Post-Transplant Renal Failure: A Comprehensive Literature Review
VerifiedAdded on 2023/06/04
|13
|4598
|490
Literature Review
AI Summary
This literature review delves into the complexities of renal failure (RF) as a prevalent complication following organ transplantation, examining its association with increased mortality and morbidity. It identifies various risk factors, including pre-existing renal function, demographic characteristics, comorbidities, kidney injury, and the nephrotoxic effects of calcineurin inhibitors (CNIs). The review explores the prevalence of RF among transplant recipients, highlighting the challenges in accurate assessment and the impact of factors like Hepatitis C virus (HCV) and polyomavirus BK infection. It further discusses the development of chronic kidney disease (CKD) post-transplantation and the nephrotoxicity induced by CNIs, emphasizing their effects on kidney function and the importance of preoperative renal assessments. This analysis synthesizes findings from multiple studies to provide a comprehensive understanding of the factors contributing to renal failure and mortality in post-organ transplant patients.
Abstract
Renal Failure (RF) is one of the most prevalent complication which can arises from various
avenues such as heart disease, heart attack, liver failure, dehydration, sepsis, kidney
complications and organ transplants from non renal solid organ transplant due to solid organ
transplant and leads to increased rate of mortality and morbidity. The risks involved entail
influence by many factors which can have direct or indirect impact on pre and post treatment
phases. Risk factors have been shown to contribute to this such as, renal function,
demographics, comorbidity, kidney injury, pre-diagnosis renal function, calcineurin inhibitor
(CNI) and nephrotoxicity. Pharmacokinetic interactions have also been shown to suppressing
the immunity and associated to renal failure medication. This literature review assess these
factors in depth and discusses them establishing literature studies on causes of high mortality
on post organ transplant in renal failure stage.
Abbreviations
RF :Renal Failure
CNI : Calcineurin inhibitor
ICU : Intensive Care Unit
CKD : Chronic Kidney Disease
GFR : Glomerular filtrate rate
HCV : Hepatitis C virus
GI : Gatro intestinal
Renal Failure (RF) is one of the most prevalent complication which can arises from various
avenues such as heart disease, heart attack, liver failure, dehydration, sepsis, kidney
complications and organ transplants from non renal solid organ transplant due to solid organ
transplant and leads to increased rate of mortality and morbidity. The risks involved entail
influence by many factors which can have direct or indirect impact on pre and post treatment
phases. Risk factors have been shown to contribute to this such as, renal function,
demographics, comorbidity, kidney injury, pre-diagnosis renal function, calcineurin inhibitor
(CNI) and nephrotoxicity. Pharmacokinetic interactions have also been shown to suppressing
the immunity and associated to renal failure medication. This literature review assess these
factors in depth and discusses them establishing literature studies on causes of high mortality
on post organ transplant in renal failure stage.
Abbreviations
RF :Renal Failure
CNI : Calcineurin inhibitor
ICU : Intensive Care Unit
CKD : Chronic Kidney Disease
GFR : Glomerular filtrate rate
HCV : Hepatitis C virus
GI : Gatro intestinal
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
Literature Review
1. Introduction
Intensive Care Unit (ICU) usually associated with the care of patient in critical condition
requiring highly specialised care and organ transplant recipients immediately post-surgery are
cared in ICU. Tailored care is essential for these type of patients so that complications such
as RF are minimised and successful recovery.
Chronic Kidney Disease (CKD) often is a common complication which can develop after
organ transplantation. Complications and mortality is increased significantly among patients
diagnosed with CKD and dialysis after post-renal failure. Studies undertaken have shown that
patients having kidney diseases ranging from stage 4 and 5 have a high mortality incidence,
(Cox, 2018). The risk associated with CKD risks include pre, peri and post-re-absorptions
setting and lead to renal failure resulting in increased morbidity and mortality. Various
factors have been shown to have an effect and contribute to the development of CKD such as
recipient demographics, kidneys injury during the preoperative period and long-term
calcineurin inhibitor exposure, (Vincenti et al., 2016).
Advances in immunosuppressant, management of preoperative phase, assessment of
cardiovascular factors and infectious states have been shown to largely account for decreased
rates of mortality incidences among the organ recipients. During the transplanting phase,
renal functionality normally declines with maintaining a slower rate later, (Chawla, Eggers,
Star & Kimmel, 2014).
1.1 Aim
This literature review aims at exploring studies which have been undertaken and published
regarding development of renal failure and mortality trends post organ transplantation.
Specific investigative goals included finding out causes of RF related to different type of
solid organ transplant, complication and recommended care.
2. Methodology
Conducting an analysis in literature studies is crucial aspect of gathering evidences and
resources needed to build a case. Literature review was undertaken using databases such as
Pubmed, CINAHL and Medline using University of Tasmania online library. The key words
used in the searches undertaken included ‘renal failure’, ‘renal organ transplants’, and ‘Renal
Literature Review
1. Introduction
Intensive Care Unit (ICU) usually associated with the care of patient in critical condition
requiring highly specialised care and organ transplant recipients immediately post-surgery are
cared in ICU. Tailored care is essential for these type of patients so that complications such
as RF are minimised and successful recovery.
Chronic Kidney Disease (CKD) often is a common complication which can develop after
organ transplantation. Complications and mortality is increased significantly among patients
diagnosed with CKD and dialysis after post-renal failure. Studies undertaken have shown that
patients having kidney diseases ranging from stage 4 and 5 have a high mortality incidence,
(Cox, 2018). The risk associated with CKD risks include pre, peri and post-re-absorptions
setting and lead to renal failure resulting in increased morbidity and mortality. Various
factors have been shown to have an effect and contribute to the development of CKD such as
recipient demographics, kidneys injury during the preoperative period and long-term
calcineurin inhibitor exposure, (Vincenti et al., 2016).
Advances in immunosuppressant, management of preoperative phase, assessment of
cardiovascular factors and infectious states have been shown to largely account for decreased
rates of mortality incidences among the organ recipients. During the transplanting phase,
renal functionality normally declines with maintaining a slower rate later, (Chawla, Eggers,
Star & Kimmel, 2014).
1.1 Aim
This literature review aims at exploring studies which have been undertaken and published
regarding development of renal failure and mortality trends post organ transplantation.
Specific investigative goals included finding out causes of RF related to different type of
solid organ transplant, complication and recommended care.
2. Methodology
Conducting an analysis in literature studies is crucial aspect of gathering evidences and
resources needed to build a case. Literature review was undertaken using databases such as
Pubmed, CINAHL and Medline using University of Tasmania online library. The key words
used in the searches undertaken included ‘renal failure’, ‘renal organ transplants’, and ‘Renal
10
Literature Review
diseases’. The search strategy used two key themes focusing on the study terms with Boolean
operator, ‘and’. Observational and randomised controlled studies and those relating to
chronic kidney diseases were included. Reviews, editorials and root cause analysis studies
were excluded from the search.
3. Result
Studies searched were reviewed for their content and screened. Duplicate articles were
removed and those addressing CKD were retained. These process yielded 29 relevant articles,
on the second process, 14 articles were further selected after meeting the priori of exclusion
and inclusion criteria.
4. Discussion
4.1 Prevalence of renal failure
Globally more than the 300,000 individuals have received the liver, lungs, intestinal and liver
transplants. An estimate of 20%-25% has often experienced a preoperative acute renal failure
while 10%-15% require renal replacement therapy. Renal failure has been attributed to
increased mortality and premature morbidity of diseases among these patients, (Go, Chertow,
Fan and McCulloch, 2004).
Prevalence rates of nonrenal patients have always ranged between 10-90% as per renal failure
diagnosis criteria. Further, these shortcomings have often emanated from non accurate
assessments which depend on the serum creatinine. Patients who have undergone transplants
have low muscle mass and less creatinine compared to the general populations. Shortcomings
have been observed from larger cohorts using the Iothalamate Glomerular Filtrate Rate
(GFR) measurements which perform 1447 liver transplant on liver candidates and those
which are undertaken through transplantation, (Sandsmark et al., 2015).
Diet modification, serum creatinine and glomerular filtrates have been assessed in renal
failure. Serum and diet modification analysis showed transplantation rates of 1.15mg/dl for
serum creative and mean for ithiolamante GFR being 90.7 ml/min. The usage of the
formulas, the Modification of diet in Renal disease tool is an effective compromise to assess
this, unfortunately other studies have shown that it lacks precisions and offers an
underestimation of renal function among post-transplant patients, (Gordon, Ladner, Caicedo
Literature Review
diseases’. The search strategy used two key themes focusing on the study terms with Boolean
operator, ‘and’. Observational and randomised controlled studies and those relating to
chronic kidney diseases were included. Reviews, editorials and root cause analysis studies
were excluded from the search.
3. Result
Studies searched were reviewed for their content and screened. Duplicate articles were
removed and those addressing CKD were retained. These process yielded 29 relevant articles,
on the second process, 14 articles were further selected after meeting the priori of exclusion
and inclusion criteria.
4. Discussion
4.1 Prevalence of renal failure
Globally more than the 300,000 individuals have received the liver, lungs, intestinal and liver
transplants. An estimate of 20%-25% has often experienced a preoperative acute renal failure
while 10%-15% require renal replacement therapy. Renal failure has been attributed to
increased mortality and premature morbidity of diseases among these patients, (Go, Chertow,
Fan and McCulloch, 2004).
Prevalence rates of nonrenal patients have always ranged between 10-90% as per renal failure
diagnosis criteria. Further, these shortcomings have often emanated from non accurate
assessments which depend on the serum creatinine. Patients who have undergone transplants
have low muscle mass and less creatinine compared to the general populations. Shortcomings
have been observed from larger cohorts using the Iothalamate Glomerular Filtrate Rate
(GFR) measurements which perform 1447 liver transplant on liver candidates and those
which are undertaken through transplantation, (Sandsmark et al., 2015).
Diet modification, serum creatinine and glomerular filtrates have been assessed in renal
failure. Serum and diet modification analysis showed transplantation rates of 1.15mg/dl for
serum creative and mean for ithiolamante GFR being 90.7 ml/min. The usage of the
formulas, the Modification of diet in Renal disease tool is an effective compromise to assess
this, unfortunately other studies have shown that it lacks precisions and offers an
underestimation of renal function among post-transplant patients, (Gordon, Ladner, Caicedo
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
10
Literature Review
& Franklin, 2010).
Mortality associated measure has been undertaken on patients diagnosed with renal failure
undergoing dialysis. This has shown that the patients have GFR of estimated glomerular
filtrate rate between15-29 and <15 ml/min/1.73m2, thus having quantifying relative mortality
of renal. An assessment study in the US on kidney failure patients at stage 4-5, approach
dialysis mortality ratios with threefold and six-fold higher mortality risks higher than
Egfr>60, compared with Swedish incident patients having a CKD stage 4-5 followed for 7
years and high ratio ranging from 3.7 to 7.4 for stage 4 patients, (Schwab , Marwitz &
Woitas, 2018) .
Dialysis mortality trends in a European study showed an eightfold age-standardized mortality
rate linked to cardiovascular and noncardiovascular disease compared to the general
population.
4.2 Factors associated with renal failure end stage mortality
4.2.1 Renal function before transplantation
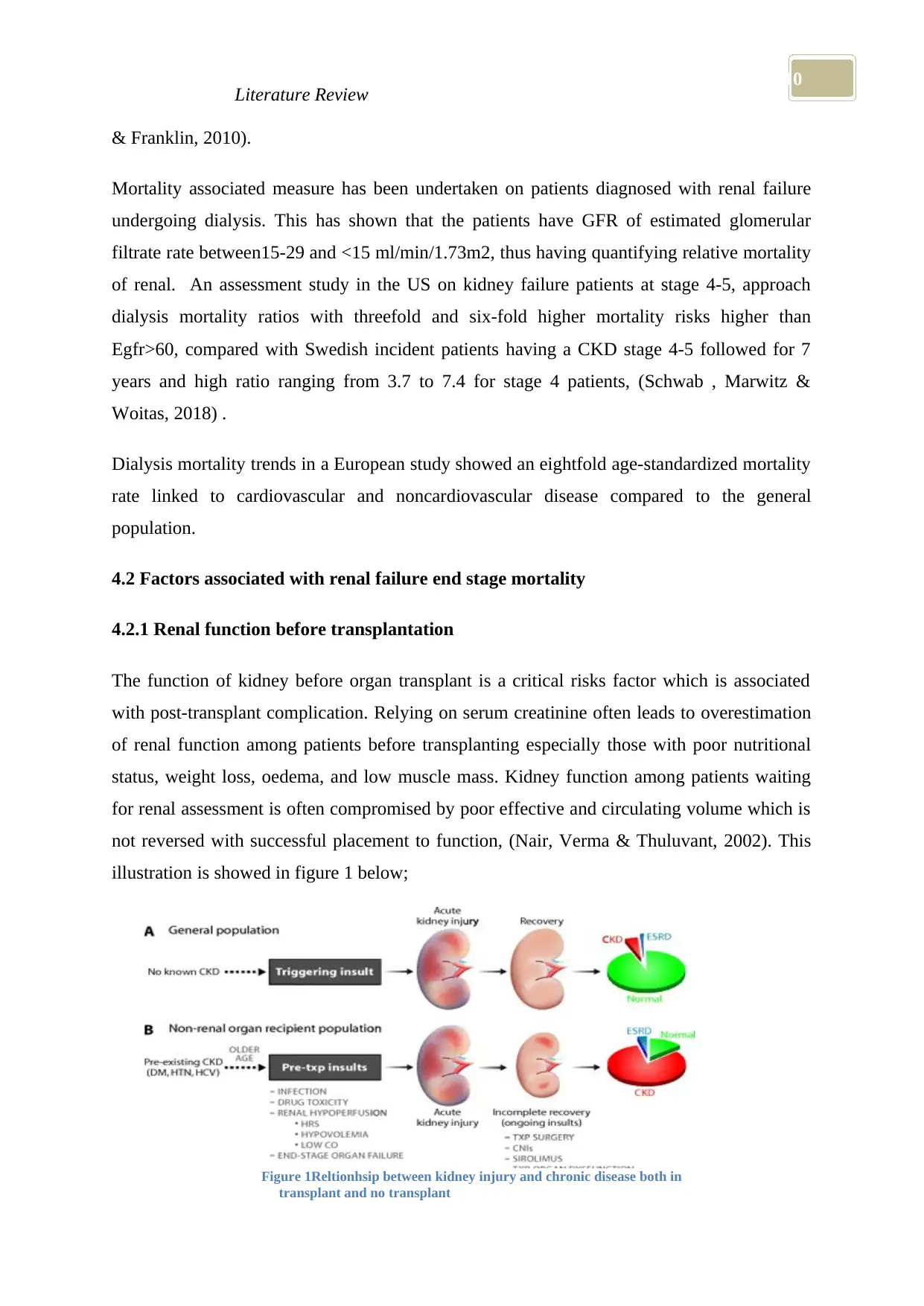
The function of kidney before organ transplant is a critical risks factor which is associated
with post-transplant complication. Relying on serum creatinine often leads to overestimation
of renal function among patients before transplanting especially those with poor nutritional
status, weight loss, oedema, and low muscle mass. Kidney function among patients waiting
for renal assessment is often compromised by poor effective and circulating volume which is
not reversed with successful placement to function, (Nair, Verma & Thuluvant, 2002). This
illustration is showed in figure 1 below;
Figure 1Reltionhsip between kidney injury and chronic disease both in
transplant and no transplant
Literature Review
& Franklin, 2010).
Mortality associated measure has been undertaken on patients diagnosed with renal failure
undergoing dialysis. This has shown that the patients have GFR of estimated glomerular
filtrate rate between15-29 and <15 ml/min/1.73m2, thus having quantifying relative mortality
of renal. An assessment study in the US on kidney failure patients at stage 4-5, approach
dialysis mortality ratios with threefold and six-fold higher mortality risks higher than
Egfr>60, compared with Swedish incident patients having a CKD stage 4-5 followed for 7
years and high ratio ranging from 3.7 to 7.4 for stage 4 patients, (Schwab , Marwitz &
Woitas, 2018) .
Dialysis mortality trends in a European study showed an eightfold age-standardized mortality
rate linked to cardiovascular and noncardiovascular disease compared to the general
population.
4.2 Factors associated with renal failure end stage mortality
4.2.1 Renal function before transplantation
The function of kidney before organ transplant is a critical risks factor which is associated
with post-transplant complication. Relying on serum creatinine often leads to overestimation
of renal function among patients before transplanting especially those with poor nutritional
status, weight loss, oedema, and low muscle mass. Kidney function among patients waiting
for renal assessment is often compromised by poor effective and circulating volume which is
not reversed with successful placement to function, (Nair, Verma & Thuluvant, 2002). This
illustration is showed in figure 1 below;
Figure 1Reltionhsip between kidney injury and chronic disease both in
transplant and no transplant
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
Literature Review
4.2.2 Demographic and comorbid factors
Baseline patient factors and comorbidities have led to mortality risks after the performance of
organ transplant. This is a linked on overestimation of pre-transplantation and attaining renal
function. Further diabetes and commodities have been found as the greatest risks factors
among heart and liver transplant patients elevating increase of renal disease (Stengel, 2018).
Hepatitis C virus (HCV) has been shown to have effects and an important risks factor for
heart and liver organ transplant. Hepatitis C liver cirrhosis is an indication of liver
transplantation. Renal failure risks associated with liver reception of HCV infection is
primarily linked to glomerulonephritis. Renal biopsies demonstrate immune complex GN
among over 80% of the patients. Clinical histology's involving abnormalities linked to liver
and none renal organ has been insufficient. The key importance of recognizing preparation
renal ability has always been underscored through observation of renal transplant leading to
poor post-transplant survival, (Saab et al., 2018).
4.2.3 Preoperative renal insults
Associated kidney infection is always associated with increased risks due to post-
transplantation process. Mechanisms involved during surgery process can precipitate
infection during hypotension and hyperfusion, nephrotoxic agents and ant diuretics. With
heart or lung transplant, the kidney infection can trigger ventricular dysfunction having low
cardiac output and poor output. Transplant dysfunction has also been associated with renal
compensation. In a retrospective study among lung, patients showed that 56% had kidney
infection while 7.7% required analysis, (Karkouti et al., 2015).
4.2.4 Polyomavirus BK infection
Polyomavirus nephropathy has been increasingly important. It has been attributed to causing
of renal injury where the virus functions effectively in contributing renal failure in organ
transplant patients. Cases of biopsy have been shown and described among heart transplant
patients, Papadimitriou et al., (2016).
A study by Funk, Gosert, Comoli, Ginevri, & Hirsch, (2008) has shown that infection has
Literature Review
4.2.2 Demographic and comorbid factors
Baseline patient factors and comorbidities have led to mortality risks after the performance of
organ transplant. This is a linked on overestimation of pre-transplantation and attaining renal
function. Further diabetes and commodities have been found as the greatest risks factors
among heart and liver transplant patients elevating increase of renal disease (Stengel, 2018).
Hepatitis C virus (HCV) has been shown to have effects and an important risks factor for
heart and liver organ transplant. Hepatitis C liver cirrhosis is an indication of liver
transplantation. Renal failure risks associated with liver reception of HCV infection is
primarily linked to glomerulonephritis. Renal biopsies demonstrate immune complex GN
among over 80% of the patients. Clinical histology's involving abnormalities linked to liver
and none renal organ has been insufficient. The key importance of recognizing preparation
renal ability has always been underscored through observation of renal transplant leading to
poor post-transplant survival, (Saab et al., 2018).
4.2.3 Preoperative renal insults
Associated kidney infection is always associated with increased risks due to post-
transplantation process. Mechanisms involved during surgery process can precipitate
infection during hypotension and hyperfusion, nephrotoxic agents and ant diuretics. With
heart or lung transplant, the kidney infection can trigger ventricular dysfunction having low
cardiac output and poor output. Transplant dysfunction has also been associated with renal
compensation. In a retrospective study among lung, patients showed that 56% had kidney
infection while 7.7% required analysis, (Karkouti et al., 2015).
4.2.4 Polyomavirus BK infection
Polyomavirus nephropathy has been increasingly important. It has been attributed to causing
of renal injury where the virus functions effectively in contributing renal failure in organ
transplant patients. Cases of biopsy have been shown and described among heart transplant
patients, Papadimitriou et al., (2016).
A study by Funk, Gosert, Comoli, Ginevri, & Hirsch, (2008) has shown that infection has
10
Literature Review
greater impact on renal failure. Early diagnosis has often been linked to infection including
immune-suppression and mortality was associated with the onset. New analysis and evidence
have linked cause of death among kidney transplants as a grossing tendency to follow up of
kidney transplant patients.
Renal failure often occasioned after orthotropic liver transplant has been observed to be the
common form of complication with an average contribution of 12% -40% linked to worse
outcomes, especially in the renal replacement therapy is needed, (Plafkin et al., 2018).
4.3 Development of chronic kidney disease
The occurrence of non-solid organ transplantation has shown the occurrence of kidney
diseases, which is increasingly becoming prevalent complication among the population. CKD
has been shown to increase and advance immuno-suppressions and the overall preoperative
environment and also factors associated with cardiovascular risk factors coupled infections
complications.
CKD is often associated with enhanced and decreased morbidity and mortality. Factors
related to kidney function and non-renal function transplantation including kidney
functioning evaluation prior to non-renal transplantation affects the transplantation processes.
Assessment of kidney function prior to non-renal organ transplant needs to be a preoperative
rule for kidney function tests, (Boers, Visser, Smith & Fuchs, 2014).
4.4 Nephrotoxicity caused by Calcineurin inhibitors
CNIs have been shown to have an effect on the vasoconstriction which often predisposes the
patient with renal failure symptoms and chronic injury especially when the patients' insults
are present. Calcineurin inhibitors often cause nephrotoxicity in conjunction with
cyclosporine A. While at organ recounts, during the cyclosporine arena, the deep decline of
kidney function has been noted to take place within a period of 6 weeks after transplantation
process. Calcineurin inhibitors have shown to have an association with nephrotoxicity levels
which increase exposure duration and often decrease exposure and limited reversibility.
4.4.1 Effects on the Kidney
Calcineurin inhibitors tend to reduce the reversal effect of vasoconstriction of different
Literature Review
greater impact on renal failure. Early diagnosis has often been linked to infection including
immune-suppression and mortality was associated with the onset. New analysis and evidence
have linked cause of death among kidney transplants as a grossing tendency to follow up of
kidney transplant patients.
Renal failure often occasioned after orthotropic liver transplant has been observed to be the
common form of complication with an average contribution of 12% -40% linked to worse
outcomes, especially in the renal replacement therapy is needed, (Plafkin et al., 2018).
4.3 Development of chronic kidney disease
The occurrence of non-solid organ transplantation has shown the occurrence of kidney
diseases, which is increasingly becoming prevalent complication among the population. CKD
has been shown to increase and advance immuno-suppressions and the overall preoperative
environment and also factors associated with cardiovascular risk factors coupled infections
complications.
CKD is often associated with enhanced and decreased morbidity and mortality. Factors
related to kidney function and non-renal function transplantation including kidney
functioning evaluation prior to non-renal transplantation affects the transplantation processes.
Assessment of kidney function prior to non-renal organ transplant needs to be a preoperative
rule for kidney function tests, (Boers, Visser, Smith & Fuchs, 2014).
4.4 Nephrotoxicity caused by Calcineurin inhibitors
CNIs have been shown to have an effect on the vasoconstriction which often predisposes the
patient with renal failure symptoms and chronic injury especially when the patients' insults
are present. Calcineurin inhibitors often cause nephrotoxicity in conjunction with
cyclosporine A. While at organ recounts, during the cyclosporine arena, the deep decline of
kidney function has been noted to take place within a period of 6 weeks after transplantation
process. Calcineurin inhibitors have shown to have an association with nephrotoxicity levels
which increase exposure duration and often decrease exposure and limited reversibility.
4.4.1 Effects on the Kidney
Calcineurin inhibitors tend to reduce the reversal effect of vasoconstriction of different
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
10
Literature Review
glomerular arterioles which have maximal hour peak for serum concentrations to take effect.
The net effect of the acute change is always reversible, with concentrate reduction based on
the reductions of Glomerular filtration rate and increase in the nonvascular resistances.
Vasoconstriction is often initiated with nitric oxide inhibition, through increased angiotensin
and thromboxane which is augmented by endothelium actions' he abnormal responses are
often potential in presence of other inhibitors such as auto regulators, blocking agents and
nonsteroidal anti-inflammatory drugs, (Moini, Schilsky & Tichy, 2015).
4.4.2 Chronic nephrotoxicity
Chronic Calcineurin inhibitors have been extensively been studied and focused. The typical
picture of the chronic Calcineurin inhibitors is often characterized by a lack of symptoms and
gradual decline of the renal function. Studies undertaken on biopsy have shown that the often
related injuries. Renal status of the patients has always revealed lower levels of GFR in line
with declined blood flow, increased mean arterial blood pressure, elevated renal vascular and
excretion of albumin. With time the perturbations often link to progressive ratio-pathy and
the ischemic collapse of the glomeruli, (Ramachandran et al., 2015).
Direct injury of Calcineurin inhibitors toxicity has been shown to have elevated levels of
oxidative stress, thus leading to systematic inflammation which has negative effects on the
endothelial function. The overall effects of this are mediated by inhibition of nitric oxide,
through increased angiotensin and thromboxane levels, (Ramachandran et al., 2015).
Chronic Calcineurin inhibitors -nephropathy has been shown to lack symptoms. It is a blend
of urine sediment and gradual decreased one of the renal. Often observation of albuminuria is
observed although nephritic levels of proteinuria are difficult to find. Renal biopsy results
among nonrenal organ recipients have shown that Calcineurin inhibitors injury is often
difficult to find. Further findings of histology assessments have shown that interstitial fibrous,
have ‘striped' appearance which later develops to tubular atrophy. Hemodynamic renal
studies have shwon decreased GFR rations and associated reduced blood flow, increased
mean arterial pressure, elevated renal vascular, increased mean, increased resistance on the
vascular pathway and excretion of albumin. With time, the perturbations lead to progressive
arteriolopathy and ischemic collapse, (Yanagisawa, Omoto, Shimizu, Ishida and Tanabe,
2015).
Literature Review
glomerular arterioles which have maximal hour peak for serum concentrations to take effect.
The net effect of the acute change is always reversible, with concentrate reduction based on
the reductions of Glomerular filtration rate and increase in the nonvascular resistances.
Vasoconstriction is often initiated with nitric oxide inhibition, through increased angiotensin
and thromboxane which is augmented by endothelium actions' he abnormal responses are
often potential in presence of other inhibitors such as auto regulators, blocking agents and
nonsteroidal anti-inflammatory drugs, (Moini, Schilsky & Tichy, 2015).
4.4.2 Chronic nephrotoxicity
Chronic Calcineurin inhibitors have been extensively been studied and focused. The typical
picture of the chronic Calcineurin inhibitors is often characterized by a lack of symptoms and
gradual decline of the renal function. Studies undertaken on biopsy have shown that the often
related injuries. Renal status of the patients has always revealed lower levels of GFR in line
with declined blood flow, increased mean arterial blood pressure, elevated renal vascular and
excretion of albumin. With time the perturbations often link to progressive ratio-pathy and
the ischemic collapse of the glomeruli, (Ramachandran et al., 2015).
Direct injury of Calcineurin inhibitors toxicity has been shown to have elevated levels of
oxidative stress, thus leading to systematic inflammation which has negative effects on the
endothelial function. The overall effects of this are mediated by inhibition of nitric oxide,
through increased angiotensin and thromboxane levels, (Ramachandran et al., 2015).
Chronic Calcineurin inhibitors -nephropathy has been shown to lack symptoms. It is a blend
of urine sediment and gradual decreased one of the renal. Often observation of albuminuria is
observed although nephritic levels of proteinuria are difficult to find. Renal biopsy results
among nonrenal organ recipients have shown that Calcineurin inhibitors injury is often
difficult to find. Further findings of histology assessments have shown that interstitial fibrous,
have ‘striped' appearance which later develops to tubular atrophy. Hemodynamic renal
studies have shwon decreased GFR rations and associated reduced blood flow, increased
mean arterial pressure, elevated renal vascular, increased mean, increased resistance on the
vascular pathway and excretion of albumin. With time, the perturbations lead to progressive
arteriolopathy and ischemic collapse, (Yanagisawa, Omoto, Shimizu, Ishida and Tanabe,
2015).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
Literature Review
Another direct and indirect mechanism identified is chronic Calcineurin inhibitors mediated
renal injury process. The direct mechanisms of Calcineurin inhibitors include elevating
oxidative stress which leads to inflame a dangerous factor in endothelial activity. Often at
times, research has shown that CNIs can have an effect on thrombotic microangiopathy
which is characterized by the spectrum of clinical findings which include kidney function
impairment. The existence of potential indirect mechanism has shown a indirect mechanisms
on the CNI mediated injury on the renal activity. Possible mechanisms of CNIs injury include
retention of sodium and hypertension elevation, diabetes and dyslipidemia occurrence which
is associated with as a risks factor for declining renal failure disease among patients,
(Brunkhorst et al., 2015).
4.4.3 Tacrolimus versus cyclosporine A (CsA)
Studies done have shown that tacrolimus offers less nephrotoxicity compared to CsA. Further
spectrum adverse effects have been noted when the comparison was made between
immunosuppressive spectrum regimens which have adverse effects and other long-term
efficacy. With respect to renal functionality, one benefits of tacrolimus over CsA. Tacrolimus
assessment cause vasoconstriction compared to CsA, which often offer an explanation on the
short term decline of creatinine which is noted from the conversion of CsA, (Gard et al.,
2015).
Elevated kidney improvement among none renal organ has shown regiments which have
tacrolimus partly distributed to less nephrotoxicity different than that observed from CsA,
which contains less nephrotoxicity compared to that observed by CsA, (Torres et al., 2018).
4.5 Organ-specific interactions on kidney renal failure
4.5.1 Liver transplant
With the introduction of cyclosporine, transplants for liver has become an effective way f
end-stage treatment process for an end-stage liver disease where there is an occurrence of 1-
year survival rate of 10%. Patients having an effective treatment for end-stage liver have 1
year survival rate. Patients with a severe liver disease, GI haemorrhagic often predisposes
themselves to development of acute renal failure. Hyperbilirubinemia have a nephrotoxic
effect and often complicate matters while asking the patients get exposed to other noxious
influence. Further hypotension effects can have massive blood loss which often complicates
Literature Review
Another direct and indirect mechanism identified is chronic Calcineurin inhibitors mediated
renal injury process. The direct mechanisms of Calcineurin inhibitors include elevating
oxidative stress which leads to inflame a dangerous factor in endothelial activity. Often at
times, research has shown that CNIs can have an effect on thrombotic microangiopathy
which is characterized by the spectrum of clinical findings which include kidney function
impairment. The existence of potential indirect mechanism has shown a indirect mechanisms
on the CNI mediated injury on the renal activity. Possible mechanisms of CNIs injury include
retention of sodium and hypertension elevation, diabetes and dyslipidemia occurrence which
is associated with as a risks factor for declining renal failure disease among patients,
(Brunkhorst et al., 2015).
4.4.3 Tacrolimus versus cyclosporine A (CsA)
Studies done have shown that tacrolimus offers less nephrotoxicity compared to CsA. Further
spectrum adverse effects have been noted when the comparison was made between
immunosuppressive spectrum regimens which have adverse effects and other long-term
efficacy. With respect to renal functionality, one benefits of tacrolimus over CsA. Tacrolimus
assessment cause vasoconstriction compared to CsA, which often offer an explanation on the
short term decline of creatinine which is noted from the conversion of CsA, (Gard et al.,
2015).
Elevated kidney improvement among none renal organ has shown regiments which have
tacrolimus partly distributed to less nephrotoxicity different than that observed from CsA,
which contains less nephrotoxicity compared to that observed by CsA, (Torres et al., 2018).
4.5 Organ-specific interactions on kidney renal failure
4.5.1 Liver transplant
With the introduction of cyclosporine, transplants for liver has become an effective way f
end-stage treatment process for an end-stage liver disease where there is an occurrence of 1-
year survival rate of 10%. Patients having an effective treatment for end-stage liver have 1
year survival rate. Patients with a severe liver disease, GI haemorrhagic often predisposes
themselves to development of acute renal failure. Hyperbilirubinemia have a nephrotoxic
effect and often complicate matters while asking the patients get exposed to other noxious
influence. Further hypotension effects can have massive blood loss which often complicates
10
Literature Review
the vascular instability, accompanying the end-stage liver diseases. Further postoperative
infection, rejection and volume overload and cyclosporine toxicity may have effects on the
maintenance of renal functionality, (Lu et al., 2018).
Long-term patients often need immune-suppression with cyclosporine which offers
preservation to liver function. Renal function is often at risks in various sections of liver
transplantation; etiological factors need to be assessed with the contribution of cyclosporine
factor being addressed. A retrospective study done on aetiologies' of renal failure among
adult patients showed that chronic renal failure was attributed to peak serum creatinine,
multiple liver transplantation, and dialysis needs, (Moini, Schilsky & Tichy, 2015).
4.5.2 Liver transplantation
Studies have shown that abnormal renal function is necessary. Clinical indications have
shown a range of limited elevations on serum creatinine which leads to hepatorenal syndrome
requiring dialysis. Here is also the occurrence of postoperative kidney injury. Further
Hepatitis C virus displays itself and a potential risk factor for renal disease occurring after
transplantation. Liver transplant patients often require immunosuppressant form solid organs
CNI related renal injuries occur, (Doi & Rabb, 2016).
4.5.3 Heart and lung transplantation
Interactions of heart and lungs, have been shown to have high rates of renal failure occurs
during the preoperative phase; this predisposes renal failure among kidney patients. Heart and
lung entail high surgical process. Left and right ventricles are often hard to achieve enough
oxygen which often persists for long after surgery process. These postoperative issues often
increase risks related o renal failure, and tubular injury. The issue is further compounded by
increased risks of heart and lungs complications, having effects on CNI dosage, (Doi & Rabb,
2016). Increased cardiovascular state and retention of sodium among renal patients have been
shown to pose more challenges.
4.5.4 Kidney transplant
Kidney transplant refers to renal replacement therapy for patients who are experiencing end-
stage renal disease of CKD. Transplant patient have higher survival rate, good quality of life
and less intake of healthcare resources as compared to the patients who undergo dialysis.
Literature Review
the vascular instability, accompanying the end-stage liver diseases. Further postoperative
infection, rejection and volume overload and cyclosporine toxicity may have effects on the
maintenance of renal functionality, (Lu et al., 2018).
Long-term patients often need immune-suppression with cyclosporine which offers
preservation to liver function. Renal function is often at risks in various sections of liver
transplantation; etiological factors need to be assessed with the contribution of cyclosporine
factor being addressed. A retrospective study done on aetiologies' of renal failure among
adult patients showed that chronic renal failure was attributed to peak serum creatinine,
multiple liver transplantation, and dialysis needs, (Moini, Schilsky & Tichy, 2015).
4.5.2 Liver transplantation
Studies have shown that abnormal renal function is necessary. Clinical indications have
shown a range of limited elevations on serum creatinine which leads to hepatorenal syndrome
requiring dialysis. Here is also the occurrence of postoperative kidney injury. Further
Hepatitis C virus displays itself and a potential risk factor for renal disease occurring after
transplantation. Liver transplant patients often require immunosuppressant form solid organs
CNI related renal injuries occur, (Doi & Rabb, 2016).
4.5.3 Heart and lung transplantation
Interactions of heart and lungs, have been shown to have high rates of renal failure occurs
during the preoperative phase; this predisposes renal failure among kidney patients. Heart and
lung entail high surgical process. Left and right ventricles are often hard to achieve enough
oxygen which often persists for long after surgery process. These postoperative issues often
increase risks related o renal failure, and tubular injury. The issue is further compounded by
increased risks of heart and lungs complications, having effects on CNI dosage, (Doi & Rabb,
2016). Increased cardiovascular state and retention of sodium among renal patients have been
shown to pose more challenges.
4.5.4 Kidney transplant
Kidney transplant refers to renal replacement therapy for patients who are experiencing end-
stage renal disease of CKD. Transplant patient have higher survival rate, good quality of life
and less intake of healthcare resources as compared to the patients who undergo dialysis.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
10
Literature Review
Despite immense improvements on immune suppression and relapse can occur. Further
patients who experience dialysis after transplant often have higher mortality rates.
Research on kidney transplant outcomes has shown that patients have often focussed on
immunologic factors and adjuvant therapies observed in renal cancer patients. Limited focus
has been directed towards nonimmunologic factors such as CKD and development of
diseases which often affect mortality and morbidity of the patients. Success attributed to
kidney transplantation has often led to high rates of patients having higher co-morbid
diseases. Further other complications have been established with factors such as those
associated with malnutrition, cardiovascular diseases, and anemia which have a positive
prediction on clinical outcomes, (Bergmann, 2015).
4.6 Conclusions
Renal failure among patients undergone the organ transplant procedures often occurs due to a
variety of reasons highlighted above. Understanding the limitations of serum creatinine and
renal functioning ability are critical factors which need to be undertaken. Medial procedures
need to be undertaken to minimize nephrotoxicity, which is an important element towards the
occurrence of a liver failure. Assessment of transplant risks factors needs to be addressed
adequately. CNI can be an effective approach in managing the progression of total renal
failure, however critical nursing decision needs to be undertaken comprehensively.
Management of chronic kidney disease plays a vital role in managing various treatment
processes for patients.
Literature Review
Despite immense improvements on immune suppression and relapse can occur. Further
patients who experience dialysis after transplant often have higher mortality rates.
Research on kidney transplant outcomes has shown that patients have often focussed on
immunologic factors and adjuvant therapies observed in renal cancer patients. Limited focus
has been directed towards nonimmunologic factors such as CKD and development of
diseases which often affect mortality and morbidity of the patients. Success attributed to
kidney transplantation has often led to high rates of patients having higher co-morbid
diseases. Further other complications have been established with factors such as those
associated with malnutrition, cardiovascular diseases, and anemia which have a positive
prediction on clinical outcomes, (Bergmann, 2015).
4.6 Conclusions
Renal failure among patients undergone the organ transplant procedures often occurs due to a
variety of reasons highlighted above. Understanding the limitations of serum creatinine and
renal functioning ability are critical factors which need to be undertaken. Medial procedures
need to be undertaken to minimize nephrotoxicity, which is an important element towards the
occurrence of a liver failure. Assessment of transplant risks factors needs to be addressed
adequately. CNI can be an effective approach in managing the progression of total renal
failure, however critical nursing decision needs to be undertaken comprehensively.
Management of chronic kidney disease plays a vital role in managing various treatment
processes for patients.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
Literature Review
References
Bergmann, C. (2015). ARPKD and early manifestations of ADPKD: the original polycystic
kidney disease and phenocopies. Pediatric Nephrology, 30(1), 15-30.
Boers, S. J., Visser, G., Smit, P. G., & Fuchs, S. A. (2014). Liver transplantation in glycogen
storage disease type I. Orphanet journal of rare diseases, 9(1), 47.
Brunkhorst, L. C., Fichtner, A., Höcker, B., Burmeister, G., Ahlenstiel-Grunow, T., Krupka,
K., ... & Pape, L. (2015). Efficacy and safety of an everolimus-vs. a mycophenolate
mofetil-based regimen in pediatric renal transplant recipients. PloS one, 10(9),
e0135439.
Chawla, L. S., Eggers, P. W., Star, R. A., & Kimmel, P. L. (2014). Acute kidney injury and
chronic kidney disease as interconnected syndromes. New England Journal of
Medicine, 371(1), 58-66.
Cox, D. R. (2018). Analysis of survival data. Routledge.
Doi, K., & Rabb, H. (2016). Impact of acute kidney injury on distant organ function: recent
findings and potential therapeutic targets. Kidney International, 89(3), 555-564.
Funk, G. A., Gosert, R., Comoli, P., Ginevri, F., & Hirsch, H. H. (2008). Polyomavirus BK
replication dynamics in vivo and in silico to predict cytopathology and viral clearance
in kidney transplants. American journal of transplantation, 8(11), 2368-2377.
Gard, L., Van Doesum, W., Niesters, B., Van Son, W., Stegeman, C. A., Riezebos-Brilman,
A., & Sanders, J. S. (2015, December). The Delicate Balance Between Rejection and
BK Virus Replication in Renal Transplant Recipients Treated With Tacrolimus Versus
Cyclosporine. In Open Forum Infectious Diseases (Vol. 2, No. suppl_1, p. 1207).
Infectious Diseases Society of America.
Go, A. S., Chertow, G. M., Fan, D., McCulloch, C. E., & Hsu, C. Y. (2004). Chronic kidney
disease and the risks of death, cardiovascular events, and hospitalization. New England
Journal of Medicine, 351(13), 1296-1305.
Literature Review
References
Bergmann, C. (2015). ARPKD and early manifestations of ADPKD: the original polycystic
kidney disease and phenocopies. Pediatric Nephrology, 30(1), 15-30.
Boers, S. J., Visser, G., Smit, P. G., & Fuchs, S. A. (2014). Liver transplantation in glycogen
storage disease type I. Orphanet journal of rare diseases, 9(1), 47.
Brunkhorst, L. C., Fichtner, A., Höcker, B., Burmeister, G., Ahlenstiel-Grunow, T., Krupka,
K., ... & Pape, L. (2015). Efficacy and safety of an everolimus-vs. a mycophenolate
mofetil-based regimen in pediatric renal transplant recipients. PloS one, 10(9),
e0135439.
Chawla, L. S., Eggers, P. W., Star, R. A., & Kimmel, P. L. (2014). Acute kidney injury and
chronic kidney disease as interconnected syndromes. New England Journal of
Medicine, 371(1), 58-66.
Cox, D. R. (2018). Analysis of survival data. Routledge.
Doi, K., & Rabb, H. (2016). Impact of acute kidney injury on distant organ function: recent
findings and potential therapeutic targets. Kidney International, 89(3), 555-564.
Funk, G. A., Gosert, R., Comoli, P., Ginevri, F., & Hirsch, H. H. (2008). Polyomavirus BK
replication dynamics in vivo and in silico to predict cytopathology and viral clearance
in kidney transplants. American journal of transplantation, 8(11), 2368-2377.
Gard, L., Van Doesum, W., Niesters, B., Van Son, W., Stegeman, C. A., Riezebos-Brilman,
A., & Sanders, J. S. (2015, December). The Delicate Balance Between Rejection and
BK Virus Replication in Renal Transplant Recipients Treated With Tacrolimus Versus
Cyclosporine. In Open Forum Infectious Diseases (Vol. 2, No. suppl_1, p. 1207).
Infectious Diseases Society of America.
Go, A. S., Chertow, G. M., Fan, D., McCulloch, C. E., & Hsu, C. Y. (2004). Chronic kidney
disease and the risks of death, cardiovascular events, and hospitalization. New England
Journal of Medicine, 351(13), 1296-1305.
10
Literature Review
Gordon, E. J., Ladner, D. P., Caicedo, J. C., & Franklin, J. (2010, January). Disparities in
kidney transplant outcomes: a review. In Seminars in nephrology (Vol. 30, No. 1, pp.
81-89). WB Saunders.
Karkouti, K., Grocott, H. P., Hall, R., Jessen, M. E., Kruger, C., Lerner, A. B., ... & Ralley, F.
(2015). Interrelationship of preoperative anemia, intraoperative anemia, and red blood
cell transfusion as potentially modifiable risk factors for acute kidney injury in cardiac
surgery: a historical multicentre cohort study. Canadian Journal of Anesthesia/Journal
canadien d'anesthésie, 62(4), 377-384.
Lu, H. Y., Ning, X. Y., Chen, Y. Q., Han, S. J., Chi, P., Zhu, S. N., & Yue, Y. (2018).
Predictive Value of Serum Creatinine, Blood Urea Nitrogen, Uric Acid, and β2-
Microglobulin in the Evaluation of Acute Kidney Injury after Orthotopic Liver
Transplantation. Chinese medical journal, 131(9), 1059.
Moini, M., Schilsky, M. L., & Tichy, E. M. (2015). Review on immunosuppression in liver
transplantation. World journal of hepatology, 7(10), 1355.
Nair, S., Verma, S., & Thuluvath, P. J. (2002). Pretransplant renal function predicts survival
in patients undergoing orthotopic liver transplantation. Hepatology, 35(5), 1179-1185.
Papadimitriou, J. C., Randhawa, P., Rinaldo, C. H., Drachenberg, C. B., Alexiev, B., &
Hirsch, H. H. (2016). BK polyomavirus infection and renourinary tumorigenesis.
American Journal of Transplantation, 16(2), 398-406.
Plafkin, C., Singh, T., Astor, B. C., Parajuli, S., Bhutani, G., Safdar, N., & Panzer, S. E.
(2018). Kidney transplant recipients with polycystic kidney disease have a lower risk of
post‐transplant BK infection than those with end‐stage renal disease due to other
causes. Transplant Infectious Disease, e12974.
Ramachandran, R., Kumar, D. A. P., Nada, R., Jha, V., Gupta, K. L., & Kohli, H. S. (2015).
Chronic nephrotoxicity limits successful use of Tacrolimus in the management of adult
steroid-dependent minimal change disease. Nephrology (Carlton), 20(5), 384-385.
Saab, S., Barnard, A., Challita, Y., Adeniyi, A., Aziz, A., Choi, G., ... & Busuttil, R. W.
(2018). Impact of Sustained Viral Response With Direct-Acting Agents on Glycemic
Literature Review
Gordon, E. J., Ladner, D. P., Caicedo, J. C., & Franklin, J. (2010, January). Disparities in
kidney transplant outcomes: a review. In Seminars in nephrology (Vol. 30, No. 1, pp.
81-89). WB Saunders.
Karkouti, K., Grocott, H. P., Hall, R., Jessen, M. E., Kruger, C., Lerner, A. B., ... & Ralley, F.
(2015). Interrelationship of preoperative anemia, intraoperative anemia, and red blood
cell transfusion as potentially modifiable risk factors for acute kidney injury in cardiac
surgery: a historical multicentre cohort study. Canadian Journal of Anesthesia/Journal
canadien d'anesthésie, 62(4), 377-384.
Lu, H. Y., Ning, X. Y., Chen, Y. Q., Han, S. J., Chi, P., Zhu, S. N., & Yue, Y. (2018).
Predictive Value of Serum Creatinine, Blood Urea Nitrogen, Uric Acid, and β2-
Microglobulin in the Evaluation of Acute Kidney Injury after Orthotopic Liver
Transplantation. Chinese medical journal, 131(9), 1059.
Moini, M., Schilsky, M. L., & Tichy, E. M. (2015). Review on immunosuppression in liver
transplantation. World journal of hepatology, 7(10), 1355.
Nair, S., Verma, S., & Thuluvath, P. J. (2002). Pretransplant renal function predicts survival
in patients undergoing orthotopic liver transplantation. Hepatology, 35(5), 1179-1185.
Papadimitriou, J. C., Randhawa, P., Rinaldo, C. H., Drachenberg, C. B., Alexiev, B., &
Hirsch, H. H. (2016). BK polyomavirus infection and renourinary tumorigenesis.
American Journal of Transplantation, 16(2), 398-406.
Plafkin, C., Singh, T., Astor, B. C., Parajuli, S., Bhutani, G., Safdar, N., & Panzer, S. E.
(2018). Kidney transplant recipients with polycystic kidney disease have a lower risk of
post‐transplant BK infection than those with end‐stage renal disease due to other
causes. Transplant Infectious Disease, e12974.
Ramachandran, R., Kumar, D. A. P., Nada, R., Jha, V., Gupta, K. L., & Kohli, H. S. (2015).
Chronic nephrotoxicity limits successful use of Tacrolimus in the management of adult
steroid-dependent minimal change disease. Nephrology (Carlton), 20(5), 384-385.
Saab, S., Barnard, A., Challita, Y., Adeniyi, A., Aziz, A., Choi, G., ... & Busuttil, R. W.
(2018). Impact of Sustained Viral Response With Direct-Acting Agents on Glycemic
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





