Interpretation and Analysis of Mr. Robert Brown's Head Injury
VerifiedAdded on 2023/04/11
|6
|1581
|445
AI Summary
This document provides an interpretation and analysis of Mr. Robert Brown's head injury, including abnormal vital signs and potential complications. It discusses the importance of monitoring and proper treatment for head injuries.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
Student number:
CNA253 AT2 Scenario: Mr Robert Brown
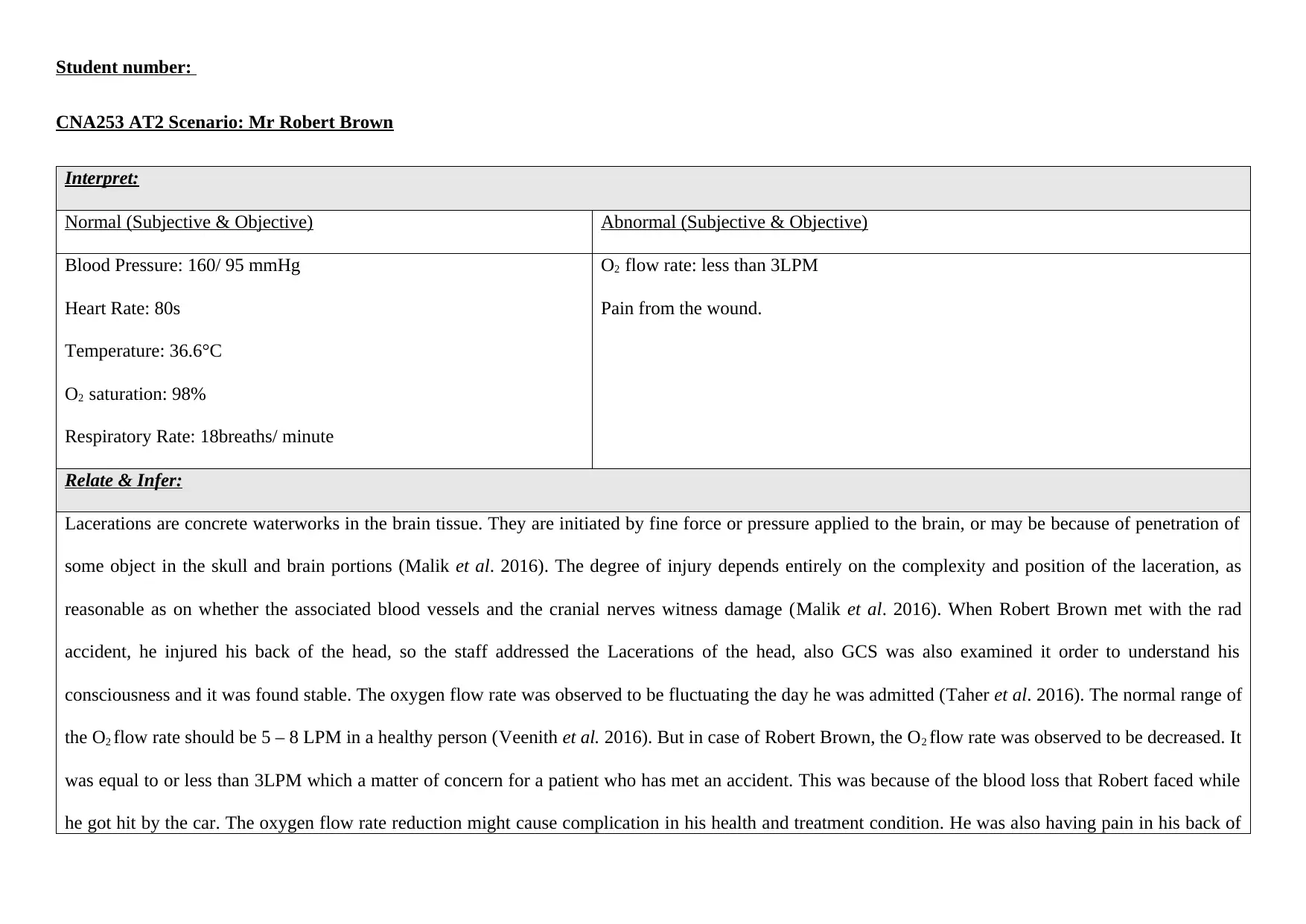
Interpret:
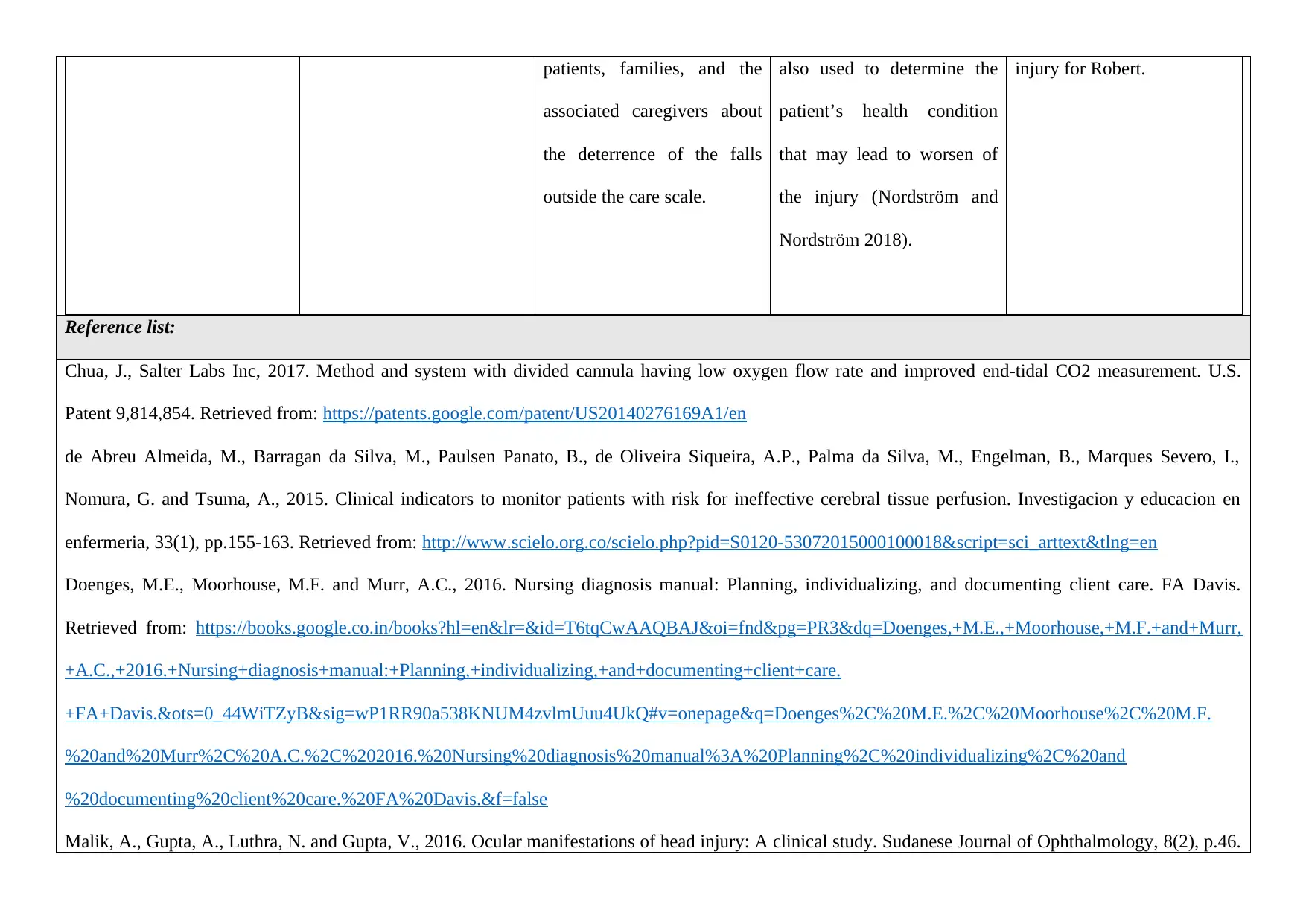
Normal (Subjective & Objective) Abnormal (Subjective & Objective)
Blood Pressure: 160/ 95 mmHg
Heart Rate: 80s
Temperature: 36.6°C
O2 saturation: 98%
Respiratory Rate: 18breaths/ minute
O2 flow rate: less than 3LPM
Pain from the wound.
Relate & Infer:
Lacerations are concrete waterworks in the brain tissue. They are initiated by fine force or pressure applied to the brain, or may be because of penetration of
some object in the skull and brain portions (Malik et al. 2016). The degree of injury depends entirely on the complexity and position of the laceration, as
reasonable as on whether the associated blood vessels and the cranial nerves witness damage (Malik et al. 2016). When Robert Brown met with the rad
accident, he injured his back of the head, so the staff addressed the Lacerations of the head, also GCS was also examined it order to understand his
consciousness and it was found stable. The oxygen flow rate was observed to be fluctuating the day he was admitted (Taher et al. 2016). The normal range of
the O2 flow rate should be 5 – 8 LPM in a healthy person (Veenith et al. 2016). But in case of Robert Brown, the O2 flow rate was observed to be decreased. It
was equal to or less than 3LPM which a matter of concern for a patient who has met an accident. This was because of the blood loss that Robert faced while
he got hit by the car. The oxygen flow rate reduction might cause complication in his health and treatment condition. He was also having pain in his back of
CNA253 AT2 Scenario: Mr Robert Brown
Interpret:
Normal (Subjective & Objective) Abnormal (Subjective & Objective)
Blood Pressure: 160/ 95 mmHg
Heart Rate: 80s
Temperature: 36.6°C
O2 saturation: 98%
Respiratory Rate: 18breaths/ minute
O2 flow rate: less than 3LPM
Pain from the wound.
Relate & Infer:
Lacerations are concrete waterworks in the brain tissue. They are initiated by fine force or pressure applied to the brain, or may be because of penetration of
some object in the skull and brain portions (Malik et al. 2016). The degree of injury depends entirely on the complexity and position of the laceration, as
reasonable as on whether the associated blood vessels and the cranial nerves witness damage (Malik et al. 2016). When Robert Brown met with the rad
accident, he injured his back of the head, so the staff addressed the Lacerations of the head, also GCS was also examined it order to understand his
consciousness and it was found stable. The oxygen flow rate was observed to be fluctuating the day he was admitted (Taher et al. 2016). The normal range of
the O2 flow rate should be 5 – 8 LPM in a healthy person (Veenith et al. 2016). But in case of Robert Brown, the O2 flow rate was observed to be decreased. It
was equal to or less than 3LPM which a matter of concern for a patient who has met an accident. This was because of the blood loss that Robert faced while
he got hit by the car. The oxygen flow rate reduction might cause complication in his health and treatment condition. He was also having pain in his back of
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
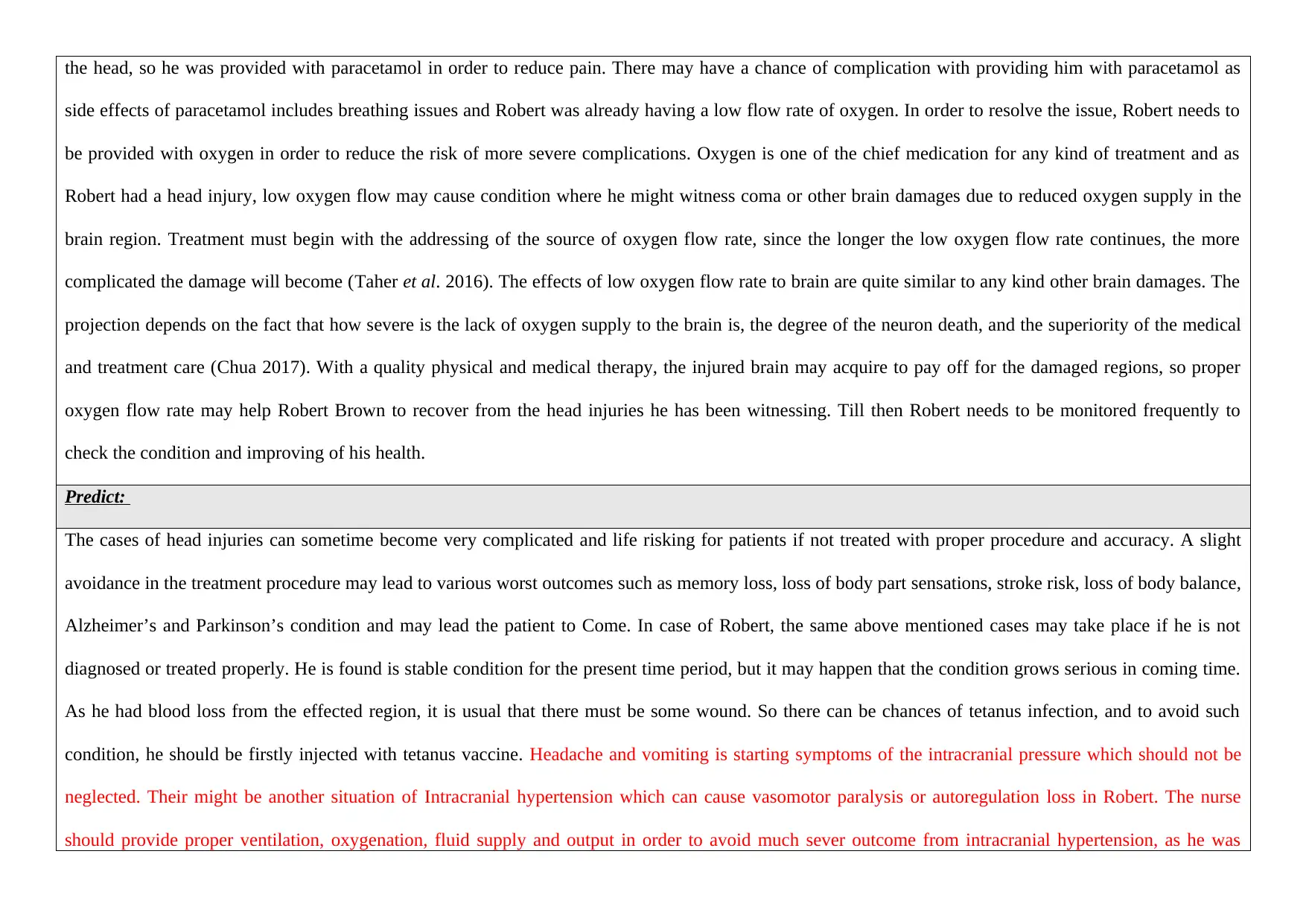
the head, so he was provided with paracetamol in order to reduce pain. There may have a chance of complication with providing him with paracetamol as
side effects of paracetamol includes breathing issues and Robert was already having a low flow rate of oxygen. In order to resolve the issue, Robert needs to
be provided with oxygen in order to reduce the risk of more severe complications. Oxygen is one of the chief medication for any kind of treatment and as
Robert had a head injury, low oxygen flow may cause condition where he might witness coma or other brain damages due to reduced oxygen supply in the
brain region. Treatment must begin with the addressing of the source of oxygen flow rate, since the longer the low oxygen flow rate continues, the more
complicated the damage will become (Taher et al. 2016). The effects of low oxygen flow rate to brain are quite similar to any kind other brain damages. The
projection depends on the fact that how severe is the lack of oxygen supply to the brain is, the degree of the neuron death, and the superiority of the medical
and treatment care (Chua 2017). With a quality physical and medical therapy, the injured brain may acquire to pay off for the damaged regions, so proper
oxygen flow rate may help Robert Brown to recover from the head injuries he has been witnessing. Till then Robert needs to be monitored frequently to
check the condition and improving of his health.
Predict:
The cases of head injuries can sometime become very complicated and life risking for patients if not treated with proper procedure and accuracy. A slight
avoidance in the treatment procedure may lead to various worst outcomes such as memory loss, loss of body part sensations, stroke risk, loss of body balance,
Alzheimer’s and Parkinson’s condition and may lead the patient to Come. In case of Robert, the same above mentioned cases may take place if he is not
diagnosed or treated properly. He is found is stable condition for the present time period, but it may happen that the condition grows serious in coming time.
As he had blood loss from the effected region, it is usual that there must be some wound. So there can be chances of tetanus infection, and to avoid such
condition, he should be firstly injected with tetanus vaccine. Headache and vomiting is starting symptoms of the intracranial pressure which should not be
neglected. Their might be another situation of Intracranial hypertension which can cause vasomotor paralysis or autoregulation loss in Robert. The nurse
should provide proper ventilation, oxygenation, fluid supply and output in order to avoid much sever outcome from intracranial hypertension, as he was
side effects of paracetamol includes breathing issues and Robert was already having a low flow rate of oxygen. In order to resolve the issue, Robert needs to
be provided with oxygen in order to reduce the risk of more severe complications. Oxygen is one of the chief medication for any kind of treatment and as
Robert had a head injury, low oxygen flow may cause condition where he might witness coma or other brain damages due to reduced oxygen supply in the
brain region. Treatment must begin with the addressing of the source of oxygen flow rate, since the longer the low oxygen flow rate continues, the more
complicated the damage will become (Taher et al. 2016). The effects of low oxygen flow rate to brain are quite similar to any kind other brain damages. The
projection depends on the fact that how severe is the lack of oxygen supply to the brain is, the degree of the neuron death, and the superiority of the medical
and treatment care (Chua 2017). With a quality physical and medical therapy, the injured brain may acquire to pay off for the damaged regions, so proper
oxygen flow rate may help Robert Brown to recover from the head injuries he has been witnessing. Till then Robert needs to be monitored frequently to
check the condition and improving of his health.
Predict:
The cases of head injuries can sometime become very complicated and life risking for patients if not treated with proper procedure and accuracy. A slight
avoidance in the treatment procedure may lead to various worst outcomes such as memory loss, loss of body part sensations, stroke risk, loss of body balance,
Alzheimer’s and Parkinson’s condition and may lead the patient to Come. In case of Robert, the same above mentioned cases may take place if he is not
diagnosed or treated properly. He is found is stable condition for the present time period, but it may happen that the condition grows serious in coming time.
As he had blood loss from the effected region, it is usual that there must be some wound. So there can be chances of tetanus infection, and to avoid such
condition, he should be firstly injected with tetanus vaccine. Headache and vomiting is starting symptoms of the intracranial pressure which should not be
neglected. Their might be another situation of Intracranial hypertension which can cause vasomotor paralysis or autoregulation loss in Robert. The nurse
should provide proper ventilation, oxygenation, fluid supply and output in order to avoid much sever outcome from intracranial hypertension, as he was
found complaining about headaches (Yuan et al. 2015). Ineffective tissue perfusion is found to be an effective measure to avoid such circumstances, it will
help in improving circulation and supply of oxygen to the capillaries which will help is restoring the damage that may have caused in the brain (de Abreu
Almeida et al. 2015).
Develop, Articulate and Prioritise Nursing Diagnoses –
1. Ineffective tissue perfusion
2. Injury risk
3. Decreased intracranial adaptive capacity.
The above mentioned are the three nursing diagnosis that are needed to be followed in case if serious head injury.
Goals, Actions and Evaluation
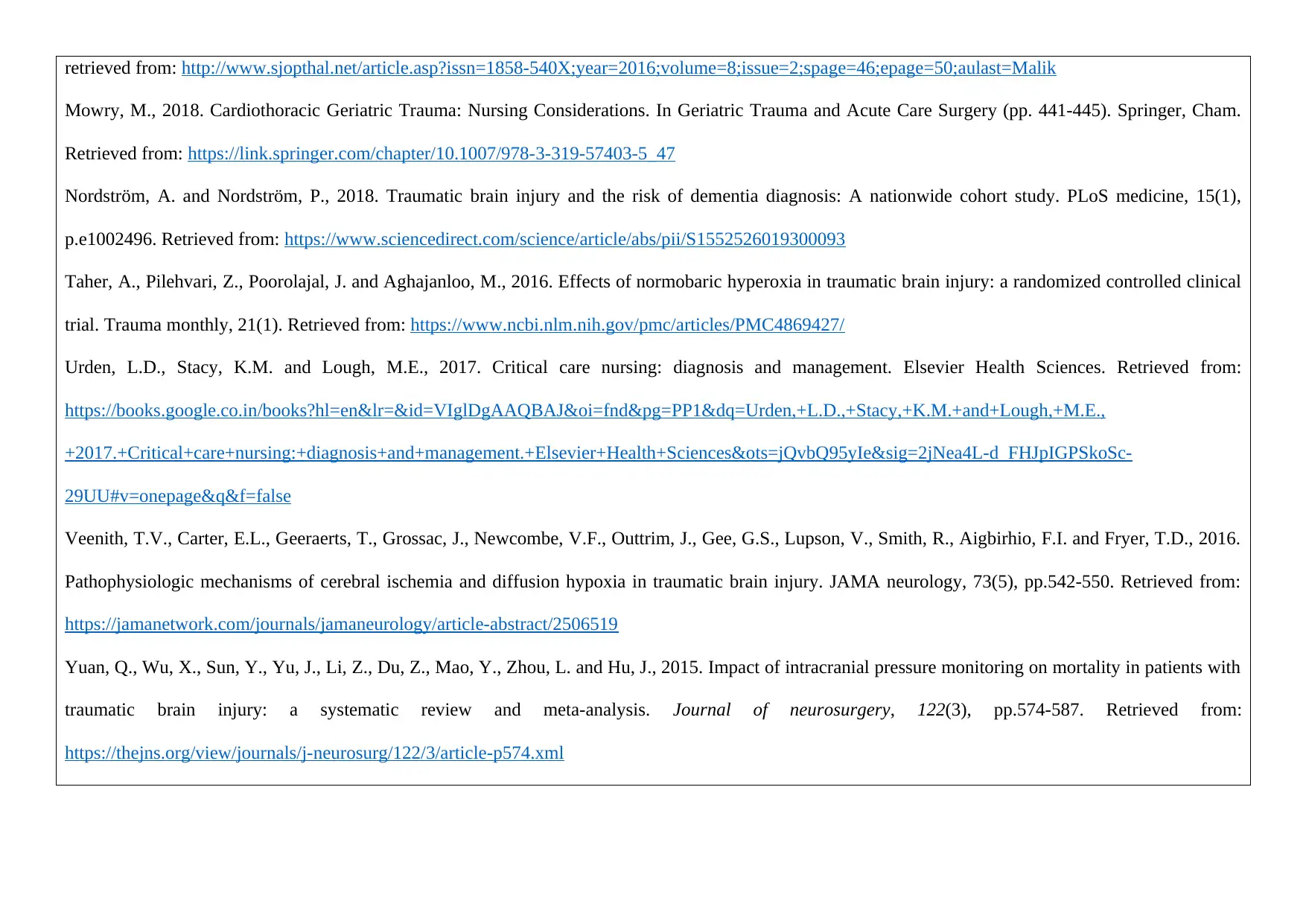
Diagnosis 1 Goal/s Related actions Rationale Evaluate outcomes
Ineffective tissue perfusion
The goal of the diagnosis is
to remove vasoconstriction
aspects, refine exterior blood
flow, and reduce metabolic
difficulties on the body (de
Abreu Almeida et al. 2015).
It also focuses on the
reduction of pressure in the
brain due to head injury
which may lead to a
Monitoring and
documentation of the
neurological condition of the
patient frequently and
compare it with the baseline
(Mowry 2018).
It influences the choice of
interventions. Worsening in
any kind of neurological
signs and sever symptoms or
failure to progress even after
a proper treatment may
reflect diminished
intracranial adaptive ability,
which states that the patient
requires a monitoring session
The patient will witness
improved circulation,
observe changes in lifestyle,
growing tolerance to various
activities, lesser cases of
patient witnessing
difficulties, reduced pain in
the effected region (Doenges
et al. 2016). It also increases
circulation, and supply of
help in improving circulation and supply of oxygen to the capillaries which will help is restoring the damage that may have caused in the brain (de Abreu
Almeida et al. 2015).
Develop, Articulate and Prioritise Nursing Diagnoses –
1. Ineffective tissue perfusion
2. Injury risk
3. Decreased intracranial adaptive capacity.
The above mentioned are the three nursing diagnosis that are needed to be followed in case if serious head injury.
Goals, Actions and Evaluation
Diagnosis 1 Goal/s Related actions Rationale Evaluate outcomes
Ineffective tissue perfusion
The goal of the diagnosis is
to remove vasoconstriction
aspects, refine exterior blood
flow, and reduce metabolic
difficulties on the body (de
Abreu Almeida et al. 2015).
It also focuses on the
reduction of pressure in the
brain due to head injury
which may lead to a
Monitoring and
documentation of the
neurological condition of the
patient frequently and
compare it with the baseline
(Mowry 2018).
It influences the choice of
interventions. Worsening in
any kind of neurological
signs and sever symptoms or
failure to progress even after
a proper treatment may
reflect diminished
intracranial adaptive ability,
which states that the patient
requires a monitoring session
The patient will witness
improved circulation,
observe changes in lifestyle,
growing tolerance to various
activities, lesser cases of
patient witnessing
difficulties, reduced pain in
the effected region (Doenges
et al. 2016). It also increases
circulation, and supply of
situation called Intracranial
hypertension (IH) where the
patient might witness
vasomotor paralysis (Yuan
et al. 2015).
Ineffective tissue perfusion
and if any kind of worse
effects and symptoms are
observed then a proper
intervention should be
incorporated.
oxygen in patients’
capillaries, which will reduce
the chances of paralysis or
coma in patients with head
injury (Yuan et al. 2015).
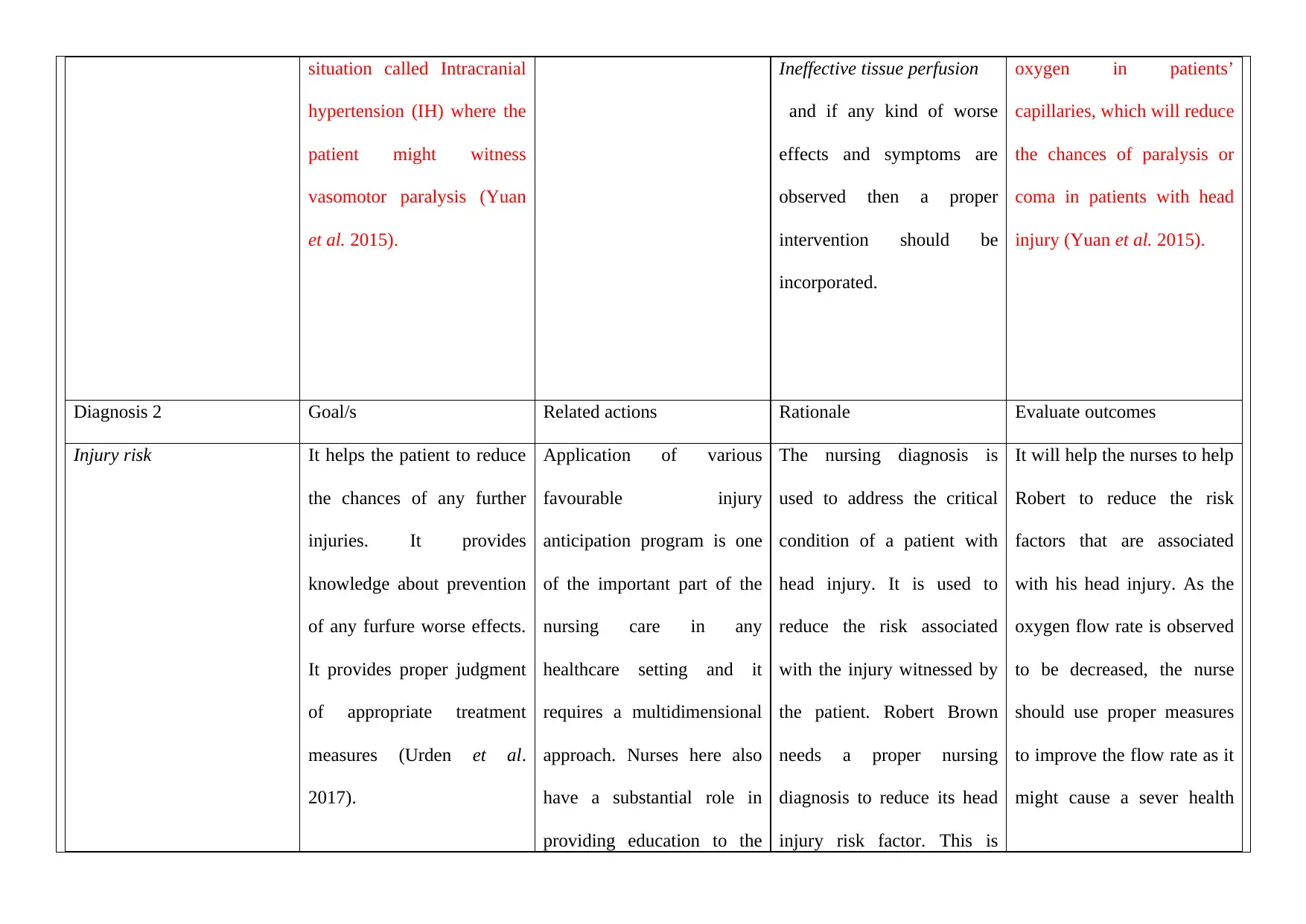
Diagnosis 2 Goal/s Related actions Rationale Evaluate outcomes
Injury risk It helps the patient to reduce
the chances of any further
injuries. It provides
knowledge about prevention
of any furfure worse effects.
It provides proper judgment
of appropriate treatment
measures (Urden et al.
2017).
Application of various
favourable injury
anticipation program is one
of the important part of the
nursing care in any
healthcare setting and it
requires a multidimensional
approach. Nurses here also
have a substantial role in
providing education to the
The nursing diagnosis is
used to address the critical
condition of a patient with
head injury. It is used to
reduce the risk associated
with the injury witnessed by
the patient. Robert Brown
needs a proper nursing
diagnosis to reduce its head
injury risk factor. This is
It will help the nurses to help
Robert to reduce the risk
factors that are associated
with his head injury. As the
oxygen flow rate is observed
to be decreased, the nurse
should use proper measures
to improve the flow rate as it
might cause a sever health
hypertension (IH) where the
patient might witness
vasomotor paralysis (Yuan
et al. 2015).
Ineffective tissue perfusion
and if any kind of worse
effects and symptoms are
observed then a proper
intervention should be
incorporated.
oxygen in patients’
capillaries, which will reduce
the chances of paralysis or
coma in patients with head
injury (Yuan et al. 2015).
Diagnosis 2 Goal/s Related actions Rationale Evaluate outcomes
Injury risk It helps the patient to reduce
the chances of any further
injuries. It provides
knowledge about prevention
of any furfure worse effects.
It provides proper judgment
of appropriate treatment
measures (Urden et al.
2017).
Application of various
favourable injury
anticipation program is one
of the important part of the
nursing care in any
healthcare setting and it
requires a multidimensional
approach. Nurses here also
have a substantial role in
providing education to the
The nursing diagnosis is
used to address the critical
condition of a patient with
head injury. It is used to
reduce the risk associated
with the injury witnessed by
the patient. Robert Brown
needs a proper nursing
diagnosis to reduce its head
injury risk factor. This is
It will help the nurses to help
Robert to reduce the risk
factors that are associated
with his head injury. As the
oxygen flow rate is observed
to be decreased, the nurse
should use proper measures
to improve the flow rate as it
might cause a sever health
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
patients, families, and the
associated caregivers about
the deterrence of the falls
outside the care scale.
also used to determine the
patient’s health condition
that may lead to worsen of
the injury (Nordström and
Nordström 2018).
injury for Robert.
Reference list:
Chua, J., Salter Labs Inc, 2017. Method and system with divided cannula having low oxygen flow rate and improved end-tidal CO2 measurement. U.S.
Patent 9,814,854. Retrieved from: https://patents.google.com/patent/US20140276169A1/en
de Abreu Almeida, M., Barragan da Silva, M., Paulsen Panato, B., de Oliveira Siqueira, A.P., Palma da Silva, M., Engelman, B., Marques Severo, I.,
Nomura, G. and Tsuma, A., 2015. Clinical indicators to monitor patients with risk for ineffective cerebral tissue perfusion. Investigacion y educacion en
enfermeria, 33(1), pp.155-163. Retrieved from: http://www.scielo.org.co/scielo.php?pid=S0120-53072015000100018&script=sci_arttext&tlng=en
Doenges, M.E., Moorhouse, M.F. and Murr, A.C., 2016. Nursing diagnosis manual: Planning, individualizing, and documenting client care. FA Davis.
Retrieved from: https://books.google.co.in/books?hl=en&lr=&id=T6tqCwAAQBAJ&oi=fnd&pg=PR3&dq=Doenges,+M.E.,+Moorhouse,+M.F.+and+Murr,
+A.C.,+2016.+Nursing+diagnosis+manual:+Planning,+individualizing,+and+documenting+client+care.
+FA+Davis.&ots=0_44WiTZyB&sig=wP1RR90a538KNUM4zvlmUuu4UkQ#v=onepage&q=Doenges%2C%20M.E.%2C%20Moorhouse%2C%20M.F.
%20and%20Murr%2C%20A.C.%2C%202016.%20Nursing%20diagnosis%20manual%3A%20Planning%2C%20individualizing%2C%20and
%20documenting%20client%20care.%20FA%20Davis.&f=false
Malik, A., Gupta, A., Luthra, N. and Gupta, V., 2016. Ocular manifestations of head injury: A clinical study. Sudanese Journal of Ophthalmology, 8(2), p.46.
associated caregivers about
the deterrence of the falls
outside the care scale.
also used to determine the
patient’s health condition
that may lead to worsen of
the injury (Nordström and
Nordström 2018).
injury for Robert.
Reference list:
Chua, J., Salter Labs Inc, 2017. Method and system with divided cannula having low oxygen flow rate and improved end-tidal CO2 measurement. U.S.
Patent 9,814,854. Retrieved from: https://patents.google.com/patent/US20140276169A1/en
de Abreu Almeida, M., Barragan da Silva, M., Paulsen Panato, B., de Oliveira Siqueira, A.P., Palma da Silva, M., Engelman, B., Marques Severo, I.,
Nomura, G. and Tsuma, A., 2015. Clinical indicators to monitor patients with risk for ineffective cerebral tissue perfusion. Investigacion y educacion en
enfermeria, 33(1), pp.155-163. Retrieved from: http://www.scielo.org.co/scielo.php?pid=S0120-53072015000100018&script=sci_arttext&tlng=en
Doenges, M.E., Moorhouse, M.F. and Murr, A.C., 2016. Nursing diagnosis manual: Planning, individualizing, and documenting client care. FA Davis.
Retrieved from: https://books.google.co.in/books?hl=en&lr=&id=T6tqCwAAQBAJ&oi=fnd&pg=PR3&dq=Doenges,+M.E.,+Moorhouse,+M.F.+and+Murr,
+A.C.,+2016.+Nursing+diagnosis+manual:+Planning,+individualizing,+and+documenting+client+care.
+FA+Davis.&ots=0_44WiTZyB&sig=wP1RR90a538KNUM4zvlmUuu4UkQ#v=onepage&q=Doenges%2C%20M.E.%2C%20Moorhouse%2C%20M.F.
%20and%20Murr%2C%20A.C.%2C%202016.%20Nursing%20diagnosis%20manual%3A%20Planning%2C%20individualizing%2C%20and
%20documenting%20client%20care.%20FA%20Davis.&f=false
Malik, A., Gupta, A., Luthra, N. and Gupta, V., 2016. Ocular manifestations of head injury: A clinical study. Sudanese Journal of Ophthalmology, 8(2), p.46.
retrieved from: http://www.sjopthal.net/article.asp?issn=1858-540X;year=2016;volume=8;issue=2;spage=46;epage=50;aulast=Malik
Mowry, M., 2018. Cardiothoracic Geriatric Trauma: Nursing Considerations. In Geriatric Trauma and Acute Care Surgery (pp. 441-445). Springer, Cham.
Retrieved from: https://link.springer.com/chapter/10.1007/978-3-319-57403-5_47
Nordström, A. and Nordström, P., 2018. Traumatic brain injury and the risk of dementia diagnosis: A nationwide cohort study. PLoS medicine, 15(1),
p.e1002496. Retrieved from: https://www.sciencedirect.com/science/article/abs/pii/S1552526019300093
Taher, A., Pilehvari, Z., Poorolajal, J. and Aghajanloo, M., 2016. Effects of normobaric hyperoxia in traumatic brain injury: a randomized controlled clinical
trial. Trauma monthly, 21(1). Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4869427/
Urden, L.D., Stacy, K.M. and Lough, M.E., 2017. Critical care nursing: diagnosis and management. Elsevier Health Sciences. Retrieved from:
https://books.google.co.in/books?hl=en&lr=&id=VIglDgAAQBAJ&oi=fnd&pg=PP1&dq=Urden,+L.D.,+Stacy,+K.M.+and+Lough,+M.E.,
+2017.+Critical+care+nursing:+diagnosis+and+management.+Elsevier+Health+Sciences&ots=jQvbQ95yIe&sig=2jNea4L-d_FHJpIGPSkoSc-
29UU#v=onepage&q&f=false
Veenith, T.V., Carter, E.L., Geeraerts, T., Grossac, J., Newcombe, V.F., Outtrim, J., Gee, G.S., Lupson, V., Smith, R., Aigbirhio, F.I. and Fryer, T.D., 2016.
Pathophysiologic mechanisms of cerebral ischemia and diffusion hypoxia in traumatic brain injury. JAMA neurology, 73(5), pp.542-550. Retrieved from:
https://jamanetwork.com/journals/jamaneurology/article-abstract/2506519
Yuan, Q., Wu, X., Sun, Y., Yu, J., Li, Z., Du, Z., Mao, Y., Zhou, L. and Hu, J., 2015. Impact of intracranial pressure monitoring on mortality in patients with
traumatic brain injury: a systematic review and meta-analysis. Journal of neurosurgery, 122(3), pp.574-587. Retrieved from:
https://thejns.org/view/journals/j-neurosurg/122/3/article-p574.xml
Mowry, M., 2018. Cardiothoracic Geriatric Trauma: Nursing Considerations. In Geriatric Trauma and Acute Care Surgery (pp. 441-445). Springer, Cham.
Retrieved from: https://link.springer.com/chapter/10.1007/978-3-319-57403-5_47
Nordström, A. and Nordström, P., 2018. Traumatic brain injury and the risk of dementia diagnosis: A nationwide cohort study. PLoS medicine, 15(1),
p.e1002496. Retrieved from: https://www.sciencedirect.com/science/article/abs/pii/S1552526019300093
Taher, A., Pilehvari, Z., Poorolajal, J. and Aghajanloo, M., 2016. Effects of normobaric hyperoxia in traumatic brain injury: a randomized controlled clinical
trial. Trauma monthly, 21(1). Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4869427/
Urden, L.D., Stacy, K.M. and Lough, M.E., 2017. Critical care nursing: diagnosis and management. Elsevier Health Sciences. Retrieved from:
https://books.google.co.in/books?hl=en&lr=&id=VIglDgAAQBAJ&oi=fnd&pg=PP1&dq=Urden,+L.D.,+Stacy,+K.M.+and+Lough,+M.E.,
+2017.+Critical+care+nursing:+diagnosis+and+management.+Elsevier+Health+Sciences&ots=jQvbQ95yIe&sig=2jNea4L-d_FHJpIGPSkoSc-
29UU#v=onepage&q&f=false
Veenith, T.V., Carter, E.L., Geeraerts, T., Grossac, J., Newcombe, V.F., Outtrim, J., Gee, G.S., Lupson, V., Smith, R., Aigbirhio, F.I. and Fryer, T.D., 2016.
Pathophysiologic mechanisms of cerebral ischemia and diffusion hypoxia in traumatic brain injury. JAMA neurology, 73(5), pp.542-550. Retrieved from:
https://jamanetwork.com/journals/jamaneurology/article-abstract/2506519
Yuan, Q., Wu, X., Sun, Y., Yu, J., Li, Z., Du, Z., Mao, Y., Zhou, L. and Hu, J., 2015. Impact of intracranial pressure monitoring on mortality in patients with
traumatic brain injury: a systematic review and meta-analysis. Journal of neurosurgery, 122(3), pp.574-587. Retrieved from:
https://thejns.org/view/journals/j-neurosurg/122/3/article-p574.xml
1 out of 6
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





