Suggested Template Nrsg355 Written Assessment 2022
VerifiedAdded on 2022/10/17
|12
|3800
|16
AI Summary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
NRSG355 2018 |
SUGGESTED TEMPLATE: NRSG355 WRITTEN ASSESSMENT
This is a guide only – you may write this as a long form essay as long as you provide
headings for each question.
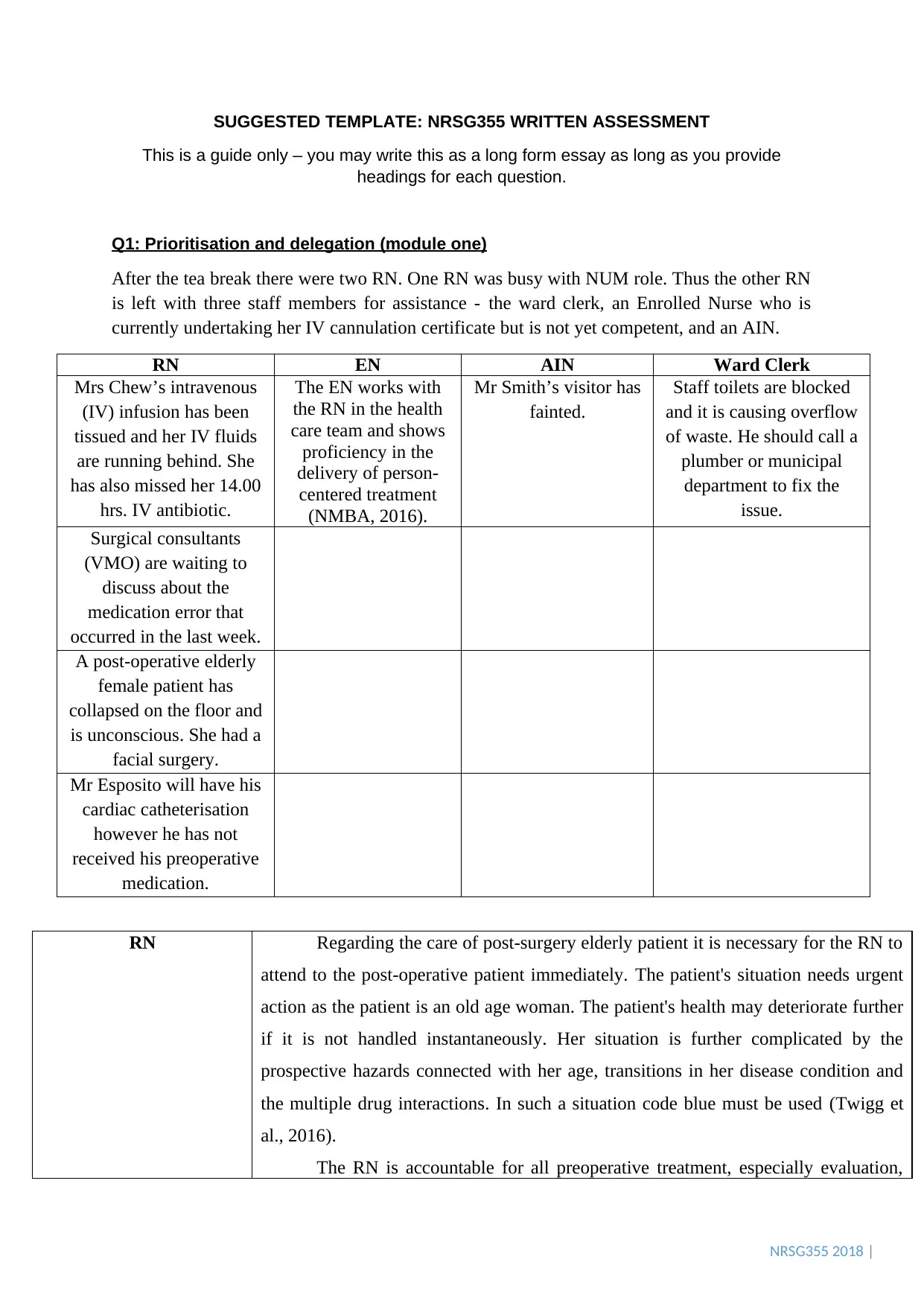
Q1: Prioritisation and delegation (module one)
After the tea break there were two RN. One RN was busy with NUM role. Thus the other RN
is left with three staff members for assistance - the ward clerk, an Enrolled Nurse who is
currently undertaking her IV cannulation certificate but is not yet competent, and an AIN.
RN EN AIN Ward Clerk
Mrs Chew’s intravenous
(IV) infusion has been
tissued and her IV fluids
are running behind. She
has also missed her 14.00
hrs. IV antibiotic.
The EN works with
the RN in the health
care team and shows
proficiency in the
delivery of person-
centered treatment
(NMBA, 2016).
Mr Smith’s visitor has
fainted.
Staff toilets are blocked
and it is causing overflow
of waste. He should call a
plumber or municipal
department to fix the
issue.
Surgical consultants
(VMO) are waiting to
discuss about the
medication error that
occurred in the last week.
A post-operative elderly
female patient has
collapsed on the floor and
is unconscious. She had a
facial surgery.
Mr Esposito will have his
cardiac catheterisation
however he has not
received his preoperative
medication.
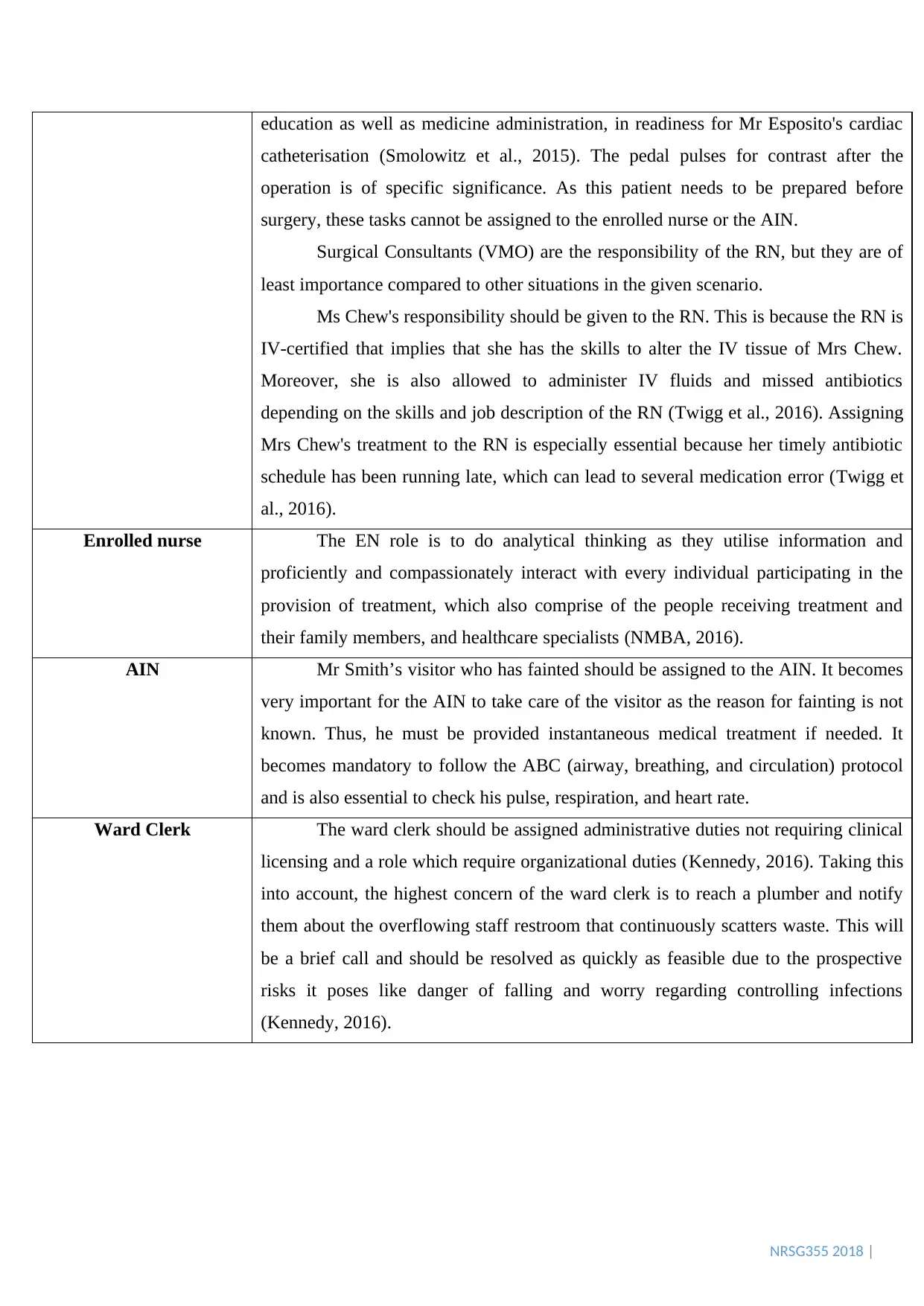
RN Regarding the care of post-surgery elderly patient it is necessary for the RN to
attend to the post-operative patient immediately. The patient's situation needs urgent
action as the patient is an old age woman. The patient's health may deteriorate further
if it is not handled instantaneously. Her situation is further complicated by the
prospective hazards connected with her age, transitions in her disease condition and
the multiple drug interactions. In such a situation code blue must be used (Twigg et
al., 2016).
The RN is accountable for all preoperative treatment, especially evaluation,
SUGGESTED TEMPLATE: NRSG355 WRITTEN ASSESSMENT
This is a guide only – you may write this as a long form essay as long as you provide
headings for each question.
Q1: Prioritisation and delegation (module one)
After the tea break there were two RN. One RN was busy with NUM role. Thus the other RN
is left with three staff members for assistance - the ward clerk, an Enrolled Nurse who is
currently undertaking her IV cannulation certificate but is not yet competent, and an AIN.
RN EN AIN Ward Clerk
Mrs Chew’s intravenous
(IV) infusion has been
tissued and her IV fluids
are running behind. She
has also missed her 14.00
hrs. IV antibiotic.
The EN works with
the RN in the health
care team and shows
proficiency in the
delivery of person-
centered treatment
(NMBA, 2016).
Mr Smith’s visitor has
fainted.
Staff toilets are blocked
and it is causing overflow
of waste. He should call a
plumber or municipal
department to fix the
issue.
Surgical consultants
(VMO) are waiting to
discuss about the
medication error that
occurred in the last week.
A post-operative elderly
female patient has
collapsed on the floor and
is unconscious. She had a
facial surgery.
Mr Esposito will have his
cardiac catheterisation
however he has not
received his preoperative
medication.
RN Regarding the care of post-surgery elderly patient it is necessary for the RN to
attend to the post-operative patient immediately. The patient's situation needs urgent
action as the patient is an old age woman. The patient's health may deteriorate further
if it is not handled instantaneously. Her situation is further complicated by the
prospective hazards connected with her age, transitions in her disease condition and
the multiple drug interactions. In such a situation code blue must be used (Twigg et
al., 2016).
The RN is accountable for all preoperative treatment, especially evaluation,
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
NRSG355 2018 |
education as well as medicine administration, in readiness for Mr Esposito's cardiac
catheterisation (Smolowitz et al., 2015). The pedal pulses for contrast after the
operation is of specific significance. As this patient needs to be prepared before
surgery, these tasks cannot be assigned to the enrolled nurse or the AIN.
Surgical Consultants (VMO) are the responsibility of the RN, but they are of
least importance compared to other situations in the given scenario.
Ms Chew's responsibility should be given to the RN. This is because the RN is
IV-certified that implies that she has the skills to alter the IV tissue of Mrs Chew.
Moreover, she is also allowed to administer IV fluids and missed antibiotics
depending on the skills and job description of the RN (Twigg et al., 2016). Assigning
Mrs Chew's treatment to the RN is especially essential because her timely antibiotic
schedule has been running late, which can lead to several medication error (Twigg et
al., 2016).
Enrolled nurse The EN role is to do analytical thinking as they utilise information and
proficiently and compassionately interact with every individual participating in the
provision of treatment, which also comprise of the people receiving treatment and
their family members, and healthcare specialists (NMBA, 2016).
AIN Mr Smith’s visitor who has fainted should be assigned to the AIN. It becomes
very important for the AIN to take care of the visitor as the reason for fainting is not
known. Thus, he must be provided instantaneous medical treatment if needed. It
becomes mandatory to follow the ABC (airway, breathing, and circulation) protocol
and is also essential to check his pulse, respiration, and heart rate.
Ward Clerk The ward clerk should be assigned administrative duties not requiring clinical
licensing and a role which require organizational duties (Kennedy, 2016). Taking this
into account, the highest concern of the ward clerk is to reach a plumber and notify
them about the overflowing staff restroom that continuously scatters waste. This will
be a brief call and should be resolved as quickly as feasible due to the prospective
risks it poses like danger of falling and worry regarding controlling infections
(Kennedy, 2016).
education as well as medicine administration, in readiness for Mr Esposito's cardiac
catheterisation (Smolowitz et al., 2015). The pedal pulses for contrast after the
operation is of specific significance. As this patient needs to be prepared before
surgery, these tasks cannot be assigned to the enrolled nurse or the AIN.
Surgical Consultants (VMO) are the responsibility of the RN, but they are of
least importance compared to other situations in the given scenario.
Ms Chew's responsibility should be given to the RN. This is because the RN is
IV-certified that implies that she has the skills to alter the IV tissue of Mrs Chew.
Moreover, she is also allowed to administer IV fluids and missed antibiotics
depending on the skills and job description of the RN (Twigg et al., 2016). Assigning
Mrs Chew's treatment to the RN is especially essential because her timely antibiotic
schedule has been running late, which can lead to several medication error (Twigg et
al., 2016).
Enrolled nurse The EN role is to do analytical thinking as they utilise information and
proficiently and compassionately interact with every individual participating in the
provision of treatment, which also comprise of the people receiving treatment and
their family members, and healthcare specialists (NMBA, 2016).
AIN Mr Smith’s visitor who has fainted should be assigned to the AIN. It becomes
very important for the AIN to take care of the visitor as the reason for fainting is not
known. Thus, he must be provided instantaneous medical treatment if needed. It
becomes mandatory to follow the ABC (airway, breathing, and circulation) protocol
and is also essential to check his pulse, respiration, and heart rate.
Ward Clerk The ward clerk should be assigned administrative duties not requiring clinical
licensing and a role which require organizational duties (Kennedy, 2016). Taking this
into account, the highest concern of the ward clerk is to reach a plumber and notify
them about the overflowing staff restroom that continuously scatters waste. This will
be a brief call and should be resolved as quickly as feasible due to the prospective
risks it poses like danger of falling and worry regarding controlling infections
(Kennedy, 2016).
NRSG355 2018 |
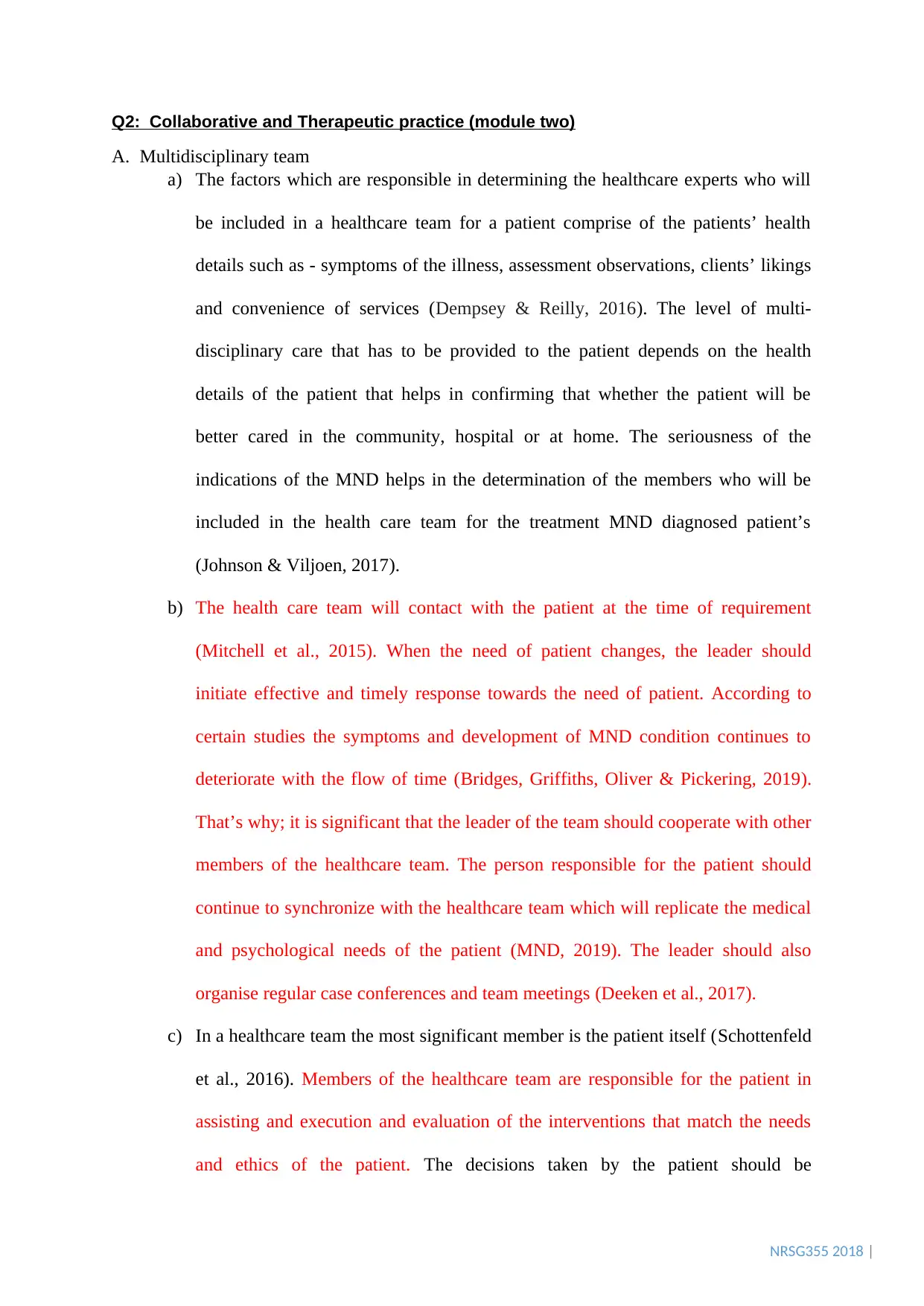
Q2: Collaborative and Therapeutic practice (module two)
A. Multidisciplinary team
a) The factors which are responsible in determining the healthcare experts who will
be included in a healthcare team for a patient comprise of the patients’ health
details such as - symptoms of the illness, assessment observations, clients’ likings
and convenience of services (Dempsey & Reilly, 2016). The level of multi-
disciplinary care that has to be provided to the patient depends on the health
details of the patient that helps in confirming that whether the patient will be
better cared in the community, hospital or at home. The seriousness of the
indications of the MND helps in the determination of the members who will be
included in the health care team for the treatment MND diagnosed patient’s
(Johnson & Viljoen, 2017).
b) The health care team will contact with the patient at the time of requirement
(Mitchell et al., 2015). When the need of patient changes, the leader should
initiate effective and timely response towards the need of patient. According to
certain studies the symptoms and development of MND condition continues to
deteriorate with the flow of time (Bridges, Griffiths, Oliver & Pickering, 2019).
That’s why; it is significant that the leader of the team should cooperate with other
members of the healthcare team. The person responsible for the patient should
continue to synchronize with the healthcare team which will replicate the medical
and psychological needs of the patient (MND, 2019). The leader should also
organise regular case conferences and team meetings (Deeken et al., 2017).
c) In a healthcare team the most significant member is the patient itself (Schottenfeld
et al., 2016). Members of the healthcare team are responsible for the patient in
assisting and execution and evaluation of the interventions that match the needs
and ethics of the patient. The decisions taken by the patient should be
Q2: Collaborative and Therapeutic practice (module two)
A. Multidisciplinary team
a) The factors which are responsible in determining the healthcare experts who will
be included in a healthcare team for a patient comprise of the patients’ health
details such as - symptoms of the illness, assessment observations, clients’ likings
and convenience of services (Dempsey & Reilly, 2016). The level of multi-
disciplinary care that has to be provided to the patient depends on the health
details of the patient that helps in confirming that whether the patient will be
better cared in the community, hospital or at home. The seriousness of the
indications of the MND helps in the determination of the members who will be
included in the health care team for the treatment MND diagnosed patient’s
(Johnson & Viljoen, 2017).
b) The health care team will contact with the patient at the time of requirement
(Mitchell et al., 2015). When the need of patient changes, the leader should
initiate effective and timely response towards the need of patient. According to
certain studies the symptoms and development of MND condition continues to
deteriorate with the flow of time (Bridges, Griffiths, Oliver & Pickering, 2019).
That’s why; it is significant that the leader of the team should cooperate with other
members of the healthcare team. The person responsible for the patient should
continue to synchronize with the healthcare team which will replicate the medical
and psychological needs of the patient (MND, 2019). The leader should also
organise regular case conferences and team meetings (Deeken et al., 2017).
c) In a healthcare team the most significant member is the patient itself (Schottenfeld
et al., 2016). Members of the healthcare team are responsible for the patient in
assisting and execution and evaluation of the interventions that match the needs
and ethics of the patient. The decisions taken by the patient should be
NRSG355 2018 |
implemented in a way to enhance the quality of life and fulfil the needs of the
patient suffering from MND (Karazivan et al., 2015).
B. Case study name: CASE STUDY 3 (Robert Hughes)
1. This case study discusses about Robert Hughes (52 year old male) who met with a
bicycle accident. There are two key issues in the case-study,
a. Aggressive nature of Robert towards the staff and other patients and
b. Robert’s mother is 75 years of age. She cannot take care of Robert because of
her old age.
2. The health care team should consist of community aged care workers, orthotist,
physiotherapist, and a social worker or psychologist (Housley, 2017). They all have
their individual roles. Community aged care workers will take care of Robert’s
mother by providing general household assistance, emotional support, care and
companionship when she will feel lonely or worry about Robert. An orthotist and
physiotherapist will help in treating the fractures in Robert’s (R) tibia/fibula and (R)
radius.An orthotist can assist Robert by providing advice and timely provision of
artificial or mechanical aids, such as braces to prevent or assist movement of the
fractured parts to help prolong function of Robert. A physiotherapist will help Robert
in doing physical activity and mobility for the improvement and fast healing of the
fractured parts (Reeves et al., 2017). As Robert has shown aggressive nature, he will
be supported by a social worker or psychologist. They will counsel his psychological,
emotional and aggressive aspects of living. The social worker can also provide
information on community services that may assist Robert and her mother with
accommodation, legal, financial and other issues (Reeves et al., 2017).
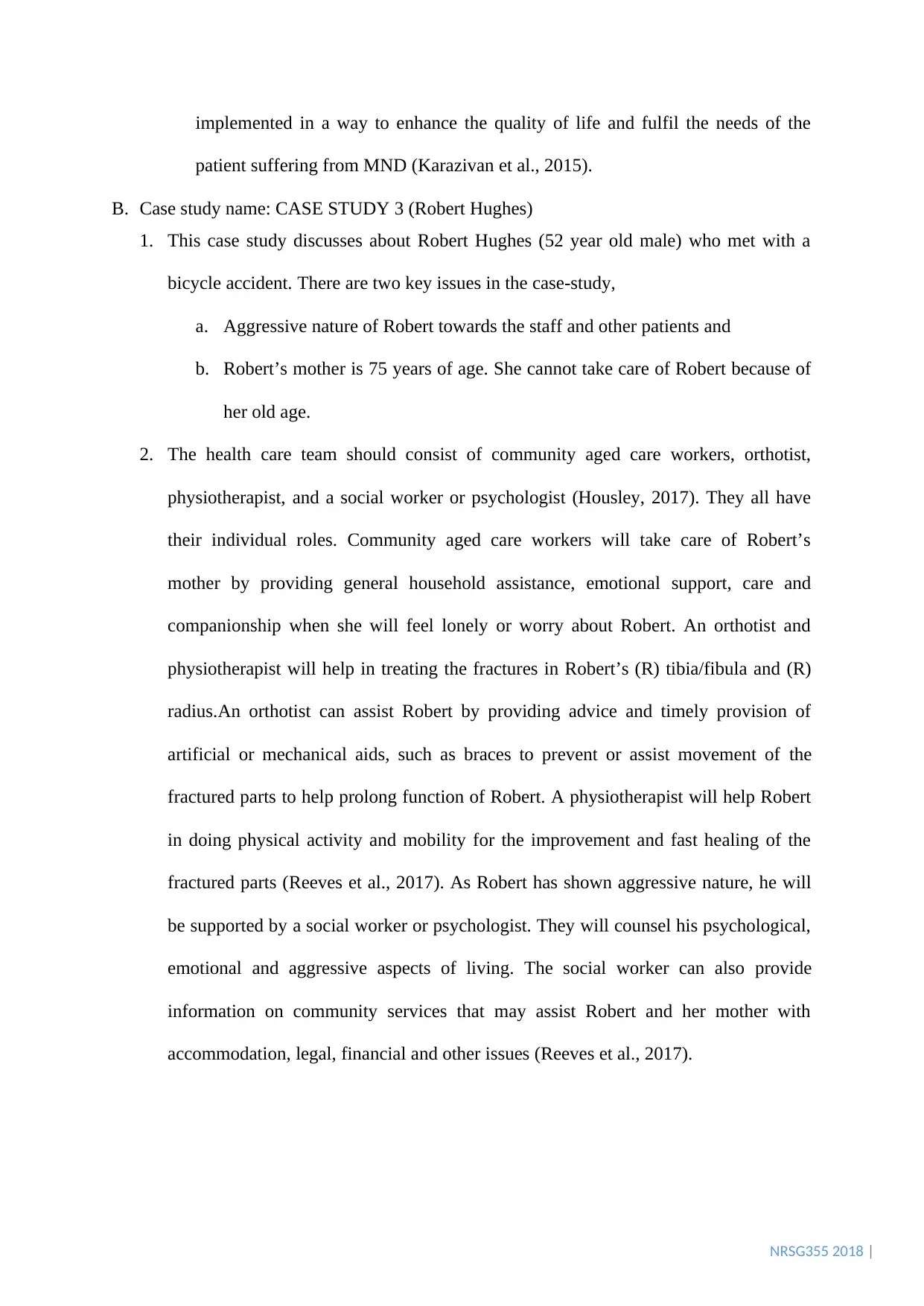
implemented in a way to enhance the quality of life and fulfil the needs of the
patient suffering from MND (Karazivan et al., 2015).
B. Case study name: CASE STUDY 3 (Robert Hughes)
1. This case study discusses about Robert Hughes (52 year old male) who met with a
bicycle accident. There are two key issues in the case-study,
a. Aggressive nature of Robert towards the staff and other patients and
b. Robert’s mother is 75 years of age. She cannot take care of Robert because of
her old age.
2. The health care team should consist of community aged care workers, orthotist,
physiotherapist, and a social worker or psychologist (Housley, 2017). They all have
their individual roles. Community aged care workers will take care of Robert’s
mother by providing general household assistance, emotional support, care and
companionship when she will feel lonely or worry about Robert. An orthotist and
physiotherapist will help in treating the fractures in Robert’s (R) tibia/fibula and (R)
radius.An orthotist can assist Robert by providing advice and timely provision of
artificial or mechanical aids, such as braces to prevent or assist movement of the
fractured parts to help prolong function of Robert. A physiotherapist will help Robert
in doing physical activity and mobility for the improvement and fast healing of the
fractured parts (Reeves et al., 2017). As Robert has shown aggressive nature, he will
be supported by a social worker or psychologist. They will counsel his psychological,
emotional and aggressive aspects of living. The social worker can also provide
information on community services that may assist Robert and her mother with
accommodation, legal, financial and other issues (Reeves et al., 2017).
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
NRSG355 2018 |
Q3: Provision and coordination of care (module three)
Activity 1
1. Questions that can be asked to the nurse are –
What is the reason for his abdominal pain? These questions will be asked to
the nurse, to understand the relationship among the abdominal pain and his
different medical history such as is the abdominal pain arising due to any side-
effects of his gastric ulcer (Mascolo et al., 2015).
Why did he lose 3 kg? Is there any injury in the abdomen which is causing
loss of blood that is leading to abdomen pain and weight loss? Or is it due to
lack of proper amount of intake of food. These questions will help in
understanding of the sudden decrease in weight.
Why is IV antibiotics like Cefazolin and Gentamicin given to Joe? What is the
purpose of giving these antibiotics and how will it help Joe?
Has his fluid balanced chart been prepared? It should be prepared as soon as
possible to recognize when Joe requires fluid intake as he goes for urinary
twice a day. If there is any abnormality, then a plan of care will be created to
treat the urinary problem. Management of adequate level of fluid is essential
to health (Scales & Pilsworth, 2008).
2. Assessments that are needed to be conducted are linked with physiological priority
and psychological priority.
Full body check-up – This will help to assess the general health of Joe. It will help in
preventing any further issues. This will help in the detection of any potential health problems.
It will help in assessment of symptom regarding the gastric ulcer; it will help in the
identification of the cause of abdominal pain (Kwee & Kwee, 2019).
Pain assessment – The pain of the patient should be assessed before implementing any
intervention for the treatment of abdominal pain. Assessment of the level of pain will help the
Q3: Provision and coordination of care (module three)
Activity 1
1. Questions that can be asked to the nurse are –
What is the reason for his abdominal pain? These questions will be asked to
the nurse, to understand the relationship among the abdominal pain and his
different medical history such as is the abdominal pain arising due to any side-
effects of his gastric ulcer (Mascolo et al., 2015).
Why did he lose 3 kg? Is there any injury in the abdomen which is causing
loss of blood that is leading to abdomen pain and weight loss? Or is it due to
lack of proper amount of intake of food. These questions will help in
understanding of the sudden decrease in weight.
Why is IV antibiotics like Cefazolin and Gentamicin given to Joe? What is the
purpose of giving these antibiotics and how will it help Joe?
Has his fluid balanced chart been prepared? It should be prepared as soon as
possible to recognize when Joe requires fluid intake as he goes for urinary
twice a day. If there is any abnormality, then a plan of care will be created to
treat the urinary problem. Management of adequate level of fluid is essential
to health (Scales & Pilsworth, 2008).
2. Assessments that are needed to be conducted are linked with physiological priority
and psychological priority.
Full body check-up – This will help to assess the general health of Joe. It will help in
preventing any further issues. This will help in the detection of any potential health problems.
It will help in assessment of symptom regarding the gastric ulcer; it will help in the
identification of the cause of abdominal pain (Kwee & Kwee, 2019).
Pain assessment – The pain of the patient should be assessed before implementing any
intervention for the treatment of abdominal pain. Assessment of the level of pain will help the
NRSG355 2018 |
nursing staffs to form effective pain management interventions (Zaccagnino & Nedeljkovic,
2017).
Examining the vital signs – This include the respiration rate, heart rate, temperature, SpO2
concentration. This will help in the understanding of how the patient is responding. This will
also help in determining the treatment protocols, and also provide critical information
regarding the patient’s health that will eventually help in formation of life-saving strategies
(Mok, Wang & Liaw, 2015).
Psychological assessment – Since Joe had his bowel opened, it is important to assess the
psychological impact he was going through. The psychological assessment will help in
understanding the level of stress or trauma Joe was going through and whether there was an
impact on his mental health due to his surrounding and also his psychosocial assessment had
to be done (Maruish, 2017).
Clinical reasoning cycle separately attached
nursing staffs to form effective pain management interventions (Zaccagnino & Nedeljkovic,
2017).
Examining the vital signs – This include the respiration rate, heart rate, temperature, SpO2
concentration. This will help in the understanding of how the patient is responding. This will
also help in determining the treatment protocols, and also provide critical information
regarding the patient’s health that will eventually help in formation of life-saving strategies
(Mok, Wang & Liaw, 2015).
Psychological assessment – Since Joe had his bowel opened, it is important to assess the
psychological impact he was going through. The psychological assessment will help in
understanding the level of stress or trauma Joe was going through and whether there was an
impact on his mental health due to his surrounding and also his psychosocial assessment had
to be done (Maruish, 2017).
Clinical reasoning cycle separately attached
NRSG355 2018 |
Q4: Time management and delegation (module four)
The nurse unit manager (NUM) is responsible for the distribution of patients to
nursing staff in order to deliver proper level of treatment to each patient. When one nurse is
assigned to a group of patient’s for the provision of complete care, then this method is called
total patient care. This approach is very important because it offers nurses with high quality,
accuracy and degree of patient autonomy, but mainly it needs all nursing employees to be
registered nurses (Wong et a., 2015).
As the registered nurse shifts to a crowded surgical ward on the afternoon, the
distribution, assignment and finishing of the work will evaluate the capacity of the nursing
team and the input of the nurses. The nursing members who are still active during their
working hours should identify the patient population and try to take benefit of the accessible
staff members by allotting to a group of patients (Hepp et al., 2015).
At first the allotment of staff to patients should be distributed reasonably and
uniformly between the 2 RN’s and EN members who are on duty. As per a research one nurse
should be allocated to a group of 8 patients (King, Long & Lisy, 2015). It would be
appropriate to divide the 14 patients returning from surgery and the 8 going for the surgical
procedure so that one nurse is not assigned to the 8 patients who returned from the surgery at
once (King, Long & Lisy, 2015). This can elevate the chances of human error while
managing the patients, as without prior knowledge post-management of patients will become
difficult. Thus, the patients should be uniformly split to reduce the workload for the nurses.
When members with a poor abilities mix during a scenario, allocating patients to different
staff becomes a safe and reasonable method. Thus, the AIN can help by providing treatment
to the patients who are under the responsibility of RN and EN within the extent of his/ her
practice and under the local guidelines. When the RN implements the decision-making
Q4: Time management and delegation (module four)
The nurse unit manager (NUM) is responsible for the distribution of patients to
nursing staff in order to deliver proper level of treatment to each patient. When one nurse is
assigned to a group of patient’s for the provision of complete care, then this method is called
total patient care. This approach is very important because it offers nurses with high quality,
accuracy and degree of patient autonomy, but mainly it needs all nursing employees to be
registered nurses (Wong et a., 2015).
As the registered nurse shifts to a crowded surgical ward on the afternoon, the
distribution, assignment and finishing of the work will evaluate the capacity of the nursing
team and the input of the nurses. The nursing members who are still active during their
working hours should identify the patient population and try to take benefit of the accessible
staff members by allotting to a group of patients (Hepp et al., 2015).
At first the allotment of staff to patients should be distributed reasonably and
uniformly between the 2 RN’s and EN members who are on duty. As per a research one nurse
should be allocated to a group of 8 patients (King, Long & Lisy, 2015). It would be
appropriate to divide the 14 patients returning from surgery and the 8 going for the surgical
procedure so that one nurse is not assigned to the 8 patients who returned from the surgery at
once (King, Long & Lisy, 2015). This can elevate the chances of human error while
managing the patients, as without prior knowledge post-management of patients will become
difficult. Thus, the patients should be uniformly split to reduce the workload for the nurses.
When members with a poor abilities mix during a scenario, allocating patients to different
staff becomes a safe and reasonable method. Thus, the AIN can help by providing treatment
to the patients who are under the responsibility of RN and EN within the extent of his/ her
practice and under the local guidelines. When the RN implements the decision-making
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NRSG355 2018 |
procedure, that time the RN can help the patients in providing them with food, assist in daily
activities, promote their flexibility, and guide them to washroom.
The AIN's ability to fulfill these duties will allow the RN's sufficient duration to
undertake intravenous antibiotics, pain relief, and medicines in a secure and efficient way,
ensuring that the practices are maintained according to the NSQHS Standard medication
safety (Ritchie et al., 2018). This will also give RN the sufficient amount of time to take
notes, make care strategies and create discharge details important for the patients in the ward.
The Registered Nurses take care of all the treatment procedures of the patients in the ward.
The Registered Nurse should undertake the task assignment with regard to the AIN
capabilities and the intricacies of the patient's treatment. This will lead in a secure,
appropriate and practical amount of treatment given to patients (Medication Safety Standard.
2019).
The model of care is very important when describing the nursing work environment.
There are evidence-based researches which show that nursing settings and job satisfaction are
affected by structure of the organization, leadership qualities, autonomy, models of care and
professional relations (King, Long & Lisy, 2015). This module comprised of the total patient
care model. This model comprises of one nurse who is assigned to a group of patient, though,
the patients are not continuously cared for from admission to release of the patients as they
are assigned on a shift-by-shift basis. Generally, while caring for a patient, it is done with the
help of both the RN and EN. This model of care is very beneficial as it helps in reducing the
workplace stress and burnout of the patients (King, Long & Lisy, 2015).
procedure, that time the RN can help the patients in providing them with food, assist in daily
activities, promote their flexibility, and guide them to washroom.
The AIN's ability to fulfill these duties will allow the RN's sufficient duration to
undertake intravenous antibiotics, pain relief, and medicines in a secure and efficient way,
ensuring that the practices are maintained according to the NSQHS Standard medication
safety (Ritchie et al., 2018). This will also give RN the sufficient amount of time to take
notes, make care strategies and create discharge details important for the patients in the ward.
The Registered Nurses take care of all the treatment procedures of the patients in the ward.
The Registered Nurse should undertake the task assignment with regard to the AIN
capabilities and the intricacies of the patient's treatment. This will lead in a secure,
appropriate and practical amount of treatment given to patients (Medication Safety Standard.
2019).
The model of care is very important when describing the nursing work environment.
There are evidence-based researches which show that nursing settings and job satisfaction are
affected by structure of the organization, leadership qualities, autonomy, models of care and
professional relations (King, Long & Lisy, 2015). This module comprised of the total patient
care model. This model comprises of one nurse who is assigned to a group of patient, though,
the patients are not continuously cared for from admission to release of the patients as they
are assigned on a shift-by-shift basis. Generally, while caring for a patient, it is done with the
help of both the RN and EN. This model of care is very beneficial as it helps in reducing the
workplace stress and burnout of the patients (King, Long & Lisy, 2015).
NRSG355 2018 |
REFERENCE
Bridges, J., Griffiths, P., Oliver, E., & Pickering, R. M. (2019). Hospital nurse staffing and
staff–patient interactions: an observational study. BMJ Qual Saf, bmjqs-2018.
Deeken, D. J., Wakefield, D., Kite, C., Linebaugh, J., Mitchell, B., Parkinson, D., & Misra,
M. (2017). Development, Validation, and Implementation of a Clinic Nurse Staffing
Guideline. Journal of Nursing Administration, 47(10), 515-521.
Dempsey, C., & Reilly, B. (2016). Nurse engagement: What are the contributing factors for
success. OJIN: The Online Journal of Issues in Nursing, 21(1).
Greysen, H. M., & Greysen, S. R. (2017). Mobility assessment in the hospital-what are “next
steps”?. Journal of hospital medicine, 12(6), 477.
Hepp, S. L., Suter, E., Jackson, K., Deutschlander, S., Makwarimba, E., Jennings, J., &
Birmingham, L. (2015). Using an interprofessional competency framework to
examine collaborative practice. Journal of interprofessional care, 29(2), 131-137.
Housley, W. (2017). Interaction in multidisciplinary teams. Routledge.
Johnson, C., & Viljoen, N. (2017). Experiences of two multidisciplinary team members of
systemic consultations in a community learning disability service. British Journal of
Learning Disabilities, 45(3), 172-179.
Karazivan, P., Dumez, V., Flora, L., Pomey, M. P., Del Grande, C., Ghadiri, D. P., ... &
Lebel, P. (2015). The patient-as-partner approach in health care: a conceptual
framework for a necessary transition. Academic Medicine, 90(4), 437-441.
Kennedy, M. (2016). The Importance of a Role-Specific, In-Hospital Ward Clerk Education
Program. Hospital topics, 94(3-4), 43-48.
REFERENCE
Bridges, J., Griffiths, P., Oliver, E., & Pickering, R. M. (2019). Hospital nurse staffing and
staff–patient interactions: an observational study. BMJ Qual Saf, bmjqs-2018.
Deeken, D. J., Wakefield, D., Kite, C., Linebaugh, J., Mitchell, B., Parkinson, D., & Misra,
M. (2017). Development, Validation, and Implementation of a Clinic Nurse Staffing
Guideline. Journal of Nursing Administration, 47(10), 515-521.
Dempsey, C., & Reilly, B. (2016). Nurse engagement: What are the contributing factors for
success. OJIN: The Online Journal of Issues in Nursing, 21(1).
Greysen, H. M., & Greysen, S. R. (2017). Mobility assessment in the hospital-what are “next
steps”?. Journal of hospital medicine, 12(6), 477.
Hepp, S. L., Suter, E., Jackson, K., Deutschlander, S., Makwarimba, E., Jennings, J., &
Birmingham, L. (2015). Using an interprofessional competency framework to
examine collaborative practice. Journal of interprofessional care, 29(2), 131-137.
Housley, W. (2017). Interaction in multidisciplinary teams. Routledge.
Johnson, C., & Viljoen, N. (2017). Experiences of two multidisciplinary team members of
systemic consultations in a community learning disability service. British Journal of
Learning Disabilities, 45(3), 172-179.
Karazivan, P., Dumez, V., Flora, L., Pomey, M. P., Del Grande, C., Ghadiri, D. P., ... &
Lebel, P. (2015). The patient-as-partner approach in health care: a conceptual
framework for a necessary transition. Academic Medicine, 90(4), 437-441.
Kennedy, M. (2016). The Importance of a Role-Specific, In-Hospital Ward Clerk Education
Program. Hospital topics, 94(3-4), 43-48.
NRSG355 2018 |
King, A., Long, L., & Lisy, K. (2015). Effectiveness of team nursing compared with total
patient care on staff wellbeing when organizing nursing work in acute care wards: a
systematic review. JBI database of systematic reviews and implementation reports,
13(11), 128-168.
Kwee, R. M., & Kwee, T. C. (2019). Whole‐Body MRI for Preventive Health Screening: A
Systematic Review of the Literature. Journal of Magnetic Resonance Imaging.
Maruish, M. E. (Ed.). (2017). Handbook of psychological assessment in primary care
settings. Taylor & Francis.
Mascolo, M., Dee, E., Townsend, R., Brinton, J. T., & Mehler, P. S. (2015). Severe gastric
dilatation due to superior mesenteric artery syndrome in anorexia nervosa.
International Journal of Eating Disorders, 48(5), 532-534.
Medication Safety Standard. (2019). Retrieved 23 September 2019, from
https://www.safetyandquality.gov.au/standards/nsqhs-standards/medication-safety-
standard
Mitchell, R., Boyle, B., Parker, V., Giles, M., Chiang, V., & Joyce, P. (2015). Managing
inclusiveness and diversity in teams: How leader inclusiveness affects performance
through status and team identity. Human Resource Management, 54(2), 217-239.
MND. (2019). Multidisciplinary care team. Retrieved 22 October 2019, from
https://www.mndaust.asn.au/Get-informed/Information-resources/Living_better_for_l
onger/WEB-MND-Australia-Fact-Sheet-EB3-Multidisciplinary.aspx
King, A., Long, L., & Lisy, K. (2015). Effectiveness of team nursing compared with total
patient care on staff wellbeing when organizing nursing work in acute care wards: a
systematic review. JBI database of systematic reviews and implementation reports,
13(11), 128-168.
Kwee, R. M., & Kwee, T. C. (2019). Whole‐Body MRI for Preventive Health Screening: A
Systematic Review of the Literature. Journal of Magnetic Resonance Imaging.
Maruish, M. E. (Ed.). (2017). Handbook of psychological assessment in primary care
settings. Taylor & Francis.
Mascolo, M., Dee, E., Townsend, R., Brinton, J. T., & Mehler, P. S. (2015). Severe gastric
dilatation due to superior mesenteric artery syndrome in anorexia nervosa.
International Journal of Eating Disorders, 48(5), 532-534.
Medication Safety Standard. (2019). Retrieved 23 September 2019, from
https://www.safetyandquality.gov.au/standards/nsqhs-standards/medication-safety-
standard
Mitchell, R., Boyle, B., Parker, V., Giles, M., Chiang, V., & Joyce, P. (2015). Managing
inclusiveness and diversity in teams: How leader inclusiveness affects performance
through status and team identity. Human Resource Management, 54(2), 217-239.
MND. (2019). Multidisciplinary care team. Retrieved 22 October 2019, from
https://www.mndaust.asn.au/Get-informed/Information-resources/Living_better_for_l
onger/WEB-MND-Australia-Fact-Sheet-EB3-Multidisciplinary.aspx
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

NRSG355 2018 |
Mok, W. Q., Wang, W., & Liaw, S. Y. (2015). Vital signs monitoring to detect patient
deterioration: An integrative literature review. International Journal of Nursing
Practice, 21, 91-98.
NMBA. (2016). Enrolled nurse standards for practice. Retrieved 22 October 2019, from
https://www.nursingmidwiferyboard.gov.au/documents/default.aspx?
record=WD15%2F18365&dbid=AP&chksum=rUxPmFs%2BqDdDw6oZ%2FFAikw
%3D%3D
Reeves, S., Pelone, F., Harrison, R., Goldman, J., & Zwarenstein, M. (2017).
Interprofessional collaboration to improve professional practice and healthcare
outcomes. Cochrane Database of Systematic Reviews, (6).
Ritchie, A., Gaca, M., Siemensma, G., Taylor, J., & Gilbert, C. (2018). Australian health
libraries’ contributions to hospital accreditation and the National Safety and Quality
Health Services (NSQHS) Standards: results of the Health Libraries for National
Standards (HeLiNS) research project.
Scales, K., & Pilsworth, J. (2008). The importance of fluid balance in clinical practice.
Nursing Standard (through 2013), 22(47), 50.
Schottenfeld, L., Petersen, D., Peikes, D., Ricciardi, R., Burak, H., McNellis, R., & Genevro,
J. (2016). Creating patient-centered team-based primary care. Rockville: Agency for
Healthcare Research and Quality.
Smolowitz, J., Speakman, E., Wojnar, D., Whelan, E. M., Ulrich, S., Hayes, C., & Wood, L.
(2015). Role of the registered nurse in primary health care: meeting health care needs
in the 21st century. Nursing Outlook, 63(2), 130-136.
Mok, W. Q., Wang, W., & Liaw, S. Y. (2015). Vital signs monitoring to detect patient
deterioration: An integrative literature review. International Journal of Nursing
Practice, 21, 91-98.
NMBA. (2016). Enrolled nurse standards for practice. Retrieved 22 October 2019, from
https://www.nursingmidwiferyboard.gov.au/documents/default.aspx?
record=WD15%2F18365&dbid=AP&chksum=rUxPmFs%2BqDdDw6oZ%2FFAikw
%3D%3D
Reeves, S., Pelone, F., Harrison, R., Goldman, J., & Zwarenstein, M. (2017).
Interprofessional collaboration to improve professional practice and healthcare
outcomes. Cochrane Database of Systematic Reviews, (6).
Ritchie, A., Gaca, M., Siemensma, G., Taylor, J., & Gilbert, C. (2018). Australian health
libraries’ contributions to hospital accreditation and the National Safety and Quality
Health Services (NSQHS) Standards: results of the Health Libraries for National
Standards (HeLiNS) research project.
Scales, K., & Pilsworth, J. (2008). The importance of fluid balance in clinical practice.
Nursing Standard (through 2013), 22(47), 50.
Schottenfeld, L., Petersen, D., Peikes, D., Ricciardi, R., Burak, H., McNellis, R., & Genevro,
J. (2016). Creating patient-centered team-based primary care. Rockville: Agency for
Healthcare Research and Quality.
Smolowitz, J., Speakman, E., Wojnar, D., Whelan, E. M., Ulrich, S., Hayes, C., & Wood, L.
(2015). Role of the registered nurse in primary health care: meeting health care needs
in the 21st century. Nursing Outlook, 63(2), 130-136.
NRSG355 2018 |
Twigg, D. E., Myers, H., Duffield, C., Pugh, J. D., Gelder, L., & Roche, M. (2016). The
impact of adding assistants in nursing to acute care hospital ward nurse staffing on
adverse patient outcomes: An analysis of administrative health data. International
journal of nursing studies, 63, 189-200.
Wong, C. A., Elliott‐Miller, P., Laschinger, H., Cuddihy, M., Meyer, R. M., Keatings, M., ...
& Szudy, N. (2015). Examining the relationships between span of control and
manager job and unit performance outcomes. Journal of nursing management, 23(2),
156-168.
Zaccagnino, M. P., & Nedeljkovic, S. S. (2017). Pain assessment tools. In Pain Medicine (pp.
77-81). Springer, Cham.
Twigg, D. E., Myers, H., Duffield, C., Pugh, J. D., Gelder, L., & Roche, M. (2016). The
impact of adding assistants in nursing to acute care hospital ward nurse staffing on
adverse patient outcomes: An analysis of administrative health data. International
journal of nursing studies, 63, 189-200.
Wong, C. A., Elliott‐Miller, P., Laschinger, H., Cuddihy, M., Meyer, R. M., Keatings, M., ...
& Szudy, N. (2015). Examining the relationships between span of control and
manager job and unit performance outcomes. Journal of nursing management, 23(2),
156-168.
Zaccagnino, M. P., & Nedeljkovic, S. S. (2017). Pain assessment tools. In Pain Medicine (pp.
77-81). Springer, Cham.
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





