(PDF) Primary Health Care: An Overview
VerifiedAdded on 2021/09/10
|14
|3111
|100
AI Summary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
Primary Health Care in Action notes
Module 1: Intro into primary health care
Health: WHO (1986) defines it as a state of complete physical, mental, and social wellbeing and not
merely the absence of disease or infirmity.
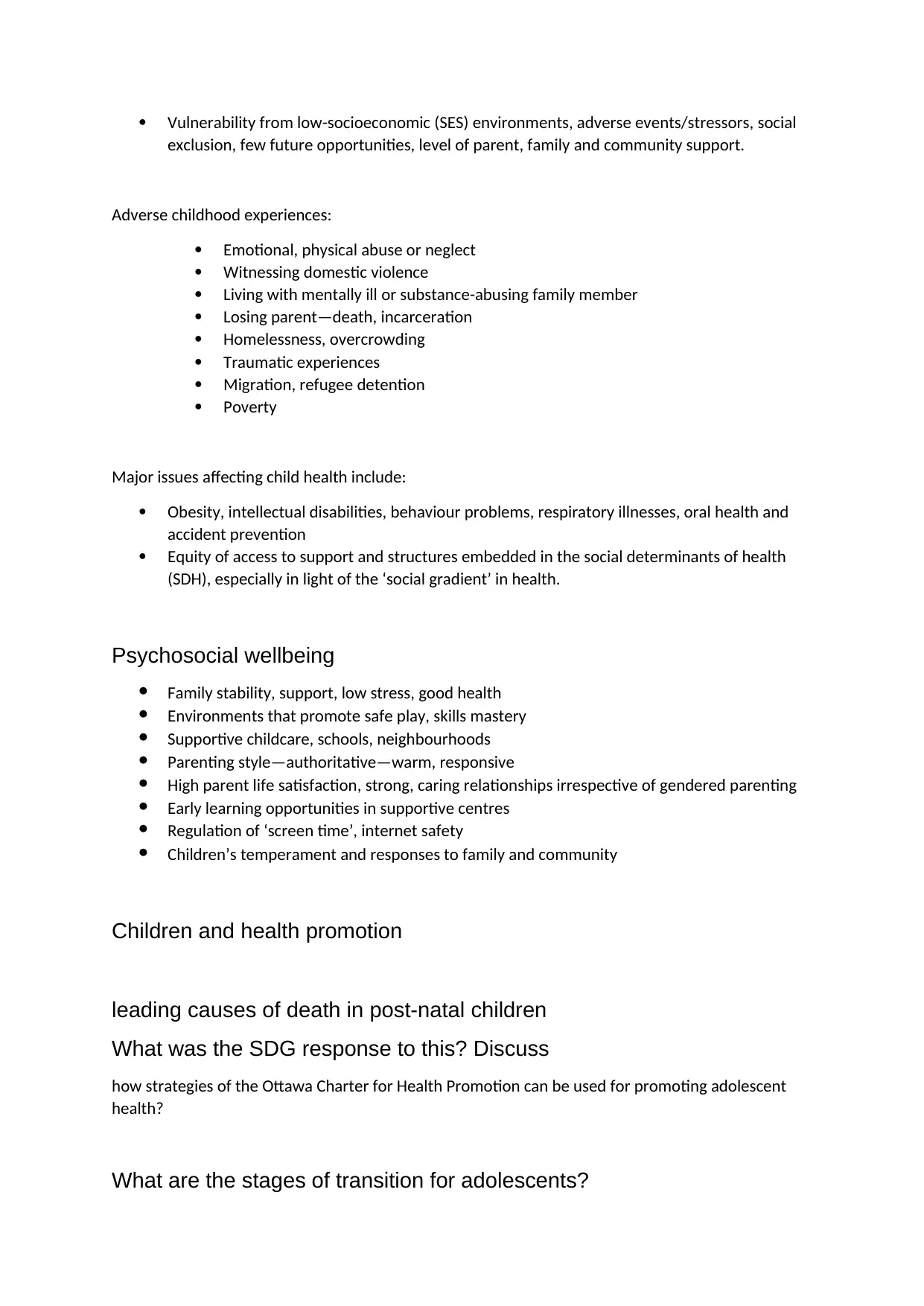
Social determinants of Health: Factors that determine health and wellbeing. → Social wellbeing,
economic wellbeing, environmental wellbeing, life satisfaction, spiritual wellbeing.
Social determinants of health
- Employment and working conditions.
- Gender, culture
- Health services, resources
- Health practices, coping skills.
- Social environments
- Physical environments
- Education, literacy
- Social support networks
- Healthy child development
- Biology, genetic characteristics
6 dimensions of health
- Physical
- Social
- Intellectual
- Environmental
- Spiritual
- Emotional
Origin of PHC
1978, The World Health Organisation (WHO), began the concept of “Health for ALL”, by the
year 2000, and Declaration of Alma Ata.
Aim: Create social justice about how countries distribute their resources of Health.
(1978) Declaration of Alma Ata: states that health is a “fundamental human right” and is a
“world-wide social goal.”
Module 1: Intro into primary health care
Health: WHO (1986) defines it as a state of complete physical, mental, and social wellbeing and not
merely the absence of disease or infirmity.
Social determinants of Health: Factors that determine health and wellbeing. → Social wellbeing,
economic wellbeing, environmental wellbeing, life satisfaction, spiritual wellbeing.
Social determinants of health
- Employment and working conditions.
- Gender, culture
- Health services, resources
- Health practices, coping skills.
- Social environments
- Physical environments
- Education, literacy
- Social support networks
- Healthy child development
- Biology, genetic characteristics
6 dimensions of health
- Physical
- Social
- Intellectual
- Environmental
- Spiritual
- Emotional
Origin of PHC
1978, The World Health Organisation (WHO), began the concept of “Health for ALL”, by the
year 2000, and Declaration of Alma Ata.
Aim: Create social justice about how countries distribute their resources of Health.
(1978) Declaration of Alma Ata: states that health is a “fundamental human right” and is a
“world-wide social goal.”
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Principles of PHC
Access equity, empowerment health literacy, community participation, cultural sensitivity,
cultural safety, intersectoral collaboration, health promotion, appropriate technology →
adaptable to local needs, acceptable to those using, maintained by people themselves, using
affordable resources.
Intersectoral collaboration: Joint action taken by health and other government sectors as well as
representatives from private, voluntary, and non-profit groups to improve health of populations
performing different roles for same purpose.
Primary Health Care: Essential care made universally acceptable to families and individuals in the
community by means acceptable to them through their full participation and at a cost the
community can afford.
Primary Health Care Primary Care
- Incorporates 6 PHC principles
- Holistic (various) focus on health
promotion and disease prevention:
treatment, cure, rehab
- It is a SOCIAL MODEL OF HEALTH
- Intersectoral collaboration between all
sections
- It is a comprehensive global health care
(McMurray & Clendon, 2015)
- A component of PHC
- 1st point of contact a person has with
the health system.
- Essentially about care for sick or injured
individuals based in the community.
- Allied health, nursing care, therapist
(e.g., medical care)
- Selective health care (McMurray &
Clendon 2015)
Module 2: Social Determinants of Health
Education
Provides individuals with the knowledge and skills to solve problems and take control of their life
circumstances + job opportunity, income security, job satisfaction.
Employment/working conditions.
Shapes social position provides sense of purpose, identity, social contacts, personal growth.
Early/Healthy child development (ECD)
ECD involves physical, social, emotional, and language/cognitive → influences wellbeing, obesity,
mental health, heart disease, competence in literacy and numeracy, criminality, economic
participation.
Socioeconomic position
- People from poorer social/economic circumstances are at great risk of poor health, higher
rates of illness, disability and death and lives shorter lives.
- Indicators such as education, occupation and income define socioeconomic position
(Galobardes et al. 2006, AIIHW, 2016)
Access equity, empowerment health literacy, community participation, cultural sensitivity,
cultural safety, intersectoral collaboration, health promotion, appropriate technology →
adaptable to local needs, acceptable to those using, maintained by people themselves, using
affordable resources.
Intersectoral collaboration: Joint action taken by health and other government sectors as well as
representatives from private, voluntary, and non-profit groups to improve health of populations
performing different roles for same purpose.
Primary Health Care: Essential care made universally acceptable to families and individuals in the
community by means acceptable to them through their full participation and at a cost the
community can afford.
Primary Health Care Primary Care
- Incorporates 6 PHC principles
- Holistic (various) focus on health
promotion and disease prevention:
treatment, cure, rehab
- It is a SOCIAL MODEL OF HEALTH
- Intersectoral collaboration between all
sections
- It is a comprehensive global health care
(McMurray & Clendon, 2015)
- A component of PHC
- 1st point of contact a person has with
the health system.
- Essentially about care for sick or injured
individuals based in the community.
- Allied health, nursing care, therapist
(e.g., medical care)
- Selective health care (McMurray &
Clendon 2015)
Module 2: Social Determinants of Health
Education
Provides individuals with the knowledge and skills to solve problems and take control of their life
circumstances + job opportunity, income security, job satisfaction.
Employment/working conditions.
Shapes social position provides sense of purpose, identity, social contacts, personal growth.
Early/Healthy child development (ECD)
ECD involves physical, social, emotional, and language/cognitive → influences wellbeing, obesity,
mental health, heart disease, competence in literacy and numeracy, criminality, economic
participation.
Socioeconomic position
- People from poorer social/economic circumstances are at great risk of poor health, higher
rates of illness, disability and death and lives shorter lives.
- Indicators such as education, occupation and income define socioeconomic position
(Galobardes et al. 2006, AIIHW, 2016)
Occupation
Higher education and income levels → increased likelihood of higher status occupation → high
income.
Income
Greater access for goods and services that provide health benefits such as housing, food, additional
health care options, healthy pursuits.
Gender
Implementing human rights.
Culture
A person’s upbringing, background, traditions, customs, and the beliefs of their family or community
→ influence how they may think, feel, act and value.
Social support networks
Provide sources to cope, find work.
Physical environment
Contaminants in water, air, food, soil
Biology/genetics
Age, sex, inherited conditions
Health services
Barriers include→ cost, availability, insurance, language.
Social environments
Share resources together, bond, values, norms, social stability, diversity, cohesiveness can help risk
to health.
Behavioural risk
Tobacco, alcohol, illicit drugs, less exercise
Social gradient: Research studies have shown that there is a ‘social gradient’ in health, whereby
those employed at successively higher levels have better health than those on lower levels.
Higher education and income levels → increased likelihood of higher status occupation → high
income.
Income
Greater access for goods and services that provide health benefits such as housing, food, additional
health care options, healthy pursuits.
Gender
Implementing human rights.
Culture
A person’s upbringing, background, traditions, customs, and the beliefs of their family or community
→ influence how they may think, feel, act and value.
Social support networks
Provide sources to cope, find work.
Physical environment
Contaminants in water, air, food, soil
Biology/genetics
Age, sex, inherited conditions
Health services
Barriers include→ cost, availability, insurance, language.
Social environments
Share resources together, bond, values, norms, social stability, diversity, cohesiveness can help risk
to health.
Behavioural risk
Tobacco, alcohol, illicit drugs, less exercise
Social gradient: Research studies have shown that there is a ‘social gradient’ in health, whereby
those employed at successively higher levels have better health than those on lower levels.
Module 3: Health Promotion
Ottawa Charter (1986)
The process of enabling people to increase control over and improve their health (WHO, 1998).
- Introduced at the first international conference on Health promotion in 1986 in Ottawa, Canada.
Aim: Emphasise importance of promoting health at a global level, for Health for ALL (HFA). SOCIAL
JUSTICE.
Fundamental prerequisites:
1. Peace
2. Shelter
3. Education
4. Food
5. Income
6. A stable ecosystem
7. Sustainable resources
8. Social justice and equity
→ Advocate, enabling (reduce difference in health status), mediate.
Strategies of the Ottawa Charter
- Strengthen community action.
- Develop personal skills.
- Build healthy public policy.
- Create supportive environments.
- Reorient health services.
- Enable, mediate, advocate.
Multi-level Health promotion
1. Upstream: Promoting, maintaining Health e.g., Vaccination, education
2. Midstream: Appropriate treatment, protection from harm or disability after illness, injury,
screening.
3. Downstream: Rehabilitation, coping (managing health/illness)
Strategies for Global Health (Labonte, 2008)
Access to resources → fundamental human right
Human security instead of national security
Reframe globalisation.
Regulate global market forces so its people centred.
Develop public policy based on a vision of the world where people matter→ social justice.
Develop a global contact.
Ottawa Charter (1986)
The process of enabling people to increase control over and improve their health (WHO, 1998).
- Introduced at the first international conference on Health promotion in 1986 in Ottawa, Canada.
Aim: Emphasise importance of promoting health at a global level, for Health for ALL (HFA). SOCIAL
JUSTICE.
Fundamental prerequisites:
1. Peace
2. Shelter
3. Education
4. Food
5. Income
6. A stable ecosystem
7. Sustainable resources
8. Social justice and equity
→ Advocate, enabling (reduce difference in health status), mediate.
Strategies of the Ottawa Charter
- Strengthen community action.
- Develop personal skills.
- Build healthy public policy.
- Create supportive environments.
- Reorient health services.
- Enable, mediate, advocate.
Multi-level Health promotion
1. Upstream: Promoting, maintaining Health e.g., Vaccination, education
2. Midstream: Appropriate treatment, protection from harm or disability after illness, injury,
screening.
3. Downstream: Rehabilitation, coping (managing health/illness)
Strategies for Global Health (Labonte, 2008)
Access to resources → fundamental human right
Human security instead of national security
Reframe globalisation.
Regulate global market forces so its people centred.
Develop public policy based on a vision of the world where people matter→ social justice.
Develop a global contact.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Module 4: SDGs and NHPAs
Social justice: the rights of all people in our community are considered in a fair and equitable
manner. E.g.:
• Information designed to educate the public about healthy lifestyles should be provided in
languages that the community can understand.
• Health policies should ensure that all people have equal access to health care services.
• People living in isolated communities should have the same access to clean water and sanitation as
a person living in an urban area.
• People of low socioeconomic backgrounds should receive the same quality of health care as a
person of higher socioeconomic background’.
Equity vs Equality
Equity: recognises that each person has different circumstances & allocates the exact resources &
opportunities needed to reach an equal outcome.
Equality: Each individual or group of people is given the same resources or opportunities.
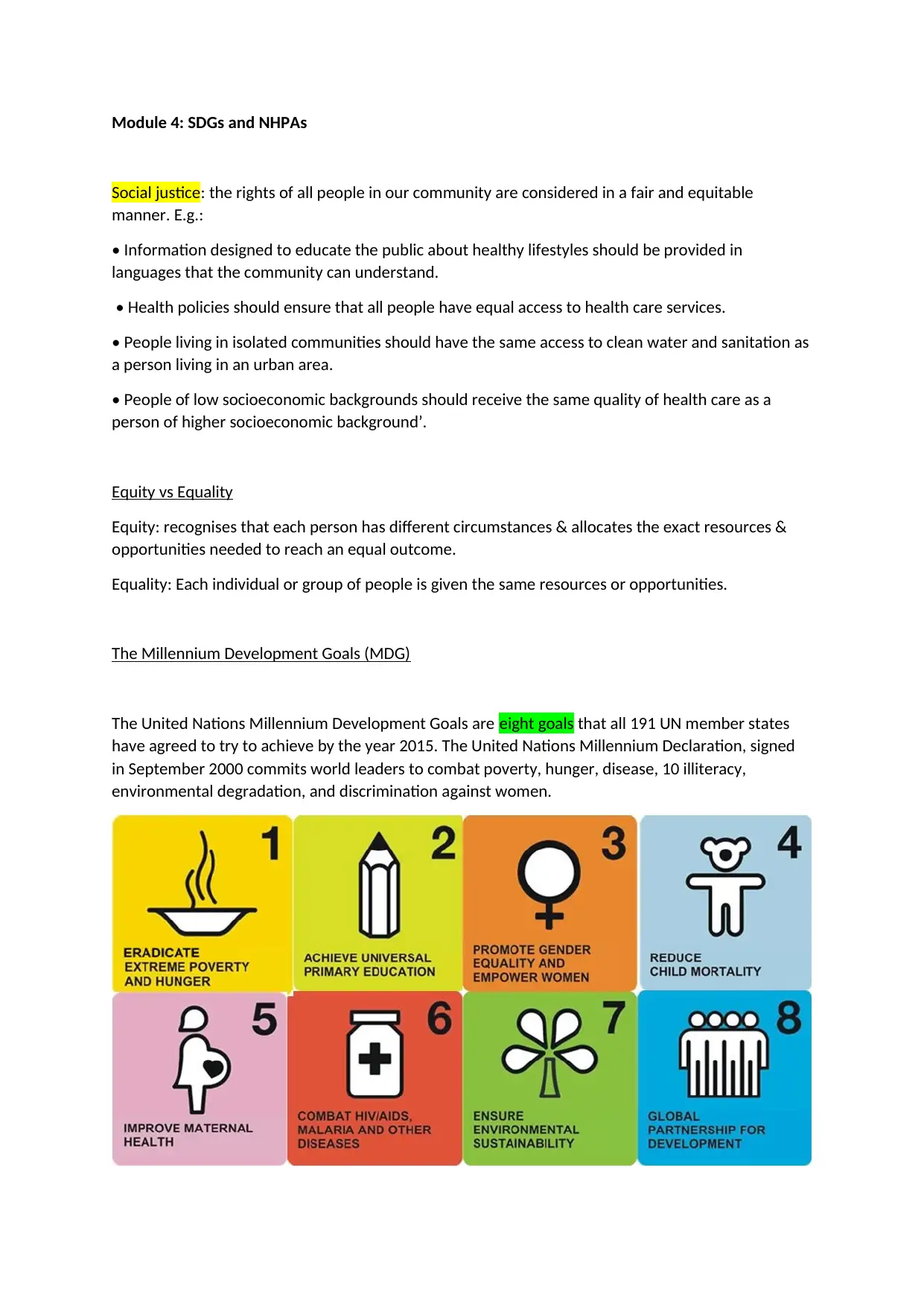
The Millennium Development Goals (MDG)
The United Nations Millennium Development Goals are eight goals that all 191 UN member states
have agreed to try to achieve by the year 2015. The United Nations Millennium Declaration, signed
in September 2000 commits world leaders to combat poverty, hunger, disease, 10 illiteracy,
environmental degradation, and discrimination against women.
Social justice: the rights of all people in our community are considered in a fair and equitable
manner. E.g.:
• Information designed to educate the public about healthy lifestyles should be provided in
languages that the community can understand.
• Health policies should ensure that all people have equal access to health care services.
• People living in isolated communities should have the same access to clean water and sanitation as
a person living in an urban area.
• People of low socioeconomic backgrounds should receive the same quality of health care as a
person of higher socioeconomic background’.
Equity vs Equality
Equity: recognises that each person has different circumstances & allocates the exact resources &
opportunities needed to reach an equal outcome.
Equality: Each individual or group of people is given the same resources or opportunities.
The Millennium Development Goals (MDG)
The United Nations Millennium Development Goals are eight goals that all 191 UN member states
have agreed to try to achieve by the year 2015. The United Nations Millennium Declaration, signed
in September 2000 commits world leaders to combat poverty, hunger, disease, 10 illiteracy,
environmental degradation, and discrimination against women.
Injury Prevention & control
- Regulated by NSW Work Health and Safety 2011.
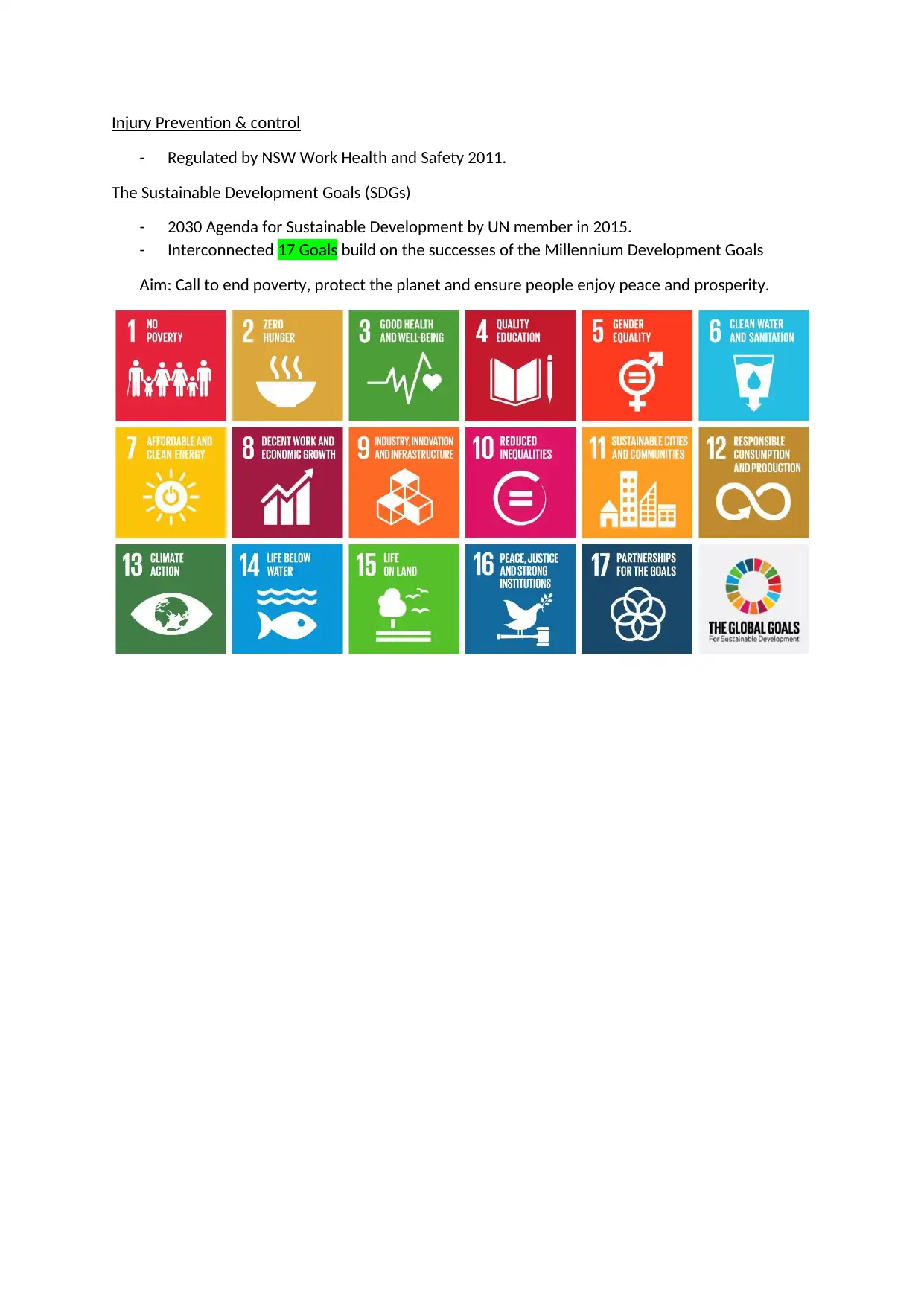
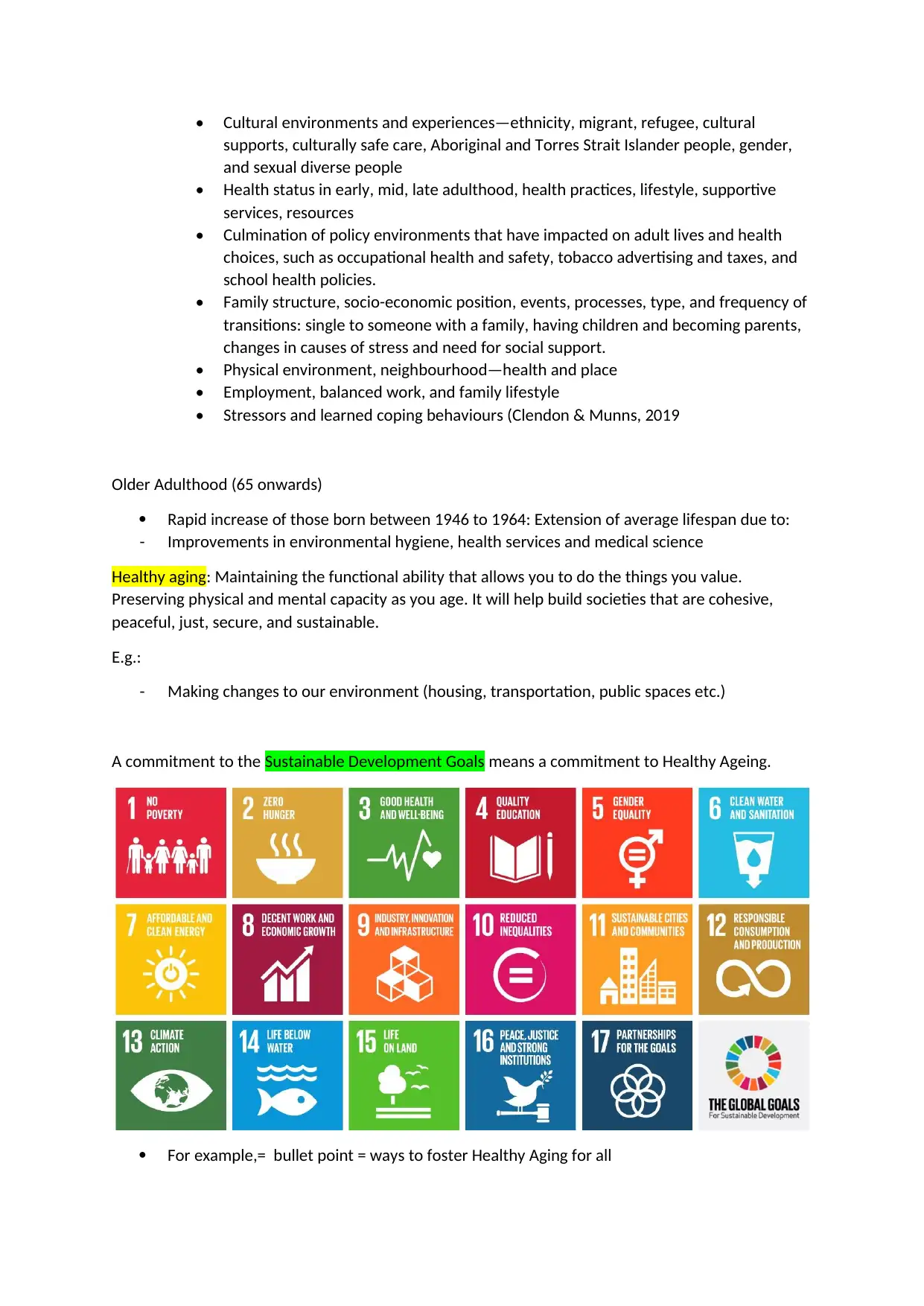
The Sustainable Development Goals (SDGs)
- 2030 Agenda for Sustainable Development by UN member in 2015.
- Interconnected 17 Goals build on the successes of the Millennium Development Goals
Aim: Call to end poverty, protect the planet and ensure people enjoy peace and prosperity.
- Regulated by NSW Work Health and Safety 2011.
The Sustainable Development Goals (SDGs)
- 2030 Agenda for Sustainable Development by UN member in 2015.
- Interconnected 17 Goals build on the successes of the Millennium Development Goals
Aim: Call to end poverty, protect the planet and ensure people enjoy peace and prosperity.
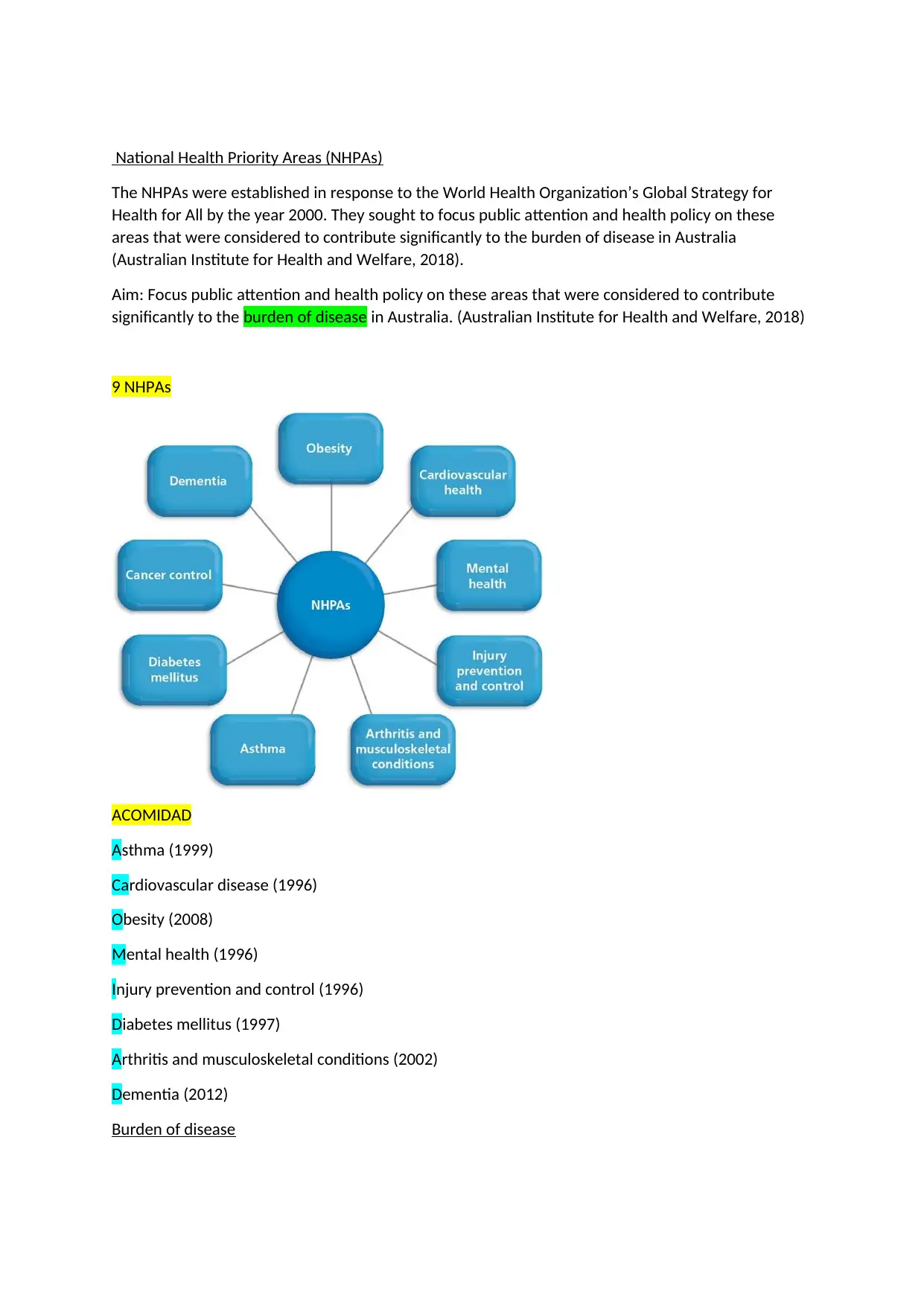
National Health Priority Areas (NHPAs)
The NHPAs were established in response to the World Health Organization’s Global Strategy for
Health for All by the year 2000. They sought to focus public attention and health policy on these
areas that were considered to contribute significantly to the burden of disease in Australia
(Australian Institute for Health and Welfare, 2018).
Aim: Focus public attention and health policy on these areas that were considered to contribute
significantly to the burden of disease in Australia. (Australian Institute for Health and Welfare, 2018)
9 NHPAs
ACOMIDAD
Asthma (1999)
Cardiovascular disease (1996)
Obesity (2008)
Mental health (1996)
Injury prevention and control (1996)
Diabetes mellitus (1997)
Arthritis and musculoskeletal conditions (2002)
Dementia (2012)
Burden of disease
The NHPAs were established in response to the World Health Organization’s Global Strategy for
Health for All by the year 2000. They sought to focus public attention and health policy on these
areas that were considered to contribute significantly to the burden of disease in Australia
(Australian Institute for Health and Welfare, 2018).
Aim: Focus public attention and health policy on these areas that were considered to contribute
significantly to the burden of disease in Australia. (Australian Institute for Health and Welfare, 2018)
9 NHPAs
ACOMIDAD
Asthma (1999)
Cardiovascular disease (1996)
Obesity (2008)
Mental health (1996)
Injury prevention and control (1996)
Diabetes mellitus (1997)
Arthritis and musculoskeletal conditions (2002)
Dementia (2012)
Burden of disease
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
- Measures the combined impact of morbidity (non-fatal burden) and mortality (fatal burden)
to assess and compare the health loss from different diseases and injuries in a population.
- Risk factors such as tobacco use, risky alcohol consumption, illicit drug use, insufficient
physical activity, and poor eating patterns can have a detrimental effect on health. Burden of
disease analysis also estimates the contribution of various risk factors to disease burden.
Module 5: Culture and Indigenous Health
Cultural sensitivity:
Cultural competence
Cultural Inclusion
Systematic Bias
Cultural conflict vs Harmony
Module 6: Sustainability
Module 7: Applying Primary Health Care
Module 8: Child and adolescent health
Healthy childhood development includes:
Physical
Social/emotional
Language/cognitive domains
Which influences well-being, obesity/stunting, mental health, heart disease, competence in literacy,
criminality, and economic participation throughout life.
Influences on child health in contemporary society:
Environmental advantage and disadvantage
Global factors-citizenship, political factors, migration, economic, cultural, religious, and
environmental disadvantage
to assess and compare the health loss from different diseases and injuries in a population.
- Risk factors such as tobacco use, risky alcohol consumption, illicit drug use, insufficient
physical activity, and poor eating patterns can have a detrimental effect on health. Burden of
disease analysis also estimates the contribution of various risk factors to disease burden.
Module 5: Culture and Indigenous Health
Cultural sensitivity:
Cultural competence
Cultural Inclusion
Systematic Bias
Cultural conflict vs Harmony
Module 6: Sustainability
Module 7: Applying Primary Health Care
Module 8: Child and adolescent health
Healthy childhood development includes:
Physical
Social/emotional
Language/cognitive domains
Which influences well-being, obesity/stunting, mental health, heart disease, competence in literacy,
criminality, and economic participation throughout life.
Influences on child health in contemporary society:
Environmental advantage and disadvantage
Global factors-citizenship, political factors, migration, economic, cultural, religious, and
environmental disadvantage
Vulnerability from low-socioeconomic (SES) environments, adverse events/stressors, social
exclusion, few future opportunities, level of parent, family and community support.
Adverse childhood experiences:
Emotional, physical abuse or neglect
Witnessing domestic violence
Living with mentally ill or substance-abusing family member
Losing parent—death, incarceration
Homelessness, overcrowding
Traumatic experiences
Migration, refugee detention
Poverty
Major issues affecting child health include:
Obesity, intellectual disabilities, behaviour problems, respiratory illnesses, oral health and
accident prevention
Equity of access to support and structures embedded in the social determinants of health
(SDH), especially in light of the ‘social gradient’ in health.
Psychosocial wellbeing
Family stability, support, low stress, good health
Environments that promote safe play, skills mastery
Supportive childcare, schools, neighbourhoods
Parenting style—authoritative—warm, responsive
High parent life satisfaction, strong, caring relationships irrespective of gendered parenting
Early learning opportunities in supportive centres
Regulation of ‘screen time’, internet safety
Children’s temperament and responses to family and community
Children and health promotion
leading causes of death in post-natal children
What was the SDG response to this? Discuss
how strategies of the Ottawa Charter for Health Promotion can be used for promoting adolescent
health?
What are the stages of transition for adolescents?
exclusion, few future opportunities, level of parent, family and community support.
Adverse childhood experiences:
Emotional, physical abuse or neglect
Witnessing domestic violence
Living with mentally ill or substance-abusing family member
Losing parent—death, incarceration
Homelessness, overcrowding
Traumatic experiences
Migration, refugee detention
Poverty
Major issues affecting child health include:
Obesity, intellectual disabilities, behaviour problems, respiratory illnesses, oral health and
accident prevention
Equity of access to support and structures embedded in the social determinants of health
(SDH), especially in light of the ‘social gradient’ in health.
Psychosocial wellbeing
Family stability, support, low stress, good health
Environments that promote safe play, skills mastery
Supportive childcare, schools, neighbourhoods
Parenting style—authoritative—warm, responsive
High parent life satisfaction, strong, caring relationships irrespective of gendered parenting
Early learning opportunities in supportive centres
Regulation of ‘screen time’, internet safety
Children’s temperament and responses to family and community
Children and health promotion
leading causes of death in post-natal children
What was the SDG response to this? Discuss
how strategies of the Ottawa Charter for Health Promotion can be used for promoting adolescent
health?
What are the stages of transition for adolescents?
Module 9: Adult Health and healthy ageing
Early Adulthood (20-40)
Middle Adulthood (40-65)
Older Adulthood (65+)
Main influences on health and illness in adulthood
Healthy living: Maintaining a healthy lifestyle and introducing habits that improve your health. E.g.,
Replacing what you eat/drink, sleep well, manage stress, practice safe sex, drink responsibly, being
physically active, aware of health risks related to illnesses, taking responsibility for your overall
healthy by heaving check-ups.
Benefits of healthy living
Feeling better mentally
Saving money
Fewer health problems
Taking control of your life
Social determinants of health
• Genetics and biology influences health and health outcomes
• Gender and social inclusion determine equitable circumstances, experiences.
Early Adulthood (20-40)
Middle Adulthood (40-65)
Older Adulthood (65+)
Main influences on health and illness in adulthood
Healthy living: Maintaining a healthy lifestyle and introducing habits that improve your health. E.g.,
Replacing what you eat/drink, sleep well, manage stress, practice safe sex, drink responsibly, being
physically active, aware of health risks related to illnesses, taking responsibility for your overall
healthy by heaving check-ups.
Benefits of healthy living
Feeling better mentally
Saving money
Fewer health problems
Taking control of your life
Social determinants of health
• Genetics and biology influences health and health outcomes
• Gender and social inclusion determine equitable circumstances, experiences.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
• Cultural environments and experiences—ethnicity, migrant, refugee, cultural
supports, culturally safe care, Aboriginal and Torres Strait Islander people, gender,
and sexual diverse people
• Health status in early, mid, late adulthood, health practices, lifestyle, supportive
services, resources
• Culmination of policy environments that have impacted on adult lives and health
choices, such as occupational health and safety, tobacco advertising and taxes, and
school health policies.
• Family structure, socio-economic position, events, processes, type, and frequency of
transitions: single to someone with a family, having children and becoming parents,
changes in causes of stress and need for social support.
• Physical environment, neighbourhood—health and place
• Employment, balanced work, and family lifestyle
• Stressors and learned coping behaviours (Clendon & Munns, 2019
Older Adulthood (65 onwards)
Rapid increase of those born between 1946 to 1964: Extension of average lifespan due to:
- Improvements in environmental hygiene, health services and medical science
Healthy aging: Maintaining the functional ability that allows you to do the things you value.
Preserving physical and mental capacity as you age. It will help build societies that are cohesive,
peaceful, just, secure, and sustainable.
E.g.:
- Making changes to our environment (housing, transportation, public spaces etc.)
A commitment to the Sustainable Development Goals means a commitment to Healthy Ageing.
For example,= bullet point = ways to foster Healthy Aging for all
supports, culturally safe care, Aboriginal and Torres Strait Islander people, gender,
and sexual diverse people
• Health status in early, mid, late adulthood, health practices, lifestyle, supportive
services, resources
• Culmination of policy environments that have impacted on adult lives and health
choices, such as occupational health and safety, tobacco advertising and taxes, and
school health policies.
• Family structure, socio-economic position, events, processes, type, and frequency of
transitions: single to someone with a family, having children and becoming parents,
changes in causes of stress and need for social support.
• Physical environment, neighbourhood—health and place
• Employment, balanced work, and family lifestyle
• Stressors and learned coping behaviours (Clendon & Munns, 2019
Older Adulthood (65 onwards)
Rapid increase of those born between 1946 to 1964: Extension of average lifespan due to:
- Improvements in environmental hygiene, health services and medical science
Healthy aging: Maintaining the functional ability that allows you to do the things you value.
Preserving physical and mental capacity as you age. It will help build societies that are cohesive,
peaceful, just, secure, and sustainable.
E.g.:
- Making changes to our environment (housing, transportation, public spaces etc.)
A commitment to the Sustainable Development Goals means a commitment to Healthy Ageing.
For example,= bullet point = ways to foster Healthy Aging for all
1. End poverty in all its forms everywhere (Goal 1): safety net for their rights and well-being
having flexible retirement policies
ensuring tax-funded minimum pensions.
Providing older workers with access to education or vocational training, re-skilling, or other
means to maintain their employability so that they can remain in the workforce for longer.
changing employers’ attitudes about the value and contributions of older workers
providing social assistance within the home and community for poor older people and for
those without family support
connecting informal workers with different forms of social security and pension
ensuring equitable access to, and utilisation of, health and long-term care services that are
integrated and coordinated to meet the needs of older people; and
helping families that care for older family members.
2. Zero hunger (Goal 2), improved nutrition: increase care dependency and decrease intrinsic
capacity.
Making improvements in the nutrient density of food such as vitamins and minerals
Maintaining intakes of energy and proteins
Recognising older people who have limited access to healthy meals.
3. Good Health and Well-being: Maintain independence and increase their social and economic
participation, reduce healthcare cost.
Equitable access to disease prevention, promotion, treatment, and rehab
Developing robust, integrated systems of health and long-term care orientated around
maximizing function in older age.
Available medicines and assistive
4. Quality Education: Knowledge and skills to manage their health, develop information,
independence, technology, adjust to changes, maintain their identity, social connections,
keep interested in life, foster contact with generations, participate in society (e.g.,
working/volunteering)
Providing basic literacy and health literacy training
Extend learning opportunities.
Reduce material and structural barriers.
5. Gender Equality: Women’s restricted participating in the paid workplace causing greater risk
of poverty, less access to quality health, reduce access to pensions. Enhanced wellbeing.
Robust systems that promote equitable workforce participation
Social pensions (raise status of older women, enable them to have role in household
decision-making, improved access to services.)
6. Industry, innovation, and infrastructure (Goal 9): Knowledge gaps because of exclusion and
participation
having flexible retirement policies
ensuring tax-funded minimum pensions.
Providing older workers with access to education or vocational training, re-skilling, or other
means to maintain their employability so that they can remain in the workforce for longer.
changing employers’ attitudes about the value and contributions of older workers
providing social assistance within the home and community for poor older people and for
those without family support
connecting informal workers with different forms of social security and pension
ensuring equitable access to, and utilisation of, health and long-term care services that are
integrated and coordinated to meet the needs of older people; and
helping families that care for older family members.
2. Zero hunger (Goal 2), improved nutrition: increase care dependency and decrease intrinsic
capacity.
Making improvements in the nutrient density of food such as vitamins and minerals
Maintaining intakes of energy and proteins
Recognising older people who have limited access to healthy meals.
3. Good Health and Well-being: Maintain independence and increase their social and economic
participation, reduce healthcare cost.
Equitable access to disease prevention, promotion, treatment, and rehab
Developing robust, integrated systems of health and long-term care orientated around
maximizing function in older age.
Available medicines and assistive
4. Quality Education: Knowledge and skills to manage their health, develop information,
independence, technology, adjust to changes, maintain their identity, social connections,
keep interested in life, foster contact with generations, participate in society (e.g.,
working/volunteering)
Providing basic literacy and health literacy training
Extend learning opportunities.
Reduce material and structural barriers.
5. Gender Equality: Women’s restricted participating in the paid workplace causing greater risk
of poverty, less access to quality health, reduce access to pensions. Enhanced wellbeing.
Robust systems that promote equitable workforce participation
Social pensions (raise status of older women, enable them to have role in household
decision-making, improved access to services.)
6. Industry, innovation, and infrastructure (Goal 9): Knowledge gaps because of exclusion and
participation
make older people visible by disaggregating data based on age and measuring Healthy
Ageing.
Ensure research is responsive to the needs of older adults and policy makers.
Foster innovation that targets the changes that population ageing brings. E.g., eHeathy
technology, that can virtually link older adults with services (improve health and social
outcomes)
Communicate data and research in ways older people can understand.
7. Reduce inequalities (Goal 10): Physical and social environments.
Ensure people with greater health need are prioritised.
Breakdown the many barriers that limit ongoing social participating
8. Sustainable cities and communities (Goal 11): Age friendly cities/communities
Anticipate and respond flexibly to aging-related needs and preferences.
Respect older people’s decisions and lifestyle choices
Protect those who are most vulnerable.
Promote older people’s inclusion and contribution to all areas of community life.
9. Peace, Justice, and strong institutions (Goal 16): Shape institutions towards sustainable
inclusivity and to empower older people to achieve.
Ageism- stereotypes, prejudice, and discrimination against older people based on their
chronological or perceived age – creates barriers to 28 developing good policies, both on
health and broader development.
Awareness campaigns about ageing
Advocacy messages to all relevant sectors on how they can contribute to Healthy Ageing.
communicating the best practices of other successful intersectoral strategies that have
contributed to Healthy Ageing.
encouraging legislation and policies against age-based discrimination in all aspects of
society.
UN Decade of Healthy Aging (2021-2030)
A global collaboration linked with the Sustainable Development Goals, that brings together
governments, civil society, international agencies, professionals, academia, the media, and the
private sector to improve the lives of older people, their families, and the communities in which they
live.
Action Areas:
Age Friendly Environments
Environment determines our physical and mental capacity and how well we adjust to loss of
function and forms of adversity. E.g., Global Network for Age Friendly Cities and Communities;
building capacity through mentoring (Age-friendly Environments Mentorship Programme
Ageing.
Ensure research is responsive to the needs of older adults and policy makers.
Foster innovation that targets the changes that population ageing brings. E.g., eHeathy
technology, that can virtually link older adults with services (improve health and social
outcomes)
Communicate data and research in ways older people can understand.
7. Reduce inequalities (Goal 10): Physical and social environments.
Ensure people with greater health need are prioritised.
Breakdown the many barriers that limit ongoing social participating
8. Sustainable cities and communities (Goal 11): Age friendly cities/communities
Anticipate and respond flexibly to aging-related needs and preferences.
Respect older people’s decisions and lifestyle choices
Protect those who are most vulnerable.
Promote older people’s inclusion and contribution to all areas of community life.
9. Peace, Justice, and strong institutions (Goal 16): Shape institutions towards sustainable
inclusivity and to empower older people to achieve.
Ageism- stereotypes, prejudice, and discrimination against older people based on their
chronological or perceived age – creates barriers to 28 developing good policies, both on
health and broader development.
Awareness campaigns about ageing
Advocacy messages to all relevant sectors on how they can contribute to Healthy Ageing.
communicating the best practices of other successful intersectoral strategies that have
contributed to Healthy Ageing.
encouraging legislation and policies against age-based discrimination in all aspects of
society.
UN Decade of Healthy Aging (2021-2030)
A global collaboration linked with the Sustainable Development Goals, that brings together
governments, civil society, international agencies, professionals, academia, the media, and the
private sector to improve the lives of older people, their families, and the communities in which they
live.
Action Areas:
Age Friendly Environments
Environment determines our physical and mental capacity and how well we adjust to loss of
function and forms of adversity. E.g., Global Network for Age Friendly Cities and Communities;
building capacity through mentoring (Age-friendly Environments Mentorship Programme
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
(MENTOR-AFE) and age Friendly in Practice (responding to older adults needs and preferences in
an equitable way) (WHO, 2021).
Combatting Ageism
Integrated Care
Older people require essential health services that include prevention, promotion, curative,
rehabilitative, palliative, End of Life care, safe, affordable, effective, good-quality essential
medicines and vaccines, dental care and health and assistive technologies, while ensuring that
use of these services does not cause the user financial hardship.
Long-term Care
Changes in physical and mental capacity can limit older people’s ability to participate in activities
of living and at a functional level 33 in society. Access to rehabilitation, assisted technologies and
supportive, inclusive environments can improve the level of capacity. Long-term care is essential
to maintain their functionality.
Module 10: Assessing the Community
an equitable way) (WHO, 2021).
Combatting Ageism
Integrated Care
Older people require essential health services that include prevention, promotion, curative,
rehabilitative, palliative, End of Life care, safe, affordable, effective, good-quality essential
medicines and vaccines, dental care and health and assistive technologies, while ensuring that
use of these services does not cause the user financial hardship.
Long-term Care
Changes in physical and mental capacity can limit older people’s ability to participate in activities
of living and at a functional level 33 in society. Access to rehabilitation, assisted technologies and
supportive, inclusive environments can improve the level of capacity. Long-term care is essential
to maintain their functionality.
Module 10: Assessing the Community
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.




