Lifespan Nutrition Research Paper 2022
VerifiedAdded on 2022/10/14
|14
|3770
|12
AI Summary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: LIFESPAN NUTRITION
LIFESPAN NUTRITION
Name of the Student:
Name of the University:
Author note:
LIFESPAN NUTRITION
Name of the Student:
Name of the University:
Author note:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1LIFESPAN NUTRITION
Part A
Physiological Changes and Nutrition Requirements
One of the major physiological changes associated with ageing is sarcopenia – which
implies an age associated loss of the numbers and size of muscle fibers. Muscle changes are also
accompanied by the loss of bone density due to hindrances in bone remodeling mechanisms [1].
Not only do these age-associated physiological changes result in lean muscle mass loss and
frailty, but also results in increased protein and calcium based nutritional needs across the elderly
[2].
Ageing is also associated increased rates of oxidative stress and resultant inflammatory
neuronal atrophy, cerebral shrinkage and emergence of neurodegenerative diseases. The
increased oxidative stress also results in immunological compromises and accumulation of
advanced glycation end products (AGEs) which increase the risk of chronic and infectious
disease acquisition across the elderly. Such immunological impacts across the elderly enhance
the nutritional needs of consuming a diet rich in antioxidants and micronutrients [3].
Nutritional Concerns
With ageing, the stomach’s ability to secret digestive juices decreases resulting in
digestive difficulties as well as hindrances in the absorption and cellular assimilation of nutrients
within the body. This results in decreased appetite, increased incidences of gastrointestinal
disturbances and reduced ability to utilize nutrients from the food consumed [4]. This implies
that the digestive and absorptive capacities of the elderly within the aged care facility must be
Part A
Physiological Changes and Nutrition Requirements
One of the major physiological changes associated with ageing is sarcopenia – which
implies an age associated loss of the numbers and size of muscle fibers. Muscle changes are also
accompanied by the loss of bone density due to hindrances in bone remodeling mechanisms [1].
Not only do these age-associated physiological changes result in lean muscle mass loss and
frailty, but also results in increased protein and calcium based nutritional needs across the elderly
[2].
Ageing is also associated increased rates of oxidative stress and resultant inflammatory
neuronal atrophy, cerebral shrinkage and emergence of neurodegenerative diseases. The
increased oxidative stress also results in immunological compromises and accumulation of
advanced glycation end products (AGEs) which increase the risk of chronic and infectious
disease acquisition across the elderly. Such immunological impacts across the elderly enhance
the nutritional needs of consuming a diet rich in antioxidants and micronutrients [3].
Nutritional Concerns
With ageing, the stomach’s ability to secret digestive juices decreases resulting in
digestive difficulties as well as hindrances in the absorption and cellular assimilation of nutrients
within the body. This results in decreased appetite, increased incidences of gastrointestinal
disturbances and reduced ability to utilize nutrients from the food consumed [4]. This implies
that the digestive and absorptive capacities of the elderly within the aged care facility must be
2LIFESPAN NUTRITION
considered and hence, calls for the need to provide them nutritious foods which are easily to
digest and hence can easily be utilized for positive health sustenance [5].
Neuronal loss during ageing is associated with decreased sensory abilities within the
elderly resulting in reduced taste and olfactory acuity. This results in the elderly finding it
difficult to acquire the same smell and taste of food as compared to adulthood as well as
encountering difficulties in the swallowing and ingestion of food. Such changes coupled with
loss of appetite and digestive capacity reduce food intake across the elderly [6]. Reduced food
intake along with age associated catabolism result in nutritional concerns in the form of
malnutrition, poor or deficient nutrient status and aggravated frailty and disease risk across the
elderly. Thus, to assist in food consumption and nutritional absorption, there is a need to provide
texturally modified and nutritionally balanced foods [7].
ABCD Indicators
Considering that osteoporosis is characterized by losses in bone mass and density – it is
likely that individuals with a small skeletal frame and reduced bone mass are at risk of acquiring
the condition. This implies that prevalence of frailty and abnormally low body mass are
anthropometric risk factors indicative of osteoporosis susceptibility across the elderly [8].
Nutrients like calcium, phosphorus and vitamin D are essential for bone development. Thus
abnormally low serum levels of calcium, phosphorous and vitamin D are key clinical indicators
that can be used to assess osteoporosis risk within the elderly of the aged care facility [9]. Due to
its association with loss of bone density, a bone density value of 2.5 standard deviations or lower
as compared to mean values in adults is indicative of osteoporosis risk within the elderly.
Additionally, a diet which is inadequate in calcium and vitamin D-rich foods like dairy, fortified
considered and hence, calls for the need to provide them nutritious foods which are easily to
digest and hence can easily be utilized for positive health sustenance [5].
Neuronal loss during ageing is associated with decreased sensory abilities within the
elderly resulting in reduced taste and olfactory acuity. This results in the elderly finding it
difficult to acquire the same smell and taste of food as compared to adulthood as well as
encountering difficulties in the swallowing and ingestion of food. Such changes coupled with
loss of appetite and digestive capacity reduce food intake across the elderly [6]. Reduced food
intake along with age associated catabolism result in nutritional concerns in the form of
malnutrition, poor or deficient nutrient status and aggravated frailty and disease risk across the
elderly. Thus, to assist in food consumption and nutritional absorption, there is a need to provide
texturally modified and nutritionally balanced foods [7].
ABCD Indicators
Considering that osteoporosis is characterized by losses in bone mass and density – it is
likely that individuals with a small skeletal frame and reduced bone mass are at risk of acquiring
the condition. This implies that prevalence of frailty and abnormally low body mass are
anthropometric risk factors indicative of osteoporosis susceptibility across the elderly [8].
Nutrients like calcium, phosphorus and vitamin D are essential for bone development. Thus
abnormally low serum levels of calcium, phosphorous and vitamin D are key clinical indicators
that can be used to assess osteoporosis risk within the elderly of the aged care facility [9]. Due to
its association with loss of bone density, a bone density value of 2.5 standard deviations or lower
as compared to mean values in adults is indicative of osteoporosis risk within the elderly.
Additionally, a diet which is inadequate in calcium and vitamin D-rich foods like dairy, fortified
3LIFESPAN NUTRITION
cereals, butter, mushrooms, soy, fatty fish, nuts and seeds is a major dietary indicator
highlighting the risk of osteoporosis [10].
Part B
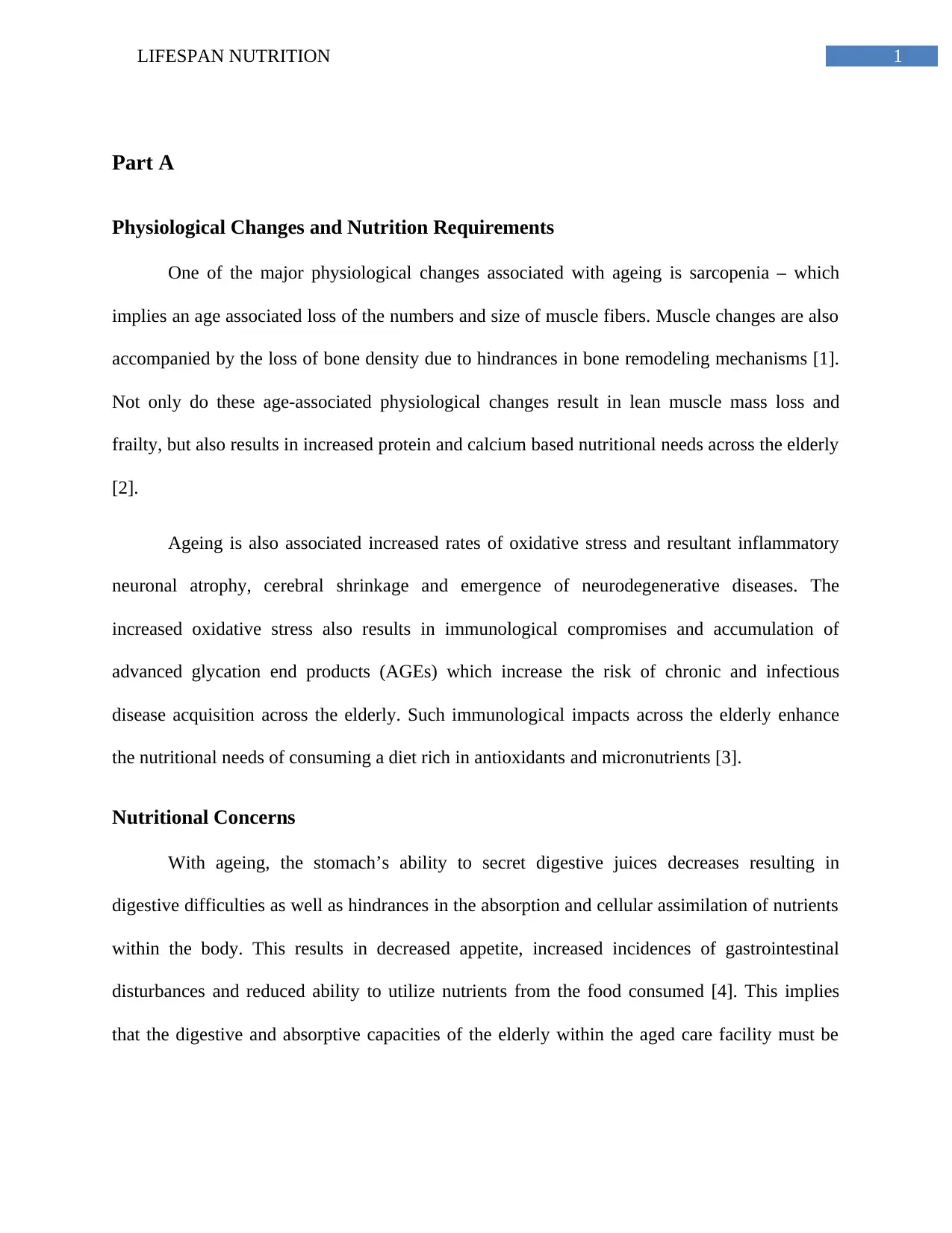
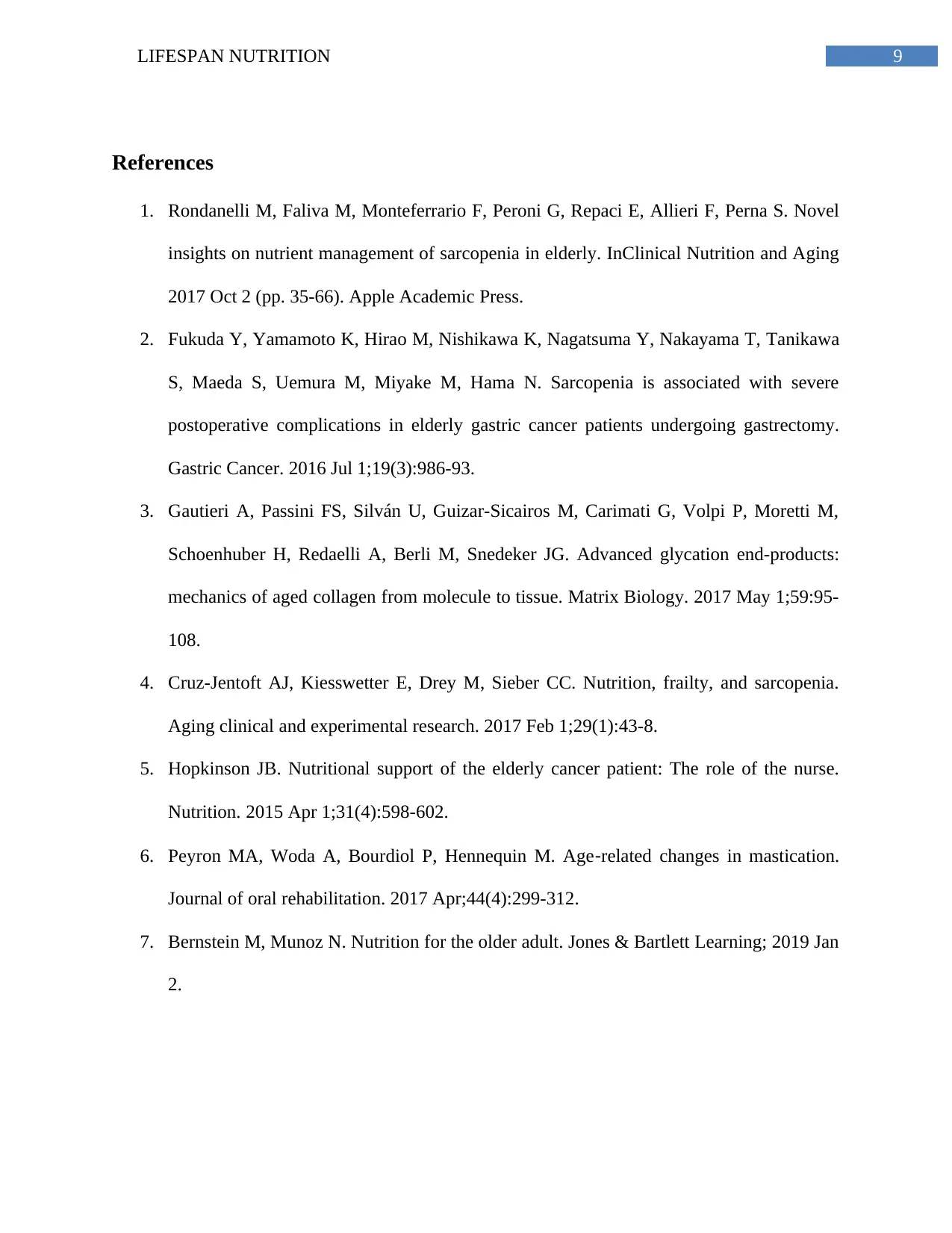
Table 1. Food Intake Analysis
Nutrient (per day) Amount Nutrient Reference Values
[11]
Energy, kJ 4307 kJ EERM: 6517 kJ, DEER: 7121
kJ
Carbohydrates: Grams, % E 115 g, 44% AMDR: 45 to 65%
Proteins: Grams, % E 51 g, 20% RDI: 47 g, AMDR: 15 to 25%
Total Fat: Grams, % E 39 g, 33% AMDR: 20 to 35%
Saturated Fat: Grams, % E 15 g, 13% AMDR: Less than 10%
Water, g 1763 g AI: 2800 g
Fiber, g 10 g AI: 25 g
Sodium, mg 1126.58 mg AI: 460 mg
Iron, mg 6.98 mg EAR: 5 mg, RDI: 8 mg, UL:
45 mg
Zinc, mg 4.60 mg EAR: 6.5 mg, RDI: 8 mg, UL:
40 mg
Iodine, μg 71.35 μmg EAR: 100 μg, RDI: 150 μg,
UL: 1100 μg
Calcium, mg 445.59 mg EAR: 1100 mg, RDI: 1300
mg, UI: 2500 mg
Vitamin C, mg 46.91 mg EAR: 30 mg, RDI: 45
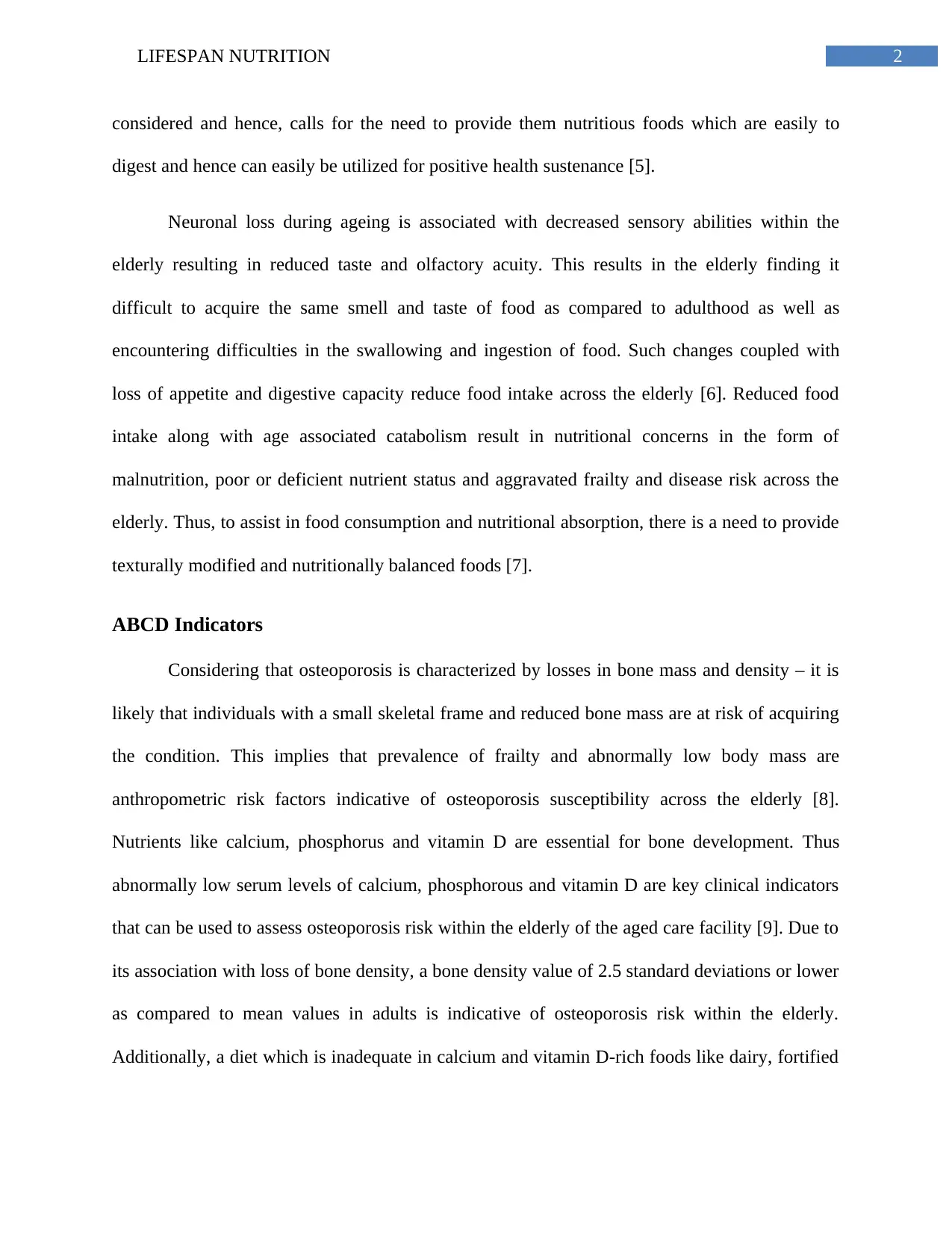
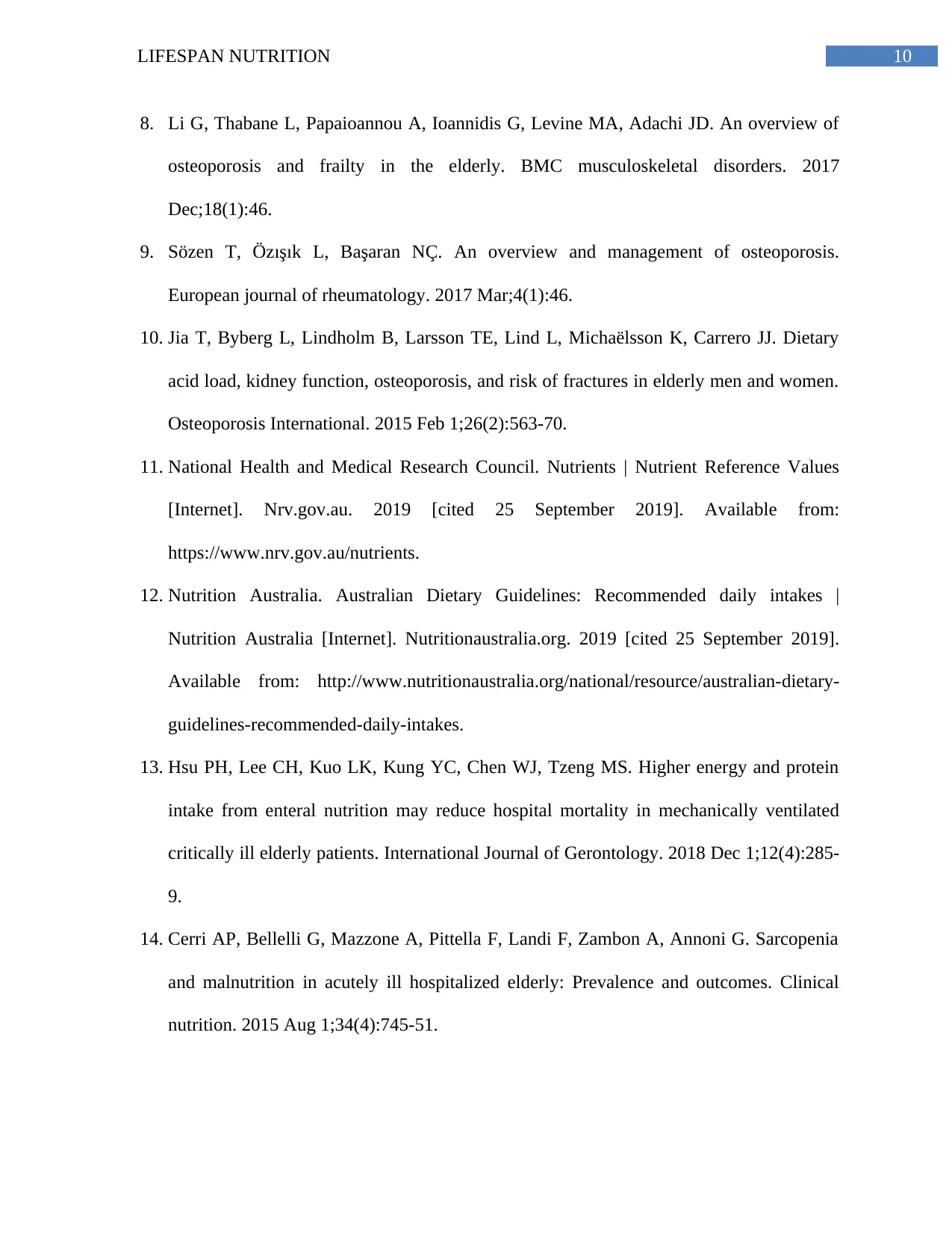
Table 2. Servings Consumed
Food Groups Number of serves consumed ADG recommended servings
[12]
Grain (cereal) foods 0.4 3
Vegetables and legume/beans Vegetables: 1.7, Legumes: 0.0 5
Fruit Fruit: 0.0 2
Lean meats and poultry, fish,
eggs, tofu, nuts, seeds and
legumes/beans
Lean meats and poultry: 0, fish:
0, eggs: 0, soy products: 0.0, nuts
and seeds: 0.0, legumes/beans:
0.0
2
Milk, yoghurt, cheese and/or
alternatives, mostly reduced fat
0.4 4
cereals, butter, mushrooms, soy, fatty fish, nuts and seeds is a major dietary indicator
highlighting the risk of osteoporosis [10].
Part B
Table 1. Food Intake Analysis
Nutrient (per day) Amount Nutrient Reference Values
[11]
Energy, kJ 4307 kJ EERM: 6517 kJ, DEER: 7121
kJ
Carbohydrates: Grams, % E 115 g, 44% AMDR: 45 to 65%
Proteins: Grams, % E 51 g, 20% RDI: 47 g, AMDR: 15 to 25%
Total Fat: Grams, % E 39 g, 33% AMDR: 20 to 35%
Saturated Fat: Grams, % E 15 g, 13% AMDR: Less than 10%
Water, g 1763 g AI: 2800 g
Fiber, g 10 g AI: 25 g
Sodium, mg 1126.58 mg AI: 460 mg
Iron, mg 6.98 mg EAR: 5 mg, RDI: 8 mg, UL:
45 mg
Zinc, mg 4.60 mg EAR: 6.5 mg, RDI: 8 mg, UL:
40 mg
Iodine, μg 71.35 μmg EAR: 100 μg, RDI: 150 μg,
UL: 1100 μg
Calcium, mg 445.59 mg EAR: 1100 mg, RDI: 1300
mg, UI: 2500 mg
Vitamin C, mg 46.91 mg EAR: 30 mg, RDI: 45
Table 2. Servings Consumed
Food Groups Number of serves consumed ADG recommended servings
[12]
Grain (cereal) foods 0.4 3
Vegetables and legume/beans Vegetables: 1.7, Legumes: 0.0 5
Fruit Fruit: 0.0 2
Lean meats and poultry, fish,
eggs, tofu, nuts, seeds and
legumes/beans
Lean meats and poultry: 0, fish:
0, eggs: 0, soy products: 0.0, nuts
and seeds: 0.0, legumes/beans:
0.0
2
Milk, yoghurt, cheese and/or
alternatives, mostly reduced fat
0.4 4
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4LIFESPAN NUTRITION
3. Dietary Intake
One of the first components of dietary intake which is of significance is the Agnes’s
inadequate consumption of energy. It can be observed that Agnes’s total energy intake is much
less as compared to the recommended Nutrient Reference Values (NRV) (Table 1). The reasons
underlying such low calorie intake can be attributed to the types of food servings prevalent in her
diet. It is known that carbohydrates, especially whole grains, fresh fruits, legumes, beans and
even foods which contain moderate quantities of fats, such as nuts and seeds, are key
contributors to an individual’s energy intake [13]. Not only is Agnes’s present diet inadequate in
total calories, she is also consuming deficient servings of the above energy-giving foods. Old age
accompanied by catabolism and increased muscle wastage. Thus, consumption of a diet low in
energy is likely to result in muscle mass loss, frailty and anthropometric measurements within
the elderly individual [14]. Indeed, such an association between inadequate dietary intake and
abnormally low anthropometric measurements like BMI can be observed in Agnes. Such
inadequate dietary consumption may aggravate rates of catabolism and result in loss of tissue and
immunological capacity in elderly individuals like Agnes – thus increasing her risk for chronic
disease acquisition in the process [15].
Findings from her dietary intake analysis indeed indicate her consumption of sodium to
much higher than the recommended NRVs (Table 1). A high consumption of sodium is
associated with hypertension – as evident in Agnes’s present conditions [16]. Further, ageing is
associated with cardiovascular changes such as: atrial fibrillation, stiffening of the blood vessels
and valves and reduced functioning of cardiac baroreceptors – the primary physiological agents
which play a key role in regulating the body’s blood pressure. Thus, age related mechanisms will
3. Dietary Intake
One of the first components of dietary intake which is of significance is the Agnes’s
inadequate consumption of energy. It can be observed that Agnes’s total energy intake is much
less as compared to the recommended Nutrient Reference Values (NRV) (Table 1). The reasons
underlying such low calorie intake can be attributed to the types of food servings prevalent in her
diet. It is known that carbohydrates, especially whole grains, fresh fruits, legumes, beans and
even foods which contain moderate quantities of fats, such as nuts and seeds, are key
contributors to an individual’s energy intake [13]. Not only is Agnes’s present diet inadequate in
total calories, she is also consuming deficient servings of the above energy-giving foods. Old age
accompanied by catabolism and increased muscle wastage. Thus, consumption of a diet low in
energy is likely to result in muscle mass loss, frailty and anthropometric measurements within
the elderly individual [14]. Indeed, such an association between inadequate dietary intake and
abnormally low anthropometric measurements like BMI can be observed in Agnes. Such
inadequate dietary consumption may aggravate rates of catabolism and result in loss of tissue and
immunological capacity in elderly individuals like Agnes – thus increasing her risk for chronic
disease acquisition in the process [15].
Findings from her dietary intake analysis indeed indicate her consumption of sodium to
much higher than the recommended NRVs (Table 1). A high consumption of sodium is
associated with hypertension – as evident in Agnes’s present conditions [16]. Further, ageing is
associated with cardiovascular changes such as: atrial fibrillation, stiffening of the blood vessels
and valves and reduced functioning of cardiac baroreceptors – the primary physiological agents
which play a key role in regulating the body’s blood pressure. Thus, age related mechanisms will
5LIFESPAN NUTRITION
aggravate the hypertensive effects of a high sodium diet and hence, increase the risk of an elderly
person like Agnes to acquire fatal cardiovascular consequences such as myocardial infarction
and stroke [17].
Additionally, it is known to us that Agnes has high levels of blood cholesterol. From the
dietary intake analysis results, it can be observed that while Agnes’s consumption of total fats is
within recommended NRV values, her saturated fat intake is exceeding the recommendations
(Table 1). Interestingly, it can be observed that Agnes is not consuming any food servings which
are potential sources of saturated fat – that is, red meats or processed foods. However, the
serving intake findings reveal that Agnes is consuming other sources of saturated fats, that is,
ham, butter and mayonnaise [18]. Further, Agnes’s diet is deficient in any form of unsaturated
fats such as oils, nuts and seeds. (Table 2). The type also reveals Agnes’s prevalent consumption
of foods rich in added sugars such as marmalade, packaged biscuits and processed fruit juices
(Table 2). As highlighted previously, ageing is associated with lower metabolic rates and
muscular mass which is why, the elderly find it difficult to metabolize nutrients in their food,
which is why it is likely that the calories obtained from Agnes’s sugar consumption are being
rapidly metabolized into adipose tissue accumulations [19]. Thus, even though Agnes’s
consumption of food servings are relatively low, her increased sugar and saturated fat
consumption coupled with the physiological and metabolic impacts of ageing have contributed to
her high cholesterol levels. If not controlled, excessive consumption of foods rich in saturated fat
and sugars have been evidenced to increase blood levels of cholesterol and triglycerides – as
observed in Agnes – which can further increase her risk of acquiring cardiovascular diseases like
stroke and myocardial infarction [20]. It has also been evidenced that cardiovascular disease risk
due to the high blood cholesterol are further enhanced due to hypertension – another condition
aggravate the hypertensive effects of a high sodium diet and hence, increase the risk of an elderly
person like Agnes to acquire fatal cardiovascular consequences such as myocardial infarction
and stroke [17].
Additionally, it is known to us that Agnes has high levels of blood cholesterol. From the
dietary intake analysis results, it can be observed that while Agnes’s consumption of total fats is
within recommended NRV values, her saturated fat intake is exceeding the recommendations
(Table 1). Interestingly, it can be observed that Agnes is not consuming any food servings which
are potential sources of saturated fat – that is, red meats or processed foods. However, the
serving intake findings reveal that Agnes is consuming other sources of saturated fats, that is,
ham, butter and mayonnaise [18]. Further, Agnes’s diet is deficient in any form of unsaturated
fats such as oils, nuts and seeds. (Table 2). The type also reveals Agnes’s prevalent consumption
of foods rich in added sugars such as marmalade, packaged biscuits and processed fruit juices
(Table 2). As highlighted previously, ageing is associated with lower metabolic rates and
muscular mass which is why, the elderly find it difficult to metabolize nutrients in their food,
which is why it is likely that the calories obtained from Agnes’s sugar consumption are being
rapidly metabolized into adipose tissue accumulations [19]. Thus, even though Agnes’s
consumption of food servings are relatively low, her increased sugar and saturated fat
consumption coupled with the physiological and metabolic impacts of ageing have contributed to
her high cholesterol levels. If not controlled, excessive consumption of foods rich in saturated fat
and sugars have been evidenced to increase blood levels of cholesterol and triglycerides – as
observed in Agnes – which can further increase her risk of acquiring cardiovascular diseases like
stroke and myocardial infarction [20]. It has also been evidenced that cardiovascular disease risk
due to the high blood cholesterol are further enhanced due to hypertension – another condition
6LIFESPAN NUTRITION
which has been observed in Agnes. Thus, the above analysis clearly reveals the link between
Agnes’s present food consumption patterns and her existing medical conditions [21 ] .
Upon closely evaluating the dietary intake analysis of Agnes’s food consumption, it can
be observed that the her intake of calcium is deficient in comparison to the recommended NRVs
(Table 1). Not only is Agnes’s diet devoid of any form of foods rich in calcium (dairy, nuts,
seeds, green leafy vegetables) (Table 2) her BMI also belongs to the below normal range. Such
findings are of concern since frailty, underweight status and a diet deficient in calcium are major
risk factors of osteoporosis within the elderly [22]. Agnes has also been found to spend most of
time indoors - thus depriving her of vitamin D from sunlight, the key nutrient responsible for the
enhancing calcium absorption. Thus, taking insights from the results of her dietary and
anthropometric measurements, therapeutic interventions must be immediately taken to correct
Agnes’s risk and her potential susceptibility of acquiring fractures in the future [23].
4. Reasons for Inadequacy
It is known that old age is associated with decreased sensory capacity and neuronal loss
result in loss of appetite and a loss of the ability to understand the olfactory qualities of food
[24]. Thus, to assess the reasons underlying Agnes’s inadequate dietary intake, an assessment
targeting her loss of appetite, that is, ‘orthorexia’ can be conducted. A useful assessment tool for
evaluating the reasons underlying Agnes’s inadequate intake would be the Bratman Test for
Orthorexia which used 10 questions to associated self-esteem and quality of life to a client’s
dietary intake [25].
It is also further known that old age is associated with dental and bone loss resulting in
difficulties to chew and swallow food. Thus, a 9 point sensory evaluation can be conducted to
which has been observed in Agnes. Thus, the above analysis clearly reveals the link between
Agnes’s present food consumption patterns and her existing medical conditions [21 ] .
Upon closely evaluating the dietary intake analysis of Agnes’s food consumption, it can
be observed that the her intake of calcium is deficient in comparison to the recommended NRVs
(Table 1). Not only is Agnes’s diet devoid of any form of foods rich in calcium (dairy, nuts,
seeds, green leafy vegetables) (Table 2) her BMI also belongs to the below normal range. Such
findings are of concern since frailty, underweight status and a diet deficient in calcium are major
risk factors of osteoporosis within the elderly [22]. Agnes has also been found to spend most of
time indoors - thus depriving her of vitamin D from sunlight, the key nutrient responsible for the
enhancing calcium absorption. Thus, taking insights from the results of her dietary and
anthropometric measurements, therapeutic interventions must be immediately taken to correct
Agnes’s risk and her potential susceptibility of acquiring fractures in the future [23].
4. Reasons for Inadequacy
It is known that old age is associated with decreased sensory capacity and neuronal loss
result in loss of appetite and a loss of the ability to understand the olfactory qualities of food
[24]. Thus, to assess the reasons underlying Agnes’s inadequate dietary intake, an assessment
targeting her loss of appetite, that is, ‘orthorexia’ can be conducted. A useful assessment tool for
evaluating the reasons underlying Agnes’s inadequate intake would be the Bratman Test for
Orthorexia which used 10 questions to associated self-esteem and quality of life to a client’s
dietary intake [25].
It is also further known that old age is associated with dental and bone loss resulting in
difficulties to chew and swallow food. Thus, a 9 point sensory evaluation can be conducted to
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7LIFESPAN NUTRITION
understand what sensory parameters in food provided contributes to Agnes’s poor appetite.
Based on the same, the aged care home may be advised to provided texturally modified foods
catered to Agnes’s needs [26]. Lastly, a lack of appetite is often associated with underlying
chronic conditions in an individual, such as hepatic, heart and renal diseases as well as cancer
and chronic pulmonary disorders. Thus, additionally respiratory, cardiovascular, renal and
hepatic enzyme assessments can be conducted to detect Agnes’ reasons for low dietary intake
[27].
5. Potential Strategies
The following strategies can be recommended to the aged care facility to improve
Agnes’s inadequate diet intake.
1. It is recommended that hard foods like toast and crackers are replaced with softer foods
such as lightly toasted or untoasted breads prepared with a mix of whole as well as
refined flours. Not only will this enhanced the intake of dietary intake across the elderly
but will also make it easier for them to chew and swallow foods [28].
2. It is recommended that the aged care facility replace all saturated fat sources with
unsaturated sources like low fat dairy, low fat cottage cheese, yoghurt and olive oil. This
will reduced the risk if hypercholesterolemia and cardiovascular disease risk in the
elderly like Agnes as well enhanced digestion and calcium and healthy unsaturated fat
consumption [29].
3. Agnes’s diet reveals the abundance of sugary foods given as snacks to the elderly. It is
advisable to replace sugary biscuits and crackers with stewed fruits (without sugars),
steamed salads with added nuts or fruit and seed smoothies. This will be easier for the
understand what sensory parameters in food provided contributes to Agnes’s poor appetite.
Based on the same, the aged care home may be advised to provided texturally modified foods
catered to Agnes’s needs [26]. Lastly, a lack of appetite is often associated with underlying
chronic conditions in an individual, such as hepatic, heart and renal diseases as well as cancer
and chronic pulmonary disorders. Thus, additionally respiratory, cardiovascular, renal and
hepatic enzyme assessments can be conducted to detect Agnes’ reasons for low dietary intake
[27].
5. Potential Strategies
The following strategies can be recommended to the aged care facility to improve
Agnes’s inadequate diet intake.
1. It is recommended that hard foods like toast and crackers are replaced with softer foods
such as lightly toasted or untoasted breads prepared with a mix of whole as well as
refined flours. Not only will this enhanced the intake of dietary intake across the elderly
but will also make it easier for them to chew and swallow foods [28].
2. It is recommended that the aged care facility replace all saturated fat sources with
unsaturated sources like low fat dairy, low fat cottage cheese, yoghurt and olive oil. This
will reduced the risk if hypercholesterolemia and cardiovascular disease risk in the
elderly like Agnes as well enhanced digestion and calcium and healthy unsaturated fat
consumption [29].
3. Agnes’s diet reveals the abundance of sugary foods given as snacks to the elderly. It is
advisable to replace sugary biscuits and crackers with stewed fruits (without sugars),
steamed salads with added nuts or fruit and seed smoothies. This will be easier for the
8LIFESPAN NUTRITION
elderly to ingest and also contribute to reduced sugar intake and improved fiber, calcium,
antioxidants, unsaturated fat and micronutrient intake [30].
4. Lastly, to improve protein, fiber, calcium and antioxidant consumption, it is advisable
that the aged care facility replace red meats with lean and vegetarian protein sources like
soy, legumes, nuts, seeds and steamed or boiled fatty fish, skinless chicken and eggs [31]
elderly to ingest and also contribute to reduced sugar intake and improved fiber, calcium,
antioxidants, unsaturated fat and micronutrient intake [30].
4. Lastly, to improve protein, fiber, calcium and antioxidant consumption, it is advisable
that the aged care facility replace red meats with lean and vegetarian protein sources like
soy, legumes, nuts, seeds and steamed or boiled fatty fish, skinless chicken and eggs [31]
9LIFESPAN NUTRITION
References
1. Rondanelli M, Faliva M, Monteferrario F, Peroni G, Repaci E, Allieri F, Perna S. Novel
insights on nutrient management of sarcopenia in elderly. InClinical Nutrition and Aging
2017 Oct 2 (pp. 35-66). Apple Academic Press.
2. Fukuda Y, Yamamoto K, Hirao M, Nishikawa K, Nagatsuma Y, Nakayama T, Tanikawa
S, Maeda S, Uemura M, Miyake M, Hama N. Sarcopenia is associated with severe
postoperative complications in elderly gastric cancer patients undergoing gastrectomy.
Gastric Cancer. 2016 Jul 1;19(3):986-93.
3. Gautieri A, Passini FS, Silván U, Guizar-Sicairos M, Carimati G, Volpi P, Moretti M,
Schoenhuber H, Redaelli A, Berli M, Snedeker JG. Advanced glycation end-products:
mechanics of aged collagen from molecule to tissue. Matrix Biology. 2017 May 1;59:95-
108.
4. Cruz-Jentoft AJ, Kiesswetter E, Drey M, Sieber CC. Nutrition, frailty, and sarcopenia.
Aging clinical and experimental research. 2017 Feb 1;29(1):43-8.
5. Hopkinson JB. Nutritional support of the elderly cancer patient: The role of the nurse.
Nutrition. 2015 Apr 1;31(4):598-602.
6. Peyron MA, Woda A, Bourdiol P, Hennequin M. Age‐related changes in mastication.
Journal of oral rehabilitation. 2017 Apr;44(4):299-312.
7. Bernstein M, Munoz N. Nutrition for the older adult. Jones & Bartlett Learning; 2019 Jan
2.
References
1. Rondanelli M, Faliva M, Monteferrario F, Peroni G, Repaci E, Allieri F, Perna S. Novel
insights on nutrient management of sarcopenia in elderly. InClinical Nutrition and Aging
2017 Oct 2 (pp. 35-66). Apple Academic Press.
2. Fukuda Y, Yamamoto K, Hirao M, Nishikawa K, Nagatsuma Y, Nakayama T, Tanikawa
S, Maeda S, Uemura M, Miyake M, Hama N. Sarcopenia is associated with severe
postoperative complications in elderly gastric cancer patients undergoing gastrectomy.
Gastric Cancer. 2016 Jul 1;19(3):986-93.
3. Gautieri A, Passini FS, Silván U, Guizar-Sicairos M, Carimati G, Volpi P, Moretti M,
Schoenhuber H, Redaelli A, Berli M, Snedeker JG. Advanced glycation end-products:
mechanics of aged collagen from molecule to tissue. Matrix Biology. 2017 May 1;59:95-
108.
4. Cruz-Jentoft AJ, Kiesswetter E, Drey M, Sieber CC. Nutrition, frailty, and sarcopenia.
Aging clinical and experimental research. 2017 Feb 1;29(1):43-8.
5. Hopkinson JB. Nutritional support of the elderly cancer patient: The role of the nurse.
Nutrition. 2015 Apr 1;31(4):598-602.
6. Peyron MA, Woda A, Bourdiol P, Hennequin M. Age‐related changes in mastication.
Journal of oral rehabilitation. 2017 Apr;44(4):299-312.
7. Bernstein M, Munoz N. Nutrition for the older adult. Jones & Bartlett Learning; 2019 Jan
2.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10LIFESPAN NUTRITION
8. Li G, Thabane L, Papaioannou A, Ioannidis G, Levine MA, Adachi JD. An overview of
osteoporosis and frailty in the elderly. BMC musculoskeletal disorders. 2017
Dec;18(1):46.
9. Sözen T, Özışık L, Başaran NÇ. An overview and management of osteoporosis.
European journal of rheumatology. 2017 Mar;4(1):46.
10. Jia T, Byberg L, Lindholm B, Larsson TE, Lind L, Michaëlsson K, Carrero JJ. Dietary
acid load, kidney function, osteoporosis, and risk of fractures in elderly men and women.
Osteoporosis International. 2015 Feb 1;26(2):563-70.
11. National Health and Medical Research Council. Nutrients | Nutrient Reference Values
[Internet]. Nrv.gov.au. 2019 [cited 25 September 2019]. Available from:
https://www.nrv.gov.au/nutrients.
12. Nutrition Australia. Australian Dietary Guidelines: Recommended daily intakes |
Nutrition Australia [Internet]. Nutritionaustralia.org. 2019 [cited 25 September 2019].
Available from: http://www.nutritionaustralia.org/national/resource/australian-dietary-
guidelines-recommended-daily-intakes.
13. Hsu PH, Lee CH, Kuo LK, Kung YC, Chen WJ, Tzeng MS. Higher energy and protein
intake from enteral nutrition may reduce hospital mortality in mechanically ventilated
critically ill elderly patients. International Journal of Gerontology. 2018 Dec 1;12(4):285-
9.
14. Cerri AP, Bellelli G, Mazzone A, Pittella F, Landi F, Zambon A, Annoni G. Sarcopenia
and malnutrition in acutely ill hospitalized elderly: Prevalence and outcomes. Clinical
nutrition. 2015 Aug 1;34(4):745-51.
8. Li G, Thabane L, Papaioannou A, Ioannidis G, Levine MA, Adachi JD. An overview of
osteoporosis and frailty in the elderly. BMC musculoskeletal disorders. 2017
Dec;18(1):46.
9. Sözen T, Özışık L, Başaran NÇ. An overview and management of osteoporosis.
European journal of rheumatology. 2017 Mar;4(1):46.
10. Jia T, Byberg L, Lindholm B, Larsson TE, Lind L, Michaëlsson K, Carrero JJ. Dietary
acid load, kidney function, osteoporosis, and risk of fractures in elderly men and women.
Osteoporosis International. 2015 Feb 1;26(2):563-70.
11. National Health and Medical Research Council. Nutrients | Nutrient Reference Values
[Internet]. Nrv.gov.au. 2019 [cited 25 September 2019]. Available from:
https://www.nrv.gov.au/nutrients.
12. Nutrition Australia. Australian Dietary Guidelines: Recommended daily intakes |
Nutrition Australia [Internet]. Nutritionaustralia.org. 2019 [cited 25 September 2019].
Available from: http://www.nutritionaustralia.org/national/resource/australian-dietary-
guidelines-recommended-daily-intakes.
13. Hsu PH, Lee CH, Kuo LK, Kung YC, Chen WJ, Tzeng MS. Higher energy and protein
intake from enteral nutrition may reduce hospital mortality in mechanically ventilated
critically ill elderly patients. International Journal of Gerontology. 2018 Dec 1;12(4):285-
9.
14. Cerri AP, Bellelli G, Mazzone A, Pittella F, Landi F, Zambon A, Annoni G. Sarcopenia
and malnutrition in acutely ill hospitalized elderly: Prevalence and outcomes. Clinical
nutrition. 2015 Aug 1;34(4):745-51.
11LIFESPAN NUTRITION
15. Samari B, Farid P, Ghapanvari MR, Mahmoudi Z. Factors associated with malnutrition in
the elderly. International Journal of Pharmaceutical Research. 2019;11(1):1009-14.
16. Eshkoor S, Hamid T, Shahar S, Ng C, Mun C. Factors affecting hypertension among the
Malaysian elderly. Journal of cardiovascular development and disease. 2016 Mar;3(1):8.
17. Lelli D, Antonelli-Incalzi R, Bandinelli S, Ferrucci L, Pedone C. Association between
sodium excretion and cardiovascular disease and mortality in the elderly: a cohort study.
Journal of the American Medical Directors Association. 2018 Mar 1;19(3):229-34.
18. Blekkenhorst LC, Prince RL, Hodgson JM, Lim WH, Zhu K, Devine A, Thompson PL,
Lewis JR. Dietary saturated fat intake and atherosclerotic vascular disease mortality in
elderly women: a prospective cohort study. The American journal of clinical nutrition.
2015 Jun 1;101(6):1263-8.
19. Praagman J, de Jonge EA, Kiefte-de Jong JC, Beulens JW, Sluijs I, Schoufour JD,
Hofman A, van der Schouw YT, Franco OH. Dietary saturated fatty acids and coronary
heart disease risk in a Dutch middle-aged and elderly population. Arteriosclerosis,
thrombosis, and vascular biology. 2016 Sep;36(9):2011-8.
20. de Oliveira PA, Kovacs C, Moreira P, Magnoni D, Saleh MH, Faintuch J. Unsaturated
fatty acids improve atherosclerosis markers in obese and overweight non-diabetic elderly
patients. Obesity surgery. 2017 Oct 1;27(10):2663-71.
21. Medina-Remón A, Tresserra-Rimbau A, Pons A, Tur JA, Martorell M, Ros E, Buil-
Cosiales P, Sacanella E, Covas MI, Corella D, Salas-Salvadó J. Effects of total dietary
polyphenols on plasma nitric oxide and blood pressure in a high cardiovascular risk
cohort. The PREDIMED randomized trial. Nutrition, Metabolism and Cardiovascular
Diseases. 2015 Jan 1;25(1):60-7.
15. Samari B, Farid P, Ghapanvari MR, Mahmoudi Z. Factors associated with malnutrition in
the elderly. International Journal of Pharmaceutical Research. 2019;11(1):1009-14.
16. Eshkoor S, Hamid T, Shahar S, Ng C, Mun C. Factors affecting hypertension among the
Malaysian elderly. Journal of cardiovascular development and disease. 2016 Mar;3(1):8.
17. Lelli D, Antonelli-Incalzi R, Bandinelli S, Ferrucci L, Pedone C. Association between
sodium excretion and cardiovascular disease and mortality in the elderly: a cohort study.
Journal of the American Medical Directors Association. 2018 Mar 1;19(3):229-34.
18. Blekkenhorst LC, Prince RL, Hodgson JM, Lim WH, Zhu K, Devine A, Thompson PL,
Lewis JR. Dietary saturated fat intake and atherosclerotic vascular disease mortality in
elderly women: a prospective cohort study. The American journal of clinical nutrition.
2015 Jun 1;101(6):1263-8.
19. Praagman J, de Jonge EA, Kiefte-de Jong JC, Beulens JW, Sluijs I, Schoufour JD,
Hofman A, van der Schouw YT, Franco OH. Dietary saturated fatty acids and coronary
heart disease risk in a Dutch middle-aged and elderly population. Arteriosclerosis,
thrombosis, and vascular biology. 2016 Sep;36(9):2011-8.
20. de Oliveira PA, Kovacs C, Moreira P, Magnoni D, Saleh MH, Faintuch J. Unsaturated
fatty acids improve atherosclerosis markers in obese and overweight non-diabetic elderly
patients. Obesity surgery. 2017 Oct 1;27(10):2663-71.
21. Medina-Remón A, Tresserra-Rimbau A, Pons A, Tur JA, Martorell M, Ros E, Buil-
Cosiales P, Sacanella E, Covas MI, Corella D, Salas-Salvadó J. Effects of total dietary
polyphenols on plasma nitric oxide and blood pressure in a high cardiovascular risk
cohort. The PREDIMED randomized trial. Nutrition, Metabolism and Cardiovascular
Diseases. 2015 Jan 1;25(1):60-7.
12LIFESPAN NUTRITION
22. Bolland MJ, Leung W, Tai V, Bastin S, Gamble GD, Grey A, Reid IR. Calcium intake
and risk of fracture: systematic review. Bmj. 2015 Sep 29;351:h4580.
23. Bougioukli S, Κollia P, Koromila T, Varitimidis S, Hantes M, Karachalios T, Malizos
ΚΝ, Dailiana ZH. Failure in diagnosis and under-treatment of osteoporosis in elderly
patients with fragility fractures. Journal of bone and mineral metabolism. 2019 Mar
15;37(2):327-35.
24. Oberle CD, Samaghabadi RO, Hughes EM. Orthorexia nervosa: Assessment and
correlates with gender, BMI, and personality. Appetite. 2017 Jan 1;108:303-10.
25. 10. Dietitians Association of Australia. Orthorexia: The unhealthy side of healthy eating
– Dietitians Association of Australia [Internet]. Daa.asn.au. 2019 [cited 25 September
2019]. Available from:
https://daa.asn.au/smart-eating-for-you/smart-eating-fast-facts/medical/orthorexia-the-
unhealthy-side-of-healthy-eating/
26. Lagast S, De Pelsmaeker S, Schouteten J, Gellynck X. Local food products in health care
facilities: Elderly sensory acceptance of a local food menu. In11th Pangborn Sensory
Science symposium 2015.
27. Aziz NA, Teng NI, Hamid MR, Ismail NH. Assessing the nutritional status of
hospitalized elderly. Clinical interventions in aging. 2017;12:1615.
28. Cichero JA. Adjustment of food textural properties for elderly patients. Journal of texture
studies. 2016 Aug;47(4):277-83.
29. Fernández‐Barrés S, Martin N, Canela T, García‐Barco M, Basora J, Arija V, Project
ATDOM‐NUT group. Dietary intake in the dependent elderly: evaluation of the risk of
nutritional deficit. Journal of Human Nutrition and Dietetics. 2016 Apr;29(2):174-84.
22. Bolland MJ, Leung W, Tai V, Bastin S, Gamble GD, Grey A, Reid IR. Calcium intake
and risk of fracture: systematic review. Bmj. 2015 Sep 29;351:h4580.
23. Bougioukli S, Κollia P, Koromila T, Varitimidis S, Hantes M, Karachalios T, Malizos
ΚΝ, Dailiana ZH. Failure in diagnosis and under-treatment of osteoporosis in elderly
patients with fragility fractures. Journal of bone and mineral metabolism. 2019 Mar
15;37(2):327-35.
24. Oberle CD, Samaghabadi RO, Hughes EM. Orthorexia nervosa: Assessment and
correlates with gender, BMI, and personality. Appetite. 2017 Jan 1;108:303-10.
25. 10. Dietitians Association of Australia. Orthorexia: The unhealthy side of healthy eating
– Dietitians Association of Australia [Internet]. Daa.asn.au. 2019 [cited 25 September
2019]. Available from:
https://daa.asn.au/smart-eating-for-you/smart-eating-fast-facts/medical/orthorexia-the-
unhealthy-side-of-healthy-eating/
26. Lagast S, De Pelsmaeker S, Schouteten J, Gellynck X. Local food products in health care
facilities: Elderly sensory acceptance of a local food menu. In11th Pangborn Sensory
Science symposium 2015.
27. Aziz NA, Teng NI, Hamid MR, Ismail NH. Assessing the nutritional status of
hospitalized elderly. Clinical interventions in aging. 2017;12:1615.
28. Cichero JA. Adjustment of food textural properties for elderly patients. Journal of texture
studies. 2016 Aug;47(4):277-83.
29. Fernández‐Barrés S, Martin N, Canela T, García‐Barco M, Basora J, Arija V, Project
ATDOM‐NUT group. Dietary intake in the dependent elderly: evaluation of the risk of
nutritional deficit. Journal of Human Nutrition and Dietetics. 2016 Apr;29(2):174-84.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13LIFESPAN NUTRITION
30. Flores TR, Nunes BP, Assunção MC, Bertoldi AD. Healthy habits: what kind of guidance
the elderly population is receiving from health professionals?. Revista Brasileira de
Epidemiologia. 2016 Mar;19(1):167-80.
31. Blekkenhorst LC, Prince RL, Hodgson JM, Lim WH, Zhu K, Devine A, Thompson PL,
Lewis JR. Dietary saturated fat intake and atherosclerotic vascular disease mortality in
elderly women: a prospective cohort study. The American journal of clinical nutrition.
2015 Jun 1;101(6):1263-8.
.
30. Flores TR, Nunes BP, Assunção MC, Bertoldi AD. Healthy habits: what kind of guidance
the elderly population is receiving from health professionals?. Revista Brasileira de
Epidemiologia. 2016 Mar;19(1):167-80.
31. Blekkenhorst LC, Prince RL, Hodgson JM, Lim WH, Zhu K, Devine A, Thompson PL,
Lewis JR. Dietary saturated fat intake and atherosclerotic vascular disease mortality in
elderly women: a prospective cohort study. The American journal of clinical nutrition.
2015 Jun 1;101(6):1263-8.
.
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





