Evidence-Based Strategies for Improving Patient Safety Culture
VerifiedAdded on 2020/04/01
|20
|5722
|375
Essay
AI Summary
This essay provides a comprehensive overview of patient safety culture in healthcare settings. It critically analyzes the issues involved, such as communication breakdowns, resource limitations, and the impact of hospital organizational culture on patient outcomes. The essay explores the reasons for change, including the need to enhance healthcare competencies and improve communication among healthcare professionals. It identifies driving and restraining forces, and discusses evidence-based strategies for implementing a patient safety culture, such as the use of electronic health records. Furthermore, it examines decision-making processes, proposes solutions, and outlines expected outcomes, including improved patient satisfaction and reduced adverse events. The essay also identifies key stakeholders, assesses the impact of change on professional practice and health service management, and offers recommendations for further improvement. Overall, the paper emphasizes the importance of a systematic approach to patient safety culture to enhance the quality of healthcare interventions and patient care outcomes.
Evidence Based Practice in Health Service Management
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1 | P a g e
Table of Content
Executive Summary…………………………………………………………………………...2
Introduction……………………………………………………………………………..……..2
A critical analysis of the issues involved……………………………………………………...3
Reasons for the change……………………………………………………………………...…6
Diving forces……………………………………………………………………………….….6
Evidence-based strategies for the implementation of patient safety culture…………………..8
The type and quality of evidence applied…………………………………………………..….9
Decision-making processes involved………………………………………………..……….10
Solutions, Rationales and Expected Outcomes……………………………….………….…..10
Identification of the key stakeholders………………………………………………………..12
The impact upon each stakeholder…………………………………………………………...12
The impact of the change upon professional practice and health service management……...13
A set of recommendations for using evidence to effect further change……………………...14
Conclusion……………………………………………………………………………………14
References……………………………………………………………………………………15
1 | P a g e
Table of Content
Executive Summary…………………………………………………………………………...2
Introduction……………………………………………………………………………..……..2
A critical analysis of the issues involved……………………………………………………...3
Reasons for the change……………………………………………………………………...…6
Diving forces……………………………………………………………………………….….6
Evidence-based strategies for the implementation of patient safety culture…………………..8
The type and quality of evidence applied…………………………………………………..….9
Decision-making processes involved………………………………………………..……….10
Solutions, Rationales and Expected Outcomes……………………………….………….…..10
Identification of the key stakeholders………………………………………………………..12
The impact upon each stakeholder…………………………………………………………...12
The impact of the change upon professional practice and health service management……...13
A set of recommendations for using evidence to effect further change……………………...14
Conclusion……………………………………………………………………………………14
References……………………………………………………………………………………15
1 | P a g e
2 | P a g e
Executive Summary
This research paper evidentially discusses the requirements and rationale for
establishing the pattern of patient safety culture in healthcare facilities. The paper critically
analyses various challenges associated with the establishment of patient safety culture in
healthcare settings and discusses in length the attributes including force field analysis,
evidence-based strategies, recommended solutions, expected outcomes and stakeholder
requirements of patient’s safety culture.
Introduction
The establishment of a safety culture in hospitals and clinical settings is the
preliminary requirement for the systematic enhancement of the healthcare outcomes. The
development of an efficient safety culture is based on the configuration of a systematic error
and incident reporting system in medical facilities (El-Jardali, Dimassi, Jamal, Jaafar, &
Hemadeh, 2011). The formulation of expert leadership and management systems with special
focus on organizational learning and safety of patients leads to the reciprocal reduction in the
length of patients stay in the inpatient units as well as the frequency of adverse events. The
research community needs to effectively correlate the outcomes and predictors of safety
culture in healthcare facilities for effectively enhancing the quality of healthcare interventions
in accordance with the treatment goals. The healthcare teams require assessing the safety
culture dimensions in clinical settings with the objective of improving the level of patient
satisfaction as well as compliance with the recommended treatment regimen (Wagner. Smits,
Sorra, & Huang, 2013). The comparative analysis of the safety cultures of various medical
facilities is highly required for exploring the potential opportunities in the healthcare practice
management system. The development of a systematic safety culture requires the
development of an effective action management system while ensuring the safety of the
associated healthcare teams as well as the treated patients (USDOL, 2017). The systematic
2 | P a g e
Executive Summary
This research paper evidentially discusses the requirements and rationale for
establishing the pattern of patient safety culture in healthcare facilities. The paper critically
analyses various challenges associated with the establishment of patient safety culture in
healthcare settings and discusses in length the attributes including force field analysis,
evidence-based strategies, recommended solutions, expected outcomes and stakeholder
requirements of patient’s safety culture.
Introduction
The establishment of a safety culture in hospitals and clinical settings is the
preliminary requirement for the systematic enhancement of the healthcare outcomes. The
development of an efficient safety culture is based on the configuration of a systematic error
and incident reporting system in medical facilities (El-Jardali, Dimassi, Jamal, Jaafar, &
Hemadeh, 2011). The formulation of expert leadership and management systems with special
focus on organizational learning and safety of patients leads to the reciprocal reduction in the
length of patients stay in the inpatient units as well as the frequency of adverse events. The
research community needs to effectively correlate the outcomes and predictors of safety
culture in healthcare facilities for effectively enhancing the quality of healthcare interventions
in accordance with the treatment goals. The healthcare teams require assessing the safety
culture dimensions in clinical settings with the objective of improving the level of patient
satisfaction as well as compliance with the recommended treatment regimen (Wagner. Smits,
Sorra, & Huang, 2013). The comparative analysis of the safety cultures of various medical
facilities is highly required for exploring the potential opportunities in the healthcare practice
management system. The development of a systematic safety culture requires the
development of an effective action management system while ensuring the safety of the
associated healthcare teams as well as the treated patients (USDOL, 2017). The systematic
2 | P a g e
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3 | P a g e
participation of healthcare workers in the configuration of safe and effective medical
practices is proactively required for reducing the scope of occurrence of errors and associated
adversities during medical management (USDOL, 2017). Healthcare professionals require
utilizing protective equipment in the healthcare settings in the context of reducing the scope
of injuries and traumatic events during medical interventions. The hospital administration
requires publishing acceptable safety norms for their effective compliance by the healthcare
teams as well as other staff members during the working hours (USDOL, 2017). The safety
culture norms endorse the requirement of systematic socialization of the new members of the
healthcare teams following the process of their induction in the clinical settings. Evidence-
based research literature considers patient safety culture as a significant attribute requiring
analysis for evaluating the healthcare quality in the clinical settings (Nie, et al., 2013). The
research analysis by (Nie, et al., 2013) defines the patient safety culture in terms of the
pattern of behaviour and values of healthcare teams that effectively motivates them in the
context of practising proactive measures for reducing the risk of patient harm in the clinical
settings. Indeed, the establishment of a positive attitude of the healthcare workers, physicians,
nursing professionals and paramedical teams towards the acquisition of patient safety culture
is highly required for reducing the prevalence of patient adversities in the clinical settings
(Nie, et al., 2013). The establishment of a safer healthcare system will not only improve the
quality of healthcare services but also advocate the acknowledgement of ethical concerns of
the treated patients for enhancing their level of trust and confidence on the patient care
strategies. This academic essay discusses in length regarding the safety culture issues and
their systematic implications on the quality of treatment interventions as well as patient care
outcomes in the medical facilities.
A critical analysis of the issues involved
3 | P a g e
participation of healthcare workers in the configuration of safe and effective medical
practices is proactively required for reducing the scope of occurrence of errors and associated
adversities during medical management (USDOL, 2017). Healthcare professionals require
utilizing protective equipment in the healthcare settings in the context of reducing the scope
of injuries and traumatic events during medical interventions. The hospital administration
requires publishing acceptable safety norms for their effective compliance by the healthcare
teams as well as other staff members during the working hours (USDOL, 2017). The safety
culture norms endorse the requirement of systematic socialization of the new members of the
healthcare teams following the process of their induction in the clinical settings. Evidence-
based research literature considers patient safety culture as a significant attribute requiring
analysis for evaluating the healthcare quality in the clinical settings (Nie, et al., 2013). The
research analysis by (Nie, et al., 2013) defines the patient safety culture in terms of the
pattern of behaviour and values of healthcare teams that effectively motivates them in the
context of practising proactive measures for reducing the risk of patient harm in the clinical
settings. Indeed, the establishment of a positive attitude of the healthcare workers, physicians,
nursing professionals and paramedical teams towards the acquisition of patient safety culture
is highly required for reducing the prevalence of patient adversities in the clinical settings
(Nie, et al., 2013). The establishment of a safer healthcare system will not only improve the
quality of healthcare services but also advocate the acknowledgement of ethical concerns of
the treated patients for enhancing their level of trust and confidence on the patient care
strategies. This academic essay discusses in length regarding the safety culture issues and
their systematic implications on the quality of treatment interventions as well as patient care
outcomes in the medical facilities.
A critical analysis of the issues involved
3 | P a g e
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4 | P a g e
The patient safety culture across the hospitals and medical facilities varies in
accordance with the pattern of medication inadequacies, feedback exchange mechanism,
event reporting system, communication protocols, team work, staffing level and working
hours of the healthcare teams (Wami, Demssie, Wassie, & Ahmed, 2016). The development
of patient morbidities and mortalities on a global scale occurs under the influence of unsafe
medical practices that continue to downgrade the care giving process across the hospital
environment. Hospital organizational culture that facilitates the blame process between the
healthcare professionals leads to the reduction in accountability towards medical
interventions (Wami, Demssie, Wassie, & Ahmed, 2016). Resultantly, the healthcare teams
refrain from administering safe medical practices and refrain from taking the responsibility
for the quality and safety of the clinical procedures. Patient safety culture also deteriorates
under the influence of lack of healthcare resources and safety management practices.
Absence of consistent communication between the healthcare teams and the treated patients
leads to their abstinence in exploring the healthcare flaws across the hospital environment.
Lack of patients’ participation in their safety programs decreases their level of awareness
regarding treatment interventions and the associated adversities (Wami, Demssie, Wassie, &
Ahmed, 2016). This reciprocally increases the risk of patients towards acquiring adverse
treatment outcomes and associated complications. The capacity and position of the work
premises, hospital characteristics and responded attributes considerably influence the pattern
of patient safety culture in the clinical settings. Moreover, the absence of critical support
systems in the hospital settings leads to the substantial degradation of patient safety culture
(Wami, Demssie, Wassie, & Ahmed, 2016). The lack of hospital funding on the maintenance
of health and hygiene reciprocally compromises the safety of medical interventions and
increases the risk of patients towards acquiring the pattern of nosocomial infections and their
deleterious complications. The healthcare agencies therefore, require undertaking systematic
4 | P a g e
The patient safety culture across the hospitals and medical facilities varies in
accordance with the pattern of medication inadequacies, feedback exchange mechanism,
event reporting system, communication protocols, team work, staffing level and working
hours of the healthcare teams (Wami, Demssie, Wassie, & Ahmed, 2016). The development
of patient morbidities and mortalities on a global scale occurs under the influence of unsafe
medical practices that continue to downgrade the care giving process across the hospital
environment. Hospital organizational culture that facilitates the blame process between the
healthcare professionals leads to the reduction in accountability towards medical
interventions (Wami, Demssie, Wassie, & Ahmed, 2016). Resultantly, the healthcare teams
refrain from administering safe medical practices and refrain from taking the responsibility
for the quality and safety of the clinical procedures. Patient safety culture also deteriorates
under the influence of lack of healthcare resources and safety management practices.
Absence of consistent communication between the healthcare teams and the treated patients
leads to their abstinence in exploring the healthcare flaws across the hospital environment.
Lack of patients’ participation in their safety programs decreases their level of awareness
regarding treatment interventions and the associated adversities (Wami, Demssie, Wassie, &
Ahmed, 2016). This reciprocally increases the risk of patients towards acquiring adverse
treatment outcomes and associated complications. The capacity and position of the work
premises, hospital characteristics and responded attributes considerably influence the pattern
of patient safety culture in the clinical settings. Moreover, the absence of critical support
systems in the hospital settings leads to the substantial degradation of patient safety culture
(Wami, Demssie, Wassie, & Ahmed, 2016). The lack of hospital funding on the maintenance
of health and hygiene reciprocally compromises the safety of medical interventions and
increases the risk of patients towards acquiring the pattern of nosocomial infections and their
deleterious complications. The healthcare agencies therefore, require undertaking systematic
4 | P a g e
5 | P a g e
measures for the effective configuration of patient safety standards, tools, guidelines and
strategies for reducing the occurrence of patient adversities in medical practice (Wami,
Demssie, Wassie, & Ahmed, 2016). The research analysis by (Alonazi, Alonazi, Saeed, &
Mohamed, 2016) reveals the pattern of sub-optimal safety culture among nurse professionals
in tertiary care hospitals. This increasingly leads to the unreported occurrence of medication
errors and associated patient adversities. Therefore, the configuration and implementation of
a systematic error reporting system are necessarily warranted in tertiary care settings with the
objective of reducing the scope of patient fatalities under the influence of inappropriate
therapeutic administration. The research study by (Noort, Reader, Shorrock, & Kirwan, 2016)
affirms an inverse relationship between patient safety culture and the cultural tendencies of
people for avoiding the state of uncertainty. The uncertainty states might arise under the
influence under the influence of ambiguous circumstances that could lead to the development
of anxiety in the healthcare teams (Noort, Reader, Shorrock, & Kirwan, 2016). The avoidance
of these circumstances by the healthcare professionals’ results in deterioration of safety
protocols that resultantly degrades the quality and efficacy of the administered healthcare
interventions. The national cultural practices followed by the healthcare teams remain out of
the direct control of the hospital management and considerably influence safety-related
beliefs and attitudes of healthcare professionals. This rationally indicates the requirement of
modifying the beliefs and apprehensions of the healthcare professionals regarding patient
safety attitudes and practices for establishing a safe healthcare environment in the clinical
settings. The absence of well-defined safety benchmarks in the hospital settings leads to the
development of various misconceptions regarding the safety and efficacy of healthcare
interventions. These safety misconceptions among healthcare teams and patient population
lead to the sustained deterioration in the quality of healthcare services in the hospital
environment. The countries experiencing elevated level of UA (uncertainty avoidance) index
5 | P a g e
measures for the effective configuration of patient safety standards, tools, guidelines and
strategies for reducing the occurrence of patient adversities in medical practice (Wami,
Demssie, Wassie, & Ahmed, 2016). The research analysis by (Alonazi, Alonazi, Saeed, &
Mohamed, 2016) reveals the pattern of sub-optimal safety culture among nurse professionals
in tertiary care hospitals. This increasingly leads to the unreported occurrence of medication
errors and associated patient adversities. Therefore, the configuration and implementation of
a systematic error reporting system are necessarily warranted in tertiary care settings with the
objective of reducing the scope of patient fatalities under the influence of inappropriate
therapeutic administration. The research study by (Noort, Reader, Shorrock, & Kirwan, 2016)
affirms an inverse relationship between patient safety culture and the cultural tendencies of
people for avoiding the state of uncertainty. The uncertainty states might arise under the
influence under the influence of ambiguous circumstances that could lead to the development
of anxiety in the healthcare teams (Noort, Reader, Shorrock, & Kirwan, 2016). The avoidance
of these circumstances by the healthcare professionals’ results in deterioration of safety
protocols that resultantly degrades the quality and efficacy of the administered healthcare
interventions. The national cultural practices followed by the healthcare teams remain out of
the direct control of the hospital management and considerably influence safety-related
beliefs and attitudes of healthcare professionals. This rationally indicates the requirement of
modifying the beliefs and apprehensions of the healthcare professionals regarding patient
safety attitudes and practices for establishing a safe healthcare environment in the clinical
settings. The absence of well-defined safety benchmarks in the hospital settings leads to the
development of various misconceptions regarding the safety and efficacy of healthcare
interventions. These safety misconceptions among healthcare teams and patient population
lead to the sustained deterioration in the quality of healthcare services in the hospital
environment. The countries experiencing elevated level of UA (uncertainty avoidance) index
5 | P a g e
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6 | P a g e
require following the safety benchmarks established by SIGN (safety culture against
international group norms) convention for identifying and implementing the best safety
practices in their healthcare settings (Noort, Reader, Shorrock, & Kirwan, 2016).
Reasons for the change
The establishment of an effective safety culture is necessarily warranted with the
objective of elevating the healthcare competencies of the medical professionals (Weaver,
Lubomski, & Wilson, 2013). The healthcare behavioural modification of the healthcare teams
will not only improve their clinical proficiency, but also enhance the commitment towards
acquiring goal-oriented treatment outcomes in the shortest timeframe. The enhancement of
the pattern of communication between the healthcare professionals will improve their mutual
trust and enhance the multidisciplinary coordination for the reciprocal improvement in the
treatment outcomes (Weaver, Lubomski, & Wilson, 2013). The modification in the safety
culture aetiology will not only improve the safety culture perceptions of the healthcare
providers but also enhance their patient-handling behaviour in the clinical settings. This will
resultantly promote the establishment of an effective safety culture warranted for the
qualitative enhancement of healthcare outcomes (Weaver, Lubomski, & Wilson, 2013). The
unit-based improvement interventions, executive engagement approaches and team training
strategies include some of the most effective measures warranting implementation for the
systematic enhancement of patient safety practices in the healthcare settings. The utilization
of these interdisciplinary and multifaceted patient-centred approaches is the need of the hour
that promises for reducing the risk of patient adversities during and after the administration of
treatment interventions (Weaver, Lubomski, & Wilson, 2013).
Diving forces
The greater resistive force or barriers to the establishment of patient’s safety culture
include the deteriorated communication between the healthcare teams, absence of resources,
6 | P a g e
require following the safety benchmarks established by SIGN (safety culture against
international group norms) convention for identifying and implementing the best safety
practices in their healthcare settings (Noort, Reader, Shorrock, & Kirwan, 2016).
Reasons for the change
The establishment of an effective safety culture is necessarily warranted with the
objective of elevating the healthcare competencies of the medical professionals (Weaver,
Lubomski, & Wilson, 2013). The healthcare behavioural modification of the healthcare teams
will not only improve their clinical proficiency, but also enhance the commitment towards
acquiring goal-oriented treatment outcomes in the shortest timeframe. The enhancement of
the pattern of communication between the healthcare professionals will improve their mutual
trust and enhance the multidisciplinary coordination for the reciprocal improvement in the
treatment outcomes (Weaver, Lubomski, & Wilson, 2013). The modification in the safety
culture aetiology will not only improve the safety culture perceptions of the healthcare
providers but also enhance their patient-handling behaviour in the clinical settings. This will
resultantly promote the establishment of an effective safety culture warranted for the
qualitative enhancement of healthcare outcomes (Weaver, Lubomski, & Wilson, 2013). The
unit-based improvement interventions, executive engagement approaches and team training
strategies include some of the most effective measures warranting implementation for the
systematic enhancement of patient safety practices in the healthcare settings. The utilization
of these interdisciplinary and multifaceted patient-centred approaches is the need of the hour
that promises for reducing the risk of patient adversities during and after the administration of
treatment interventions (Weaver, Lubomski, & Wilson, 2013).
Diving forces
The greater resistive force or barriers to the establishment of patient’s safety culture
include the deteriorated communication between the healthcare teams, absence of resources,
6 | P a g e
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7 | P a g e
time-deficit as well as elevated workloads of the medical professionals (Zecevic, Li , Ngo ,
Halligan , & Kothari , 2017). The facilitators of patient safety culture establishment include
the hospital management systems, federal governments, nurses, physicians, social groups,
non-profit organizations and patient population (Zecevic, Li, Ngo, Halligan, & Kothari,
2017). The limitation of healthcare staff leads to the frequent movement of the healthcare
team members between the new and established patients that eventually reduces the
assessment time and deterioration in the healthcare outcomes. The limitation in hospital beds
leads to their sharing between the patients that substantially elevates the pattern of cross-
infection and associated adverse manifestations (Landefeld, Sivaraman, & Arora, 2015).
Acute shortages in medicine stock lead to the acquisition of the missing drug from outside of
the hospital premises. Purchased medicine might differ from the recommended drug in terms
of dosage and concentration that could adversely affect the pattern of drug response and
associated treatment outcomes (Landefeld, Sivaraman, & Arora, 2015). The inappropriate
professional culture in the medical facilities leads to the unnecessary administration of
investigations due to the defensive attitude of the treating physicians after the occurrence of
an adverse treatment episode. This unprofessional culture proves to be the biggest constraint
in the establishment of safe medical practices in the healthcare settings (Landefeld,
Sivaraman, & Arora, 2015). The unwillingness of the nursing team (due to additional work
load) in attaining healthcare training also restrains the implementation of an appropriate
patient safety culture between the medical teams. The absence of patient education
interventions leads to the unnecessary administration of injections on demand by the patient
population in the context of acquiring an immediate cure (Landefeld, Sivaraman, & Arora,
2015). This results in the occurrence of adverse reactions and resultant patient fatalities.
These evidence-based facts warrant the requirement of utilizing systematic safety culture
7 | P a g e
time-deficit as well as elevated workloads of the medical professionals (Zecevic, Li , Ngo ,
Halligan , & Kothari , 2017). The facilitators of patient safety culture establishment include
the hospital management systems, federal governments, nurses, physicians, social groups,
non-profit organizations and patient population (Zecevic, Li, Ngo, Halligan, & Kothari,
2017). The limitation of healthcare staff leads to the frequent movement of the healthcare
team members between the new and established patients that eventually reduces the
assessment time and deterioration in the healthcare outcomes. The limitation in hospital beds
leads to their sharing between the patients that substantially elevates the pattern of cross-
infection and associated adverse manifestations (Landefeld, Sivaraman, & Arora, 2015).
Acute shortages in medicine stock lead to the acquisition of the missing drug from outside of
the hospital premises. Purchased medicine might differ from the recommended drug in terms
of dosage and concentration that could adversely affect the pattern of drug response and
associated treatment outcomes (Landefeld, Sivaraman, & Arora, 2015). The inappropriate
professional culture in the medical facilities leads to the unnecessary administration of
investigations due to the defensive attitude of the treating physicians after the occurrence of
an adverse treatment episode. This unprofessional culture proves to be the biggest constraint
in the establishment of safe medical practices in the healthcare settings (Landefeld,
Sivaraman, & Arora, 2015). The unwillingness of the nursing team (due to additional work
load) in attaining healthcare training also restrains the implementation of an appropriate
patient safety culture between the medical teams. The absence of patient education
interventions leads to the unnecessary administration of injections on demand by the patient
population in the context of acquiring an immediate cure (Landefeld, Sivaraman, & Arora,
2015). This results in the occurrence of adverse reactions and resultant patient fatalities.
These evidence-based facts warrant the requirement of utilizing systematic safety culture
7 | P a g e
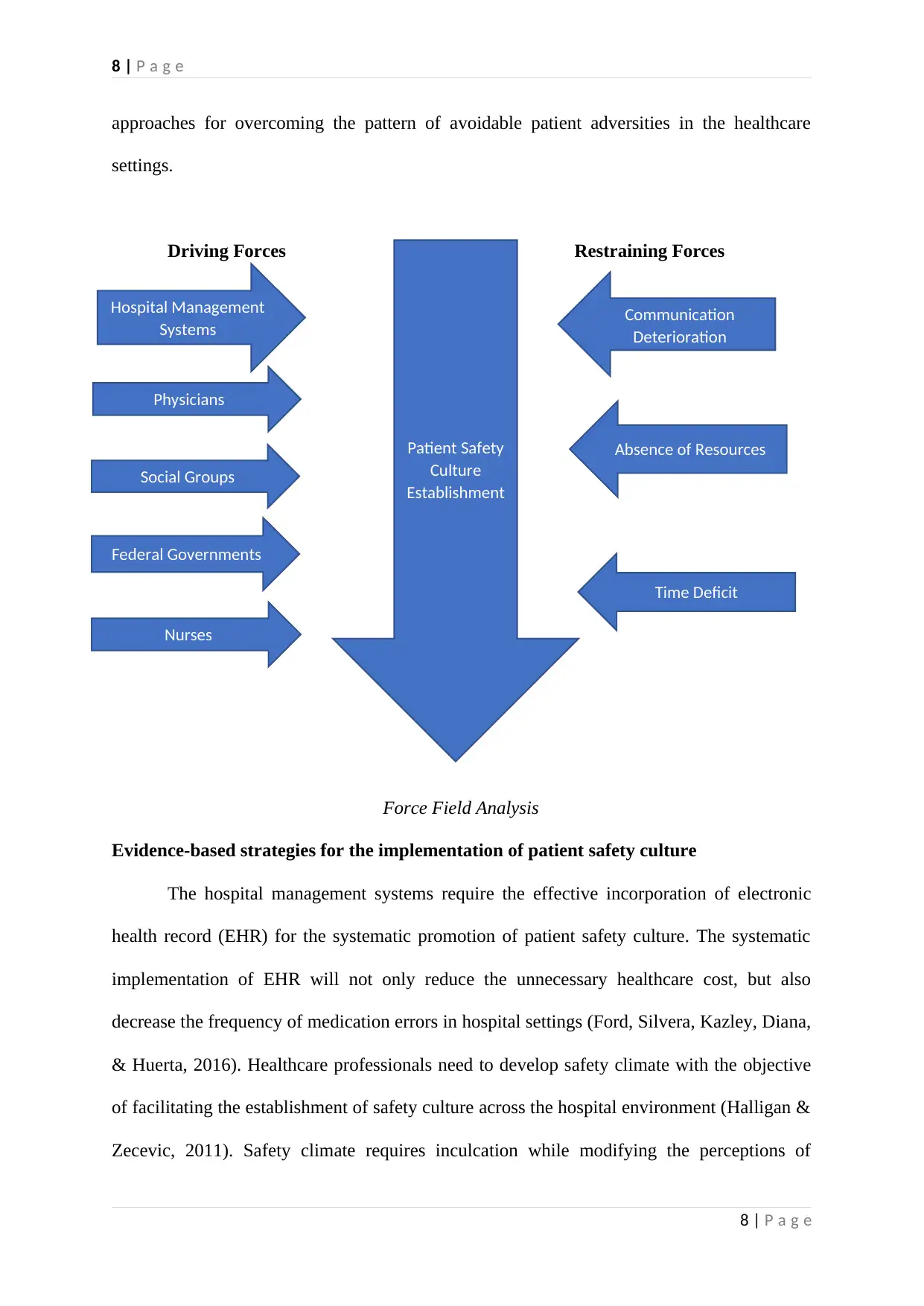
8 | P a g e
approaches for overcoming the pattern of avoidable patient adversities in the healthcare
settings.
Driving Forces Restraining Forces
Force Field Analysis
Evidence-based strategies for the implementation of patient safety culture
The hospital management systems require the effective incorporation of electronic
health record (EHR) for the systematic promotion of patient safety culture. The systematic
implementation of EHR will not only reduce the unnecessary healthcare cost, but also
decrease the frequency of medication errors in hospital settings (Ford, Silvera, Kazley, Diana,
& Huerta, 2016). Healthcare professionals need to develop safety climate with the objective
of facilitating the establishment of safety culture across the hospital environment (Halligan &
Zecevic, 2011). Safety climate requires inculcation while modifying the perceptions of
8 | P a g e
Patient Safety
Culture
Establishment
Hospital Management
Systems
Physicians
Nurses
Federal Governments
Social Groups
Communication
Deterioration
Absence of Resources
Time Deficit
approaches for overcoming the pattern of avoidable patient adversities in the healthcare
settings.
Driving Forces Restraining Forces
Force Field Analysis
Evidence-based strategies for the implementation of patient safety culture
The hospital management systems require the effective incorporation of electronic
health record (EHR) for the systematic promotion of patient safety culture. The systematic
implementation of EHR will not only reduce the unnecessary healthcare cost, but also
decrease the frequency of medication errors in hospital settings (Ford, Silvera, Kazley, Diana,
& Huerta, 2016). Healthcare professionals need to develop safety climate with the objective
of facilitating the establishment of safety culture across the hospital environment (Halligan &
Zecevic, 2011). Safety climate requires inculcation while modifying the perceptions of
8 | P a g e
Patient Safety
Culture
Establishment
Hospital Management
Systems
Physicians
Nurses
Federal Governments
Social Groups
Communication
Deterioration
Absence of Resources
Time Deficit
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9 | P a g e
healthcare teams in relation to the establishment of patient safety in their medical facility
(Hoffmann, et al., 2013). The establishment of organizational safety climate will positively
influence the attitudes and motivation of healthcare professionals. The enhancement of these
attributes will eventually facilitate the implementation of patient safety measures warranted
for the systematic improvement of the quality of healthcare interventions and associated
safety outcomes (Hoffmann, et al., 2013).
The type and quality of evidence applied
Survey intervention by (Farup, 2015) reveals the reciprocal relationship between the
pattern of adverse events and patient safety culture in the clinical settings. This rationally
indicates the requirement of consistent improvement in patients’ safety culture for reducing
the frequency of adverse treatment outcomes. The findings of systematic analysis by
(DiCuccio, 2015) advocate the requirement of utilizing PSCMT (patient safety culture
measurement tools) for evaluating the pattern of patient safety culture and associated
treatment outcomes in the clinical settings. Evidence-based clinical literature recommends the
regular evaluation of pertinent patient information by the registered nurse professionals and
treating physicians for the systematic improvement in safety outcomes. Therefore, the
treating clinicians must evaluate patient’s functional status, risk of falls, allergy history, pain
management pattern, laboratory/radiology findings and abnormal vital signs for reducing the
risk of occurrence of adverse patient outcomes in the clinical setting (White, Dudley-Brown,
& Terhaar, 2016, pp. 402-404). The survey intervention administered by (Lee, Phan,
Dorman, Weaver, & Pronovost, 2016) attempted to evaluate the influence of clinical handoffs
on the patient safety culture. The findings advocate the requirement of improving the
behaviour, attitude and perception of healthcare teams for the effective implementation of
safety protocols (during clinical handover) in the context of reducing the scope of adverse
patient outcomes (Lee, Phan, Dorman, Weaver, & Pronovost, 2016). Survey intervention by
9 | P a g e
healthcare teams in relation to the establishment of patient safety in their medical facility
(Hoffmann, et al., 2013). The establishment of organizational safety climate will positively
influence the attitudes and motivation of healthcare professionals. The enhancement of these
attributes will eventually facilitate the implementation of patient safety measures warranted
for the systematic improvement of the quality of healthcare interventions and associated
safety outcomes (Hoffmann, et al., 2013).
The type and quality of evidence applied
Survey intervention by (Farup, 2015) reveals the reciprocal relationship between the
pattern of adverse events and patient safety culture in the clinical settings. This rationally
indicates the requirement of consistent improvement in patients’ safety culture for reducing
the frequency of adverse treatment outcomes. The findings of systematic analysis by
(DiCuccio, 2015) advocate the requirement of utilizing PSCMT (patient safety culture
measurement tools) for evaluating the pattern of patient safety culture and associated
treatment outcomes in the clinical settings. Evidence-based clinical literature recommends the
regular evaluation of pertinent patient information by the registered nurse professionals and
treating physicians for the systematic improvement in safety outcomes. Therefore, the
treating clinicians must evaluate patient’s functional status, risk of falls, allergy history, pain
management pattern, laboratory/radiology findings and abnormal vital signs for reducing the
risk of occurrence of adverse patient outcomes in the clinical setting (White, Dudley-Brown,
& Terhaar, 2016, pp. 402-404). The survey intervention administered by (Lee, Phan,
Dorman, Weaver, & Pronovost, 2016) attempted to evaluate the influence of clinical handoffs
on the patient safety culture. The findings advocate the requirement of improving the
behaviour, attitude and perception of healthcare teams for the effective implementation of
safety protocols (during clinical handover) in the context of reducing the scope of adverse
patient outcomes (Lee, Phan, Dorman, Weaver, & Pronovost, 2016). Survey intervention by
9 | P a g e
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10 | P a g e
researchers appears to be the only methodological approach utilized by researchers for the
systematic evaluation of patient safety culture in healthcare settings.
Decision-making processes involved
Healthcare professionals require undertaking calculated evidence-based decisions
while handling medical emergencies in the context of reducing the prevalence of adverse
patient outcomes across the healthcare settings (O’Hara, et al., 2014). Physicians and nurses
must identify the extent of patient’s vulnerability to the development of adverse treatment
outcomes and accordingly utilize various risk aversion strategies while considering the
available healthcare resources as well as the treatment requirements. The treating physicians,
nurses and other members of the healthcare teams require undertaking collaborative efforts in
the context of improving the pattern of their interpersonal relationships, job satisfaction and
team work for the effective enhancement of organizational safety culture and associated
patient outcomes (Körner, Wirtz, Bengel, & Göritz, 2015). These decision-making strategies
and collaborative interventions substantially improve the pattern of patient safety culture in
the healthcare settings.
Solutions, Rationales and Expected Outcomes
The systematic solution for implementing an evidence-based patient safety culture
across hospital environment attributes to the implantation of an effective, transparent and
non-punitive event reporting system (Kear & Ulrich, 2015). This event reporting system will
facilitate the timely recording of healthcare adversities for their effective mitigation.
Furthermore, the periodic organization of safety meetings and safety huddles by healthcare
teams would also suffice the requirement of establishing patient safety culture in the clinical
settings (Kear & Ulrich, 2015). Medical practitioners need to enhance their medication
administration as well as fall reduction strategies for reducing the scope of occurrence of
10 | P a g e
researchers appears to be the only methodological approach utilized by researchers for the
systematic evaluation of patient safety culture in healthcare settings.
Decision-making processes involved
Healthcare professionals require undertaking calculated evidence-based decisions
while handling medical emergencies in the context of reducing the prevalence of adverse
patient outcomes across the healthcare settings (O’Hara, et al., 2014). Physicians and nurses
must identify the extent of patient’s vulnerability to the development of adverse treatment
outcomes and accordingly utilize various risk aversion strategies while considering the
available healthcare resources as well as the treatment requirements. The treating physicians,
nurses and other members of the healthcare teams require undertaking collaborative efforts in
the context of improving the pattern of their interpersonal relationships, job satisfaction and
team work for the effective enhancement of organizational safety culture and associated
patient outcomes (Körner, Wirtz, Bengel, & Göritz, 2015). These decision-making strategies
and collaborative interventions substantially improve the pattern of patient safety culture in
the healthcare settings.
Solutions, Rationales and Expected Outcomes
The systematic solution for implementing an evidence-based patient safety culture
across hospital environment attributes to the implantation of an effective, transparent and
non-punitive event reporting system (Kear & Ulrich, 2015). This event reporting system will
facilitate the timely recording of healthcare adversities for their effective mitigation.
Furthermore, the periodic organization of safety meetings and safety huddles by healthcare
teams would also suffice the requirement of establishing patient safety culture in the clinical
settings (Kear & Ulrich, 2015). Medical practitioners need to enhance their medication
administration as well as fall reduction strategies for reducing the scope of occurrence of
10 | P a g e
11 | P a g e
patient fatalities under the influence of inappropriate treatment interventions (Kear & Ulrich,
2015). The research analysis by (Parker, Wensing, Esmail, & Valderas, 2015) indicates the
requirement of improving healthcare processes, rather than the care outcomes for the
systematic establishment of safety culture in the hospital settings. Healthcare professionals
need to conceptualize the patient safety culture in the context of its equitable establishment
across the hospital environment (Parker, Wensing, Esmail, & Valderas, 2015). The
physicians also require exploring the causes of nosocomial infections and undertake
preventive and prophylactic measures for reducing the pattern of their occurrence. The
organization of healthcare awareness sessions is necessarily required for improving the
standards of health and hygiene in the hospital locations. The utilization of hand hygiene
measures proves to be highly effective in preventing the progression of hospital acquired
infections in healthcare settings (Parker, Wensing, Esmail, & Valderas, 2015). Evidence-
based analysis by (Hessels, Murray, Cohen, & Larson, 2017) advocates the requirement of
periodic administration of nursing home and hospital surveys with the objective of
determining the pattern of patient safety culture in the healthcare facilities. Outcomes of these
survey interventions require the systematic analysis by the research professionals in the
context of mitigating the sustained patient safety deficits in the healthcare system. For
example, the staffing deficit in the healthcare facilities warrants mitigation through the
deployment of additional staff or by imparting work management training to the existing
physicians, nurses and other medical professionals associated with the hospital setting. The
systematic documentation of adverse events is necessarily required with the objective of
undertaking proactive measures for reducing the scope of their recurrence in the healthcare
settings (Bertozzi, 2016). The researchers and healthcare professionals also require exploring
the untoward events risks associated with each medical intervention for configuring the
appropriate mitigating strategies warranted for the systematic handling of healthcare
11 | P a g e
patient fatalities under the influence of inappropriate treatment interventions (Kear & Ulrich,
2015). The research analysis by (Parker, Wensing, Esmail, & Valderas, 2015) indicates the
requirement of improving healthcare processes, rather than the care outcomes for the
systematic establishment of safety culture in the hospital settings. Healthcare professionals
need to conceptualize the patient safety culture in the context of its equitable establishment
across the hospital environment (Parker, Wensing, Esmail, & Valderas, 2015). The
physicians also require exploring the causes of nosocomial infections and undertake
preventive and prophylactic measures for reducing the pattern of their occurrence. The
organization of healthcare awareness sessions is necessarily required for improving the
standards of health and hygiene in the hospital locations. The utilization of hand hygiene
measures proves to be highly effective in preventing the progression of hospital acquired
infections in healthcare settings (Parker, Wensing, Esmail, & Valderas, 2015). Evidence-
based analysis by (Hessels, Murray, Cohen, & Larson, 2017) advocates the requirement of
periodic administration of nursing home and hospital surveys with the objective of
determining the pattern of patient safety culture in the healthcare facilities. Outcomes of these
survey interventions require the systematic analysis by the research professionals in the
context of mitigating the sustained patient safety deficits in the healthcare system. For
example, the staffing deficit in the healthcare facilities warrants mitigation through the
deployment of additional staff or by imparting work management training to the existing
physicians, nurses and other medical professionals associated with the hospital setting. The
systematic documentation of adverse events is necessarily required with the objective of
undertaking proactive measures for reducing the scope of their recurrence in the healthcare
settings (Bertozzi, 2016). The researchers and healthcare professionals also require exploring
the untoward events risks associated with each medical intervention for configuring the
appropriate mitigating strategies warranted for the systematic handling of healthcare
11 | P a g e
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 20
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




