Critical Analysis: Queensland Maternity and Neonatal Guideline
VerifiedAdded on 2023/04/25
|12
|3544
|379
Report
AI Summary
This report offers a critical analysis of the Queensland Maternity and Neonatal Clinical Guideline for Normal Birth, examining its alignment with Griffith midwifery meta-values. The analysis focuses on key aspects such as woman-centered care, the promotion of normal birth, the social model of care, continuity of midwifery care, culturally safe practices, and the political and reflexive meta-values. The report assesses how the guideline supports these meta-values in the context of maternity and neonatal care, highlighting the importance of evidence-based practice and holistic care throughout the different stages of labor and delivery. The report emphasizes the role of midwives in ensuring positive outcomes for mothers and babies, and the guideline's contribution to improving perinatal consequences. The report also provides insights into the guideline's strengths and weaknesses, and its overall impact on midwifery practice.

Running head: QUEENSLAND MATERNITY AND NEONATAL CLINICAL
GUIDELINE
CRITICAL ANALYSIS OF QUEENSLAND MATERNITY AND NEONATAL
CLINICAL GUIDELINE FOR NORMAL BIRTH
Name of the Student:
Name of the University:
Author Note:
GUIDELINE
CRITICAL ANALYSIS OF QUEENSLAND MATERNITY AND NEONATAL
CLINICAL GUIDELINE FOR NORMAL BIRTH
Name of the Student:
Name of the University:
Author Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1QUEENSLAND MATERNITY AND NEONATAL CLINICAL GUIDELINE
Introduction
Maternity and neonatal care is a crucial aspect of healthcare in Australia. Queensland
Government has published a guideline regarding maternity and neonatal care for normal birth
to help the midwives during their practice and care providing. In this essay, this guideline
will be critically appraised on the basis of Griffith midwifery meta-values. Normal birth can
be defined as a delivery without being managed my clinical interventions. The delivery is
usually safer and the baby is born after the completion of 37th gestational week. The baby
comes out in the vertex position. Generally, the mother and the baby have healthy condition
after the delivery. Protecting, promoting and supporting normal birth through collaborative
woman-centred care is the main objective behind publishing the guideline. Ensuring positive
outcomes for mothers and babies, reducing cost of healthcare during delivery, safeguarding
the wellbeing of mental and physical health of the mother and reducing induced adverse
events during clinical intervention are the aims to achieve during normal birth in the hospital.
The trend of caesarean section is rising in Australia where the complications and cost are
higher. Ensuring proper care to the mother before and during delivery and implantation of a
strategy for all the stages of normal birth will definitely improve the perinatal consequences.
Discussion
Griffith midwifery meta-values are the guiding principal for the midwives working in
the healthcare industry. Acquiring knowledge, way of conducting and serving care to the
mothers are directed by these core principles for a midwife. For a midwife the decision
making, planning of strategy, responding to a problem and communication, collaboration
with other professionals in the health industry are precisely outlined in the meta-values
(Sidebotham et al., 2017).
Introduction
Maternity and neonatal care is a crucial aspect of healthcare in Australia. Queensland
Government has published a guideline regarding maternity and neonatal care for normal birth
to help the midwives during their practice and care providing. In this essay, this guideline
will be critically appraised on the basis of Griffith midwifery meta-values. Normal birth can
be defined as a delivery without being managed my clinical interventions. The delivery is
usually safer and the baby is born after the completion of 37th gestational week. The baby
comes out in the vertex position. Generally, the mother and the baby have healthy condition
after the delivery. Protecting, promoting and supporting normal birth through collaborative
woman-centred care is the main objective behind publishing the guideline. Ensuring positive
outcomes for mothers and babies, reducing cost of healthcare during delivery, safeguarding
the wellbeing of mental and physical health of the mother and reducing induced adverse
events during clinical intervention are the aims to achieve during normal birth in the hospital.
The trend of caesarean section is rising in Australia where the complications and cost are
higher. Ensuring proper care to the mother before and during delivery and implantation of a
strategy for all the stages of normal birth will definitely improve the perinatal consequences.
Discussion
Griffith midwifery meta-values are the guiding principal for the midwives working in
the healthcare industry. Acquiring knowledge, way of conducting and serving care to the
mothers are directed by these core principles for a midwife. For a midwife the decision
making, planning of strategy, responding to a problem and communication, collaboration
with other professionals in the health industry are precisely outlined in the meta-values
(Sidebotham et al., 2017).

2QUEENSLAND MATERNITY AND NEONATAL CLINICAL GUIDELINE
’
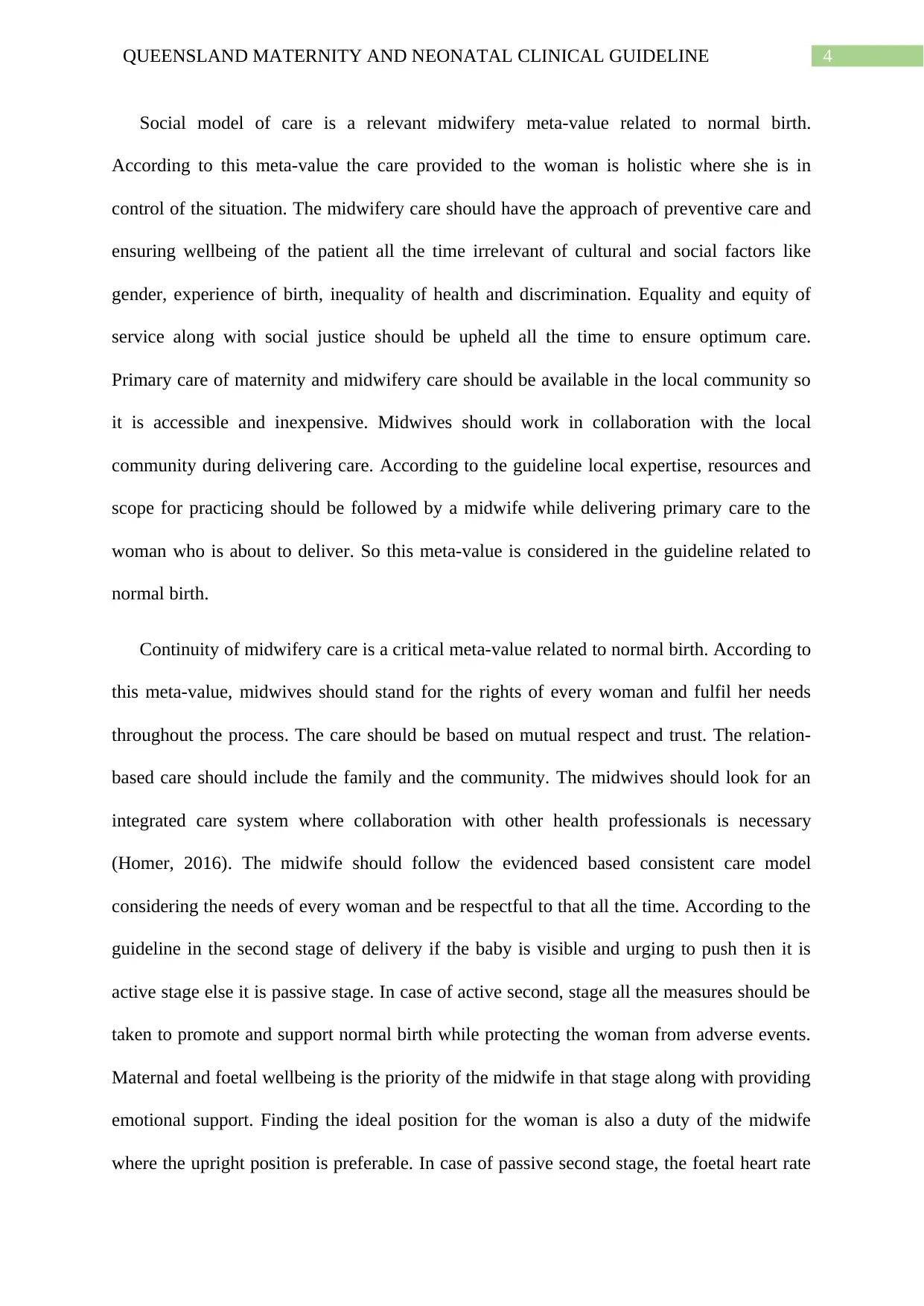
Fig: Midwifery Meta-Values
Woman centred care is the most important meta-value for a midwife during providing
care to a mother during normal delivery. Respecting the belief and value of a woman and
giving priority to the decision making of the woman is the core value of woman centred care.
Responding and reacting to the requirements of the mother is also very crucial. The midwife
should work in a collaborative way with the woman respecting her rights to self-
determination. This will help the woman in self-care for herself and her baby after the
delivery. Midwife should be empathetic to the woman and maintain human rights, gender
equity throughout. Listening to the woman to support her emotionally is also an important
aspect of woman centred care (Renfrew et al., 2014). The clinical guideline by the
Queensland authority has prioritised the woman centred care approach. Verbal
communication where preferences for labour and delivery along with psychological and
emotional aspects is necessary between the pregnant woman and the midwife is important
according to the guidelines. Information about the medical history, maternal health check-up,
wellbeing of the foetus, abdominal assessment of the mother, contraction details, vagina and
’
Fig: Midwifery Meta-Values
Woman centred care is the most important meta-value for a midwife during providing
care to a mother during normal delivery. Respecting the belief and value of a woman and
giving priority to the decision making of the woman is the core value of woman centred care.
Responding and reacting to the requirements of the mother is also very crucial. The midwife
should work in a collaborative way with the woman respecting her rights to self-
determination. This will help the woman in self-care for herself and her baby after the
delivery. Midwife should be empathetic to the woman and maintain human rights, gender
equity throughout. Listening to the woman to support her emotionally is also an important
aspect of woman centred care (Renfrew et al., 2014). The clinical guideline by the
Queensland authority has prioritised the woman centred care approach. Verbal
communication where preferences for labour and delivery along with psychological and
emotional aspects is necessary between the pregnant woman and the midwife is important
according to the guidelines. Information about the medical history, maternal health check-up,
wellbeing of the foetus, abdominal assessment of the mother, contraction details, vagina and
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3QUEENSLAND MATERNITY AND NEONATAL CLINICAL GUIDELINE
vaginal discharge examination and complications regarding maternal health should be
collected to assess the risk factors and set a clinical plan for the health professionals in the
hospitals including the midwife. All the information should be communicated with the
woman and possible clinical interventions should be consulted during all the stages of
delivery. These aspects about the guideline focus on the woman centred midwifery care.
Birth is a physiological event, which is normal and this is a meta-value, which is
significant in terms of normal birth. According to this meta-value, childbirth is a
transformational and emotional journey for a woman where her family is closely involved.
Promoting the normal delivery of baby is important, as it is beneficial for the mother and the
baby related outcomes (Cheyne, Abhyankar & McCourt, 2013). Considering the physical,
mental, emotional, social, religious, spiritual and sexual aspects of birth and providing
holistic care to the woman to ensure her proper health by using basic maternity models of
care is a priority according to this meta-value where midwives play the anchor role as the
primary care provider. In the clinical guideline supportive care promoting normal birth has
been proposed by providing individual midwifery support, making strategies to control pain
and provide comfort, involving professionals to provide mental support, evaluating birth plan,
providing calm and private environment for delivery and ensuring proper mobilisation of the
woman under care. In the first stage if the woman experience painful and regular
contractions, cervical effacement along with 4–6 cm of dilatation then it is active first stage
else it is latent first stage (Carolan-Olah, Kruger & Garvey-Graham, 2015). In both the cases
individual midwifery care is provided, mental, physical, psychological and clinical support is
provided along with an ideal environment. In case of any clinical interventions, the woman is
informed and all the medical examination are done accordingly to avoid any adverse
outcome. Proper clinical settings are also made for both the conditions. These clinical
guidelines do follow the birth is normal meta-value concept.
vaginal discharge examination and complications regarding maternal health should be
collected to assess the risk factors and set a clinical plan for the health professionals in the
hospitals including the midwife. All the information should be communicated with the
woman and possible clinical interventions should be consulted during all the stages of
delivery. These aspects about the guideline focus on the woman centred midwifery care.
Birth is a physiological event, which is normal and this is a meta-value, which is
significant in terms of normal birth. According to this meta-value, childbirth is a
transformational and emotional journey for a woman where her family is closely involved.
Promoting the normal delivery of baby is important, as it is beneficial for the mother and the
baby related outcomes (Cheyne, Abhyankar & McCourt, 2013). Considering the physical,
mental, emotional, social, religious, spiritual and sexual aspects of birth and providing
holistic care to the woman to ensure her proper health by using basic maternity models of
care is a priority according to this meta-value where midwives play the anchor role as the
primary care provider. In the clinical guideline supportive care promoting normal birth has
been proposed by providing individual midwifery support, making strategies to control pain
and provide comfort, involving professionals to provide mental support, evaluating birth plan,
providing calm and private environment for delivery and ensuring proper mobilisation of the
woman under care. In the first stage if the woman experience painful and regular
contractions, cervical effacement along with 4–6 cm of dilatation then it is active first stage
else it is latent first stage (Carolan-Olah, Kruger & Garvey-Graham, 2015). In both the cases
individual midwifery care is provided, mental, physical, psychological and clinical support is
provided along with an ideal environment. In case of any clinical interventions, the woman is
informed and all the medical examination are done accordingly to avoid any adverse
outcome. Proper clinical settings are also made for both the conditions. These clinical
guidelines do follow the birth is normal meta-value concept.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4QUEENSLAND MATERNITY AND NEONATAL CLINICAL GUIDELINE
Social model of care is a relevant midwifery meta-value related to normal birth.
According to this meta-value the care provided to the woman is holistic where she is in
control of the situation. The midwifery care should have the approach of preventive care and
ensuring wellbeing of the patient all the time irrelevant of cultural and social factors like
gender, experience of birth, inequality of health and discrimination. Equality and equity of
service along with social justice should be upheld all the time to ensure optimum care.
Primary care of maternity and midwifery care should be available in the local community so
it is accessible and inexpensive. Midwives should work in collaboration with the local
community during delivering care. According to the guideline local expertise, resources and
scope for practicing should be followed by a midwife while delivering primary care to the
woman who is about to deliver. So this meta-value is considered in the guideline related to
normal birth.
Continuity of midwifery care is a critical meta-value related to normal birth. According to
this meta-value, midwives should stand for the rights of every woman and fulfil her needs
throughout the process. The care should be based on mutual respect and trust. The relation-
based care should include the family and the community. The midwives should look for an
integrated care system where collaboration with other health professionals is necessary
(Homer, 2016). The midwife should follow the evidenced based consistent care model
considering the needs of every woman and be respectful to that all the time. According to the
guideline in the second stage of delivery if the baby is visible and urging to push then it is
active stage else it is passive stage. In case of active second, stage all the measures should be
taken to promote and support normal birth while protecting the woman from adverse events.
Maternal and foetal wellbeing is the priority of the midwife in that stage along with providing
emotional support. Finding the ideal position for the woman is also a duty of the midwife
where the upright position is preferable. In case of passive second stage, the foetal heart rate
Social model of care is a relevant midwifery meta-value related to normal birth.
According to this meta-value the care provided to the woman is holistic where she is in
control of the situation. The midwifery care should have the approach of preventive care and
ensuring wellbeing of the patient all the time irrelevant of cultural and social factors like
gender, experience of birth, inequality of health and discrimination. Equality and equity of
service along with social justice should be upheld all the time to ensure optimum care.
Primary care of maternity and midwifery care should be available in the local community so
it is accessible and inexpensive. Midwives should work in collaboration with the local
community during delivering care. According to the guideline local expertise, resources and
scope for practicing should be followed by a midwife while delivering primary care to the
woman who is about to deliver. So this meta-value is considered in the guideline related to
normal birth.
Continuity of midwifery care is a critical meta-value related to normal birth. According to
this meta-value, midwives should stand for the rights of every woman and fulfil her needs
throughout the process. The care should be based on mutual respect and trust. The relation-
based care should include the family and the community. The midwives should look for an
integrated care system where collaboration with other health professionals is necessary
(Homer, 2016). The midwife should follow the evidenced based consistent care model
considering the needs of every woman and be respectful to that all the time. According to the
guideline in the second stage of delivery if the baby is visible and urging to push then it is
active stage else it is passive stage. In case of active second, stage all the measures should be
taken to promote and support normal birth while protecting the woman from adverse events.
Maternal and foetal wellbeing is the priority of the midwife in that stage along with providing
emotional support. Finding the ideal position for the woman is also a duty of the midwife
where the upright position is preferable. In case of passive second stage, the foetal heart rate
5QUEENSLAND MATERNITY AND NEONATAL CLINICAL GUIDELINE
(FHR) should be monitored in every 15 minutes and differentiated with the heart rate of the
mother. Pushing should be delayed if there is no urge of the woman under care. Other clinical
assessment for the maternal and foetal wellbeing are similar for both the conditions (Page &
Mander, 2014). Regional analgesia, ARM, episiotomy can be considered. Midwives continue
their care to the woman in all the stages of delivery irrespective of the criticality of the
situation (Homer et al, 2019).
After the baby is born, the midwives should continue their care to the mother along with
the newborn baby. They should setup an environment that is ideal for the adaptation of the
baby (Hammond et al., 2013). The mother and the baby should be kept in direct skin contact
for at least an hour without interruption. The midwife should not interrupt without any
emergency between the mother and the baby. They should provide support to breastfeed
according to the choice of the mother. The assessment of health of the mother and baby at the
same time managing and supporting physiological care should be the priority of the midwife.
Ensuring proper diet, rest, environment for recovery and providing primary care to the baby
is the primary responsibility of the midwife (Tracy et al., 2014). Therefore, the clinical
guidelines clearly follows the continuity of midwifery care meta-value as the care continues
throughout all the stages of delivery.
Culturally safe and respectful care is a midwifery meta-value, which effects the
personal relationship with the pregnant woman and her family. As a good relationship
between the caregiver and the client can ensure positive patient related outcome. Adverse
events related to the mother and the baby can be greatly reduced in there is active interaction
and communication between the midwife and the women. Holistic care can only be achieved
if the midwife respects the culture and personal believes of the woman and her family (Lewis,
Jones & Hunter, 2017). The relation between them is strengthened with mutual respect for
each other (Attarha et al., 2016). In the clinical guideline by the Queensland Government
(FHR) should be monitored in every 15 minutes and differentiated with the heart rate of the
mother. Pushing should be delayed if there is no urge of the woman under care. Other clinical
assessment for the maternal and foetal wellbeing are similar for both the conditions (Page &
Mander, 2014). Regional analgesia, ARM, episiotomy can be considered. Midwives continue
their care to the woman in all the stages of delivery irrespective of the criticality of the
situation (Homer et al, 2019).
After the baby is born, the midwives should continue their care to the mother along with
the newborn baby. They should setup an environment that is ideal for the adaptation of the
baby (Hammond et al., 2013). The mother and the baby should be kept in direct skin contact
for at least an hour without interruption. The midwife should not interrupt without any
emergency between the mother and the baby. They should provide support to breastfeed
according to the choice of the mother. The assessment of health of the mother and baby at the
same time managing and supporting physiological care should be the priority of the midwife.
Ensuring proper diet, rest, environment for recovery and providing primary care to the baby
is the primary responsibility of the midwife (Tracy et al., 2014). Therefore, the clinical
guidelines clearly follows the continuity of midwifery care meta-value as the care continues
throughout all the stages of delivery.
Culturally safe and respectful care is a midwifery meta-value, which effects the
personal relationship with the pregnant woman and her family. As a good relationship
between the caregiver and the client can ensure positive patient related outcome. Adverse
events related to the mother and the baby can be greatly reduced in there is active interaction
and communication between the midwife and the women. Holistic care can only be achieved
if the midwife respects the culture and personal believes of the woman and her family (Lewis,
Jones & Hunter, 2017). The relation between them is strengthened with mutual respect for
each other (Attarha et al., 2016). In the clinical guideline by the Queensland Government
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6QUEENSLAND MATERNITY AND NEONATAL CLINICAL GUIDELINE
mentions to consider and respect the cultural aspects and believes of the admitted woman
about to deliver. The guideline suggests that the midwives should be particularly careful
about respecting the different cultural aspects of the woman and her family during the
delivery of primary care. So the guideline follows the meta-value of culturally safe and
respectful care for the midwives.
Political meta-value is important for women empowerment in healthcare industry. In
case of maternity care and normal birth, the midwives play the most important role and that
should be recognised. So promoting the value of midwifery care model is important as they
ensure physical and psychological wellbeing of the women, new born babies and the
associated families for the first thousand days. The meta-value suggests to cleave out all
forms of discrimination against woman who are under the supervision of a midwife
(Koblinsky et al., 2016). When the midwives take the leading role during maternity care and
normal birth, their value is reflected and they can ensure holistic care of the woman admitted
in the hospital. They can also stand up for the needs of the woman. In the guidelines, the
responsibilities of the midwives are clearly highlighted. The midwives play the leading role
in the healthcare of the mother and the newborn baby after successful delivery. They are the
ones who are ensuring positive maternity related outcomes so guidelines follow the meta-
value (Perriman, Davis & Ferguson, 2018).
Critically reflexive meta-value ensures cognitive and reflective practice for the
midwives (Carter, Creedy & Sidebotham, 2017). It encourages the midwives to practice
evidence based and holistic care for the patients especially in maternity care. According to
this meta-value, the midwife needs to consider all the aspects in the working environment,
evaluate the evidences, assess those and plan accordingly to ensure optimal care for the
woman. The clinical guideline focuses on the importance of evidence based practice and
holistic care where physical, cultural, emotional, psychological and spiritual aspects of the
mentions to consider and respect the cultural aspects and believes of the admitted woman
about to deliver. The guideline suggests that the midwives should be particularly careful
about respecting the different cultural aspects of the woman and her family during the
delivery of primary care. So the guideline follows the meta-value of culturally safe and
respectful care for the midwives.
Political meta-value is important for women empowerment in healthcare industry. In
case of maternity care and normal birth, the midwives play the most important role and that
should be recognised. So promoting the value of midwifery care model is important as they
ensure physical and psychological wellbeing of the women, new born babies and the
associated families for the first thousand days. The meta-value suggests to cleave out all
forms of discrimination against woman who are under the supervision of a midwife
(Koblinsky et al., 2016). When the midwives take the leading role during maternity care and
normal birth, their value is reflected and they can ensure holistic care of the woman admitted
in the hospital. They can also stand up for the needs of the woman. In the guidelines, the
responsibilities of the midwives are clearly highlighted. The midwives play the leading role
in the healthcare of the mother and the newborn baby after successful delivery. They are the
ones who are ensuring positive maternity related outcomes so guidelines follow the meta-
value (Perriman, Davis & Ferguson, 2018).
Critically reflexive meta-value ensures cognitive and reflective practice for the
midwives (Carter, Creedy & Sidebotham, 2017). It encourages the midwives to practice
evidence based and holistic care for the patients especially in maternity care. According to
this meta-value, the midwife needs to consider all the aspects in the working environment,
evaluate the evidences, assess those and plan accordingly to ensure optimal care for the
woman. The clinical guideline focuses on the importance of evidence based practice and
holistic care where physical, cultural, emotional, psychological and spiritual aspects of the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7QUEENSLAND MATERNITY AND NEONATAL CLINICAL GUIDELINE
woman should be addressed by the midwife (Toohill et al., 2017). In all the four stages of
normal birth and care the evidenced based care giving have been mentioned and prioritised
(Renfrew et al., 2014). Different measures have been suggested based on the physical
condition and delivery symptom of the mother. So the guideline does follow the critically
reflexive meta-value for midwifery practice.
The guideline published by the Queensland Government regarding the maternity and
neonatal care for normal birth follows all the Griffith meta-values of midwifery. It
encourages delivery of patient centred and holistic care to the women and ensures positive
maternity related outcomes successful delivery with the support of the midwives. Although to
ensure optimum care, the guideline should include all the elements related to standard
practice. Some of the elements of caregiving are solely dependent on the responsibility of the
practitioner which may vary from a person to person. Interventions like application of
precautions before delivery, meeting the legislative requirements, taking consent of all the
stakeholders before delivering care, respecting consumer rights in shared decision-making,
respecting cultural aspects and using local resources in a community and ensuring
communication by any means. As communication between the midwife and the woman is of
optimal importance using an interpreter can be considered (Yelland et al., 2017). The
interpreter can bridge the gap between the mother and the midwife which is crucial (Yelland
et al., 2016). Government can consider enacting laws so that the guideline can be maintained
religiously at the same time training programs can be conducted for the midwives to enhance
their knowledge, skill and efficiency to follow the guidelines (Goemaes et al., 2016). This can
ensure evidenced based, woman centred and holistic practice from the midwife in maternity
care and natural birth.
woman should be addressed by the midwife (Toohill et al., 2017). In all the four stages of
normal birth and care the evidenced based care giving have been mentioned and prioritised
(Renfrew et al., 2014). Different measures have been suggested based on the physical
condition and delivery symptom of the mother. So the guideline does follow the critically
reflexive meta-value for midwifery practice.
The guideline published by the Queensland Government regarding the maternity and
neonatal care for normal birth follows all the Griffith meta-values of midwifery. It
encourages delivery of patient centred and holistic care to the women and ensures positive
maternity related outcomes successful delivery with the support of the midwives. Although to
ensure optimum care, the guideline should include all the elements related to standard
practice. Some of the elements of caregiving are solely dependent on the responsibility of the
practitioner which may vary from a person to person. Interventions like application of
precautions before delivery, meeting the legislative requirements, taking consent of all the
stakeholders before delivering care, respecting consumer rights in shared decision-making,
respecting cultural aspects and using local resources in a community and ensuring
communication by any means. As communication between the midwife and the woman is of
optimal importance using an interpreter can be considered (Yelland et al., 2017). The
interpreter can bridge the gap between the mother and the midwife which is crucial (Yelland
et al., 2016). Government can consider enacting laws so that the guideline can be maintained
religiously at the same time training programs can be conducted for the midwives to enhance
their knowledge, skill and efficiency to follow the guidelines (Goemaes et al., 2016). This can
ensure evidenced based, woman centred and holistic practice from the midwife in maternity
care and natural birth.
8QUEENSLAND MATERNITY AND NEONATAL CLINICAL GUIDELINE
Conclusion
This can be concluded from the essay that the Queensland Government has published
the guidelines to focus on the midwifery practice regarding maternity care and normal birth.
The guideline has been critically appraised on the basis of Griffith midwifery meta-values.
The guideline reflects on all the meta-values related to midwifery practice. Woman centred
care and normal delivery has been encouraged in the guideline. The guideline suggests that
the midwifery practice should also consider the cultural and social background of the woman
and her family and respect that during any kind of clinical interventions. Continuity of care
from the midwife during all the stages of delivery has been suggested in the guideline.
Reflective and cognitive care giving from the midwives and woman empowerment in the
health industry where midwives will take the leading role in maternity care and normal
delivery is the primary outcome of the guideline. All the clinical interventions suggested
related to the mother is purely based on observation of the physical condition and evidences.
So a professional yet woman centred care giving based on reflective decision-making
supported by knowledge is the future of midwifery practice.
Conclusion
This can be concluded from the essay that the Queensland Government has published
the guidelines to focus on the midwifery practice regarding maternity care and normal birth.
The guideline has been critically appraised on the basis of Griffith midwifery meta-values.
The guideline reflects on all the meta-values related to midwifery practice. Woman centred
care and normal delivery has been encouraged in the guideline. The guideline suggests that
the midwifery practice should also consider the cultural and social background of the woman
and her family and respect that during any kind of clinical interventions. Continuity of care
from the midwife during all the stages of delivery has been suggested in the guideline.
Reflective and cognitive care giving from the midwives and woman empowerment in the
health industry where midwives will take the leading role in maternity care and normal
delivery is the primary outcome of the guideline. All the clinical interventions suggested
related to the mother is purely based on observation of the physical condition and evidences.
So a professional yet woman centred care giving based on reflective decision-making
supported by knowledge is the future of midwifery practice.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9QUEENSLAND MATERNITY AND NEONATAL CLINICAL GUIDELINE
References
Attarha, M., Keshavarz, Z., Bakhtiari, M., & Jamilian, M. (2016). The outcome of midwife-
mother relationship in delivery room: a qualitative content analysis. Health, 8(04),
336.
Carolan-Olah, M., Kruger, G., & Garvey-Graham, A. (2015). Midwives׳ experiences of the
factors that facilitate normal birth among low risk women at a public hospital in
Australia. Midwifery, 31(1), 112-121.
Carter, A. G., Creedy, D. K., & Sidebotham, M. (2017). Critical thinking skills in midwifery
practice: Development of a self-assessment tool for students. Midwifery, 50, 184-192.
Cheyne, H., Abhyankar, P., & McCourt, C. (2013). Empowering change: realist evaluation of
a Scottish Government programme to support normal birth. Midwifery, 29(10), 1110-
1121.
Goemaes, R., Beeckman, D., Goossens, J., Shawe, J., Verhaeghe, S., & Van Hecke, A.
(2016). Advanced midwifery practice: An evolutionary concept
analysis. Midwifery, 42, 29-37.
Hammond, A., Foureur, M., Homer, C. S., & Davis, D. (2013). Space, place and the midwife:
exploring the relationship between the birth environment, neurobiology and
midwifery practice. Women and Birth, 26(4), 277-281.
Homer, C. S. (2016). Models of maternity care: evidence for midwifery continuity of
care. Medical Journal of Australia, 205(8), 370-374.
Homer, C., Brodie, P., Sandall, J., & Leap, N. (2019). Midwifery continuity of care. Elsevier.
References
Attarha, M., Keshavarz, Z., Bakhtiari, M., & Jamilian, M. (2016). The outcome of midwife-
mother relationship in delivery room: a qualitative content analysis. Health, 8(04),
336.
Carolan-Olah, M., Kruger, G., & Garvey-Graham, A. (2015). Midwives׳ experiences of the
factors that facilitate normal birth among low risk women at a public hospital in
Australia. Midwifery, 31(1), 112-121.
Carter, A. G., Creedy, D. K., & Sidebotham, M. (2017). Critical thinking skills in midwifery
practice: Development of a self-assessment tool for students. Midwifery, 50, 184-192.
Cheyne, H., Abhyankar, P., & McCourt, C. (2013). Empowering change: realist evaluation of
a Scottish Government programme to support normal birth. Midwifery, 29(10), 1110-
1121.
Goemaes, R., Beeckman, D., Goossens, J., Shawe, J., Verhaeghe, S., & Van Hecke, A.
(2016). Advanced midwifery practice: An evolutionary concept
analysis. Midwifery, 42, 29-37.
Hammond, A., Foureur, M., Homer, C. S., & Davis, D. (2013). Space, place and the midwife:
exploring the relationship between the birth environment, neurobiology and
midwifery practice. Women and Birth, 26(4), 277-281.
Homer, C. S. (2016). Models of maternity care: evidence for midwifery continuity of
care. Medical Journal of Australia, 205(8), 370-374.
Homer, C., Brodie, P., Sandall, J., & Leap, N. (2019). Midwifery continuity of care. Elsevier.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10QUEENSLAND MATERNITY AND NEONATAL CLINICAL GUIDELINE
Koblinsky, M., Moyer, C. A., Calvert, C., Campbell, J., Campbell, O. M., Feigl, A. B., ... &
McDougall, L. (2016). Quality maternity care for every woman, everywhere: a call to
action. The Lancet, 388(10057), 2307-2320.
Lewis, M., Jones, A., & Hunter, B. (2017). Women’s experience of trust within the midwife–
mother relationship. International Journal of Childbirth, 7(1), 40-52.
Page, M., & Mander, R. (2014). Intrapartum uncertainty: a feature of normal birth, as
experienced by midwives in Scotland. Midwifery, 30(1), 28-35.
Perriman, N., Davis, D. L., & Ferguson, S. (2018). What women value in the midwifery
continuity of care model: A systematic review with meta-synthesis. Midwifery, 62,
220-229.
Renfrew, M. J., McFadden, A., Bastos, M. H., Campbell, J., Channon, A. A., Cheung, N.
F., ... & McCormick, F. (2014). Midwifery and quality care: findings from a new
evidence-informed framework for maternal and newborn care. The Lancet, 384(9948),
1129-1145.
Sidebotham, M., Walters, C., Chipperfield, J., & Gamble, J. (2017). Midwifery participatory
curriculum development: Transformation through active partnership. Nurse education
in practice, 25, 5-13.
Toohill, J., Sidebotham, M., Gamble, J., Fenwick, J., & Creedy, D. K. (2017). Factors
influencing midwives' use of an evidenced based Normal Birth Guideline. Women
and birth: journal of the Australian College of Midwives, 30(5), 415-423.
Tracy, S. K., Welsh, A., Hall, B., Hartz, D., Lainchbury, A., Bisits, A., ... & Tracy, M. B.
(2014). Caseload midwifery compared to standard or private obstetric care for first
Koblinsky, M., Moyer, C. A., Calvert, C., Campbell, J., Campbell, O. M., Feigl, A. B., ... &
McDougall, L. (2016). Quality maternity care for every woman, everywhere: a call to
action. The Lancet, 388(10057), 2307-2320.
Lewis, M., Jones, A., & Hunter, B. (2017). Women’s experience of trust within the midwife–
mother relationship. International Journal of Childbirth, 7(1), 40-52.
Page, M., & Mander, R. (2014). Intrapartum uncertainty: a feature of normal birth, as
experienced by midwives in Scotland. Midwifery, 30(1), 28-35.
Perriman, N., Davis, D. L., & Ferguson, S. (2018). What women value in the midwifery
continuity of care model: A systematic review with meta-synthesis. Midwifery, 62,
220-229.
Renfrew, M. J., McFadden, A., Bastos, M. H., Campbell, J., Channon, A. A., Cheung, N.
F., ... & McCormick, F. (2014). Midwifery and quality care: findings from a new
evidence-informed framework for maternal and newborn care. The Lancet, 384(9948),
1129-1145.
Sidebotham, M., Walters, C., Chipperfield, J., & Gamble, J. (2017). Midwifery participatory
curriculum development: Transformation through active partnership. Nurse education
in practice, 25, 5-13.
Toohill, J., Sidebotham, M., Gamble, J., Fenwick, J., & Creedy, D. K. (2017). Factors
influencing midwives' use of an evidenced based Normal Birth Guideline. Women
and birth: journal of the Australian College of Midwives, 30(5), 415-423.
Tracy, S. K., Welsh, A., Hall, B., Hartz, D., Lainchbury, A., Bisits, A., ... & Tracy, M. B.
(2014). Caseload midwifery compared to standard or private obstetric care for first
11QUEENSLAND MATERNITY AND NEONATAL CLINICAL GUIDELINE
time mothers in a public teaching hospital in Australia: a cross sectional study of cost
and birth outcomes. BMC Pregnancy and Childbirth, 14(1), 46.
Yelland, J., Biro, M. A., Dawson, W., Riggs, E., Vanpraag, D., Wigg, K., ... & Brown, S.
(2017). Bridging the language gap: a co-designed quality improvement project to
engage professional interpreters for women duing labour. Australian Health
Review, 41(5), 499-504.
Yelland, J., Riggs, E., Szwarc, J., Casey, S., Duell-Piening, P., Chesters, D., ... & Brown, S.
(2016). Compromised communication: a qualitative study exploring Afghan families
and health professionals’ experience of interpreting support in Australian maternity
care. BMJ Qual Saf, 25(4), e1-e1.
time mothers in a public teaching hospital in Australia: a cross sectional study of cost
and birth outcomes. BMC Pregnancy and Childbirth, 14(1), 46.
Yelland, J., Biro, M. A., Dawson, W., Riggs, E., Vanpraag, D., Wigg, K., ... & Brown, S.
(2017). Bridging the language gap: a co-designed quality improvement project to
engage professional interpreters for women duing labour. Australian Health
Review, 41(5), 499-504.
Yelland, J., Riggs, E., Szwarc, J., Casey, S., Duell-Piening, P., Chesters, D., ... & Brown, S.
(2016). Compromised communication: a qualitative study exploring Afghan families
and health professionals’ experience of interpreting support in Australian maternity
care. BMJ Qual Saf, 25(4), e1-e1.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




