On comparing the results, the researchers also found that the hospital
wards required more special mattresses or beds (OR 2.216) and specialised questions that
were attached to wheelchairs (OR 2.277) during the second time period (2005-2008). This
second time frame was also supported by an increase in information related to repositioning
question and was plannedin careful manner. The essential problem of subject that was
intended to be investigated was defined initially, followed by identification of the key
concepts such as,‘pressure ulcer’,‘prevalence’,‘incidence’, ‘rate’, ‘hospital’. This was
followed by selection of suitable electronic databases and performing the search process.
Below given are the initial results of the studies that were evaluated based on their quality,
reliability, and relevance to the research question:
A retrospective study had been conducted to investigate the prevalence of PU across
Dutch general hospitals, since the year 2001. The primary objective of the researchers was to
investigate the impact of different factors such as, prevention strategies of PU, patient
characteristics, and structural quality indicators that were implemented by hospital wards and
institutions for an apparent reduction in the prevalence rate of the condition from 2001-2008.
The researchers collected data from the Dutch National Prevalence Survey of Care Problems
(Also referred to as the LPZ database) from the year 2001 to 2008, with the aim of exploring
the existing variations in characteristics of patients, the prevention strategies and the
indicators. Health indicators wereassessedduring two different time periods namely 2005-
2008, wherePU was evaluated as an external health quality indicator and during 2001-2004,
where it functioned as an internal indicator. Upon comparing the results from 2001-2004, the
authors found that there were fewer participants who reported hemiparesis/CVA (OR 0.485),
surgery that lasted more than 2 hours (OR 0.637), infectious or contagious diseases (OR
0.861), and those who were at risk for Braden scale scores (OR 0.844). However, high
prevalence was found for patients who reported diabetes mellitus (OR 1.693), corresponding
to the 2005-2008 group. On comparing the results, the researchers also found that the hospital
wards required more special mattresses or beds (OR 2.216) and specialised questions that
were attached to wheelchairs (OR 2.277) during the second time period (2005-2008). This
second time frame was also supported by an increase in information related to repositioning
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
28MSC NURSING
of patients, prevention of malnutrition and or dehydration in them, prevention of PU and
information on its appropriate treatment. Further investigation suggested that more Dutch
hospitals disseminated information leaflets and pamphlets on PUs (OR 5.894), prevention
guidelines (OR 4.625), and formed committees related to its management during 2005-2008
(OR 2.503). An increase was also seen and the number of PU wound care nurses who were
recruited at different wards during the time period (OR 2.434). This made the researchers
conclude that the high prevalence of PU across Dutch hospitals after the year 2004could be
attributed to differences that existed in characteristics of patients, and an improvement in the
structural quality indicators and prevention strategies for PU (Amir, Meijers and Halfens
2011).
The increase in use of data related to prevalence and incidence of PU as indicators of
quality of care and their effectiveness in formulating prevention protocols were identified by
another group of researchers. The researchers tried to investigate the dilemma that was
associated with measurement of the incidence and prevalence rates and suggested that there
existed confusion over the definitions, the uses and implication of the terms. Although used
interchangeably, the term incidence referred to the total number of new cases that were
reported within a certain period of time in relation to a particular disease. On the other hand,
prevalence referred to the total number of people alive with a certain disease during a
particular period of time that was being investigated. The researchers also suggested that they
often encountered difficulties in conducting studies on the incidence and prevalence of PU, in
relation to different aspects namely, (1) collection and recording of data, (2) definition of the
population being study, (3) identification of PUs, and (4) subsequent classification of PUs.
The researchers also elaborated on the need for increasing awareness on the perils related to
interpretation, evaluation and comparison of the incidence and prevalence rates. Some of the
major indicators that were identified by them as effective prevention strategies were, a
of patients, prevention of malnutrition and or dehydration in them, prevention of PU and
information on its appropriate treatment. Further investigation suggested that more Dutch
hospitals disseminated information leaflets and pamphlets on PUs (OR 5.894), prevention
guidelines (OR 4.625), and formed committees related to its management during 2005-2008
(OR 2.503). An increase was also seen and the number of PU wound care nurses who were
recruited at different wards during the time period (OR 2.434). This made the researchers
conclude that the high prevalence of PU across Dutch hospitals after the year 2004could be
attributed to differences that existed in characteristics of patients, and an improvement in the
structural quality indicators and prevention strategies for PU (Amir, Meijers and Halfens
2011).
The increase in use of data related to prevalence and incidence of PU as indicators of
quality of care and their effectiveness in formulating prevention protocols were identified by
another group of researchers. The researchers tried to investigate the dilemma that was
associated with measurement of the incidence and prevalence rates and suggested that there
existed confusion over the definitions, the uses and implication of the terms. Although used
interchangeably, the term incidence referred to the total number of new cases that were
reported within a certain period of time in relation to a particular disease. On the other hand,
prevalence referred to the total number of people alive with a certain disease during a
particular period of time that was being investigated. The researchers also suggested that they
often encountered difficulties in conducting studies on the incidence and prevalence of PU, in
relation to different aspects namely, (1) collection and recording of data, (2) definition of the
population being study, (3) identification of PUs, and (4) subsequent classification of PUs.
The researchers also elaborated on the need for increasing awareness on the perils related to
interpretation, evaluation and comparison of the incidence and prevalence rates. Some of the
major indicators that were identified by them as effective prevention strategies were, a
29MSC NURSING
reduction in PU incidence and prevalence, decrease of treatment costs, presence of a prompt
and effective monitoring or assessment, decreased risks of adverse effects of PU on the
quality of life, and reduced litigation risks. Furthermore, the authors also illustrated that
pressure also should be classified according to etiology, reverse staging, deep tissue injury,
and non-blanchable erythema (Baharestani et al. 2009).
Another cross-sectional study was conducted in the year 2004 to determine the
prevalence rates of PU across French hospitals. The researchers carried out the survey over a
period of one week, across all public hospitals that were enlisted in the French National
Public Hospital directory, of which 29 university hospitals were excluded. All patients,
except those who were admitted to the outpatient, emergency, and accident departments were
included in the study, following which questionnaires were sent to nurses, in order to
determine the prevalence rates. Analysis of the questionnaires resulted in 93.5% response
rates from an approximate 37307 inpatients, who were admitted to 1170 wards, present
across 1149 hospitals.The mean age of all the respondents was an estimated 72.3 years, and
62% of them were women. 3314 patients reported confirmed presence of one PU in them,
which resulted in a prevalence rate of 8.9 %. Records were obtained for a total of 4991 PUs
and 64% of the patients reported only one PU. A minimum of two connected diseases were
reported by 55% of the patient. Upon assessing the patients who reported one PU, the most
common regions of ulcer formation were found to be the sacrum and the heels, with rates of
29% and 53%, respectively. Heel PU were frequent among patients who had obliterative
arterial disease. Conversely, patients who reported incontinence in urine or fecal matter
reported sacral PU, more commonly than others. Severe lesions were found among patients
with multiple sites of PU. These findings made the researchers conclude that there was a
stability or saturation in the prevalence of Pus, across inpatients in French hospitals, since a
reduction in PU incidence and prevalence, decrease of treatment costs, presence of a prompt
and effective monitoring or assessment, decreased risks of adverse effects of PU on the
quality of life, and reduced litigation risks. Furthermore, the authors also illustrated that
pressure also should be classified according to etiology, reverse staging, deep tissue injury,
and non-blanchable erythema (Baharestani et al. 2009).
Another cross-sectional study was conducted in the year 2004 to determine the
prevalence rates of PU across French hospitals. The researchers carried out the survey over a
period of one week, across all public hospitals that were enlisted in the French National
Public Hospital directory, of which 29 university hospitals were excluded. All patients,
except those who were admitted to the outpatient, emergency, and accident departments were
included in the study, following which questionnaires were sent to nurses, in order to
determine the prevalence rates. Analysis of the questionnaires resulted in 93.5% response
rates from an approximate 37307 inpatients, who were admitted to 1170 wards, present
across 1149 hospitals.The mean age of all the respondents was an estimated 72.3 years, and
62% of them were women. 3314 patients reported confirmed presence of one PU in them,
which resulted in a prevalence rate of 8.9 %. Records were obtained for a total of 4991 PUs
and 64% of the patients reported only one PU. A minimum of two connected diseases were
reported by 55% of the patient. Upon assessing the patients who reported one PU, the most
common regions of ulcer formation were found to be the sacrum and the heels, with rates of
29% and 53%, respectively. Heel PU were frequent among patients who had obliterative
arterial disease. Conversely, patients who reported incontinence in urine or fecal matter
reported sacral PU, more commonly than others. Severe lesions were found among patients
with multiple sites of PU. These findings made the researchers conclude that there was a
stability or saturation in the prevalence of Pus, across inpatients in French hospitals, since a
30MSC NURSING
similar study was undertaken 10 years earlier, which also had a prevalence rate of 8.9 %
(Barrois et al. 2008).
Similar cross-sectional study was conducted across two Swedish County Councils, in
order to determine the prevalence of hospital acquired PUs. The entire study comprised of
data collection conducted across a single day, on 1192 patients who were aged more than 18
years. Following conduction of a descriptive statistical analysis, the researchers found that
14.29% was the overall prevalence of PU among the patients, of which 11.6% was found
among patients with HAPU, and 3.3% among those who had community acquired PUs.
Majority of the cases of PUs were hospital acquired, with the prevalence of 78% and most of
them were categorised to stage 1 that corresponded to non-blanchable erythema. 26% and
18% HAPU belonged tocategory 2 and 3, respectively that corresponded to partial thickness
of skin loss, or full thickness of skin loss. Moreover, the most severe locations of HAPU were
the sacrum, heels and the hips (32.6%, 37%, and 3.0%).Of the 11 cases of PUs that belonged
to category 4, nine were located in the heels. This made the authors draw the conclusion that
an increase in age, longer hospitalization period, less physical activity, reduction in sensory
perception and problems associated with friction or shear were the major contributor factors
to the high rates of HAPU among the patients (Gunningberg, Stotts and Idvall 2011).
Gunningberg et al. (2013) also conducted the first national survey on the prevalence
of PU in municipality settings and County Councils in Sweden. They focused their study on
the fact that only few countries in the Europe had effectively conducted PU prevalence
researches that acted as a benchmark for evaluating the efficacy of the care that was being
provided to patients in different hospital settings. The authors employed a cross-sectional
study design that invited all municipalities and County Councils to help in the determination
of the prevalence rates in the year 2011. A specific day was selected for collecting
information from the PU survey that encompassed questions on age, gender, risk assessment,
similar study was undertaken 10 years earlier, which also had a prevalence rate of 8.9 %
(Barrois et al. 2008).
Similar cross-sectional study was conducted across two Swedish County Councils, in
order to determine the prevalence of hospital acquired PUs. The entire study comprised of
data collection conducted across a single day, on 1192 patients who were aged more than 18
years. Following conduction of a descriptive statistical analysis, the researchers found that
14.29% was the overall prevalence of PU among the patients, of which 11.6% was found
among patients with HAPU, and 3.3% among those who had community acquired PUs.
Majority of the cases of PUs were hospital acquired, with the prevalence of 78% and most of
them were categorised to stage 1 that corresponded to non-blanchable erythema. 26% and
18% HAPU belonged tocategory 2 and 3, respectively that corresponded to partial thickness
of skin loss, or full thickness of skin loss. Moreover, the most severe locations of HAPU were
the sacrum, heels and the hips (32.6%, 37%, and 3.0%).Of the 11 cases of PUs that belonged
to category 4, nine were located in the heels. This made the authors draw the conclusion that
an increase in age, longer hospitalization period, less physical activity, reduction in sensory
perception and problems associated with friction or shear were the major contributor factors
to the high rates of HAPU among the patients (Gunningberg, Stotts and Idvall 2011).
Gunningberg et al. (2013) also conducted the first national survey on the prevalence
of PU in municipality settings and County Councils in Sweden. They focused their study on
the fact that only few countries in the Europe had effectively conducted PU prevalence
researches that acted as a benchmark for evaluating the efficacy of the care that was being
provided to patients in different hospital settings. The authors employed a cross-sectional
study design that invited all municipalities and County Councils to help in the determination
of the prevalence rates in the year 2011. A specific day was selected for collecting
information from the PU survey that encompassed questions on age, gender, risk assessment,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
31MSC NURSING
observation of skin, PU location, PU categories, and prevention strategies. After entering the
collected data in the SALAR national database, an estimated 16,466 people were found to
participate in the survey. The entire PU prevalence was 16.6% (2737 patients) for categories
1-4. A total of 2737 patients had reported cases of 3276 PUs. 11% (291 patients) of them
provided responses that suggested the likely onset of PU, before they were admitted to the
hospital units. The prevalence rates of PU differed from 17.8% in county hospitals to 15.5%
in university hospitals. Furthermore, approximately 50% PU cases belonged to the category
1. The rates ranged from 9-31% in 21 different counties. Heels and sacrum were identified as
the most affected regions. Of the 18,592 participants from the municipalities, 14.5% was the
overall PU prevalence (2693 patients). Moreover, prevalence rate varied from 12.3%-21.9%
for special housing and short-term care, respectively. Sacrum, feet and heels were the most
affected regions among people in the municipality settings as well. At-risk people had a
proportion of 26.1-34.7%. Furthermore, most person at-risks were not receiving bed
repositioning (50.2–57.5%) or pressure relieving mattresses (23.3-27.9%).
Another study aimed to provide an estimate related to the costs that were associated
with treatment of Pus, in the UK as per prices in the year 2011. The authors used resources
with theapplication of a bottom-up methodology that was based on all the daily resources,
which were required for delivering care protocol that reflected a good clinical practice. This
approach was utilised by the authors for estimating costs of treatment, per episode of PU care
for each patient,suffering from PUs that were of different levels of complication and severity.
Findings from the authors suggested that the cost of treatment variedfrom £1214, for category
1 that corresponded to non-blanchable erythema to £14108, for category 4PU that was
concomitant with full thickness tissue-loss, associated with exposed tendons, muscles, and
bones. The average daily treatment costs varied from £43 to £374 for patients, and the
presence of complications that needed additional diagnostic tests, increase in the length of
observation of skin, PU location, PU categories, and prevention strategies. After entering the
collected data in the SALAR national database, an estimated 16,466 people were found to
participate in the survey. The entire PU prevalence was 16.6% (2737 patients) for categories
1-4. A total of 2737 patients had reported cases of 3276 PUs. 11% (291 patients) of them
provided responses that suggested the likely onset of PU, before they were admitted to the
hospital units. The prevalence rates of PU differed from 17.8% in county hospitals to 15.5%
in university hospitals. Furthermore, approximately 50% PU cases belonged to the category
1. The rates ranged from 9-31% in 21 different counties. Heels and sacrum were identified as
the most affected regions. Of the 18,592 participants from the municipalities, 14.5% was the
overall PU prevalence (2693 patients). Moreover, prevalence rate varied from 12.3%-21.9%
for special housing and short-term care, respectively. Sacrum, feet and heels were the most
affected regions among people in the municipality settings as well. At-risk people had a
proportion of 26.1-34.7%. Furthermore, most person at-risks were not receiving bed
repositioning (50.2–57.5%) or pressure relieving mattresses (23.3-27.9%).
Another study aimed to provide an estimate related to the costs that were associated
with treatment of Pus, in the UK as per prices in the year 2011. The authors used resources
with theapplication of a bottom-up methodology that was based on all the daily resources,
which were required for delivering care protocol that reflected a good clinical practice. This
approach was utilised by the authors for estimating costs of treatment, per episode of PU care
for each patient,suffering from PUs that were of different levels of complication and severity.
Findings from the authors suggested that the cost of treatment variedfrom £1214, for category
1 that corresponded to non-blanchable erythema to £14108, for category 4PU that was
concomitant with full thickness tissue-loss, associated with exposed tendons, muscles, and
bones. The average daily treatment costs varied from £43 to £374 for patients, and the
presence of complications that needed additional diagnostic tests, increase in the length of
32MSC NURSING
stay in hospitals, and expensive pressure relieving surfaces, acted as significant factors in
increasing the treatment costs. This made the authors suggest that PUs represented a
significant rate burden to the patients and healthcare providers in the UK. These costs
showedlikelihood to increase in future practice, with an increase in age of the population
(Dealey, Posnett and Walker 2012).
da Silva Cardoso et al. (2010) also conducted a similar cross-sectional study to
investigate the prevalence of PU across Brazilian hospitals. They based their study on
previously conducted epidemiological research that assessed the incidence and prevalence of
the condition in hospitals and long-term care units. Following approval from the Research
Ethics Committee of the São Paulo Hospital (UNIFESP-EPM), the prevalence of PU was
measured at two different time frames among all patients who had been admitted to the São
Paulo Hospital, with 752 beds. The researchers primarily focused on acute care wards
namely, intensive care, surgical, medical, and emergency units. On collecting information on
the prevalence rates on June 16 and October 20, in the year 2004. Results collected on the
first day emphasized on the presence of PU among 43 hospitalised patients among the total
population of 376, thus indicating a prevalence rate of 11.4%. Conversely, data collected on
the second day provided evidence for PU among 35 of 340 patients. This indicated a
prevalence rate of 10.3%. The total number of days since hospitalization ranged from 1-224
days, with a mean average of 36 days. Further analysis made by the researchers suggested
that the condition of the patients diagnosed with PU was the major factor that was evident in
both the patient populations. Furthermore, most of the patients reported presence of a single
PU (61.5%) and 47% of those were present in the sacral region. 32.7% PU prevalence was
found in patients admitted to the ICU, on both the days. In addition, 8.7% PU was prevalent
in the medical unit on the second day, and 22.7% in emergency department on the first day,
stay in hospitals, and expensive pressure relieving surfaces, acted as significant factors in
increasing the treatment costs. This made the authors suggest that PUs represented a
significant rate burden to the patients and healthcare providers in the UK. These costs
showedlikelihood to increase in future practice, with an increase in age of the population
(Dealey, Posnett and Walker 2012).
da Silva Cardoso et al. (2010) also conducted a similar cross-sectional study to
investigate the prevalence of PU across Brazilian hospitals. They based their study on
previously conducted epidemiological research that assessed the incidence and prevalence of
the condition in hospitals and long-term care units. Following approval from the Research
Ethics Committee of the São Paulo Hospital (UNIFESP-EPM), the prevalence of PU was
measured at two different time frames among all patients who had been admitted to the São
Paulo Hospital, with 752 beds. The researchers primarily focused on acute care wards
namely, intensive care, surgical, medical, and emergency units. On collecting information on
the prevalence rates on June 16 and October 20, in the year 2004. Results collected on the
first day emphasized on the presence of PU among 43 hospitalised patients among the total
population of 376, thus indicating a prevalence rate of 11.4%. Conversely, data collected on
the second day provided evidence for PU among 35 of 340 patients. This indicated a
prevalence rate of 10.3%. The total number of days since hospitalization ranged from 1-224
days, with a mean average of 36 days. Further analysis made by the researchers suggested
that the condition of the patients diagnosed with PU was the major factor that was evident in
both the patient populations. Furthermore, most of the patients reported presence of a single
PU (61.5%) and 47% of those were present in the sacral region. 32.7% PU prevalence was
found in patients admitted to the ICU, on both the days. In addition, 8.7% PU was prevalent
in the medical unit on the second day, and 22.7% in emergency department on the first day,
33MSC NURSING
respectively. These expected results made the authors recognize the need of formulating
specific PU prevention protocols, in future practice.
Another study was conducted with the aim of determining the factors that played a
role on the effects of PU on health-related quality of life of all patients (HRQoL). The
researchers included adult patients having diagnosed with different categories of PU in any
location, based on their stay in hospitals, community or rehabilitation centres. A purposive
sampling method was adopted by the researchers for gaining an insight into the diversity and
range of PU population that including severity, age, grades, location and experiences.
Following collection of data by face-to-face interviews, results suggested that the age of the
participants ranged from 22-94 years, with a mean age of 62.2 years. 56% of the participants
were men and 19 had chronic disorders. The responses suggested that PU patients displayed
an adherence to treatment only if they were assured of the effectiveness of the treatment in
improving their PU condition. Continued hospitalization made the PU patients feel restricted
and prevented their participation in leisure or social activities. Moreover, inconsistencies in
management of PU also contributed to feelings of worry and anxiety among the patients.
Inconsistent usage of different healthcare terminologies, differences in the time that the staff
spent on wound care, and reduced patient satisfaction, when compared to burden of treatment
were some of the major complaints made the patients (Gorecki et al. 2012).
Bernardes and Caliri(2016) conducted another cross-sectional study for recognizing
PU point prevalence in different emergency units of a hospital. The researchers collected data
on a single day, by showing adherence to the international guidelines and used the Braden
Scale for assessing the PU risk in each patient. The age of the patients ranged from 20-90
years, with a mean age of 54.01 years. Distribution of the patients as per the prevalence of
pressure ulcer was 16%, 3%, 4%, in the infirmaries, emergency rooms, semi-intensive units,
respectively. Highest point prevalence of PU was reported in the ICU (75%), followed by
respectively. These expected results made the authors recognize the need of formulating
specific PU prevention protocols, in future practice.
Another study was conducted with the aim of determining the factors that played a
role on the effects of PU on health-related quality of life of all patients (HRQoL). The
researchers included adult patients having diagnosed with different categories of PU in any
location, based on their stay in hospitals, community or rehabilitation centres. A purposive
sampling method was adopted by the researchers for gaining an insight into the diversity and
range of PU population that including severity, age, grades, location and experiences.
Following collection of data by face-to-face interviews, results suggested that the age of the
participants ranged from 22-94 years, with a mean age of 62.2 years. 56% of the participants
were men and 19 had chronic disorders. The responses suggested that PU patients displayed
an adherence to treatment only if they were assured of the effectiveness of the treatment in
improving their PU condition. Continued hospitalization made the PU patients feel restricted
and prevented their participation in leisure or social activities. Moreover, inconsistencies in
management of PU also contributed to feelings of worry and anxiety among the patients.
Inconsistent usage of different healthcare terminologies, differences in the time that the staff
spent on wound care, and reduced patient satisfaction, when compared to burden of treatment
were some of the major complaints made the patients (Gorecki et al. 2012).
Bernardes and Caliri(2016) conducted another cross-sectional study for recognizing
PU point prevalence in different emergency units of a hospital. The researchers collected data
on a single day, by showing adherence to the international guidelines and used the Braden
Scale for assessing the PU risk in each patient. The age of the patients ranged from 20-90
years, with a mean age of 54.01 years. Distribution of the patients as per the prevalence of
pressure ulcer was 16%, 3%, 4%, in the infirmaries, emergency rooms, semi-intensive units,
respectively. Highest point prevalence of PU was reported in the ICU (75%), followed by
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
34MSC NURSING
55.56% in the semi-ICU. Category 2 ulcers were found more among the patients (42.86%).
This prevalence was followed by category 1 and category 3 ulcers, with a prevalence of
42.86% and 20.24%, respectively. Category 4 ulcers and subjective deep tissue injuries were
found among 3.57% and 5.95% of the participants. Furthermore, most PU were found in the
calcaneus region (28.57%), and sacral region (22.61%). Moreover, PU point prevalence was
found to be 35.29% in the hospital after 4 patients reporting category 1 ulcer were excluded
from the data findings. Besides, patients being diagnosed with PU reported increased length
of hospitalization, when compared to their non-ulcer counterparts. The difference of
p<0.0001 was statistically significant.The mean and median of PU patients was found to be
higher for the total diagnosis. However, this difference failed to show a statistical
significance (p=0.065).
Another study was conducted with the aim of determining the prevalence of PU
among hospitalized patients in a tertiary public hospital of Jordan, in order to formulate
effective strategies for avoiding harms and minimizing healthcare costs. The authors adopted
a cross-sectional study design that was conducted over a period of four weeks in two different
medical wards of the selected AlBashir hospital. The researchers calculated the prevalence
rate as the total number of patients who were diagnosed with PU, divided by the assessed
patients. 190 participants were included in the research, of whom 123 were identified to stay
an an increased risk of development of PU. Over a period of five years, 30 PU cases were
identified among the patients. Of these identified cases, 53% were men, and 75% of the
patients were aged more than 60 years. Furthermore, the prevalence rate was approximately
24%. 8 cases (27%) reporred category 1 PU, followed by 13 patients (43%) for category 2,
and 6 patients (20%) for category 3 pressure ulcers. In addition, 1 patient (3%) reported
category 4 PU. Reports from 2 patients also reported mixed categories of the condition.
Highest prevalence of PU was chiefly found in the sacral region(43%=13 cases), followed by
55.56% in the semi-ICU. Category 2 ulcers were found more among the patients (42.86%).
This prevalence was followed by category 1 and category 3 ulcers, with a prevalence of
42.86% and 20.24%, respectively. Category 4 ulcers and subjective deep tissue injuries were
found among 3.57% and 5.95% of the participants. Furthermore, most PU were found in the
calcaneus region (28.57%), and sacral region (22.61%). Moreover, PU point prevalence was
found to be 35.29% in the hospital after 4 patients reporting category 1 ulcer were excluded
from the data findings. Besides, patients being diagnosed with PU reported increased length
of hospitalization, when compared to their non-ulcer counterparts. The difference of
p<0.0001 was statistically significant.The mean and median of PU patients was found to be
higher for the total diagnosis. However, this difference failed to show a statistical
significance (p=0.065).
Another study was conducted with the aim of determining the prevalence of PU
among hospitalized patients in a tertiary public hospital of Jordan, in order to formulate
effective strategies for avoiding harms and minimizing healthcare costs. The authors adopted
a cross-sectional study design that was conducted over a period of four weeks in two different
medical wards of the selected AlBashir hospital. The researchers calculated the prevalence
rate as the total number of patients who were diagnosed with PU, divided by the assessed
patients. 190 participants were included in the research, of whom 123 were identified to stay
an an increased risk of development of PU. Over a period of five years, 30 PU cases were
identified among the patients. Of these identified cases, 53% were men, and 75% of the
patients were aged more than 60 years. Furthermore, the prevalence rate was approximately
24%. 8 cases (27%) reporred category 1 PU, followed by 13 patients (43%) for category 2,
and 6 patients (20%) for category 3 pressure ulcers. In addition, 1 patient (3%) reported
category 4 PU. Reports from 2 patients also reported mixed categories of the condition.
Highest prevalence of PU was chiefly found in the sacral region(43%=13 cases), followed by
35MSC NURSING
the heel region (24%= 7 cases), hip trochanters (10%= 3 cases), calf (3%= 1 case), and
multiple region (20%= 6 cases).Over a time frame of 4 weeks, the researchers could identify
29 new cases of PU. Furthermore, older people were found at an increased risk of PU
development, when compared to their younger counterparts. However, the researchers failed
to draw a significant difference between the prevalence rates based on gender (47% and 53%,
p<0.6) (Alja'afreh and Mosleh 2013).
An exhaustive review was conducted by different researchers to discover the
incidence, prevalence, costs, and risk factors of PU among persons having suffered spinal
cord injury (SCI), in the developing world. The authors conducted a PubMed search of
relevant scholarly articles that were published in English between the year 1998 and August
2014. They used search terms as ‘pressure ulcers’, and ‘spinal cord injury’ for retrieving
important articles. This made them obtain 938 article hits. This was followed byreviewing the
abstracts of pertinent titles, which when considered relevant were followed by a thorough
analysis of the full texts. 10 scholarly papers were found to report a prevalence of PU 26.7 –
46.2%. The mean prevalence rate was found to be 35.2%. A single article cited a prevalence
rate of 30% that referred to a population paraplegic persons in Brazil. 37.5% prevalence was
found among participants enrolled in a cross-sectional study conducted in Nepal that
comprised of home visits of SCI injured people suffering from complete or incomplete
paraplegia. The authors identified low educational attainment as a major risk factorfor PU
development in patients who belonged to developed nations. Further analysis of the data
findings suggested that developing nations also had low educational levels on an average,
which in turn acted as a significant barrier to the condition (Zakrasek, Creasey and Crew
2015).
Keelaghan et al. (2008) conducted a study among patients who had been recently
admitted to hospital units, with the purpose of investigating and comparing the prevalence
the heel region (24%= 7 cases), hip trochanters (10%= 3 cases), calf (3%= 1 case), and
multiple region (20%= 6 cases).Over a time frame of 4 weeks, the researchers could identify
29 new cases of PU. Furthermore, older people were found at an increased risk of PU
development, when compared to their younger counterparts. However, the researchers failed
to draw a significant difference between the prevalence rates based on gender (47% and 53%,
p<0.6) (Alja'afreh and Mosleh 2013).
An exhaustive review was conducted by different researchers to discover the
incidence, prevalence, costs, and risk factors of PU among persons having suffered spinal
cord injury (SCI), in the developing world. The authors conducted a PubMed search of
relevant scholarly articles that were published in English between the year 1998 and August
2014. They used search terms as ‘pressure ulcers’, and ‘spinal cord injury’ for retrieving
important articles. This made them obtain 938 article hits. This was followed byreviewing the
abstracts of pertinent titles, which when considered relevant were followed by a thorough
analysis of the full texts. 10 scholarly papers were found to report a prevalence of PU 26.7 –
46.2%. The mean prevalence rate was found to be 35.2%. A single article cited a prevalence
rate of 30% that referred to a population paraplegic persons in Brazil. 37.5% prevalence was
found among participants enrolled in a cross-sectional study conducted in Nepal that
comprised of home visits of SCI injured people suffering from complete or incomplete
paraplegia. The authors identified low educational attainment as a major risk factorfor PU
development in patients who belonged to developed nations. Further analysis of the data
findings suggested that developing nations also had low educational levels on an average,
which in turn acted as a significant barrier to the condition (Zakrasek, Creasey and Crew
2015).
Keelaghan et al. (2008) conducted a study among patients who had been recently
admitted to hospital units, with the purpose of investigating and comparing the prevalence
36MSC NURSING
rates of pressure ulcers. Comparisons were drawn between patients who were newly
hospitalized across different nursing homes, with recently admitted ones from non-nursing
home settings. They conducted secondary analysis of a study that was conducted across two
inner city hospitals held in Philadelphia, between the years 1998 and 2001. All of the study
participants were aged at least 65 years and had been admitted to emergency department in
either of the two hospitals. The nurses also determined the presence of PU among the patients
(categories 1–4) by conducting a visual skin assessment. This assessment was performed on
the third day, after the patients were admitted to the hospital units. The nurses also collected
data followinginterview,clinical examination, and review of medical records. 26.2% was the
prevalence of already existing pressure ulcers during admission among people who were
present in nursing homes, compared to 4.8% among patients who had been admitted to other
living situations (OR= 5.5, 95% CI; 4.3–7.1). Following adjustment for the confounding
variables, the link between admission of patients from nursing homes and prevalence of PU
on admission showed a significant reduction (OR=1.51, 95% CI; 1.03–2.23). These results
indicated provided evidence for the fact that admission of patients from a nursing home acted
as a potential marker for risks of pressure ulcer.
An earlier study conducted by Fogerty et al. (2009) had provided evidence for a
significantly high risk of PU diagnosis following hospital discharge of African Americans.
These patients were found to belong to the higher age groups, and had already been
diagnosed with specific medical disorders. The key objectives of the researchers were to (a)
examine the demographics that were related to increased odds ratio (OR) among African
Americans and (b) definepresence of medical risk factors among the African Americans.
They queried the 2003 Nationwide Inpatient Sample database. Patients diagnosed with PU
were recognized by release diagnoses, with the use of ICD‐9 codes 707.0–707.09. African
Americans demonstrated an elevated incidence for 28 recognized CCS risk factors (OR>2)
rates of pressure ulcers. Comparisons were drawn between patients who were newly
hospitalized across different nursing homes, with recently admitted ones from non-nursing
home settings. They conducted secondary analysis of a study that was conducted across two
inner city hospitals held in Philadelphia, between the years 1998 and 2001. All of the study
participants were aged at least 65 years and had been admitted to emergency department in
either of the two hospitals. The nurses also determined the presence of PU among the patients
(categories 1–4) by conducting a visual skin assessment. This assessment was performed on
the third day, after the patients were admitted to the hospital units. The nurses also collected
data followinginterview,clinical examination, and review of medical records. 26.2% was the
prevalence of already existing pressure ulcers during admission among people who were
present in nursing homes, compared to 4.8% among patients who had been admitted to other
living situations (OR= 5.5, 95% CI; 4.3–7.1). Following adjustment for the confounding
variables, the link between admission of patients from nursing homes and prevalence of PU
on admission showed a significant reduction (OR=1.51, 95% CI; 1.03–2.23). These results
indicated provided evidence for the fact that admission of patients from a nursing home acted
as a potential marker for risks of pressure ulcer.
An earlier study conducted by Fogerty et al. (2009) had provided evidence for a
significantly high risk of PU diagnosis following hospital discharge of African Americans.
These patients were found to belong to the higher age groups, and had already been
diagnosed with specific medical disorders. The key objectives of the researchers were to (a)
examine the demographics that were related to increased odds ratio (OR) among African
Americans and (b) definepresence of medical risk factors among the African Americans.
They queried the 2003 Nationwide Inpatient Sample database. Patients diagnosed with PU
were recognized by release diagnoses, with the use of ICD‐9 codes 707.0–707.09. African
Americans demonstrated an elevated incidence for 28 recognized CCS risk factors (OR>2)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
37MSC NURSING
for PU. The diagnosis of PU was found to occur more among African Americans, who
belonged to the younger age group. Following conduction of a sub-analysis, the researchers
failed to produce any significant difference in African Americans having pressure ulcers.
Another 3 year unit-specific analysis was also conducted to determine the prevalence
of PU, in addition to results of the 2008 – 2009 International Pressure Ulcer Prevalence
Survey. The key purpose of this cross-sectional, observational cohort study was to conclude
findings from the International Pressure Ulcer Prevalence Survey (IPUP) that was conducted
in the United States from 2008-2009. Additionally, the researchers also focused on data that
was collected previously during 2006-2007for reporting unit-specific and general prevalence
rates of PU, among patients admitted to acute care facilities. The overall prevalence and rates
of PUwas found to be 13.5% and 6%, in the year 2008 (N = 90,398). Results that
corresponded to the year 2009 were12.3 and 5% (N = 92,408). Furthermore,the overall
prevalence rates in 2008 and 2009 were also found to be highest (22%) in long-term acute
care. Rates of facility-acquired ulcers were maximum in adult patients present in intensive
care units and fluctuated from 9.2%-12.1% forgeneral cardiac care and medical ICU units,
respectively, in the year 2008. Corresponding results for 2009 varied from 8.8% (CCU) to
10.3% (ICU). Besides, 3.3% ICU patients acquired severe FA ulcers that were categorized to
category 3, category 4, deep tissue injury, and eschar/unable to stage. An estimated 10%
ulcers (n = 1,631) were recognized as device-related. The sacral or coccyx region (17%) and
ear (20%) were the most affected areas. The findings made the authors conclude that the
prevalence rates of PU were significantly low in 2008-2009, compared to 2006-2007
(Catherine VanGilder et al. 2009).
Similar study was also conducted by Shahin, Dassen and Halfens(2008) to assess the
prevalence rate of PU across patients who were admitted to intensive care units. The authors
conducted an exhaustive study of electronic databases such as, PubMed and CINAHL, for
for PU. The diagnosis of PU was found to occur more among African Americans, who
belonged to the younger age group. Following conduction of a sub-analysis, the researchers
failed to produce any significant difference in African Americans having pressure ulcers.
Another 3 year unit-specific analysis was also conducted to determine the prevalence
of PU, in addition to results of the 2008 – 2009 International Pressure Ulcer Prevalence
Survey. The key purpose of this cross-sectional, observational cohort study was to conclude
findings from the International Pressure Ulcer Prevalence Survey (IPUP) that was conducted
in the United States from 2008-2009. Additionally, the researchers also focused on data that
was collected previously during 2006-2007for reporting unit-specific and general prevalence
rates of PU, among patients admitted to acute care facilities. The overall prevalence and rates
of PUwas found to be 13.5% and 6%, in the year 2008 (N = 90,398). Results that
corresponded to the year 2009 were12.3 and 5% (N = 92,408). Furthermore,the overall
prevalence rates in 2008 and 2009 were also found to be highest (22%) in long-term acute
care. Rates of facility-acquired ulcers were maximum in adult patients present in intensive
care units and fluctuated from 9.2%-12.1% forgeneral cardiac care and medical ICU units,
respectively, in the year 2008. Corresponding results for 2009 varied from 8.8% (CCU) to
10.3% (ICU). Besides, 3.3% ICU patients acquired severe FA ulcers that were categorized to
category 3, category 4, deep tissue injury, and eschar/unable to stage. An estimated 10%
ulcers (n = 1,631) were recognized as device-related. The sacral or coccyx region (17%) and
ear (20%) were the most affected areas. The findings made the authors conclude that the
prevalence rates of PU were significantly low in 2008-2009, compared to 2006-2007
(Catherine VanGilder et al. 2009).
Similar study was also conducted by Shahin, Dassen and Halfens(2008) to assess the
prevalence rate of PU across patients who were admitted to intensive care units. The authors
conducted an exhaustive study of electronic databases such as, PubMed and CINAHL, for
38MSC NURSING
retrieving scholarly articles that were published from 2000-2005. Some of the key words that
were used by the researchers were ‘pressure ulcer’, ‘decubitus ulcer’, ‘pressure sore’, ‘bed
sore’, ‘incidence’, and ‘prevalence’. Findings of the review suggested that the prevalence of
PU ranged from 4% in ICUs across Denmark, to an estimated 49% in Germany. The
incidence rate was found to vary between 38-124%. Wide differences were observed in the
incidence and prevalence of pressure ulcer among patients admitted to the intensive care
units. Furthermore, the review also suggested that the sacrum and the heels were the most
commonly affected parts of the body (25.2% and 39.4%, respectively). Besides, results
presented in the scholarly articles suggested that the highest prevalence (56.9%) of PU was
found among patients who had acquired some form of infection (commonly sepsis). Some of
the most common factors that were identified to play a crucial role in the prevalence rates
were length of hospitalization, age, mobility status and presence of moisture.
Owing to the fact that pressure ulcers have been recognized as a significant problem
in healthcare facilities and patients, authors of another study attempted to evaluate the results
of nine surveys that were conducted between the year 1989 to 2005, for assessing the
prevalence rates of PU. During all of the nine surveys that were conducted from 1989-2005,
all the clinical teams present in the participating facilities, were predominantly located in the
US. Some of the surveys were conducted across healthcare facilities in Saudi Arabia, Canada,
and Australia after 2003. The researchers primarily assessed the patients who had been
admitted on specific study dates. The prevalence rate for nosocomial and overall PU ranged
from 5.6% and 9.2% in 1989 to 10% and 15.5% in 2003 and 2004, respectively. The
maximum prevalence of 8.5% nosocomial PU and 27.3% overall PU was acknowledged in
the long-term acute care. Most frequently, PU were found located among patients at the heels
(23.6%), sacrum (28%), and the buttocks (17.2%). The PU were more generally measured as
category 1 and category 2 (>70%). However, patients having a darker skin tone (n = 162,296
retrieving scholarly articles that were published from 2000-2005. Some of the key words that
were used by the researchers were ‘pressure ulcer’, ‘decubitus ulcer’, ‘pressure sore’, ‘bed
sore’, ‘incidence’, and ‘prevalence’. Findings of the review suggested that the prevalence of
PU ranged from 4% in ICUs across Denmark, to an estimated 49% in Germany. The
incidence rate was found to vary between 38-124%. Wide differences were observed in the
incidence and prevalence of pressure ulcer among patients admitted to the intensive care
units. Furthermore, the review also suggested that the sacrum and the heels were the most
commonly affected parts of the body (25.2% and 39.4%, respectively). Besides, results
presented in the scholarly articles suggested that the highest prevalence (56.9%) of PU was
found among patients who had acquired some form of infection (commonly sepsis). Some of
the most common factors that were identified to play a crucial role in the prevalence rates
were length of hospitalization, age, mobility status and presence of moisture.
Owing to the fact that pressure ulcers have been recognized as a significant problem
in healthcare facilities and patients, authors of another study attempted to evaluate the results
of nine surveys that were conducted between the year 1989 to 2005, for assessing the
prevalence rates of PU. During all of the nine surveys that were conducted from 1989-2005,
all the clinical teams present in the participating facilities, were predominantly located in the
US. Some of the surveys were conducted across healthcare facilities in Saudi Arabia, Canada,
and Australia after 2003. The researchers primarily assessed the patients who had been
admitted on specific study dates. The prevalence rate for nosocomial and overall PU ranged
from 5.6% and 9.2% in 1989 to 10% and 15.5% in 2003 and 2004, respectively. The
maximum prevalence of 8.5% nosocomial PU and 27.3% overall PU was acknowledged in
the long-term acute care. Most frequently, PU were found located among patients at the heels
(23.6%), sacrum (28%), and the buttocks (17.2%). The PU were more generally measured as
category 1 and category 2 (>70%). However, patients having a darker skin tone (n = 162,296
39MSC NURSING
in 2004 and 2005) reported a prevalence rate of 13% category 1 PU, in contrast to38%
patients with lighter and 32% patients with medium skin tone. An estimated 48% of all the
patients who had been diagnosed with PU and 48% of them who had nosocomial pressure
ulcers were found to stay at no risk or mild risk (Braden scale scores>14) (VanGilder,
MacFarlane and Meyer 2008).
Amir et al. (2013) also conducted a cross-sectional study with the aim of exploring
the quality of PU care among patients who had suffered stroke and were admitted to a stroke-
specialised hospital in Indonesia. The researchers included all the patients who were present
on the day of prevalence measurement and used two questionnaires namely, the Dutch
National Prevalence Measurement of Care Problems (LPZ) and the European Pressure Ulcer
Prevalence Study Minimum Data Set for assessing the prevalence rates. Upon analyzing the
responses of the aforementioned two questionnaires, the authors found that there was a high
rate of prevalence of PU in the Indonesian hospital that included and excluded Category 1
(28% and 17%, respectively). More than half of all families and patients (56%) received
proper education on PU prevention strategies and 74% of them reported that they were
repositioned. However, this repositioning rate was irregularly managed by the families and
nurses. Patients having category 1 PU did not receive any treatment. Treatment of category 2
PUs were done using 0.9% NaCl solution, for cleansing the wound, without application of
dressings. Anti-microbial gauze dressings were used for treating category 3 PU. Category 4
PU was not reported among any patient.
in 2004 and 2005) reported a prevalence rate of 13% category 1 PU, in contrast to38%
patients with lighter and 32% patients with medium skin tone. An estimated 48% of all the
patients who had been diagnosed with PU and 48% of them who had nosocomial pressure
ulcers were found to stay at no risk or mild risk (Braden scale scores>14) (VanGilder,
MacFarlane and Meyer 2008).
Amir et al. (2013) also conducted a cross-sectional study with the aim of exploring
the quality of PU care among patients who had suffered stroke and were admitted to a stroke-
specialised hospital in Indonesia. The researchers included all the patients who were present
on the day of prevalence measurement and used two questionnaires namely, the Dutch
National Prevalence Measurement of Care Problems (LPZ) and the European Pressure Ulcer
Prevalence Study Minimum Data Set for assessing the prevalence rates. Upon analyzing the
responses of the aforementioned two questionnaires, the authors found that there was a high
rate of prevalence of PU in the Indonesian hospital that included and excluded Category 1
(28% and 17%, respectively). More than half of all families and patients (56%) received
proper education on PU prevention strategies and 74% of them reported that they were
repositioned. However, this repositioning rate was irregularly managed by the families and
nurses. Patients having category 1 PU did not receive any treatment. Treatment of category 2
PUs were done using 0.9% NaCl solution, for cleansing the wound, without application of
dressings. Anti-microbial gauze dressings were used for treating category 3 PU. Category 4
PU was not reported among any patient.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
40MSC NURSING
Chapter 4:
Results
The procedure of thematic synthesis was used to combine the studies that contained
information on prevalence of pressure ulcer (PU), followed by identification of key themes,
with the aim of exploring the research objectives. This thematic analysis examined and
recorded specific patterns within the data that were collected from the scholarly articles, and
were considered essential for description of the phenomenon being investigated.
Theme 1: Following NPUAP and EPUAP classification pattern
The US National and European PU advisory panel have proposed the classification
pattern for categorising PU, depending on their severity, with the help of clinical tools. 10
studies classified PU into different stages that have been proposed in the aforementioned two
assessment tools. The study conducted by Amir, Meijers and Halfens (2011) used the EPUAP
classification system for categorising PU that was found among patients enrolled in the Dutch
General Hospitals. However, the major drawback of the study was that the researchers
excluded category 1 PU, while determining prevalence of the condition among the patients,
every year. Another study conducted by Barrois et al. (2008) use the NPUAP classification
system for categorising an approximate 3238 cases of PU, among French hospital inpatients.
Results of the study indicated that there were 32% cases of stage 1, 13% stage 2, 18% stage
3, and 18% stage 4 PU, respectively. Moreover, the classification system was also used for
grading the types of ulcer among patients who reported only one such PU. Stage 1 and 3 PUs
corresponded to 31% and 19% prevalence, respectively. While stage 2 PU that caused
damage to the epidermis was found among 16% of the inpatients, those that resulted in
granulation tissue were prevalent among 20% of them. The EPUAP Classification system
was used, following a modification with the CALNOC prevalence procedure, in another
Chapter 4:
Results
The procedure of thematic synthesis was used to combine the studies that contained
information on prevalence of pressure ulcer (PU), followed by identification of key themes,
with the aim of exploring the research objectives. This thematic analysis examined and
recorded specific patterns within the data that were collected from the scholarly articles, and
were considered essential for description of the phenomenon being investigated.
Theme 1: Following NPUAP and EPUAP classification pattern
The US National and European PU advisory panel have proposed the classification
pattern for categorising PU, depending on their severity, with the help of clinical tools. 10
studies classified PU into different stages that have been proposed in the aforementioned two
assessment tools. The study conducted by Amir, Meijers and Halfens (2011) used the EPUAP
classification system for categorising PU that was found among patients enrolled in the Dutch
General Hospitals. However, the major drawback of the study was that the researchers
excluded category 1 PU, while determining prevalence of the condition among the patients,
every year. Another study conducted by Barrois et al. (2008) use the NPUAP classification
system for categorising an approximate 3238 cases of PU, among French hospital inpatients.
Results of the study indicated that there were 32% cases of stage 1, 13% stage 2, 18% stage
3, and 18% stage 4 PU, respectively. Moreover, the classification system was also used for
grading the types of ulcer among patients who reported only one such PU. Stage 1 and 3 PUs
corresponded to 31% and 19% prevalence, respectively. While stage 2 PU that caused
damage to the epidermis was found among 16% of the inpatients, those that resulted in
granulation tissue were prevalent among 20% of them. The EPUAP Classification system
was used, following a modification with the CALNOC prevalence procedure, in another
41MSC NURSING
study that determined PU prevalence in Swedish County Councils. Results presented by the
researchers suggested that the overall prevalence of PU based on the classification system
was 8.2%, 3.3%, 2.0 %, and 1.3%, respectively for category 1, 2, 3, and 4. The total overall
prevalence of PU was found to be 14.9%, among all the patient, which included both
community acquired and hospital acquired PU (Gunningberg, Stotts and Idvall 2011). Similar
study was also developed with the use of EPUAP classification data, and made the
researchers conclude that category 1 PU was found among 8.1% of the total participants
(n=18592). While category 2 PU was found among 3% of the participants, category 3 and 4
were found in 2% and 1.3%, respectively of all people, included in the study (Gunningberg et
al. 2013). In another study the in NPUAP Staging system was followed for grading PU, and
results obtained from the cross-sectional studies suggested that 32.1% and 47% of the people
were classified into stage 1 and stage 2 PU categories. Stage 3 and 4 were found among
13.4% and 2.2% of the patients (da Silva Cardoso et al. 2010).
The NPUAP PU Assessment tool was also used in a study conducted in AlBashir
hospital of Jordan, where 27% had stage 1, 43% had stage 2, 20% had stage 3, and 3%
patients reported stage 4 PU, respectively. Moreover, results from the study indicated that
stage 1 and stage 2 PU were more prevalent among females, when compared to their male
counterparts. On the other hand, stage 3 was found in equal proportion in both males and
females (Alja'afreh and Mosleh 2013). Although the study conducted by Keelaghan et al.
(2008) reported the prevalence of the different stages of PU among the nursing home
residents who had been transferred to hospital, adequate information was not present,
regarding which assessment tool was used by the nurses for determining the same.
In another research the stage 1 classification tool was excluded from the final findings, since
the researchers argued that stage 1 PU was associated with subsequent data problem and
substantial errors. Overall prevalence of PU in all US Healthcare facilities was 13.5%, 13.7%,
study that determined PU prevalence in Swedish County Councils. Results presented by the
researchers suggested that the overall prevalence of PU based on the classification system
was 8.2%, 3.3%, 2.0 %, and 1.3%, respectively for category 1, 2, 3, and 4. The total overall
prevalence of PU was found to be 14.9%, among all the patient, which included both
community acquired and hospital acquired PU (Gunningberg, Stotts and Idvall 2011). Similar
study was also developed with the use of EPUAP classification data, and made the
researchers conclude that category 1 PU was found among 8.1% of the total participants
(n=18592). While category 2 PU was found among 3% of the participants, category 3 and 4
were found in 2% and 1.3%, respectively of all people, included in the study (Gunningberg et
al. 2013). In another study the in NPUAP Staging system was followed for grading PU, and
results obtained from the cross-sectional studies suggested that 32.1% and 47% of the people
were classified into stage 1 and stage 2 PU categories. Stage 3 and 4 were found among
13.4% and 2.2% of the patients (da Silva Cardoso et al. 2010).
The NPUAP PU Assessment tool was also used in a study conducted in AlBashir
hospital of Jordan, where 27% had stage 1, 43% had stage 2, 20% had stage 3, and 3%
patients reported stage 4 PU, respectively. Moreover, results from the study indicated that
stage 1 and stage 2 PU were more prevalent among females, when compared to their male
counterparts. On the other hand, stage 3 was found in equal proportion in both males and
females (Alja'afreh and Mosleh 2013). Although the study conducted by Keelaghan et al.
(2008) reported the prevalence of the different stages of PU among the nursing home
residents who had been transferred to hospital, adequate information was not present,
regarding which assessment tool was used by the nurses for determining the same.
In another research the stage 1 classification tool was excluded from the final findings, since
the researchers argued that stage 1 PU was associated with subsequent data problem and
substantial errors. Overall prevalence of PU in all US Healthcare facilities was 13.5%, 13.7%,
42MSC NURSING
13.50%, and 12.3%, respectively in the year 2006, 2007, 2008, and 2009, respectively.
Furthermore, the overall preference in acute care units was 13.3%, 13.4%, 13.10%, and
11.9% for the corresponding years from 2006 to 2009 (Catherine VanGilder et al. 2009).
The study that reported findings from the first International PU Prevalence™ Study
followed the NPUAP classification system and categorised PU prevalence in four different
stages from the year 1989 to 2005. While prevalence of stage 1 ranged from 39 % to 34%,
those for stage 2 and stage 3 range from 39% to 37% and 14% to 7% respectively. Stage 4
ulcer prevalence was found to range from 8% to 7%, from 1989 to 2005 (VanGilder, C.,
MacFarlane and Meyer 2008). The EPUAP-NPUAP PU classification system was also used
in a study conducted in Indonesia, where the prevalence of PU including category 1 was
found to be 28%, while that excluding category 1 was 7%. Moreover, upon classifying the
frequency of PU based on these category, category 1 (57%) was found to be the most
prevalent, followed by category 2 (29%) and 3 (14%). None of the patients reported presence
of category for PU wounds.
Theme 2: Methodological quality of the studies
Differences were observed between the studies that were included in the review,
based on their characteristics and their methodological quality. While most of the studies
were based on cross-sectional observations, some also utilised retrospective data for
determining the prevalence of PU and their outcomes on the selected population. A cross-
sectional approach was employed in nine of the included studies, for assessing the prevalence
rate of PU among members of the target population. Barrois et al. (2008) adopted a cross-
sectional research approach for assessing the rates of PU in the year 2004, across different
French hospital and primarily used a methodology where data was analysed from a
representative subset of a population at a specific point of time. The study conducted across
the Swedish County Councils by Gunningberg, Stotts and Idvall (2011) and Gunningberg et
13.50%, and 12.3%, respectively in the year 2006, 2007, 2008, and 2009, respectively.
Furthermore, the overall preference in acute care units was 13.3%, 13.4%, 13.10%, and
11.9% for the corresponding years from 2006 to 2009 (Catherine VanGilder et al. 2009).
The study that reported findings from the first International PU Prevalence™ Study
followed the NPUAP classification system and categorised PU prevalence in four different
stages from the year 1989 to 2005. While prevalence of stage 1 ranged from 39 % to 34%,
those for stage 2 and stage 3 range from 39% to 37% and 14% to 7% respectively. Stage 4
ulcer prevalence was found to range from 8% to 7%, from 1989 to 2005 (VanGilder, C.,
MacFarlane and Meyer 2008). The EPUAP-NPUAP PU classification system was also used
in a study conducted in Indonesia, where the prevalence of PU including category 1 was
found to be 28%, while that excluding category 1 was 7%. Moreover, upon classifying the
frequency of PU based on these category, category 1 (57%) was found to be the most
prevalent, followed by category 2 (29%) and 3 (14%). None of the patients reported presence
of category for PU wounds.
Theme 2: Methodological quality of the studies
Differences were observed between the studies that were included in the review,
based on their characteristics and their methodological quality. While most of the studies
were based on cross-sectional observations, some also utilised retrospective data for
determining the prevalence of PU and their outcomes on the selected population. A cross-
sectional approach was employed in nine of the included studies, for assessing the prevalence
rate of PU among members of the target population. Barrois et al. (2008) adopted a cross-
sectional research approach for assessing the rates of PU in the year 2004, across different
French hospital and primarily used a methodology where data was analysed from a
representative subset of a population at a specific point of time. The study conducted across
the Swedish County Councils by Gunningberg, Stotts and Idvall (2011) and Gunningberg et
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
43MSC NURSING
al. (2013) also focused on cross-sectional study designs, where all participants from the
County Councils and Municipalities were invited for determining the presence of PU among
them. Both of these cross-sectional studies is involved collection of data across one day, with
the use of different surveys that contained questions on risk assessment, gender, age, location
of PU, its categories, prevention, strategies and skin observation. Similar cross-sectional
design was also adopted across Brazilian hospitals for determining the incidence and
prevalence of PU in long-term care units, and the data were collected with the use of a paper-
based instruments, the records of which related on statistical analysis using chi-square test,
Fisher's exact test, student's T test, and analysis of variance (da Silva Cardoso et al. 2010).
Alja'afreh and Mosleh (2013) and Bernardes and Caliri (2016) also adopted this observational
research design for recognising the point prevalence of PU in emergency units of different
hospitals, and tertiary public hospital in Jordan, respectively.
The research that was based on concluding findings from the US based International
PU Prevalence Survey (IPUP) also adopted a cross-sectional and observational cohort design
for determining the overall prevalence of PU in the years 2008 and 2009. The quality of care
that was provided to patients having suffered stroke, diagnosed with PU was also determined
by another cross-sectional study conducted by Amir et al. (2013) in Indonesia. Therefore, it
can be suggested that most of the studies had high methodological quality, owing to the
advantages of a cross-sectional approach namely, the ease of gathering much needed
information, cost-effectiveness of the design, collection of data on multiple variables within a
snapshot of time, and ability to utilise the outcomes or findings for creating new theories. The
study conducted by Amir, Meijers and Halfens (2011) utilised the retrospective approach
where the primary aim of the research is to evaluate exposure to certain suspected risk factors
of production factors, in relation to the outcome, specifically PU that was established at the
beginning of the research. The primary advantage of conducting this kind of longitudinal
al. (2013) also focused on cross-sectional study designs, where all participants from the
County Councils and Municipalities were invited for determining the presence of PU among
them. Both of these cross-sectional studies is involved collection of data across one day, with
the use of different surveys that contained questions on risk assessment, gender, age, location
of PU, its categories, prevention, strategies and skin observation. Similar cross-sectional
design was also adopted across Brazilian hospitals for determining the incidence and
prevalence of PU in long-term care units, and the data were collected with the use of a paper-
based instruments, the records of which related on statistical analysis using chi-square test,
Fisher's exact test, student's T test, and analysis of variance (da Silva Cardoso et al. 2010).
Alja'afreh and Mosleh (2013) and Bernardes and Caliri (2016) also adopted this observational
research design for recognising the point prevalence of PU in emergency units of different
hospitals, and tertiary public hospital in Jordan, respectively.
The research that was based on concluding findings from the US based International
PU Prevalence Survey (IPUP) also adopted a cross-sectional and observational cohort design
for determining the overall prevalence of PU in the years 2008 and 2009. The quality of care
that was provided to patients having suffered stroke, diagnosed with PU was also determined
by another cross-sectional study conducted by Amir et al. (2013) in Indonesia. Therefore, it
can be suggested that most of the studies had high methodological quality, owing to the
advantages of a cross-sectional approach namely, the ease of gathering much needed
information, cost-effectiveness of the design, collection of data on multiple variables within a
snapshot of time, and ability to utilise the outcomes or findings for creating new theories. The
study conducted by Amir, Meijers and Halfens (2011) utilised the retrospective approach
where the primary aim of the research is to evaluate exposure to certain suspected risk factors
of production factors, in relation to the outcome, specifically PU that was established at the
beginning of the research. The primary advantage of conducting this kind of longitudinal
44MSC NURSING
cohort study is that it provides clarity regarding the temporal sequence of whether a certain
exposure preceded the outcome that is being investigated, and facilitates calculation of
incidence of a particular disease, with respect to the absolute risk relative risk and attributable
proportion. However, measurement of incidence is not the primary focus of this systematic
review.
One major disadvantage that can be attributed to the methodological quality of those
scholarly articles that had employed retrospective approach is that it often becomes difficult
to recognise an accurately exposed cohort and a corresponding comparison group in such
studies. In addition, differential losses might also have added to bias in the results of the
retrospective studies. A similar retrospective design was also adopted in two other articles
that presented findings from a secondary analysis of data conducted in Philadelphia hospitals
during 1998 and 2001, and nine surveys that were conducted between 1989-2005 (Keelaghan
et al. 2008; VanGilder, MacFarlane and Meyer 2008).
The inclusion and exclusion criteria were not clearly defined in all of the studies.
While the retrospective study by Amir, Meijers and Halfens (2011) clearly stated that adult
patients (≥ 18 years old) in all acute care units were considered eligible to participate, the
study by Barrois et al. (2008) included all placement except those who are admitted to the
accident on emergency department. Patients belonging to the psychiatric, maternity/obstetric,
skin, rehabilitation, and ENT units were excluded from the first study, based on expectations
of low prevalence of PU cases in those units. Gunningberg, Stotts and Idvall (2011) also
included patients aged ≥18 years, who were admitted before midnight to critical care,
geriatric, medical-surgical or gero-psychiatric units, the day the study was conducted and
excluded those from maternity, psychiatric or hospice units. However, Gunningberg et al.
(2013) only mentioned that adult patients who had been admitted to the hospital on the day of
data collection, prior to 7:00 a.m. were included in the study. Adult patients who had earlier
cohort study is that it provides clarity regarding the temporal sequence of whether a certain
exposure preceded the outcome that is being investigated, and facilitates calculation of
incidence of a particular disease, with respect to the absolute risk relative risk and attributable
proportion. However, measurement of incidence is not the primary focus of this systematic
review.
One major disadvantage that can be attributed to the methodological quality of those
scholarly articles that had employed retrospective approach is that it often becomes difficult
to recognise an accurately exposed cohort and a corresponding comparison group in such
studies. In addition, differential losses might also have added to bias in the results of the
retrospective studies. A similar retrospective design was also adopted in two other articles
that presented findings from a secondary analysis of data conducted in Philadelphia hospitals
during 1998 and 2001, and nine surveys that were conducted between 1989-2005 (Keelaghan
et al. 2008; VanGilder, MacFarlane and Meyer 2008).
The inclusion and exclusion criteria were not clearly defined in all of the studies.
While the retrospective study by Amir, Meijers and Halfens (2011) clearly stated that adult
patients (≥ 18 years old) in all acute care units were considered eligible to participate, the
study by Barrois et al. (2008) included all placement except those who are admitted to the
accident on emergency department. Patients belonging to the psychiatric, maternity/obstetric,
skin, rehabilitation, and ENT units were excluded from the first study, based on expectations
of low prevalence of PU cases in those units. Gunningberg, Stotts and Idvall (2011) also
included patients aged ≥18 years, who were admitted before midnight to critical care,
geriatric, medical-surgical or gero-psychiatric units, the day the study was conducted and
excluded those from maternity, psychiatric or hospice units. However, Gunningberg et al.
(2013) only mentioned that adult patients who had been admitted to the hospital on the day of
data collection, prior to 7:00 a.m. were included in the study. Adult patients who had earlier
45MSC NURSING
been diagnosed with PU and who had developed the condition upon admission to Brazilian
hospitals were considered to meet the eligibility criteria for another study that excluded
psychiatric, obstetric, and paediatric wards from the data collection procedure (da Silva
Cardoso et al. 2010). Similar inclusion and exclusion criteria were also defined by Bernardes
and Caliri (2016) who included adult patients admitted on the data collection day and
excluded those who were present in burn units. Alja'afreh and Mosleh (2013) and Keelaghan
(2008) failed to provide accurate description regarding the inclusion and exclusion criteria
that was followed during the data collection procedure. Although no exclusion criteria was
provided by Amir et al. (2013) they clearly stated that all stroke patients who had been
staying in the ICU, CVCU, and neurological units were included in the research. Thus, it can
be stated that most of the studies included in the review were able to report adequately only
the inclusion criteria that was followed. Adequate information on obtaining informed consent
was also presented in the articles.
Theme 3: Location of the PU
The localised injuries of PU are most commonly found in sites that overlay the heels,
sacrum, hips, coccyx, knees, elbows, and ankles. Barrois et al. (2008) stated that maximum
prevalence of PU was found in the heels (53%) and the sacrum (29%) among the patients
with obliterative arterial disease, and urine or fecal matter incontinence, respectively. Similar
findings were reported by Gunningberg, Stotts and Idvall (2011) that the maximum
prevalence of PU was found in the heels (37%), followed by the sacrum (32.6%) and the hips
(3.0%). These results were consistent to the data presented in another study, where the
sacrum (5.7%), foot (1.8%), and heels (4.9%) were identified to be the most affected regions,
among people in hospital settings. The value of corresponded to 3.5%, 3.5% and 4.7% for the
regions, among patients who were present in home or municipal settings (Gunningberg et al.
2013). In the words of da Silva Cardoso et al. (2010) 47% PU was found in the central region
been diagnosed with PU and who had developed the condition upon admission to Brazilian
hospitals were considered to meet the eligibility criteria for another study that excluded
psychiatric, obstetric, and paediatric wards from the data collection procedure (da Silva
Cardoso et al. 2010). Similar inclusion and exclusion criteria were also defined by Bernardes
and Caliri (2016) who included adult patients admitted on the data collection day and
excluded those who were present in burn units. Alja'afreh and Mosleh (2013) and Keelaghan
(2008) failed to provide accurate description regarding the inclusion and exclusion criteria
that was followed during the data collection procedure. Although no exclusion criteria was
provided by Amir et al. (2013) they clearly stated that all stroke patients who had been
staying in the ICU, CVCU, and neurological units were included in the research. Thus, it can
be stated that most of the studies included in the review were able to report adequately only
the inclusion criteria that was followed. Adequate information on obtaining informed consent
was also presented in the articles.
Theme 3: Location of the PU
The localised injuries of PU are most commonly found in sites that overlay the heels,
sacrum, hips, coccyx, knees, elbows, and ankles. Barrois et al. (2008) stated that maximum
prevalence of PU was found in the heels (53%) and the sacrum (29%) among the patients
with obliterative arterial disease, and urine or fecal matter incontinence, respectively. Similar
findings were reported by Gunningberg, Stotts and Idvall (2011) that the maximum
prevalence of PU was found in the heels (37%), followed by the sacrum (32.6%) and the hips
(3.0%). These results were consistent to the data presented in another study, where the
sacrum (5.7%), foot (1.8%), and heels (4.9%) were identified to be the most affected regions,
among people in hospital settings. The value of corresponded to 3.5%, 3.5% and 4.7% for the
regions, among patients who were present in home or municipal settings (Gunningberg et al.
2013). In the words of da Silva Cardoso et al. (2010) 47% PU was found in the central region
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
46MSC NURSING
among patients, who had only one such ulcer in their body. Maximum cases of PU were
found to occur in the calcaneus region (28.75%), followed by the sacrum (22.61%) in a cross-
sectional study that was conducted across emergency hospital. Furthermore, the heels and the
sacral plant were associated with maximum deep tissue injury (Bernardes and Caliri (2016).
These findings were consistent with study carried out by Alja'afreh and Mosleh
(2013) in Jordan, where highest prevalence was found in the sacrum (43%), followed by the
heels (24%), calf (3%), and hip (10%). PUs were most commonly found in the sacrum
(39.2%), heels (19.6%), ischium (14.6%), and trochanter (5%), among residents of a nursing
home who had been transferred to a hospital (Keelaghan et al. 2008). Analysis of a 3 year-
unit specific research made the researchers conclude that PUs were most prevalent in the
sacral region (17%) and ear (20%) among all the patients. These findings were consistent
with those presented by Shahin, Dassen and Halfens (2008) who identified the heels and
sacrum to be the most affected regions of the body (39.4% and 25.2%, respectively).
VanGilder, MacFarlane and Meyer (2008) also provided exhaustive evidence for the fact that
the sacrum (28%), heels (23.6%) and buttocks (17.2%) were primarily affected among
patients being diagnosed with PU.
Discussion
Impacts of pressure ulcer
Pressure ulcers are considered as a significant health problem in most parts of the
world, not only due to the financial constraints that they put on the patient and the healthcare
providers, but also in terms of the pain, human suffering, loss of productive time,
disfigurement, and changes in body images that follow the condition. From the articles
discussed above it can be stated that PU is widely prevalent among people who are admitted
to acute units in all hospitals, which in turn creates an impact on their overall wellbeing,
among patients, who had only one such ulcer in their body. Maximum cases of PU were
found to occur in the calcaneus region (28.75%), followed by the sacrum (22.61%) in a cross-
sectional study that was conducted across emergency hospital. Furthermore, the heels and the
sacral plant were associated with maximum deep tissue injury (Bernardes and Caliri (2016).
These findings were consistent with study carried out by Alja'afreh and Mosleh
(2013) in Jordan, where highest prevalence was found in the sacrum (43%), followed by the
heels (24%), calf (3%), and hip (10%). PUs were most commonly found in the sacrum
(39.2%), heels (19.6%), ischium (14.6%), and trochanter (5%), among residents of a nursing
home who had been transferred to a hospital (Keelaghan et al. 2008). Analysis of a 3 year-
unit specific research made the researchers conclude that PUs were most prevalent in the
sacral region (17%) and ear (20%) among all the patients. These findings were consistent
with those presented by Shahin, Dassen and Halfens (2008) who identified the heels and
sacrum to be the most affected regions of the body (39.4% and 25.2%, respectively).
VanGilder, MacFarlane and Meyer (2008) also provided exhaustive evidence for the fact that
the sacrum (28%), heels (23.6%) and buttocks (17.2%) were primarily affected among
patients being diagnosed with PU.
Discussion
Impacts of pressure ulcer
Pressure ulcers are considered as a significant health problem in most parts of the
world, not only due to the financial constraints that they put on the patient and the healthcare
providers, but also in terms of the pain, human suffering, loss of productive time,
disfigurement, and changes in body images that follow the condition. From the articles
discussed above it can be stated that PU is widely prevalent among people who are admitted
to acute units in all hospitals, which in turn creates an impact on their overall wellbeing,
47MSC NURSING
health related quality of life (HRQoL), length of hospitalization and health care costs. A
retrospective population-based study was conducted with the use of the minimum Data Set
Health Assessment among long-term care residents, in Ontario who had been subjected to
these assessments from May 2004- November 2007. Analysis of the results suggested that an
estimated 9% of the total 16531 LTC residence had been diagnosed with PU that
corresponded to Stage 2 or higher degree. 0.26 ± 0.13 and 0.36 ± 0.17 were the mean ± SD
MDS-HSI scores, for all the residents, with or without PU. Furthermore, the factors that were
associated with the highest prevalence comprised of female gender, increase in age, and
previous presence of PU, recent fracture in the hip, presence of multiple comorbid conditions,
incontinence, end stage disease, and clinical depression. All of the mentioned factors
contributed to a low health related quality of life among all the LTC residents, who had been
diagnosed with ulcer, when compared to their known non-ulcer counterparts (Thein et al.
2010).
The findings presented by Lala et al. (2014) suggested that presence of PU among
381 individuals resulted in a reduction of daily activities to some extent (65.3%) among the
people. PU was also found to reduce ability of all individuals who had suffered from spinal
cord injury to actively participate in 19 of the 26 enlisted daily and community activities.
Moreover, the findings also suggested that individuals who had been diagnosed with one or
two PU reported more dissatisfaction with their disability and incapability to take part in
activities of daily living, when compared to those people who did not have any PU
(p=0.0077). Pus increased prevalence were also correlated with a significant number of
consultations with nurses, family, physicians, wound care nurses, specialists, and
occupational therapist, thereby providing evidence for the high healthcare costs that are
associated with the condition. Iizaka et al. (2010) also conducted a study to investigate the
impact that nutrition related factors and nutritional status created on the severity and
health related quality of life (HRQoL), length of hospitalization and health care costs. A
retrospective population-based study was conducted with the use of the minimum Data Set
Health Assessment among long-term care residents, in Ontario who had been subjected to
these assessments from May 2004- November 2007. Analysis of the results suggested that an
estimated 9% of the total 16531 LTC residence had been diagnosed with PU that
corresponded to Stage 2 or higher degree. 0.26 ± 0.13 and 0.36 ± 0.17 were the mean ± SD
MDS-HSI scores, for all the residents, with or without PU. Furthermore, the factors that were
associated with the highest prevalence comprised of female gender, increase in age, and
previous presence of PU, recent fracture in the hip, presence of multiple comorbid conditions,
incontinence, end stage disease, and clinical depression. All of the mentioned factors
contributed to a low health related quality of life among all the LTC residents, who had been
diagnosed with ulcer, when compared to their known non-ulcer counterparts (Thein et al.
2010).
The findings presented by Lala et al. (2014) suggested that presence of PU among
381 individuals resulted in a reduction of daily activities to some extent (65.3%) among the
people. PU was also found to reduce ability of all individuals who had suffered from spinal
cord injury to actively participate in 19 of the 26 enlisted daily and community activities.
Moreover, the findings also suggested that individuals who had been diagnosed with one or
two PU reported more dissatisfaction with their disability and incapability to take part in
activities of daily living, when compared to those people who did not have any PU
(p=0.0077). Pus increased prevalence were also correlated with a significant number of
consultations with nurses, family, physicians, wound care nurses, specialists, and
occupational therapist, thereby providing evidence for the high healthcare costs that are
associated with the condition. Iizaka et al. (2010) also conducted a study to investigate the
impact that nutrition related factors and nutritional status created on the severity and
48MSC NURSING
development of PU that were acquired in home settings. The data collected by the researchers
established a strong correlation between malnutrition and higher rates of ulcer, following and
adjustment of the other risk factors (OR-2.29, 95% CI; 1.53-3.44). Besides, after assessing
the nutritional status of all the enrolled patients, the researchers established an association
between adequate dietary intakes with lower odds for developing the condition. Severity of
PU was also considered to be a major manifestation of malnutrition among patients who were
present in home settings (OR= 1.88, 95% CI; 1.03-3.45).
Results from another retrospective observational study that was conducted among
3198 patients who were aged more than 75 years at a German university hospital suggested
that 7.1 % of them had a quiet PU during their stay in the hospital. Of these, 7.3% were
classified into categories 1 and 2. While the mean age for all the patients was 81.6 years,
those for PU patients 83.2 years. The impacts of PU were associated with an increased
overall stay in hospitals (19.0 vs 9.9 days) and excess length of stay (.6 vs 0.3 days). A
statistically significant association was established between hospital acquired PU and the
increase in the length of hospitalization among the affected patients, when compared to those
who had acquired ulcer at the time of hospital admission (p=0.0011) (Theisen, Drabik and
Stock 2012). According to Pieper (2012) PU prevalence was considered as a second
diagnosis for an estimated 300,000 patients and accounted for more than $43,180 costs
related to hospitalization. Data findings established the fact that facility associated pressure
ulcers were responsible for an increase in length of stay, subsequent increase in risk of
developing health complications, and resulted in a delay in the recuperation of all patients.
Besides, the data presented in this study were also able to establish the fact that
hospitalization is most often required for severe PU, due to the need for surgical repair or
debridement for sepsis treatment.
development of PU that were acquired in home settings. The data collected by the researchers
established a strong correlation between malnutrition and higher rates of ulcer, following and
adjustment of the other risk factors (OR-2.29, 95% CI; 1.53-3.44). Besides, after assessing
the nutritional status of all the enrolled patients, the researchers established an association
between adequate dietary intakes with lower odds for developing the condition. Severity of
PU was also considered to be a major manifestation of malnutrition among patients who were
present in home settings (OR= 1.88, 95% CI; 1.03-3.45).
Results from another retrospective observational study that was conducted among
3198 patients who were aged more than 75 years at a German university hospital suggested
that 7.1 % of them had a quiet PU during their stay in the hospital. Of these, 7.3% were
classified into categories 1 and 2. While the mean age for all the patients was 81.6 years,
those for PU patients 83.2 years. The impacts of PU were associated with an increased
overall stay in hospitals (19.0 vs 9.9 days) and excess length of stay (.6 vs 0.3 days). A
statistically significant association was established between hospital acquired PU and the
increase in the length of hospitalization among the affected patients, when compared to those
who had acquired ulcer at the time of hospital admission (p=0.0011) (Theisen, Drabik and
Stock 2012). According to Pieper (2012) PU prevalence was considered as a second
diagnosis for an estimated 300,000 patients and accounted for more than $43,180 costs
related to hospitalization. Data findings established the fact that facility associated pressure
ulcers were responsible for an increase in length of stay, subsequent increase in risk of
developing health complications, and resulted in a delay in the recuperation of all patients.
Besides, the data presented in this study were also able to establish the fact that
hospitalization is most often required for severe PU, due to the need for surgical repair or
debridement for sepsis treatment.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
49MSC NURSING
Nursing knowledge and attitude on pressure ulcer
One major consideration that needs to be taken into account from the thematic
analysis is that all nursing professionals should hold adequate knowledge and a positive
attitude towards prevention of PU in all patients whom they deliver care. Results presented in
a cross-sectional study conducted across Belgian hospital suggested that the prevalence of
category 1-4 PU among 2105 patients was approximately 13.5% (n=284). However, as much
is 30% of all the patients (n=625) were found to be at a risk (presence of PU and or Braden
score <17). The findings suggested that only 87 of the 625 patients (13.92%) had received
adequate prevention strategies when they were seated or present in bed. The mean attitude
and knowledge score among the nurses working in the Belgian hospitals were 71.3% and
49.7%, respectively. The authors failed to establish any independent correlation between
nursing knowledge and application of appropriate intervention strategies. Hence, the findings
provided enough evidence to suggest that knowledge among the nurses working in Belgian
hospitals on PU and its treatment was quite inadequate (Beeckman et al. 2011). These
findings were consistent with those presented by Demarré et al. (2012) who conducted
similar study across Belgian nursing homes and stated that only 6.9% of the nursing home
residents, found at risk demonstrated adequate compliance to the prevention strategies. The
mean knowledge scores were 28.7% for all nursing assistants, in comparison to 29.3% of the
nurses. Significant differences were also observed in their overall attitude scores, with a total
score of 74.5%. The nursing professionals were found to display a positive attitude towards
prevention of PU, when compared to nursing assistants (78.3% vs 72.3%, respectively). This
made the authors conclude that positive attitude among nursing professionals acted as a
significant predictor for showing compliance with the prevention guidelines on PU, which
were provided to all the residents who were identified at an increased risk of development of
the condition.
Nursing knowledge and attitude on pressure ulcer
One major consideration that needs to be taken into account from the thematic
analysis is that all nursing professionals should hold adequate knowledge and a positive
attitude towards prevention of PU in all patients whom they deliver care. Results presented in
a cross-sectional study conducted across Belgian hospital suggested that the prevalence of
category 1-4 PU among 2105 patients was approximately 13.5% (n=284). However, as much
is 30% of all the patients (n=625) were found to be at a risk (presence of PU and or Braden
score <17). The findings suggested that only 87 of the 625 patients (13.92%) had received
adequate prevention strategies when they were seated or present in bed. The mean attitude
and knowledge score among the nurses working in the Belgian hospitals were 71.3% and
49.7%, respectively. The authors failed to establish any independent correlation between
nursing knowledge and application of appropriate intervention strategies. Hence, the findings
provided enough evidence to suggest that knowledge among the nurses working in Belgian
hospitals on PU and its treatment was quite inadequate (Beeckman et al. 2011). These
findings were consistent with those presented by Demarré et al. (2012) who conducted
similar study across Belgian nursing homes and stated that only 6.9% of the nursing home
residents, found at risk demonstrated adequate compliance to the prevention strategies. The
mean knowledge scores were 28.7% for all nursing assistants, in comparison to 29.3% of the
nurses. Significant differences were also observed in their overall attitude scores, with a total
score of 74.5%. The nursing professionals were found to display a positive attitude towards
prevention of PU, when compared to nursing assistants (78.3% vs 72.3%, respectively). This
made the authors conclude that positive attitude among nursing professionals acted as a
significant predictor for showing compliance with the prevention guidelines on PU, which
were provided to all the residents who were identified at an increased risk of development of
the condition.
50MSC NURSING
On assessing the knowledge and attitudes towards prevention of PU among patients,
admitted to intensive care units (ICUs), researchers of a particular study found that the means
scores for attitudes were 34 ± 4. The research findings made the authors identify that 48.6%
of the nursing professionals were able to correctly categorise PU based on their severity, with
the use of assessment scales. However, the enrolled nurses demonstrated less capability of
correct categorisation of the condition. Preventive measures that were most commonly known
to the nursing staff were adequate nutritional support (36.1%) and pressure relief systems
(97.3%). In addition, some of the major barriers that were reported by the nurses that
impeded the delivery of appropriate care services to PU patients were severity in illness of
the patient (28.9%), lack of proper time (57.8%), inadequate access to pressure relieving
mattress and other equipment (35.5%), and poor knowledge (38%). These findings also
highlighted on the fact that increasing the knowledge among nursing professionals would
serve as an essential step towards prevention of PU (Strand and Lindgren 2010).
The results were in accordance to the findings presented by Iranmanesh et al. (2011)
that elaborated on the fact that the nursing professionals enrolled for the study could correctly
provide answer to 54.36% of the questions that were administered to them. The results of the
study showed that the category of PU evaluation had 83·35% correct answers, highest in
comparison to other categories. This insufficiency in the level of knowledge about PU among
the nursing professionals therefore calls the need for increasing an awareness and creating
provisions for adequate training and education. These would help them identify the
underlying factors and pathophysiology associated with the condition and implement
appropriate intervention strategies in their future practice.
Approximately half of the nursing staff demonstrated good knowledge (54.4%) and
14.4% of them manifested adequate practice on prevention of PU, in another study that was
conducted in Northwest Ethiopia. Significant correlation was established on knowledge on
On assessing the knowledge and attitudes towards prevention of PU among patients,
admitted to intensive care units (ICUs), researchers of a particular study found that the means
scores for attitudes were 34 ± 4. The research findings made the authors identify that 48.6%
of the nursing professionals were able to correctly categorise PU based on their severity, with
the use of assessment scales. However, the enrolled nurses demonstrated less capability of
correct categorisation of the condition. Preventive measures that were most commonly known
to the nursing staff were adequate nutritional support (36.1%) and pressure relief systems
(97.3%). In addition, some of the major barriers that were reported by the nurses that
impeded the delivery of appropriate care services to PU patients were severity in illness of
the patient (28.9%), lack of proper time (57.8%), inadequate access to pressure relieving
mattress and other equipment (35.5%), and poor knowledge (38%). These findings also
highlighted on the fact that increasing the knowledge among nursing professionals would
serve as an essential step towards prevention of PU (Strand and Lindgren 2010).
The results were in accordance to the findings presented by Iranmanesh et al. (2011)
that elaborated on the fact that the nursing professionals enrolled for the study could correctly
provide answer to 54.36% of the questions that were administered to them. The results of the
study showed that the category of PU evaluation had 83·35% correct answers, highest in
comparison to other categories. This insufficiency in the level of knowledge about PU among
the nursing professionals therefore calls the need for increasing an awareness and creating
provisions for adequate training and education. These would help them identify the
underlying factors and pathophysiology associated with the condition and implement
appropriate intervention strategies in their future practice.
Approximately half of the nursing staff demonstrated good knowledge (54.4%) and
14.4% of them manifested adequate practice on prevention of PU, in another study that was
conducted in Northwest Ethiopia. Significant correlation was established on knowledge on
51MSC NURSING
PU prevention with work experience (OR = 4.8, 95% CI; 1.31-10.62), formal training
experience (OR = 4.1, 95% CI; 1.29-9.92), and educational status (OR = 2.4, 95% CI; 1.39-
4.15). Moreover, satisfaction with the leadership exhibited by nursing seniors, inadequate
equipment and facility for pressure relief and shortage of staff were associated with reduced
practice and poor attitude towards the condition among nurses (Nurut al. 2015).
Upon conducting a similar cross-sectional multicenter study across four hospitals
situated in Jordan, the researchers found that experience of all the participants (nursing
assistants and registered nurses) were significant factors that created a positive attitude
among them regarding the prevailing condition. An increase in the number of years of
professional experience was significantly correlated with enhancement of positive attitude.
However, showing similarity with the previously discussed study, lack of time management
(83.6%), severity of patient conditions (68.6%) and inadequate nursing staff (86.2%) acted as
major barriers to the practice.
Nursing implications and preventive strategies in pressure ulcer
According to Chou et al. (2013), PUs are associated with substantial health burden
but it is preventable. The review of the literature highlighted that PU significantly affect the
health-related quality of life (HRQoL) of the patients. So in order to improve HROoL, the
first attention that comes into consideration in nursing implication include therapy plan for
the prevention and cure of pressure ulcers. The systematic review conducted by McInneset al.
(2015)highlighted that use pressure-relieving support surfaces like beds, mattresses, seat
cushions can be used to prevent the occurrence of pressure ulcers in elderly patients who are
suffering from chronic illness and are bedridden for a prolong period of time. McInnes et al.
(2015) mainly stressed over the use of high-specific foam mattresses in comparison to the
standard foam mattresses available in hospital for the prevention of pressure ulcers. However,
the study failed to highlight relative merits of higher-specific low pressure constant and
PU prevention with work experience (OR = 4.8, 95% CI; 1.31-10.62), formal training
experience (OR = 4.1, 95% CI; 1.29-9.92), and educational status (OR = 2.4, 95% CI; 1.39-
4.15). Moreover, satisfaction with the leadership exhibited by nursing seniors, inadequate
equipment and facility for pressure relief and shortage of staff were associated with reduced
practice and poor attitude towards the condition among nurses (Nurut al. 2015).
Upon conducting a similar cross-sectional multicenter study across four hospitals
situated in Jordan, the researchers found that experience of all the participants (nursing
assistants and registered nurses) were significant factors that created a positive attitude
among them regarding the prevailing condition. An increase in the number of years of
professional experience was significantly correlated with enhancement of positive attitude.
However, showing similarity with the previously discussed study, lack of time management
(83.6%), severity of patient conditions (68.6%) and inadequate nursing staff (86.2%) acted as
major barriers to the practice.
Nursing implications and preventive strategies in pressure ulcer
According to Chou et al. (2013), PUs are associated with substantial health burden
but it is preventable. The review of the literature highlighted that PU significantly affect the
health-related quality of life (HRQoL) of the patients. So in order to improve HROoL, the
first attention that comes into consideration in nursing implication include therapy plan for
the prevention and cure of pressure ulcers. The systematic review conducted by McInneset al.
(2015)highlighted that use pressure-relieving support surfaces like beds, mattresses, seat
cushions can be used to prevent the occurrence of pressure ulcers in elderly patients who are
suffering from chronic illness and are bedridden for a prolong period of time. McInnes et al.
(2015) mainly stressed over the use of high-specific foam mattresses in comparison to the
standard foam mattresses available in hospital for the prevention of pressure ulcers. However,
the study failed to highlight relative merits of higher-specific low pressure constant and
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
52MSC NURSING
alternating-pressure support surfaces in reduces the chances of developing pressure ulcers.
McInnes et al. (2015) further recommended that the nursing professionals must use foams for
the pressure reliefs in order to treat high-risk patients in the operating theaters. In relation to
the use pressure mattress, Chouet al. (2013)stated that advanced static support surfaces are
more effective in comparison to the standard mattress for the prevention of ulcers among the
higher-risk population. However, Gillespie et al. (20114) highlighted that thought the use of
foam mattresses might be regarded as an effective means of controlling pressure ulcers
especially in the hips and the low-backside of the body but it at times turn out to be cost. It
that case, one of the effective intervention proposed by the Gillespie et al. (20114) include
repositioning. Gillespie et al. (20114) highlighted that bed sores or the pressure ulcers mainly
results from rubbing or friction over the weight bearing bony points of the body like the
heels, elbows and the hips. Repositioning can be regarded as an important cost effective
strategy that can use used alongside with other effective preventive strategies in order to
relieve pressure and thereby relieving pressure ulcers. Repositioning mainly involves moving
the person in different position in order to redistribute the pressure from any specific part of
the body. However, Gillespieet al. (20114)failed to highlight any particular position which is
effective in comparison to others towards preventing PU. Callet al. (2015)highlighted the use
of proper wound dressing in preventing PU. Call et al. (2015) stated that use of wound
dressing helps to reduce the amplitude of shear stress and friction damaging the skin of the
patient’s a risk. The use of wound dressing mainly causes re-distribution of pressure based
upon the effect of Poisson ratio and greater area of deflection and thereby providing greater
load redistribution. Other preventive strategy of pressure ulcers include use of antibiotic,
negative pressure wound therapy and reconstructive surgery (Bhattacharya and Mishra 2015).
The study conducted by Gorecki et al. (2012) highlighted that the patient only accepts
to adhere to the treatment only if they are assured about the effectiveness of the treatment in
alternating-pressure support surfaces in reduces the chances of developing pressure ulcers.
McInnes et al. (2015) further recommended that the nursing professionals must use foams for
the pressure reliefs in order to treat high-risk patients in the operating theaters. In relation to
the use pressure mattress, Chouet al. (2013)stated that advanced static support surfaces are
more effective in comparison to the standard mattress for the prevention of ulcers among the
higher-risk population. However, Gillespie et al. (20114) highlighted that thought the use of
foam mattresses might be regarded as an effective means of controlling pressure ulcers
especially in the hips and the low-backside of the body but it at times turn out to be cost. It
that case, one of the effective intervention proposed by the Gillespie et al. (20114) include
repositioning. Gillespie et al. (20114) highlighted that bed sores or the pressure ulcers mainly
results from rubbing or friction over the weight bearing bony points of the body like the
heels, elbows and the hips. Repositioning can be regarded as an important cost effective
strategy that can use used alongside with other effective preventive strategies in order to
relieve pressure and thereby relieving pressure ulcers. Repositioning mainly involves moving
the person in different position in order to redistribute the pressure from any specific part of
the body. However, Gillespieet al. (20114)failed to highlight any particular position which is
effective in comparison to others towards preventing PU. Callet al. (2015)highlighted the use
of proper wound dressing in preventing PU. Call et al. (2015) stated that use of wound
dressing helps to reduce the amplitude of shear stress and friction damaging the skin of the
patient’s a risk. The use of wound dressing mainly causes re-distribution of pressure based
upon the effect of Poisson ratio and greater area of deflection and thereby providing greater
load redistribution. Other preventive strategy of pressure ulcers include use of antibiotic,
negative pressure wound therapy and reconstructive surgery (Bhattacharya and Mishra 2015).
The study conducted by Gorecki et al. (2012) highlighted that the patient only accepts
to adhere to the treatment only if they are assured about the effectiveness of the treatment in
53MSC NURSING
improving their overall condition from debilitating PU. Moreover, inconsistent management
of PU also contributes to the generation of anxiety, depression and loss of hope. Moreover,
patient also feels restricted as occurrence of PU limits their social activities which further
increase the level of depression and a sense of social isolation. Inconsistent use of complex
healthcare terminologies increases the confusion about the overall therapy plan and thereby
decreasing the overall healthoutcome (Gorecki et al. 2012). So it is the duty of the nursing
professionals to explain the concept of treatment of pressure ulcer to the patient’s before in
clear and understandable language. According to Hibbard and Greene (2013) proper
explanation of the care plan to the patient equates to patient activation along with
understanding of one’s role in the care process and this increases the adherence to the
treatment along with patient engagement which leads to the overall increase in the therapy
outcome. This concept is extremely significant during the process of skin grafting. Proper
explanation to the patient about the necessity of skin grafting in treatment PU increases
patient participation in the care process. A successful skin grafting not only provides
therapeutic benefits but also helps to increase the health related quality of life of the patients
along with increase in the overall self-esteem(Lourenco et al. 2014). Salomé, Blanes and
Ferreira (2014) tested the efficacy of skin-grafting along with nursing counseling with patient
with venous leg ulcers and found to record improved outcome in comparison to the
compression therapy done by Unna’s boot.
Taking into consideration of the high rate of occurrence of PU in the acute ward, it is
better to conduct risk assessment in order to denote the high risk patients for PU. Moore and
Cowman (2014) stated that the use of pressure ulcer risk assessment tools helps in
comprehensive assessment process in order to identify patients who are at risk of developing
pressure ulcer. Moore and Cowman (2014) mainly stressed over Braden risk assessment toll
over successful risk assessment of PU. Moore and Cowman (2014) are of the opinion that
improving their overall condition from debilitating PU. Moreover, inconsistent management
of PU also contributes to the generation of anxiety, depression and loss of hope. Moreover,
patient also feels restricted as occurrence of PU limits their social activities which further
increase the level of depression and a sense of social isolation. Inconsistent use of complex
healthcare terminologies increases the confusion about the overall therapy plan and thereby
decreasing the overall healthoutcome (Gorecki et al. 2012). So it is the duty of the nursing
professionals to explain the concept of treatment of pressure ulcer to the patient’s before in
clear and understandable language. According to Hibbard and Greene (2013) proper
explanation of the care plan to the patient equates to patient activation along with
understanding of one’s role in the care process and this increases the adherence to the
treatment along with patient engagement which leads to the overall increase in the therapy
outcome. This concept is extremely significant during the process of skin grafting. Proper
explanation to the patient about the necessity of skin grafting in treatment PU increases
patient participation in the care process. A successful skin grafting not only provides
therapeutic benefits but also helps to increase the health related quality of life of the patients
along with increase in the overall self-esteem(Lourenco et al. 2014). Salomé, Blanes and
Ferreira (2014) tested the efficacy of skin-grafting along with nursing counseling with patient
with venous leg ulcers and found to record improved outcome in comparison to the
compression therapy done by Unna’s boot.
Taking into consideration of the high rate of occurrence of PU in the acute ward, it is
better to conduct risk assessment in order to denote the high risk patients for PU. Moore and
Cowman (2014) stated that the use of pressure ulcer risk assessment tools helps in
comprehensive assessment process in order to identify patients who are at risk of developing
pressure ulcer. Moore and Cowman (2014) mainly stressed over Braden risk assessment toll
over successful risk assessment of PU. Moore and Cowman (2014) are of the opinion that
54MSC NURSING
risk assessment tool helps to provide standard results in comparison to other tools which are
denoted to be unstructured. However, detection of at risk patients does not reduce the risk of
developing PU. Only proper application of the nursing interventions like pressure bed or
repositioning along with proper mental counselling helps in reducing the occurrence and
chornicity of PU. Sving et al. (2014) state that the chances of developing PU increases with
age however, nursing professionals plays less significant role in determining the high risk
patients and this increases the overall prevalence rate of PU. So the healthcare leaders must
come forward in establishing routines of different evidence-based practices in PU prevention
and at the same time registered nurses need to assume their best responsibility at the bed-side
(Sving et al. 2014).
Limitations
However, there were some limitations in the review. One major limitation is related to
the fact that the review did not adequately report on RCTs that might have predisposed the
assessment and thematic analysis to bias. It is usually difficult to ascertain as to which
elements of quality assessment are extrapolative of valid outcomes and which checklist is
able to best assesses the quality of the papers. Small sample size was another major
limitation. Owing to the fact that only 12 articles were included in the thematic analysis, it
might have affected reliability of the results. Thus, it might have resulted in settling down for
less conclusive results, owing to higher variability. Not performing a meta-analysis by
combining the prevalence data obtained from the 12 studies was another significant
limitation. This would have facilitated increasing the precision of the prevalence effects and
analysing the differences that existed in the results among the included studies.
risk assessment tool helps to provide standard results in comparison to other tools which are
denoted to be unstructured. However, detection of at risk patients does not reduce the risk of
developing PU. Only proper application of the nursing interventions like pressure bed or
repositioning along with proper mental counselling helps in reducing the occurrence and
chornicity of PU. Sving et al. (2014) state that the chances of developing PU increases with
age however, nursing professionals plays less significant role in determining the high risk
patients and this increases the overall prevalence rate of PU. So the healthcare leaders must
come forward in establishing routines of different evidence-based practices in PU prevention
and at the same time registered nurses need to assume their best responsibility at the bed-side
(Sving et al. 2014).
Limitations
However, there were some limitations in the review. One major limitation is related to
the fact that the review did not adequately report on RCTs that might have predisposed the
assessment and thematic analysis to bias. It is usually difficult to ascertain as to which
elements of quality assessment are extrapolative of valid outcomes and which checklist is
able to best assesses the quality of the papers. Small sample size was another major
limitation. Owing to the fact that only 12 articles were included in the thematic analysis, it
might have affected reliability of the results. Thus, it might have resulted in settling down for
less conclusive results, owing to higher variability. Not performing a meta-analysis by
combining the prevalence data obtained from the 12 studies was another significant
limitation. This would have facilitated increasing the precision of the prevalence effects and
analysing the differences that existed in the results among the included studies.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
55MSC NURSING
Chapter 5:
Conclusion
Thus from the detailed analysis conducted in the literature review in relation to the
prevalence of PU, it can be concluded that the prevalence rate of pressure ulcer is
significantly higher in the acute wards and it is a major health concern. The main target group
of population for PU are the patients suffering from diabetes mellitus and is patients who
belong to the category of older adults. The increase in the rate of occurrence of PU with
diabetes indicated that delay in wound healing and poor nutritional backup increase the
prevalence rate of PU. Among male and female, the female gender is more prone in getting
affected with PU due to their high tenderness in skin. Increase in age increases the tendency
of developing chronic diseases which demands prolong bed rest or at times forces the patients
to become bed-ridden all these increase the total amount to time spent while lying over the
bed. Increase in the bed rest time causes increase in friction of the skin of the body over the
surface of the bed, leading to the development of PU. Main the parts of the body which
carriers the maximum body load like the hips, heels, sacrum and the elbows are the main
target for PUs. Patient with frequent obliterative arterial disease have higher chances of
developing heel PU. Whereas patients with urine or fecal matter complications have high
reported cases of sacral PU which is one of the most common form of PU. Apart from these
main pressure points of the body, PUs, also leads to the formation of severe lesions through
the body. The review of literature also highlighted that there are no strict of clear values of
the reported cases of PU under the hospital ward and the main reason highlighted against this
is difficulties in conducting studies over incidence and prevalence and difficulty in defining
the population which is being studied. The main modes of studies which are attempted in
order to detect the prevalence rate of PU include cross-sectional study. It was regarded as an
important approach in determining the PU in the French hospital; ward. In this cross-sectional
Chapter 5:
Conclusion
Thus from the detailed analysis conducted in the literature review in relation to the
prevalence of PU, it can be concluded that the prevalence rate of pressure ulcer is
significantly higher in the acute wards and it is a major health concern. The main target group
of population for PU are the patients suffering from diabetes mellitus and is patients who
belong to the category of older adults. The increase in the rate of occurrence of PU with
diabetes indicated that delay in wound healing and poor nutritional backup increase the
prevalence rate of PU. Among male and female, the female gender is more prone in getting
affected with PU due to their high tenderness in skin. Increase in age increases the tendency
of developing chronic diseases which demands prolong bed rest or at times forces the patients
to become bed-ridden all these increase the total amount to time spent while lying over the
bed. Increase in the bed rest time causes increase in friction of the skin of the body over the
surface of the bed, leading to the development of PU. Main the parts of the body which
carriers the maximum body load like the hips, heels, sacrum and the elbows are the main
target for PUs. Patient with frequent obliterative arterial disease have higher chances of
developing heel PU. Whereas patients with urine or fecal matter complications have high
reported cases of sacral PU which is one of the most common form of PU. Apart from these
main pressure points of the body, PUs, also leads to the formation of severe lesions through
the body. The review of literature also highlighted that there are no strict of clear values of
the reported cases of PU under the hospital ward and the main reason highlighted against this
is difficulties in conducting studies over incidence and prevalence and difficulty in defining
the population which is being studied. The main modes of studies which are attempted in
order to detect the prevalence rate of PU include cross-sectional study. It was regarded as an
important approach in determining the PU in the French hospital; ward. In this cross-sectional
56MSC NURSING
studies mainly used representative subset of a population at any definite point of time in order
to access the rate of prevalence of PU. The main mode of data collection used for detecting
PU include paper-based instruments and records because these mode of data collection can be
easily related with the statistical analysis via the use of chi-square test. Apart from corss-
sectional study design, retrospective approach is also found to be effective in detecting the
rate of occurrence of PU as this type of study design help to evaluate the exposure of
suspected risk factors behind the development of PU. The main risk factor underlying the
prevalence of PU revealed the occurrence of PU is mainly hospital acquired and most of
these are characterised under stage 1 non-blanchable erythema rest hospital acquired PUs
belong to category 2 and 3 and these indicates partial thickness or skin loss or full thickness
of skin loss respectively. Thus on visualizing the prevalence story of PU, it can be stated that
the vulnerability of developing PU mostly increases with age, the tenure of hospitalization,
lack of adequate physical activity, decrease in the overall sensory perception and increase in
the rate of friction or shear of the skin with the surface of the bed.
The analysis of the papers in relation to pressure ulcer highlighted that the pressure
ulcers cause pain increases human suffering along with the loss of productive time and
change in the overall image of the body and all these lead to decrease in the overall health
related quality of life of the patient along with an increase in the rate of hospitalization and
increase in the overall healthcare cost. Loss of productive time is mainly attributed with the
lack of proper physical activity. Lack of proper physical activity decreases the scope of
performing daily living activities which decreases the overall self-esteem of the individual.
This decrease in self-esteem is mostly profound among the people who are suffering from the
spinal cord injury as their chronicity of PU are higher in comparison to others. The
prevalence of PU is also co-related with the significant number of consultations with the
nurses, family members, healthcare professionals and other wound care nurses and thus
studies mainly used representative subset of a population at any definite point of time in order
to access the rate of prevalence of PU. The main mode of data collection used for detecting
PU include paper-based instruments and records because these mode of data collection can be
easily related with the statistical analysis via the use of chi-square test. Apart from corss-
sectional study design, retrospective approach is also found to be effective in detecting the
rate of occurrence of PU as this type of study design help to evaluate the exposure of
suspected risk factors behind the development of PU. The main risk factor underlying the
prevalence of PU revealed the occurrence of PU is mainly hospital acquired and most of
these are characterised under stage 1 non-blanchable erythema rest hospital acquired PUs
belong to category 2 and 3 and these indicates partial thickness or skin loss or full thickness
of skin loss respectively. Thus on visualizing the prevalence story of PU, it can be stated that
the vulnerability of developing PU mostly increases with age, the tenure of hospitalization,
lack of adequate physical activity, decrease in the overall sensory perception and increase in
the rate of friction or shear of the skin with the surface of the bed.
The analysis of the papers in relation to pressure ulcer highlighted that the pressure
ulcers cause pain increases human suffering along with the loss of productive time and
change in the overall image of the body and all these lead to decrease in the overall health
related quality of life of the patient along with an increase in the rate of hospitalization and
increase in the overall healthcare cost. Loss of productive time is mainly attributed with the
lack of proper physical activity. Lack of proper physical activity decreases the scope of
performing daily living activities which decreases the overall self-esteem of the individual.
This decrease in self-esteem is mostly profound among the people who are suffering from the
spinal cord injury as their chronicity of PU are higher in comparison to others. The
prevalence of PU is also co-related with the significant number of consultations with the
nurses, family members, healthcare professionals and other wound care nurses and thus
57MSC NURSING
leading to an overall hike in the health care cost. It is obvious that development of PU
increases the overall stay in the hospital which further increases the overall healthcare cost.
Delay in healing of the PU and lack of proper treatment of PU is mainly attributed
towards the lack of proper risk assessment tool for the detection of the high risk patients with
PU along with lack of proper knowledge of the nursing professionals tin treating PU
effectively. Thematic analysis highlighted that the attitude and knowledge score among the
nursing professionals who are working in the acute care unit are considerably poor in
treatment PU. Nurses also showed inadequate complication to the prevention strategies
towards PU. The nursed lack positive attitude and proper bedside knowledge in treating PU
among the hospital patients. Their lack of knowledge increases the overall prevalence rate of
pressure ulcers in the acute ward of the hospitals. ICU wards nurses at times failed to
correctly categorise PUs and demonstrate less capability of proper therapy plan for the PU.
Due to their lack of knowledge they are unable to explain the therapy plan to the patient
properly in easy language which are understandable to the patients. This lack of knowledge
and failure in explaining the patient about the impending therapy and expected outcome
decreases the overall participation of the patient in the therapy plan. Lack of patient consent
in the therapy plan decreases the overall therapy outcome. It recommended that increase in
knowledge of the nursing professionals about the therapy planning under the training of the
doctors or the physicians help in improving the overall health related outcomes and thereby
helping to improve the overall quality of life.
Recommendation
Proper nursing education towards the prevention of the pressure ulcer must be
directed towards the utilization of the proper nursing interventions in treating PUs. Some of
the popular nursing interventions that are found effective in treating PUs include use of
support surfaces like beds, seat cushions and mattresses. This pressure surfaces like the foam
leading to an overall hike in the health care cost. It is obvious that development of PU
increases the overall stay in the hospital which further increases the overall healthcare cost.
Delay in healing of the PU and lack of proper treatment of PU is mainly attributed
towards the lack of proper risk assessment tool for the detection of the high risk patients with
PU along with lack of proper knowledge of the nursing professionals tin treating PU
effectively. Thematic analysis highlighted that the attitude and knowledge score among the
nursing professionals who are working in the acute care unit are considerably poor in
treatment PU. Nurses also showed inadequate complication to the prevention strategies
towards PU. The nursed lack positive attitude and proper bedside knowledge in treating PU
among the hospital patients. Their lack of knowledge increases the overall prevalence rate of
pressure ulcers in the acute ward of the hospitals. ICU wards nurses at times failed to
correctly categorise PUs and demonstrate less capability of proper therapy plan for the PU.
Due to their lack of knowledge they are unable to explain the therapy plan to the patient
properly in easy language which are understandable to the patients. This lack of knowledge
and failure in explaining the patient about the impending therapy and expected outcome
decreases the overall participation of the patient in the therapy plan. Lack of patient consent
in the therapy plan decreases the overall therapy outcome. It recommended that increase in
knowledge of the nursing professionals about the therapy planning under the training of the
doctors or the physicians help in improving the overall health related outcomes and thereby
helping to improve the overall quality of life.
Recommendation
Proper nursing education towards the prevention of the pressure ulcer must be
directed towards the utilization of the proper nursing interventions in treating PUs. Some of
the popular nursing interventions that are found effective in treating PUs include use of
support surfaces like beds, seat cushions and mattresses. This pressure surfaces like the foam
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
58MSC NURSING
mattresses helps in the redistribution of the pressures throughout the body and thus helping to
reduce the chances of developing PUs. However, the use of foam or the pressure mattress are
at times creates financial constraints and thereby leading to an increase in the overall
healthcare cost. So an effective alternative of pressure mattress is repositioning of the
patients, Repositioning also helps to decrease rubbing or friction of the skin surface bearing
body points of body and thus decreases the chance of encountering PU. However, most
effective location of prepositioning are not highlighted in the studies and is usually done in a
trial and error method. So use of repositioning is recommended along with the use of the
pressure mattresses. Use of wound dressing is also found to provide effective results in
treatment of PU and thus regarded as an important nursing intervention under the prevention
strategies of PU. Wound dressing helps to decrease the amplitude of the sheer stress and the
friction which damages the skin. Use of wound dressing helps in re-distribution of pressure
and thus providing greater load distribution and decreasing the severity or the chances of
occurrence of PUs.
However, before the application of any particular therapy plan, proper risk assessment
of the patients must be conducted. Here risk assessment means the chances of developing PU
among the high risk patients. The main risk assessment tool that is used to identify the high
risk patient of PU is Braden risk assessment tool. It is one of the most structured tools that
help in identifying the high risk patients of PU. However, detection of at risk patients does
not help in reducing or chances of developing PU. Proper application of non-pharmacological
and pharmacological interventions will help in successful prevention of PU. Of
pharmacological preventive strategy of PU, there are use of antibiotic therapy and skin
grafting. The analysis of the results highlighted that the use of proper skin grafting surgery
use to improve the severity of PU along with an improvement of self-esteem of the patient.
However, it is the duty of the nursing professionals to make the patient understand the
mattresses helps in the redistribution of the pressures throughout the body and thus helping to
reduce the chances of developing PUs. However, the use of foam or the pressure mattress are
at times creates financial constraints and thereby leading to an increase in the overall
healthcare cost. So an effective alternative of pressure mattress is repositioning of the
patients, Repositioning also helps to decrease rubbing or friction of the skin surface bearing
body points of body and thus decreases the chance of encountering PU. However, most
effective location of prepositioning are not highlighted in the studies and is usually done in a
trial and error method. So use of repositioning is recommended along with the use of the
pressure mattresses. Use of wound dressing is also found to provide effective results in
treatment of PU and thus regarded as an important nursing intervention under the prevention
strategies of PU. Wound dressing helps to decrease the amplitude of the sheer stress and the
friction which damages the skin. Use of wound dressing helps in re-distribution of pressure
and thus providing greater load distribution and decreasing the severity or the chances of
occurrence of PUs.
However, before the application of any particular therapy plan, proper risk assessment
of the patients must be conducted. Here risk assessment means the chances of developing PU
among the high risk patients. The main risk assessment tool that is used to identify the high
risk patient of PU is Braden risk assessment tool. It is one of the most structured tools that
help in identifying the high risk patients of PU. However, detection of at risk patients does
not help in reducing or chances of developing PU. Proper application of non-pharmacological
and pharmacological interventions will help in successful prevention of PU. Of
pharmacological preventive strategy of PU, there are use of antibiotic therapy and skin
grafting. The analysis of the results highlighted that the use of proper skin grafting surgery
use to improve the severity of PU along with an improvement of self-esteem of the patient.
However, it is the duty of the nursing professionals to make the patient understand the
59MSC NURSING
importance of the therapy and its expected outcomes. Explaining the therapy process clearly
to the patient helps to increase the overall patient participation in the care plan and hereby
helping to increase the overall health outcomes. However, explanation must be done in
simple langue so that it becomes easier for the patients to understand the overall prognosis of
the therapy and the disease. For these proper nursing training about the required interventions
for the prevention of PU is important. Optimal application of the non-pharmacological and
the pharmacological interventions for the prevention of PU helps to decrease the prevalence
rate of PU along with an improvement of HROoL of the patients.
importance of the therapy and its expected outcomes. Explaining the therapy process clearly
to the patient helps to increase the overall patient participation in the care plan and hereby
helping to increase the overall health outcomes. However, explanation must be done in
simple langue so that it becomes easier for the patients to understand the overall prognosis of
the therapy and the disease. For these proper nursing training about the required interventions
for the prevention of PU is important. Optimal application of the non-pharmacological and
the pharmacological interventions for the prevention of PU helps to decrease the prevalence
rate of PU along with an improvement of HROoL of the patients.
60MSC NURSING
References
Alja'afreh, M. and Mosleh, S.M., 2013. Pressure ulcers in Jordan: a snapshot survey of a
tertiary public hospital. British Journal of Nursing, 22(Sup15), pp.S10-S16.
Amir, Y., Halfens, R.J.G., Lohrmann, C. and Schols, J.M.G.A., 2013. Pressure ulcer
prevalence and quality of care in stroke patients in an Indonesian hospital. Journal of wound
care, 22(5), pp.254-260.
Amir, Y., Meijers, J. and Halfens, R., 2011. Retrospective study of pressure ulcer prevalence
in Dutch general hospitals since 2001. Journal of wound care, 20(1), pp.18-25.
Anderson, D.J., Podgorny, K., Berrios-Torres, S.I., Bratzler, D.W., Dellinger, E.P., Greene,
L., Nyquist, A.C., Saiman, L., Yokoe, D.S., Maragakis, L.L. and Kaye, K.S., 2014. Strategies
to prevent surgical site infections in acute care hospitals: 2014 update. Infection Control &
Hospital Epidemiology, 35(S2), pp.S66-S88.
Austin, P.C., 2011. An introduction to propensity score methods for reducing the effects of
confounding in observational studies. Multivariate behavioral research, 46(3), pp.399-424.
Aveyard, H., 2014. Doing a literature review in health and social care: A practical guide.
McGraw-Hill Education (UK).
Baharestani, M.M., Black, J.M., Carville, K., Clark, M., Cuddigan, J.E., Dealey, C., Defloor,
T., Harding, K.G., Lahmann, N.A., Lubbers, M.J. and Lyder, C.H., 2009. Dilemmas in
measuring and using pressure ulcer prevalence and incidence: an international consensus.
International wound journal, 6(2), pp.97-104.
Bain, L.E., Awah, P.K., Geraldine, N., Kindong, N.P., Siga, Y., Bernard, N. and Tanjeko,
A.T., 2013. Malnutrition in Sub–Saharan Africa: burden, causes and prospects. Pan African
Medical Journal, 15(1).
References
Alja'afreh, M. and Mosleh, S.M., 2013. Pressure ulcers in Jordan: a snapshot survey of a
tertiary public hospital. British Journal of Nursing, 22(Sup15), pp.S10-S16.
Amir, Y., Halfens, R.J.G., Lohrmann, C. and Schols, J.M.G.A., 2013. Pressure ulcer
prevalence and quality of care in stroke patients in an Indonesian hospital. Journal of wound
care, 22(5), pp.254-260.
Amir, Y., Meijers, J. and Halfens, R., 2011. Retrospective study of pressure ulcer prevalence
in Dutch general hospitals since 2001. Journal of wound care, 20(1), pp.18-25.
Anderson, D.J., Podgorny, K., Berrios-Torres, S.I., Bratzler, D.W., Dellinger, E.P., Greene,
L., Nyquist, A.C., Saiman, L., Yokoe, D.S., Maragakis, L.L. and Kaye, K.S., 2014. Strategies
to prevent surgical site infections in acute care hospitals: 2014 update. Infection Control &
Hospital Epidemiology, 35(S2), pp.S66-S88.
Austin, P.C., 2011. An introduction to propensity score methods for reducing the effects of
confounding in observational studies. Multivariate behavioral research, 46(3), pp.399-424.
Aveyard, H., 2014. Doing a literature review in health and social care: A practical guide.
McGraw-Hill Education (UK).
Baharestani, M.M., Black, J.M., Carville, K., Clark, M., Cuddigan, J.E., Dealey, C., Defloor,
T., Harding, K.G., Lahmann, N.A., Lubbers, M.J. and Lyder, C.H., 2009. Dilemmas in
measuring and using pressure ulcer prevalence and incidence: an international consensus.
International wound journal, 6(2), pp.97-104.
Bain, L.E., Awah, P.K., Geraldine, N., Kindong, N.P., Siga, Y., Bernard, N. and Tanjeko,
A.T., 2013. Malnutrition in Sub–Saharan Africa: burden, causes and prospects. Pan African
Medical Journal, 15(1).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
61MSC NURSING
Barrois, B., Labalette, C., Rousseau, P., Corbin, A., Colin, D., Allaert, F. and Saumet, J.L.,
2008. A national prevalence study of pressure ulcers in French hospital inpatients. Journal of
wound care, 17(9), pp.373-379.
Beeckman, D., Defloor, T., Schoonhoven, L. and Vanderwee, K., 2011. Knowledge and
attitudes of nurses on pressure ulcer prevention: a cross‐sectional multicenter study in
Belgian hospitals. Worldviews on Evidence‐Based Nursing, 8(3), pp.166-176.
Beeckman, D., Van Lancker, A., Van Hecke, A. and Verhaeghe, S., 2014. A systematic
review and meta‐analysis of incontinence‐associated dermatitis, incontinence, and moisture
as risk factors for pressure ulcer development. Research in nursing & health, 37(3), pp.204-
218.
Bergh, D., and Ketchen, D. J., 2011. Research methodology in Strategy and Management, 1st
ed. Bingley: Emerald Group Publishing Ltd
Bernardes, R.M. and Caliri, M.H.L., 2016. Pressure ulcer prevalence in emergency hospitals:
a cross-sectional study. Online Brazilian Journal of Nursing, 15(2), pp.236-244.
Bettany-Saltikov, J., 2012. How to do a systematic literature review in nursing: a step-by-
step guide. McGraw-Hill Education (UK).
Bhattacharya, S. and Mishra, R.K., 2015. Pressure ulcers: current understanding and newer
modalities of treatment. Indian Journal of Plastic Surgery: Official Publication of the
Association of Plastic Surgeons of India, 48(1), p.4.
Biglari, B., Büchler, A., Reitzel, T., Swing, T., Gerner, H.J., Ferbert, T. and Moghaddam, A.,
2014. A retrospective study on flap complications after pressure ulcer surgery in spinal cord-
injured patients. Spinal Cord, 52(1), p.80.
Barrois, B., Labalette, C., Rousseau, P., Corbin, A., Colin, D., Allaert, F. and Saumet, J.L.,
2008. A national prevalence study of pressure ulcers in French hospital inpatients. Journal of
wound care, 17(9), pp.373-379.
Beeckman, D., Defloor, T., Schoonhoven, L. and Vanderwee, K., 2011. Knowledge and
attitudes of nurses on pressure ulcer prevention: a cross‐sectional multicenter study in
Belgian hospitals. Worldviews on Evidence‐Based Nursing, 8(3), pp.166-176.
Beeckman, D., Van Lancker, A., Van Hecke, A. and Verhaeghe, S., 2014. A systematic
review and meta‐analysis of incontinence‐associated dermatitis, incontinence, and moisture
as risk factors for pressure ulcer development. Research in nursing & health, 37(3), pp.204-
218.
Bergh, D., and Ketchen, D. J., 2011. Research methodology in Strategy and Management, 1st
ed. Bingley: Emerald Group Publishing Ltd
Bernardes, R.M. and Caliri, M.H.L., 2016. Pressure ulcer prevalence in emergency hospitals:
a cross-sectional study. Online Brazilian Journal of Nursing, 15(2), pp.236-244.
Bettany-Saltikov, J., 2012. How to do a systematic literature review in nursing: a step-by-
step guide. McGraw-Hill Education (UK).
Bhattacharya, S. and Mishra, R.K., 2015. Pressure ulcers: current understanding and newer
modalities of treatment. Indian Journal of Plastic Surgery: Official Publication of the
Association of Plastic Surgeons of India, 48(1), p.4.
Biglari, B., Büchler, A., Reitzel, T., Swing, T., Gerner, H.J., Ferbert, T. and Moghaddam, A.,
2014. A retrospective study on flap complications after pressure ulcer surgery in spinal cord-
injured patients. Spinal Cord, 52(1), p.80.
62MSC NURSING
Boland, A., Cherry, M G and Dickson, R. 2014. Doing a systematic review :
a student's guide. Sage Publications. London.
Brienza, D., Antokal, S., Herbe, L., Logan, S., Maguire, J., Van Ranst, J. and Siddiqui, A.,
2015. Friction-induced skin injuries—are they pressure ulcers? An updated NPUAP white
paper. Journal of Wound Ostomy & Continence Nursing, 42(1), pp.62-64.
Call, E., Pedersen, J., Bill, B., Black, J., Alves, P., Brindle, C.T., Dealey, C., Santamaria, N.
and Clark, M., 2015. Enhancing pressure ulcer prevention using wound dressings: what are
the modes of action?. International wound journal, 12(4), pp.408-413.
Catherine Houghton, R.G.N., Dympna Casey, R.G.N. and David Shaw PhD, C., 2013. Rigour
in qualitative case-study research. Nurse Researcher (through 2013), 20(4), p.12.
Catherine VanGilder, M., Amlung, S., Harrison, P. and Meyer, S., 2009. Results of the 2008–
2009 International Pressure Ulcer Prevalence™ Survey and a 3-year, acute care, unit-specific
analysis. Ostomy Wound Manage, 55, pp.39-45.
Chan, B.C., Nanwa, N., Mittmann, N., Bryant, D., Coyte, P.C. and Houghton, P.E., 2013.
The average cost of pressure ulcer management in a community dwelling spinal cord injury
population. International wound journal, 10(4), pp.431-440.
Chou, R., Dana, T., Bougatsos, C., Blazina, I., Starmer, A.J., Reitel, K. and Buckley, D.I.,
2013. Pressure ulcer risk assessment and prevention: a systematic comparative effectiveness
review. Annals of Internal Medicine, 159(1), pp.28-38.
Coleman, S., Nixon, J., Keen, J., Wilson, L., McGinnis, E., Dealey, C., Stubbs, N., Farrin, A.,
Dowding, D., Schols, J.M. and Cuddigan, J., 2014. A new pressure ulcer conceptual
framework. Journal of advanced nursing, 70(10), pp.2222-2234.
Boland, A., Cherry, M G and Dickson, R. 2014. Doing a systematic review :
a student's guide. Sage Publications. London.
Brienza, D., Antokal, S., Herbe, L., Logan, S., Maguire, J., Van Ranst, J. and Siddiqui, A.,
2015. Friction-induced skin injuries—are they pressure ulcers? An updated NPUAP white
paper. Journal of Wound Ostomy & Continence Nursing, 42(1), pp.62-64.
Call, E., Pedersen, J., Bill, B., Black, J., Alves, P., Brindle, C.T., Dealey, C., Santamaria, N.
and Clark, M., 2015. Enhancing pressure ulcer prevention using wound dressings: what are
the modes of action?. International wound journal, 12(4), pp.408-413.
Catherine Houghton, R.G.N., Dympna Casey, R.G.N. and David Shaw PhD, C., 2013. Rigour
in qualitative case-study research. Nurse Researcher (through 2013), 20(4), p.12.
Catherine VanGilder, M., Amlung, S., Harrison, P. and Meyer, S., 2009. Results of the 2008–
2009 International Pressure Ulcer Prevalence™ Survey and a 3-year, acute care, unit-specific
analysis. Ostomy Wound Manage, 55, pp.39-45.
Chan, B.C., Nanwa, N., Mittmann, N., Bryant, D., Coyte, P.C. and Houghton, P.E., 2013.
The average cost of pressure ulcer management in a community dwelling spinal cord injury
population. International wound journal, 10(4), pp.431-440.
Chou, R., Dana, T., Bougatsos, C., Blazina, I., Starmer, A.J., Reitel, K. and Buckley, D.I.,
2013. Pressure ulcer risk assessment and prevention: a systematic comparative effectiveness
review. Annals of Internal Medicine, 159(1), pp.28-38.
Coleman, S., Nixon, J., Keen, J., Wilson, L., McGinnis, E., Dealey, C., Stubbs, N., Farrin, A.,
Dowding, D., Schols, J.M. and Cuddigan, J., 2014. A new pressure ulcer conceptual
framework. Journal of advanced nursing, 70(10), pp.2222-2234.
63MSC NURSING
Cooper, K.L., 2013. Evidence-based prevention of pressure ulcers in the intensive care
unit. Critical care nurse, 33(6), pp.57-66.
Coughlan, M., Cronin, P. and Ryan, F., 2013. Doing a Literature Review in Nursing, Health
and Social Care: SAGE Publications. Sage.
Cremasco, M.F., Wenzel, F., Zanei, S.S. and Whitaker, I.Y., 2013. Pressure ulcers in the
intensive care unit: the relationship between nursing workload, illness severity and pressure
ulcer risk. Journal of Clinical Nursing, 22(15-16), pp.2183-2191.
Creswell, J.W. and Clark, V.L.P., 2017. Designing and conducting mixed methods research.
Sage publications.
Crowther, D., and Lancaster, G., 2012. Research Methods, 2nd ed. London: Routledge.
da Silva Cardoso, J.R., Blanes, L., Augusto Calil, J., Ferreira Chacon, J.M. and Masako
Ferreira, L., 2010. Prevalence of pressure ulcers in a Brazilian hospital: results of a cross-
sectional study. Ostomy/wound management, 56(10), p.52.
Dealey, C., Posnett, J. and Walker, A., 2012. The cost of pressure ulcers in the United
Kingdom. Journal of wound care, 21(6), pp.261-266.
Delmore, B., Cox, J., Rolnitzky, L., Chu, A. and Stolfi, A., 2015. Differentiating a pressure
ulcer from acute skin failure in the adult critical care patient. Advances in skin & wound
care, 28(11), pp.514-524.
Demarré, L., Van Lancker, A., Van Hecke, A., Verhaeghe, S., Grypdonck, M., Lemey, J.,
Annemans, L. and Beeckman, D., 2015. The cost of prevention and treatment of pressure
ulcers: a systematic review. International journal of nursing studies, 52(11), pp.1754-1774.
Cooper, K.L., 2013. Evidence-based prevention of pressure ulcers in the intensive care
unit. Critical care nurse, 33(6), pp.57-66.
Coughlan, M., Cronin, P. and Ryan, F., 2013. Doing a Literature Review in Nursing, Health
and Social Care: SAGE Publications. Sage.
Cremasco, M.F., Wenzel, F., Zanei, S.S. and Whitaker, I.Y., 2013. Pressure ulcers in the
intensive care unit: the relationship between nursing workload, illness severity and pressure
ulcer risk. Journal of Clinical Nursing, 22(15-16), pp.2183-2191.
Creswell, J.W. and Clark, V.L.P., 2017. Designing and conducting mixed methods research.
Sage publications.
Crowther, D., and Lancaster, G., 2012. Research Methods, 2nd ed. London: Routledge.
da Silva Cardoso, J.R., Blanes, L., Augusto Calil, J., Ferreira Chacon, J.M. and Masako
Ferreira, L., 2010. Prevalence of pressure ulcers in a Brazilian hospital: results of a cross-
sectional study. Ostomy/wound management, 56(10), p.52.
Dealey, C., Posnett, J. and Walker, A., 2012. The cost of pressure ulcers in the United
Kingdom. Journal of wound care, 21(6), pp.261-266.
Delmore, B., Cox, J., Rolnitzky, L., Chu, A. and Stolfi, A., 2015. Differentiating a pressure
ulcer from acute skin failure in the adult critical care patient. Advances in skin & wound
care, 28(11), pp.514-524.
Demarré, L., Van Lancker, A., Van Hecke, A., Verhaeghe, S., Grypdonck, M., Lemey, J.,
Annemans, L. and Beeckman, D., 2015. The cost of prevention and treatment of pressure
ulcers: a systematic review. International journal of nursing studies, 52(11), pp.1754-1774.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
64MSC NURSING
Demarré, L., Vanderwee, K., Defloor, T., Verhaeghe, S., Schoonhoven, L. and Beeckman,
D., 2012. Pressure ulcers: knowledge and attitude of nurses and nursing assistants in Belgian
nursing homes. Journal of clinical nursing, 21(9‐10), pp.1425-1434.
Edsberg, L.E., Black, J.M., Goldberg, M., McNichol, L., Moore, L. and Sieggreen, M., 2016.
Revised National Pressure Ulcer Advisory Panel pressure injury staging system: revised
pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing, 43(6),
p.585.
Edwards, H., Finlayson, K., Skerman, H., Alexander, K., Miaskowski, C., Aouizerat, B. and
Gibb, M., 2014. Identification of symptom clusters in patients with chronic venous leg
ulcers. Journal of pain and symptom management, 47(5), pp.867-875.
Ellis, T., and Levy, Y., 2012. ‘Towards a guide for novice researchers on research
methodology: Review and proposed methods’, Issues in Informing Science and Information
Technology, 6, 323-337.
Fogerty, M., Guy, J., Barbul, A., Nanney, L.B. and Abumrad, N.N., 2009. African Americans
show increased risk for pressure ulcers: a retrospective analysis of acute care hospitals in
America. Wound repair and regeneration, 17(5), pp.678-684.
Fu Shaw, L., Chang, P.C., Lee, J.F., Kung, H.Y. and Tung, T.H., 2014. Incidence and
predicted risk factors of pressure ulcers in surgical patients: experience at a medical center in
Taipei, Taiwan. BioMed research international, 2014.
Gillespie, B.M., Chaboyer, W.P., McInnis, E., Kent, B., Whitty, J.A. and Thalib, L., 2014.
Repositioning for pressure ulcer prevention in adults. Cochrane Database of Systematic
Reviews, 4(4).
Demarré, L., Vanderwee, K., Defloor, T., Verhaeghe, S., Schoonhoven, L. and Beeckman,
D., 2012. Pressure ulcers: knowledge and attitude of nurses and nursing assistants in Belgian
nursing homes. Journal of clinical nursing, 21(9‐10), pp.1425-1434.
Edsberg, L.E., Black, J.M., Goldberg, M., McNichol, L., Moore, L. and Sieggreen, M., 2016.
Revised National Pressure Ulcer Advisory Panel pressure injury staging system: revised
pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing, 43(6),
p.585.
Edwards, H., Finlayson, K., Skerman, H., Alexander, K., Miaskowski, C., Aouizerat, B. and
Gibb, M., 2014. Identification of symptom clusters in patients with chronic venous leg
ulcers. Journal of pain and symptom management, 47(5), pp.867-875.
Ellis, T., and Levy, Y., 2012. ‘Towards a guide for novice researchers on research
methodology: Review and proposed methods’, Issues in Informing Science and Information
Technology, 6, 323-337.
Fogerty, M., Guy, J., Barbul, A., Nanney, L.B. and Abumrad, N.N., 2009. African Americans
show increased risk for pressure ulcers: a retrospective analysis of acute care hospitals in
America. Wound repair and regeneration, 17(5), pp.678-684.
Fu Shaw, L., Chang, P.C., Lee, J.F., Kung, H.Y. and Tung, T.H., 2014. Incidence and
predicted risk factors of pressure ulcers in surgical patients: experience at a medical center in
Taipei, Taiwan. BioMed research international, 2014.
Gillespie, B.M., Chaboyer, W.P., McInnis, E., Kent, B., Whitty, J.A. and Thalib, L., 2014.
Repositioning for pressure ulcer prevention in adults. Cochrane Database of Systematic
Reviews, 4(4).
65MSC NURSING
Girard, R., Baboi, L., Ayzac, L., Richard, J.C., Guérin, C. and Proseva Trial Group, 2014.
The impact of patient positioning on pressure ulcers in patients with severe ARDS: results
from a multicentre randomised controlled trial on prone positioning. Intensive care
medicine, 40(3), pp.397-403.
Gorecki, C., Nixon, J., Madill, A., Firth, J. and Brown, J.M., 2012. What influences the
impact of pressure ulcers on health-related quality of life? A qualitative patient-focused
exploration of contributory factors. Journal of Tissue Viability, 21(1), pp.3-12.
Goug D., Oliver S., and Thomas J. 2012. An introduction to systematic
reviews. [e-book] Los Angeles, Calif.] ; London: Los Angeles, Calif. ;
London : SAGE.
GOV.UK. (2018). Pressure ulcers: applying All Our Health. [online] Available at:
https://www.gov.uk/government/publications/pressure-ulcers-applying-all-our-health/
pressure-ulcers-applying-all-our-health [Accessed 21 Aug. 2018].
Greenhalgh, T. and Peacock, R., 2005. Effectiveness and efficiency of search methods in
systematic reviews of complex evidence: audit of primary sources. Bmj, 331(7524), pp.1064-
1065.
Gunningberg, L., Hommel, A., Bååth, C. and Idvall, E., 2013. The first national pressure
ulcer prevalence survey in county council and municipality settings in Sweden. Journal of
evaluation in clinical practice, 19(5), pp.862-867.
Gunningberg, L., Stotts, N.A. and Idvall, E., 2011. Hospital‐acquired pressure ulcers in two
Swedish County Councils: cross‐sectional data as the foundation for future quality
improvement. International wound journal, 8(5), pp.465-473.
Girard, R., Baboi, L., Ayzac, L., Richard, J.C., Guérin, C. and Proseva Trial Group, 2014.
The impact of patient positioning on pressure ulcers in patients with severe ARDS: results
from a multicentre randomised controlled trial on prone positioning. Intensive care
medicine, 40(3), pp.397-403.
Gorecki, C., Nixon, J., Madill, A., Firth, J. and Brown, J.M., 2012. What influences the
impact of pressure ulcers on health-related quality of life? A qualitative patient-focused
exploration of contributory factors. Journal of Tissue Viability, 21(1), pp.3-12.
Goug D., Oliver S., and Thomas J. 2012. An introduction to systematic
reviews. [e-book] Los Angeles, Calif.] ; London: Los Angeles, Calif. ;
London : SAGE.
GOV.UK. (2018). Pressure ulcers: applying All Our Health. [online] Available at:
https://www.gov.uk/government/publications/pressure-ulcers-applying-all-our-health/
pressure-ulcers-applying-all-our-health [Accessed 21 Aug. 2018].
Greenhalgh, T. and Peacock, R., 2005. Effectiveness and efficiency of search methods in
systematic reviews of complex evidence: audit of primary sources. Bmj, 331(7524), pp.1064-
1065.
Gunningberg, L., Hommel, A., Bååth, C. and Idvall, E., 2013. The first national pressure
ulcer prevalence survey in county council and municipality settings in Sweden. Journal of
evaluation in clinical practice, 19(5), pp.862-867.
Gunningberg, L., Stotts, N.A. and Idvall, E., 2011. Hospital‐acquired pressure ulcers in two
Swedish County Councils: cross‐sectional data as the foundation for future quality
improvement. International wound journal, 8(5), pp.465-473.
66MSC NURSING
Hibbard, J.H. and Greene, J., 2013. What the evidence shows about patient activation: better
health outcomes and care experiences; fewer data on costs. Health affairs, 32(2), pp.207-214.
Holloway, I. and Galvin, K., 2016. Qualitative research in nursing and healthcare. John
Wiley & Sons.
Iizaka, S., Okuwa, M., Sugama, J. and Sanada, H., 2010. The impact of malnutrition and
nutrition-related factors on the development and severity of pressure ulcers in older patients
receiving home care. Clinical Nutrition, 29(1), pp.47-53.
Iranmanesh, S., Rafiei, H. and Foroogh Ameri, G., 2011. Critical care nurses' knowledge
about pressure ulcer in southeast of Iran. International wound journal, 8(5), pp.459-464.
Kasuya, A., Sakabe, J.I. and Tokura, Y., 2014. Potential application of in vivo imaging of
impaired lymphatic duct to evaluate the severity of pressure ulcer in mouse model. Scientific
reports, 4, p.4173.
Keelaghan, E., Margolis, D., Zhan, M. and Baumgarten, M., 2008. Prevalence of pressure
ulcers on hospital admission among nursing home residents transferred to the
hospital. Wound Repair and Regeneration, 16(3), pp.331-336.
Lala, D., Dumont, F.S., Leblond, J., Houghton, P.E. and Noreau, L., 2014. Impact of pressure
ulcers on individuals living with a spinal cord injury. Archives of physical medicine and
rehabilitation, 95(12), pp.2312-2319.
Lourenco, L., Blanes, L., Salomé, G.M. and Ferreira, L.M., 2014. Quality of life and self-
esteem in patients with paraplegia and pressure ulcers: a controlled cross-sectional
study. Journal of wound care, 23(6), pp.331-337.
Hibbard, J.H. and Greene, J., 2013. What the evidence shows about patient activation: better
health outcomes and care experiences; fewer data on costs. Health affairs, 32(2), pp.207-214.
Holloway, I. and Galvin, K., 2016. Qualitative research in nursing and healthcare. John
Wiley & Sons.
Iizaka, S., Okuwa, M., Sugama, J. and Sanada, H., 2010. The impact of malnutrition and
nutrition-related factors on the development and severity of pressure ulcers in older patients
receiving home care. Clinical Nutrition, 29(1), pp.47-53.
Iranmanesh, S., Rafiei, H. and Foroogh Ameri, G., 2011. Critical care nurses' knowledge
about pressure ulcer in southeast of Iran. International wound journal, 8(5), pp.459-464.
Kasuya, A., Sakabe, J.I. and Tokura, Y., 2014. Potential application of in vivo imaging of
impaired lymphatic duct to evaluate the severity of pressure ulcer in mouse model. Scientific
reports, 4, p.4173.
Keelaghan, E., Margolis, D., Zhan, M. and Baumgarten, M., 2008. Prevalence of pressure
ulcers on hospital admission among nursing home residents transferred to the
hospital. Wound Repair and Regeneration, 16(3), pp.331-336.
Lala, D., Dumont, F.S., Leblond, J., Houghton, P.E. and Noreau, L., 2014. Impact of pressure
ulcers on individuals living with a spinal cord injury. Archives of physical medicine and
rehabilitation, 95(12), pp.2312-2319.
Lourenco, L., Blanes, L., Salomé, G.M. and Ferreira, L.M., 2014. Quality of life and self-
esteem in patients with paraplegia and pressure ulcers: a controlled cross-sectional
study. Journal of wound care, 23(6), pp.331-337.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
67MSC NURSING
Manorama, A., Meyer, R., Wiseman, R. and Bush, T.R., 2013. Quantifying the effects of
external shear loads on arterial and venous blood flow: implications for pressure ulcer
development. Clinical biomechanics, 28(5), pp.574-578.
McGinnis, E., Briggs, M., Collinson, M., Wilson, L., Dealey, C., Brown, J., Coleman, S.,
Stubbs, N., Stevenson, R., Nelson, E.A. and Nixon, J., 2014. Pressure ulcer related pain in
community populations: a prevalence survey. BMC nursing, 13(1), p.16.
McInnes, E., Jammali‐Blasi, A., Bell‐Syer, S.E., Dumville, J.C., Middleton, V. and Cullum,
N., 2015. Support surfaces for pressure ulcer prevention. Cochrane Database of Systematic
Reviews, (9), 1-144.
McIntosh-Scott, A., Mason, T., Mason-Whitehead, E. and Coyle, D., 2013. Key concepts in
nursing and healthcare research. Sage.
Moore, Z.E. and Cowman, S., 2014. Risk assessment tools for the prevention of pressure
ulcers. Cochrane Database of Systematic Reviews, (2).
Nuru, N., Zewdu, F., Amsalu, S. and Mehretie, Y., 2015. Knowledge and practice of nurses
towards prevention of pressure ulcer and associated factors in Gondar University Hospital,
Northwest Ethiopia. BMC nursing, 14(1), p.34.
Padula, W.V., Mishra, M.K., Makic, M.B.F. and Valuck, R.J., 2014. A framework of quality
improvement interventions to implement evidence-based practices for pressure ulcer
prevention. Advances in skin & wound care, 27(6), pp.280-284.
Parahoo, K., (2014). Nursing research: principles, process and issues. Palgrave Macmillan.
Pieper, B., 2012. Pressure ulcers: impact, etiology, and classification. Acute and Chronic
Wounds: Current Management Concepts. 4th ed. St Louis, MO: Mosby, pp.123-135.
Manorama, A., Meyer, R., Wiseman, R. and Bush, T.R., 2013. Quantifying the effects of
external shear loads on arterial and venous blood flow: implications for pressure ulcer
development. Clinical biomechanics, 28(5), pp.574-578.
McGinnis, E., Briggs, M., Collinson, M., Wilson, L., Dealey, C., Brown, J., Coleman, S.,
Stubbs, N., Stevenson, R., Nelson, E.A. and Nixon, J., 2014. Pressure ulcer related pain in
community populations: a prevalence survey. BMC nursing, 13(1), p.16.
McInnes, E., Jammali‐Blasi, A., Bell‐Syer, S.E., Dumville, J.C., Middleton, V. and Cullum,
N., 2015. Support surfaces for pressure ulcer prevention. Cochrane Database of Systematic
Reviews, (9), 1-144.
McIntosh-Scott, A., Mason, T., Mason-Whitehead, E. and Coyle, D., 2013. Key concepts in
nursing and healthcare research. Sage.
Moore, Z.E. and Cowman, S., 2014. Risk assessment tools for the prevention of pressure
ulcers. Cochrane Database of Systematic Reviews, (2).
Nuru, N., Zewdu, F., Amsalu, S. and Mehretie, Y., 2015. Knowledge and practice of nurses
towards prevention of pressure ulcer and associated factors in Gondar University Hospital,
Northwest Ethiopia. BMC nursing, 14(1), p.34.
Padula, W.V., Mishra, M.K., Makic, M.B.F. and Valuck, R.J., 2014. A framework of quality
improvement interventions to implement evidence-based practices for pressure ulcer
prevention. Advances in skin & wound care, 27(6), pp.280-284.
Parahoo, K., (2014). Nursing research: principles, process and issues. Palgrave Macmillan.
Pieper, B., 2012. Pressure ulcers: impact, etiology, and classification. Acute and Chronic
Wounds: Current Management Concepts. 4th ed. St Louis, MO: Mosby, pp.123-135.
68MSC NURSING
Polit, D.F. and Beck, C.T., 2008. Nursing research: Generating and assessing evidence for
nursing practice. Lippincott Williams & Wilkins.
Posthauer, M.E., Banks, M., Dorner, B. and Schols, J.M., 2015. The role of nutrition for
pressure ulcer management: national pressure ulcer advisory panel, European pressure ulcer
advisory panel, and pan pacific pressure injury alliance white paper. Advances in skin &
wound care, 28(4), pp.175-188.
Qaddumi, J. and Khawaldeh, A., 2014. Pressure ulcer prevention knowledge among
Jordanian nurses: a cross-sectional study. BMC nursing, 13(1), p.6.
Robb, M. and Shellenbarger, T., 2014. Strategies for searching and managing evidence-based
practice resources. The Journal of Continuing Education in Nursing, 45(10), pp.461-466.
Ross, J., Stevenson, F., Lau, R. and Murray, E. 2016. Factors that influence the
implementation of e-health: a systematic review of systematic reviews (an
update). Implementation Science, 11(1), pp.729-735.
Salomé, G.M., Blanes, L. and Ferreira, L.M., 2014. The impact of skin grafting on the quality
of life and self-esteem of patients with venous leg ulcers. World journal of surgery, 38(1),
pp.233-240.
Saumure, K. and Given, L.M., 2008. Data saturation. The SAGE encyclopedia of qualitative
research methods, 1, pp.195-196.
Saunders, M.N. and Rojon, C., 2014. There's no madness in my method: explaining how your
coaching research findings are built on firm foundations. Coaching: An International Journal
of Theory, Research and Practice, 7(1), pp.74-83.
Polit, D.F. and Beck, C.T., 2008. Nursing research: Generating and assessing evidence for
nursing practice. Lippincott Williams & Wilkins.
Posthauer, M.E., Banks, M., Dorner, B. and Schols, J.M., 2015. The role of nutrition for
pressure ulcer management: national pressure ulcer advisory panel, European pressure ulcer
advisory panel, and pan pacific pressure injury alliance white paper. Advances in skin &
wound care, 28(4), pp.175-188.
Qaddumi, J. and Khawaldeh, A., 2014. Pressure ulcer prevention knowledge among
Jordanian nurses: a cross-sectional study. BMC nursing, 13(1), p.6.
Robb, M. and Shellenbarger, T., 2014. Strategies for searching and managing evidence-based
practice resources. The Journal of Continuing Education in Nursing, 45(10), pp.461-466.
Ross, J., Stevenson, F., Lau, R. and Murray, E. 2016. Factors that influence the
implementation of e-health: a systematic review of systematic reviews (an
update). Implementation Science, 11(1), pp.729-735.
Salomé, G.M., Blanes, L. and Ferreira, L.M., 2014. The impact of skin grafting on the quality
of life and self-esteem of patients with venous leg ulcers. World journal of surgery, 38(1),
pp.233-240.
Saumure, K. and Given, L.M., 2008. Data saturation. The SAGE encyclopedia of qualitative
research methods, 1, pp.195-196.
Saunders, M.N. and Rojon, C., 2014. There's no madness in my method: explaining how your
coaching research findings are built on firm foundations. Coaching: An International Journal
of Theory, Research and Practice, 7(1), pp.74-83.
69MSC NURSING
Seth, A.K., Geringer, M.R., Hong, S.J., Leung, K.P., Mustoe, T.A. and Galiano, R.D., 2012.
In vivo modeling of biofilm-infected wounds: a review. Journal of surgical research, 178(1),
pp.330-338.
Shahin, E.S., Dassen, T. and Halfens, R.J., 2008. Pressure ulcer prevalence and incidence in
intensive care patients: a literature review. Nursing in critical care, 13(2), pp.71-79.
Solovyev, A., Mi, Q., Tzen, Y.T., Brienza, D. and Vodovotz, Y., 2013. Hybrid
equation/agent-based model of ischemia-induced hyperemia and pressure ulcer formation
predicts greater propensity to ulcerate in subjects with spinal cord injury. PLoS
computational biology, 9(5), p.e1003070.
Strand, T. and Lindgren, M., 2010. Knowledge, attitudes and barriers towards prevention of
pressure ulcers in intensive care units: a descriptive cross-sectional study. Intensive and
critical care nursing, 26(6), pp.335-342.
Sving, E., Idvall, E., Högberg, H. and Gunningberg, L., 2014. Factors contributing to
evidence-based pressure ulcer prevention. A cross-sectional study. International journal of
nursing studies, 51(5), pp.717-725.
Thein, H.H., Gomes, T., Krahn, M.D. and Wodchis, W.P., 2010. Health status utilities and
the impact of pressure ulcers in long-term care residents in Ontario. Quality of life
research, 19(1), pp.81-89.
Theisen, S., Drabik, A. and Stock, S., 2012. Pressure ulcers in older hospitalised patients and
its impact on length of stay: a retrospective observational study. Journal of Clinical
Nursing, 21(3‐4), pp.380-387.
Treadwell, J.R., Singh, S., Talati, R., McPheeters, M.L. and Reston, J.T., 2011. A framework
for" best evidence" approaches in systematic reviews.
Seth, A.K., Geringer, M.R., Hong, S.J., Leung, K.P., Mustoe, T.A. and Galiano, R.D., 2012.
In vivo modeling of biofilm-infected wounds: a review. Journal of surgical research, 178(1),
pp.330-338.
Shahin, E.S., Dassen, T. and Halfens, R.J., 2008. Pressure ulcer prevalence and incidence in
intensive care patients: a literature review. Nursing in critical care, 13(2), pp.71-79.
Solovyev, A., Mi, Q., Tzen, Y.T., Brienza, D. and Vodovotz, Y., 2013. Hybrid
equation/agent-based model of ischemia-induced hyperemia and pressure ulcer formation
predicts greater propensity to ulcerate in subjects with spinal cord injury. PLoS
computational biology, 9(5), p.e1003070.
Strand, T. and Lindgren, M., 2010. Knowledge, attitudes and barriers towards prevention of
pressure ulcers in intensive care units: a descriptive cross-sectional study. Intensive and
critical care nursing, 26(6), pp.335-342.
Sving, E., Idvall, E., Högberg, H. and Gunningberg, L., 2014. Factors contributing to
evidence-based pressure ulcer prevention. A cross-sectional study. International journal of
nursing studies, 51(5), pp.717-725.
Thein, H.H., Gomes, T., Krahn, M.D. and Wodchis, W.P., 2010. Health status utilities and
the impact of pressure ulcers in long-term care residents in Ontario. Quality of life
research, 19(1), pp.81-89.
Theisen, S., Drabik, A. and Stock, S., 2012. Pressure ulcers in older hospitalised patients and
its impact on length of stay: a retrospective observational study. Journal of Clinical
Nursing, 21(3‐4), pp.380-387.
Treadwell, J.R., Singh, S., Talati, R., McPheeters, M.L. and Reston, J.T., 2011. A framework
for" best evidence" approaches in systematic reviews.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
70MSC NURSING
Tubaishat, A., Aljezawi, M. and Al Qadire, M., 2013. Nurses' attitudes and perceived barriers
to pressure ulcer prevention in Jordan. Journal of wound care, 22(9), pp.490-497.
VanGilder, C., MacFarlane, G.D. and Meyer, S., 2008. Results of nine international pressure
ulcer prevalence surveys: 1989 to 2005. Ostomy Wound Management, 54(2), p.40.
Zakrasek, E.C., Creasey, G. and Crew, J.D., 2015. Pressure ulcers in people with spinal cord
injury in developing nations. Spinal Cord, 53(1), p.7.
Tubaishat, A., Aljezawi, M. and Al Qadire, M., 2013. Nurses' attitudes and perceived barriers
to pressure ulcer prevention in Jordan. Journal of wound care, 22(9), pp.490-497.
VanGilder, C., MacFarlane, G.D. and Meyer, S., 2008. Results of nine international pressure
ulcer prevalence surveys: 1989 to 2005. Ostomy Wound Management, 54(2), p.40.
Zakrasek, E.C., Creasey, G. and Crew, J.D., 2015. Pressure ulcers in people with spinal cord
injury in developing nations. Spinal Cord, 53(1), p.7.
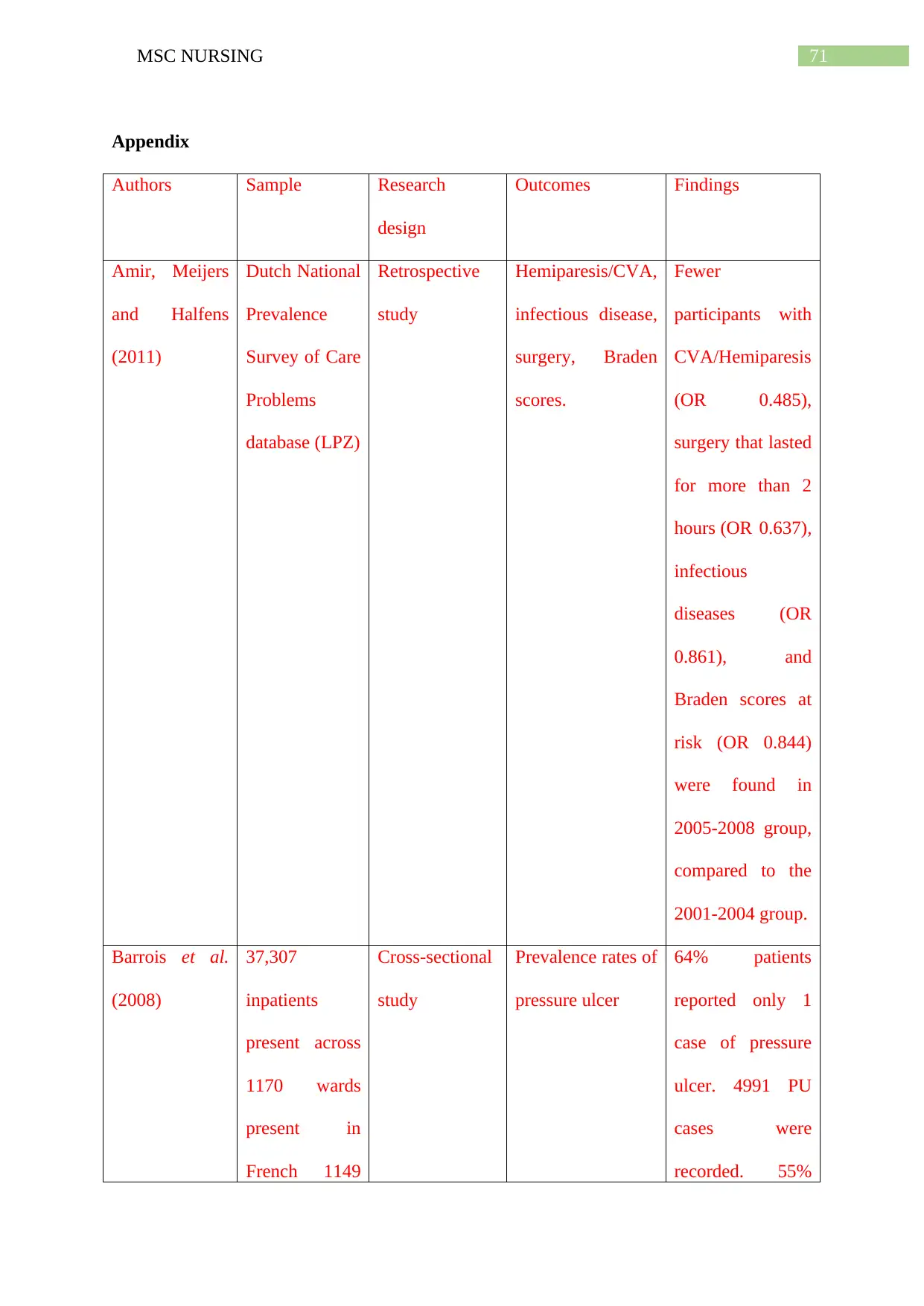
71MSC NURSING
Appendix
Authors Sample Research
design
Outcomes Findings
Amir, Meijers
and Halfens
(2011)
Dutch National
Prevalence
Survey of Care
Problems
database (LPZ)
Retrospective
study
Hemiparesis/CVA,
infectious disease,
surgery, Braden
scores.
Fewer
participants with
CVA/Hemiparesis
(OR 0.485),
surgery that lasted
for more than 2
hours (OR 0.637),
infectious
diseases (OR
0.861), and
Braden scores at
risk (OR 0.844)
were found in
2005-2008 group,
compared to the
2001-2004 group.
Barrois et al.
(2008)
37,307
inpatients
present across
1170 wards
present in
French 1149
Cross-sectional
study
Prevalence rates of
pressure ulcer
64% patients
reported only 1
case of pressure
ulcer. 4991 PU
cases were
recorded. 55%
Appendix
Authors Sample Research
design
Outcomes Findings
Amir, Meijers
and Halfens
(2011)
Dutch National
Prevalence
Survey of Care
Problems
database (LPZ)
Retrospective
study
Hemiparesis/CVA,
infectious disease,
surgery, Braden
scores.
Fewer
participants with
CVA/Hemiparesis
(OR 0.485),
surgery that lasted
for more than 2
hours (OR 0.637),
infectious
diseases (OR
0.861), and
Braden scores at
risk (OR 0.844)
were found in
2005-2008 group,
compared to the
2001-2004 group.
Barrois et al.
(2008)
37,307
inpatients
present across
1170 wards
present in
French 1149
Cross-sectional
study
Prevalence rates of
pressure ulcer
64% patients
reported only 1
case of pressure
ulcer. 4991 PU
cases were
recorded. 55%
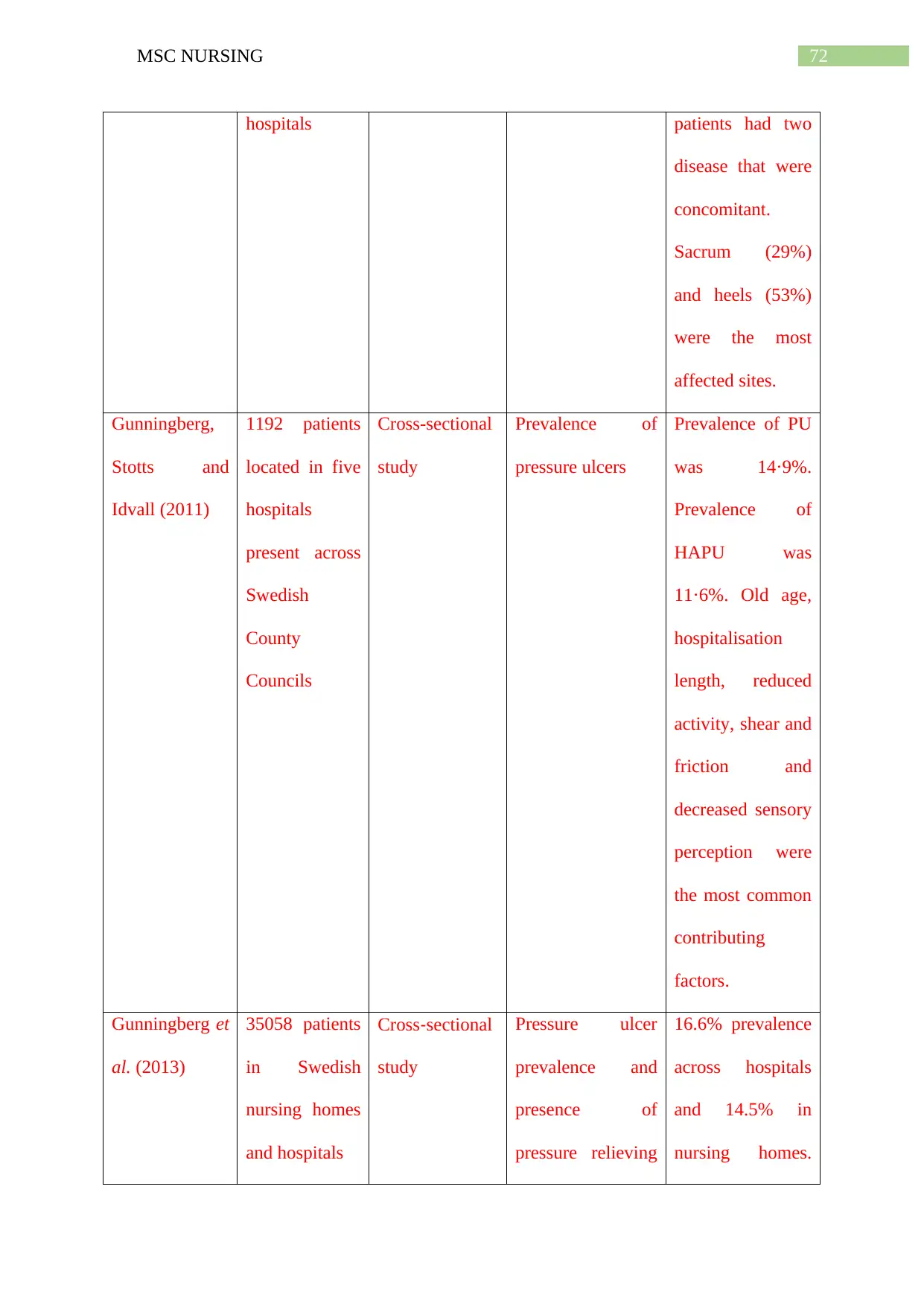
72MSC NURSING
hospitals patients had two
disease that were
concomitant.
Sacrum (29%)
and heels (53%)
were the most
affected sites.
Gunningberg,
Stotts and
Idvall (2011)
1192 patients
located in five
hospitals
present across
Swedish
County
Councils
Cross-sectional
study
Prevalence of
pressure ulcers
Prevalence of PU
was 14·9%.
Prevalence of
HAPU was
11·6%. Old age,
hospitalisation
length, reduced
activity, shear and
friction and
decreased sensory
perception were
the most common
contributing
factors.
Gunningberg et
al. (2013)
35058 patients
in Swedish
nursing homes
and hospitals
Cross‐sectional
study
Pressure ulcer
prevalence and
presence of
pressure relieving
16.6% prevalence
across hospitals
and 14.5% in
nursing homes.
hospitals patients had two
disease that were
concomitant.
Sacrum (29%)
and heels (53%)
were the most
affected sites.
Gunningberg,
Stotts and
Idvall (2011)
1192 patients
located in five
hospitals
present across
Swedish
County
Councils
Cross-sectional
study
Prevalence of
pressure ulcers
Prevalence of PU
was 14·9%.
Prevalence of
HAPU was
11·6%. Old age,
hospitalisation
length, reduced
activity, shear and
friction and
decreased sensory
perception were
the most common
contributing
factors.
Gunningberg et
al. (2013)
35058 patients
in Swedish
nursing homes
and hospitals
Cross‐sectional
study
Pressure ulcer
prevalence and
presence of
pressure relieving
16.6% prevalence
across hospitals
and 14.5% in
nursing homes.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
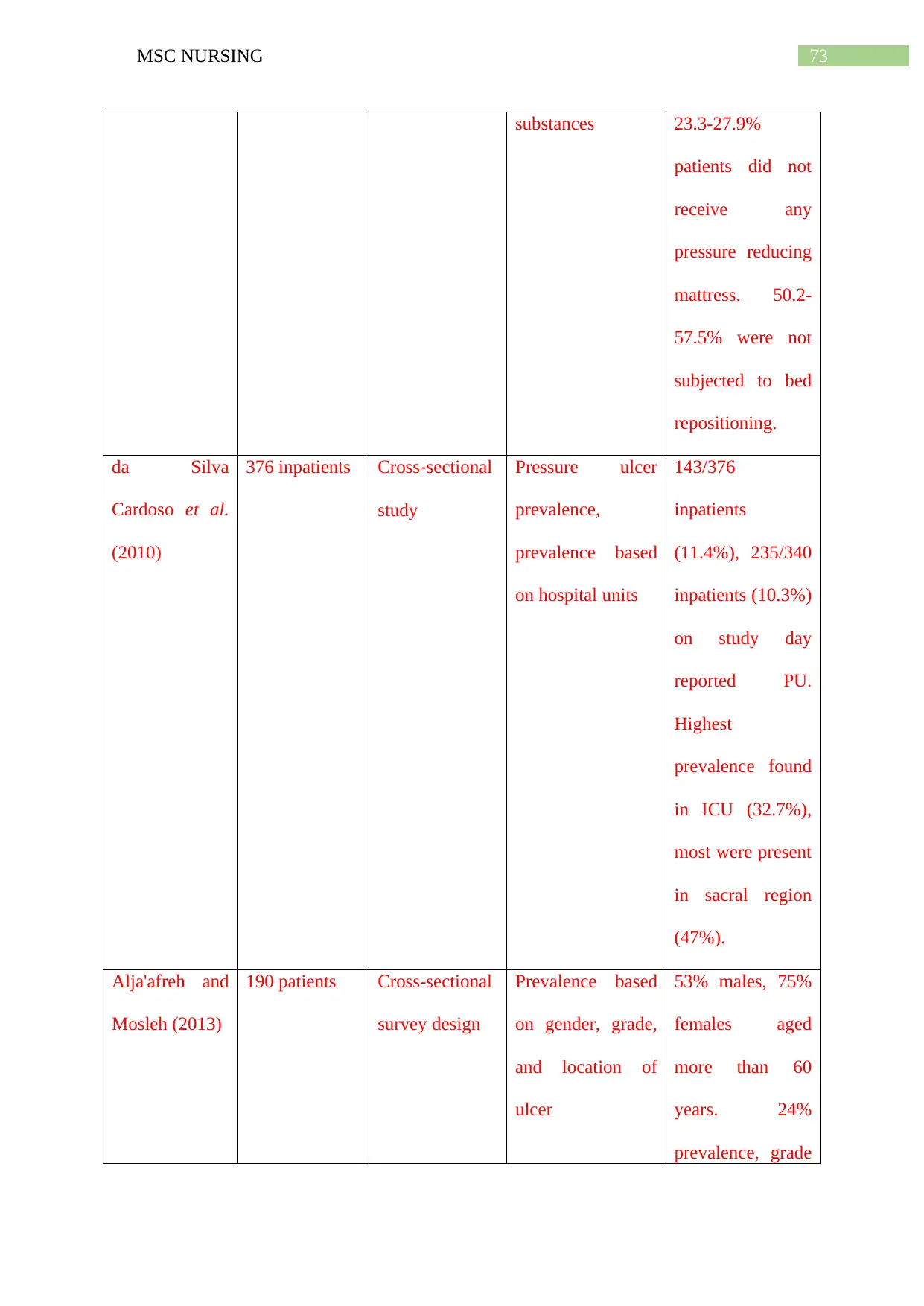
73MSC NURSING
substances 23.3-27.9%
patients did not
receive any
pressure reducing
mattress. 50.2-
57.5% were not
subjected to bed
repositioning.
da Silva
Cardoso et al.
(2010)
376 inpatients Cross‐sectional
study
Pressure ulcer
prevalence,
prevalence based
on hospital units
143/376
inpatients
(11.4%), 235/340
inpatients (10.3%)
on study day
reported PU.
Highest
prevalence found
in ICU (32.7%),
most were present
in sacral region
(47%).
Alja'afreh and
Mosleh (2013)
190 patients Cross-sectional
survey design
Prevalence based
on gender, grade,
and location of
ulcer
53% males, 75%
females aged
more than 60
years. 24%
prevalence, grade
substances 23.3-27.9%
patients did not
receive any
pressure reducing
mattress. 50.2-
57.5% were not
subjected to bed
repositioning.
da Silva
Cardoso et al.
(2010)
376 inpatients Cross‐sectional
study
Pressure ulcer
prevalence,
prevalence based
on hospital units
143/376
inpatients
(11.4%), 235/340
inpatients (10.3%)
on study day
reported PU.
Highest
prevalence found
in ICU (32.7%),
most were present
in sacral region
(47%).
Alja'afreh and
Mosleh (2013)
190 patients Cross-sectional
survey design
Prevalence based
on gender, grade,
and location of
ulcer
53% males, 75%
females aged
more than 60
years. 24%
prevalence, grade
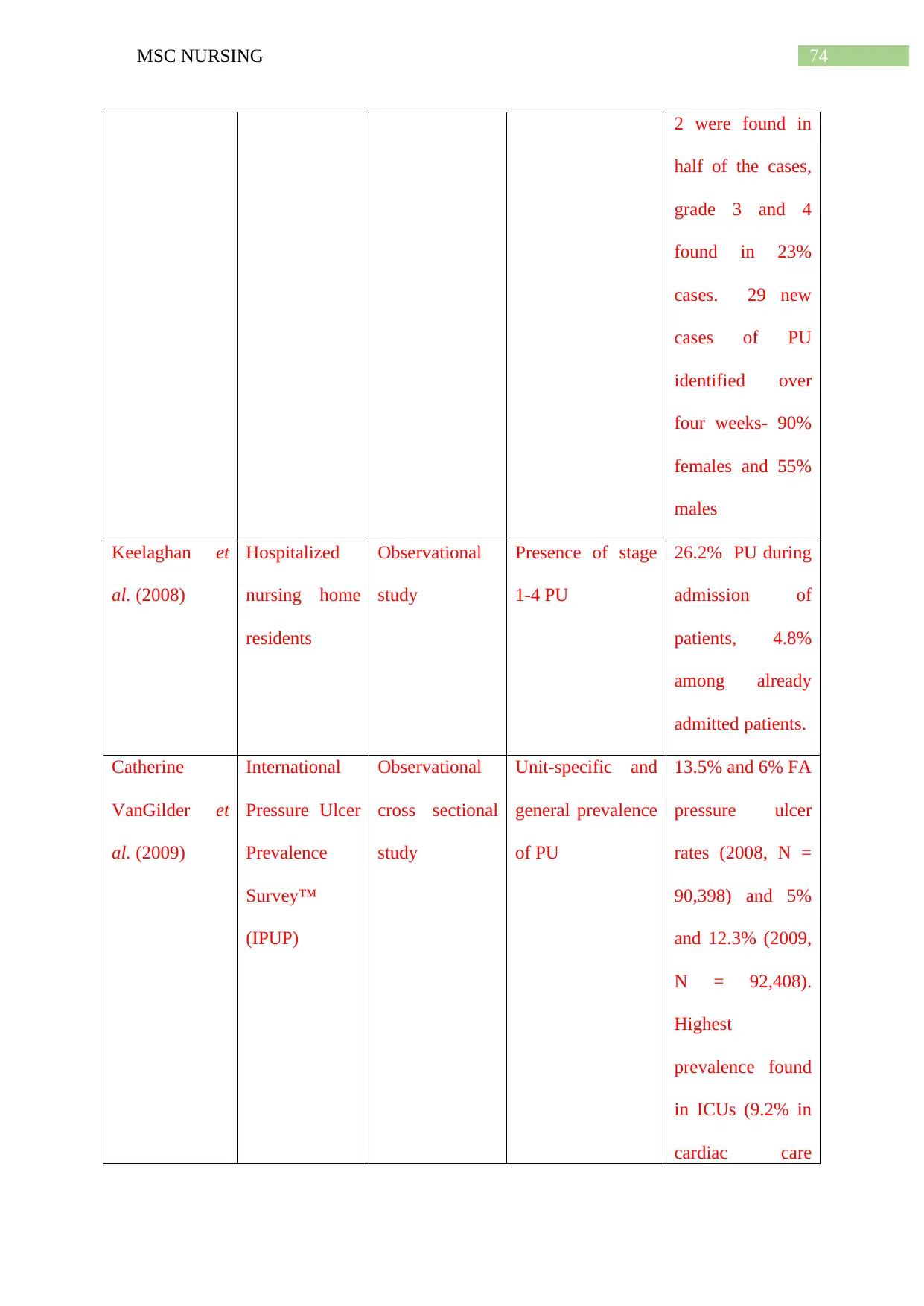
74MSC NURSING
2 were found in
half of the cases,
grade 3 and 4
found in 23%
cases. 29 new
cases of PU
identified over
four weeks- 90%
females and 55%
males
Keelaghan et
al. (2008)
Hospitalized
nursing home
residents
Observational
study
Presence of stage
1-4 PU
26.2% PU during
admission of
patients, 4.8%
among already
admitted patients.
Catherine
VanGilder et
al. (2009)
International
Pressure Ulcer
Prevalence
Survey™
(IPUP)
Observational
cross sectional
study
Unit-specific and
general prevalence
of PU
13.5% and 6% FA
pressure ulcer
rates (2008, N =
90,398) and 5%
and 12.3% (2009,
N = 92,408).
Highest
prevalence found
in ICUs (9.2% in
cardiac care
2 were found in
half of the cases,
grade 3 and 4
found in 23%
cases. 29 new
cases of PU
identified over
four weeks- 90%
females and 55%
males
Keelaghan et
al. (2008)
Hospitalized
nursing home
residents
Observational
study
Presence of stage
1-4 PU
26.2% PU during
admission of
patients, 4.8%
among already
admitted patients.
Catherine
VanGilder et
al. (2009)
International
Pressure Ulcer
Prevalence
Survey™
(IPUP)
Observational
cross sectional
study
Unit-specific and
general prevalence
of PU
13.5% and 6% FA
pressure ulcer
rates (2008, N =
90,398) and 5%
and 12.3% (2009,
N = 92,408).
Highest
prevalence found
in ICUs (9.2% in
cardiac care
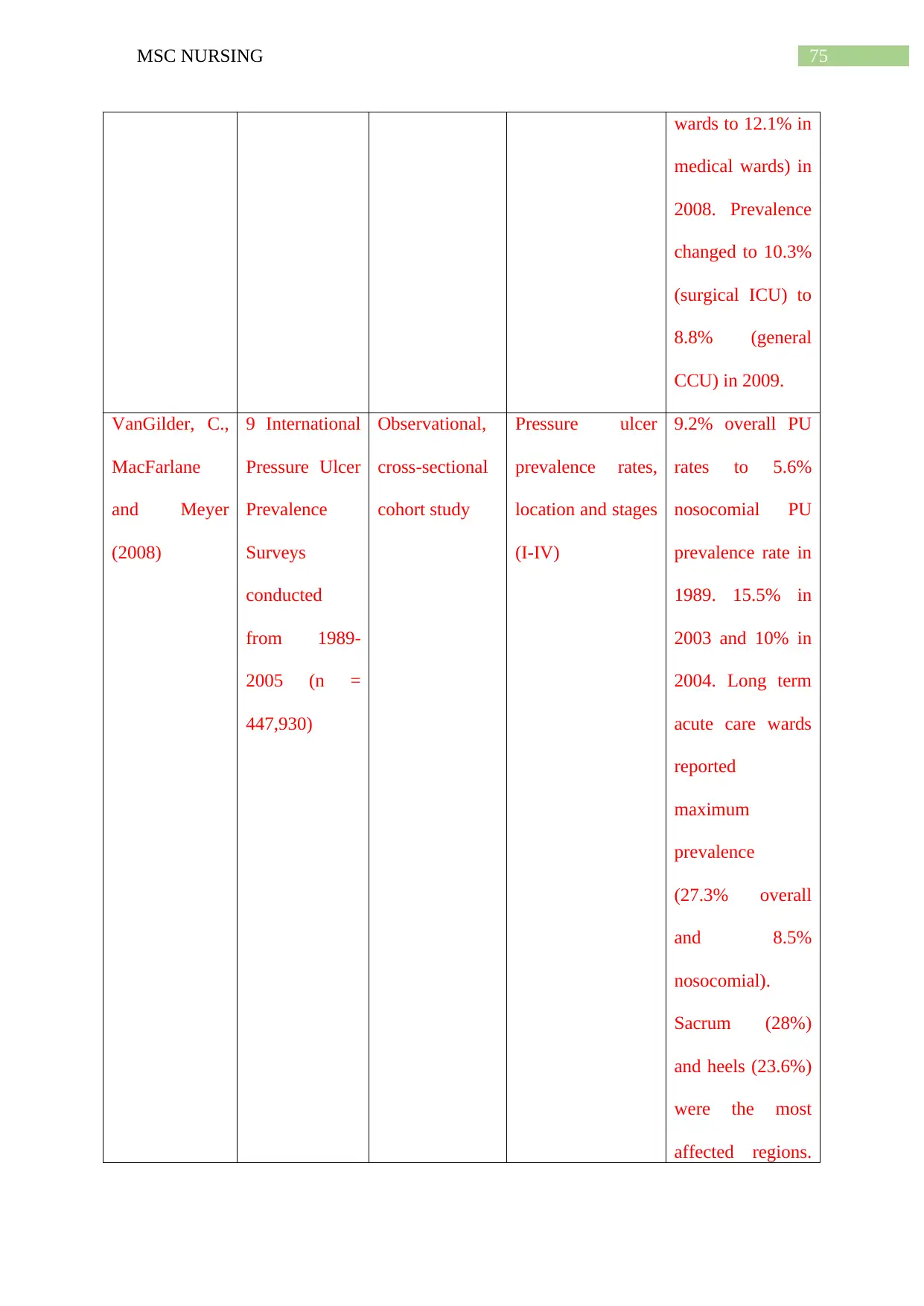
75MSC NURSING
wards to 12.1% in
medical wards) in
2008. Prevalence
changed to 10.3%
(surgical ICU) to
8.8% (general
CCU) in 2009.
VanGilder, C.,
MacFarlane
and Meyer
(2008)
9 International
Pressure Ulcer
Prevalence
Surveys
conducted
from 1989-
2005 (n =
447,930)
Observational,
cross-sectional
cohort study
Pressure ulcer
prevalence rates,
location and stages
(I-IV)
9.2% overall PU
rates to 5.6%
nosocomial PU
prevalence rate in
1989. 15.5% in
2003 and 10% in
2004. Long term
acute care wards
reported
maximum
prevalence
(27.3% overall
and 8.5%
nosocomial).
Sacrum (28%)
and heels (23.6%)
were the most
affected regions.
wards to 12.1% in
medical wards) in
2008. Prevalence
changed to 10.3%
(surgical ICU) to
8.8% (general
CCU) in 2009.
VanGilder, C.,
MacFarlane
and Meyer
(2008)
9 International
Pressure Ulcer
Prevalence
Surveys
conducted
from 1989-
2005 (n =
447,930)
Observational,
cross-sectional
cohort study
Pressure ulcer
prevalence rates,
location and stages
(I-IV)
9.2% overall PU
rates to 5.6%
nosocomial PU
prevalence rate in
1989. 15.5% in
2003 and 10% in
2004. Long term
acute care wards
reported
maximum
prevalence
(27.3% overall
and 8.5%
nosocomial).
Sacrum (28%)
and heels (23.6%)
were the most
affected regions.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
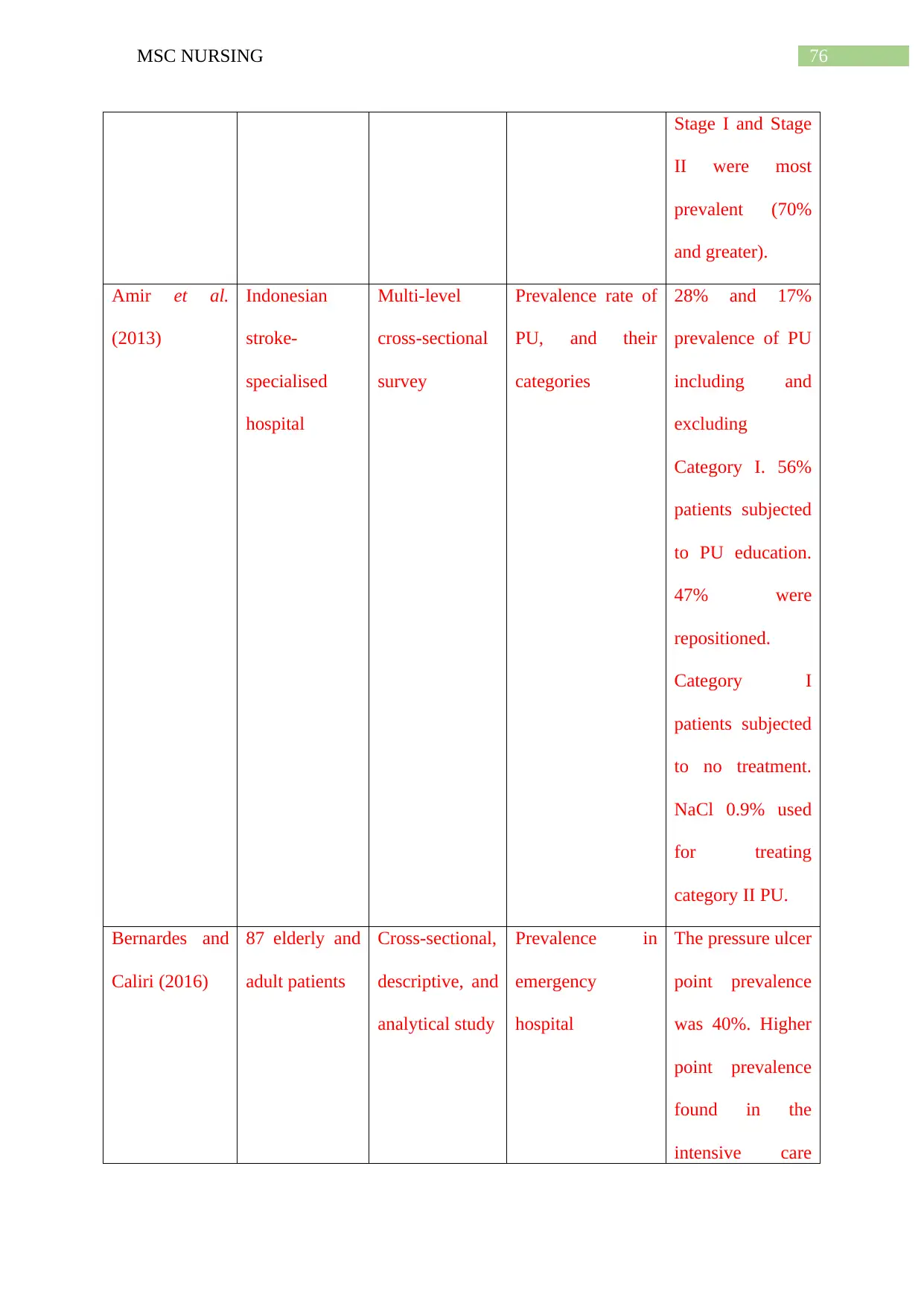
76MSC NURSING
Stage I and Stage
II were most
prevalent (70%
and greater).
Amir et al.
(2013)
Indonesian
stroke-
specialised
hospital
Multi-level
cross-sectional
survey
Prevalence rate of
PU, and their
categories
28% and 17%
prevalence of PU
including and
excluding
Category I. 56%
patients subjected
to PU education.
47% were
repositioned.
Category I
patients subjected
to no treatment.
NaCl 0.9% used
for treating
category II PU.
Bernardes and
Caliri (2016)
87 elderly and
adult patients
Cross-sectional,
descriptive, and
analytical study
Prevalence in
emergency
hospital
The pressure ulcer
point prevalence
was 40%. Higher
point prevalence
found in the
intensive care
Stage I and Stage
II were most
prevalent (70%
and greater).
Amir et al.
(2013)
Indonesian
stroke-
specialised
hospital
Multi-level
cross-sectional
survey
Prevalence rate of
PU, and their
categories
28% and 17%
prevalence of PU
including and
excluding
Category I. 56%
patients subjected
to PU education.
47% were
repositioned.
Category I
patients subjected
to no treatment.
NaCl 0.9% used
for treating
category II PU.
Bernardes and
Caliri (2016)
87 elderly and
adult patients
Cross-sectional,
descriptive, and
analytical study
Prevalence in
emergency
hospital
The pressure ulcer
point prevalence
was 40%. Higher
point prevalence
found in the
intensive care
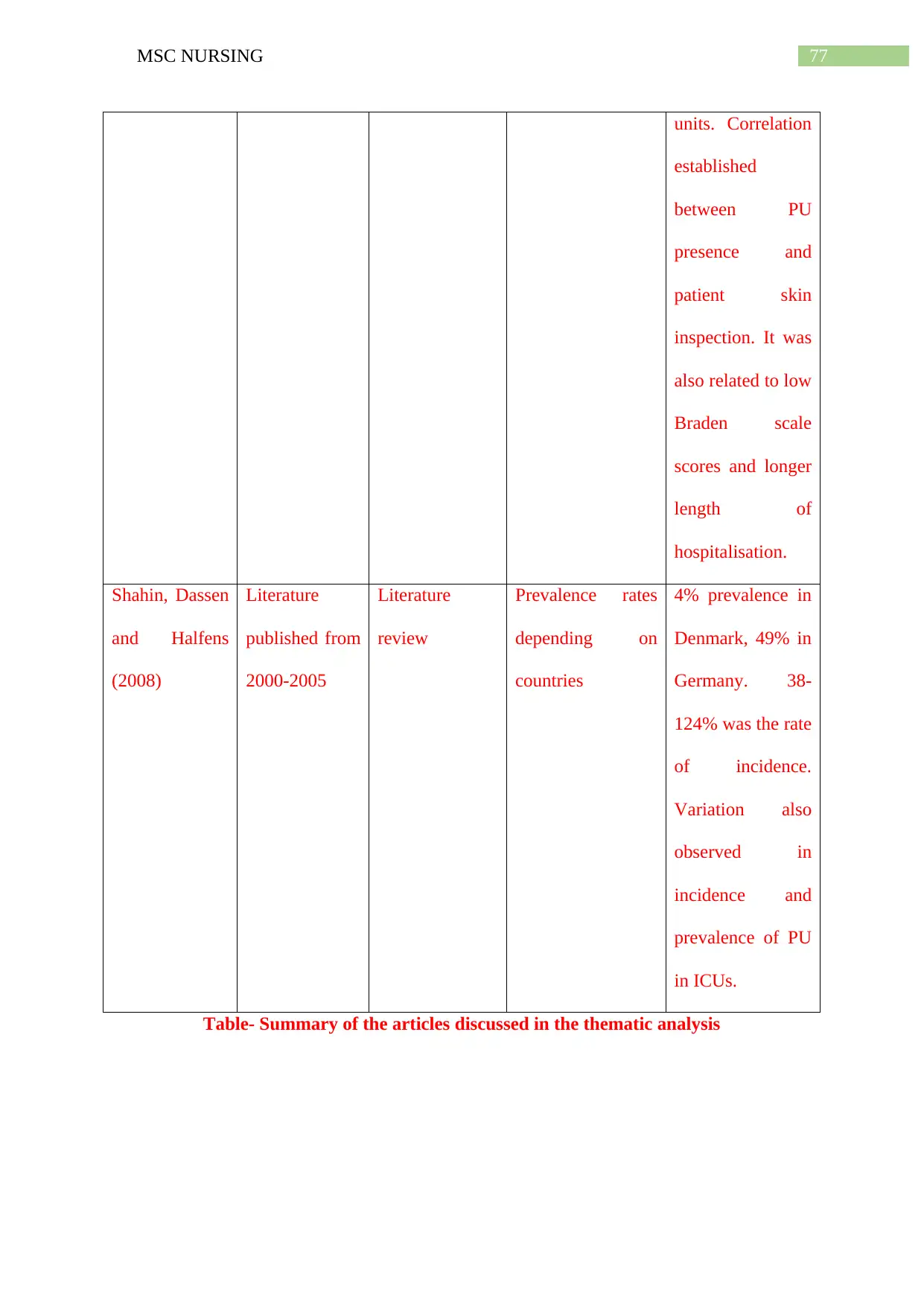
77MSC NURSING
units. Correlation
established
between PU
presence and
patient skin
inspection. It was
also related to low
Braden scale
scores and longer
length of
hospitalisation.
Shahin, Dassen
and Halfens
(2008)
Literature
published from
2000-2005
Literature
review
Prevalence rates
depending on
countries
4% prevalence in
Denmark, 49% in
Germany. 38-
124% was the rate
of incidence.
Variation also
observed in
incidence and
prevalence of PU
in ICUs.
Table- Summary of the articles discussed in the thematic analysis
units. Correlation
established
between PU
presence and
patient skin
inspection. It was
also related to low
Braden scale
scores and longer
length of
hospitalisation.
Shahin, Dassen
and Halfens
(2008)
Literature
published from
2000-2005
Literature
review
Prevalence rates
depending on
countries
4% prevalence in
Denmark, 49% in
Germany. 38-
124% was the rate
of incidence.
Variation also
observed in
incidence and
prevalence of PU
in ICUs.
Table- Summary of the articles discussed in the thematic analysis
1 out of 78
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





