Report on Chronic Cardiac Failure and Asthma
VerifiedAdded on 2023/04/08
|15
|3232
|432
AI Summary
This academic paper contains a detailed report of a patient with chronic cardiac failure and asthma. It discusses the pathophysiology, treatment strategies, and legal and ethical aspects of nursing. Find the complete report on Desklib.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: REPORT
Assignment 3
Name of the Student
Name of the University
Author Note
Assignment 3
Name of the Student
Name of the University
Author Note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1REPORT
Executive summary
This academic paper contains a detailed report of a patient, presented at the Clinical Case
Conference. Mrs P is an octogenarian and has been living in a residential care facility, since
the death of her husband. The report illustrated the pathophysiology of the two major
concerns that have been identified in her namely, chronic cardiac failure and asthma. The
report provided an overview of the pharmacological and non-pharmacological treatment
strategies that will be administered, in addition to elucidating on the approaches that will help
in addressing her emotional, psychosocial and economic needs. The report also provided
detailed information on the legal and ethical aspects of nursing, and framed a discharge plan
that will be followed, prior to her release from the healthcare setting.
Executive summary
This academic paper contains a detailed report of a patient, presented at the Clinical Case
Conference. Mrs P is an octogenarian and has been living in a residential care facility, since
the death of her husband. The report illustrated the pathophysiology of the two major
concerns that have been identified in her namely, chronic cardiac failure and asthma. The
report provided an overview of the pharmacological and non-pharmacological treatment
strategies that will be administered, in addition to elucidating on the approaches that will help
in addressing her emotional, psychosocial and economic needs. The report also provided
detailed information on the legal and ethical aspects of nursing, and framed a discharge plan
that will be followed, prior to her release from the healthcare setting.
2REPORT
Table of Contents
Discussion..................................................................................................................................3
Medical condition...................................................................................................................3
Nursing assessment................................................................................................................3
Medical management and treatment......................................................................................5
Clinical inference...................................................................................................................6
Psychosocial/Environmental/Economic aspects....................................................................7
Ethical and legal aspects........................................................................................................8
Discharge planning.................................................................................................................9
Education needs of patient /family.......................................................................................10
Conclusion................................................................................................................................10
References................................................................................................................................11
Table of Contents
Discussion..................................................................................................................................3
Medical condition...................................................................................................................3
Nursing assessment................................................................................................................3
Medical management and treatment......................................................................................5
Clinical inference...................................................................................................................6
Psychosocial/Environmental/Economic aspects....................................................................7
Ethical and legal aspects........................................................................................................8
Discharge planning.................................................................................................................9
Education needs of patient /family.......................................................................................10
Conclusion................................................................................................................................10
References................................................................................................................................11
3REPORT
Discussion
Medical condition
Chronic Cardiac Failure (CCF) can be accredited to the onset of a condition that
results in a decrease in the efficiency of the cardiac muscles, which in turn is a direct
manifestation of overloading or damage (Bloom et al., 2016). In addition, the heart of the
patients suffering from CCG also demonstrate a decreased force of contraction, when the
ventricles get overloaded. Under circumstances when the upper chambers of the heart get
filled, there occurs an increased contraction force, concomitant with an elevation in cardiac
output. Furthermore, Tham et al. (2015) stated that the condition is also characterised by an
increase in the size of the cardiomyocytes and subsequent thickening of the walls of the
ventricles that reduces efficiency of heart contraction. In contrast, exposure of risk factors
lead to irritation in the airways that trigger crosslinking with the receptors of IgE located on
the bronchial wall mast cells. Chronic inflammation of the airways lead to lamina reticularis
thickening and increase in the number of eosinophil, this increasing the contractibility of the
smooth muscles that surround them (Maslan & Mims, 2014).
Nursing assessment
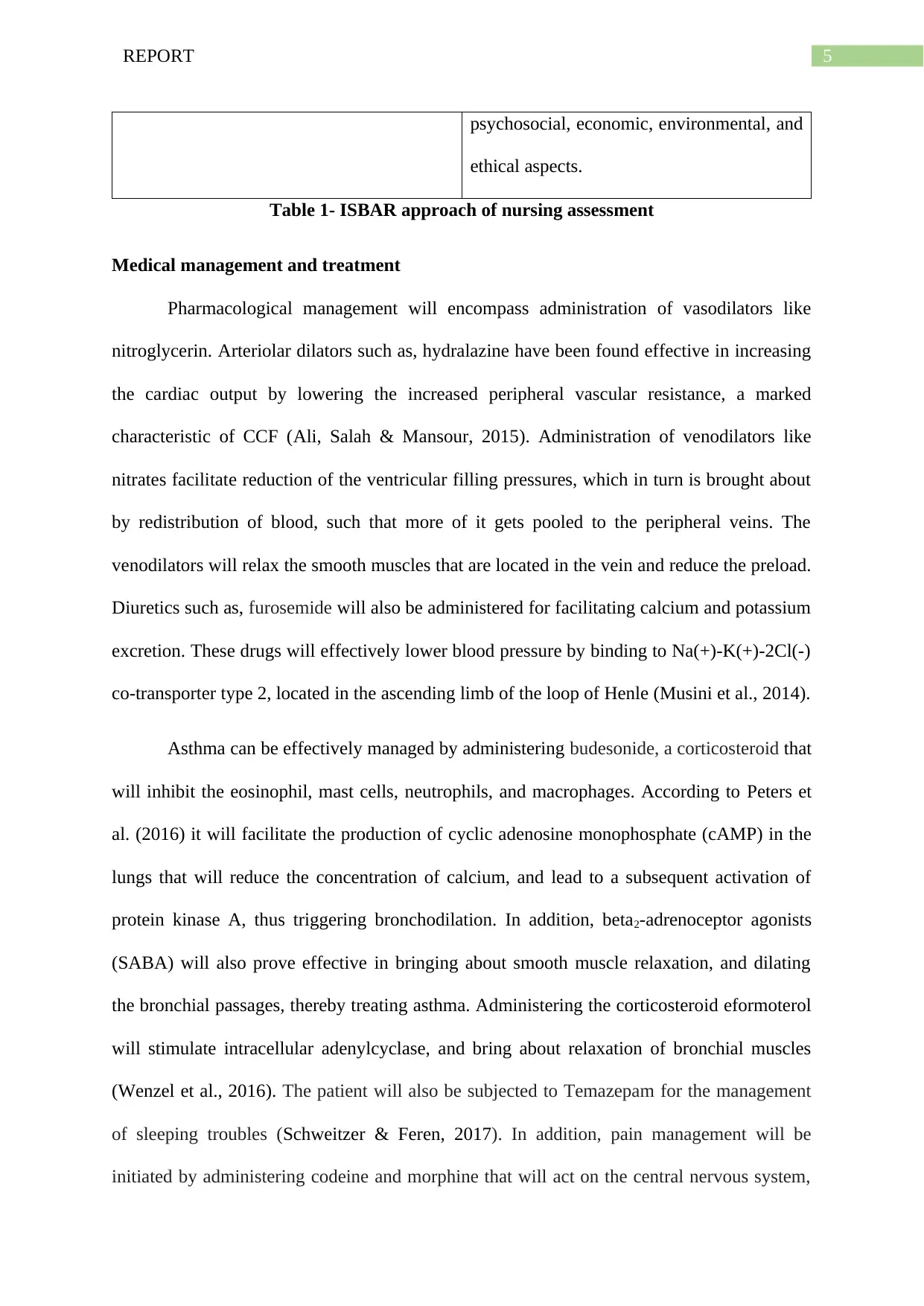
I (Introduction) I am calling because the patient needs to be
treated for congestive heart failure and
asthmatic conditions.
S (Situation) This is urgent because the patient reports
difficulty in falling asleep due to pain and
had been admitted, following an overdose of
Temazepam. In addition, past suicidal
attempt and regular administration of
Discussion
Medical condition
Chronic Cardiac Failure (CCF) can be accredited to the onset of a condition that
results in a decrease in the efficiency of the cardiac muscles, which in turn is a direct
manifestation of overloading or damage (Bloom et al., 2016). In addition, the heart of the
patients suffering from CCG also demonstrate a decreased force of contraction, when the
ventricles get overloaded. Under circumstances when the upper chambers of the heart get
filled, there occurs an increased contraction force, concomitant with an elevation in cardiac
output. Furthermore, Tham et al. (2015) stated that the condition is also characterised by an
increase in the size of the cardiomyocytes and subsequent thickening of the walls of the
ventricles that reduces efficiency of heart contraction. In contrast, exposure of risk factors
lead to irritation in the airways that trigger crosslinking with the receptors of IgE located on
the bronchial wall mast cells. Chronic inflammation of the airways lead to lamina reticularis
thickening and increase in the number of eosinophil, this increasing the contractibility of the
smooth muscles that surround them (Maslan & Mims, 2014).
Nursing assessment
I (Introduction) I am calling because the patient needs to be
treated for congestive heart failure and
asthmatic conditions.
S (Situation) This is urgent because the patient reports
difficulty in falling asleep due to pain and
had been admitted, following an overdose of
Temazepam. In addition, past suicidal
attempt and regular administration of
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
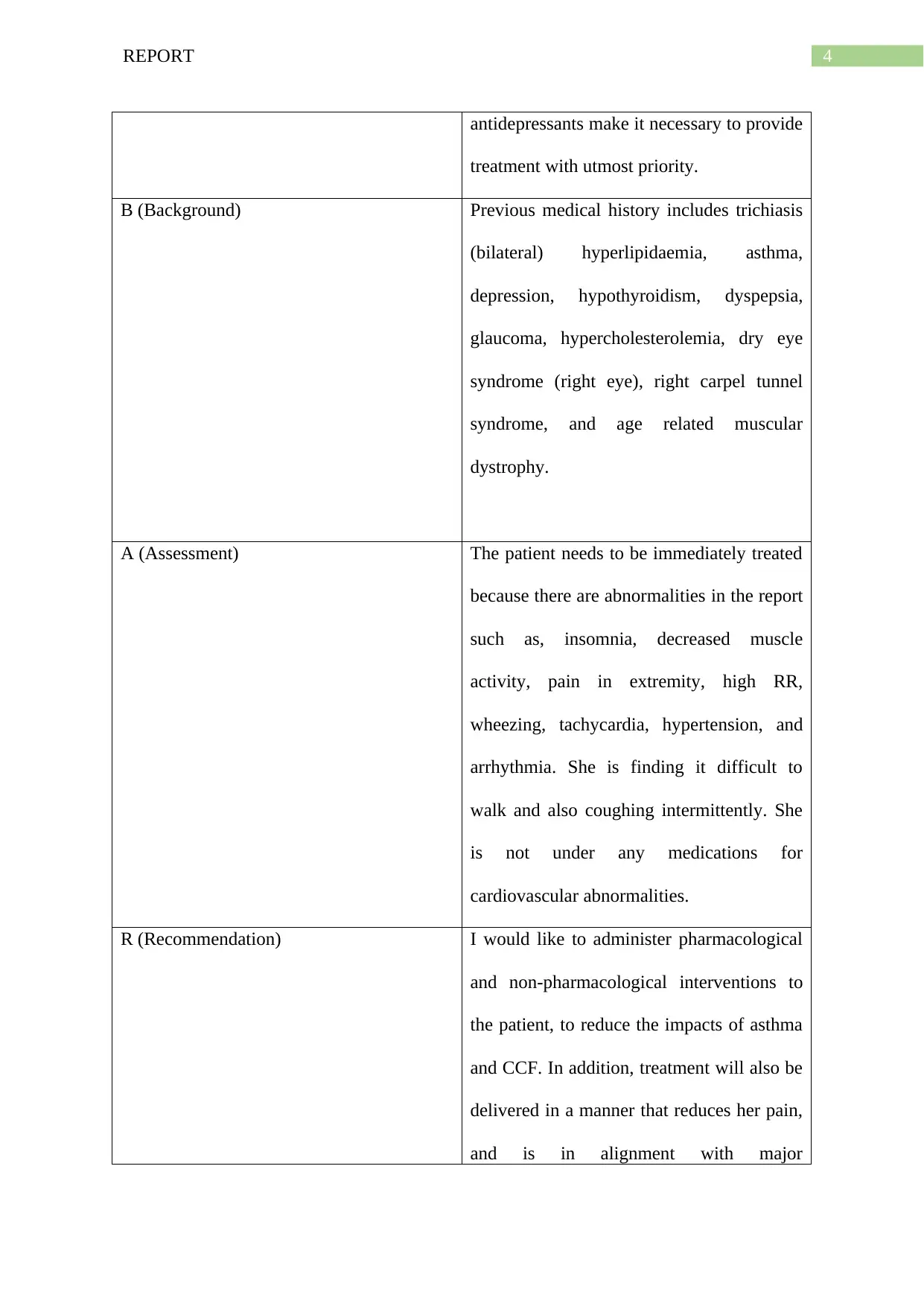
4REPORT
antidepressants make it necessary to provide
treatment with utmost priority.
B (Background) Previous medical history includes trichiasis
(bilateral) hyperlipidaemia, asthma,
depression, hypothyroidism, dyspepsia,
glaucoma, hypercholesterolemia, dry eye
syndrome (right eye), right carpel tunnel
syndrome, and age related muscular
dystrophy.
A (Assessment) The patient needs to be immediately treated
because there are abnormalities in the report
such as, insomnia, decreased muscle
activity, pain in extremity, high RR,
wheezing, tachycardia, hypertension, and
arrhythmia. She is finding it difficult to
walk and also coughing intermittently. She
is not under any medications for
cardiovascular abnormalities.
R (Recommendation) I would like to administer pharmacological
and non-pharmacological interventions to
the patient, to reduce the impacts of asthma
and CCF. In addition, treatment will also be
delivered in a manner that reduces her pain,
and is in alignment with major
antidepressants make it necessary to provide
treatment with utmost priority.
B (Background) Previous medical history includes trichiasis
(bilateral) hyperlipidaemia, asthma,
depression, hypothyroidism, dyspepsia,
glaucoma, hypercholesterolemia, dry eye
syndrome (right eye), right carpel tunnel
syndrome, and age related muscular
dystrophy.
A (Assessment) The patient needs to be immediately treated
because there are abnormalities in the report
such as, insomnia, decreased muscle
activity, pain in extremity, high RR,
wheezing, tachycardia, hypertension, and
arrhythmia. She is finding it difficult to
walk and also coughing intermittently. She
is not under any medications for
cardiovascular abnormalities.
R (Recommendation) I would like to administer pharmacological
and non-pharmacological interventions to
the patient, to reduce the impacts of asthma
and CCF. In addition, treatment will also be
delivered in a manner that reduces her pain,
and is in alignment with major
5REPORT
psychosocial, economic, environmental, and
ethical aspects.
Table 1- ISBAR approach of nursing assessment
Medical management and treatment
Pharmacological management will encompass administration of vasodilators like
nitroglycerin. Arteriolar dilators such as, hydralazine have been found effective in increasing
the cardiac output by lowering the increased peripheral vascular resistance, a marked
characteristic of CCF (Ali, Salah & Mansour, 2015). Administration of venodilators like
nitrates facilitate reduction of the ventricular filling pressures, which in turn is brought about
by redistribution of blood, such that more of it gets pooled to the peripheral veins. The
venodilators will relax the smooth muscles that are located in the vein and reduce the preload.
Diuretics such as, furosemide will also be administered for facilitating calcium and potassium
excretion. These drugs will effectively lower blood pressure by binding to Na(+)-K(+)-2Cl(-)
co-transporter type 2, located in the ascending limb of the loop of Henle (Musini et al., 2014).
Asthma can be effectively managed by administering budesonide, a corticosteroid that
will inhibit the eosinophil, mast cells, neutrophils, and macrophages. According to Peters et
al. (2016) it will facilitate the production of cyclic adenosine monophosphate (cAMP) in the
lungs that will reduce the concentration of calcium, and lead to a subsequent activation of
protein kinase A, thus triggering bronchodilation. In addition, beta2-adrenoceptor agonists
(SABA) will also prove effective in bringing about smooth muscle relaxation, and dilating
the bronchial passages, thereby treating asthma. Administering the corticosteroid eformoterol
will stimulate intracellular adenylcyclase, and bring about relaxation of bronchial muscles
(Wenzel et al., 2016). The patient will also be subjected to Temazepam for the management
of sleeping troubles (Schweitzer & Feren, 2017). In addition, pain management will be
initiated by administering codeine and morphine that will act on the central nervous system,
psychosocial, economic, environmental, and
ethical aspects.
Table 1- ISBAR approach of nursing assessment
Medical management and treatment
Pharmacological management will encompass administration of vasodilators like
nitroglycerin. Arteriolar dilators such as, hydralazine have been found effective in increasing
the cardiac output by lowering the increased peripheral vascular resistance, a marked
characteristic of CCF (Ali, Salah & Mansour, 2015). Administration of venodilators like
nitrates facilitate reduction of the ventricular filling pressures, which in turn is brought about
by redistribution of blood, such that more of it gets pooled to the peripheral veins. The
venodilators will relax the smooth muscles that are located in the vein and reduce the preload.
Diuretics such as, furosemide will also be administered for facilitating calcium and potassium
excretion. These drugs will effectively lower blood pressure by binding to Na(+)-K(+)-2Cl(-)
co-transporter type 2, located in the ascending limb of the loop of Henle (Musini et al., 2014).
Asthma can be effectively managed by administering budesonide, a corticosteroid that
will inhibit the eosinophil, mast cells, neutrophils, and macrophages. According to Peters et
al. (2016) it will facilitate the production of cyclic adenosine monophosphate (cAMP) in the
lungs that will reduce the concentration of calcium, and lead to a subsequent activation of
protein kinase A, thus triggering bronchodilation. In addition, beta2-adrenoceptor agonists
(SABA) will also prove effective in bringing about smooth muscle relaxation, and dilating
the bronchial passages, thereby treating asthma. Administering the corticosteroid eformoterol
will stimulate intracellular adenylcyclase, and bring about relaxation of bronchial muscles
(Wenzel et al., 2016). The patient will also be subjected to Temazepam for the management
of sleeping troubles (Schweitzer & Feren, 2017). In addition, pain management will be
initiated by administering codeine and morphine that will act on the central nervous system,
6REPORT
and produce an analgesic effect. Non-pharmacological interventions would encompass
avoidance of asthma triggers like smoking, pollution, and sulphite-containing food. She will
also be assisted in adhering to certain behavioural modifications like dietary intake and
physical activity that will help in cardiac rehabilitation. Non-pharmacological pain
management will also involve subjecting the patient to music therapy that has proved
beneficial in lowering the amount of pain perceived by patients (Korhan et al., 2014).
Clinical inference
Presence of a pain score of 4/10 in the Verbal Descriptor Scale (VDS) indicated that
the patient suffered from moderate pain that is expected to create a significant impact on the
activities of her daily living (Wysham et al., 2015). Moreover, a score of 0/10, following the
administration of paracetamol and Norspan Patch suggests that buprenorphine was able to
lower the type, duration and severity of pain in the lower extremities of the patient. Absence
of visual acuity in the right eye suggests that there was lack of clarity of vision, which in turn
was allied with a range of neural and optical factors like retinal focus sharpness, retina
functioning, and sensitivity of the brain interpretative faculties (Bastawrous et al., 2015). In
addition, presence of entropion, itchiness, redness, and dryness in the eyes suggested that
there was probable scarring of the conjunctiva and/or muscle spasm (Ding et al., 2014).
In addition, RR of 24-32 breaths/ min and wheezing indicated that the asthmatic
condition made breathing difficult and narrowing of the airways located in the lungs, due to
inflammation and blockage, produced the sound. Presence of tachycardia and hypertension
can also be accredited to atrial fibrillation and pain (Rolf et al., 2014). In addition, taking into
consideration the fact that the patient reported dry skin, it can be attributed to the presence of
atopic dermatitis or eczema that is a chronic skin disease, marked by appearance of dry scaly
patches on the skin surface. Positive laboratory results for peripheral oedema suggests the
and produce an analgesic effect. Non-pharmacological interventions would encompass
avoidance of asthma triggers like smoking, pollution, and sulphite-containing food. She will
also be assisted in adhering to certain behavioural modifications like dietary intake and
physical activity that will help in cardiac rehabilitation. Non-pharmacological pain
management will also involve subjecting the patient to music therapy that has proved
beneficial in lowering the amount of pain perceived by patients (Korhan et al., 2014).
Clinical inference
Presence of a pain score of 4/10 in the Verbal Descriptor Scale (VDS) indicated that
the patient suffered from moderate pain that is expected to create a significant impact on the
activities of her daily living (Wysham et al., 2015). Moreover, a score of 0/10, following the
administration of paracetamol and Norspan Patch suggests that buprenorphine was able to
lower the type, duration and severity of pain in the lower extremities of the patient. Absence
of visual acuity in the right eye suggests that there was lack of clarity of vision, which in turn
was allied with a range of neural and optical factors like retinal focus sharpness, retina
functioning, and sensitivity of the brain interpretative faculties (Bastawrous et al., 2015). In
addition, presence of entropion, itchiness, redness, and dryness in the eyes suggested that
there was probable scarring of the conjunctiva and/or muscle spasm (Ding et al., 2014).
In addition, RR of 24-32 breaths/ min and wheezing indicated that the asthmatic
condition made breathing difficult and narrowing of the airways located in the lungs, due to
inflammation and blockage, produced the sound. Presence of tachycardia and hypertension
can also be accredited to atrial fibrillation and pain (Rolf et al., 2014). In addition, taking into
consideration the fact that the patient reported dry skin, it can be attributed to the presence of
atopic dermatitis or eczema that is a chronic skin disease, marked by appearance of dry scaly
patches on the skin surface. Positive laboratory results for peripheral oedema suggests the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7REPORT
accumulation of fluid in the tissues that are perfused by peripheral vascular system located in
the lower extremities.
Psychosocial/Environmental/Economic aspects
Assistance must be provided to the patient for meeting her basic needs that
encompasses mental and emotional wellbeing. Efforts will be taken to create an environment
in the healthcare facility that makes the patient feel loved and secure. According to Swash et
al. (2014) being emotionally and mentally healthy suggests the presence of adequate coping
skills, in addition to gaining the competence of getting adjusted to major life changes such as,
depending on others, loss of loved ones, and alterations in social life. Those patients who feel
virtuous of their past, are able to cope in an effective manner with the aging process and also
become hopeful about their future. Taking into consideration the fact that the patient was also
under anti-depressant medications, care management will involve spending adequate time
her, demonstrating active listening skills, showing a willingness about her life and concerns,
and encouraging her to socially interact with others (Kanter et al., 2014). Efforts must be
taken to display kindness, concern, compassion, and empathy that will facilitate recovery
from the presenting complaints (Richardson, Percy & Hughes, 2015). In addition,
encouraging her friends and family members to pay her regular visits, will meet her social
needs.
Being aware of the unique desires, desires, and values of a patient, based on the
cultural principles, forms an essential aspect of care giving. This is predominantly significant
during care planning for residents, which in turn increases patient satisfaction and helps in the
development of a therapeutic nurse-patient relationship. Hence, the cultural beliefs of the
patient, in relation to how it perceives infirmity or illness, and the subsequent response to
health ailments must be paid due attention (Abdollahzadeh et al., 2014). The concept of
spirituality is most often allied with formal and organised religion that comprises of rituals
accumulation of fluid in the tissues that are perfused by peripheral vascular system located in
the lower extremities.
Psychosocial/Environmental/Economic aspects
Assistance must be provided to the patient for meeting her basic needs that
encompasses mental and emotional wellbeing. Efforts will be taken to create an environment
in the healthcare facility that makes the patient feel loved and secure. According to Swash et
al. (2014) being emotionally and mentally healthy suggests the presence of adequate coping
skills, in addition to gaining the competence of getting adjusted to major life changes such as,
depending on others, loss of loved ones, and alterations in social life. Those patients who feel
virtuous of their past, are able to cope in an effective manner with the aging process and also
become hopeful about their future. Taking into consideration the fact that the patient was also
under anti-depressant medications, care management will involve spending adequate time
her, demonstrating active listening skills, showing a willingness about her life and concerns,
and encouraging her to socially interact with others (Kanter et al., 2014). Efforts must be
taken to display kindness, concern, compassion, and empathy that will facilitate recovery
from the presenting complaints (Richardson, Percy & Hughes, 2015). In addition,
encouraging her friends and family members to pay her regular visits, will meet her social
needs.
Being aware of the unique desires, desires, and values of a patient, based on the
cultural principles, forms an essential aspect of care giving. This is predominantly significant
during care planning for residents, which in turn increases patient satisfaction and helps in the
development of a therapeutic nurse-patient relationship. Hence, the cultural beliefs of the
patient, in relation to how it perceives infirmity or illness, and the subsequent response to
health ailments must be paid due attention (Abdollahzadeh et al., 2014). The concept of
spirituality is most often allied with formal and organised religion that comprises of rituals
8REPORT
and a plethora of behaviours that focus on expression of faith. Hence, an essential way of
supporting the spiritual needs of the patient is to establish a good rapport with her, which in
turn will allow her to openly discuss her preferences and values. Presence of financial strain
has been frequently cited as imperative in the process of delivery of healthcare services.
Owing to the fact that family caregivers of the elderly patients often report fiscal strain allied
with their role as caregivers, efforts must be taken to reduce out-of-pocket expenses for the
patient, while increasing the availability of financial resources (Adelman et al., 2014). In
addition, the patient will also be referred to societal benefits that will encompass potential
cost saving amenities.
Ethical and legal aspects
It is imperative for the nursing professionals to comprehend that the standard of care
delivered to the patient must be reasonable, and in accordance to the codes of practice that
have been framed for the nation (Nicol & Nyatanga, 2017). Efforts will be taken to prevent
nursing malpractice that involves actions of misconduct, negligence, and breach of duty
(Butler & Lostritto, 2015). Care will be delivered to the patient in a way that does not
involve any offensive or harmful contact. In addition, the codes of practice will also be
followed for ensuring the presence of an effective communication, while providing support to
the patient, and fostering a culture of patient safety (NMBA, 2016). Patient advocacy will
also form a crucial aspect of care giving, whereby the aims and objectives of the treatment
interventions will be clarified (Cole, Wellard & Mummery, 2014). Necessary actions will be
taken to safeguard patient confidentiality, while adopting a person-centred approach that
allows the patient to take a lead in healthcare discussion and clinical decision making.
The standards will also be followed for conducting comprehensive health assessment,
and evaluating the outcomes of the patient, for informing nursing practice (NMBA, 2016).
Medical errors that lead to patient injury, and advanced directives will be taken into
and a plethora of behaviours that focus on expression of faith. Hence, an essential way of
supporting the spiritual needs of the patient is to establish a good rapport with her, which in
turn will allow her to openly discuss her preferences and values. Presence of financial strain
has been frequently cited as imperative in the process of delivery of healthcare services.
Owing to the fact that family caregivers of the elderly patients often report fiscal strain allied
with their role as caregivers, efforts must be taken to reduce out-of-pocket expenses for the
patient, while increasing the availability of financial resources (Adelman et al., 2014). In
addition, the patient will also be referred to societal benefits that will encompass potential
cost saving amenities.
Ethical and legal aspects
It is imperative for the nursing professionals to comprehend that the standard of care
delivered to the patient must be reasonable, and in accordance to the codes of practice that
have been framed for the nation (Nicol & Nyatanga, 2017). Efforts will be taken to prevent
nursing malpractice that involves actions of misconduct, negligence, and breach of duty
(Butler & Lostritto, 2015). Care will be delivered to the patient in a way that does not
involve any offensive or harmful contact. In addition, the codes of practice will also be
followed for ensuring the presence of an effective communication, while providing support to
the patient, and fostering a culture of patient safety (NMBA, 2016). Patient advocacy will
also form a crucial aspect of care giving, whereby the aims and objectives of the treatment
interventions will be clarified (Cole, Wellard & Mummery, 2014). Necessary actions will be
taken to safeguard patient confidentiality, while adopting a person-centred approach that
allows the patient to take a lead in healthcare discussion and clinical decision making.
The standards will also be followed for conducting comprehensive health assessment,
and evaluating the outcomes of the patient, for informing nursing practice (NMBA, 2016).
Medical errors that lead to patient injury, and advanced directives will be taken into
9REPORT
consideration. Owing to the fact that the patient’s daughter has the power of attorney and
guardianship, she will be given the responsibility of making healthcare decisions, when her
mother is incompetent. Hence, all information regarding the treatment modalities, their
potential impacts and adverse effects will be communicated to her daughter (DeMartino et
al., 2017).
Discharge planning
The process of discharge planning encompasses the carer, patient, family members
and other healthcare staff who have been involved in the caring for the patient. Thus, the
primary aim of discharge planning would be to ensure that the patient experiences a smooth
and safe discharge from the hospital (Hesselink et al., 2014). Input will be taken from her
carers, son and daughter, prior to formulating a plan. A discharge planning meeting will be
held at least a day, before she is released. Referral will be made for the patient receiving a
programmed fee under Medicare. Taking into consideration the future care needs of the
patient, she will be referred to meal-on-wheels program that will deliver her food under
circumstances when she is not able to participate in activities of daily living.
She will be informed about all medication changes, their dosage, timing, and route of
administration, in addition to providing contact numbers where she can seek immediate
assistance on observing certain adverse effects (Bowles et al., 2014). Provisions for follow-up
appointments will also be created with the general physician in order to facilitate faster
recovery. Referrals for community care packages will also be provided, with the aim of
meeting the tailored demands and preferences of the patient. This will be supervised by a case
manager who will support the patient. In addition, drawing up a family roster, creating back-
up plan, and making a discharge summary is imperative for easy transition from the hospital
to home (Gonçalves‐Bradley et al., 2016).
consideration. Owing to the fact that the patient’s daughter has the power of attorney and
guardianship, she will be given the responsibility of making healthcare decisions, when her
mother is incompetent. Hence, all information regarding the treatment modalities, their
potential impacts and adverse effects will be communicated to her daughter (DeMartino et
al., 2017).
Discharge planning
The process of discharge planning encompasses the carer, patient, family members
and other healthcare staff who have been involved in the caring for the patient. Thus, the
primary aim of discharge planning would be to ensure that the patient experiences a smooth
and safe discharge from the hospital (Hesselink et al., 2014). Input will be taken from her
carers, son and daughter, prior to formulating a plan. A discharge planning meeting will be
held at least a day, before she is released. Referral will be made for the patient receiving a
programmed fee under Medicare. Taking into consideration the future care needs of the
patient, she will be referred to meal-on-wheels program that will deliver her food under
circumstances when she is not able to participate in activities of daily living.
She will be informed about all medication changes, their dosage, timing, and route of
administration, in addition to providing contact numbers where she can seek immediate
assistance on observing certain adverse effects (Bowles et al., 2014). Provisions for follow-up
appointments will also be created with the general physician in order to facilitate faster
recovery. Referrals for community care packages will also be provided, with the aim of
meeting the tailored demands and preferences of the patient. This will be supervised by a case
manager who will support the patient. In addition, drawing up a family roster, creating back-
up plan, and making a discharge summary is imperative for easy transition from the hospital
to home (Gonçalves‐Bradley et al., 2016).
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10REPORT
Education needs of patient /family
According to Feltner et al. (2014) preventing patient re-hospitalization is a vast
responsibility, particularly in consideration of expensive prices that are imposed for early
readmissions. Hence, patient teaching must be constantly improved, prior to
discharge. Support staff must be delegated with additional responsibilities that focus on
educating the patient and her family members on her presenting complaints, particular CCF
and asthma. All misinformation must be rectified, followed by questioning patient
understanding of care, and using return demonstration, at the time of caregiving. Patient
education will use technology for customising and printing education resources (Shin, Park &
Kim, 2015). In addition, the limitations and strengths of the patient will be taken into
consideration, while providing verbal instructions and/or visual education materials.
Involving the family members in patient education will also improves the probabilities the
directions are followed.
Conclusion
To conclude, the case involves a patient Mrs P, who reports a history of two major
medical conditions namely, CCF and asthma, besides the signs and symptoms of insomnia,
atrial fibrillation, and oedema in the lower extremities. While the short-term outcomes
encompass management of the narrowed airways, and overloaded ventricles, the long-term
outcomes focus on improving her physical and mental wellbeing. Therefore, a person-centred
care approach must be adopted for treatment of the patient, and enhancing her quick
recuperation.
Education needs of patient /family
According to Feltner et al. (2014) preventing patient re-hospitalization is a vast
responsibility, particularly in consideration of expensive prices that are imposed for early
readmissions. Hence, patient teaching must be constantly improved, prior to
discharge. Support staff must be delegated with additional responsibilities that focus on
educating the patient and her family members on her presenting complaints, particular CCF
and asthma. All misinformation must be rectified, followed by questioning patient
understanding of care, and using return demonstration, at the time of caregiving. Patient
education will use technology for customising and printing education resources (Shin, Park &
Kim, 2015). In addition, the limitations and strengths of the patient will be taken into
consideration, while providing verbal instructions and/or visual education materials.
Involving the family members in patient education will also improves the probabilities the
directions are followed.
Conclusion
To conclude, the case involves a patient Mrs P, who reports a history of two major
medical conditions namely, CCF and asthma, besides the signs and symptoms of insomnia,
atrial fibrillation, and oedema in the lower extremities. While the short-term outcomes
encompass management of the narrowed airways, and overloaded ventricles, the long-term
outcomes focus on improving her physical and mental wellbeing. Therefore, a person-centred
care approach must be adopted for treatment of the patient, and enhancing her quick
recuperation.
11REPORT
References
Abdollahzadeh, F., Moradi, N., Pakpour, V., Rahmani, A., Zamanzadeh, V.,
Mohammadpoorasl, A., & Howard, F. (2014). Un-met supportive care needs of
Iranian breast cancer patients. Asian Pac J Cancer Prev, 15(9), 3933-8.
Adelman, R. D., Tmanova, L. L., Delgado, D., Dion, S., & Lachs, M. S. (2014). Caregiver
burden: a clinical review. Jama, 311(10), 1052-1060.
Ali, R. M., Salah, D., & Mansour, D. Y. (2015). The effect of nitroglycerin infusion versus
hydralazine infusion as antihypertensive therapy in acute management of patients with
severe pre-eclampsia. Ain-Shams Journal of Anaesthesiology, 8(4), 499.
Bastawrous, A., Rono, H. K., Livingstone, I. A., Weiss, H. A., Jordan, S., Kuper, H., &
Burton, M. J. (2015). Development and validation of a smartphone-based visual
acuity test (peek acuity) for clinical practice and community-based fieldwork. JAMA
ophthalmology, 133(8), 930-937.
Bloom, M. W., Hamo, C. E., Cardinale, D., Ky, B., Nohria, A., Baer, L., ... & Butler, J.
(2016). Cancer Therapy–Related Cardiac Dysfunction and Heart Failure: Part 1:
Definitions, Pathophysiology, Risk Factors, and Imaging. Circulation: Heart
Failure, 9(1), e002661.
Bowles, K. H., Hanlon, A., Holland, D., Potashnik, S. L., & Topaz, M. (2014). Impact of
discharge planning decision support on time to readmission among older adult
medical patients. Professional case management, 19(1), 29.
Butler, K. A., & Lostritto, M. D. (2015). Malpractice 101: strategies for defending your
practice. Journal of Radiology Nursing, 34(1), 13-24.
References
Abdollahzadeh, F., Moradi, N., Pakpour, V., Rahmani, A., Zamanzadeh, V.,
Mohammadpoorasl, A., & Howard, F. (2014). Un-met supportive care needs of
Iranian breast cancer patients. Asian Pac J Cancer Prev, 15(9), 3933-8.
Adelman, R. D., Tmanova, L. L., Delgado, D., Dion, S., & Lachs, M. S. (2014). Caregiver
burden: a clinical review. Jama, 311(10), 1052-1060.
Ali, R. M., Salah, D., & Mansour, D. Y. (2015). The effect of nitroglycerin infusion versus
hydralazine infusion as antihypertensive therapy in acute management of patients with
severe pre-eclampsia. Ain-Shams Journal of Anaesthesiology, 8(4), 499.
Bastawrous, A., Rono, H. K., Livingstone, I. A., Weiss, H. A., Jordan, S., Kuper, H., &
Burton, M. J. (2015). Development and validation of a smartphone-based visual
acuity test (peek acuity) for clinical practice and community-based fieldwork. JAMA
ophthalmology, 133(8), 930-937.
Bloom, M. W., Hamo, C. E., Cardinale, D., Ky, B., Nohria, A., Baer, L., ... & Butler, J.
(2016). Cancer Therapy–Related Cardiac Dysfunction and Heart Failure: Part 1:
Definitions, Pathophysiology, Risk Factors, and Imaging. Circulation: Heart
Failure, 9(1), e002661.
Bowles, K. H., Hanlon, A., Holland, D., Potashnik, S. L., & Topaz, M. (2014). Impact of
discharge planning decision support on time to readmission among older adult
medical patients. Professional case management, 19(1), 29.
Butler, K. A., & Lostritto, M. D. (2015). Malpractice 101: strategies for defending your
practice. Journal of Radiology Nursing, 34(1), 13-24.
12REPORT
Cole, C., Wellard, S., & Mummery, J. (2014). Problematising autonomy and advocacy in
nursing. Nursing ethics, 21(5), 576-582.
DeMartino, E. S., Dudzinski, D. M., Doyle, C. K., Sperry, B. P., Gregory, S. E., Siegler,
M., ... & Kramer, D. B. (2017). Who decides when a patient can’t? Statutes on
alternate decision makers. The New England journal of medicine, 376(15), 1478.
Ding, J., Chen, F., Zhai, W., Zhao, H., & Pan, Y. (2014). Orbicularis oculi muscle
transposition for repairing involutional lower eyelid entropion. Graefe's Archive for
Clinical and Experimental Ophthalmology, 252(8), 1315-1318.
Feltner, C., Jones, C. D., Cené, C. W., Zheng, Z. J., Sueta, C. A., Coker-Schwimmer, E. J., ...
& Jonas, D. E. (2014). Transitional care interventions to prevent readmissions for
persons with heart failure: a systematic review and meta-analysis. Annals of internal
medicine, 160(11), 774-784.
Gonçalves‐Bradley, D. C., Lannin, N. A., Clemson, L. M., Cameron, I. D., & Shepperd, S.
(2016). Discharge planning from hospital. Cochrane Database of Systematic Reviews,
(1).
Hesselink, G., Zegers, M., Vernooij-Dassen, M., Barach, P., Kalkman, C., Flink, M., ... &
Suñol, R. (2014). Improving patient discharge and reducing hospital readmissions by
using Intervention Mapping. BMC health services research, 14(1), 389.
Kanter, C., D’Agostino, N. M., Daniels, M., Stone, A., & Edelstein, K. (2014). Together and
apart: providing psychosocial support for patients and families living with brain
tumors. Supportive Care in Cancer, 22(1), 43-52.
Cole, C., Wellard, S., & Mummery, J. (2014). Problematising autonomy and advocacy in
nursing. Nursing ethics, 21(5), 576-582.
DeMartino, E. S., Dudzinski, D. M., Doyle, C. K., Sperry, B. P., Gregory, S. E., Siegler,
M., ... & Kramer, D. B. (2017). Who decides when a patient can’t? Statutes on
alternate decision makers. The New England journal of medicine, 376(15), 1478.
Ding, J., Chen, F., Zhai, W., Zhao, H., & Pan, Y. (2014). Orbicularis oculi muscle
transposition for repairing involutional lower eyelid entropion. Graefe's Archive for
Clinical and Experimental Ophthalmology, 252(8), 1315-1318.
Feltner, C., Jones, C. D., Cené, C. W., Zheng, Z. J., Sueta, C. A., Coker-Schwimmer, E. J., ...
& Jonas, D. E. (2014). Transitional care interventions to prevent readmissions for
persons with heart failure: a systematic review and meta-analysis. Annals of internal
medicine, 160(11), 774-784.
Gonçalves‐Bradley, D. C., Lannin, N. A., Clemson, L. M., Cameron, I. D., & Shepperd, S.
(2016). Discharge planning from hospital. Cochrane Database of Systematic Reviews,
(1).
Hesselink, G., Zegers, M., Vernooij-Dassen, M., Barach, P., Kalkman, C., Flink, M., ... &
Suñol, R. (2014). Improving patient discharge and reducing hospital readmissions by
using Intervention Mapping. BMC health services research, 14(1), 389.
Kanter, C., D’Agostino, N. M., Daniels, M., Stone, A., & Edelstein, K. (2014). Together and
apart: providing psychosocial support for patients and families living with brain
tumors. Supportive Care in Cancer, 22(1), 43-52.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13REPORT
Korhan, E. A., Uyar, M., Eyigör, C., Yönt, G. H., Çelik, S., & Khorshıd, L. (2014). The
effects of music therapy on pain in patients with neuropathic pain. Pain Management
Nursing, 15(1), 306-314.
Maslan, J., & Mims, J. W. (2014). What is asthma? Pathophysiology, demographics, and
health care costs. Otolaryngologic Clinics of North America, 47(1), 13-22.
Musini, V. M., Nazer, M., Bassett, K., & Wright, J. M. (2014). Blood pressure‐lowering
efficacy of monotherapy with thiazide diuretics for primary hypertension. Cochrane
Database of Systematic Reviews, (5).
Nicol, J., & Nyatanga, B. (2017). Palliative and end of life care in nursing. Learning Matters.
Nursing and Midwifery Board of Australia. (2016). Registered nurse standards for practice.
Retrieved from https://www.nursingmidwiferyboard.gov.au/codes-guidelines-
statements/professional-standards/registered-nurse-standards-for-practice.aspx
Peters, S. P., Bleecker, E. R., Canonica, G. W., Park, Y. B., Ramirez, R., Hollis, S., ... &
Martin, U. J. (2016). Serious asthma events with budesonide plus formoterol vs.
budesonide alone. New England Journal of Medicine, 375(9), 850-860.
Richardson, C., Percy, M., & Hughes, J. (2015). Nursing therapeutics: teaching student
nurses care, compassion and empathy. Nurse Education Today, 35(5), e1-e5.
Rolf, S., Kircher, S., Arya, A., Eitel, C., Sommer, P., Richter, S., ... & Hindricks, G. (2014).
Tailored atrial substrate modification based on low-voltage areas in catheter ablation
of atrial fibrillation. Circulation: Arrhythmia and Electrophysiology, 7(5), 825-833.
Schweitzer, P. K., & Feren, S. D. (2017). Pharmacological treatment of insomnia. In Clinical
handbook of insomnia(pp. 97-132). Springer, Cham.
Korhan, E. A., Uyar, M., Eyigör, C., Yönt, G. H., Çelik, S., & Khorshıd, L. (2014). The
effects of music therapy on pain in patients with neuropathic pain. Pain Management
Nursing, 15(1), 306-314.
Maslan, J., & Mims, J. W. (2014). What is asthma? Pathophysiology, demographics, and
health care costs. Otolaryngologic Clinics of North America, 47(1), 13-22.
Musini, V. M., Nazer, M., Bassett, K., & Wright, J. M. (2014). Blood pressure‐lowering
efficacy of monotherapy with thiazide diuretics for primary hypertension. Cochrane
Database of Systematic Reviews, (5).
Nicol, J., & Nyatanga, B. (2017). Palliative and end of life care in nursing. Learning Matters.
Nursing and Midwifery Board of Australia. (2016). Registered nurse standards for practice.
Retrieved from https://www.nursingmidwiferyboard.gov.au/codes-guidelines-
statements/professional-standards/registered-nurse-standards-for-practice.aspx
Peters, S. P., Bleecker, E. R., Canonica, G. W., Park, Y. B., Ramirez, R., Hollis, S., ... &
Martin, U. J. (2016). Serious asthma events with budesonide plus formoterol vs.
budesonide alone. New England Journal of Medicine, 375(9), 850-860.
Richardson, C., Percy, M., & Hughes, J. (2015). Nursing therapeutics: teaching student
nurses care, compassion and empathy. Nurse Education Today, 35(5), e1-e5.
Rolf, S., Kircher, S., Arya, A., Eitel, C., Sommer, P., Richter, S., ... & Hindricks, G. (2014).
Tailored atrial substrate modification based on low-voltage areas in catheter ablation
of atrial fibrillation. Circulation: Arrhythmia and Electrophysiology, 7(5), 825-833.
Schweitzer, P. K., & Feren, S. D. (2017). Pharmacological treatment of insomnia. In Clinical
handbook of insomnia(pp. 97-132). Springer, Cham.
14REPORT
Shin, S., Park, J. H., & Kim, J. H. (2015). Effectiveness of patient simulation in nursing
education: meta-analysis. Nurse education today, 35(1), 176-182.
Swash, B., Hulbert-Williams, N., & Bramwell, R. (2014). Unmet psychosocial needs in
haematological cancer: a systematic review. Supportive Care in Cancer, 22(4), 1131-
1141.
Tham, Y. K., Bernardo, B. C., Ooi, J. Y., Weeks, K. L., & McMullen, J. R. (2015).
Pathophysiology of cardiac hypertrophy and heart failure: signaling pathways and
novel therapeutic targets. Archives of toxicology, 89(9), 1401-1438.
Wenzel, S., Castro, M., Corren, J., Maspero, J., Wang, L., Zhang, B., ... & Eckert, L. (2016).
Dupilumab efficacy and safety in adults with uncontrolled persistent asthma despite
use of medium-to-high-dose inhaled corticosteroids plus a long-acting β2 agonist: a
randomised double-blind placebo-controlled pivotal phase 2b dose-ranging trial. The
Lancet, 388(10039), 31-44.
Wysham, N. G., Miriovsky, B. J., Currow, D. C., Herndon II, J. E., Samsa, G. P., Wilcock,
A., & Abernethy, A. P. (2015). Practical dyspnea assessment: relationship between
the 0–10 numerical rating scale and the four-level categorical verbal descriptor scale
of dyspnea intensity. Journal of pain and symptom management, 50(4), 480-487.
Shin, S., Park, J. H., & Kim, J. H. (2015). Effectiveness of patient simulation in nursing
education: meta-analysis. Nurse education today, 35(1), 176-182.
Swash, B., Hulbert-Williams, N., & Bramwell, R. (2014). Unmet psychosocial needs in
haematological cancer: a systematic review. Supportive Care in Cancer, 22(4), 1131-
1141.
Tham, Y. K., Bernardo, B. C., Ooi, J. Y., Weeks, K. L., & McMullen, J. R. (2015).
Pathophysiology of cardiac hypertrophy and heart failure: signaling pathways and
novel therapeutic targets. Archives of toxicology, 89(9), 1401-1438.
Wenzel, S., Castro, M., Corren, J., Maspero, J., Wang, L., Zhang, B., ... & Eckert, L. (2016).
Dupilumab efficacy and safety in adults with uncontrolled persistent asthma despite
use of medium-to-high-dose inhaled corticosteroids plus a long-acting β2 agonist: a
randomised double-blind placebo-controlled pivotal phase 2b dose-ranging trial. The
Lancet, 388(10039), 31-44.
Wysham, N. G., Miriovsky, B. J., Currow, D. C., Herndon II, J. E., Samsa, G. P., Wilcock,
A., & Abernethy, A. P. (2015). Practical dyspnea assessment: relationship between
the 0–10 numerical rating scale and the four-level categorical verbal descriptor scale
of dyspnea intensity. Journal of pain and symptom management, 50(4), 480-487.
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





