Reflective Journal: Insulin Administration in Patient 7
VerifiedAdded on 2020/05/11
|9
|2430
|4515
Journal and Reflective Writing
AI Summary
This reflective journal details a nursing student's experience administering subcutaneous insulin to a patient with type 1 diabetes post-surgery. The student discusses the assessment of vital signs, the importance of safe medication practices, and the challenges encountered, such as selecting the appropriate injection site due to the patient's recent umbilical hernia surgery. The reflection covers the student's feelings, evaluation of the process, and analysis of relevant factors like insulin types, injection techniques, and the importance of aseptic conditions. The student identifies areas for improvement, including gaining more confidence and proficiency, and outlines an action plan to enhance skills in medication administration, site selection, and maintaining an aseptic environment. The document also references key nursing principles and research related to insulin administration and patient safety, including the six rights of medication administration and the importance of hand hygiene.

Running head: REFLECTION ON INSULIN ADMINISTRATION IN PATIENT
REFLECTION ON INSULIN ADMINISTRATION IN PATIENT
Name of the Student
Name of the university
Author’s note
REFLECTION ON INSULIN ADMINISTRATION IN PATIENT
Name of the Student
Name of the university
Author’s note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1REFLECTION ON INSULIN ADMINISTRATION IN PATIENT
REFLECTION ON INSULIN ADMINISTRATION IN PATIENT
Description
During my nursing placement in a hospital, I got the task of administering subcutaneous
(SC) insulin injection to Oliver Hunter, a 55 year old who underwent a surgery for umbilical
hernia two days ago. I identified the indications for subcutaneous (SC) insulin injection by
reviewing the medication chart for patient. Before administrating the medication, I had to collect
objective data of patient by means of vital sign assessments. His heart rate was 88 beats per
minutes, BP 125/78, temperature 36.4. respiratory rate 18/min and blood glucose level 10.2
ml/mol. Vital sign assessment is essential before and after medication administration according
to safe medication practice to ensure that patient is receiving correct medication for the correct
cause (Holland et al., 2013). By doing the vital sign assessment, I became clear why SC insulin
injection was important for patient. The injection was necessary for him because he had type 1
diabetes, a condition in which body cannot make enough insulin and amount of sugar in blood
cannot be controlled. Insulin injection helps to perform the function of normal insulin and
controls the blood sugar level Steineck et al., 2015)(. However, I faced issue during the
administration of the medication because the patients underwent an umbilical hernia surgey and I
was not sure about the appropriate location to give the injection.
Feeling
As I have never administered insulin injection before in real setting, I was a bit nervous
and doubtful regarding how the whole process will be conducted. However, I tried to recall all
my nursing education regarding safe medication administration safety. These six rights included
right patients, right medication, right dose, right time, right route and right documentation
REFLECTION ON INSULIN ADMINISTRATION IN PATIENT
Description
During my nursing placement in a hospital, I got the task of administering subcutaneous
(SC) insulin injection to Oliver Hunter, a 55 year old who underwent a surgery for umbilical
hernia two days ago. I identified the indications for subcutaneous (SC) insulin injection by
reviewing the medication chart for patient. Before administrating the medication, I had to collect
objective data of patient by means of vital sign assessments. His heart rate was 88 beats per
minutes, BP 125/78, temperature 36.4. respiratory rate 18/min and blood glucose level 10.2
ml/mol. Vital sign assessment is essential before and after medication administration according
to safe medication practice to ensure that patient is receiving correct medication for the correct
cause (Holland et al., 2013). By doing the vital sign assessment, I became clear why SC insulin
injection was important for patient. The injection was necessary for him because he had type 1
diabetes, a condition in which body cannot make enough insulin and amount of sugar in blood
cannot be controlled. Insulin injection helps to perform the function of normal insulin and
controls the blood sugar level Steineck et al., 2015)(. However, I faced issue during the
administration of the medication because the patients underwent an umbilical hernia surgey and I
was not sure about the appropriate location to give the injection.
Feeling
As I have never administered insulin injection before in real setting, I was a bit nervous
and doubtful regarding how the whole process will be conducted. However, I tried to recall all
my nursing education regarding safe medication administration safety. These six rights included
right patients, right medication, right dose, right time, right route and right documentation
2REFLECTION ON INSULIN ADMINISTRATION IN PATIENT
(Adhikari et al., 2014). By recalling these rights, I gained some confidence as I knew that if I
follow all these stages carefully, I can safely administer the injection to patient without causing
any harm. I will evaluate my action in complying to the six rights in the evaluation section.
During the medication administration stage, I was a bit nervous about the site of application of
the insulin, however some critical thinking helped me to solve the dilemma. However, as a
trainee nurse, I was confident regarding the appropriate equipments needed to inject patient and I
followed all the 5 moments of hand hygiene too.
At first I washed my hand with soap and water before administering the injection and
touching the patient.. First I performed an air shot of about 2 to 3 times to remove the air bubbles
from the needle. I was not getting a steady stream so I repeated the procedure until I got a steady
flow (King, 2010). At first I pinched the skin of the thigh and put the needle in at 45 degree angle
to the skin. The person whom I was attending had thick tissues. In such a case I had to inject the
insulin straight up and down at 90 degree angle (Heni et al., 2014). I pushed the plunger to inject
the dose at a relatively slower pace. I kept the patient in the semi fowler position. I disinfected
the area with alcohol. I took the needle and injected all the way to the skin. I kept the syringe in
place for about 5 minutes after the injection (Heni et al., 2014). During the process I found a bit
of blood oozing out, which I wiped off with sterile cotton. After finishing the task I made it sure
that I dispose off the needles. I cleared of the trays with disinfectants to maintain the cleanliness
(Ellingson et al., 2014). After the application, this is how I accomplished the task in 15 minutes
under the supervision of my supervisor.
(Adhikari et al., 2014). By recalling these rights, I gained some confidence as I knew that if I
follow all these stages carefully, I can safely administer the injection to patient without causing
any harm. I will evaluate my action in complying to the six rights in the evaluation section.
During the medication administration stage, I was a bit nervous about the site of application of
the insulin, however some critical thinking helped me to solve the dilemma. However, as a
trainee nurse, I was confident regarding the appropriate equipments needed to inject patient and I
followed all the 5 moments of hand hygiene too.
At first I washed my hand with soap and water before administering the injection and
touching the patient.. First I performed an air shot of about 2 to 3 times to remove the air bubbles
from the needle. I was not getting a steady stream so I repeated the procedure until I got a steady
flow (King, 2010). At first I pinched the skin of the thigh and put the needle in at 45 degree angle
to the skin. The person whom I was attending had thick tissues. In such a case I had to inject the
insulin straight up and down at 90 degree angle (Heni et al., 2014). I pushed the plunger to inject
the dose at a relatively slower pace. I kept the patient in the semi fowler position. I disinfected
the area with alcohol. I took the needle and injected all the way to the skin. I kept the syringe in
place for about 5 minutes after the injection (Heni et al., 2014). During the process I found a bit
of blood oozing out, which I wiped off with sterile cotton. After finishing the task I made it sure
that I dispose off the needles. I cleared of the trays with disinfectants to maintain the cleanliness
(Ellingson et al., 2014). After the application, this is how I accomplished the task in 15 minutes
under the supervision of my supervisor.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3REFLECTION ON INSULIN ADMINISTRATION IN PATIENT
Evaluation
Based on my experience with Oliver Hunt, I can say that I struggled in the fifth right of
the safe medication administration. The other process went smooth. For instance, the first
responsibility for me was to assess whether the medication order matched the patient or not. I did
this by checking the medication chart and asking the patient his name. Once he told me the
name, I was sure that order is for the same patient (Adhikari et al., 2014). Next I followed the
aseptic procedure to touch the medication and match the medication label with the order. I had to
provide SC injection to patient. I also followed appropriate positioning and dosage step to ensure
that the patient was in a comfortable position during the administration. I also verified by time of
administration by asking the patient when he has received the last injection. It is critical to verify
the time interval between insulin injection because delay in injection or using shorter intervals
can lead to complications like hypoglycaemia and other complications. Patients mainly require
two insulin shots and I got to know that Oliver has taken it last night (Tumminia et al., 2015).
Hence, the time was right.
However, I faced major dilemma in deciding the route or site of injection. This is
because has had a surgery for the umbilical hernia and it would not be appropriate to give him
injection in his abdomen. As far as I knew, abdomen was the best route to give insulin injection.
I was just about to give the injection when I suddenly realized it may lead to complications in his
surgery. I had to consult the senior for this dilemma and I found the thighs to be the appropriate
site for administering insulin. Injection sites are mainly chosen based on the presence of fatty
tissue, accessibility and rate of insulin absorption. Thigh was chosen because this site will
minimize any harm done to the surgical site. (Heni et al., 2014). However, injecting the injection
in thigh area was difficult because of less body fat in the area compared to stomach. Normally it
Evaluation
Based on my experience with Oliver Hunt, I can say that I struggled in the fifth right of
the safe medication administration. The other process went smooth. For instance, the first
responsibility for me was to assess whether the medication order matched the patient or not. I did
this by checking the medication chart and asking the patient his name. Once he told me the
name, I was sure that order is for the same patient (Adhikari et al., 2014). Next I followed the
aseptic procedure to touch the medication and match the medication label with the order. I had to
provide SC injection to patient. I also followed appropriate positioning and dosage step to ensure
that the patient was in a comfortable position during the administration. I also verified by time of
administration by asking the patient when he has received the last injection. It is critical to verify
the time interval between insulin injection because delay in injection or using shorter intervals
can lead to complications like hypoglycaemia and other complications. Patients mainly require
two insulin shots and I got to know that Oliver has taken it last night (Tumminia et al., 2015).
Hence, the time was right.
However, I faced major dilemma in deciding the route or site of injection. This is
because has had a surgery for the umbilical hernia and it would not be appropriate to give him
injection in his abdomen. As far as I knew, abdomen was the best route to give insulin injection.
I was just about to give the injection when I suddenly realized it may lead to complications in his
surgery. I had to consult the senior for this dilemma and I found the thighs to be the appropriate
site for administering insulin. Injection sites are mainly chosen based on the presence of fatty
tissue, accessibility and rate of insulin absorption. Thigh was chosen because this site will
minimize any harm done to the surgical site. (Heni et al., 2014). However, injecting the injection
in thigh area was difficult because of less body fat in the area compared to stomach. Normally it
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4REFLECTION ON INSULIN ADMINISTRATION IN PATIENT
was a standard practice to pinch up a layer of the skin at the site of the injection, therefore I
pinched the skin for the application of insulin, but later on as per the feedback from the peers I
came to know that, injecting insulin into the muscle causes faster uptake of insulin that can cause
hyperglycemic risk (King, 2010). We were being taught that normally application of insulin does
not hurt, but if it hurts, then the application must have been in a wrong way. After the
application, I took feedback from the patient and peer nurses, whether the procedures were
alright and whether the patient faced any complication.
Analysis
Type 1 diabetes is normally an autoimmune disease and in general does not have any
relation with umbilical hernia. It’s just the fact that it is essential to get a track of the blood sugar
level as it increases the chance of wound infection after the surgery. A blood sugar level greater
than 140 is associated with wound infection (Freeborn et al., 2013). There are certain factors that
should be kept in mind while the application of insulin, previously the syringes were made up of
glass, which had to be sterilized and there were long surgical needles that had to be reshaped and
resharpened. Nowadays insulin pens are also used. These pens are usable and are easy to use. It
is necessary to prepare the doses of patients as excessive insulin in the circulation may lead to
hyperglycemia (Freeborn et al., 2013). I have already mentioned before regarding the removal of
the air bubbles before the administration of the insulin. I should mention that letting a small
percentage of air with insulin will not be that dangerous because I am applying it to the fat layer,
but a large amount of air in the vein could be dangerous. The injection sites should be rotated as
using a same site over and over again may cause scarring (King, 2010). The timing for taking
insulin should be consistent. It has been found from the researches that fast acting insulin should
be taken before the meals. The hospital environment like the sharps and the trays should be
was a standard practice to pinch up a layer of the skin at the site of the injection, therefore I
pinched the skin for the application of insulin, but later on as per the feedback from the peers I
came to know that, injecting insulin into the muscle causes faster uptake of insulin that can cause
hyperglycemic risk (King, 2010). We were being taught that normally application of insulin does
not hurt, but if it hurts, then the application must have been in a wrong way. After the
application, I took feedback from the patient and peer nurses, whether the procedures were
alright and whether the patient faced any complication.
Analysis
Type 1 diabetes is normally an autoimmune disease and in general does not have any
relation with umbilical hernia. It’s just the fact that it is essential to get a track of the blood sugar
level as it increases the chance of wound infection after the surgery. A blood sugar level greater
than 140 is associated with wound infection (Freeborn et al., 2013). There are certain factors that
should be kept in mind while the application of insulin, previously the syringes were made up of
glass, which had to be sterilized and there were long surgical needles that had to be reshaped and
resharpened. Nowadays insulin pens are also used. These pens are usable and are easy to use. It
is necessary to prepare the doses of patients as excessive insulin in the circulation may lead to
hyperglycemia (Freeborn et al., 2013). I have already mentioned before regarding the removal of
the air bubbles before the administration of the insulin. I should mention that letting a small
percentage of air with insulin will not be that dangerous because I am applying it to the fat layer,
but a large amount of air in the vein could be dangerous. The injection sites should be rotated as
using a same site over and over again may cause scarring (King, 2010). The timing for taking
insulin should be consistent. It has been found from the researches that fast acting insulin should
be taken before the meals. The hospital environment like the sharps and the trays should be
5REFLECTION ON INSULIN ADMINISTRATION IN PATIENT
thoroughly cleaned with disinfectants to prevent any infection. In this whole procedure of 15
minutes, I made sure, that I follow all the parameters mentioned above and act accordingly.
Conclusion
Looking back at the procedures, I thought that I should have been more proficient and faster. I
should have flattened the skin instead of pinching it, as my action could have been risky for my
patient.
Throughout the application process I have tried to maintain an aseptic condition, keeping
in mind, that the patient does not feel any pain. I have also tried to choose the correct site of
injection in the thighs. I have noted the dose prescribed by the doctor before the administration
of the injection. The injection has been given straight at a 90 degree angle. I have also noted to
remove any air bubbles from the syringe. I realized that I need to be more confident to my
practice and should also be supportive to my colleagues, as they helped me out by providing me
with the feed backs and pointing out my flaws after the procedure
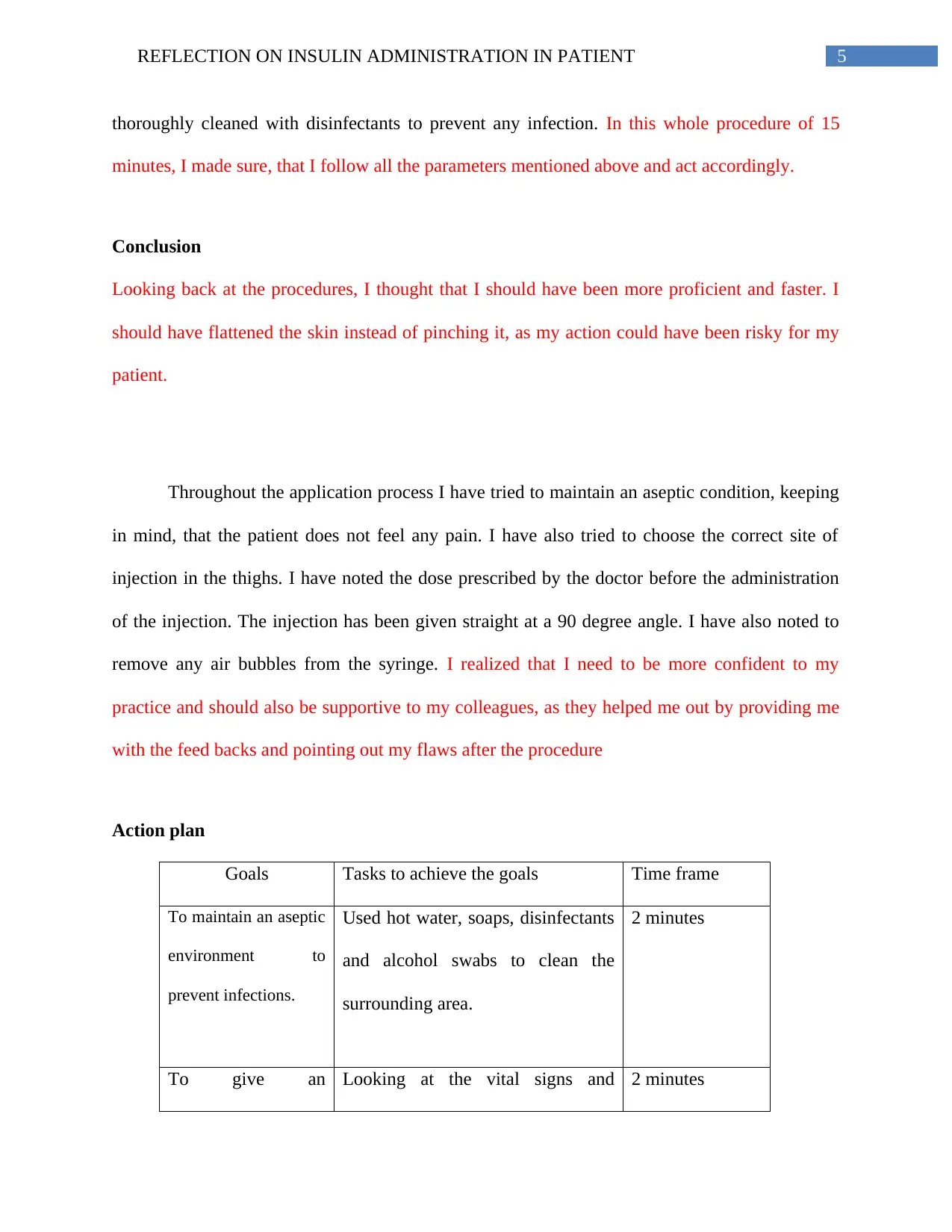
Action plan
Goals Tasks to achieve the goals Time frame
To maintain an aseptic
environment to
prevent infections.
Used hot water, soaps, disinfectants
and alcohol swabs to clean the
surrounding area.
2 minutes
To give an Looking at the vital signs and 2 minutes
thoroughly cleaned with disinfectants to prevent any infection. In this whole procedure of 15
minutes, I made sure, that I follow all the parameters mentioned above and act accordingly.
Conclusion
Looking back at the procedures, I thought that I should have been more proficient and faster. I
should have flattened the skin instead of pinching it, as my action could have been risky for my
patient.
Throughout the application process I have tried to maintain an aseptic condition, keeping
in mind, that the patient does not feel any pain. I have also tried to choose the correct site of
injection in the thighs. I have noted the dose prescribed by the doctor before the administration
of the injection. The injection has been given straight at a 90 degree angle. I have also noted to
remove any air bubbles from the syringe. I realized that I need to be more confident to my
practice and should also be supportive to my colleagues, as they helped me out by providing me
with the feed backs and pointing out my flaws after the procedure
Action plan
Goals Tasks to achieve the goals Time frame
To maintain an aseptic
environment to
prevent infections.
Used hot water, soaps, disinfectants
and alcohol swabs to clean the
surrounding area.
2 minutes
To give an Looking at the vital signs and 2 minutes
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
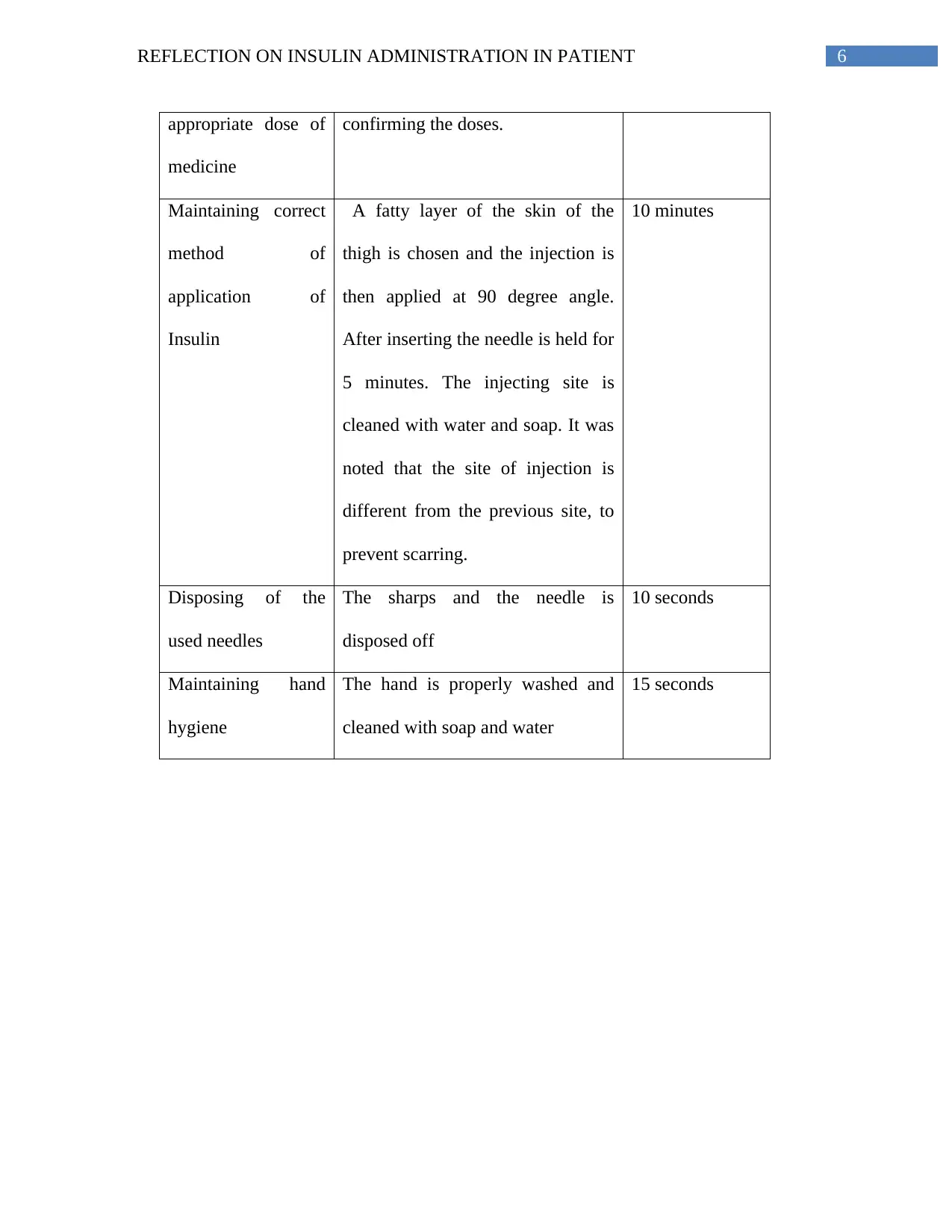
6REFLECTION ON INSULIN ADMINISTRATION IN PATIENT
appropriate dose of
medicine
confirming the doses.
Maintaining correct
method of
application of
Insulin
A fatty layer of the skin of the
thigh is chosen and the injection is
then applied at 90 degree angle.
After inserting the needle is held for
5 minutes. The injecting site is
cleaned with water and soap. It was
noted that the site of injection is
different from the previous site, to
prevent scarring.
10 minutes
Disposing of the
used needles
The sharps and the needle is
disposed off
10 seconds
Maintaining hand
hygiene
The hand is properly washed and
cleaned with soap and water
15 seconds
appropriate dose of
medicine
confirming the doses.
Maintaining correct
method of
application of
Insulin
A fatty layer of the skin of the
thigh is chosen and the injection is
then applied at 90 degree angle.
After inserting the needle is held for
5 minutes. The injecting site is
cleaned with water and soap. It was
noted that the site of injection is
different from the previous site, to
prevent scarring.
10 minutes
Disposing of the
used needles
The sharps and the needle is
disposed off
10 seconds
Maintaining hand
hygiene
The hand is properly washed and
cleaned with soap and water
15 seconds
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

7REFLECTION ON INSULIN ADMINISTRATION IN PATIENT
References
Adhikari, R., Tocher, J., Smith, P., Corcoran, J., & MacArthur, J. (2014). A multi-disciplinary
approach to medication safety and the implication for nursing education and
practice. Nurse education today, 34(2), 185-190.
Ellingson, K., Haas, J. P., Aiello, A. E., Kusek, L., Maragakis, L. L., Olmsted, R. N., ... &
VanAmringe, M. (2014). Strategies to prevent healthcare-associated infections through
hand hygiene. Infection Control & Hospital Epidemiology, 35(8), 937-960.
Freeborn, D., Dyches, T., Roper, S. O., & Mandleco, B. (2013). Identifying challenges of living
with type 1 diabetes: child and youth perspectives. Journal of clinical nursing, 22(13-14),
1890-1898.
Heni, M., Wagner, R., Kullmann, S., Veit, R., Husin, H. M., Linder, K., ... & Preissl, H. (2014).
Central insulin administration improves whole-body insulin sensitivity via hypothalamus
and parasympathetic outputs in men. Diabetes, 63(12), 4083-4088.
Holland, A., Smith, F., McCrossan, G., Adamson, E., Watt, S., & Penny, K. (2013). Online video
in clinical skills education of oral medication administration for undergraduate student
nurses: a mixed methods, prospective cohort study. Nurse Education Today, 33(6), 663-
670.
King, A. (2010). How much do I give? Reevaluation of insulin dosing estimation formulas using
continuous glucose monitoring. Endocrine Practice, 16(3), 428-432.
References
Adhikari, R., Tocher, J., Smith, P., Corcoran, J., & MacArthur, J. (2014). A multi-disciplinary
approach to medication safety and the implication for nursing education and
practice. Nurse education today, 34(2), 185-190.
Ellingson, K., Haas, J. P., Aiello, A. E., Kusek, L., Maragakis, L. L., Olmsted, R. N., ... &
VanAmringe, M. (2014). Strategies to prevent healthcare-associated infections through
hand hygiene. Infection Control & Hospital Epidemiology, 35(8), 937-960.
Freeborn, D., Dyches, T., Roper, S. O., & Mandleco, B. (2013). Identifying challenges of living
with type 1 diabetes: child and youth perspectives. Journal of clinical nursing, 22(13-14),
1890-1898.
Heni, M., Wagner, R., Kullmann, S., Veit, R., Husin, H. M., Linder, K., ... & Preissl, H. (2014).
Central insulin administration improves whole-body insulin sensitivity via hypothalamus
and parasympathetic outputs in men. Diabetes, 63(12), 4083-4088.
Holland, A., Smith, F., McCrossan, G., Adamson, E., Watt, S., & Penny, K. (2013). Online video
in clinical skills education of oral medication administration for undergraduate student
nurses: a mixed methods, prospective cohort study. Nurse Education Today, 33(6), 663-
670.
King, A. (2010). How much do I give? Reevaluation of insulin dosing estimation formulas using
continuous glucose monitoring. Endocrine Practice, 16(3), 428-432.
8REFLECTION ON INSULIN ADMINISTRATION IN PATIENT
Mitchell, V. D., Porter, K., & Beatty, S. J. (2012). Administration technique and storage of
disposable insulin pens reported by patients with diabetes. The Diabetes Educator, 38(5),
651-658.
Nitesh, S. C., Sanjeev, C., Vandana, H., Alka, A., & Vijender, S. (2010). Recent advances in
insulin delivery systems: An update. World Appl Sci J, 11(12), 1552-1556.
Steineck, I., Cederholm, J., Eliasson, B., Rawshani, A., Eeg-Olofsson, K., Svensson, A. M., ... &
Gudbjörnsdóttir, S. (2015). Insulin pump therapy, multiple daily injections, and
cardiovascular mortality in 18 168 people with type 1 diabetes: observational
study. bmj, 350, h3234.
Tumminia, A., Crimi, S., Sciacca, L., Buscema, M., Frittitta, L., Squatrito, S., ... & Tomaselli, L.
(2015). Efficacy of real‐time continuous glucose monitoring on glycaemic control and
glucose variability in type 1 diabetic patients treated with either insulin pumps or
multiple insulin injection therapy: a randomized controlled crossover
trial. Diabetes/metabolism research and reviews, 31(1), 61-68.
Mitchell, V. D., Porter, K., & Beatty, S. J. (2012). Administration technique and storage of
disposable insulin pens reported by patients with diabetes. The Diabetes Educator, 38(5),
651-658.
Nitesh, S. C., Sanjeev, C., Vandana, H., Alka, A., & Vijender, S. (2010). Recent advances in
insulin delivery systems: An update. World Appl Sci J, 11(12), 1552-1556.
Steineck, I., Cederholm, J., Eliasson, B., Rawshani, A., Eeg-Olofsson, K., Svensson, A. M., ... &
Gudbjörnsdóttir, S. (2015). Insulin pump therapy, multiple daily injections, and
cardiovascular mortality in 18 168 people with type 1 diabetes: observational
study. bmj, 350, h3234.
Tumminia, A., Crimi, S., Sciacca, L., Buscema, M., Frittitta, L., Squatrito, S., ... & Tomaselli, L.
(2015). Efficacy of real‐time continuous glucose monitoring on glycaemic control and
glucose variability in type 1 diabetic patients treated with either insulin pumps or
multiple insulin injection therapy: a randomized controlled crossover
trial. Diabetes/metabolism research and reviews, 31(1), 61-68.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.



