Prioritisation and Delegation in Clinical Settings
VerifiedAdded on 2023/06/05
|13
|4713
|234
AI Summary
This article discusses the importance of prioritisation and delegation in clinical settings, with examples of tasks that need to be prioritised and delegated to different healthcare professionals. It also covers collaborative and therapeutic practice, provision and coordination of care, and time management and delegation. The article is relevant to NRSG355 and other related courses in nursing and healthcare.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
NRSG355 2018 |
NRSG355 WRITTEN ASSESSMENT
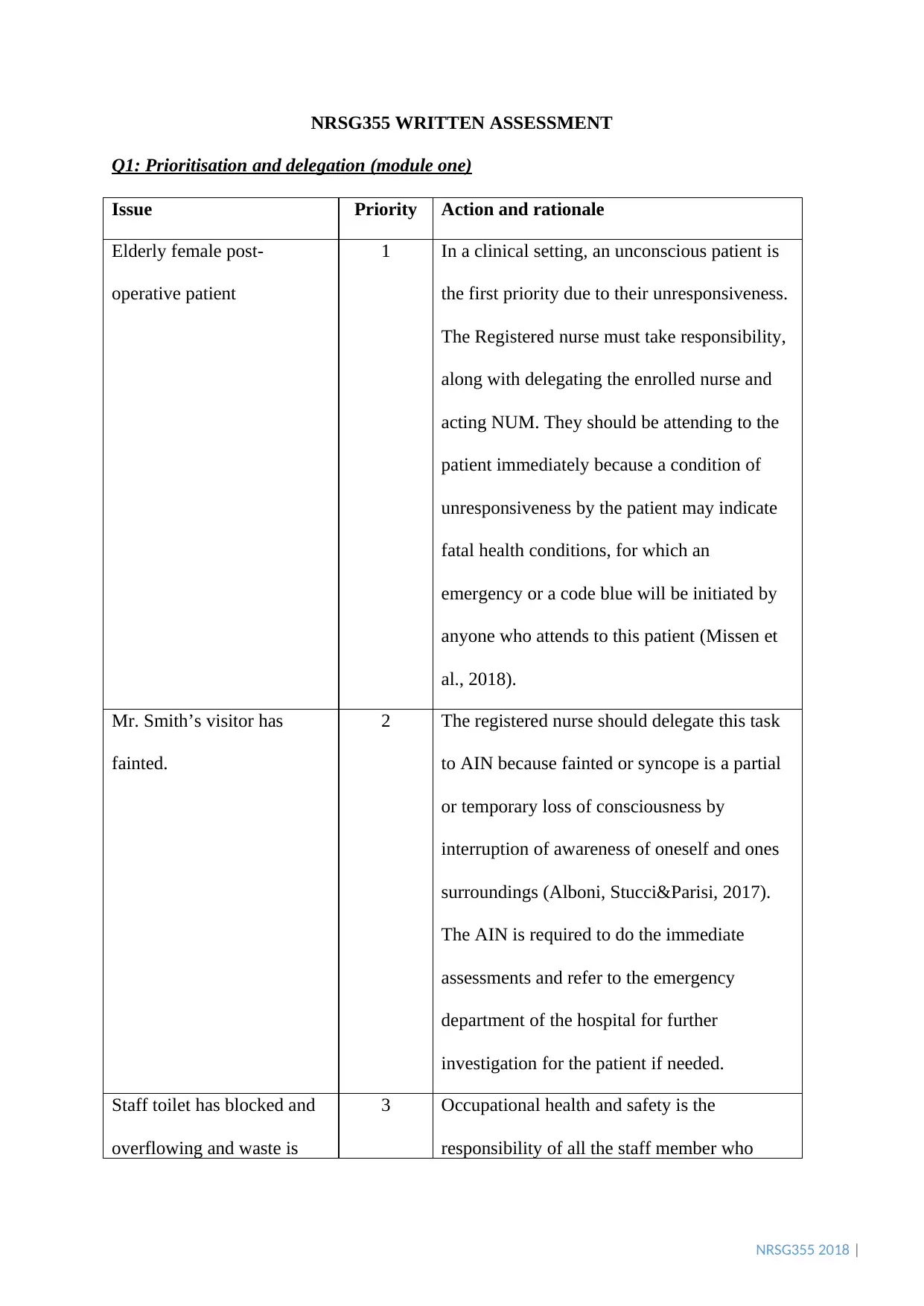
Q1: Prioritisation and delegation (module one)
Issue Priority Action and rationale
Elderly female post-
operative patient
1 In a clinical setting, an unconscious patient is
the first priority due to their unresponsiveness.
The Registered nurse must take responsibility,
along with delegating the enrolled nurse and
acting NUM. They should be attending to the
patient immediately because a condition of
unresponsiveness by the patient may indicate
fatal health conditions, for which an
emergency or a code blue will be initiated by
anyone who attends to this patient (Missen et
al., 2018).
Mr. Smith’s visitor has
fainted.
2 The registered nurse should delegate this task
to AIN because fainted or syncope is a partial
or temporary loss of consciousness by
interruption of awareness of oneself and ones
surroundings (Alboni, Stucci&Parisi, 2017).
The AIN is required to do the immediate
assessments and refer to the emergency
department of the hospital for further
investigation for the patient if needed.
Staff toilet has blocked and
overflowing and waste is
3 Occupational health and safety is the
responsibility of all the staff member who
NRSG355 WRITTEN ASSESSMENT
Q1: Prioritisation and delegation (module one)
Issue Priority Action and rationale
Elderly female post-
operative patient
1 In a clinical setting, an unconscious patient is
the first priority due to their unresponsiveness.
The Registered nurse must take responsibility,
along with delegating the enrolled nurse and
acting NUM. They should be attending to the
patient immediately because a condition of
unresponsiveness by the patient may indicate
fatal health conditions, for which an
emergency or a code blue will be initiated by
anyone who attends to this patient (Missen et
al., 2018).
Mr. Smith’s visitor has
fainted.
2 The registered nurse should delegate this task
to AIN because fainted or syncope is a partial
or temporary loss of consciousness by
interruption of awareness of oneself and ones
surroundings (Alboni, Stucci&Parisi, 2017).
The AIN is required to do the immediate
assessments and refer to the emergency
department of the hospital for further
investigation for the patient if needed.
Staff toilet has blocked and
overflowing and waste is
3 Occupational health and safety is the
responsibility of all the staff member who
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
NRSG355 2018 |
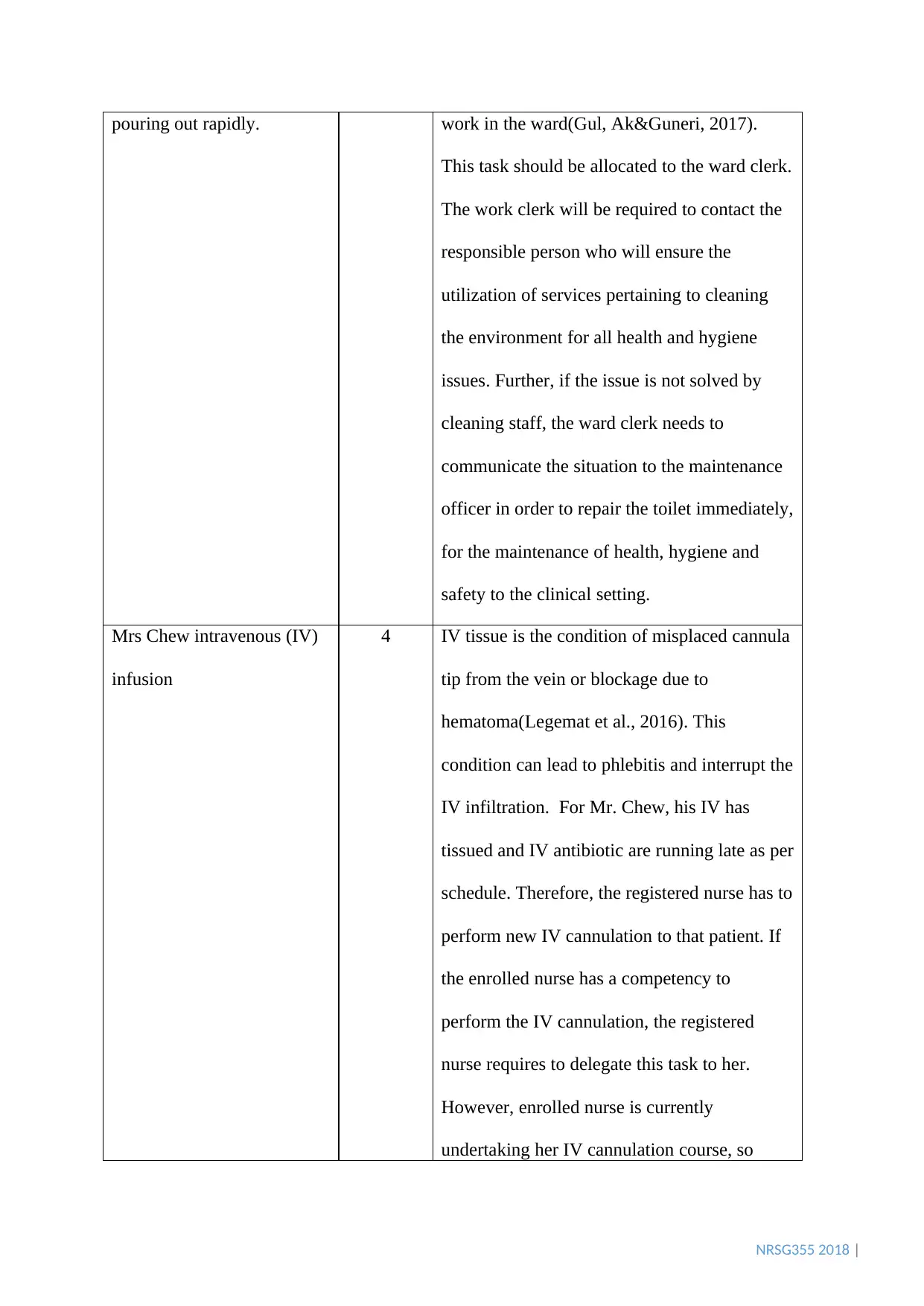
pouring out rapidly. work in the ward(Gul, Ak&Guneri, 2017).
This task should be allocated to the ward clerk.
The work clerk will be required to contact the
responsible person who will ensure the
utilization of services pertaining to cleaning
the environment for all health and hygiene
issues. Further, if the issue is not solved by
cleaning staff, the ward clerk needs to
communicate the situation to the maintenance
officer in order to repair the toilet immediately,
for the maintenance of health, hygiene and
safety to the clinical setting.
Mrs Chew intravenous (IV)
infusion
4 IV tissue is the condition of misplaced cannula
tip from the vein or blockage due to
hematoma(Legemat et al., 2016). This
condition can lead to phlebitis and interrupt the
IV infiltration. For Mr. Chew, his IV has
tissued and IV antibiotic are running late as per
schedule. Therefore, the registered nurse has to
perform new IV cannulation to that patient. If
the enrolled nurse has a competency to
perform the IV cannulation, the registered
nurse requires to delegate this task to her.
However, enrolled nurse is currently
undertaking her IV cannulation course, so
pouring out rapidly. work in the ward(Gul, Ak&Guneri, 2017).
This task should be allocated to the ward clerk.
The work clerk will be required to contact the
responsible person who will ensure the
utilization of services pertaining to cleaning
the environment for all health and hygiene
issues. Further, if the issue is not solved by
cleaning staff, the ward clerk needs to
communicate the situation to the maintenance
officer in order to repair the toilet immediately,
for the maintenance of health, hygiene and
safety to the clinical setting.
Mrs Chew intravenous (IV)
infusion
4 IV tissue is the condition of misplaced cannula
tip from the vein or blockage due to
hematoma(Legemat et al., 2016). This
condition can lead to phlebitis and interrupt the
IV infiltration. For Mr. Chew, his IV has
tissued and IV antibiotic are running late as per
schedule. Therefore, the registered nurse has to
perform new IV cannulation to that patient. If
the enrolled nurse has a competency to
perform the IV cannulation, the registered
nurse requires to delegate this task to her.
However, enrolled nurse is currently
undertaking her IV cannulation course, so
NRSG355 2018 |
registered nurse is the only person to perform
the task in this case.
Mr. Esposito perioperative
medication
5 Administration of perioperative medication is
important for patient who will undergo the
procedure in order to avoid any complications
during the procedure(Orser, David & Cohen,
2016). This task should be delegated to
enrolled nurse. Therefore, enrolled nurse
should administer the required medication to
Mr. Esposito after attending the fainted patient.
Discussion of medication
error
6 The acting NUM is the most responsible
person to attend the medication error
discussion with surgical consultant because she
is the only person who have authority and
extensive clinical experience than others
(Manning et al., 2015).
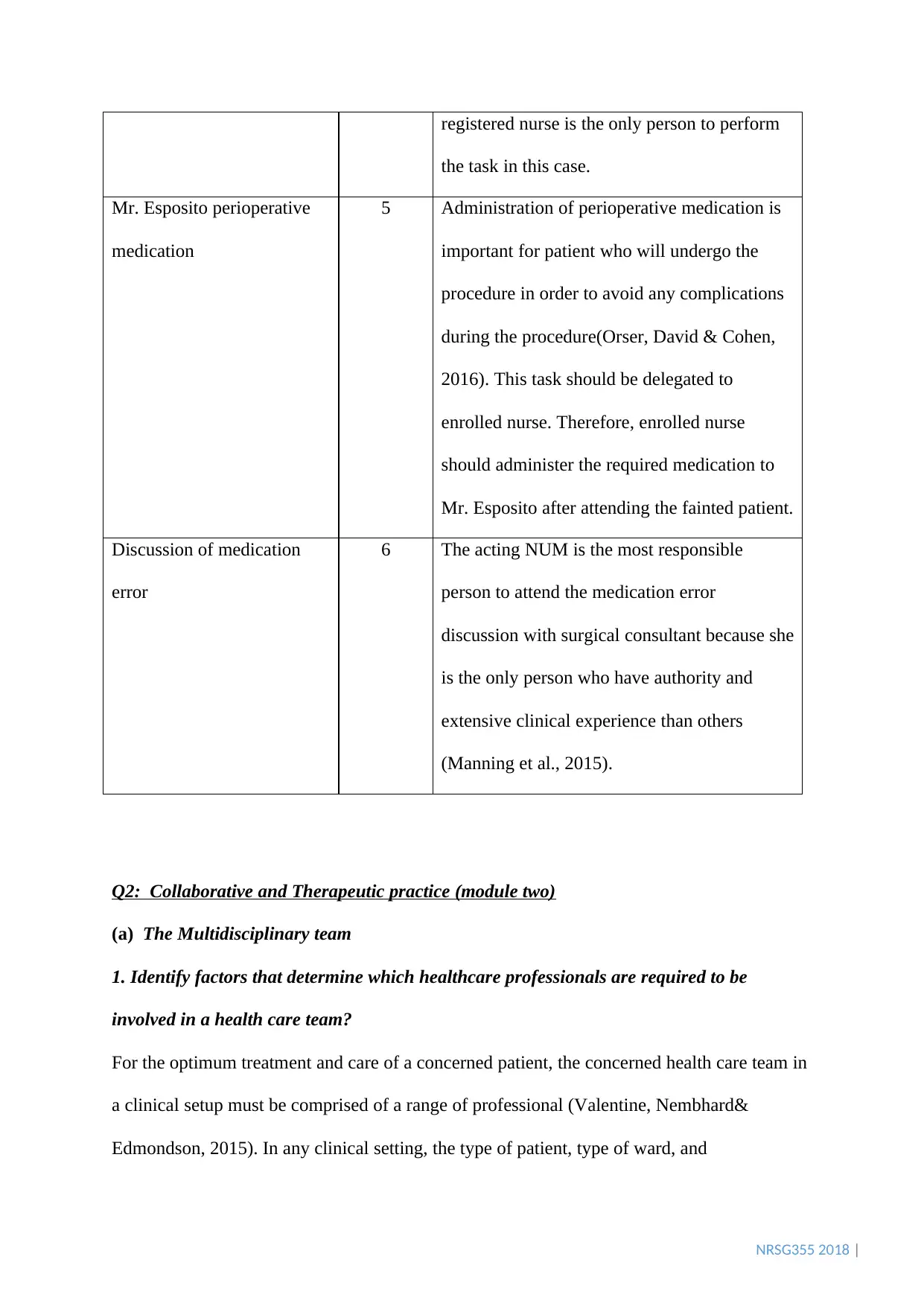
Q2: Collaborative and Therapeutic practice (module two)
(a) The Multidisciplinary team
1. Identify factors that determine which healthcare professionals are required to be
involved in a health care team?
For the optimum treatment and care of a concerned patient, the concerned health care team in
a clinical setup must be comprised of a range of professional (Valentine, Nembhard&
Edmondson, 2015). In any clinical setting, the type of patient, type of ward, and
registered nurse is the only person to perform
the task in this case.
Mr. Esposito perioperative
medication
5 Administration of perioperative medication is
important for patient who will undergo the
procedure in order to avoid any complications
during the procedure(Orser, David & Cohen,
2016). This task should be delegated to
enrolled nurse. Therefore, enrolled nurse
should administer the required medication to
Mr. Esposito after attending the fainted patient.
Discussion of medication
error
6 The acting NUM is the most responsible
person to attend the medication error
discussion with surgical consultant because she
is the only person who have authority and
extensive clinical experience than others
(Manning et al., 2015).
Q2: Collaborative and Therapeutic practice (module two)
(a) The Multidisciplinary team
1. Identify factors that determine which healthcare professionals are required to be
involved in a health care team?
For the optimum treatment and care of a concerned patient, the concerned health care team in
a clinical setup must be comprised of a range of professional (Valentine, Nembhard&
Edmondson, 2015). In any clinical setting, the type of patient, type of ward, and
NRSG355 2018 |
organizational policy are the primary factors which will determine the health care team.
Alsoavailability of staff member is the main concern to form required health care team, since
a reduced workforce will be unavailable to perform the required treatment procedures due to
the excessive workload. For example, doctor needs to be involved in order to diagnose the
patient, as well as for the effective implementation of care plan (Powell et al., 2016). Nurses
should be included in multidisciplinary team to provide personalized care to patient
(Andregård & Jangland, 2015). Moreover, occupational therapeutic professionals are required
to be involved in the health care team to demonstrate the safe mobility of patient (Dahl-
Popolizio et al., 2016) and dietitians are also required to provide the nutritional advice for
quick recovery through recommendation of meals containing the required nutrients. (Shoham
et al., 2016).
2. Who should lead the health care team?
The doctor is the most responsible person who will perform the required diagnosis and
implement the care plan according to the diagnosis (Boquiren et al., 2015). Therefore, the
doctor should lead the health care team.
3. Who is the most important member of the health care team?
The patient is the most important person of the health care team because patient is the
decision maker of their treatment. Hence, for the adequate functioning of a healthcare team, a
patient centered approach must be followed where the concerned patient must be informed
about the treatment plan chosen (Constand et al., 2014). However, the doctor is also one of
the most important person in health care treatment and the nurses are also main caregivers
who perform all the treatments delegated by doctors, as they will be significantly involved in
assisting as well as attending to the patient when the doctor will be absent (Casmiro et al.,
2015).
organizational policy are the primary factors which will determine the health care team.
Alsoavailability of staff member is the main concern to form required health care team, since
a reduced workforce will be unavailable to perform the required treatment procedures due to
the excessive workload. For example, doctor needs to be involved in order to diagnose the
patient, as well as for the effective implementation of care plan (Powell et al., 2016). Nurses
should be included in multidisciplinary team to provide personalized care to patient
(Andregård & Jangland, 2015). Moreover, occupational therapeutic professionals are required
to be involved in the health care team to demonstrate the safe mobility of patient (Dahl-
Popolizio et al., 2016) and dietitians are also required to provide the nutritional advice for
quick recovery through recommendation of meals containing the required nutrients. (Shoham
et al., 2016).
2. Who should lead the health care team?
The doctor is the most responsible person who will perform the required diagnosis and
implement the care plan according to the diagnosis (Boquiren et al., 2015). Therefore, the
doctor should lead the health care team.
3. Who is the most important member of the health care team?
The patient is the most important person of the health care team because patient is the
decision maker of their treatment. Hence, for the adequate functioning of a healthcare team, a
patient centered approach must be followed where the concerned patient must be informed
about the treatment plan chosen (Constand et al., 2014). However, the doctor is also one of
the most important person in health care treatment and the nurses are also main caregivers
who perform all the treatments delegated by doctors, as they will be significantly involved in
assisting as well as attending to the patient when the doctor will be absent (Casmiro et al.,
2015).
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
NRSG355 2018 |
(b) Case Study 2
1. What are the key issues in this dilemma?
The key issue here is the ethical dilemma as an outcome of patient medical choices, which
advocates the idea of consideration of the opinion of the patient or the family, in the decision-
making process. (Ganz, Wagner &Toren, 2015). Despite Norma encountering complete
recovery followed by allocation of a multidisciplinary for her care, there is also a need to
consider her son’s demands since patient opinion is intrinsic for the maintenance of quality
healthcare.
2. How would you deal with Norma’s son? Are his objections warranted?
With respect to the Norma’s condition, a team leader should consider Norma’s preferences of
staying in the nursing home, since she had established several compatible relationships there.
Concerning Norma’s son, a team leader should elaborate another group discussion, which
would involve patient, patient’s family(her son) and the multidisciplinary team (Ganz,
Wagner &Toren, 2015). Teamleadercan even arrange for a demonstration where Norma’s son
can observe the care his mother is receiving or refer the second opinion service that provide
an interactive session between a clinical specialist and Norma’s son, where the specialist will
consult and provide him with a one-time opinion about the required action to be taken
(Meyer, Singh & Graber, 2015). Furthermore, team leaders are required toexplain the
increased financial burden which Norma’s son might face upon unnecessary inpatient
administration, along with a personal interest of patient, preferring to reside in the nursing
home as usual (Truog et al., 2015).
Q3: Provision and coordination of care (module three
1. What further questions will you need to ask the nurse?
According to the handover, the emergency nurse did not mention patient GCS level. Patient
GCS level is very important to continue further assessment and treatment. Therefore it is
(b) Case Study 2
1. What are the key issues in this dilemma?
The key issue here is the ethical dilemma as an outcome of patient medical choices, which
advocates the idea of consideration of the opinion of the patient or the family, in the decision-
making process. (Ganz, Wagner &Toren, 2015). Despite Norma encountering complete
recovery followed by allocation of a multidisciplinary for her care, there is also a need to
consider her son’s demands since patient opinion is intrinsic for the maintenance of quality
healthcare.
2. How would you deal with Norma’s son? Are his objections warranted?
With respect to the Norma’s condition, a team leader should consider Norma’s preferences of
staying in the nursing home, since she had established several compatible relationships there.
Concerning Norma’s son, a team leader should elaborate another group discussion, which
would involve patient, patient’s family(her son) and the multidisciplinary team (Ganz,
Wagner &Toren, 2015). Teamleadercan even arrange for a demonstration where Norma’s son
can observe the care his mother is receiving or refer the second opinion service that provide
an interactive session between a clinical specialist and Norma’s son, where the specialist will
consult and provide him with a one-time opinion about the required action to be taken
(Meyer, Singh & Graber, 2015). Furthermore, team leaders are required toexplain the
increased financial burden which Norma’s son might face upon unnecessary inpatient
administration, along with a personal interest of patient, preferring to reside in the nursing
home as usual (Truog et al., 2015).
Q3: Provision and coordination of care (module three
1. What further questions will you need to ask the nurse?
According to the handover, the emergency nurse did not mention patient GCS level. Patient
GCS level is very important to continue further assessment and treatment. Therefore it is

NRSG355 2018 |
necessary to ask the level of patient’s consciousness. The Glasgow Coma Scale is a necessary
neurological assessment tool for the purpose of measuring the level of consciousness of a
patient, who has suffered from head injuries (Teasedale et al., 2014).
Patient is admitted to the hospital due to his abdominal pain. However, the emergency nurse
has not mentioned the score of the pain and what measure or treatment of pain they have
done. Therefore, information related to pain should be asked because pain can alter patient
base line vital signs, coping ability, and anxiety level. Hence a PQRST pain assessment tool
will be required to be conducted (Fink & Brant, 2018).
Emergency nurse mentioned that patient’s output was good but did not mentioned about fluid
balance chart. So registered nurse will be required to ask fluid balance chartin order to update
the fluid consuming and outputting which will indicate the level of electrolytes present in the
patient, the status of hydration along with amount of water ingested and excreted by the
patient. This will ultimately determine the required medications to be administered as well
the treatments to be prescribed(de Oliveira et al., 2015).
Patient regular medications information is missing in handover, so the nurse also needs to
enquire about the medications because patient may have co-morbidities. Social status of
patient is required to know in case of emergency contact, where the concerned family must be
informed about the treatment as per the rules of adhering to family centered care in a clinical
setting (Tang et al., 2018).
2. List specifically what further assessments you would complete when the patient arrives
onto the ward?
Neurological assessment GCS: The Glasgow Coma Scale is used with the rationale to
determine the level at which the patient is conscious, especially for patients who have
underwent a head injury. The tool requires an assessment of 15 points in which three aspects
necessary to ask the level of patient’s consciousness. The Glasgow Coma Scale is a necessary
neurological assessment tool for the purpose of measuring the level of consciousness of a
patient, who has suffered from head injuries (Teasedale et al., 2014).
Patient is admitted to the hospital due to his abdominal pain. However, the emergency nurse
has not mentioned the score of the pain and what measure or treatment of pain they have
done. Therefore, information related to pain should be asked because pain can alter patient
base line vital signs, coping ability, and anxiety level. Hence a PQRST pain assessment tool
will be required to be conducted (Fink & Brant, 2018).
Emergency nurse mentioned that patient’s output was good but did not mentioned about fluid
balance chart. So registered nurse will be required to ask fluid balance chartin order to update
the fluid consuming and outputting which will indicate the level of electrolytes present in the
patient, the status of hydration along with amount of water ingested and excreted by the
patient. This will ultimately determine the required medications to be administered as well
the treatments to be prescribed(de Oliveira et al., 2015).
Patient regular medications information is missing in handover, so the nurse also needs to
enquire about the medications because patient may have co-morbidities. Social status of
patient is required to know in case of emergency contact, where the concerned family must be
informed about the treatment as per the rules of adhering to family centered care in a clinical
setting (Tang et al., 2018).
2. List specifically what further assessments you would complete when the patient arrives
onto the ward?
Neurological assessment GCS: The Glasgow Coma Scale is used with the rationale to
determine the level at which the patient is conscious, especially for patients who have
underwent a head injury. The tool requires an assessment of 15 points in which three aspects
NRSG355 2018 |
will be measured such as motor responses, eye opening and verbal responses. Through this
assessment tool, two levels of the consciousness of the patient is evaluated: Namely
awareness, which relates to how much the patient has understood when spoken to, and
wakefulness or a sense of arousal concerning his or environment. The Glasgow Coma Scale
should be performed in order to understand the level of unconsciousness in a patient who has
suffered from a severe injury in the brain. This will help to understand how severely the
functions of the brain have been affected (Chandrasekhar et al., 2017).
Vital signs: The rationale behind this assessment is rate of the efficiency of highly basic
functions of the human body, which include pulse rate, body temperature, blood pressure and
rate of respiration. This assessment must be performed to understand how severely basic
body functions have been affected, since a lack of basic functioning may indicate medical
emergency and immediate treatment for the patient (Fridkin et al., 2014).
Abdominal assessment: The rationale behind this assessment is to understand if the patients
abdominal functions are being carried out normally and includes, inspecting the abdominal
area for appropriate sounds or for the presence of any protrusions, and feeling or palpating
the abdomen. This should be performed to detect the presence of any oedema or
accumulation of fluids, which may pose to be an underlying cause of possible renal disorders
(Slayton et al., 2015).
Pain assessment: Upon ward arrival, for the purpose of evaluating the magnitude of pain
experienced by the patient, the nurse may be required to execute a pain assessment, which
represents the PQRST principles required to obtain a comprehensive history of the pain
suffered by the patient. The rationale behind this assessment is to accurately measure the
nature of pain felt by the patient and must be performed to understand the severity of pain
through assessment of Paliation/provocation, Quantity/Quality, Region/Radiation, Severty
and Timings of pain felt (MacSorley et al., 2014)
will be measured such as motor responses, eye opening and verbal responses. Through this
assessment tool, two levels of the consciousness of the patient is evaluated: Namely
awareness, which relates to how much the patient has understood when spoken to, and
wakefulness or a sense of arousal concerning his or environment. The Glasgow Coma Scale
should be performed in order to understand the level of unconsciousness in a patient who has
suffered from a severe injury in the brain. This will help to understand how severely the
functions of the brain have been affected (Chandrasekhar et al., 2017).
Vital signs: The rationale behind this assessment is rate of the efficiency of highly basic
functions of the human body, which include pulse rate, body temperature, blood pressure and
rate of respiration. This assessment must be performed to understand how severely basic
body functions have been affected, since a lack of basic functioning may indicate medical
emergency and immediate treatment for the patient (Fridkin et al., 2014).
Abdominal assessment: The rationale behind this assessment is to understand if the patients
abdominal functions are being carried out normally and includes, inspecting the abdominal
area for appropriate sounds or for the presence of any protrusions, and feeling or palpating
the abdomen. This should be performed to detect the presence of any oedema or
accumulation of fluids, which may pose to be an underlying cause of possible renal disorders
(Slayton et al., 2015).
Pain assessment: Upon ward arrival, for the purpose of evaluating the magnitude of pain
experienced by the patient, the nurse may be required to execute a pain assessment, which
represents the PQRST principles required to obtain a comprehensive history of the pain
suffered by the patient. The rationale behind this assessment is to accurately measure the
nature of pain felt by the patient and must be performed to understand the severity of pain
through assessment of Paliation/provocation, Quantity/Quality, Region/Radiation, Severty
and Timings of pain felt (MacSorley et al., 2014)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NRSG355 2018 |
Respiratory assessment: The rationale behind this is the detected of any disease of
pathological condition of the lungs. An assessment of the pulmonary system must be
performed in order to determine whether the patient is suffering from suspected pneumonia.
The doctor and nurse must carefully observe the breathing of the patient, and presence of
wheezing may indicate pneumonia. The lungs which are affected with pneumonia may also
produce abnormal sounds of bubbling, rumbling and crackling (Self et al., 2015).
Cardiac assessment: The rationale behind this assessment is to detect in pathological
condition or disorder of the heart, especially if the patient complaints of angina pectoris or
severe chest pain. This will include evaluating whether the patient possesses a history of
cardiovascular disorders, such as high blood pressure, occurrences of heart attacks or strokes.
This must be performed to detect existing patient problem concerning his cardiovascular
system and also to determine the possibilities of future myocardial risks of the patient (Myers
et al., 2015).
Q4: Time management and delegation(module four)
According to the New South Wales Government, there are a total of 5 nursing allocation
models, namely, Team, Modular, Task, Allocation and Primary Nursing Models. In team
nursing, a team leader must be present, who will engage in adequately bringing coordination
in the medical workforce, through appropriate delegation and identification of roles. Modular
model is a modified version of team nursing where the workforce duties are mentioned on the
basis of modules – which are groups of patients. The task allocation model focuses on
delegating and performing tasks based on the level of expertise and competency of the
workforce. Model of allocation nursing is based on delegating a number of patients to one
nurse who is capable of delivering complete treatment care. Finally the primary care model
involves delegating a single registered nurse to each patient (Slatyer et al., 2016).
Respiratory assessment: The rationale behind this is the detected of any disease of
pathological condition of the lungs. An assessment of the pulmonary system must be
performed in order to determine whether the patient is suffering from suspected pneumonia.
The doctor and nurse must carefully observe the breathing of the patient, and presence of
wheezing may indicate pneumonia. The lungs which are affected with pneumonia may also
produce abnormal sounds of bubbling, rumbling and crackling (Self et al., 2015).
Cardiac assessment: The rationale behind this assessment is to detect in pathological
condition or disorder of the heart, especially if the patient complaints of angina pectoris or
severe chest pain. This will include evaluating whether the patient possesses a history of
cardiovascular disorders, such as high blood pressure, occurrences of heart attacks or strokes.
This must be performed to detect existing patient problem concerning his cardiovascular
system and also to determine the possibilities of future myocardial risks of the patient (Myers
et al., 2015).
Q4: Time management and delegation(module four)
According to the New South Wales Government, there are a total of 5 nursing allocation
models, namely, Team, Modular, Task, Allocation and Primary Nursing Models. In team
nursing, a team leader must be present, who will engage in adequately bringing coordination
in the medical workforce, through appropriate delegation and identification of roles. Modular
model is a modified version of team nursing where the workforce duties are mentioned on the
basis of modules – which are groups of patients. The task allocation model focuses on
delegating and performing tasks based on the level of expertise and competency of the
workforce. Model of allocation nursing is based on delegating a number of patients to one
nurse who is capable of delivering complete treatment care. Finally the primary care model
involves delegating a single registered nurse to each patient (Slatyer et al., 2016).
NRSG355 2018 |
According to the given details, it can be observed that the total number of patients is 22, from
which 14 patients have encountered surgical procedures. The number of patients who have
received regular care is 8, along with 4 patients who have received access to intravenous
procedures. In addition to services, the position of a nurse unit manager is undertaken by
another nurse, followed by 3 AINs and 1 enrolled nurse. Hence, for this case we will be using
a team nursing model, would be a beneficial decision for the provision of optimum treatment
and care to the concerned patients, resulting in beneficial health implications and outcomes
(Bender, 2017). The usage of team nursing involves appropriate cooperation between nurses
as a team for the purpose of fulfilling organizational and treatment objectives. The major
advantages of this approach is increase of nurse satisfaction, provision of a collaborative
environment, improved communication between staff and most importantly, enhancement of
the quality and safety of the treatment given to the patient (Fairbrother, Chiarella&
Braithwaite, 2015).
What is delegation? When the registered nurse delegate, what you have to be aware to
other healthcare professional’s competencies?
Considering the dynamic principles of today’s organizations, registered nurses are required to
undertake a variety of activities such as leadership and delegation. Delegation is the act by
which the experienced nurse will be required to assign or instruct appropriate tasks to the
workforce. For the conductance of appropriate delegation activities, the registered nurse must
consider undertaking a transformational style of leadership, which will require of her to
delegate activities in accordance to the level of competency exhibited by the workforce
(Siegel et al., 2018). Hence, a registered nurse may not delegate critical or medical
emergency tasks to enrolled or AIN nurse due to their low level of competency and
experience (National Council of State Boards of Nursing, 2016). Hence for the following
case scenario, the patients who require surgical treatments require immediate assistance as
According to the given details, it can be observed that the total number of patients is 22, from
which 14 patients have encountered surgical procedures. The number of patients who have
received regular care is 8, along with 4 patients who have received access to intravenous
procedures. In addition to services, the position of a nurse unit manager is undertaken by
another nurse, followed by 3 AINs and 1 enrolled nurse. Hence, for this case we will be using
a team nursing model, would be a beneficial decision for the provision of optimum treatment
and care to the concerned patients, resulting in beneficial health implications and outcomes
(Bender, 2017). The usage of team nursing involves appropriate cooperation between nurses
as a team for the purpose of fulfilling organizational and treatment objectives. The major
advantages of this approach is increase of nurse satisfaction, provision of a collaborative
environment, improved communication between staff and most importantly, enhancement of
the quality and safety of the treatment given to the patient (Fairbrother, Chiarella&
Braithwaite, 2015).
What is delegation? When the registered nurse delegate, what you have to be aware to
other healthcare professional’s competencies?
Considering the dynamic principles of today’s organizations, registered nurses are required to
undertake a variety of activities such as leadership and delegation. Delegation is the act by
which the experienced nurse will be required to assign or instruct appropriate tasks to the
workforce. For the conductance of appropriate delegation activities, the registered nurse must
consider undertaking a transformational style of leadership, which will require of her to
delegate activities in accordance to the level of competency exhibited by the workforce
(Siegel et al., 2018). Hence, a registered nurse may not delegate critical or medical
emergency tasks to enrolled or AIN nurse due to their low level of competency and
experience (National Council of State Boards of Nursing, 2016). Hence for the following
case scenario, the patients who require surgical treatments require immediate assistance as
NRSG355 2018 |
compared to the rest of the patient group. For this purpose, the registered nurse is entrusted
with the utmost responsibility for the provision of such care, due to her advanced expertise
and experience in the management of patients requiring post-operative procedures. Due to
their low competency, the task of management of patients receiving conventional care will be
delegated to the newly enrolled or assistant nurses.
compared to the rest of the patient group. For this purpose, the registered nurse is entrusted
with the utmost responsibility for the provision of such care, due to her advanced expertise
and experience in the management of patients requiring post-operative procedures. Due to
their low competency, the task of management of patients receiving conventional care will be
delegated to the newly enrolled or assistant nurses.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
NRSG355 2018 |
References
Alboni, P., Stucci, N., & Parisi, C. (2017). Sinus bradycardia and syncope: what
pathophysiological mechanism and what management of the patient?. Giornaleitaliano di
cardiologia (2006), 18(11), 774-780.doi: https://doi.org/10.1714/2803.28363.
Andregård, A. C., &Jangland, E. (2015). The tortuous journey of introducing the Nurse
Practitioner as a new member of the healthcare team: A meta‐synthesis. Scandinavian
Journal of Caring Sciences, 29(1), 3-14.doi: https://doi.org/10.1111/scs.12120.
Bender, M., Williams, M., Su, W., &Hites, L. (2017). Refining and validating a conceptual
model of Clinical Nurse Leader integrated care delivery. Journal of advanced nursing, 73(2),
448-464.doi: https://doi.org/10.1111/jan.13113.
Boquiren, V. M., Hack, T. F., Beaver, K., & Williamson, S. (2015). What do measures of
patient satisfaction with the doctor tell us?. Patient education and counseling, 98(12), 1465-
1473.doi: https://doi.org/10.1016/j.pec.2015.05.020.
Casimiro, L. M., Hall, P., Kuziemsky, C., O'Connor, M., &Varpio, L. (2015). Enhancing
patient-engaged teamwork in healthcare: An observational case study. Journal of
interprofessional care, 29(1), 55-61.doi: https://doi.org/10.3109/13561820.2014.940038.
Chandrasekhar, S., Rahim, M. A., Quraishi, S. M., Theja, C. R., & Kiran, K. S. (2017). An
observational clinical study of assessing the utility of PSS (Poison Severity Score) and GCS
(Glasgow Coma Scale) scoring systems in predicting severity and clinical outcomes in op
poisoning. J Evidence Based Med Healthcare, 4(38), 2325-2332.doi:
10.18410/jebmh/2017/458.
Constand, M. K., MacDermid, J. C., Dal Bello-Haas, V., & Law, M. (2014). Scoping review of
patient-centered care approaches in healthcare. BMC health services research, 14(1),
271.doi: https://doi.org/10.1186/1472-6963-14-271.
Dahl-Popolizio, S., Manson, L., Muir, S., & Rogers, O. (2016). Enhancing the value of
integrated primary care: The role of occupational therapy. Families, Systems, &
Health, 34(3), 270.doi: http://psycnet.apa.org/doi/10.1037/fsh0000208.
de Oliveira, F. S. V., Freitas, F. G. R., Ferreira, E. M., de Castro, I., Bafi, A. T., de Azevedo,
L. C. P., & Machado, F. R. (2015). Positive fluid balance as a prognostic factor for mortality
and acute kidney injury in severe sepsis and septic shock. Journal of critical care, 30(1), 97-
101.doi: https://doi.org/10.1016/j.jcrc.2014.09.002.
Fairbrother, G., Chiarella, M., & Braithwaite, J. (2015). Models of care choices in today’s
nursing workplace: where does team nursing sit?. Australian Health Review, 39(5), 489-
493.doi: https://doi.org/10.1071/AH14091.
Fink, R. M., & Brant, J. M. (2018). Complex Cancer Pain Assessment. Hematology/oncology
clinics of North America, 32(3), 353-369.doi: https://doi.org/10.1016/j.hoc.2018.01.001.
Fridkin, S., Baggs, J., Fagan, R., Magill, S., Pollack, L. A., Malpiedi, P., ... & Samore, M. H.
(2014). Vital signs: improving antibiotic use among hospitalized patients. Morbidity and
mortality weekly report, 63(9), 194-200. doi:
https://europepmc.org/backend/ptpmcrender.fcgi?accid=PMC4584728&blobtype=pdf.
References
Alboni, P., Stucci, N., & Parisi, C. (2017). Sinus bradycardia and syncope: what
pathophysiological mechanism and what management of the patient?. Giornaleitaliano di
cardiologia (2006), 18(11), 774-780.doi: https://doi.org/10.1714/2803.28363.
Andregård, A. C., &Jangland, E. (2015). The tortuous journey of introducing the Nurse
Practitioner as a new member of the healthcare team: A meta‐synthesis. Scandinavian
Journal of Caring Sciences, 29(1), 3-14.doi: https://doi.org/10.1111/scs.12120.
Bender, M., Williams, M., Su, W., &Hites, L. (2017). Refining and validating a conceptual
model of Clinical Nurse Leader integrated care delivery. Journal of advanced nursing, 73(2),
448-464.doi: https://doi.org/10.1111/jan.13113.
Boquiren, V. M., Hack, T. F., Beaver, K., & Williamson, S. (2015). What do measures of
patient satisfaction with the doctor tell us?. Patient education and counseling, 98(12), 1465-
1473.doi: https://doi.org/10.1016/j.pec.2015.05.020.
Casimiro, L. M., Hall, P., Kuziemsky, C., O'Connor, M., &Varpio, L. (2015). Enhancing
patient-engaged teamwork in healthcare: An observational case study. Journal of
interprofessional care, 29(1), 55-61.doi: https://doi.org/10.3109/13561820.2014.940038.
Chandrasekhar, S., Rahim, M. A., Quraishi, S. M., Theja, C. R., & Kiran, K. S. (2017). An
observational clinical study of assessing the utility of PSS (Poison Severity Score) and GCS
(Glasgow Coma Scale) scoring systems in predicting severity and clinical outcomes in op
poisoning. J Evidence Based Med Healthcare, 4(38), 2325-2332.doi:
10.18410/jebmh/2017/458.
Constand, M. K., MacDermid, J. C., Dal Bello-Haas, V., & Law, M. (2014). Scoping review of
patient-centered care approaches in healthcare. BMC health services research, 14(1),
271.doi: https://doi.org/10.1186/1472-6963-14-271.
Dahl-Popolizio, S., Manson, L., Muir, S., & Rogers, O. (2016). Enhancing the value of
integrated primary care: The role of occupational therapy. Families, Systems, &
Health, 34(3), 270.doi: http://psycnet.apa.org/doi/10.1037/fsh0000208.
de Oliveira, F. S. V., Freitas, F. G. R., Ferreira, E. M., de Castro, I., Bafi, A. T., de Azevedo,
L. C. P., & Machado, F. R. (2015). Positive fluid balance as a prognostic factor for mortality
and acute kidney injury in severe sepsis and septic shock. Journal of critical care, 30(1), 97-
101.doi: https://doi.org/10.1016/j.jcrc.2014.09.002.
Fairbrother, G., Chiarella, M., & Braithwaite, J. (2015). Models of care choices in today’s
nursing workplace: where does team nursing sit?. Australian Health Review, 39(5), 489-
493.doi: https://doi.org/10.1071/AH14091.
Fink, R. M., & Brant, J. M. (2018). Complex Cancer Pain Assessment. Hematology/oncology
clinics of North America, 32(3), 353-369.doi: https://doi.org/10.1016/j.hoc.2018.01.001.
Fridkin, S., Baggs, J., Fagan, R., Magill, S., Pollack, L. A., Malpiedi, P., ... & Samore, M. H.
(2014). Vital signs: improving antibiotic use among hospitalized patients. Morbidity and
mortality weekly report, 63(9), 194-200. doi:
https://europepmc.org/backend/ptpmcrender.fcgi?accid=PMC4584728&blobtype=pdf.
NRSG355 2018 |
Ganz, F. D., Wagner, N., &Toren, O. (2015). Nurse middle manager ethical dilemmas and
moral distress. Nursing ethics, 22(1), 43-51.doi:
https://doi.org/10.1177%2F0969733013515490.
Gul, M., Ak, M. F., &Guneri, A. F. (2017). Occupational health and safety risk assessment in
hospitals: A case study using two-stage fuzzy multi-criteria approach. Human and Ecological
Risk Assessment: An International Journal, 23(2), 187-202.doi:
https://doi.org/10.1080/10807039.2016.1234363.
Legemaat, M., Carr, P. J., van Rens, R. M., van Dijk, M., Poslawsky, I. E., & van den
Hoogen, A. (2016). Peripheral intravenous cannulation: complication rates in the neonatal
population: a multicenter observational study. The journal of vascular access, 17(4), 360-
365.doi: https://doi.org/10.5301%2Fjva.5000558.
MacSorley, R., White, J., Conerly, V. H., Walker, J. T., Lofton, S., Ragland, G., ...&
Robertson, A. (2014). Pain assessment and management strategies for elderly
patients. Home Healthcare Now, 32(5), 272-285.doi: 10.1097/NHH.0000000000000065.
Manning, V., Jones, A., Jones, P., & Fernandez, R. S. (2015). Planning for a smooth
transition: evaluation of a succession planning program for prospective nurse unit
managers. Nursing administration quarterly, 39(1), 58-68.doi:
10.1097/NAQ.0000000000000072.
Meyer, A. N., Singh, H., & Graber, M. L. (2015). Evaluation of outcomes from a national
patient-initiated second-opinion program. The American journal of medicine, 128(10), 1138-
e25.doi: https://doi.org/10.1016/j.amjmed.2015.04.020.
Missen, K., Porter, J. E., Raymond, A., de Vent, K., & Larkins, J. A. (2018). Adult
Deterioration Detection System (ADDS): An evaluation of the impact on MET and Code blue
activations in a regional healthcare service. Collegian, 25(2), 157-161.doi:
https://doi.org/10.1016/j.colegn.2017.05.002.
Myers, J., McAuley, P., Lavie, C. J., Despres, J. P., Arena, R., & Kokkinos, P. (2015).
Physical activity and cardiorespiratory fitness as major markers of cardiovascular risk: their
independent and interwoven importance to health status. Progress in cardiovascular
diseases, 57(4), 306-314.doi: https://doi.org/10.1016/j.pcad.2014.09.011.
National Council of State Boards of Nursing. (2016). National guidelines for nursing
delegation. Journal of Nursing Regulation, 7(1), 5-14.doi: https://doi.org/10.1016/S2155-
8256(16)31035-3.
Orser, B. A., David, U., & Cohen, M. R. (2016). Perioperative Medication ErrorsBuilding
Safer Systems. Anesthesiology: The Journal of the American Society of
Anesthesiologists, 124(1), 1-3.doi: 10.1097/ALN.0000000000000905.
Powell, R. E., Doty, A., Casten, R. J., Rovner, B. W., & Rising, K. L. (2016). A qualitative
analysis of interprofessional healthcare team members’ perceptions of patient barriers to
healthcare engagement. BMC health services research, 16(1), 493.doi:
https://doi.org/10.1186/s12913-016-1751-5.
Self, W. H., Williams, D. J., Zhu, Y., Ampofo, K., Pavia, A. T., Chappell, J. D., ... & Erdman,
D. (2015). Respiratory viral detection in children and adults: comparing asymptomatic
controls and patients with community-acquired pneumonia. The Journal of infectious
diseases, 213(4), 584-591.doi: https://doi.org/10.1093/infdis/jiv323.
Ganz, F. D., Wagner, N., &Toren, O. (2015). Nurse middle manager ethical dilemmas and
moral distress. Nursing ethics, 22(1), 43-51.doi:
https://doi.org/10.1177%2F0969733013515490.
Gul, M., Ak, M. F., &Guneri, A. F. (2017). Occupational health and safety risk assessment in
hospitals: A case study using two-stage fuzzy multi-criteria approach. Human and Ecological
Risk Assessment: An International Journal, 23(2), 187-202.doi:
https://doi.org/10.1080/10807039.2016.1234363.
Legemaat, M., Carr, P. J., van Rens, R. M., van Dijk, M., Poslawsky, I. E., & van den
Hoogen, A. (2016). Peripheral intravenous cannulation: complication rates in the neonatal
population: a multicenter observational study. The journal of vascular access, 17(4), 360-
365.doi: https://doi.org/10.5301%2Fjva.5000558.
MacSorley, R., White, J., Conerly, V. H., Walker, J. T., Lofton, S., Ragland, G., ...&
Robertson, A. (2014). Pain assessment and management strategies for elderly
patients. Home Healthcare Now, 32(5), 272-285.doi: 10.1097/NHH.0000000000000065.
Manning, V., Jones, A., Jones, P., & Fernandez, R. S. (2015). Planning for a smooth
transition: evaluation of a succession planning program for prospective nurse unit
managers. Nursing administration quarterly, 39(1), 58-68.doi:
10.1097/NAQ.0000000000000072.
Meyer, A. N., Singh, H., & Graber, M. L. (2015). Evaluation of outcomes from a national
patient-initiated second-opinion program. The American journal of medicine, 128(10), 1138-
e25.doi: https://doi.org/10.1016/j.amjmed.2015.04.020.
Missen, K., Porter, J. E., Raymond, A., de Vent, K., & Larkins, J. A. (2018). Adult
Deterioration Detection System (ADDS): An evaluation of the impact on MET and Code blue
activations in a regional healthcare service. Collegian, 25(2), 157-161.doi:
https://doi.org/10.1016/j.colegn.2017.05.002.
Myers, J., McAuley, P., Lavie, C. J., Despres, J. P., Arena, R., & Kokkinos, P. (2015).
Physical activity and cardiorespiratory fitness as major markers of cardiovascular risk: their
independent and interwoven importance to health status. Progress in cardiovascular
diseases, 57(4), 306-314.doi: https://doi.org/10.1016/j.pcad.2014.09.011.
National Council of State Boards of Nursing. (2016). National guidelines for nursing
delegation. Journal of Nursing Regulation, 7(1), 5-14.doi: https://doi.org/10.1016/S2155-
8256(16)31035-3.
Orser, B. A., David, U., & Cohen, M. R. (2016). Perioperative Medication ErrorsBuilding
Safer Systems. Anesthesiology: The Journal of the American Society of
Anesthesiologists, 124(1), 1-3.doi: 10.1097/ALN.0000000000000905.
Powell, R. E., Doty, A., Casten, R. J., Rovner, B. W., & Rising, K. L. (2016). A qualitative
analysis of interprofessional healthcare team members’ perceptions of patient barriers to
healthcare engagement. BMC health services research, 16(1), 493.doi:
https://doi.org/10.1186/s12913-016-1751-5.
Self, W. H., Williams, D. J., Zhu, Y., Ampofo, K., Pavia, A. T., Chappell, J. D., ... & Erdman,
D. (2015). Respiratory viral detection in children and adults: comparing asymptomatic
controls and patients with community-acquired pneumonia. The Journal of infectious
diseases, 213(4), 584-591.doi: https://doi.org/10.1093/infdis/jiv323.
NRSG355 2018 |
Shoham, D. A., Harris, J. K., Mundt, M., &McGaghie, W. (2016). A network model of
communication in an interprofessional team of healthcare professionals: A cross-sectional
study of a burn unit. Journal of interprofessional care, 30(5), 661-667.doi:
https://doi.org/10.1080/13561820.2016.1203296.
Siegel, E. O., Bettega, K., Bakerjian, D., & Sikma, S. (2018). Leadership in Nursing Homes:
Directors of Nursing Aligning Practice With Regulations. Journal of gerontological
nursing, 44(6), 10-14.doi: https://doi.org/10.3928/00989134-20180322-03.
Slatyer, S., Coventry, L. L., Twigg, D., & Davis, S. (2016). Professional practice models for
nursing: a review of the literature and synthesis of key components. Journal of nursing
management, 24(2), 139-150. doi: https://doi.org/10.1111/jonm.12309.
Slayton, R. B., Toth, D., Lee, B. Y., Tanner, W., Bartsch, S. M., Khader, K., ...& Miller, L. G.
(2015). Vital signs: estimated effects of a coordinated approach for action to reduce
antibiotic-resistant infections in health care facilities—United States. MMWR. Morbidity and
mortality weekly report, 64(30), 826. Retrieved from:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4654955/pdf/826-831.pdf.
Tang, K. L., Pilote, L., Behlouli, H., Godley, J., &Ghali, W. A. (2018). An exploration of the
subjective social status construct in patients with acute coronary syndrome. BMC
cardiovascular disorders, 18(1), 22.doi: https://doi.org/10.1186/s12872-018-0759-7.
Teasdale, G., Maas, A., Lecky, F., Manley, G., Stocchetti, N., & Murray, G. (2014). The
Glasgow Coma Scale at 40 years: standing the test of time. The Lancet Neurology, 13(8),
844-854.doi: https://doi.org/10.1016/S1474-4422(14)70120-6.
Truog, R. D., Brown, S. D., Browning, D., Hundert, E. M., Rider, E. A., Bell, S. K., & Meyer,
E. C. (2015). Microethics: the ethics of everyday clinical practice. Hastings Center
Report, 45(1), 11-17.doi: https://doi.org/10.1002/hast.413.
Valentine, M. A., Nembhard, I. M., & Edmondson, A. C. (2015). Measuring teamwork in
health care settings: a review of survey instruments. Medical care, 53(4), e16-e30.doi:
10.1097/MLR.0b013e31827feef6.
Shoham, D. A., Harris, J. K., Mundt, M., &McGaghie, W. (2016). A network model of
communication in an interprofessional team of healthcare professionals: A cross-sectional
study of a burn unit. Journal of interprofessional care, 30(5), 661-667.doi:
https://doi.org/10.1080/13561820.2016.1203296.
Siegel, E. O., Bettega, K., Bakerjian, D., & Sikma, S. (2018). Leadership in Nursing Homes:
Directors of Nursing Aligning Practice With Regulations. Journal of gerontological
nursing, 44(6), 10-14.doi: https://doi.org/10.3928/00989134-20180322-03.
Slatyer, S., Coventry, L. L., Twigg, D., & Davis, S. (2016). Professional practice models for
nursing: a review of the literature and synthesis of key components. Journal of nursing
management, 24(2), 139-150. doi: https://doi.org/10.1111/jonm.12309.
Slayton, R. B., Toth, D., Lee, B. Y., Tanner, W., Bartsch, S. M., Khader, K., ...& Miller, L. G.
(2015). Vital signs: estimated effects of a coordinated approach for action to reduce
antibiotic-resistant infections in health care facilities—United States. MMWR. Morbidity and
mortality weekly report, 64(30), 826. Retrieved from:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4654955/pdf/826-831.pdf.
Tang, K. L., Pilote, L., Behlouli, H., Godley, J., &Ghali, W. A. (2018). An exploration of the
subjective social status construct in patients with acute coronary syndrome. BMC
cardiovascular disorders, 18(1), 22.doi: https://doi.org/10.1186/s12872-018-0759-7.
Teasdale, G., Maas, A., Lecky, F., Manley, G., Stocchetti, N., & Murray, G. (2014). The
Glasgow Coma Scale at 40 years: standing the test of time. The Lancet Neurology, 13(8),
844-854.doi: https://doi.org/10.1016/S1474-4422(14)70120-6.
Truog, R. D., Brown, S. D., Browning, D., Hundert, E. M., Rider, E. A., Bell, S. K., & Meyer,
E. C. (2015). Microethics: the ethics of everyday clinical practice. Hastings Center
Report, 45(1), 11-17.doi: https://doi.org/10.1002/hast.413.
Valentine, M. A., Nembhard, I. M., & Edmondson, A. C. (2015). Measuring teamwork in
health care settings: a review of survey instruments. Medical care, 53(4), e16-e30.doi:
10.1097/MLR.0b013e31827feef6.
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





