Impact of Language and Interpreters on Therapy Alliance Study
VerifiedAdded on 2022/10/15
|11
|11921
|401
Report
AI Summary
This research article, "Effects of Language Concordance and Interpreter Use on Therapeutic Alliance in Spanish-Speaking Integrated Behavioral Health Care Patients" by Villalobos et al. (2016), investigates the impact of interpreter use and language concordance on the therapeutic alliance in a sample of 458 Spanish-speaking patients. The study employs a mixed-methods approach, combining quantitative data from a therapeutic alliance scale with qualitative interviews of patients, behavioral health consultants, and interpreters. Quantitative findings revealed no significant relationship between interpreter use and therapeutic alliance. However, qualitative data highlighted patient preferences for bilingual providers, emphasizing trust, privacy, and ease of communication. While interpreters were seen as valuable for access to services, the study underscores the importance of interpreter training and collaboration to minimize potential negative impacts on care quality. The study contributes to the understanding of language barriers in mental health and the role of interpreters in bridging this gap.

Effects of Language Concordance and Interpreter Use on Therapeutic
Alliance in Spanish-Speaking Integrated Behavioral Health Care Patients
Bianca T. Villalobos, Ana J. Bridges, Elizabeth A. Anastasia, Carlos A. Ojeda,
Juventino Hernandez Rodriguez, and Debbie Gomez
University of Arkansas
The discrepancy between the growing number of Spanish speakers in the U.S. and the availability of
bilingual providers creates a barrier to accessing quality mental health care. Use of interpreters provides
one strategy for overcoming this linguistic barrier; however, concerns about whether sessions with
interpreters, versus bilingual providers, impede therapeutic alliance remain. The current study explored
associations between the use of interpreters and therapeutic alliance in a sample of 458 Spanish-speaking
patients seen for integrated behavioral health visits at primary care clinics. Patients completed a brief (4
item) therapeutic alliance scale at their behavioral health appointment. In addition, to supplement the
quantitative study data, a pilot study of 30 qualitative interviews was conducted with a new sample of
10 Spanish-speaking patients, 10 behavioral health consultants (BHCs), and 10 trained interpreters.
Quantitative results showed that interpreter use did not relate to therapeutic alliance, even when
controlling for relevant demographic variables. However, qualitative interviews suggested major themes
regarding the relative benefits and challenges of using interpreters for patients, interpreters, and BHCs.
In interviews, patients expressed a strong preference for bilingual providers. Benefits included greater
privacy, sense of trust, and accuracy of communication. However, in their absence, interpreters were seen
as increasing access to services and facilitating communication with providers, thereby addressing the
behavioral health needs of patients with limited English proficiency. BHCs and interpreters emphasized
the importance of interpreter training and a good collaborative relationship with interpreters to minimize
negative effects on the quality of care.
Keywords: integrated behavioral health care, interpreters, language concordance, limited English
proficiency, therapeutic alliance
Recently, one of the authors had a behavioral health session
with a primary care patient. The patient, a 49-year-old Hispanic
woman from Chile, had been previously seen by another be-
havioral health consultant (BHC) in the clinic. Because the
patient was fairly fluent in English, she and the previous BHC,
a monolingual English speaker, were able to communicate
without the use of an interpreter. However, when she learned
that her new BHC, a bilingual male from Mexico, spoke Span-
ish, she stated effusively how excited she was that she could use
her native language for her sessions. She stated that talking in
Spanish with her BHC was like being “en casa” [at home] and
that she could express herself more freely. Although the patient
praised her prior BHC, she noted readily that “we need more
bilingual providers” and that she could “connect” more easily
with someone who spoke her own language. In this two-part
study, we explore further language concordance between BHCs
and Spanish speaking patients.
As of 2010, the Hispanic population constituted one of the
largest ethnic minority groups in the U.S. (Ennis, Rios-Vargas, &
Albert, 2011). Spanish is the second most spoken language in the
U.S. (Shin & Kominski, 2010). This growth places an increasing
demand for language-responsive mental health services. Indeed,
language incompatibility is a structural barrier to accessing mental
health treatment for many Spanish-speaking people (Bridges, An-
drews, & Deen, 2012). Nationwide, there is a shortage of bilingual,
trained mental health providers (Annapolis Coalition on the Be-
havioral Health Workforce, 2007). Although precise figures are
not available, a search on the American Psychological Associa-
tion’s “Find a Psychologist” link revealed 6,083 therapists with a
specialization in depression but only 226 therapists nationwide
could work with primarily Spanish-speaking patients needing
treatment for depression (or 3.7% of the original 6,083 therapists;
American Psychological Association, 2015).
This article was published Online First September 7, 2015.
Bianca T. Villalobos, Ana J. Bridges, Elizabeth A. Anastasia, Carlos A.
Ojeda, Juventino Hernandez Rodriguez, and Debbie Gomez, Department
of Psychological Science, University of Arkansas.
Bridges would like to disclose that she receives fees for consultation and
supervision from Community Clinic. This project was supported by grant
D40HP19640 (PI: Ana J. Bridges) from the U.S. Department of Health and
Human Services/Health Resources and Services Administration (USD-
HHS/HRSA). The authors are grateful to Arthur Andrews, Joel Berroa,
Liviu Bunaciu, Blanca Estrada, Alexis Garza, Kelly Grey, Samantha Gre-
gus, Megan Group, Araceli Mancia, Rosemary Palacios, Freddie Pastrana,
Edwin Perez, Rosie Rueda, Stacey Santos, and Edna Trejo for their
assistance with this project. The authors also thank Kathy Grisham and
Kim Shuler of Community Clinic at St. Francis House for partnering with
us in the provision and evaluation of integrated care services.
Correspondence concerning this article should be addressed to Ana J.
Bridges, Department of Psychological Science, University of Arkansas,
216 Memorial Hall, Fayetteville, AR 72701. E-mail: abridges@uark.edu
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
Psychological Services © 2015 American Psychological Association
2016, Vol. 13, No. 1, 49 –59 1541-1559/16/$12.00 http://dx.doi.org/10.1037/ser0000051
49
Alliance in Spanish-Speaking Integrated Behavioral Health Care Patients
Bianca T. Villalobos, Ana J. Bridges, Elizabeth A. Anastasia, Carlos A. Ojeda,
Juventino Hernandez Rodriguez, and Debbie Gomez
University of Arkansas
The discrepancy between the growing number of Spanish speakers in the U.S. and the availability of
bilingual providers creates a barrier to accessing quality mental health care. Use of interpreters provides
one strategy for overcoming this linguistic barrier; however, concerns about whether sessions with
interpreters, versus bilingual providers, impede therapeutic alliance remain. The current study explored
associations between the use of interpreters and therapeutic alliance in a sample of 458 Spanish-speaking
patients seen for integrated behavioral health visits at primary care clinics. Patients completed a brief (4
item) therapeutic alliance scale at their behavioral health appointment. In addition, to supplement the
quantitative study data, a pilot study of 30 qualitative interviews was conducted with a new sample of
10 Spanish-speaking patients, 10 behavioral health consultants (BHCs), and 10 trained interpreters.
Quantitative results showed that interpreter use did not relate to therapeutic alliance, even when
controlling for relevant demographic variables. However, qualitative interviews suggested major themes
regarding the relative benefits and challenges of using interpreters for patients, interpreters, and BHCs.
In interviews, patients expressed a strong preference for bilingual providers. Benefits included greater
privacy, sense of trust, and accuracy of communication. However, in their absence, interpreters were seen
as increasing access to services and facilitating communication with providers, thereby addressing the
behavioral health needs of patients with limited English proficiency. BHCs and interpreters emphasized
the importance of interpreter training and a good collaborative relationship with interpreters to minimize
negative effects on the quality of care.
Keywords: integrated behavioral health care, interpreters, language concordance, limited English
proficiency, therapeutic alliance
Recently, one of the authors had a behavioral health session
with a primary care patient. The patient, a 49-year-old Hispanic
woman from Chile, had been previously seen by another be-
havioral health consultant (BHC) in the clinic. Because the
patient was fairly fluent in English, she and the previous BHC,
a monolingual English speaker, were able to communicate
without the use of an interpreter. However, when she learned
that her new BHC, a bilingual male from Mexico, spoke Span-
ish, she stated effusively how excited she was that she could use
her native language for her sessions. She stated that talking in
Spanish with her BHC was like being “en casa” [at home] and
that she could express herself more freely. Although the patient
praised her prior BHC, she noted readily that “we need more
bilingual providers” and that she could “connect” more easily
with someone who spoke her own language. In this two-part
study, we explore further language concordance between BHCs
and Spanish speaking patients.
As of 2010, the Hispanic population constituted one of the
largest ethnic minority groups in the U.S. (Ennis, Rios-Vargas, &
Albert, 2011). Spanish is the second most spoken language in the
U.S. (Shin & Kominski, 2010). This growth places an increasing
demand for language-responsive mental health services. Indeed,
language incompatibility is a structural barrier to accessing mental
health treatment for many Spanish-speaking people (Bridges, An-
drews, & Deen, 2012). Nationwide, there is a shortage of bilingual,
trained mental health providers (Annapolis Coalition on the Be-
havioral Health Workforce, 2007). Although precise figures are
not available, a search on the American Psychological Associa-
tion’s “Find a Psychologist” link revealed 6,083 therapists with a
specialization in depression but only 226 therapists nationwide
could work with primarily Spanish-speaking patients needing
treatment for depression (or 3.7% of the original 6,083 therapists;
American Psychological Association, 2015).
This article was published Online First September 7, 2015.
Bianca T. Villalobos, Ana J. Bridges, Elizabeth A. Anastasia, Carlos A.
Ojeda, Juventino Hernandez Rodriguez, and Debbie Gomez, Department
of Psychological Science, University of Arkansas.
Bridges would like to disclose that she receives fees for consultation and
supervision from Community Clinic. This project was supported by grant
D40HP19640 (PI: Ana J. Bridges) from the U.S. Department of Health and
Human Services/Health Resources and Services Administration (USD-
HHS/HRSA). The authors are grateful to Arthur Andrews, Joel Berroa,
Liviu Bunaciu, Blanca Estrada, Alexis Garza, Kelly Grey, Samantha Gre-
gus, Megan Group, Araceli Mancia, Rosemary Palacios, Freddie Pastrana,
Edwin Perez, Rosie Rueda, Stacey Santos, and Edna Trejo for their
assistance with this project. The authors also thank Kathy Grisham and
Kim Shuler of Community Clinic at St. Francis House for partnering with
us in the provision and evaluation of integrated care services.
Correspondence concerning this article should be addressed to Ana J.
Bridges, Department of Psychological Science, University of Arkansas,
216 Memorial Hall, Fayetteville, AR 72701. E-mail: abridges@uark.edu
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
Psychological Services © 2015 American Psychological Association
2016, Vol. 13, No. 1, 49 –59 1541-1559/16/$12.00 http://dx.doi.org/10.1037/ser0000051
49
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Trained interpreters can help bridge the gap between patients’
need for Spanish-speaking services and provider availability; how-
ever, the scientific literature provides conflicting reports regarding
the value of interpreters. Positive reports note interpreters may
help patients feel understood by their therapists (Kline, Acosta,
Austin, & Johnson, 1980). Patients have indeed reported the pres-
ence of interpreters and other staff members who speak their
language is an important component of their health care (Alvarez,
Marroquin, Sandoval, & Carlson, 2014).
On the other hand, negative reports of interpreter use reveal
numerous concerns. One issue involves choosing the best inter-
preting model. The U.S. recognizes four models of interpreting
with varying perspectives about the roles of interpreters in the
provider-patient relationship (e.g., as strictly invisible messengers;
as responsible for the accuracy of information; as cultural-
linguistic ambassadors; and as cultural brokers and advocates;
Beltran Avery, 2001). Another concern is interpreter training.
Currently, there is no national or legal certification for interpreting.
Instead, major advocacy groups have developed standards of prac-
tice and ethical codes of conduct for the development of profes-
sional interpreters (for a list of advocacy groups, see Dysart-Gale,
2007). Based on terms defined by the National Council on Inter-
preting in Health Care (2001), trained interpreters are those indi-
viduals who are qualified to interpret through appropriate training
and experience and who demonstrate high proficiency in at least
two languages. Untrained interpreters, or ad hoc interpreters, are
family members, bilingual staff, or volunteers with limited to no
training in interpreting. Most research on interpreters in mental
health care, reviewed below, focuses on the issue of trained versus
untrained interpreters. Finally, potential problems may arise be-
tween the interpreter and clinician. For example, the clinician may
feel uncomfortable with or lack trust in the interpreter (Raval &
Smith, 2003).
Use of Interpreters in Primary Care and Traditional
Mental Health Settings
The primary care setting is often the entry point of an individual
patient into the health care delivery system. Primary care visits are
typically aimed at alleviating acute symptoms, managing chronic
conditions, and providing preventative care. Primary care teams
typically consist of a number of individuals who work collabora-
tively to coordinate patient care, including medical assistants,
nurses, physician assistants, general physicians, medical interpret-
ers, and, increasingly, psychologists and other behavioral health
specialists.
Given their benefit in the primary care setting (Karliner, Jacobs,
Chen, & Mutha, 2007), medical interpreters are essential members
of the health care team. On the whole, studies in the medical field
suggest visits facilitated by trained interpreters are just as satisfac-
tory as visits with bilingual providers, and both are better than
using untrained interpreters (Lee, Batal, Maselli, & Kutner, 2002;
Moreno & Morales, 2010; Ngo-Metzger et al., 2007). Studies also
suggest diagnostic conclusions are similar when physicians and
patients are language concordant or discordant (e.g., Dodd, 1984;
Farooq, Fear, & Oyebode, 1997).
When examining psychotherapeutic, versus medical, outcomes,
studies again suggest the use of trained interpreters results in
similar benefits to clients as what is obtained by seeing a bilingual
therapist. Numerous examples of the benefits of trained interpret-
ers for clients with posttraumatic stress disorder (PTSD) have been
reported (e.g., Brune, Eiroá-Orosa, Fischer-Ortman, Delijaj, &
Haasen, 2011; Schulz, Resick, Huber, & Griffin, 2006). On the
other hand, interpreter use may impact assessment and diagnosis.
Price and Cuellar (1981) found bilingual Mexican American pa-
tients diagnosed with schizophrenia were more likely to disclose
psychopathology symptomatology when interviewed in Spanish
than English, but Marcos, Alpert, Urcuyo, and Kesselman (1973)
found bilingual patients with schizophrenia disclosed more psy-
chopathology in English than Spanish interviews.
Several researchers discuss possible detriments to interpreter
use in therapy, primarily in terms of perceived threats to therapeu-
tic alliance (Bolton, 2002; Tribe & Tunariu, 2009). Therapeutic
alliance is the degree of involvement between the client and
therapist, as evidenced by their mutual collaboration on treatment
processes and personal rapport (Orlinsky, Ronnestad, & Willutzki,
2004). Developing treatment alliance with clients who prefer to
receive clinical services in Spanish presents unique challenges. For
instance, it is possible that a Spanish-speaking client may feel
unsatisfied with a language-matched clinician who does not un-
derstand particular linguistic expressions or culturally bound be-
haviors that are specific to a region.
Very few studies have explored therapist, interpreter, and/or
client perspectives on how interpreters relate to therapeutic alli-
ance in traditional care. Kline and colleagues (1980) found twice
as many clients who used interpreters in session reported being
pleased with the services provided by mental health providers in
comparison with clients who did not use interpreters. Raval and
Smith (2003) conducted semistructured interviews with nine men-
tal health professionals regarding their experiences providing men-
tal health services to children and adolescents with the assistance
of an interpreter. Therapists expressed concern that interpreters
tend to filter out emotional content provided by clients, hampering
the therapist’s ability to share in the intensity of the client’s
experience and develop a therapeutic bond with the client. Addi-
tionally, mental health professionals perceived that techniques
intended to foster rapport with clients, such as reflective listening,
were less effective when mediated through an interpreter. Some
participants discussed experiences in which interpreters’ responses
to information shared by clients delayed the development of ther-
apeutic alliance or even damaged existing rapport (for instance, by
having an interpreter laugh at the disclosure of a client’s sexual
dysfunction). Mental health professionals also indicated challenges
related to forming a working alliance with the interpreter. Profes-
sionals reported doubting that interpreters were accurately com-
municating their statements to clients and feeling disempowered
when providing therapy with the assistance of an interpreter.
Miller, Martell, Pazdirek, Caruth, and Lopez (2005) conducted
semistructured interviews with 15 therapists and 15 interpreters in
the U.S. The authors did not specify whether interpreters had
formal training. Most therapists and interpreters ascribed value to
the alliance an interpreter forms with both therapist and client.
Most therapists reported interpreter use during sessions prolonged
the process of developing rapport with the client. Some therapists
indicated clients developed rapport more rapidly with the inter-
preter than with the therapist; a few therapists felt excluded or
competitive with the interpreter in obtaining therapeutic alliance
with the client. Several therapists reported experiences of inter-
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
50 VILLALOBOS ET AL.
need for Spanish-speaking services and provider availability; how-
ever, the scientific literature provides conflicting reports regarding
the value of interpreters. Positive reports note interpreters may
help patients feel understood by their therapists (Kline, Acosta,
Austin, & Johnson, 1980). Patients have indeed reported the pres-
ence of interpreters and other staff members who speak their
language is an important component of their health care (Alvarez,
Marroquin, Sandoval, & Carlson, 2014).
On the other hand, negative reports of interpreter use reveal
numerous concerns. One issue involves choosing the best inter-
preting model. The U.S. recognizes four models of interpreting
with varying perspectives about the roles of interpreters in the
provider-patient relationship (e.g., as strictly invisible messengers;
as responsible for the accuracy of information; as cultural-
linguistic ambassadors; and as cultural brokers and advocates;
Beltran Avery, 2001). Another concern is interpreter training.
Currently, there is no national or legal certification for interpreting.
Instead, major advocacy groups have developed standards of prac-
tice and ethical codes of conduct for the development of profes-
sional interpreters (for a list of advocacy groups, see Dysart-Gale,
2007). Based on terms defined by the National Council on Inter-
preting in Health Care (2001), trained interpreters are those indi-
viduals who are qualified to interpret through appropriate training
and experience and who demonstrate high proficiency in at least
two languages. Untrained interpreters, or ad hoc interpreters, are
family members, bilingual staff, or volunteers with limited to no
training in interpreting. Most research on interpreters in mental
health care, reviewed below, focuses on the issue of trained versus
untrained interpreters. Finally, potential problems may arise be-
tween the interpreter and clinician. For example, the clinician may
feel uncomfortable with or lack trust in the interpreter (Raval &
Smith, 2003).
Use of Interpreters in Primary Care and Traditional
Mental Health Settings
The primary care setting is often the entry point of an individual
patient into the health care delivery system. Primary care visits are
typically aimed at alleviating acute symptoms, managing chronic
conditions, and providing preventative care. Primary care teams
typically consist of a number of individuals who work collabora-
tively to coordinate patient care, including medical assistants,
nurses, physician assistants, general physicians, medical interpret-
ers, and, increasingly, psychologists and other behavioral health
specialists.
Given their benefit in the primary care setting (Karliner, Jacobs,
Chen, & Mutha, 2007), medical interpreters are essential members
of the health care team. On the whole, studies in the medical field
suggest visits facilitated by trained interpreters are just as satisfac-
tory as visits with bilingual providers, and both are better than
using untrained interpreters (Lee, Batal, Maselli, & Kutner, 2002;
Moreno & Morales, 2010; Ngo-Metzger et al., 2007). Studies also
suggest diagnostic conclusions are similar when physicians and
patients are language concordant or discordant (e.g., Dodd, 1984;
Farooq, Fear, & Oyebode, 1997).
When examining psychotherapeutic, versus medical, outcomes,
studies again suggest the use of trained interpreters results in
similar benefits to clients as what is obtained by seeing a bilingual
therapist. Numerous examples of the benefits of trained interpret-
ers for clients with posttraumatic stress disorder (PTSD) have been
reported (e.g., Brune, Eiroá-Orosa, Fischer-Ortman, Delijaj, &
Haasen, 2011; Schulz, Resick, Huber, & Griffin, 2006). On the
other hand, interpreter use may impact assessment and diagnosis.
Price and Cuellar (1981) found bilingual Mexican American pa-
tients diagnosed with schizophrenia were more likely to disclose
psychopathology symptomatology when interviewed in Spanish
than English, but Marcos, Alpert, Urcuyo, and Kesselman (1973)
found bilingual patients with schizophrenia disclosed more psy-
chopathology in English than Spanish interviews.
Several researchers discuss possible detriments to interpreter
use in therapy, primarily in terms of perceived threats to therapeu-
tic alliance (Bolton, 2002; Tribe & Tunariu, 2009). Therapeutic
alliance is the degree of involvement between the client and
therapist, as evidenced by their mutual collaboration on treatment
processes and personal rapport (Orlinsky, Ronnestad, & Willutzki,
2004). Developing treatment alliance with clients who prefer to
receive clinical services in Spanish presents unique challenges. For
instance, it is possible that a Spanish-speaking client may feel
unsatisfied with a language-matched clinician who does not un-
derstand particular linguistic expressions or culturally bound be-
haviors that are specific to a region.
Very few studies have explored therapist, interpreter, and/or
client perspectives on how interpreters relate to therapeutic alli-
ance in traditional care. Kline and colleagues (1980) found twice
as many clients who used interpreters in session reported being
pleased with the services provided by mental health providers in
comparison with clients who did not use interpreters. Raval and
Smith (2003) conducted semistructured interviews with nine men-
tal health professionals regarding their experiences providing men-
tal health services to children and adolescents with the assistance
of an interpreter. Therapists expressed concern that interpreters
tend to filter out emotional content provided by clients, hampering
the therapist’s ability to share in the intensity of the client’s
experience and develop a therapeutic bond with the client. Addi-
tionally, mental health professionals perceived that techniques
intended to foster rapport with clients, such as reflective listening,
were less effective when mediated through an interpreter. Some
participants discussed experiences in which interpreters’ responses
to information shared by clients delayed the development of ther-
apeutic alliance or even damaged existing rapport (for instance, by
having an interpreter laugh at the disclosure of a client’s sexual
dysfunction). Mental health professionals also indicated challenges
related to forming a working alliance with the interpreter. Profes-
sionals reported doubting that interpreters were accurately com-
municating their statements to clients and feeling disempowered
when providing therapy with the assistance of an interpreter.
Miller, Martell, Pazdirek, Caruth, and Lopez (2005) conducted
semistructured interviews with 15 therapists and 15 interpreters in
the U.S. The authors did not specify whether interpreters had
formal training. Most therapists and interpreters ascribed value to
the alliance an interpreter forms with both therapist and client.
Most therapists reported interpreter use during sessions prolonged
the process of developing rapport with the client. Some therapists
indicated clients developed rapport more rapidly with the inter-
preter than with the therapist; a few therapists felt excluded or
competitive with the interpreter in obtaining therapeutic alliance
with the client. Several therapists reported experiences of inter-
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
50 VILLALOBOS ET AL.
preters showing resistance to interpreting certain statements for the
client (e.g., too upsetting, unnecessary information).
Ebersole (2011) conducted an empirical study to compare de-
velopment of therapeutic alliance with an interpreter or a language
concordant mental health practitioner. Social workers conducted
psychosocial interviews with parents of children who were being
evaluated for special education services in a public school district.
Results showed parents, social workers, and interpreters reported
strong therapeutic alliance in nearly every case; these findings
were consistent with qualitative information obtained from focus
groups with social workers.
In contrast to traditional therapy settings, integrated care settings
allow primary care patients with behavioral health needs opportu-
nities to be seen by mental health care professionals in the primary
care clinic, oftentimes the same day as a behavioral health need is
identified (Robinson & Reiter, 2007). Sessions with mental health
professionals who are integrated into primary care clinics tend to
be much briefer than sessions conducted in traditional mental
health care settings, both in terms of session duration (typically 15-
to 20-minute sessions) and frequency (oftentimes visits are spaced
2 or more weeks apart, with most patients receiving only 1– 4
sessions; Corso et al., 2012). This model has been shown to be
efficacious at improving the behavioral health of primary care
patients (Bryan, Morrow, & Appolonio, 2009), even in clinics
where the majority of patients are of LEP (Bridges et al., 2014).
To date, no study has examined how therapeutic alliance or
patient outcomes are affected by the use of bilingual interpreters
for primary care patients receiving behavioral health care services.
Although the research on use of interpreters in traditional mental
health care settings is instructive, the significantly compressed
time of behavioral health care visits in primary care makes gen-
eralization from traditional mental health care difficult. In addi-
tion, although research on alliance and patient outcomes in primary
care settings suggests trained interpreters are useful to patients, the
content of medical visits and of behavioral health visits may be
quite different.
Study Aims
The primary purpose of this study, therefore, was to explore
how the use of trained interpreters related to therapeutic alliance in
integrated behavioral health care patients with LEP (in particular,
with a group of Spanish speaking patients). A second purpose of
this study was to contextualize the quantitative data by providing
pilot qualitative data on how patients, behavioral health care pro-
viders, and interpreters viewed behavioral health care services
delivered through interpreters versus language-concordant provid-
ers. We expected these exploratory qualitative data would provide
a richer context for the interpretation of our quantitative analyses.
Method
Participants
Quantitative data collection. Participants were 458 Spanish-
speaking patients seen for behavioral health services at two pri-
mary care clinics, both part of a local federally qualified health
center (FQHC) in northwest Arkansas. This region has experi-
enced significant growth in its Hispanic population over the past
decade (U.S. Census Bureau, 2015). The two primary care clinics
were located in cities with populations of approximately 75,000
and 60,000. The Hispanic population comprises approximately
30% to 35% of all city residents (U.S. Census Bureau, 2015).
Patients of the primary care clinics are more diverse than those of
the cities in which they are situated: more than half of patients are
Hispanic and prefer to speak a language other than English. Most
patients (more than 90%) are of lower socioeconomic status,
earning 200% or less of the Federal Poverty Level (Arkansas
Center for Health Improvement, 2015; see also http://www
.communityclinicnwa.org/). For more details about the clinics and
patients, please refer to Bridges et al. (2014).
Data were taken from consecutive patients seen over a 43-month
period (September 2010 to April 2014) who met inclusionary
criteria. Inclusionary criteria were as follows: (a) adult patient
(age ⬎17 years); (b) never received behavioral health sessions
before; (c) spoke Spanish during the behavioral health session; and
(d) completed self-report questionnaires at the conclusion of ses-
sion that included a measure of therapeutic alliance. A total of
56.6% of sessions were conducted by bilingual BHCs, whereas
43.4% of sessions were conducted with the aid of a professional
interpreter (a medical assistant trained in behavioral health inter-
pretation). Training for interpreters takes place during an in-depth
orientation to clinic services in addition to shadowing experienced
medical assistants during medical and behavioral health visits. The
length of time spent shadowing varies and depends on the medical
assistants’ comfort in their ability to function independently. Cur-
rently, the FQHC designates the use of specific interpreters for
BHCs. These BHC-specific interpreters undergo the same training,
with a special focus on ensuring confidentiality, accuracy to facil-
itate diagnoses and treatment interventions, and establishing the
role of the interpreter as a channel between the patient and clini-
cian.
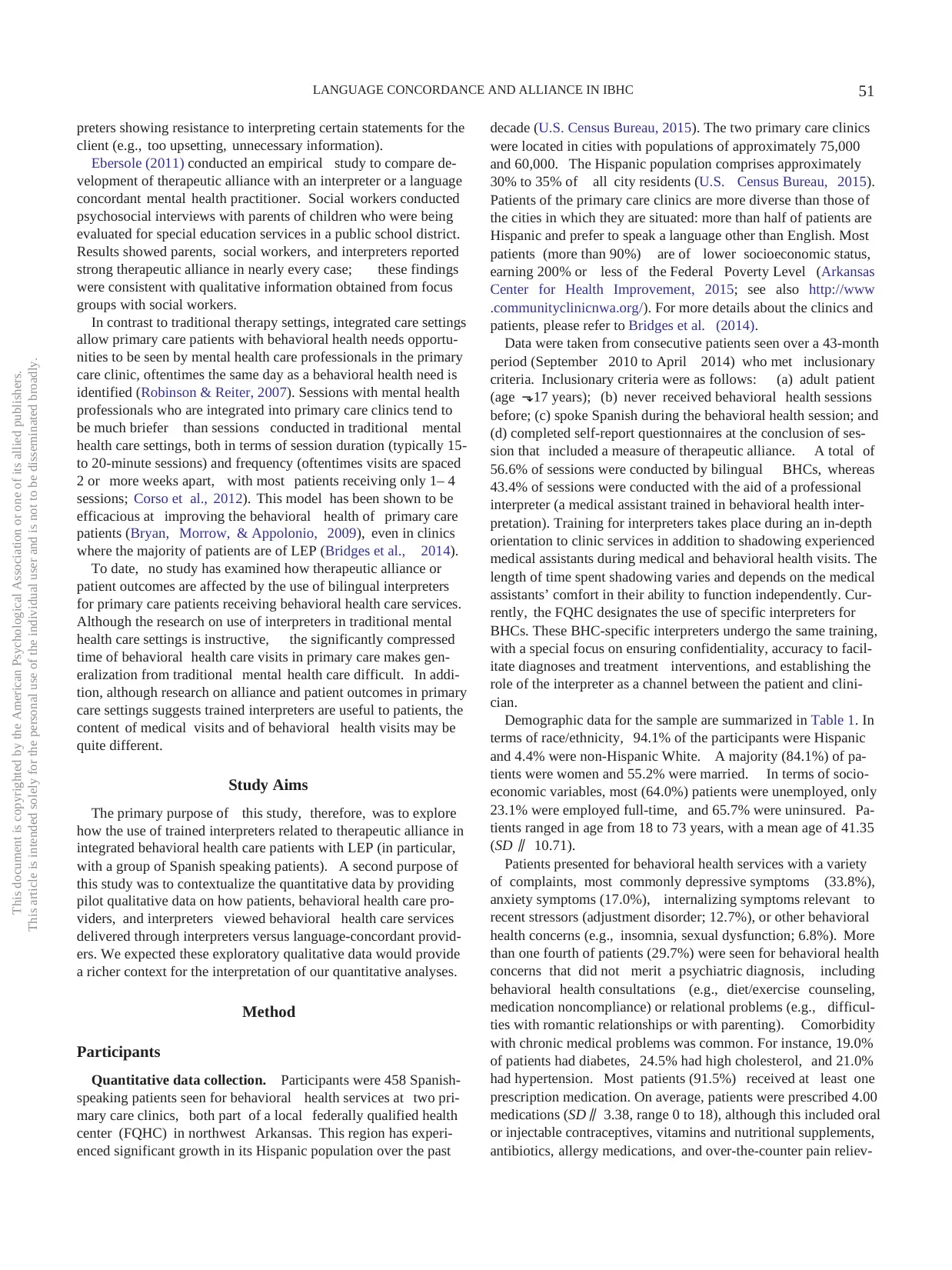
Demographic data for the sample are summarized in Table 1. In
terms of race/ethnicity, 94.1% of the participants were Hispanic
and 4.4% were non-Hispanic White. A majority (84.1%) of pa-
tients were women and 55.2% were married. In terms of socio-
economic variables, most (64.0%) patients were unemployed, only
23.1% were employed full-time, and 65.7% were uninsured. Pa-
tients ranged in age from 18 to 73 years, with a mean age of 41.35
(SD ⫽ 10.71).
Patients presented for behavioral health services with a variety
of complaints, most commonly depressive symptoms (33.8%),
anxiety symptoms (17.0%), internalizing symptoms relevant to
recent stressors (adjustment disorder; 12.7%), or other behavioral
health concerns (e.g., insomnia, sexual dysfunction; 6.8%). More
than one fourth of patients (29.7%) were seen for behavioral health
concerns that did not merit a psychiatric diagnosis, including
behavioral health consultations (e.g., diet/exercise counseling,
medication noncompliance) or relational problems (e.g., difficul-
ties with romantic relationships or with parenting). Comorbidity
with chronic medical problems was common. For instance, 19.0%
of patients had diabetes, 24.5% had high cholesterol, and 21.0%
had hypertension. Most patients (91.5%) received at least one
prescription medication. On average, patients were prescribed 4.00
medications (SD ⫽ 3.38, range 0 to 18), although this included oral
or injectable contraceptives, vitamins and nutritional supplements,
antibiotics, allergy medications, and over-the-counter pain reliev-
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
51LANGUAGE CONCORDANCE AND ALLIANCE IN IBHC
client (e.g., too upsetting, unnecessary information).
Ebersole (2011) conducted an empirical study to compare de-
velopment of therapeutic alliance with an interpreter or a language
concordant mental health practitioner. Social workers conducted
psychosocial interviews with parents of children who were being
evaluated for special education services in a public school district.
Results showed parents, social workers, and interpreters reported
strong therapeutic alliance in nearly every case; these findings
were consistent with qualitative information obtained from focus
groups with social workers.
In contrast to traditional therapy settings, integrated care settings
allow primary care patients with behavioral health needs opportu-
nities to be seen by mental health care professionals in the primary
care clinic, oftentimes the same day as a behavioral health need is
identified (Robinson & Reiter, 2007). Sessions with mental health
professionals who are integrated into primary care clinics tend to
be much briefer than sessions conducted in traditional mental
health care settings, both in terms of session duration (typically 15-
to 20-minute sessions) and frequency (oftentimes visits are spaced
2 or more weeks apart, with most patients receiving only 1– 4
sessions; Corso et al., 2012). This model has been shown to be
efficacious at improving the behavioral health of primary care
patients (Bryan, Morrow, & Appolonio, 2009), even in clinics
where the majority of patients are of LEP (Bridges et al., 2014).
To date, no study has examined how therapeutic alliance or
patient outcomes are affected by the use of bilingual interpreters
for primary care patients receiving behavioral health care services.
Although the research on use of interpreters in traditional mental
health care settings is instructive, the significantly compressed
time of behavioral health care visits in primary care makes gen-
eralization from traditional mental health care difficult. In addi-
tion, although research on alliance and patient outcomes in primary
care settings suggests trained interpreters are useful to patients, the
content of medical visits and of behavioral health visits may be
quite different.
Study Aims
The primary purpose of this study, therefore, was to explore
how the use of trained interpreters related to therapeutic alliance in
integrated behavioral health care patients with LEP (in particular,
with a group of Spanish speaking patients). A second purpose of
this study was to contextualize the quantitative data by providing
pilot qualitative data on how patients, behavioral health care pro-
viders, and interpreters viewed behavioral health care services
delivered through interpreters versus language-concordant provid-
ers. We expected these exploratory qualitative data would provide
a richer context for the interpretation of our quantitative analyses.
Method
Participants
Quantitative data collection. Participants were 458 Spanish-
speaking patients seen for behavioral health services at two pri-
mary care clinics, both part of a local federally qualified health
center (FQHC) in northwest Arkansas. This region has experi-
enced significant growth in its Hispanic population over the past
decade (U.S. Census Bureau, 2015). The two primary care clinics
were located in cities with populations of approximately 75,000
and 60,000. The Hispanic population comprises approximately
30% to 35% of all city residents (U.S. Census Bureau, 2015).
Patients of the primary care clinics are more diverse than those of
the cities in which they are situated: more than half of patients are
Hispanic and prefer to speak a language other than English. Most
patients (more than 90%) are of lower socioeconomic status,
earning 200% or less of the Federal Poverty Level (Arkansas
Center for Health Improvement, 2015; see also http://www
.communityclinicnwa.org/). For more details about the clinics and
patients, please refer to Bridges et al. (2014).
Data were taken from consecutive patients seen over a 43-month
period (September 2010 to April 2014) who met inclusionary
criteria. Inclusionary criteria were as follows: (a) adult patient
(age ⬎17 years); (b) never received behavioral health sessions
before; (c) spoke Spanish during the behavioral health session; and
(d) completed self-report questionnaires at the conclusion of ses-
sion that included a measure of therapeutic alliance. A total of
56.6% of sessions were conducted by bilingual BHCs, whereas
43.4% of sessions were conducted with the aid of a professional
interpreter (a medical assistant trained in behavioral health inter-
pretation). Training for interpreters takes place during an in-depth
orientation to clinic services in addition to shadowing experienced
medical assistants during medical and behavioral health visits. The
length of time spent shadowing varies and depends on the medical
assistants’ comfort in their ability to function independently. Cur-
rently, the FQHC designates the use of specific interpreters for
BHCs. These BHC-specific interpreters undergo the same training,
with a special focus on ensuring confidentiality, accuracy to facil-
itate diagnoses and treatment interventions, and establishing the
role of the interpreter as a channel between the patient and clini-
cian.
Demographic data for the sample are summarized in Table 1. In
terms of race/ethnicity, 94.1% of the participants were Hispanic
and 4.4% were non-Hispanic White. A majority (84.1%) of pa-
tients were women and 55.2% were married. In terms of socio-
economic variables, most (64.0%) patients were unemployed, only
23.1% were employed full-time, and 65.7% were uninsured. Pa-
tients ranged in age from 18 to 73 years, with a mean age of 41.35
(SD ⫽ 10.71).
Patients presented for behavioral health services with a variety
of complaints, most commonly depressive symptoms (33.8%),
anxiety symptoms (17.0%), internalizing symptoms relevant to
recent stressors (adjustment disorder; 12.7%), or other behavioral
health concerns (e.g., insomnia, sexual dysfunction; 6.8%). More
than one fourth of patients (29.7%) were seen for behavioral health
concerns that did not merit a psychiatric diagnosis, including
behavioral health consultations (e.g., diet/exercise counseling,
medication noncompliance) or relational problems (e.g., difficul-
ties with romantic relationships or with parenting). Comorbidity
with chronic medical problems was common. For instance, 19.0%
of patients had diabetes, 24.5% had high cholesterol, and 21.0%
had hypertension. Most patients (91.5%) received at least one
prescription medication. On average, patients were prescribed 4.00
medications (SD ⫽ 3.38, range 0 to 18), although this included oral
or injectable contraceptives, vitamins and nutritional supplements,
antibiotics, allergy medications, and over-the-counter pain reliev-
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
51LANGUAGE CONCORDANCE AND ALLIANCE IN IBHC
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
ers. A total of 27.7% of patients were prescribed a psychotropic
medication.
Qualitative data collection. Following the analyses of our
quantitative data, we opted to conduct an exploratory pilot quali-
tative study that would permit richer context for our quantitative
study. Ten new Spanish-speaking Hispanic patients who had not
participated in the quantitative study (70% female; M age ⫽ 38.30
years, SD ⫽ 6.77, range ⫽ 29 –50), 10 behavioral health care
providers (60% female; 40% Hispanic; M age ⫽ 29.20 years, SD ⫽
5.60, range ⫽ 25– 44), and 10 medical assistants (80% female;
100% Hispanic; M age ⫽ 25.80 years, SD ⫽ 4.61, range ⫽ 22–36)
who had served as trained interpreters in behavioral health ap-
pointments were recruited to provide qualitative information about
their experiences with therapeutic alliance. Of the Spanish-
speaking patients, half (n ⫽ 5) reported on a session in which they
had used an interpreter and half (n ⫽ 5) reported on a session in
which they had seen a bilingual BHC. Of the BHCs, 1 was a native
Spanish speaker, 5 spoke Spanish fluently as a second language,
and 4 used an interpreter when working with Spanish-speaking
patients. BHCs had an average of 5.90 years of general clinical
experience (SD ⫽ 5.62, range ⫽ 2–21) and 1.94 years of experi-
ence in integrated behavioral health care (SD ⫽ 1.66, range ⫽ 5
weeks to 6 years). Of the trained interpreters, all were native
Spanish speakers. Interpreters had an average of 4.42 years work-
ing as interpreters (SD ⫽ 2.57, range ⫽ 8 months to 7 years).
Measures
Demographic data. We culled preexisting information from
patient electronic medical records, including demographic vari-
ables (age, ethnicity, race, marital status, employment status, in-
surance status, and primary language). We also obtained dates of
BHC appointments, global assessment of functioning (GAF)
scores given at each BHC appointment, and medical and psychi-
atric diagnoses from electronic records.
Psychiatric distress. To assess patient symptoms and func-
tional impairment, the A Collaborative Outcomes Resource Net-
work (ACORN) questionnaire was utilized (Brown, 2011). The
18-item ACORN assesses global levels of psychiatric symptoms.
The adult version (for people 18 years or older) asks questions
about mood, anxiety, sleep, alcohol and drug use, and functional
impairment. Items inquire about how often the person has expe-
rienced each of the symptoms in the past two weeks. Responses are
scored on a 5-point Likert scale, from 0 (never) to 4 (very often).
Items are then averaged to form a global score. According to the
ACORN manual, Cronbach’s alpha for the global distress items is
.92 in clinical samples. Concurrent validity was demonstrated with
a significant relation between ACORN global distress scores and
the Beck Depression Inventory (r ⫽ .78).
Therapeutic alliance. In the ACORN, there are four ques-
tions assessing therapeutic alliance, also scored on a 5-point Likert
scale (from 0 ⫽ do not agree to 4 ⫽ agree). Items assess the
relevance of the information discussed during the behavioral
health visit for the patient and the patient’s perceptions of the
working relationship with the behavioral health consultant. These
four items are averaged to form a session alliance score, with
higher scores indicating higher alliance. In the current study,
internal consistency reliability was good, Cronbach’s alpha ⫽ .80.
In qualitative interviews conducted by the study authors,
Spanish-speaking patients, behavioral health care providers, and
medical assistants who had served as interpreters were asked a few
open-ended questions about their perceptions of the influence of
using an interpreter or receiving services from a bilingual behav-
ioral health care provider on therapeutic alliance. Table 2 provides
a list of questions asked of each participant group.
Procedures
A sequential exploratory mixed-methods design was used, such
that after quantitative data were collected and analyzed, qualitative
data were collected to facilitate a more enriched interpretation of
the results (Hanson, Creswell, Clark, Petska, & Creswell, 2005).
The qualitative pilot study, in particular, was designed to enrich
our understanding of the topic by providing an initial exploration
into categories that represent the myriad benefits and challenges of
utilizing interpreters in behavioral health sessions conducted in
primary care settings. All procedures were approved by the exec-
Table 1
Patient Demographic Information
Variable M SD N %
Gender
Male 73 15.9%
Female 385 84.1%
Age, in years 41.35 10.71
Marital status
Single 122 26.6%
Married 253 55.2%
Divorced or separated 30 6.5%
Widowed 7 1.5%
Other 46 10.0%
Employment status
Employed full-time 106 23.1%
Employed part-time 40 8.7%
Unemployed 293 64.0%
Retired 2 .4%
Other 17 3.7%
Race/ethnicity
Hispanic 431 94.1%
Non-Hispanic White 20 4.4%
Insurance coverage
Public insurance 75 16.4%
Private insurance 53 11.6%
Other insurance 29 6.3%
Uninsured 301 65.7%
Chronic health condition
Diabetes 87 19.0%
High cholesterol 112 24.5%
Hypertension 96 21.0%
Mental health condition
Depressive disorder 155 33.8%
Anxiety disorder 78 17.0%
Adjustment disorder 58 12.7%
Other 31 6.8%
Patient is prescribed medication 419 91.5%
Number of prescription medications 4.00 3.38
Patient is prescribed psychotropic
medication 127 27.7%
Prior year clinic encounters 5.40 4.07
ACORN Global Distress 1.98 .84
Interpreter used during behavioral
health session 199 43.4%
ACORN therapeutic alliance 3.87 .32
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
52 VILLALOBOS ET AL.
medication.
Qualitative data collection. Following the analyses of our
quantitative data, we opted to conduct an exploratory pilot quali-
tative study that would permit richer context for our quantitative
study. Ten new Spanish-speaking Hispanic patients who had not
participated in the quantitative study (70% female; M age ⫽ 38.30
years, SD ⫽ 6.77, range ⫽ 29 –50), 10 behavioral health care
providers (60% female; 40% Hispanic; M age ⫽ 29.20 years, SD ⫽
5.60, range ⫽ 25– 44), and 10 medical assistants (80% female;
100% Hispanic; M age ⫽ 25.80 years, SD ⫽ 4.61, range ⫽ 22–36)
who had served as trained interpreters in behavioral health ap-
pointments were recruited to provide qualitative information about
their experiences with therapeutic alliance. Of the Spanish-
speaking patients, half (n ⫽ 5) reported on a session in which they
had used an interpreter and half (n ⫽ 5) reported on a session in
which they had seen a bilingual BHC. Of the BHCs, 1 was a native
Spanish speaker, 5 spoke Spanish fluently as a second language,
and 4 used an interpreter when working with Spanish-speaking
patients. BHCs had an average of 5.90 years of general clinical
experience (SD ⫽ 5.62, range ⫽ 2–21) and 1.94 years of experi-
ence in integrated behavioral health care (SD ⫽ 1.66, range ⫽ 5
weeks to 6 years). Of the trained interpreters, all were native
Spanish speakers. Interpreters had an average of 4.42 years work-
ing as interpreters (SD ⫽ 2.57, range ⫽ 8 months to 7 years).
Measures
Demographic data. We culled preexisting information from
patient electronic medical records, including demographic vari-
ables (age, ethnicity, race, marital status, employment status, in-
surance status, and primary language). We also obtained dates of
BHC appointments, global assessment of functioning (GAF)
scores given at each BHC appointment, and medical and psychi-
atric diagnoses from electronic records.
Psychiatric distress. To assess patient symptoms and func-
tional impairment, the A Collaborative Outcomes Resource Net-
work (ACORN) questionnaire was utilized (Brown, 2011). The
18-item ACORN assesses global levels of psychiatric symptoms.
The adult version (for people 18 years or older) asks questions
about mood, anxiety, sleep, alcohol and drug use, and functional
impairment. Items inquire about how often the person has expe-
rienced each of the symptoms in the past two weeks. Responses are
scored on a 5-point Likert scale, from 0 (never) to 4 (very often).
Items are then averaged to form a global score. According to the
ACORN manual, Cronbach’s alpha for the global distress items is
.92 in clinical samples. Concurrent validity was demonstrated with
a significant relation between ACORN global distress scores and
the Beck Depression Inventory (r ⫽ .78).
Therapeutic alliance. In the ACORN, there are four ques-
tions assessing therapeutic alliance, also scored on a 5-point Likert
scale (from 0 ⫽ do not agree to 4 ⫽ agree). Items assess the
relevance of the information discussed during the behavioral
health visit for the patient and the patient’s perceptions of the
working relationship with the behavioral health consultant. These
four items are averaged to form a session alliance score, with
higher scores indicating higher alliance. In the current study,
internal consistency reliability was good, Cronbach’s alpha ⫽ .80.
In qualitative interviews conducted by the study authors,
Spanish-speaking patients, behavioral health care providers, and
medical assistants who had served as interpreters were asked a few
open-ended questions about their perceptions of the influence of
using an interpreter or receiving services from a bilingual behav-
ioral health care provider on therapeutic alliance. Table 2 provides
a list of questions asked of each participant group.
Procedures
A sequential exploratory mixed-methods design was used, such
that after quantitative data were collected and analyzed, qualitative
data were collected to facilitate a more enriched interpretation of
the results (Hanson, Creswell, Clark, Petska, & Creswell, 2005).
The qualitative pilot study, in particular, was designed to enrich
our understanding of the topic by providing an initial exploration
into categories that represent the myriad benefits and challenges of
utilizing interpreters in behavioral health sessions conducted in
primary care settings. All procedures were approved by the exec-
Table 1
Patient Demographic Information
Variable M SD N %
Gender
Male 73 15.9%
Female 385 84.1%
Age, in years 41.35 10.71
Marital status
Single 122 26.6%
Married 253 55.2%
Divorced or separated 30 6.5%
Widowed 7 1.5%
Other 46 10.0%
Employment status
Employed full-time 106 23.1%
Employed part-time 40 8.7%
Unemployed 293 64.0%
Retired 2 .4%
Other 17 3.7%
Race/ethnicity
Hispanic 431 94.1%
Non-Hispanic White 20 4.4%
Insurance coverage
Public insurance 75 16.4%
Private insurance 53 11.6%
Other insurance 29 6.3%
Uninsured 301 65.7%
Chronic health condition
Diabetes 87 19.0%
High cholesterol 112 24.5%
Hypertension 96 21.0%
Mental health condition
Depressive disorder 155 33.8%
Anxiety disorder 78 17.0%
Adjustment disorder 58 12.7%
Other 31 6.8%
Patient is prescribed medication 419 91.5%
Number of prescription medications 4.00 3.38
Patient is prescribed psychotropic
medication 127 27.7%
Prior year clinic encounters 5.40 4.07
ACORN Global Distress 1.98 .84
Interpreter used during behavioral
health session 199 43.4%
ACORN therapeutic alliance 3.87 .32
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
52 VILLALOBOS ET AL.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

utive director of the FQHC and the university’s Institutional Re-
view Board.
Quantitative data collection. Patients presented to their pri-
mary care provider for a variety of reasons, including annual
physical examinations, infections, pain, diabetes management, and
asthma. During their visit, the primary care provider identified a
behavioral health issue and referred the patient to a behavioral
health consultant for a same-day appointment. Behavioral health
consultants were licensed clinical social workers (n ⫽ 5), a li-
censed psychologist (n ⫽ 1), or psychology doctoral students in
training (n ⫽ 6). At that visit and all subsequent behavioral health
appointments, patients were instructed to complete the ACORN
questionnaire. Patients were seen for an average of 1.53 visits
(SD ⫽ 1.00, range 1– 8). Each visit lasted between 15 and 30
minutes and visits were spaced approximately 2 to 4 weeks apart.
Sessions were problem-focused and generally employed brief
cognitive– behavioral interventions such as behavioral activation,
motivational enhancement, exposure therapy, and psychoeduca-
tion. As part of standard operating procedures, patients of the
FQHC sign a consent form that specifies information in their
medical chart may be used for research purposes. Therefore,
additional consent to access preexisting data from electronic med-
ical records for this part of the study was not requested from
patients.
Qualitative data collection. Qualitative data collection took
place over a 2-month span (mid-September through mid-
November 2014). During times when research assistants were
present at the primary care sites, behavioral health care providers
having sessions with Spanish-speaking patients would request the
patient’s permission to allow a researcher to ask them a few
open-ended questions at the end of their appointment. Patients
were not selected by any other criteria. In addition, during that
span of time researchers arranged in-person or telephone inter-
views with behavioral health care providers and medical assistants.
We interviewed all BHCs who were currently employed by the
clinic (n ⫽ 4) and all BHCs who were or had completed an
externship at the clinic as part of their doctoral training (n ⫽ 6).
We also solicited interviews with medical assistants who were
currently employed by the clinic, frequently provided interpreta-
tion services for BHCs, and could schedule an interview.
All participants provided verbal consent and received a copy of
a consent form describing the purpose of the study, procedures,
and how data would be utilized. Interviews were conducted in
Spanish by bilingual clinical psychology doctoral students and a
licensed psychologist (all study authors). Interviews lasted be-
tween five and 10 minutes each. Interview responses were typed
out verbatim by the interviewer. Qualitative interview responses
were then content analyzed by the researchers for identification of
emerging themes. The process of identifying thematic categories
involved reading through interview transcripts, identifying as a
group the themes reflected in the responses, and then detailing
these themes into a codebook. Because of the exploratory nature of
the study, we avoided collapsing categories and opted instead to
create independent categories for all identified themes. Following
creation of the codebook, the first two authors independently
coded each interview. We assessed intercoder reliability separately
for each sample, using percent agreement (total agreements/total
coding instances). Interrater reliabilities were 97% (patient data),
86% (behavioral health provider data), and 92% (medical assistant
data). Disagreements were resolved via consensus by the two
coders.
Results
Quantitative Results
A one-way between-subjects analysis of variance (ANOVA)
was conducted to determine whether the use of an interpreter in the
behavioral health session (yes/no) was related to patients’ self-
reported therapeutic alliance with the behavioral health consultant.
No significant main effect of interpreter use was found, F(1,
456) ⫽ 1.81, p ⫽ .179. Patients who had an interpreter in the room
(M ⫽ 3.89, SD ⫽ 0.32, N ⫽ 199) had alliance ratings comparable
to those of patients who received services from a bilingual BHC
(M ⫽ 3.85, SD ⫽ 0.32, N ⫽ 259). Even when controlling for
relevant demographic covariates in a multiple regression (see
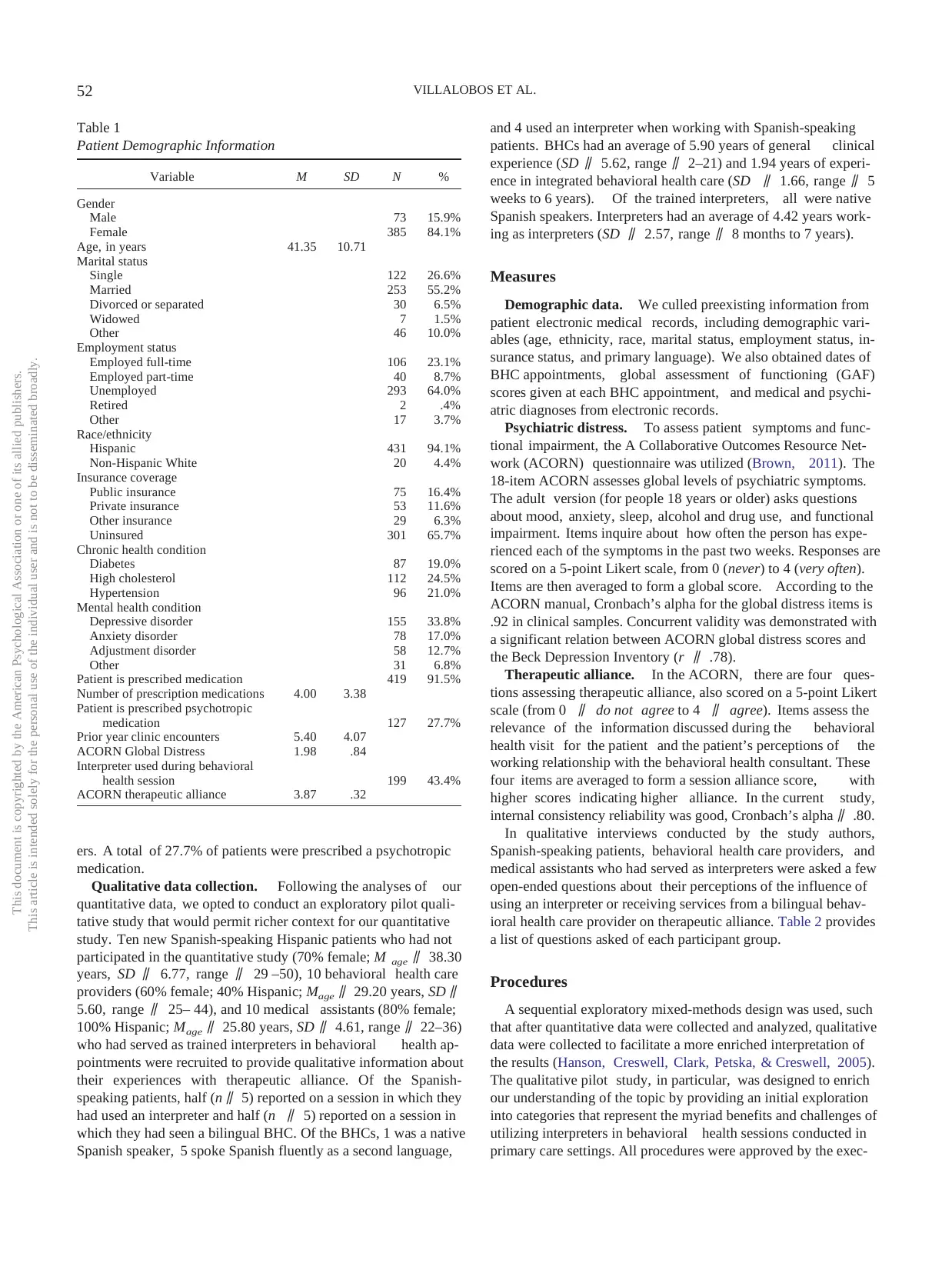
Table 2
Qualitative Interview Questions
Group Questions
Patients 1. How was your visit with [name of BHC]?
2. What did you think of the Spanish speaking abilities of [name of bilingual BHC or name of interpreter]? Was it
easy to understand his/her Spanish?
3. How well do you think [name of bilingual BHC or name of interpreter] understood your Spanish?
4. Do you think you had a good relationship with [name of BHC]?
5. Do you think it made that a difference that [name of BHC] could/could not speak Spanish?
6. Had you used an interpreter before?
7. For sessions with bilingual BHCs: Would it have been preferable to have an interpreter in your visit with [name
of bilingual BHC]? Why or why not?
8. For sessions with interpreters: Would it have been preferable if [name of BHC] spoke Spanish? Why or why not?
9. We want to improve our services for Spanish speaking patients. What could we do to make our services better?
Interpreters 1. What is your experience like providing interpreter services for Spanish speaking patients of the clinic?
2. Are these experiences similar for medical visits and behavioral health visits? If not, what is different?
3. How do you think the quality of patient care is affected by interpreter services?
BHCs 1. What is your experience like providing bilingual services for Spanish speaking patients of the clinic?
2. What about using interpreter services (if applicable)—how have you found that to be?
3. How do you think the quality of patient care is affected by interpreter services?
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
53LANGUAGE CONCORDANCE AND ALLIANCE IN IBHC
view Board.
Quantitative data collection. Patients presented to their pri-
mary care provider for a variety of reasons, including annual
physical examinations, infections, pain, diabetes management, and
asthma. During their visit, the primary care provider identified a
behavioral health issue and referred the patient to a behavioral
health consultant for a same-day appointment. Behavioral health
consultants were licensed clinical social workers (n ⫽ 5), a li-
censed psychologist (n ⫽ 1), or psychology doctoral students in
training (n ⫽ 6). At that visit and all subsequent behavioral health
appointments, patients were instructed to complete the ACORN
questionnaire. Patients were seen for an average of 1.53 visits
(SD ⫽ 1.00, range 1– 8). Each visit lasted between 15 and 30
minutes and visits were spaced approximately 2 to 4 weeks apart.
Sessions were problem-focused and generally employed brief
cognitive– behavioral interventions such as behavioral activation,
motivational enhancement, exposure therapy, and psychoeduca-
tion. As part of standard operating procedures, patients of the
FQHC sign a consent form that specifies information in their
medical chart may be used for research purposes. Therefore,
additional consent to access preexisting data from electronic med-
ical records for this part of the study was not requested from
patients.
Qualitative data collection. Qualitative data collection took
place over a 2-month span (mid-September through mid-
November 2014). During times when research assistants were
present at the primary care sites, behavioral health care providers
having sessions with Spanish-speaking patients would request the
patient’s permission to allow a researcher to ask them a few
open-ended questions at the end of their appointment. Patients
were not selected by any other criteria. In addition, during that
span of time researchers arranged in-person or telephone inter-
views with behavioral health care providers and medical assistants.
We interviewed all BHCs who were currently employed by the
clinic (n ⫽ 4) and all BHCs who were or had completed an
externship at the clinic as part of their doctoral training (n ⫽ 6).
We also solicited interviews with medical assistants who were
currently employed by the clinic, frequently provided interpreta-
tion services for BHCs, and could schedule an interview.
All participants provided verbal consent and received a copy of
a consent form describing the purpose of the study, procedures,
and how data would be utilized. Interviews were conducted in
Spanish by bilingual clinical psychology doctoral students and a
licensed psychologist (all study authors). Interviews lasted be-
tween five and 10 minutes each. Interview responses were typed
out verbatim by the interviewer. Qualitative interview responses
were then content analyzed by the researchers for identification of
emerging themes. The process of identifying thematic categories
involved reading through interview transcripts, identifying as a
group the themes reflected in the responses, and then detailing
these themes into a codebook. Because of the exploratory nature of
the study, we avoided collapsing categories and opted instead to
create independent categories for all identified themes. Following
creation of the codebook, the first two authors independently
coded each interview. We assessed intercoder reliability separately
for each sample, using percent agreement (total agreements/total
coding instances). Interrater reliabilities were 97% (patient data),
86% (behavioral health provider data), and 92% (medical assistant
data). Disagreements were resolved via consensus by the two
coders.
Results
Quantitative Results
A one-way between-subjects analysis of variance (ANOVA)
was conducted to determine whether the use of an interpreter in the
behavioral health session (yes/no) was related to patients’ self-
reported therapeutic alliance with the behavioral health consultant.
No significant main effect of interpreter use was found, F(1,
456) ⫽ 1.81, p ⫽ .179. Patients who had an interpreter in the room
(M ⫽ 3.89, SD ⫽ 0.32, N ⫽ 199) had alliance ratings comparable
to those of patients who received services from a bilingual BHC
(M ⫽ 3.85, SD ⫽ 0.32, N ⫽ 259). Even when controlling for
relevant demographic covariates in a multiple regression (see
Table 2
Qualitative Interview Questions
Group Questions
Patients 1. How was your visit with [name of BHC]?
2. What did you think of the Spanish speaking abilities of [name of bilingual BHC or name of interpreter]? Was it
easy to understand his/her Spanish?
3. How well do you think [name of bilingual BHC or name of interpreter] understood your Spanish?
4. Do you think you had a good relationship with [name of BHC]?
5. Do you think it made that a difference that [name of BHC] could/could not speak Spanish?
6. Had you used an interpreter before?
7. For sessions with bilingual BHCs: Would it have been preferable to have an interpreter in your visit with [name
of bilingual BHC]? Why or why not?
8. For sessions with interpreters: Would it have been preferable if [name of BHC] spoke Spanish? Why or why not?
9. We want to improve our services for Spanish speaking patients. What could we do to make our services better?
Interpreters 1. What is your experience like providing interpreter services for Spanish speaking patients of the clinic?
2. Are these experiences similar for medical visits and behavioral health visits? If not, what is different?
3. How do you think the quality of patient care is affected by interpreter services?
BHCs 1. What is your experience like providing bilingual services for Spanish speaking patients of the clinic?
2. What about using interpreter services (if applicable)—how have you found that to be?
3. How do you think the quality of patient care is affected by interpreter services?
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
53LANGUAGE CONCORDANCE AND ALLIANCE IN IBHC
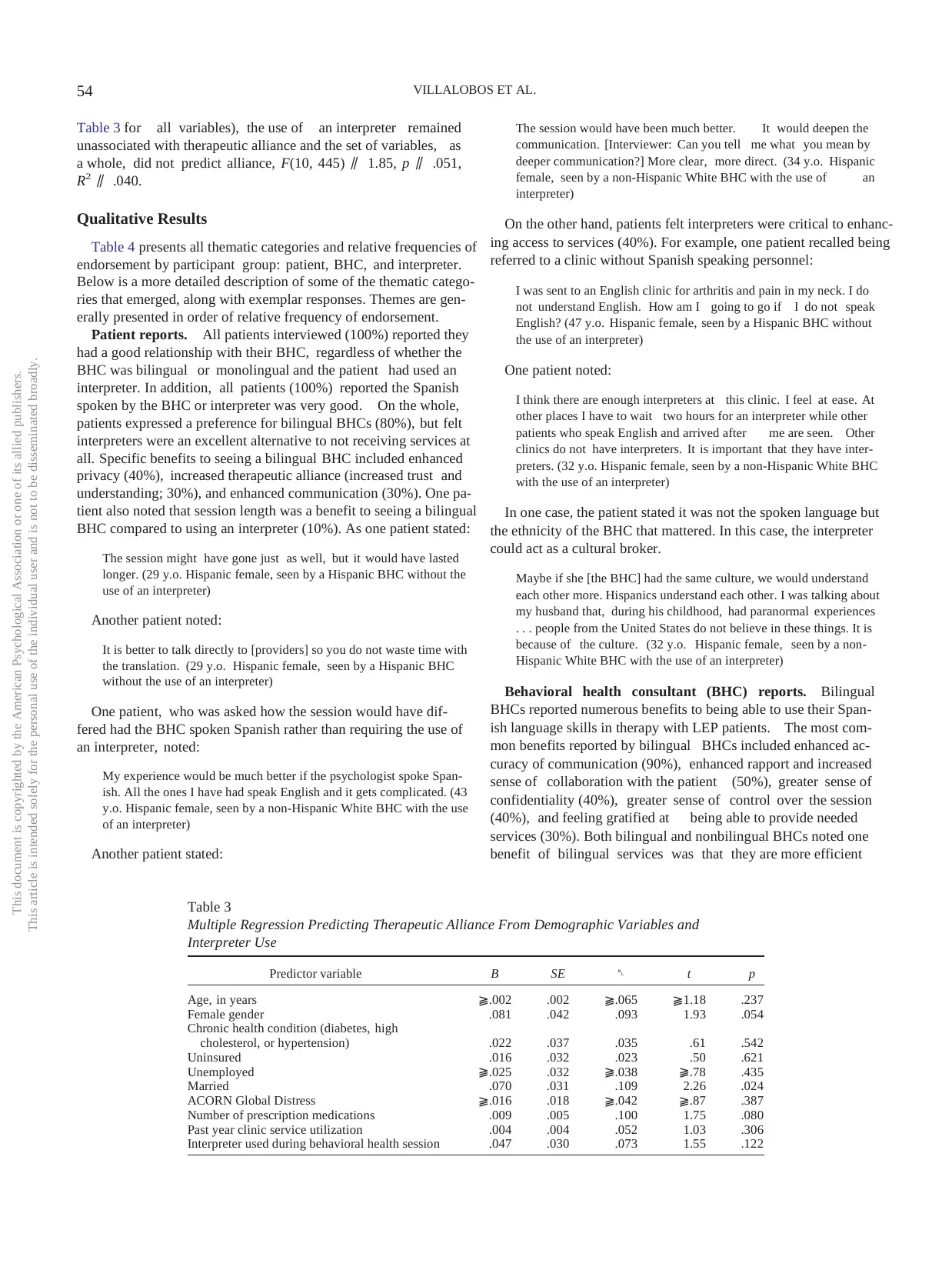
Table 3 for all variables), the use of an interpreter remained
unassociated with therapeutic alliance and the set of variables, as
a whole, did not predict alliance, F(10, 445) ⫽ 1.85, p ⫽ .051,
R 2 ⫽ .040.
Qualitative Results
Table 4 presents all thematic categories and relative frequencies of
endorsement by participant group: patient, BHC, and interpreter.
Below is a more detailed description of some of the thematic catego-
ries that emerged, along with exemplar responses. Themes are gen-
erally presented in order of relative frequency of endorsement.
Patient reports. All patients interviewed (100%) reported they
had a good relationship with their BHC, regardless of whether the
BHC was bilingual or monolingual and the patient had used an
interpreter. In addition, all patients (100%) reported the Spanish
spoken by the BHC or interpreter was very good. On the whole,
patients expressed a preference for bilingual BHCs (80%), but felt
interpreters were an excellent alternative to not receiving services at
all. Specific benefits to seeing a bilingual BHC included enhanced
privacy (40%), increased therapeutic alliance (increased trust and
understanding; 30%), and enhanced communication (30%). One pa-
tient also noted that session length was a benefit to seeing a bilingual
BHC compared to using an interpreter (10%). As one patient stated:
The session might have gone just as well, but it would have lasted
longer. (29 y.o. Hispanic female, seen by a Hispanic BHC without the
use of an interpreter)
Another patient noted:
It is better to talk directly to [providers] so you do not waste time with
the translation. (29 y.o. Hispanic female, seen by a Hispanic BHC
without the use of an interpreter)
One patient, who was asked how the session would have dif-
fered had the BHC spoken Spanish rather than requiring the use of
an interpreter, noted:
My experience would be much better if the psychologist spoke Span-
ish. All the ones I have had speak English and it gets complicated. (43
y.o. Hispanic female, seen by a non-Hispanic White BHC with the use
of an interpreter)
Another patient stated:
The session would have been much better. It would deepen the
communication. [Interviewer: Can you tell me what you mean by
deeper communication?] More clear, more direct. (34 y.o. Hispanic
female, seen by a non-Hispanic White BHC with the use of an
interpreter)
On the other hand, patients felt interpreters were critical to enhanc-
ing access to services (40%). For example, one patient recalled being
referred to a clinic without Spanish speaking personnel:
I was sent to an English clinic for arthritis and pain in my neck. I do
not understand English. How am I going to go if I do not speak
English? (47 y.o. Hispanic female, seen by a Hispanic BHC without
the use of an interpreter)
One patient noted:
I think there are enough interpreters at this clinic. I feel at ease. At
other places I have to wait two hours for an interpreter while other
patients who speak English and arrived after me are seen. Other
clinics do not have interpreters. It is important that they have inter-
preters. (32 y.o. Hispanic female, seen by a non-Hispanic White BHC
with the use of an interpreter)
In one case, the patient stated it was not the spoken language but
the ethnicity of the BHC that mattered. In this case, the interpreter
could act as a cultural broker.
Maybe if she [the BHC] had the same culture, we would understand
each other more. Hispanics understand each other. I was talking about
my husband that, during his childhood, had paranormal experiences
. . . people from the United States do not believe in these things. It is
because of the culture. (32 y.o. Hispanic female, seen by a non-
Hispanic White BHC with the use of an interpreter)
Behavioral health consultant (BHC) reports. Bilingual
BHCs reported numerous benefits to being able to use their Span-
ish language skills in therapy with LEP patients. The most com-
mon benefits reported by bilingual BHCs included enhanced ac-
curacy of communication (90%), enhanced rapport and increased
sense of collaboration with the patient (50%), greater sense of
confidentiality (40%), greater sense of control over the session
(40%), and feeling gratified at being able to provide needed
services (30%). Both bilingual and nonbilingual BHCs noted one
benefit of bilingual services was that they are more efficient
Table 3
Multiple Regression Predicting Therapeutic Alliance From Demographic Variables and
Interpreter Use
Predictor variable B SE  t p
Age, in years ⫺.002 .002 ⫺.065 ⫺1.18 .237
Female gender .081 .042 .093 1.93 .054
Chronic health condition (diabetes, high
cholesterol, or hypertension) .022 .037 .035 .61 .542
Uninsured .016 .032 .023 .50 .621
Unemployed ⫺.025 .032 ⫺.038 ⫺.78 .435
Married .070 .031 .109 2.26 .024
ACORN Global Distress ⫺.016 .018 ⫺.042 ⫺.87 .387
Number of prescription medications .009 .005 .100 1.75 .080
Past year clinic service utilization .004 .004 .052 1.03 .306
Interpreter used during behavioral health session .047 .030 .073 1.55 .122
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
54 VILLALOBOS ET AL.
unassociated with therapeutic alliance and the set of variables, as
a whole, did not predict alliance, F(10, 445) ⫽ 1.85, p ⫽ .051,
R 2 ⫽ .040.
Qualitative Results
Table 4 presents all thematic categories and relative frequencies of
endorsement by participant group: patient, BHC, and interpreter.
Below is a more detailed description of some of the thematic catego-
ries that emerged, along with exemplar responses. Themes are gen-
erally presented in order of relative frequency of endorsement.
Patient reports. All patients interviewed (100%) reported they
had a good relationship with their BHC, regardless of whether the
BHC was bilingual or monolingual and the patient had used an
interpreter. In addition, all patients (100%) reported the Spanish
spoken by the BHC or interpreter was very good. On the whole,
patients expressed a preference for bilingual BHCs (80%), but felt
interpreters were an excellent alternative to not receiving services at
all. Specific benefits to seeing a bilingual BHC included enhanced
privacy (40%), increased therapeutic alliance (increased trust and
understanding; 30%), and enhanced communication (30%). One pa-
tient also noted that session length was a benefit to seeing a bilingual
BHC compared to using an interpreter (10%). As one patient stated:
The session might have gone just as well, but it would have lasted
longer. (29 y.o. Hispanic female, seen by a Hispanic BHC without the
use of an interpreter)
Another patient noted:
It is better to talk directly to [providers] so you do not waste time with
the translation. (29 y.o. Hispanic female, seen by a Hispanic BHC
without the use of an interpreter)
One patient, who was asked how the session would have dif-
fered had the BHC spoken Spanish rather than requiring the use of
an interpreter, noted:
My experience would be much better if the psychologist spoke Span-
ish. All the ones I have had speak English and it gets complicated. (43
y.o. Hispanic female, seen by a non-Hispanic White BHC with the use
of an interpreter)
Another patient stated:
The session would have been much better. It would deepen the
communication. [Interviewer: Can you tell me what you mean by
deeper communication?] More clear, more direct. (34 y.o. Hispanic
female, seen by a non-Hispanic White BHC with the use of an
interpreter)
On the other hand, patients felt interpreters were critical to enhanc-
ing access to services (40%). For example, one patient recalled being
referred to a clinic without Spanish speaking personnel:
I was sent to an English clinic for arthritis and pain in my neck. I do
not understand English. How am I going to go if I do not speak
English? (47 y.o. Hispanic female, seen by a Hispanic BHC without
the use of an interpreter)
One patient noted:
I think there are enough interpreters at this clinic. I feel at ease. At
other places I have to wait two hours for an interpreter while other
patients who speak English and arrived after me are seen. Other
clinics do not have interpreters. It is important that they have inter-
preters. (32 y.o. Hispanic female, seen by a non-Hispanic White BHC
with the use of an interpreter)
In one case, the patient stated it was not the spoken language but
the ethnicity of the BHC that mattered. In this case, the interpreter
could act as a cultural broker.
Maybe if she [the BHC] had the same culture, we would understand
each other more. Hispanics understand each other. I was talking about
my husband that, during his childhood, had paranormal experiences
. . . people from the United States do not believe in these things. It is
because of the culture. (32 y.o. Hispanic female, seen by a non-
Hispanic White BHC with the use of an interpreter)
Behavioral health consultant (BHC) reports. Bilingual
BHCs reported numerous benefits to being able to use their Span-
ish language skills in therapy with LEP patients. The most com-
mon benefits reported by bilingual BHCs included enhanced ac-
curacy of communication (90%), enhanced rapport and increased
sense of collaboration with the patient (50%), greater sense of
confidentiality (40%), greater sense of control over the session
(40%), and feeling gratified at being able to provide needed
services (30%). Both bilingual and nonbilingual BHCs noted one
benefit of bilingual services was that they are more efficient
Table 3
Multiple Regression Predicting Therapeutic Alliance From Demographic Variables and
Interpreter Use
Predictor variable B SE  t p
Age, in years ⫺.002 .002 ⫺.065 ⫺1.18 .237
Female gender .081 .042 .093 1.93 .054
Chronic health condition (diabetes, high
cholesterol, or hypertension) .022 .037 .035 .61 .542
Uninsured .016 .032 .023 .50 .621
Unemployed ⫺.025 .032 ⫺.038 ⫺.78 .435
Married .070 .031 .109 2.26 .024
ACORN Global Distress ⫺.016 .018 ⫺.042 ⫺.87 .387
Number of prescription medications .009 .005 .100 1.75 .080
Past year clinic service utilization .004 .004 .052 1.03 .306
Interpreter used during behavioral health session .047 .030 .073 1.55 .122
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
54 VILLALOBOS ET AL.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

compared to using an interpreter (10% noted efficiency of bilin-
gual sessions and 30% noted problems with long wait times for
interpreters). For instance, one BHC noted:
Sometimes they [the patients] have to wait longer because there is a
lack of translators when it is busy. (32 y.o. non-Hispanic White female
who is not bilingual)
Another BHC noted:
I felt that there was more openness and more time to discuss their [the
patient’s] difficulties because there was not someone else that then had to
take what I said, interpret it based on their own understanding, and then
send that message back to the patient. (25 y.o. bilingual Hispanic female)
In addition to helping increase access to services and to making
patients feel welcome, BHCs noted benefits to their own profes-
sional development. One bilingual BHC noted:
My experience so far has been wonderful to be able to offer services
to a community that is in need that sometimes has difficulty or is
unable to receive adequate care. It’s important to me that the Latino
community is receiving evidence-based interventions in practice. I
think as much as the experience details . . . they also help me as a
trainee clinician/student in my efforts to provide the best services
possible in English or in Spanish. It’s been a wonderful life-changing
experience. (26 y.o. bilingual Hispanic male)
Forty percent of BHCs struggled with finding words or learning
the technical vocabulary associated with behavioral health inter-
ventions. However, one bilingual BHC noted this was beneficial to
her, because she would simplify her language and avoid psycho-
babble in her delivery of specific interventions:
It made me slow down and think about the processes of what I was
describing because I had to use smaller words and not use vocabulary
that patients didn’t understand, such as behavioral activation or mind-
fulness that do not have direct translations. (26 y.o. bilingual non-
Hispanic White female, referring to sessions she has conducted with
Marshallese patients facilitated by interpreters)
When asking about their experiences with using interpreters in
sessions with LEP patients, monolingual BHCs reported numerous
Table 4
Frequency of Qualitative Interview Themes
Theme % Patients % BHCs % Interpreters
Bilingual services . . .
. . . Benefit the patient
1. Increased access to services 0% 20% 0%
2. Enhanced rapport, sense of collaboration (or interpreter services may present barriers to
rapport between BHC and patient, such as having a third person in the room, or having
the interpreter’s reactions) 30% 50% 10%
3. Enhanced trust, understanding, privacy, willingness to self-disclose (or interpreter services
may compromise confidentiality and trust) 40% 40% 0%
4. Better communication (increased accuracy of communication, including avoiding use of
psychobabble) 30% 90% 20%
5. Are more efficient (shorter sessions than if you have to have everything interpreted) 10% 10% 20%
. . . Benefit the BHC
6. Improve BHC’s Spanish speaking abilities 0% 10% 0%
7. Enhance clinical skills and knowledge 0% 10% 0%
8. Satisfaction with providing a needed service 0% 30% 0%
9. BHC maintains more control over the session, session less effort (e.g., making sure the
message is understood as intended, rather than communicating indirectly; managing self
and patient reactions to session content, without worrying about interpreter reactions) 0% 40% 0%
. . . Are challenging to provide
10. Trouble with word finding, dialects, phrasing, or technical vocabulary 0% 40% 0%
Interpreter services . . .
. . . Benefit the patient
11. Increased access to services 40% 70% 40%
12. Interpreter (or BHC) can be a “cultural broker” in the room (or the shared culture matters) 10% 30% 10%
13. Help make patients feel welcome and comfortable 10% 10% 50%
14. Facilitate intervention (can go very smoothly) 0% 20% 20%
. . . Benefit the interpreter
15. Enhance Spanish speaking abilities/vocabulary 0% 0% 20%
16. Provide an enriching professional experience 0% 0% 30%
. . . Are challenging to provide
17. Resource-intensive 0% 10% 0%
18. Interpreters not always available 20% 30% 0%
19. Trouble with word finding, dialects, phrasing, or technical vocabulary 0% 0% 60%
. . . Can be helpful or harmful, depending on the interpreter
20. Good working relationship with the BHC 0% 20% 0%
21. Comfort with psychological material 0% 30% 20%
22. Degree of professionalism, training, and experience 0% 30% 30%
Interpreter ⬍ Bilingual BHC 80% 30% 10%
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
55LANGUAGE CONCORDANCE AND ALLIANCE IN IBHC
gual sessions and 30% noted problems with long wait times for
interpreters). For instance, one BHC noted:
Sometimes they [the patients] have to wait longer because there is a
lack of translators when it is busy. (32 y.o. non-Hispanic White female
who is not bilingual)
Another BHC noted:
I felt that there was more openness and more time to discuss their [the
patient’s] difficulties because there was not someone else that then had to
take what I said, interpret it based on their own understanding, and then
send that message back to the patient. (25 y.o. bilingual Hispanic female)
In addition to helping increase access to services and to making
patients feel welcome, BHCs noted benefits to their own profes-
sional development. One bilingual BHC noted:
My experience so far has been wonderful to be able to offer services
to a community that is in need that sometimes has difficulty or is
unable to receive adequate care. It’s important to me that the Latino
community is receiving evidence-based interventions in practice. I
think as much as the experience details . . . they also help me as a
trainee clinician/student in my efforts to provide the best services
possible in English or in Spanish. It’s been a wonderful life-changing
experience. (26 y.o. bilingual Hispanic male)
Forty percent of BHCs struggled with finding words or learning
the technical vocabulary associated with behavioral health inter-
ventions. However, one bilingual BHC noted this was beneficial to
her, because she would simplify her language and avoid psycho-
babble in her delivery of specific interventions:
It made me slow down and think about the processes of what I was
describing because I had to use smaller words and not use vocabulary
that patients didn’t understand, such as behavioral activation or mind-
fulness that do not have direct translations. (26 y.o. bilingual non-
Hispanic White female, referring to sessions she has conducted with
Marshallese patients facilitated by interpreters)
When asking about their experiences with using interpreters in
sessions with LEP patients, monolingual BHCs reported numerous
Table 4
Frequency of Qualitative Interview Themes
Theme % Patients % BHCs % Interpreters
Bilingual services . . .
. . . Benefit the patient
1. Increased access to services 0% 20% 0%
2. Enhanced rapport, sense of collaboration (or interpreter services may present barriers to
rapport between BHC and patient, such as having a third person in the room, or having
the interpreter’s reactions) 30% 50% 10%
3. Enhanced trust, understanding, privacy, willingness to self-disclose (or interpreter services
may compromise confidentiality and trust) 40% 40% 0%
4. Better communication (increased accuracy of communication, including avoiding use of
psychobabble) 30% 90% 20%
5. Are more efficient (shorter sessions than if you have to have everything interpreted) 10% 10% 20%
. . . Benefit the BHC
6. Improve BHC’s Spanish speaking abilities 0% 10% 0%
7. Enhance clinical skills and knowledge 0% 10% 0%
8. Satisfaction with providing a needed service 0% 30% 0%
9. BHC maintains more control over the session, session less effort (e.g., making sure the
message is understood as intended, rather than communicating indirectly; managing self
and patient reactions to session content, without worrying about interpreter reactions) 0% 40% 0%
. . . Are challenging to provide
10. Trouble with word finding, dialects, phrasing, or technical vocabulary 0% 40% 0%
Interpreter services . . .
. . . Benefit the patient
11. Increased access to services 40% 70% 40%
12. Interpreter (or BHC) can be a “cultural broker” in the room (or the shared culture matters) 10% 30% 10%
13. Help make patients feel welcome and comfortable 10% 10% 50%
14. Facilitate intervention (can go very smoothly) 0% 20% 20%
. . . Benefit the interpreter
15. Enhance Spanish speaking abilities/vocabulary 0% 0% 20%
16. Provide an enriching professional experience 0% 0% 30%
. . . Are challenging to provide
17. Resource-intensive 0% 10% 0%
18. Interpreters not always available 20% 30% 0%
19. Trouble with word finding, dialects, phrasing, or technical vocabulary 0% 0% 60%
. . . Can be helpful or harmful, depending on the interpreter
20. Good working relationship with the BHC 0% 20% 0%
21. Comfort with psychological material 0% 30% 20%
22. Degree of professionalism, training, and experience 0% 30% 30%
Interpreter ⬍ Bilingual BHC 80% 30% 10%
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
55LANGUAGE CONCORDANCE AND ALLIANCE IN IBHC
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
benefits, especially when they came to trust the interpreter and his
skills. A notable benefit was that interpreters could serve as cul-
tural brokers, educating BHCs by providing context to understand
word meanings (30%). When the BHC and the interpreter had
developed a good working relationship, the interpreter was often
seen as enhancing service delivery (20%). One BHC noted:
The rapport I build with each translator, I thought, is what did it for
me. Once I worked for a bit with each of them they kind of already
knew what I was going to say so sometimes, with minor revisions,
they knew exactly what I was going to do with someone with sleep
difficulties or anxiety difficulties, which made the whole process that
much smoother. (30 y.o. non-Hispanic White male who is not
bilingual)
On the other hand, experiences with the use of interpreters
resulted in some cautionary tales. In particular, BHCs noted con-
cerns with the accuracy of interpretation (30%). This was both a
concern for loss of information and for occasions where an inter-
preter was seen as “overstepping” her role. One BHC stated:
I have to be careful that the interpreter doesn’t get carried away.
Sometimes I can watch by their tone or body language how they are
relaying information and sometimes it might not be in the same
manner that I am. I think at times they might be more forceful, more
punitive, like with a diabetic patient not being compliant. (42 y.o.
bilingual non-Hispanic White female, referring to sessions she has
conducted with Marshallese patients facilitated by interpreters)
Another noted:
The interpreters would intervene and provide a lot of commentary and
I would have to wrangle the translator as much as I was providing
services. (28 y.o. bilingual non-Hispanic White male, referring to
sessions he has conducted with Marshallese patients facilitated by
interpreters)
Barriers to rapport and alliance were also noted by some BHCs
(30%).
I feel as though the patients are sometimes uncomfortable with an-
other person present in the room. I’ve also found that sometimes the
interpreters seem to be uncomfortable with the content of session and
that in turn affects the patient and they [the patients] start speaking
less about their problem (27 y.o. Hispanic female who is not bilingual)
Finally, some BHCs noted sessions required additional effort on
their part, especially attending to the emotions of both the patients
and the interpreters. A BHC stated in her interview:
I have to try harder [with personal interactions] and find I am more
focused on nonverbals: tone, posture . . . all nonverbals. I am more
expressive and use more nonverbal facial expressions and hand mo-
tions. (44 y.o. bilingual non-Hispanic White female, referring to
sessions she has conducted with Marshallese patients facilitated by
interpreters)
Interpreter reports. Interpreters had insightful observations
regarding the benefits and challenges they face providing interpre-
tation services for BHCs and patients. Many of the same benefits
noted by BHCs were noted by interpreters, including making
patients feel welcome (50%), helping enhance access to services
(40%), and feeling enriched professionally (30%). Interpreters
noted some professional obstacles to their work, including navi-
gating differences among diverse Spanish dialects or acquiring the
specific technical language of mental health providers (60%) and
becoming more comfortable with the more sensitive material of
behavioral health, versus medical, sessions (20%). This was true
despite having received additional training in interpretation for
behavioral health sessions, in particular. As one interpreter noted:
At times it was hard because I learned there is not just one type of
Spanish. One word can have different meanings. (22 y.o. Hispanic
female)
When asked about her experiences interpreting for medical
visits compared to BHC visits, one interpreter noted:
I would have to say there is a slight difference between the both. In a
medical visit, things are interpreted in a faster pace than in behavioral
health, which goes more into depth. In a behavioral health visit
emotions get more involved than in a regular medical visit, which
could make it hard for an interpreter if they’re [the interpreter] an
emotional person. (24 y.o. Hispanic female)
Comparisons among reporters. Several similarities and dif-
ferences among the three participant groups emerged. Across all
groups, there was a strong sense that interpreter services were vital
to increasing access to needed care. There was also an appreciation
for the benefit of bilingual providers for both enhanced rapport
between provider and patient and enhanced communication. Bi-
lingual services were also seen as more efficient in comparison
with interpreter services. However, differences among the groups
also emerged. Providers and interpreters saw benefits to their
professional development from providing services in Spanish or
through the use of interpreters, but also noted challenges of nav-
igating diverse dialects and technical vocabulary. They also fo-
cused more on the importance of the relationship between provider
and interpreter for a smooth session. BHCs and interpreters were
somewhat agnostic about the relative benefits of bilingual provid-
ers versus interpreters, seeing both as quite similar in efficacy.
Patients were more likely to express a strong preference for direct
communication with providers.
Discussion
In this study, we asked how therapeutic alliance between pri-
mary care patients with limited English proficiency (LEP) and
their behavioral health care providers (BHCs) was impacted by
language concordance between the BHC and the patient, versus
when a trained interpreter was present. Quantitative data from 458
patients revealed comparable satisfaction with the BHC and the
session in LEP patients who saw bilingual BHCs versus those who
saw an English-speaking BHC with the aid of a trained interpreter.
Importantly, therapeutic alliance was very high in both groups,
suggesting sessions conducted by bilingual BHCs and sessions
facilitated by trained interpreters are equally effective at address-
ing the behavioral health care needs of LEP patients. Our finding
is consistent with a growing body of research suggesting health
care services can be effectively delivered with trained interpreters
(Brune et al., 2011; Karliner et al., 2007; Schulz et al., 2006).
Content analyses of interviews conducted with LEP patients,
BHCs, and trained interpreters revealed a richer and more complex
picture. With almost no exception, patients revealed a preference
for language concordance between the BHC and the patient. In
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
56 VILLALOBOS ET AL.
skills. A notable benefit was that interpreters could serve as cul-
tural brokers, educating BHCs by providing context to understand
word meanings (30%). When the BHC and the interpreter had
developed a good working relationship, the interpreter was often
seen as enhancing service delivery (20%). One BHC noted:
The rapport I build with each translator, I thought, is what did it for
me. Once I worked for a bit with each of them they kind of already
knew what I was going to say so sometimes, with minor revisions,
they knew exactly what I was going to do with someone with sleep
difficulties or anxiety difficulties, which made the whole process that
much smoother. (30 y.o. non-Hispanic White male who is not
bilingual)
On the other hand, experiences with the use of interpreters
resulted in some cautionary tales. In particular, BHCs noted con-
cerns with the accuracy of interpretation (30%). This was both a
concern for loss of information and for occasions where an inter-
preter was seen as “overstepping” her role. One BHC stated:
I have to be careful that the interpreter doesn’t get carried away.
Sometimes I can watch by their tone or body language how they are
relaying information and sometimes it might not be in the same
manner that I am. I think at times they might be more forceful, more
punitive, like with a diabetic patient not being compliant. (42 y.o.
bilingual non-Hispanic White female, referring to sessions she has
conducted with Marshallese patients facilitated by interpreters)
Another noted:
The interpreters would intervene and provide a lot of commentary and
I would have to wrangle the translator as much as I was providing
services. (28 y.o. bilingual non-Hispanic White male, referring to
sessions he has conducted with Marshallese patients facilitated by
interpreters)
Barriers to rapport and alliance were also noted by some BHCs
(30%).
I feel as though the patients are sometimes uncomfortable with an-
other person present in the room. I’ve also found that sometimes the
interpreters seem to be uncomfortable with the content of session and
that in turn affects the patient and they [the patients] start speaking
less about their problem (27 y.o. Hispanic female who is not bilingual)
Finally, some BHCs noted sessions required additional effort on
their part, especially attending to the emotions of both the patients
and the interpreters. A BHC stated in her interview:
I have to try harder [with personal interactions] and find I am more
focused on nonverbals: tone, posture . . . all nonverbals. I am more
expressive and use more nonverbal facial expressions and hand mo-
tions. (44 y.o. bilingual non-Hispanic White female, referring to
sessions she has conducted with Marshallese patients facilitated by
interpreters)
Interpreter reports. Interpreters had insightful observations
regarding the benefits and challenges they face providing interpre-
tation services for BHCs and patients. Many of the same benefits
noted by BHCs were noted by interpreters, including making
patients feel welcome (50%), helping enhance access to services
(40%), and feeling enriched professionally (30%). Interpreters
noted some professional obstacles to their work, including navi-
gating differences among diverse Spanish dialects or acquiring the
specific technical language of mental health providers (60%) and
becoming more comfortable with the more sensitive material of
behavioral health, versus medical, sessions (20%). This was true
despite having received additional training in interpretation for
behavioral health sessions, in particular. As one interpreter noted:
At times it was hard because I learned there is not just one type of
Spanish. One word can have different meanings. (22 y.o. Hispanic
female)
When asked about her experiences interpreting for medical
visits compared to BHC visits, one interpreter noted:
I would have to say there is a slight difference between the both. In a
medical visit, things are interpreted in a faster pace than in behavioral
health, which goes more into depth. In a behavioral health visit
emotions get more involved than in a regular medical visit, which
could make it hard for an interpreter if they’re [the interpreter] an
emotional person. (24 y.o. Hispanic female)
Comparisons among reporters. Several similarities and dif-
ferences among the three participant groups emerged. Across all
groups, there was a strong sense that interpreter services were vital
to increasing access to needed care. There was also an appreciation
for the benefit of bilingual providers for both enhanced rapport
between provider and patient and enhanced communication. Bi-
lingual services were also seen as more efficient in comparison
with interpreter services. However, differences among the groups
also emerged. Providers and interpreters saw benefits to their
professional development from providing services in Spanish or
through the use of interpreters, but also noted challenges of nav-
igating diverse dialects and technical vocabulary. They also fo-
cused more on the importance of the relationship between provider
and interpreter for a smooth session. BHCs and interpreters were
somewhat agnostic about the relative benefits of bilingual provid-
ers versus interpreters, seeing both as quite similar in efficacy.
Patients were more likely to express a strong preference for direct
communication with providers.
Discussion
In this study, we asked how therapeutic alliance between pri-
mary care patients with limited English proficiency (LEP) and
their behavioral health care providers (BHCs) was impacted by
language concordance between the BHC and the patient, versus
when a trained interpreter was present. Quantitative data from 458
patients revealed comparable satisfaction with the BHC and the
session in LEP patients who saw bilingual BHCs versus those who
saw an English-speaking BHC with the aid of a trained interpreter.
Importantly, therapeutic alliance was very high in both groups,
suggesting sessions conducted by bilingual BHCs and sessions
facilitated by trained interpreters are equally effective at address-
ing the behavioral health care needs of LEP patients. Our finding
is consistent with a growing body of research suggesting health
care services can be effectively delivered with trained interpreters
(Brune et al., 2011; Karliner et al., 2007; Schulz et al., 2006).
Content analyses of interviews conducted with LEP patients,
BHCs, and trained interpreters revealed a richer and more complex
picture. With almost no exception, patients revealed a preference
for language concordance between the BHC and the patient. In
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
56 VILLALOBOS ET AL.

particular, language concordant services were thought to be more
efficient, more effective in terms of communication of content,
easier for the establishment of trust and rapport, and more confi-
dential. Multiple patients reported an increased willingness to
disclose sensitive information when it was just the patient and the
BHC, versus when a third party was present.
However, the use of trained interpreters was also seen positively
by nearly all patients, providers, and interpreters. Sessions with
interpreters were valued for numerous reasons, including increas-
ing access to needed services for LEP patients and enhancing
professional development in BHCs and interpreters. The common
refrain across multiple informants was that interpreters were val-
ued members of the health care team and critical for receiving
timely care. Most participants recognized the disparity between
need for bilingual professionals and workforce skills; in this con-
text, trained interpreters were seen as essential to bridging the gap.
Similar to cautions articulated by Raval and Smith (2003) and
Tribe and Tunariu (2009), we found patients, BHCs, and interpret-
ers expressed caveats to the benefits of interpreter services. Some
of these were not unique to interpreter services per se. For exam-
ple, both bilingual BHCs and interpreters noted concerns regarding
navigating the different Spanish dialects, regionalisms, and nu-
ances in expression. On the other hand, working with diverse
Spanish-speaking populations provided opportunities for profes-
sional growth in both BHCs and trained interpreters— both noted
the benefits of enhancing their technical language skills and valued
additional training specific to behavioral health interpretation.
Other caveats to the benefits of providing services to LEP
patients through the use of trained interpreters were more specific
to that situation. Patients, BHCs, and interpreters all noted the
challenges of establishing rapport and navigating the reactions of
all persons in the room when an interpreter was present—the
material revealed during behavioral health sessions was often
personal, sometimes stigmatizing, and frequently emotional. Al-
though mental health professionals have specific training in man-
aging such content with a high degree of openness, compassion,
and empathy, some trained interpreters found the difference be-
tween medical and behavioral health interpretation to be challeng-
ing. Some interpreters also noted they felt like a “third wheel” in
session, a sentiment echoed by a few BHCs and patients.
Limitations and Future Directions
Although we are encouraged by our results, readers should
consider the limitations to our study. First and foremost, the
current study examined therapeutic alliance when trained inter-
preters were used in behavioral health care sessions. We do not
know how patients would have felt about sessions that included ad
hoc interpretation by untrained individuals; however, a robust
body of research suggests untrained interpreters can be problem-
atic for patient satisfaction and outcomes (see Karliner et al.,
2007). A second but related concern is that the interpreters used in
the current study were not specifically trained for mental health
care interpretation. Although all were provided with some training
in behavioral health interpretation, the training was limited to one
presentation and additional shadowing experiences of varying du-
ration. It is possible that additional in-depth training specific to
mental health care would alleviate many of the potential concerns
raised by patients, BHCs, and interpreters. d’Ardenne, Farmer,
Ruaro, and Priebe (2007) developed an interpreting protocol for
trauma-focused cognitive– behavioral therapy that provides spe-
cific recommendations for clinic services, therapists, and interpret-
ers. In addition, the National Latino Behavioral Health Association
and the National Asian American Pacific Islander Mental Health
Association provide an interpreter training program for mental
health interpreter certification.
Third, the unique structure of integrated care sessions (brief,
problem-focused, few visits) limits the generalizability of our
findings. It is unclear whether similar benefits and caveats to
interpreter services would be present for more traditional men-
tal health settings. It is possible that some concerns would be
amplified in traditional care, including the need to manage
emotional responses of people in the room or concerns regard-
ing disclosure of confidential information; on the other hand, it
may be that the longer duration and greater intensity of tradi-
tional mental health services give patients and therapists oppor-
tunities to acclimate to the presence of the interpreter, rendering
many concerns moot. Future studies examining interpreter service
satisfaction in more traditional mental health care settings are
therefore sorely needed.
Fourth, the quantitative and qualitative portions of the study
were complementary, but not redundant. In particular the quanti-
tative portion of the study had a limited measure of therapeutic
alliance (four questions), none of which assessed satisfaction with
the linguistic abilities of the BHC or the relative preference of a
bilingual BHC versus a trained interpreter. It is possible that more
pointed and specific questions regarding alliance and satisfaction
with linguistically competent services would have revealed differ-
ences between LEP patients seen by language concordant provid-
ers versus those seen by interpreters. Future studies may wish to
expand the quantitative measurement of alliance and satisfaction.
Relatedly, although the qualitative portion of the study specifically
asked patients to consider how the session might have differed if
they had used an interpreter (for those who saw a bilingual BHC)
or had seen a bilingual BHC (for those who used an interpreter),
patients were not directly asked to compare and contrast sessions
with bilingual BHCs and interpreters, nor did patients necessarily
have experiences with both types of sessions. Responses that
indicate relative comparisons, therefore, should be interpreted with
some degree of caution and future studies could select patients
who have experienced both types of sessions in order to compare
the two more directly. The qualitative portion of the study included
interviews with essentially all BHCs the clinic employed, but only
a limited number of interpreters and patients. In addition, we did
not specifically select patients who were representative of the
original sample, nor did we have an independent auditor for coding
of interview responses. It is unclear whether additional themes
would have emerged had more people participated, or whether
themes were reflective of the original sample. Future researchers
may continue enrolling participants until themes are saturated.
Relatedly, the interviews were designed to be brief so as to
minimally disrupt clinic flow. A more detailed and in-depth inter-
view may have revealed additional complexities and preferences
that did not emerge in this briefer format. Finally, even the bilin-
gual BHCs frequently had experience using interpreters for pa-
tients who spoke languages other than English and Spanish; there-
fore, the emerging themes may have not been unique to
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
57LANGUAGE CONCORDANCE AND ALLIANCE IN IBHC
efficient, more effective in terms of communication of content,
easier for the establishment of trust and rapport, and more confi-
dential. Multiple patients reported an increased willingness to
disclose sensitive information when it was just the patient and the
BHC, versus when a third party was present.
However, the use of trained interpreters was also seen positively
by nearly all patients, providers, and interpreters. Sessions with
interpreters were valued for numerous reasons, including increas-
ing access to needed services for LEP patients and enhancing
professional development in BHCs and interpreters. The common
refrain across multiple informants was that interpreters were val-
ued members of the health care team and critical for receiving
timely care. Most participants recognized the disparity between
need for bilingual professionals and workforce skills; in this con-
text, trained interpreters were seen as essential to bridging the gap.
Similar to cautions articulated by Raval and Smith (2003) and
Tribe and Tunariu (2009), we found patients, BHCs, and interpret-
ers expressed caveats to the benefits of interpreter services. Some
of these were not unique to interpreter services per se. For exam-
ple, both bilingual BHCs and interpreters noted concerns regarding
navigating the different Spanish dialects, regionalisms, and nu-
ances in expression. On the other hand, working with diverse
Spanish-speaking populations provided opportunities for profes-
sional growth in both BHCs and trained interpreters— both noted
the benefits of enhancing their technical language skills and valued
additional training specific to behavioral health interpretation.
Other caveats to the benefits of providing services to LEP
patients through the use of trained interpreters were more specific
to that situation. Patients, BHCs, and interpreters all noted the
challenges of establishing rapport and navigating the reactions of
all persons in the room when an interpreter was present—the
material revealed during behavioral health sessions was often
personal, sometimes stigmatizing, and frequently emotional. Al-
though mental health professionals have specific training in man-
aging such content with a high degree of openness, compassion,
and empathy, some trained interpreters found the difference be-
tween medical and behavioral health interpretation to be challeng-
ing. Some interpreters also noted they felt like a “third wheel” in
session, a sentiment echoed by a few BHCs and patients.
Limitations and Future Directions
Although we are encouraged by our results, readers should
consider the limitations to our study. First and foremost, the
current study examined therapeutic alliance when trained inter-
preters were used in behavioral health care sessions. We do not
know how patients would have felt about sessions that included ad
hoc interpretation by untrained individuals; however, a robust
body of research suggests untrained interpreters can be problem-
atic for patient satisfaction and outcomes (see Karliner et al.,
2007). A second but related concern is that the interpreters used in
the current study were not specifically trained for mental health
care interpretation. Although all were provided with some training
in behavioral health interpretation, the training was limited to one
presentation and additional shadowing experiences of varying du-
ration. It is possible that additional in-depth training specific to
mental health care would alleviate many of the potential concerns
raised by patients, BHCs, and interpreters. d’Ardenne, Farmer,
Ruaro, and Priebe (2007) developed an interpreting protocol for
trauma-focused cognitive– behavioral therapy that provides spe-
cific recommendations for clinic services, therapists, and interpret-
ers. In addition, the National Latino Behavioral Health Association
and the National Asian American Pacific Islander Mental Health
Association provide an interpreter training program for mental
health interpreter certification.
Third, the unique structure of integrated care sessions (brief,
problem-focused, few visits) limits the generalizability of our
findings. It is unclear whether similar benefits and caveats to
interpreter services would be present for more traditional men-
tal health settings. It is possible that some concerns would be
amplified in traditional care, including the need to manage
emotional responses of people in the room or concerns regard-
ing disclosure of confidential information; on the other hand, it
may be that the longer duration and greater intensity of tradi-
tional mental health services give patients and therapists oppor-
tunities to acclimate to the presence of the interpreter, rendering
many concerns moot. Future studies examining interpreter service
satisfaction in more traditional mental health care settings are
therefore sorely needed.
Fourth, the quantitative and qualitative portions of the study
were complementary, but not redundant. In particular the quanti-
tative portion of the study had a limited measure of therapeutic
alliance (four questions), none of which assessed satisfaction with
the linguistic abilities of the BHC or the relative preference of a
bilingual BHC versus a trained interpreter. It is possible that more
pointed and specific questions regarding alliance and satisfaction
with linguistically competent services would have revealed differ-
ences between LEP patients seen by language concordant provid-
ers versus those seen by interpreters. Future studies may wish to
expand the quantitative measurement of alliance and satisfaction.
Relatedly, although the qualitative portion of the study specifically
asked patients to consider how the session might have differed if
they had used an interpreter (for those who saw a bilingual BHC)
or had seen a bilingual BHC (for those who used an interpreter),
patients were not directly asked to compare and contrast sessions
with bilingual BHCs and interpreters, nor did patients necessarily
have experiences with both types of sessions. Responses that
indicate relative comparisons, therefore, should be interpreted with
some degree of caution and future studies could select patients
who have experienced both types of sessions in order to compare
the two more directly. The qualitative portion of the study included
interviews with essentially all BHCs the clinic employed, but only
a limited number of interpreters and patients. In addition, we did
not specifically select patients who were representative of the
original sample, nor did we have an independent auditor for coding
of interview responses. It is unclear whether additional themes
would have emerged had more people participated, or whether
themes were reflective of the original sample. Future researchers
may continue enrolling participants until themes are saturated.
Relatedly, the interviews were designed to be brief so as to
minimally disrupt clinic flow. A more detailed and in-depth inter-
view may have revealed additional complexities and preferences
that did not emerge in this briefer format. Finally, even the bilin-
gual BHCs frequently had experience using interpreters for pa-
tients who spoke languages other than English and Spanish; there-
fore, the emerging themes may have not been unique to
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
57LANGUAGE CONCORDANCE AND ALLIANCE IN IBHC
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
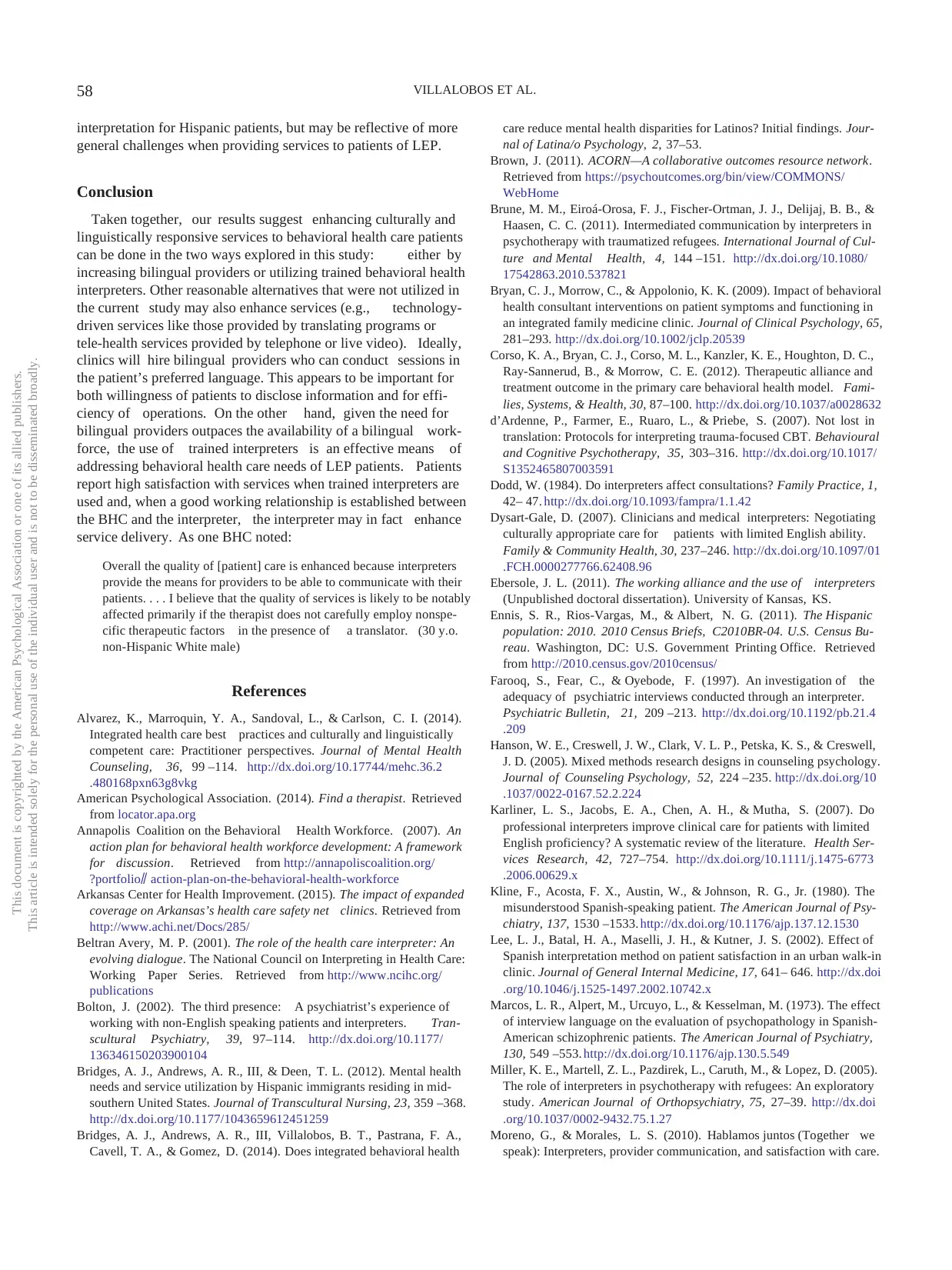
interpretation for Hispanic patients, but may be reflective of more
general challenges when providing services to patients of LEP.
Conclusion
Taken together, our results suggest enhancing culturally and
linguistically responsive services to behavioral health care patients
can be done in the two ways explored in this study: either by
increasing bilingual providers or utilizing trained behavioral health
interpreters. Other reasonable alternatives that were not utilized in
the current study may also enhance services (e.g., technology-
driven services like those provided by translating programs or
tele-health services provided by telephone or live video). Ideally,
clinics will hire bilingual providers who can conduct sessions in
the patient’s preferred language. This appears to be important for
both willingness of patients to disclose information and for effi-
ciency of operations. On the other hand, given the need for
bilingual providers outpaces the availability of a bilingual work-
force, the use of trained interpreters is an effective means of
addressing behavioral health care needs of LEP patients. Patients
report high satisfaction with services when trained interpreters are
used and, when a good working relationship is established between
the BHC and the interpreter, the interpreter may in fact enhance
service delivery. As one BHC noted:
Overall the quality of [patient] care is enhanced because interpreters
provide the means for providers to be able to communicate with their
patients. . . . I believe that the quality of services is likely to be notably
affected primarily if the therapist does not carefully employ nonspe-
cific therapeutic factors in the presence of a translator. (30 y.o.
non-Hispanic White male)
References
Alvarez, K., Marroquin, Y. A., Sandoval, L., & Carlson, C. I. (2014).
Integrated health care best practices and culturally and linguistically
competent care: Practitioner perspectives. Journal of Mental Health
Counseling, 36, 99 –114. http://dx.doi.org/10.17744/mehc.36.2
.480168pxn63g8vkg
American Psychological Association. (2014). Find a therapist. Retrieved
from locator.apa.org
Annapolis Coalition on the Behavioral Health Workforce. (2007). An
action plan for behavioral health workforce development: A framework
for discussion. Retrieved from http://annapoliscoalition.org/
?portfolio⫽ action-plan-on-the-behavioral-health-workforce
Arkansas Center for Health Improvement. (2015). The impact of expanded
coverage on Arkansas’s health care safety net clinics. Retrieved from
http://www.achi.net/Docs/285/
Beltran Avery, M. P. (2001). The role of the health care interpreter: An
evolving dialogue. The National Council on Interpreting in Health Care:
Working Paper Series. Retrieved from http://www.ncihc.org/
publications
Bolton, J. (2002). The third presence: A psychiatrist’s experience of
working with non-English speaking patients and interpreters. Tran-
scultural Psychiatry, 39, 97–114. http://dx.doi.org/10.1177/
136346150203900104
Bridges, A. J., Andrews, A. R., III, & Deen, T. L. (2012). Mental health
needs and service utilization by Hispanic immigrants residing in mid-
southern United States. Journal of Transcultural Nursing, 23, 359 –368.
http://dx.doi.org/10.1177/1043659612451259
Bridges, A. J., Andrews, A. R., III, Villalobos, B. T., Pastrana, F. A.,
Cavell, T. A., & Gomez, D. (2014). Does integrated behavioral health
care reduce mental health disparities for Latinos? Initial findings. Jour-
nal of Latina/o Psychology, 2, 37–53.
Brown, J. (2011). ACORN—A collaborative outcomes resource network.
Retrieved from https://psychoutcomes.org/bin/view/COMMONS/
WebHome
Brune, M. M., Eiroá-Orosa, F. J., Fischer-Ortman, J. J., Delijaj, B. B., &
Haasen, C. C. (2011). Intermediated communication by interpreters in
psychotherapy with traumatized refugees. International Journal of Cul-
ture and Mental Health, 4, 144 –151. http://dx.doi.org/10.1080/
17542863.2010.537821
Bryan, C. J., Morrow, C., & Appolonio, K. K. (2009). Impact of behavioral
health consultant interventions on patient symptoms and functioning in
an integrated family medicine clinic. Journal of Clinical Psychology, 65,
281–293. http://dx.doi.org/10.1002/jclp.20539
Corso, K. A., Bryan, C. J., Corso, M. L., Kanzler, K. E., Houghton, D. C.,
Ray-Sannerud, B., & Morrow, C. E. (2012). Therapeutic alliance and
treatment outcome in the primary care behavioral health model. Fami-
lies, Systems, & Health, 30, 87–100. http://dx.doi.org/10.1037/a0028632
d’Ardenne, P., Farmer, E., Ruaro, L., & Priebe, S. (2007). Not lost in
translation: Protocols for interpreting trauma-focused CBT. Behavioural
and Cognitive Psychotherapy, 35, 303–316. http://dx.doi.org/10.1017/
S1352465807003591
Dodd, W. (1984). Do interpreters affect consultations? Family Practice, 1,
42– 47. http://dx.doi.org/10.1093/fampra/1.1.42
Dysart-Gale, D. (2007). Clinicians and medical interpreters: Negotiating
culturally appropriate care for patients with limited English ability.
Family & Community Health, 30, 237–246. http://dx.doi.org/10.1097/01
.FCH.0000277766.62408.96
Ebersole, J. L. (2011). The working alliance and the use of interpreters
(Unpublished doctoral dissertation). University of Kansas, KS.
Ennis, S. R., Rios-Vargas, M., & Albert, N. G. (2011). The Hispanic
population: 2010. 2010 Census Briefs, C2010BR-04. U.S. Census Bu-
reau. Washington, DC: U.S. Government Printing Office. Retrieved
from http://2010.census.gov/2010census/
Farooq, S., Fear, C., & Oyebode, F. (1997). An investigation of the
adequacy of psychiatric interviews conducted through an interpreter.
Psychiatric Bulletin, 21, 209 –213. http://dx.doi.org/10.1192/pb.21.4
.209
Hanson, W. E., Creswell, J. W., Clark, V. L. P., Petska, K. S., & Creswell,
J. D. (2005). Mixed methods research designs in counseling psychology.
Journal of Counseling Psychology, 52, 224 –235. http://dx.doi.org/10
.1037/0022-0167.52.2.224
Karliner, L. S., Jacobs, E. A., Chen, A. H., & Mutha, S. (2007). Do
professional interpreters improve clinical care for patients with limited
English proficiency? A systematic review of the literature. Health Ser-
vices Research, 42, 727–754. http://dx.doi.org/10.1111/j.1475-6773
.2006.00629.x
Kline, F., Acosta, F. X., Austin, W., & Johnson, R. G., Jr. (1980). The
misunderstood Spanish-speaking patient. The American Journal of Psy-
chiatry, 137, 1530 –1533. http://dx.doi.org/10.1176/ajp.137.12.1530
Lee, L. J., Batal, H. A., Maselli, J. H., & Kutner, J. S. (2002). Effect of
Spanish interpretation method on patient satisfaction in an urban walk-in
clinic. Journal of General Internal Medicine, 17, 641– 646. http://dx.doi
.org/10.1046/j.1525-1497.2002.10742.x
Marcos, L. R., Alpert, M., Urcuyo, L., & Kesselman, M. (1973). The effect
of interview language on the evaluation of psychopathology in Spanish-
American schizophrenic patients. The American Journal of Psychiatry,
130, 549 –553. http://dx.doi.org/10.1176/ajp.130.5.549
Miller, K. E., Martell, Z. L., Pazdirek, L., Caruth, M., & Lopez, D. (2005).
The role of interpreters in psychotherapy with refugees: An exploratory
study. American Journal of Orthopsychiatry, 75, 27–39. http://dx.doi
.org/10.1037/0002-9432.75.1.27
Moreno, G., & Morales, L. S. (2010). Hablamos juntos (Together we
speak): Interpreters, provider communication, and satisfaction with care.
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
58 VILLALOBOS ET AL.
general challenges when providing services to patients of LEP.
Conclusion
Taken together, our results suggest enhancing culturally and
linguistically responsive services to behavioral health care patients
can be done in the two ways explored in this study: either by
increasing bilingual providers or utilizing trained behavioral health
interpreters. Other reasonable alternatives that were not utilized in
the current study may also enhance services (e.g., technology-
driven services like those provided by translating programs or
tele-health services provided by telephone or live video). Ideally,
clinics will hire bilingual providers who can conduct sessions in
the patient’s preferred language. This appears to be important for
both willingness of patients to disclose information and for effi-
ciency of operations. On the other hand, given the need for
bilingual providers outpaces the availability of a bilingual work-
force, the use of trained interpreters is an effective means of
addressing behavioral health care needs of LEP patients. Patients
report high satisfaction with services when trained interpreters are
used and, when a good working relationship is established between
the BHC and the interpreter, the interpreter may in fact enhance
service delivery. As one BHC noted:
Overall the quality of [patient] care is enhanced because interpreters
provide the means for providers to be able to communicate with their
patients. . . . I believe that the quality of services is likely to be notably
affected primarily if the therapist does not carefully employ nonspe-
cific therapeutic factors in the presence of a translator. (30 y.o.
non-Hispanic White male)
References
Alvarez, K., Marroquin, Y. A., Sandoval, L., & Carlson, C. I. (2014).
Integrated health care best practices and culturally and linguistically
competent care: Practitioner perspectives. Journal of Mental Health
Counseling, 36, 99 –114. http://dx.doi.org/10.17744/mehc.36.2
.480168pxn63g8vkg
American Psychological Association. (2014). Find a therapist. Retrieved
from locator.apa.org
Annapolis Coalition on the Behavioral Health Workforce. (2007). An
action plan for behavioral health workforce development: A framework
for discussion. Retrieved from http://annapoliscoalition.org/
?portfolio⫽ action-plan-on-the-behavioral-health-workforce
Arkansas Center for Health Improvement. (2015). The impact of expanded
coverage on Arkansas’s health care safety net clinics. Retrieved from
http://www.achi.net/Docs/285/
Beltran Avery, M. P. (2001). The role of the health care interpreter: An
evolving dialogue. The National Council on Interpreting in Health Care:
Working Paper Series. Retrieved from http://www.ncihc.org/
publications
Bolton, J. (2002). The third presence: A psychiatrist’s experience of
working with non-English speaking patients and interpreters. Tran-
scultural Psychiatry, 39, 97–114. http://dx.doi.org/10.1177/
136346150203900104
Bridges, A. J., Andrews, A. R., III, & Deen, T. L. (2012). Mental health
needs and service utilization by Hispanic immigrants residing in mid-
southern United States. Journal of Transcultural Nursing, 23, 359 –368.
http://dx.doi.org/10.1177/1043659612451259
Bridges, A. J., Andrews, A. R., III, Villalobos, B. T., Pastrana, F. A.,
Cavell, T. A., & Gomez, D. (2014). Does integrated behavioral health
care reduce mental health disparities for Latinos? Initial findings. Jour-
nal of Latina/o Psychology, 2, 37–53.
Brown, J. (2011). ACORN—A collaborative outcomes resource network.
Retrieved from https://psychoutcomes.org/bin/view/COMMONS/
WebHome
Brune, M. M., Eiroá-Orosa, F. J., Fischer-Ortman, J. J., Delijaj, B. B., &
Haasen, C. C. (2011). Intermediated communication by interpreters in
psychotherapy with traumatized refugees. International Journal of Cul-
ture and Mental Health, 4, 144 –151. http://dx.doi.org/10.1080/
17542863.2010.537821
Bryan, C. J., Morrow, C., & Appolonio, K. K. (2009). Impact of behavioral
health consultant interventions on patient symptoms and functioning in
an integrated family medicine clinic. Journal of Clinical Psychology, 65,
281–293. http://dx.doi.org/10.1002/jclp.20539
Corso, K. A., Bryan, C. J., Corso, M. L., Kanzler, K. E., Houghton, D. C.,
Ray-Sannerud, B., & Morrow, C. E. (2012). Therapeutic alliance and
treatment outcome in the primary care behavioral health model. Fami-
lies, Systems, & Health, 30, 87–100. http://dx.doi.org/10.1037/a0028632
d’Ardenne, P., Farmer, E., Ruaro, L., & Priebe, S. (2007). Not lost in
translation: Protocols for interpreting trauma-focused CBT. Behavioural
and Cognitive Psychotherapy, 35, 303–316. http://dx.doi.org/10.1017/
S1352465807003591
Dodd, W. (1984). Do interpreters affect consultations? Family Practice, 1,
42– 47. http://dx.doi.org/10.1093/fampra/1.1.42
Dysart-Gale, D. (2007). Clinicians and medical interpreters: Negotiating
culturally appropriate care for patients with limited English ability.
Family & Community Health, 30, 237–246. http://dx.doi.org/10.1097/01
.FCH.0000277766.62408.96
Ebersole, J. L. (2011). The working alliance and the use of interpreters
(Unpublished doctoral dissertation). University of Kansas, KS.
Ennis, S. R., Rios-Vargas, M., & Albert, N. G. (2011). The Hispanic
population: 2010. 2010 Census Briefs, C2010BR-04. U.S. Census Bu-
reau. Washington, DC: U.S. Government Printing Office. Retrieved
from http://2010.census.gov/2010census/
Farooq, S., Fear, C., & Oyebode, F. (1997). An investigation of the
adequacy of psychiatric interviews conducted through an interpreter.
Psychiatric Bulletin, 21, 209 –213. http://dx.doi.org/10.1192/pb.21.4
.209
Hanson, W. E., Creswell, J. W., Clark, V. L. P., Petska, K. S., & Creswell,
J. D. (2005). Mixed methods research designs in counseling psychology.
Journal of Counseling Psychology, 52, 224 –235. http://dx.doi.org/10
.1037/0022-0167.52.2.224
Karliner, L. S., Jacobs, E. A., Chen, A. H., & Mutha, S. (2007). Do
professional interpreters improve clinical care for patients with limited
English proficiency? A systematic review of the literature. Health Ser-
vices Research, 42, 727–754. http://dx.doi.org/10.1111/j.1475-6773
.2006.00629.x
Kline, F., Acosta, F. X., Austin, W., & Johnson, R. G., Jr. (1980). The
misunderstood Spanish-speaking patient. The American Journal of Psy-
chiatry, 137, 1530 –1533. http://dx.doi.org/10.1176/ajp.137.12.1530
Lee, L. J., Batal, H. A., Maselli, J. H., & Kutner, J. S. (2002). Effect of
Spanish interpretation method on patient satisfaction in an urban walk-in
clinic. Journal of General Internal Medicine, 17, 641– 646. http://dx.doi
.org/10.1046/j.1525-1497.2002.10742.x
Marcos, L. R., Alpert, M., Urcuyo, L., & Kesselman, M. (1973). The effect
of interview language on the evaluation of psychopathology in Spanish-
American schizophrenic patients. The American Journal of Psychiatry,
130, 549 –553. http://dx.doi.org/10.1176/ajp.130.5.549
Miller, K. E., Martell, Z. L., Pazdirek, L., Caruth, M., & Lopez, D. (2005).
The role of interpreters in psychotherapy with refugees: An exploratory
study. American Journal of Orthopsychiatry, 75, 27–39. http://dx.doi
.org/10.1037/0002-9432.75.1.27
Moreno, G., & Morales, L. S. (2010). Hablamos juntos (Together we
speak): Interpreters, provider communication, and satisfaction with care.
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
58 VILLALOBOS ET AL.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Journal of General Internal Medicine, 25, 1282–1288. http://dx.doi.org/
10.1007/s11606-010-1467-x
National Council on Interpreting in Health Care. (2001). The terminol-
ogy of health care interpreting: A glossary of terms. Working Paper
Series: The National Council on Interpreting in Health Care, 1–10.
Retrieved from https://ncihc.memberclicks.net/assets/documents/
NCIHC%20Terms%20Final080408.pdf
Ngo-Metzger, Q., Sorkin, D. H., Phillips, R. S., Greenfield, S., Massagli,
M. P., Clarridge, B., & Kaplan, S. H. (2007). Providing high-quality care
for limited English proficient patients: The importance of language
concordance and interpreter use. Journal of General Internal Medicine,
22, 324 –330. http://dx.doi.org/10.1007/s11606-007-0340-z
Orlinsky, D. E., Rønnestad, M. H., & Willutzki, U. (2004). Fifty years of
process-outcome research: Continuity and change. In M. J. Lambert
(Ed.), Bergin and Garfield’s handbook of psychotherapy and behavior
change (5th ed., pp. 307–390). New York, NY: Wiley.
Price, C. S., & Cuellar, I. (1981). Effects of language and related variables
on the expression of psychopathology in Mexican American psychiatric
patients. Hispanic Journal of Behavioral Sciences, 3, 145–160.
Raval, H., & Smith, J. A. (2003). Therapists’ experiences of working with
language interpreters. International Journal of Mental Health, 32, 6 –31.
Robinson, P. J., & Reiter, J. T. (2007). Behavioral consultation and
primary care: A guide to integrating services. New York, NY: Springer.
http://dx.doi.org/10.1007/978-0-387-32973-4
Schulz, P. M., Resick, P. A., Huber, L., & Griffin, M. G. (2006). The
effectiveness of cognitive processing therapy for PTSD with refugees in
a community setting. Cognitive and Behavioral Practice, 13, 322–331.
http://dx.doi.org/10.1016/j.cbpra.2006.04.011
Shin, H. B., & Kominski, R. A. (2010). Language use in the United States:
2007. American Community Survey Reports, ACS-12. U.S. Census
Bureau. Washington, DC: U. S. Government Printing Office. Retrieved
from http://www.census.gov/hhes/socdemo/language/
Tribe, R., & Tunariu, A. (2009). Mind your language: Working with
interpreters in healthcare settings and therapeutic encounters. Sexual and
Relationship Therapy, 24, 74 – 84. http://dx.doi.org/10.1080/
14681990802666023
U.S. Census Bureau. (2015). State and county quickfacts. Retrieved from
http://quickfacts.census.gov/qfd/states/05/0560410.html
Received March 6, 2015
Revision received June 25, 2015
Accepted July 10, 2015 䡲
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
59LANGUAGE CONCORDANCE AND ALLIANCE IN IBHC
10.1007/s11606-010-1467-x
National Council on Interpreting in Health Care. (2001). The terminol-
ogy of health care interpreting: A glossary of terms. Working Paper
Series: The National Council on Interpreting in Health Care, 1–10.
Retrieved from https://ncihc.memberclicks.net/assets/documents/
NCIHC%20Terms%20Final080408.pdf
Ngo-Metzger, Q., Sorkin, D. H., Phillips, R. S., Greenfield, S., Massagli,
M. P., Clarridge, B., & Kaplan, S. H. (2007). Providing high-quality care
for limited English proficient patients: The importance of language
concordance and interpreter use. Journal of General Internal Medicine,
22, 324 –330. http://dx.doi.org/10.1007/s11606-007-0340-z
Orlinsky, D. E., Rønnestad, M. H., & Willutzki, U. (2004). Fifty years of
process-outcome research: Continuity and change. In M. J. Lambert
(Ed.), Bergin and Garfield’s handbook of psychotherapy and behavior
change (5th ed., pp. 307–390). New York, NY: Wiley.
Price, C. S., & Cuellar, I. (1981). Effects of language and related variables
on the expression of psychopathology in Mexican American psychiatric
patients. Hispanic Journal of Behavioral Sciences, 3, 145–160.
Raval, H., & Smith, J. A. (2003). Therapists’ experiences of working with
language interpreters. International Journal of Mental Health, 32, 6 –31.
Robinson, P. J., & Reiter, J. T. (2007). Behavioral consultation and
primary care: A guide to integrating services. New York, NY: Springer.
http://dx.doi.org/10.1007/978-0-387-32973-4
Schulz, P. M., Resick, P. A., Huber, L., & Griffin, M. G. (2006). The
effectiveness of cognitive processing therapy for PTSD with refugees in
a community setting. Cognitive and Behavioral Practice, 13, 322–331.
http://dx.doi.org/10.1016/j.cbpra.2006.04.011
Shin, H. B., & Kominski, R. A. (2010). Language use in the United States:
2007. American Community Survey Reports, ACS-12. U.S. Census
Bureau. Washington, DC: U. S. Government Printing Office. Retrieved
from http://www.census.gov/hhes/socdemo/language/
Tribe, R., & Tunariu, A. (2009). Mind your language: Working with
interpreters in healthcare settings and therapeutic encounters. Sexual and
Relationship Therapy, 24, 74 – 84. http://dx.doi.org/10.1080/
14681990802666023
U.S. Census Bureau. (2015). State and county quickfacts. Retrieved from
http://quickfacts.census.gov/qfd/states/05/0560410.html
Received March 6, 2015
Revision received June 25, 2015
Accepted July 10, 2015 䡲
This document is copyrighted by the American Psychological Association or one of its allied publishers.
This article is intended solely for the personal use of the individual user and is not to be disseminated broadly.
59LANGUAGE CONCORDANCE AND ALLIANCE IN IBHC
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





