Case Study: Melanie Johnson's Renal Failure and Treatment
VerifiedAdded on 2022/10/10
|13
|3738
|70
Case Study
AI Summary
This case study examines the case of Melanie Johnson, a 55-year-old woman diagnosed with chronic renal failure. The assignment details the anatomy and physiology of the renal system, the pathophysiology of renal failure, and the specific risk factors associated with Melanie's condition, including her high blood pressure, low GFR, and elevated serum urea levels. It explores potential complications such as fluid retention and cardiovascular issues, along with treatment options like haemodialysis and medication (Vaisartan and Eprex). The document also compares acute and chronic renal failure, explains the mechanisms of action of Vaisartan and Eprex, discusses the importance of GFR and Hb tests, and outlines nursing considerations for medication administration. Finally, the study addresses the management of chronic renal failure using the 'teach-back' method to educate patients on fluid intake and diet.

Running head: RENAL FAILURE: CASE STUDY
RENAL FAILURE: CASE STUDY
Name of Student:
Name of University:
Author’s Note:
RENAL FAILURE: CASE STUDY
Name of Student:
Name of University:
Author’s Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1RENAL FAILURE: CASE STUDY
Introduction
Part 1.
1.1 Anatomy and physiology of renal
Kidney is the primary organ of the renal system whose major function is filtration and
absorption of water. Kidney is located in the retroperitoneal space in parietal peritoneum
protected by the muscle and fats. The physiology of the renal highlights that the organ is bean
shape and highly vascularized (Chalmers et al., 2019). They are brown in colour and enclosed by
renal capsule which is the hard capsule made up of fibrous connective tissue. The renal organ has
two layer of fats that cushion them. Concerning the internal anatomy, kidney shows three major
section, the outer section renal cortex, renal pelvis and inner region medulla (Glassock & Rule,
2016).
The main functional unit of the renal system is nephron which is masses of tiny tubules,
mainly located in the medulla. The renal cortex gives space for the venules and arterioles and
glomerulus capillaries in order to perfuse the nephron of the kidney. The inner region of the
kidney, medulla consist of renal pyramids which comprises of numerous nephrons. In the cortex
of the kidney, bowman capsule is located at end of each nephron which also contains
glomerulus. Through the capsule PCT, loop Henle, DCT and collecting duct emerge which play
major role in absorption of ions, nutrient and water (Chalmers, 2019).
1.2 Pathophysiology
Renal failure is characterized by the dysfunction of the kidney where the organ is not able
to absorb water and perform ultrafiltration. It cannot maintain optimum level of sodium,
Introduction
Part 1.
1.1 Anatomy and physiology of renal
Kidney is the primary organ of the renal system whose major function is filtration and
absorption of water. Kidney is located in the retroperitoneal space in parietal peritoneum
protected by the muscle and fats. The physiology of the renal highlights that the organ is bean
shape and highly vascularized (Chalmers et al., 2019). They are brown in colour and enclosed by
renal capsule which is the hard capsule made up of fibrous connective tissue. The renal organ has
two layer of fats that cushion them. Concerning the internal anatomy, kidney shows three major
section, the outer section renal cortex, renal pelvis and inner region medulla (Glassock & Rule,
2016).
The main functional unit of the renal system is nephron which is masses of tiny tubules,
mainly located in the medulla. The renal cortex gives space for the venules and arterioles and
glomerulus capillaries in order to perfuse the nephron of the kidney. The inner region of the
kidney, medulla consist of renal pyramids which comprises of numerous nephrons. In the cortex
of the kidney, bowman capsule is located at end of each nephron which also contains
glomerulus. Through the capsule PCT, loop Henle, DCT and collecting duct emerge which play
major role in absorption of ions, nutrient and water (Chalmers, 2019).
1.2 Pathophysiology
Renal failure is characterized by the dysfunction of the kidney where the organ is not able
to absorb water and perform ultrafiltration. It cannot maintain optimum level of sodium,
2RENAL FAILURE: CASE STUDY
haematocrit, potassium, urea, blood pressure and acid-base balance. The pathophysiology of the
renal failure is either due to dysfunction of glomerular or tubular. The renal failure is initiated
with the loss of function of renal tissue. It result in the medullary hypoxia due to absorption of
oxygen by thick ascending limbs and its counter current mechanism (Malek & Nematbakhsh,
2015).
As effect of it, there is high delivery of sodium to the macula densa and high arteriolar
vasoconstriction. This leads to two consequence, the high release of prostaglandin, NO and
Adenosine, and cytoskeletal distortion of the tubular cells. The loss of polarity of the tubular
cells result in loss of local adhesion of the cells. There is sloughing of tubular cells which causes
extensive damage to the tubules (Schefold et al., 2016). Therefore, loss of tubules cells, kidney is
not able to reabsorb water which results in voiding of the large volume of dilute urine which is of
low specific gravity. However, with increase in level of prostaglandin and nitric oxide there is
high amount of blood flow in the medulla and decrease in transport of the fluid to the thick
ascending limb of the renal tubules (Ali et al., 2016). Thus, it also consequently lead to
glomerulus infiltration (glomerulus hypertrophy). All such factor contribute to loss of renal
function and cause renal failure. As the consequence of it there is high amount of urea and toxin
in the blood which lead to huge infection. There is low number of nephron and low renal mass
(Harjola et al., 2017).
Risk factor of Melanie
The major risk factor for Melanie are related with high blood pressure (hypertension),
low GFR and high serum urea level. According to the review of Grams et al. (2016) it was
observed that patient who have high blood pressure contribute to high flow of blood which
happen due to narrowing of the arteries. As the response to it, kidney receives low blood flow
haematocrit, potassium, urea, blood pressure and acid-base balance. The pathophysiology of the
renal failure is either due to dysfunction of glomerular or tubular. The renal failure is initiated
with the loss of function of renal tissue. It result in the medullary hypoxia due to absorption of
oxygen by thick ascending limbs and its counter current mechanism (Malek & Nematbakhsh,
2015).
As effect of it, there is high delivery of sodium to the macula densa and high arteriolar
vasoconstriction. This leads to two consequence, the high release of prostaglandin, NO and
Adenosine, and cytoskeletal distortion of the tubular cells. The loss of polarity of the tubular
cells result in loss of local adhesion of the cells. There is sloughing of tubular cells which causes
extensive damage to the tubules (Schefold et al., 2016). Therefore, loss of tubules cells, kidney is
not able to reabsorb water which results in voiding of the large volume of dilute urine which is of
low specific gravity. However, with increase in level of prostaglandin and nitric oxide there is
high amount of blood flow in the medulla and decrease in transport of the fluid to the thick
ascending limb of the renal tubules (Ali et al., 2016). Thus, it also consequently lead to
glomerulus infiltration (glomerulus hypertrophy). All such factor contribute to loss of renal
function and cause renal failure. As the consequence of it there is high amount of urea and toxin
in the blood which lead to huge infection. There is low number of nephron and low renal mass
(Harjola et al., 2017).
Risk factor of Melanie
The major risk factor for Melanie are related with high blood pressure (hypertension),
low GFR and high serum urea level. According to the review of Grams et al. (2016) it was
observed that patient who have high blood pressure contribute to high flow of blood which
happen due to narrowing of the arteries. As the response to it, kidney receives low blood flow
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3RENAL FAILURE: CASE STUDY
which sent signal of dehydration. Thus, it result in low absorption of the water and ions. Melanie
was reported to have blood pressure of 190/110mm Hg which is the major risk factor of renal
failure. High level of serum urea can increase the toxin level in the blood which is other risk
factor for infection. Low GFR level can result in inefficient absorption of water that lead to high
accumulation of waste material in the bod (Tujios et al., 2015).
Complication
Reviewing the symptom of the patient, she is having high potassium level in the blood
which can result in paralysis, muscle weakness and cardiovascular complication. Other possible
complication of the renal failure that can take place are fluid retention, pulmonary edema, heart
disease and metabolic acidosis (Gavazzi et al., 2016).
Treatment option
As per the current sign and symptom of the Melanie which has shown low GFR, high
serum urea and high potassium, the possible treatment option for her would be renal replacement
therapy which is known as haemodialysis after administering arteriovenous fistula (Liyanage et
al., 2015).
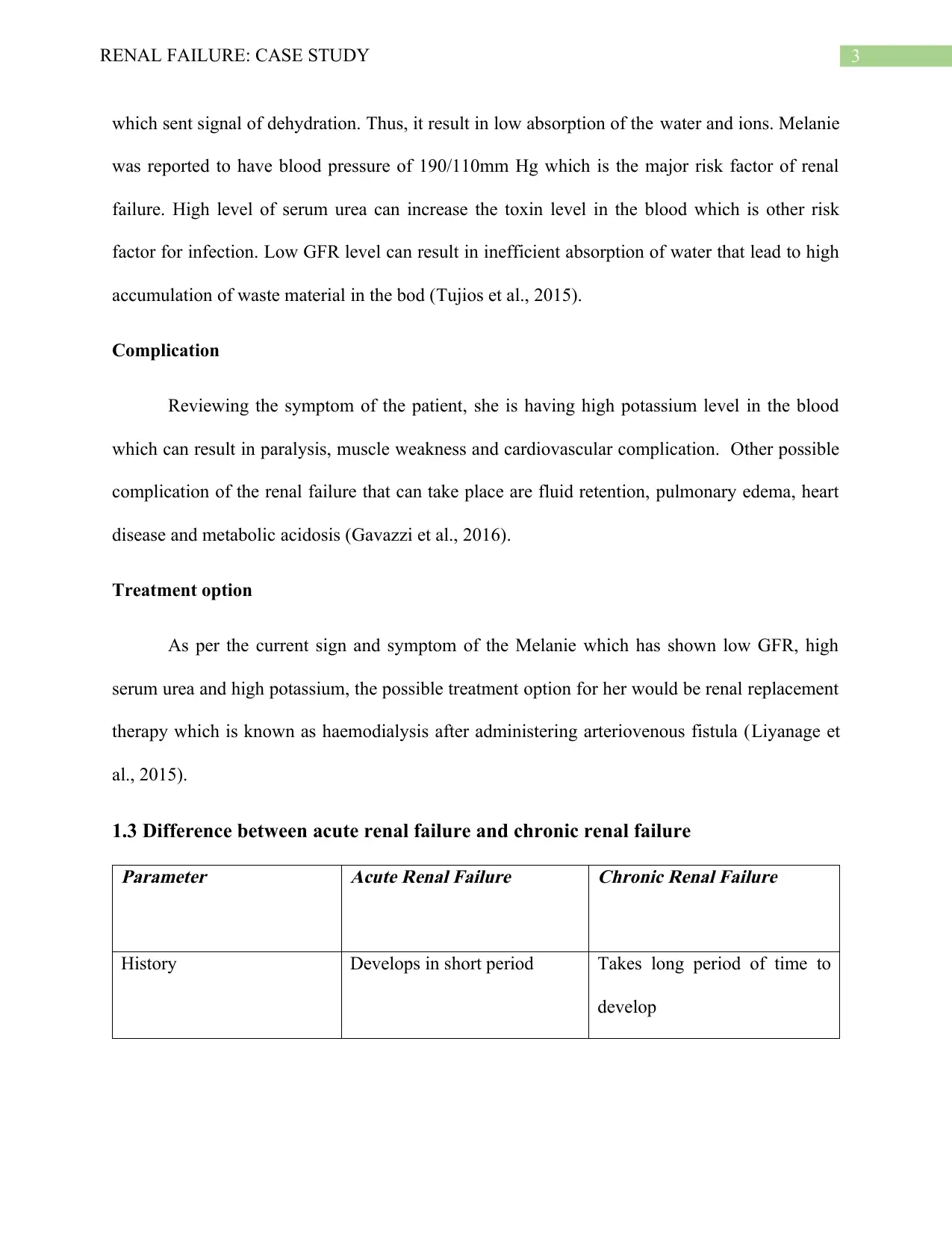
1.3 Difference between acute renal failure and chronic renal failure
Parameter
Acute Renal Failure
Chronic Renal Failure
History Develops in short period Takes long period of time to
develop
which sent signal of dehydration. Thus, it result in low absorption of the water and ions. Melanie
was reported to have blood pressure of 190/110mm Hg which is the major risk factor of renal
failure. High level of serum urea can increase the toxin level in the blood which is other risk
factor for infection. Low GFR level can result in inefficient absorption of water that lead to high
accumulation of waste material in the bod (Tujios et al., 2015).
Complication
Reviewing the symptom of the patient, she is having high potassium level in the blood
which can result in paralysis, muscle weakness and cardiovascular complication. Other possible
complication of the renal failure that can take place are fluid retention, pulmonary edema, heart
disease and metabolic acidosis (Gavazzi et al., 2016).
Treatment option
As per the current sign and symptom of the Melanie which has shown low GFR, high
serum urea and high potassium, the possible treatment option for her would be renal replacement
therapy which is known as haemodialysis after administering arteriovenous fistula (Liyanage et
al., 2015).
1.3 Difference between acute renal failure and chronic renal failure
Parameter
Acute Renal Failure
Chronic Renal Failure
History Develops in short period Takes long period of time to
develop
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4RENAL FAILURE: CASE STUDY
Concentration of
haemoglobin
Has normal level Has low level
Size of renal organ Has normal size Has reduced size
Cause Infection, wound, accident Hypertension, dysfunction of
renal tubules (Webster et al.,
2017).
Treatment Special diet, temporary
dialysis and fluid restriction
Haemodialysis, kidney
transplant.
Action Reversible. The function of
kidney can be brought back to
normal (Hoste et al., 2015).
Irreversible. Treatment gives
temporary relieve.
1.4 Renal replacement therapy (Haemodialysis)
Renal replacement therapy is done to replace the nonendocrine function of kidney who is
reported to have renal failure. The most common is haemodialysis. In the case of Melanie, she
has been shown the sign of low GFR, high serum urea and high potassium, indicate that kidney
is not able to filter the water and perform its normal function. In account of that haemodialysis is
given to bring the process of filtration to normal (Robinson et al., 2016). Haemodialysis is the
process which purify the blood of the patient by the help of haemodialysis machine. It also
remove the waste of the body such as creatinine and urea. It can be said in Haemodialysis, the
function of kidney is performed by the machine (Gilbert et al., 2018). In the process the patient
blood is transferred to the dialyzer which has two compartment attached as hollow fibre tubes
which is sandwiched by semipermeable membrane. In the first compartment, blood is pumped on
Concentration of
haemoglobin
Has normal level Has low level
Size of renal organ Has normal size Has reduced size
Cause Infection, wound, accident Hypertension, dysfunction of
renal tubules (Webster et al.,
2017).
Treatment Special diet, temporary
dialysis and fluid restriction
Haemodialysis, kidney
transplant.
Action Reversible. The function of
kidney can be brought back to
normal (Hoste et al., 2015).
Irreversible. Treatment gives
temporary relieve.
1.4 Renal replacement therapy (Haemodialysis)
Renal replacement therapy is done to replace the nonendocrine function of kidney who is
reported to have renal failure. The most common is haemodialysis. In the case of Melanie, she
has been shown the sign of low GFR, high serum urea and high potassium, indicate that kidney
is not able to filter the water and perform its normal function. In account of that haemodialysis is
given to bring the process of filtration to normal (Robinson et al., 2016). Haemodialysis is the
process which purify the blood of the patient by the help of haemodialysis machine. It also
remove the waste of the body such as creatinine and urea. It can be said in Haemodialysis, the
function of kidney is performed by the machine (Gilbert et al., 2018). In the process the patient
blood is transferred to the dialyzer which has two compartment attached as hollow fibre tubes
which is sandwiched by semipermeable membrane. In the first compartment, blood is pumped on
5RENAL FAILURE: CASE STUDY
one side of semi-permeable membrane and dialysate is pumped to the other side in opposite
direction. This result in concentration gradient between the blood and crystalloid solutions which
lowers the amount of urea nitrogen, creatinine and remove excess fluid from the patient.
Therefore, the main objective of the process is to correct the electrolyte, remove toxin and
balance the fluid (Mårtensson & Bellomo, 2016).
Part 2.
2.1 Mechanism of vaisartan 80 mg
It is an angiotensin receptor blocker which is majorly used for the treating high blood
pressure. As seen in the case of Melanie, she has been reported to show high blood pressure of
190/110 mm Hg. It is very important in the case of Melanie to bring the blood pressure down to
normal, as high blood pressure can have adverse effect on the kidney function. Therefore, the
drug vaisartan is known to inhibit the pressor effect of angiotensin hormone (Meng & Yu, 2015).
The hormone causes high blood pressure, therefore, the drug help to manage the blood
pressure of the patient. According to the study of Sui, Wei and Wang (2015) the author has
indicated that the drug is beneficial in decreasing the urinary albumin and excretion of protein in
renal failure. Thus, the drug is beneficial for Melanie as kit lower the blood pressure and
simultaneously improve the function of kidney.
Mechanism of eprex 50 IU/kg
Eprex is the known to treat the condition of the anemia in patient suffering from kidney
failure. The medicine is known to contain epoetin alfa protein which has great potential to work
as natural erythropoietin present the human body. Thus, the drug take the function of EPO and
synthesise new red blood cell in haemoglobin deficient people. It is evident from the case study
one side of semi-permeable membrane and dialysate is pumped to the other side in opposite
direction. This result in concentration gradient between the blood and crystalloid solutions which
lowers the amount of urea nitrogen, creatinine and remove excess fluid from the patient.
Therefore, the main objective of the process is to correct the electrolyte, remove toxin and
balance the fluid (Mårtensson & Bellomo, 2016).
Part 2.
2.1 Mechanism of vaisartan 80 mg
It is an angiotensin receptor blocker which is majorly used for the treating high blood
pressure. As seen in the case of Melanie, she has been reported to show high blood pressure of
190/110 mm Hg. It is very important in the case of Melanie to bring the blood pressure down to
normal, as high blood pressure can have adverse effect on the kidney function. Therefore, the
drug vaisartan is known to inhibit the pressor effect of angiotensin hormone (Meng & Yu, 2015).
The hormone causes high blood pressure, therefore, the drug help to manage the blood
pressure of the patient. According to the study of Sui, Wei and Wang (2015) the author has
indicated that the drug is beneficial in decreasing the urinary albumin and excretion of protein in
renal failure. Thus, the drug is beneficial for Melanie as kit lower the blood pressure and
simultaneously improve the function of kidney.
Mechanism of eprex 50 IU/kg
Eprex is the known to treat the condition of the anemia in patient suffering from kidney
failure. The medicine is known to contain epoetin alfa protein which has great potential to work
as natural erythropoietin present the human body. Thus, the drug take the function of EPO and
synthesise new red blood cell in haemoglobin deficient people. It is evident from the case study
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6RENAL FAILURE: CASE STUDY
that Melanie has low haemoglobin level which account to only 90g/l. The Drug is administered
to her with aim to increase the haemoglobin level, which is known to increase the oxygen
carrying capacity and improve medullary hypoxia, which is the condition of kidney failure. It is
seen from the study of Yoon et al. (2017) that people with kidney disease are not able to produce
enough erythropoietin and there is the need to replenish the lost amount in the patient.
Four major side effect of the Vaisartan
1. Difficulty in breathing
2. It can raise the situation of bloody urine and cold sweat
3. Severe headache if taken in very high dose
4. Diarrhoea with cold symptoms (Yorek, 2018).
Four major side effect of Eprex 50 IU/kg
1. Can clot the vascular access site in the people with Haemodialysis.
2. Can lead to swelling of body including face, feet, ankles and legs
3. Has high probability of occurrence of flu like symptoms example dizziness, fever and
headache (Fouda et al., 2018).
4. Can increase the blood pressure when it is administered too quickly.
Nursing consideration for Vaisartan
1. Nurse should be aware about its route of administration as it can have adverse side
effects.
2. Nurse should check the dose size before administration because it is reported that high or
low dose can cause dizziness and leave the patient unconscious.
that Melanie has low haemoglobin level which account to only 90g/l. The Drug is administered
to her with aim to increase the haemoglobin level, which is known to increase the oxygen
carrying capacity and improve medullary hypoxia, which is the condition of kidney failure. It is
seen from the study of Yoon et al. (2017) that people with kidney disease are not able to produce
enough erythropoietin and there is the need to replenish the lost amount in the patient.
Four major side effect of the Vaisartan
1. Difficulty in breathing
2. It can raise the situation of bloody urine and cold sweat
3. Severe headache if taken in very high dose
4. Diarrhoea with cold symptoms (Yorek, 2018).
Four major side effect of Eprex 50 IU/kg
1. Can clot the vascular access site in the people with Haemodialysis.
2. Can lead to swelling of body including face, feet, ankles and legs
3. Has high probability of occurrence of flu like symptoms example dizziness, fever and
headache (Fouda et al., 2018).
4. Can increase the blood pressure when it is administered too quickly.
Nursing consideration for Vaisartan
1. Nurse should be aware about its route of administration as it can have adverse side
effects.
2. Nurse should check the dose size before administration because it is reported that high or
low dose can cause dizziness and leave the patient unconscious.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7RENAL FAILURE: CASE STUDY
3. Nurse need to check the medical history of the patient for allergic complain (Carrington
et al., 2016).
4. Nurse have to review the blood pressure after administration of drug.
Nursing consideration for Eprex 50 IU/kg
1. Nurse should not administer the medicine with benzyl alcohol, as it can cause high blood
pressure.
2. Nurse should not shake the solution, as it can denature the glycoprotein.
3. Nurse need to check the colour of the drug as discoloured product is known to contain
foreign particle (Crathorne et al., 2016).
4. Nurse should be conscious enough to not use the drug with other drug solution.
2.2
The blood test of estimating the glomerular filtration rate is test to detect the functionality
of the kidney. When the kidney function well, it filter out the waste and excess fluid thus the
GFR level is normal to 60ml/min. However, the level is low when kidney is not able to function
filter the waste material (Opotowsky et al., 2017). Thus in case of Melanie, there is very low
GFR which indicate that she is having kidney dysfunction.
The test for Hb is done to detect the amount of Red blood cell and haemoglobin level in
the body. In situation of Melanie, she is having low Hb level which specify that she is deficient
of RBC and HB. It is reviewed from the study of Matysiak et al. (2015) that person having
kidney disease is unable to produce adequate amount of EPO due to which RBC is not able to be
to synthesise in required amount. Thus, this test in Melanie give idea of kidney failure to the
health professionals.
3. Nurse need to check the medical history of the patient for allergic complain (Carrington
et al., 2016).
4. Nurse have to review the blood pressure after administration of drug.
Nursing consideration for Eprex 50 IU/kg
1. Nurse should not administer the medicine with benzyl alcohol, as it can cause high blood
pressure.
2. Nurse should not shake the solution, as it can denature the glycoprotein.
3. Nurse need to check the colour of the drug as discoloured product is known to contain
foreign particle (Crathorne et al., 2016).
4. Nurse should be conscious enough to not use the drug with other drug solution.
2.2
The blood test of estimating the glomerular filtration rate is test to detect the functionality
of the kidney. When the kidney function well, it filter out the waste and excess fluid thus the
GFR level is normal to 60ml/min. However, the level is low when kidney is not able to function
filter the waste material (Opotowsky et al., 2017). Thus in case of Melanie, there is very low
GFR which indicate that she is having kidney dysfunction.
The test for Hb is done to detect the amount of Red blood cell and haemoglobin level in
the body. In situation of Melanie, she is having low Hb level which specify that she is deficient
of RBC and HB. It is reviewed from the study of Matysiak et al. (2015) that person having
kidney disease is unable to produce adequate amount of EPO due to which RBC is not able to be
to synthesise in required amount. Thus, this test in Melanie give idea of kidney failure to the
health professionals.
8RENAL FAILURE: CASE STUDY
2.3 Management of chronic renal failure
Teach back method
It is also known as show-me-method which make use of communication skill of the
health care professional. It is the communication confirmation method which is used by the care
provider to teach the patient about the illness management and ensuring whether the patient has
understood the explanation provider to them (Dinh et a., 2016). The understanding is confirmed
when the patient explains the teaching back to the health care professional. The method not only
analyse the client knowledge but also assess how the health professional has communicated to
the patient. This involve asking to the patient about the instruction given before initiating the
treatment plan in their own words.
I would educate Melanie to manage the fluid intake in relation to her diet. First I will
explain to her about the amount of fluid she needs to take in a day. I will take an active session
where I will provide all the relevant information about the diet plan. I will explain her to avoid
excess fluid intake and teach how to keep check on it. I will explain which food to be taken in
the morning, afternoon and night in addition with which food need to be avoided. After finishing
my part, I will motivate Melanie to revert back and explain whatever I have taught her in own
words. If she is able to do it, it will confirm that she has understood the fluid management
process.
2.3 Management of chronic renal failure
Teach back method
It is also known as show-me-method which make use of communication skill of the
health care professional. It is the communication confirmation method which is used by the care
provider to teach the patient about the illness management and ensuring whether the patient has
understood the explanation provider to them (Dinh et a., 2016). The understanding is confirmed
when the patient explains the teaching back to the health care professional. The method not only
analyse the client knowledge but also assess how the health professional has communicated to
the patient. This involve asking to the patient about the instruction given before initiating the
treatment plan in their own words.
I would educate Melanie to manage the fluid intake in relation to her diet. First I will
explain to her about the amount of fluid she needs to take in a day. I will take an active session
where I will provide all the relevant information about the diet plan. I will explain her to avoid
excess fluid intake and teach how to keep check on it. I will explain which food to be taken in
the morning, afternoon and night in addition with which food need to be avoided. After finishing
my part, I will motivate Melanie to revert back and explain whatever I have taught her in own
words. If she is able to do it, it will confirm that she has understood the fluid management
process.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9RENAL FAILURE: CASE STUDY
Reference
Ali, Z. A., Karimi Galougahi, K., Nazif, T., Maehara, A., Hardy, M. A., Cohen, D. J., ... &
Stone, G. W. (2016). Imaging-and physiology-guided percutaneous coronary intervention
without contrast administration in advanced renal failure: a feasibility, safety, and
outcome study. European heart journal, 37(40), 3090-3095.
Carrington, M. J., Jennings, G. L., Harris, M., Nelson, M., Schlaich, M., Stocks, N. P., ... &
Kurstjens, N. P. (2016). Impact of nurse-mediated management on achieving blood
pressure goal levels in primary care: Insights from the Valsartan Intensified Primary carE
Reduction of Blood Pressure Study. European Journal of Cardiovascular Nursing, 15(6),
409-416.
Chalmers, C. (2019). Applied anatomy and physiology and the renal disease process. Renal
Nursing: Care and Management of People with Kidney Disease, 21-58.
Chalmers, C. (2019). Applied anatomy and physiology and the renal disease process. Renal
Nursing: Care and Management of People with Kidney Disease, 21-58.
Crathorne, L., Huxley, N., Haasova, M., Snowsill, T., Jones-Hughes, T., Hoyle, M., ... & Mujica-
Mota, R. (2016). The effectiveness and cost-effectiveness of erythropoiesis-stimulating
agents (epoetin and darbepoetin) for treating cancer-treatment induced anaemia
(including review of TA142): a systematic review and economic model.
Dinh, T. T. H., Bonner, A., Clark, R., Ramsbotham, J., & Hines, S. (2016). The effectiveness of
the teach-back method on adherence and self-management in health education for people
Reference
Ali, Z. A., Karimi Galougahi, K., Nazif, T., Maehara, A., Hardy, M. A., Cohen, D. J., ... &
Stone, G. W. (2016). Imaging-and physiology-guided percutaneous coronary intervention
without contrast administration in advanced renal failure: a feasibility, safety, and
outcome study. European heart journal, 37(40), 3090-3095.
Carrington, M. J., Jennings, G. L., Harris, M., Nelson, M., Schlaich, M., Stocks, N. P., ... &
Kurstjens, N. P. (2016). Impact of nurse-mediated management on achieving blood
pressure goal levels in primary care: Insights from the Valsartan Intensified Primary carE
Reduction of Blood Pressure Study. European Journal of Cardiovascular Nursing, 15(6),
409-416.
Chalmers, C. (2019). Applied anatomy and physiology and the renal disease process. Renal
Nursing: Care and Management of People with Kidney Disease, 21-58.
Chalmers, C. (2019). Applied anatomy and physiology and the renal disease process. Renal
Nursing: Care and Management of People with Kidney Disease, 21-58.
Crathorne, L., Huxley, N., Haasova, M., Snowsill, T., Jones-Hughes, T., Hoyle, M., ... & Mujica-
Mota, R. (2016). The effectiveness and cost-effectiveness of erythropoiesis-stimulating
agents (epoetin and darbepoetin) for treating cancer-treatment induced anaemia
(including review of TA142): a systematic review and economic model.
Dinh, T. T. H., Bonner, A., Clark, R., Ramsbotham, J., & Hines, S. (2016). The effectiveness of
the teach-back method on adherence and self-management in health education for people
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10RENAL FAILURE: CASE STUDY
with chronic disease: a systematic review. JBI database of systematic reviews and
implementation reports, 14(1), 210-247.
Fouda, A. M., Ashour, R. H., El-Banna, F., Saad, M. A., Mostafa, F. A., & Fouda, M. I. (2018).
Differential Effects of Low-Dose Erythropoietin in Rat Model of Diabetic
Nephropathy. Advances in Medicine and Medical Research, 1(1), 25-33.
Gavazzi, A., de Rino, F., Boveri, M. C., Picozzi, A., & Franceschi, M. (2016). Prevalence of
peripheral nervous system complications after major heart surgery. Neurological
Sciences, 37(2), 205-209.
Gilbert, J., Lovibond, K., Mooney, A., & Dudley, J. (2018). Renal replacement therapy:
summary of NICE guidance. Bmj, 363, k4303.
Glassock, R. J., & Rule, A. D. (2016). Aging and the kidneys: anatomy, physiology and
consequences for defining chronic kidney disease. Nephron, 134(1), 25-29.
Grams, M. E., Sang, Y., Levey, A. S., Matsushita, K., Ballew, S., Chang, A. R., ... & Shalev, V.
(2016). Kidney-failure risk projection for the living kidney-donor candidate. New
England Journal of Medicine, 374(5), 411-421.
Harjola, V. P., Mullens, W., Banaszewski, M., Bauersachs, J., Brunner‐La Rocca, H. P.,
Chioncel, O., ... & Fuhrmann, V. (2017). Organ dysfunction, injury and failure in acute
heart failure: from pathophysiology to diagnosis and management. A review on behalf of
the Acute Heart Failure Committee of the Heart Failure Association (HFA) of the
European Society of Cardiology (ESC). European journal of heart failure, 19(7), 821-
836.
with chronic disease: a systematic review. JBI database of systematic reviews and
implementation reports, 14(1), 210-247.
Fouda, A. M., Ashour, R. H., El-Banna, F., Saad, M. A., Mostafa, F. A., & Fouda, M. I. (2018).
Differential Effects of Low-Dose Erythropoietin in Rat Model of Diabetic
Nephropathy. Advances in Medicine and Medical Research, 1(1), 25-33.
Gavazzi, A., de Rino, F., Boveri, M. C., Picozzi, A., & Franceschi, M. (2016). Prevalence of
peripheral nervous system complications after major heart surgery. Neurological
Sciences, 37(2), 205-209.
Gilbert, J., Lovibond, K., Mooney, A., & Dudley, J. (2018). Renal replacement therapy:
summary of NICE guidance. Bmj, 363, k4303.
Glassock, R. J., & Rule, A. D. (2016). Aging and the kidneys: anatomy, physiology and
consequences for defining chronic kidney disease. Nephron, 134(1), 25-29.
Grams, M. E., Sang, Y., Levey, A. S., Matsushita, K., Ballew, S., Chang, A. R., ... & Shalev, V.
(2016). Kidney-failure risk projection for the living kidney-donor candidate. New
England Journal of Medicine, 374(5), 411-421.
Harjola, V. P., Mullens, W., Banaszewski, M., Bauersachs, J., Brunner‐La Rocca, H. P.,
Chioncel, O., ... & Fuhrmann, V. (2017). Organ dysfunction, injury and failure in acute
heart failure: from pathophysiology to diagnosis and management. A review on behalf of
the Acute Heart Failure Committee of the Heart Failure Association (HFA) of the
European Society of Cardiology (ESC). European journal of heart failure, 19(7), 821-
836.
11RENAL FAILURE: CASE STUDY
Hoste, E. A., Bagshaw, S. M., Bellomo, R., Cely, C. M., Colman, R., Cruz, D. N., ... & Honoré,
P. M. (2015). Epidemiology of acute kidney injury in critically ill patients: the
multinational AKI-EPI study. Intensive care medicine, 41(8), 1411-1423.
Liyanage, T., Ninomiya, T., Jha, V., Neal, B., Patrice, H. M., Okpechi, I., ... & Rodgers, A.
(2015). Worldwide access to treatment for end-stage kidney disease: a systematic
review. The Lancet, 385(9981), 1975-1982.
Malek, M., & Nematbakhsh, M. (2015). Renal ischemia/reperfusion injury; from
pathophysiology to treatment. Journal of renal injury prevention, 4(2), 20.
Mårtensson, J., & Bellomo, R. (2016). Continuous Renal Replacement Therapy Versus
Intermittent Haemodialysis: Impact on Clinical Outcomes. In Reducing Mortality in
Acute Kidney Injury (pp. 43-49). Springer, Cham.
Matysiak, E., Donten, M., Kowalczyk, A., Bystrzejewski, M., Grudzinski, I. P., & Nowicka, A.
M. (2015). A novel type of electrochemical sensor based on ferromagnetic carbon-
encapsulated iron nanoparticles for direct determination of hemoglobin in blood
samples. Biosensors and Bioelectronics, 64, 554-559.
Meng, L., & Yu, Q. (2015). GW26-e2914 A study of the mechanism of valsartan pre-protecting
adriamycin-induced cardiotoxicity. Journal of the American College of
Cardiology, 66(16 Supplement), C96.
Opotowsky, A. R., Baraona, F. R., Mc Causland, F. R., Loukas, B., Landzberg, E., Landzberg,
M. J., ... & Waikar, S. S. (2017). Estimated glomerular filtration rate and urine
biomarkers in patients with single-ventricle Fontan circulation. Heart, 103(6), 434-442.
Hoste, E. A., Bagshaw, S. M., Bellomo, R., Cely, C. M., Colman, R., Cruz, D. N., ... & Honoré,
P. M. (2015). Epidemiology of acute kidney injury in critically ill patients: the
multinational AKI-EPI study. Intensive care medicine, 41(8), 1411-1423.
Liyanage, T., Ninomiya, T., Jha, V., Neal, B., Patrice, H. M., Okpechi, I., ... & Rodgers, A.
(2015). Worldwide access to treatment for end-stage kidney disease: a systematic
review. The Lancet, 385(9981), 1975-1982.
Malek, M., & Nematbakhsh, M. (2015). Renal ischemia/reperfusion injury; from
pathophysiology to treatment. Journal of renal injury prevention, 4(2), 20.
Mårtensson, J., & Bellomo, R. (2016). Continuous Renal Replacement Therapy Versus
Intermittent Haemodialysis: Impact on Clinical Outcomes. In Reducing Mortality in
Acute Kidney Injury (pp. 43-49). Springer, Cham.
Matysiak, E., Donten, M., Kowalczyk, A., Bystrzejewski, M., Grudzinski, I. P., & Nowicka, A.
M. (2015). A novel type of electrochemical sensor based on ferromagnetic carbon-
encapsulated iron nanoparticles for direct determination of hemoglobin in blood
samples. Biosensors and Bioelectronics, 64, 554-559.
Meng, L., & Yu, Q. (2015). GW26-e2914 A study of the mechanism of valsartan pre-protecting
adriamycin-induced cardiotoxicity. Journal of the American College of
Cardiology, 66(16 Supplement), C96.
Opotowsky, A. R., Baraona, F. R., Mc Causland, F. R., Loukas, B., Landzberg, E., Landzberg,
M. J., ... & Waikar, S. S. (2017). Estimated glomerular filtration rate and urine
biomarkers in patients with single-ventricle Fontan circulation. Heart, 103(6), 434-442.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





