NURBN2016 Assignment: Case Study on Chronic Renal Failure
VerifiedAdded on 2022/09/16
|12
|3079
|17
Report
AI Summary
This nursing assignment analyzes a case study of a 55-year-old patient diagnosed with chronic renal failure. The report begins with a review of the human excretory system and renal physiology, including the functions of the kidneys and nephrons. It then delves into the pathophysiology of chronic kidney failure (CKF), its causes, risk factors, and complications, including hypertension, anemia, and electrolyte imbalances. The case study details the patient's medical history, symptoms, and blood test results, including a low GFR. The report also covers the differences between acute and chronic kidney disease and provides a detailed explanation of hemodialysis, including the types of access and nursing considerations. The assignment further examines the patient's medications, valsartan and injection Eprex, discussing their mechanisms of action, side effects, and nursing implications. It also explains GFR calculations and the significance of hemoglobin tests. Finally, the report emphasizes the importance of the teach-back method for patient education, particularly regarding fluid intake management and the consequences of non-compliance.

Running head: NURSING ASSIGNMENT
NURSING ASSIGNMENT
Name of the Student
Name of the university
Author note
NURSING ASSIGNMENT
Name of the Student
Name of the university
Author note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1NURSING ASSIGNMENT
Table of Contents
Part 1................................................................................................................................................2
Part 2................................................................................................................................................6
Part 3................................................................................................................................................8
References........................................................................................................................................9
Table of Contents
Part 1................................................................................................................................................2
Part 2................................................................................................................................................6
Part 3................................................................................................................................................8
References........................................................................................................................................9
2NURSING ASSIGNMENT
Part 1
1.1. The human excretory system is comprised of two kidneys, two ureters, one urethra and one
bladder. The kidney is the primary organ of the renal system. The internal region of kidney has
three regions renal cortex, renal medulla and pelvis. The outermost region of kidney is the cortex
and the innermost region is the medulla. The function of the renal pelvis is to connect the kidney
to the circulatory system. The nephron, the basic unit of kidney, filters the blood to regulate the
concentrations of chemicals and also it is responsible for the production of urine (Ramanathan et
al., 2016).
The renal physiology means study of the kidney physiology including its functions. The
function of kidney involves regulating the concentration of potassium, sodium and other
electrolytes. The other important functions of kidney are clearing of toxins, absorption of
glucose, amino acids and other small molecules, regulation of the blood pressure, making of
different hormones and also in the activation of vitamin D. The renal physiology are studied on
the nephron level (Sharma, Ramesh & Gupta, 2015).
1.2. The chronic failure of kidney, also known as the finale stage renal disease is the irreversible
and rapid decrease in the functions of kidneys. During this condition, the capacity of the human
body in maintaining the metabolic activity and the balance of fluids and electrolyte fails which
result in the development of uraemia. The disease uraemia is the increment in the concentration
of urea and nitrogenous wastes in the blood. Uraemia occurs as the result of systematic effect of
several diseases like type II diabetes, hypertension, obstruction in the urinary tract, from
medications or different infections. Uraemia also occurs because of the living environment of a
person and the occupations of patient. The patient of this case study was not suffering from
Part 1
1.1. The human excretory system is comprised of two kidneys, two ureters, one urethra and one
bladder. The kidney is the primary organ of the renal system. The internal region of kidney has
three regions renal cortex, renal medulla and pelvis. The outermost region of kidney is the cortex
and the innermost region is the medulla. The function of the renal pelvis is to connect the kidney
to the circulatory system. The nephron, the basic unit of kidney, filters the blood to regulate the
concentrations of chemicals and also it is responsible for the production of urine (Ramanathan et
al., 2016).
The renal physiology means study of the kidney physiology including its functions. The
function of kidney involves regulating the concentration of potassium, sodium and other
electrolytes. The other important functions of kidney are clearing of toxins, absorption of
glucose, amino acids and other small molecules, regulation of the blood pressure, making of
different hormones and also in the activation of vitamin D. The renal physiology are studied on
the nephron level (Sharma, Ramesh & Gupta, 2015).
1.2. The chronic failure of kidney, also known as the finale stage renal disease is the irreversible
and rapid decrease in the functions of kidneys. During this condition, the capacity of the human
body in maintaining the metabolic activity and the balance of fluids and electrolyte fails which
result in the development of uraemia. The disease uraemia is the increment in the concentration
of urea and nitrogenous wastes in the blood. Uraemia occurs as the result of systematic effect of
several diseases like type II diabetes, hypertension, obstruction in the urinary tract, from
medications or different infections. Uraemia also occurs because of the living environment of a
person and the occupations of patient. The patient of this case study was not suffering from
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3NURSING ASSIGNMENT
hypertension but the medical history of the patient showed that he had been suffering from
severe headaches, palpitations since the last five years as she used to worry about the drought. At
the time of admission in the hospital, the patient showed an increased level of blood pressure
(190/110 mm Hg). The pathophysiology behind this is, as the functions of the renal organs
decreases, the end products of the metabolism (proteins) gets accumulated in the body which are
normally excreted out from the body through urine. Uraemia develops and because of this the
other body systems are also affected. The severity of the symptoms are dependent on the
concentration of the accumulated waste products (Levey, Inker & Coresh, 2015). The conditions
become more severe when the amount of protein increases and also if the hypertension get
increased. In the given case study, the blood report showed that the amount of creatinine is very
high. The patient also showed an increased level of hypertension.
There are several risk factors associated with chronic kidney failure. The genetics of any
person is another important risk factor of the disease and it is very essential to find whether any
the family members had suffered from kidney diseases or not. Another important risk factor is
the age as people who have crossed 45 years of age have tendencies to suffer from failures of
kidney. The next important risk factor is the type II diabetes, especially if the onset of the disease
happens within 20 years of age. During the later stages of their life, the disease may get
transformed into severe form. Increased blood pressure is another important risk factor, the
condition worsen at the later stages of their life if the blood pressure is uncontrollable for a long
period of time. Poor control of blood glucose, smoking and obesity are the other reasons of
kidney failure. The patient is 55 years of age, showed symptoms of palpitation and the blood
pressure was also very high (Tsai et al., 2016).
hypertension but the medical history of the patient showed that he had been suffering from
severe headaches, palpitations since the last five years as she used to worry about the drought. At
the time of admission in the hospital, the patient showed an increased level of blood pressure
(190/110 mm Hg). The pathophysiology behind this is, as the functions of the renal organs
decreases, the end products of the metabolism (proteins) gets accumulated in the body which are
normally excreted out from the body through urine. Uraemia develops and because of this the
other body systems are also affected. The severity of the symptoms are dependent on the
concentration of the accumulated waste products (Levey, Inker & Coresh, 2015). The conditions
become more severe when the amount of protein increases and also if the hypertension get
increased. In the given case study, the blood report showed that the amount of creatinine is very
high. The patient also showed an increased level of hypertension.
There are several risk factors associated with chronic kidney failure. The genetics of any
person is another important risk factor of the disease and it is very essential to find whether any
the family members had suffered from kidney diseases or not. Another important risk factor is
the age as people who have crossed 45 years of age have tendencies to suffer from failures of
kidney. The next important risk factor is the type II diabetes, especially if the onset of the disease
happens within 20 years of age. During the later stages of their life, the disease may get
transformed into severe form. Increased blood pressure is another important risk factor, the
condition worsen at the later stages of their life if the blood pressure is uncontrollable for a long
period of time. Poor control of blood glucose, smoking and obesity are the other reasons of
kidney failure. The patient is 55 years of age, showed symptoms of palpitation and the blood
pressure was also very high (Tsai et al., 2016).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4NURSING ASSIGNMENT
The complications of the disease are anaemia, increased potassium levels, bone diseases,
development of heart diseases and fluid increase. The kidney help in creating the blood cells, so
if the kidney fails anaemia will happen. When the kidneys are not working properly, the other
organs may also be affected. The consumption of potassium needs to be reduced as the kidney is
not able to filter extra potassium. The healthy fluids can filter and remove the extra fluids from
the body but when the kidneys are not working properly, it will not be able to excrete the extra
fluids from the body (Shang et al., 2016).
There are only two types of treatment options of kidney failures which are haemodialysis
or peritoneal dialysis. Apart from this the other option left is kidney transplantation. In the
present case scenario, the patient had undergone haemodialysis.
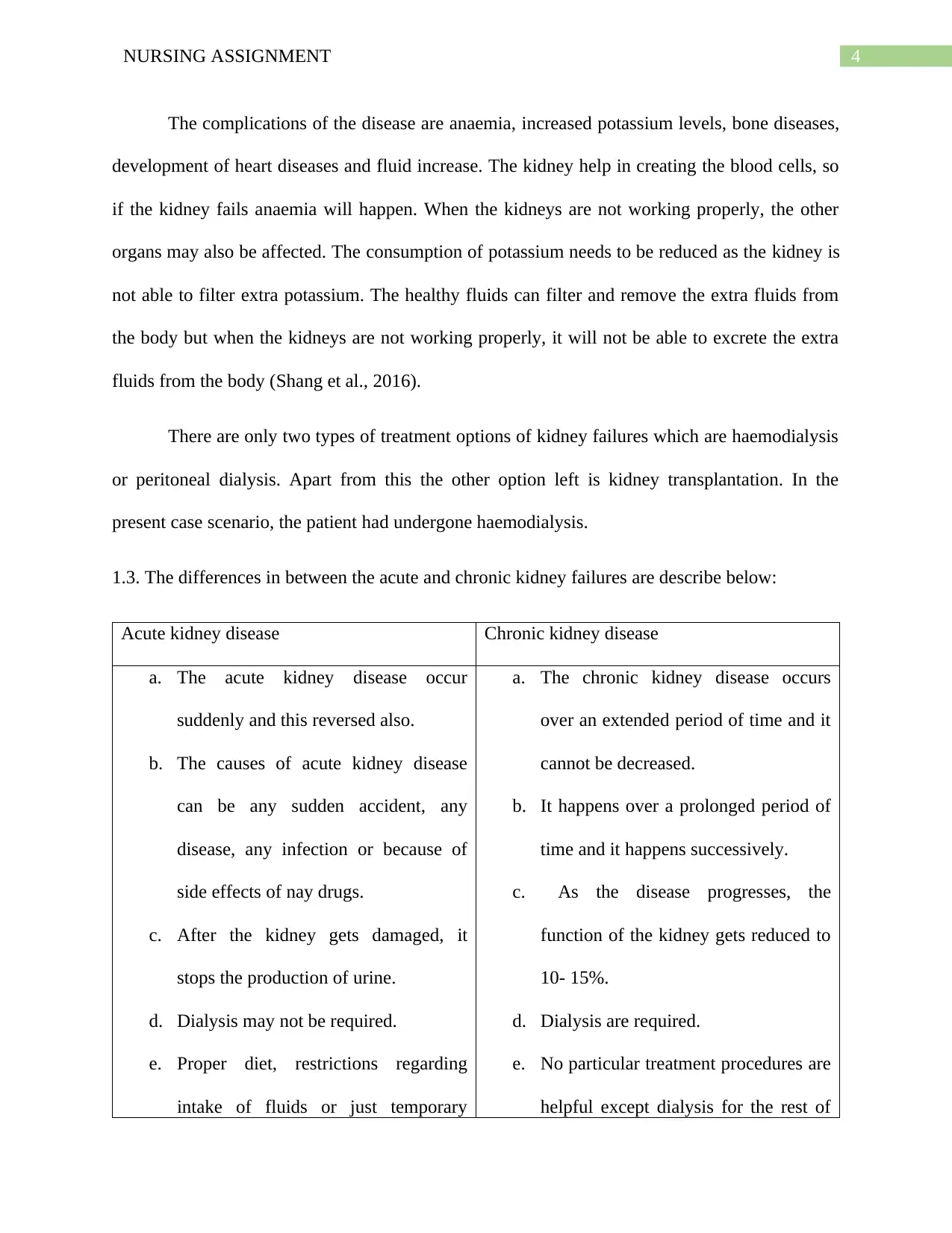
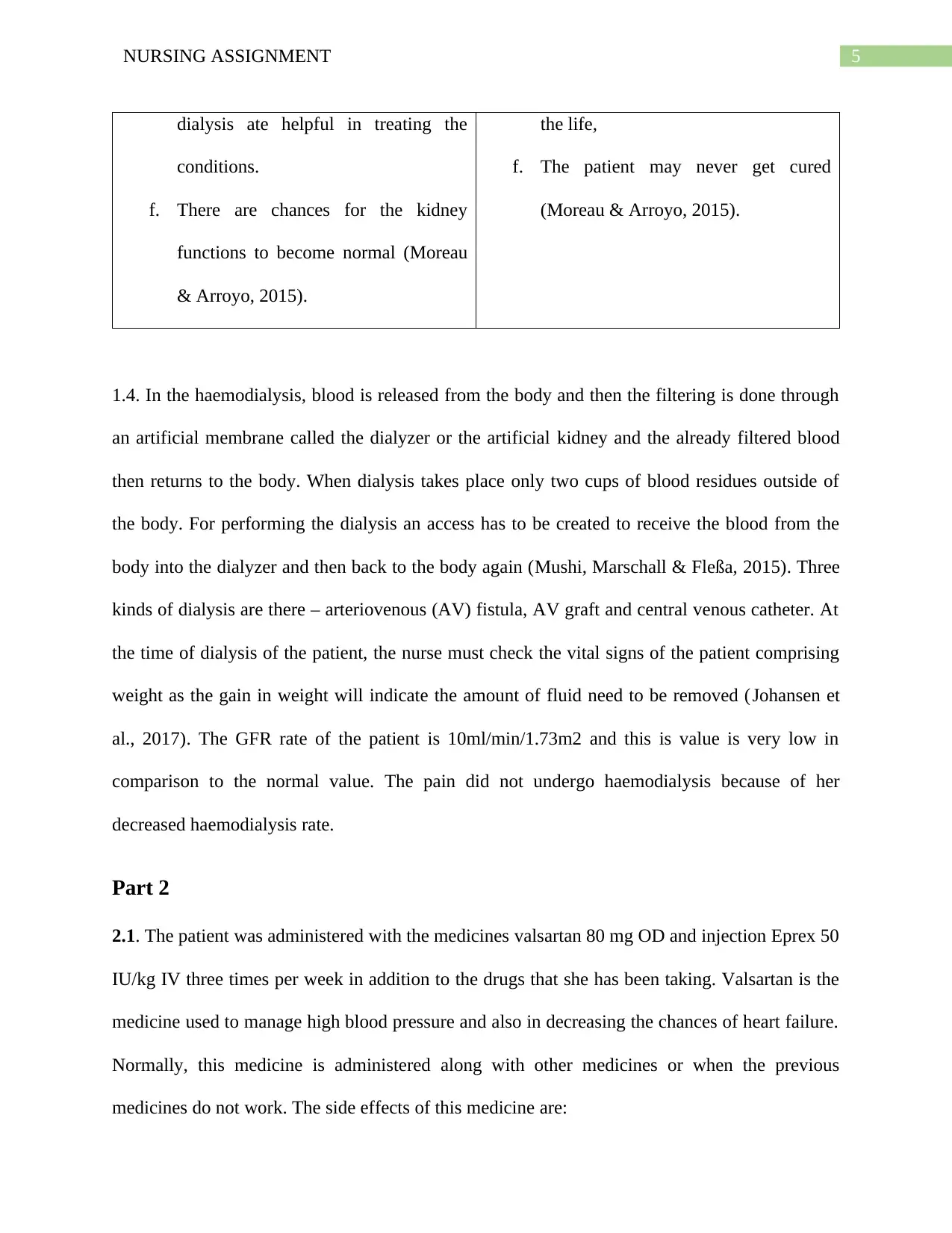
1.3. The differences in between the acute and chronic kidney failures are describe below:
Acute kidney disease Chronic kidney disease
a. The acute kidney disease occur
suddenly and this reversed also.
b. The causes of acute kidney disease
can be any sudden accident, any
disease, any infection or because of
side effects of nay drugs.
c. After the kidney gets damaged, it
stops the production of urine.
d. Dialysis may not be required.
e. Proper diet, restrictions regarding
intake of fluids or just temporary
a. The chronic kidney disease occurs
over an extended period of time and it
cannot be decreased.
b. It happens over a prolonged period of
time and it happens successively.
c. As the disease progresses, the
function of the kidney gets reduced to
10- 15%.
d. Dialysis are required.
e. No particular treatment procedures are
helpful except dialysis for the rest of
The complications of the disease are anaemia, increased potassium levels, bone diseases,
development of heart diseases and fluid increase. The kidney help in creating the blood cells, so
if the kidney fails anaemia will happen. When the kidneys are not working properly, the other
organs may also be affected. The consumption of potassium needs to be reduced as the kidney is
not able to filter extra potassium. The healthy fluids can filter and remove the extra fluids from
the body but when the kidneys are not working properly, it will not be able to excrete the extra
fluids from the body (Shang et al., 2016).
There are only two types of treatment options of kidney failures which are haemodialysis
or peritoneal dialysis. Apart from this the other option left is kidney transplantation. In the
present case scenario, the patient had undergone haemodialysis.
1.3. The differences in between the acute and chronic kidney failures are describe below:
Acute kidney disease Chronic kidney disease
a. The acute kidney disease occur
suddenly and this reversed also.
b. The causes of acute kidney disease
can be any sudden accident, any
disease, any infection or because of
side effects of nay drugs.
c. After the kidney gets damaged, it
stops the production of urine.
d. Dialysis may not be required.
e. Proper diet, restrictions regarding
intake of fluids or just temporary
a. The chronic kidney disease occurs
over an extended period of time and it
cannot be decreased.
b. It happens over a prolonged period of
time and it happens successively.
c. As the disease progresses, the
function of the kidney gets reduced to
10- 15%.
d. Dialysis are required.
e. No particular treatment procedures are
helpful except dialysis for the rest of
5NURSING ASSIGNMENT
dialysis ate helpful in treating the
conditions.
f. There are chances for the kidney
functions to become normal (Moreau
& Arroyo, 2015).
the life,
f. The patient may never get cured
(Moreau & Arroyo, 2015).
1.4. In the haemodialysis, blood is released from the body and then the filtering is done through
an artificial membrane called the dialyzer or the artificial kidney and the already filtered blood
then returns to the body. When dialysis takes place only two cups of blood residues outside of
the body. For performing the dialysis an access has to be created to receive the blood from the
body into the dialyzer and then back to the body again (Mushi, Marschall & Fleßa, 2015). Three
kinds of dialysis are there – arteriovenous (AV) fistula, AV graft and central venous catheter. At
the time of dialysis of the patient, the nurse must check the vital signs of the patient comprising
weight as the gain in weight will indicate the amount of fluid need to be removed (Johansen et
al., 2017). The GFR rate of the patient is 10ml/min/1.73m2 and this is value is very low in
comparison to the normal value. The pain did not undergo haemodialysis because of her
decreased haemodialysis rate.
Part 2
2.1. The patient was administered with the medicines valsartan 80 mg OD and injection Eprex 50
IU/kg IV three times per week in addition to the drugs that she has been taking. Valsartan is the
medicine used to manage high blood pressure and also in decreasing the chances of heart failure.
Normally, this medicine is administered along with other medicines or when the previous
medicines do not work. The side effects of this medicine are:
dialysis ate helpful in treating the
conditions.
f. There are chances for the kidney
functions to become normal (Moreau
& Arroyo, 2015).
the life,
f. The patient may never get cured
(Moreau & Arroyo, 2015).
1.4. In the haemodialysis, blood is released from the body and then the filtering is done through
an artificial membrane called the dialyzer or the artificial kidney and the already filtered blood
then returns to the body. When dialysis takes place only two cups of blood residues outside of
the body. For performing the dialysis an access has to be created to receive the blood from the
body into the dialyzer and then back to the body again (Mushi, Marschall & Fleßa, 2015). Three
kinds of dialysis are there – arteriovenous (AV) fistula, AV graft and central venous catheter. At
the time of dialysis of the patient, the nurse must check the vital signs of the patient comprising
weight as the gain in weight will indicate the amount of fluid need to be removed (Johansen et
al., 2017). The GFR rate of the patient is 10ml/min/1.73m2 and this is value is very low in
comparison to the normal value. The pain did not undergo haemodialysis because of her
decreased haemodialysis rate.
Part 2
2.1. The patient was administered with the medicines valsartan 80 mg OD and injection Eprex 50
IU/kg IV three times per week in addition to the drugs that she has been taking. Valsartan is the
medicine used to manage high blood pressure and also in decreasing the chances of heart failure.
Normally, this medicine is administered along with other medicines or when the previous
medicines do not work. The side effects of this medicine are:
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6NURSING ASSIGNMENT
Common side effects – The common side effects of Valsartan are feeling dizzy or feeling
of spinning. Severe headaches and sudden feeling of sickness are other side effects. The
patient may also suffer from diarrhoea or vomiting or excess pain in the joints (Jhund &
McMurray, 2016).
Serious side effects- Sudden yellowing of the skin or yellowing of the eyes have may also
happen. These are the signs of extreme problems of liver. The other serious side effects
includes paling of skin, frequently feeling tired, appearance of purple colour spots, any
kind of bleeding, sore throat or sudden fever. The other side effects also includes,
irregular heartbeat and muscle cramp (McCormack, 2016).
The patient was also administered ibuprofen, so before administering the medicines the nurse
must consider the mechanism and side effects of other medicines. The nurses should administer
medicines to the patient after considering the age. The third consideration is that the nurse should
apply the dose after analysing the blood pressure of the patient. The patient was already suffering
from headaches, so the nurse should notice that the headache of the patient does not get
increased.
The patient was also administered with injection Eprex 50 IU/kg IV to treat the anaemia
associated with chronic kidney failure. The patient was administered with this medicine as she
was unable to produce sufficient erythropoietin. The side effects of this medicine are described
below:
Common side effects – The common lateral effects includes feeling of weakness and
tiredness. The side effects also includes pain, redness, stinging and swelling beside the
areas of infection (Guarienti et al., 2015).
Common side effects – The common side effects of Valsartan are feeling dizzy or feeling
of spinning. Severe headaches and sudden feeling of sickness are other side effects. The
patient may also suffer from diarrhoea or vomiting or excess pain in the joints (Jhund &
McMurray, 2016).
Serious side effects- Sudden yellowing of the skin or yellowing of the eyes have may also
happen. These are the signs of extreme problems of liver. The other serious side effects
includes paling of skin, frequently feeling tired, appearance of purple colour spots, any
kind of bleeding, sore throat or sudden fever. The other side effects also includes,
irregular heartbeat and muscle cramp (McCormack, 2016).
The patient was also administered ibuprofen, so before administering the medicines the nurse
must consider the mechanism and side effects of other medicines. The nurses should administer
medicines to the patient after considering the age. The third consideration is that the nurse should
apply the dose after analysing the blood pressure of the patient. The patient was already suffering
from headaches, so the nurse should notice that the headache of the patient does not get
increased.
The patient was also administered with injection Eprex 50 IU/kg IV to treat the anaemia
associated with chronic kidney failure. The patient was administered with this medicine as she
was unable to produce sufficient erythropoietin. The side effects of this medicine are described
below:
Common side effects – The common lateral effects includes feeling of weakness and
tiredness. The side effects also includes pain, redness, stinging and swelling beside the
areas of infection (Guarienti et al., 2015).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7NURSING ASSIGNMENT
Serious side effects- The severe side effects involves clotting of the vascular access site
because of dialysis. The other side effects involves diarrhoea, oedema of face, fingers,
lower legs and feet. The patient of the given case study might suffer from all these
symptoms. A patient should immediately consul with the doctor if allergy, chest pain or
stroke happens (Oh, Yoon & Cho, 2015).
The most important aspect of consideration in the given case is the vital signs, so the
nurses must consider the vital signs before the administration of the injection. Secondly the
nurse must consider the condition of heart as she was suffering from hypertension. Thirdly,
the nurse must also consider the issue of high blood pressure of the patient. Lastly, the nurse
should carefully analyse the actions and side effects of the other medicines before
administering the infection.
2.2 The glomerular filtration rate gives the doctor the clear indication about the extent of the
damage of kidney and also it helps in determining the stage of the kidney disease. The
doctors regulate the stage of kidney disease after carefully noticing the changes in GFR over
a specific period of time. The test gives the definition of the sum total of the filtration rates of
all nephrons which functions together (Levey, Becker & Inker, 2015). The formula for
calculating GFR = 140 – (age of the patient). The normal value of GFR is 100 -140 ml/min
(Monseu et al., 2015). The GFR value of the patient of the given case study is 10 ml/min,
which means she was suffering from severe kidney disease.
The haemoglobin test is done for measuring the concentration of dissolved oxygen in the
blood. The test also provides people with information about the overall health conditions of
the patient, for diagnosing a medical condition and to look after a particular medical function.
Before performing the test a person need to eat and drink before the test is being done
Serious side effects- The severe side effects involves clotting of the vascular access site
because of dialysis. The other side effects involves diarrhoea, oedema of face, fingers,
lower legs and feet. The patient of the given case study might suffer from all these
symptoms. A patient should immediately consul with the doctor if allergy, chest pain or
stroke happens (Oh, Yoon & Cho, 2015).
The most important aspect of consideration in the given case is the vital signs, so the
nurses must consider the vital signs before the administration of the injection. Secondly the
nurse must consider the condition of heart as she was suffering from hypertension. Thirdly,
the nurse must also consider the issue of high blood pressure of the patient. Lastly, the nurse
should carefully analyse the actions and side effects of the other medicines before
administering the infection.
2.2 The glomerular filtration rate gives the doctor the clear indication about the extent of the
damage of kidney and also it helps in determining the stage of the kidney disease. The
doctors regulate the stage of kidney disease after carefully noticing the changes in GFR over
a specific period of time. The test gives the definition of the sum total of the filtration rates of
all nephrons which functions together (Levey, Becker & Inker, 2015). The formula for
calculating GFR = 140 – (age of the patient). The normal value of GFR is 100 -140 ml/min
(Monseu et al., 2015). The GFR value of the patient of the given case study is 10 ml/min,
which means she was suffering from severe kidney disease.
The haemoglobin test is done for measuring the concentration of dissolved oxygen in the
blood. The test also provides people with information about the overall health conditions of
the patient, for diagnosing a medical condition and to look after a particular medical function.
Before performing the test a person need to eat and drink before the test is being done
8NURSING ASSIGNMENT
(Ghimire, et al., 2015). The normal value of this test is 12 to 15.5 gm. /dl and the value of the
patient was 95 gm. /L. So the patient was suffering from anaemia.
Part 3
The teach-back method is the communication confirmation method which the healthcare
providers use to confirm whether the patients have understood everything or not that was
explained to them. If the patients have clearly understood every details of their diseases or
test, then the teach back method is successful but if the patient did not understood everything
then the method of teach back is not effective. The nurse must communicate effectively with
the patient in order to make her understand the need for taking care of herself (Dinh et al.,
2016). The patient was suffering from chronic kidney failure, so she must manage the intake
the fluid intake according to the diet. As a nurse I must describe and demonstrate the patient
about all the severe consequences that can happen if the patent is not able to manage the fluid
intake in accordance with her diet. I shall also make her understand about the significance of
several medicines which are administered to her.
(Ghimire, et al., 2015). The normal value of this test is 12 to 15.5 gm. /dl and the value of the
patient was 95 gm. /L. So the patient was suffering from anaemia.
Part 3
The teach-back method is the communication confirmation method which the healthcare
providers use to confirm whether the patients have understood everything or not that was
explained to them. If the patients have clearly understood every details of their diseases or
test, then the teach back method is successful but if the patient did not understood everything
then the method of teach back is not effective. The nurse must communicate effectively with
the patient in order to make her understand the need for taking care of herself (Dinh et al.,
2016). The patient was suffering from chronic kidney failure, so she must manage the intake
the fluid intake according to the diet. As a nurse I must describe and demonstrate the patient
about all the severe consequences that can happen if the patent is not able to manage the fluid
intake in accordance with her diet. I shall also make her understand about the significance of
several medicines which are administered to her.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9NURSING ASSIGNMENT
References
Dinh, T. T. H., Bonner, A., Clark, R., Ramsbotham, J., & Hines, S. (2016). The effectiveness of
the teach-back method on adherence and self-management in health education for people
with chronic disease: a systematic review. JBI database of systematic reviews and
implementation reports, 14(1), 210-247.
Ghimire, S., Castelino, R. L., Lioufas, N. M., Peterson, G. M., & Zaidi, S. T. R. (2015).
Nonadherence to medication therapy in haemodialysis patients: a systematic review. PloS
one, 10(12), e0144119.
Guarienti, M., Giacopuzzi, E., Gianoncelli, A., Sigala, S., Spano, P., Pecorelli, S., ... & Memo,
M. (2015). Computational and functional analysis of biopharmaceutical drugs in
zebrafish: Erythropoietin as a test model. Pharmacological research, 102, 12-21.
Jhund, P. S., & McMurray, J. J. (2016). The neprilysin pathway in heart failure: a review and
guide on the use of sacubitril/valsartan. Heart, 102(17), 1342-1347.
Johansen, K. L., Dalrymple, L. S., Delgado, C., Chertow, G. M., Segal, M. R., Chiang, J., ... &
Kaysen, G. A. (2017). Factors associated with frailty and its trajectory among patients on
hemodialysis. Clinical Journal of the American Society of Nephrology, 12(7), 1100-1108.
Levey, A. S., Becker, C., & Inker, L. A. (2015). Glomerular filtration rate and albuminuria for
detection and staging of acute and chronic kidney disease in adults: a systematic
review. Jama, 313(8), 837-846.
Levey, A. S., Inker, L. A., & Coresh, J. (2015). Chronic kidney disease in older
people. Jama, 314(6), 557-558.
References
Dinh, T. T. H., Bonner, A., Clark, R., Ramsbotham, J., & Hines, S. (2016). The effectiveness of
the teach-back method on adherence and self-management in health education for people
with chronic disease: a systematic review. JBI database of systematic reviews and
implementation reports, 14(1), 210-247.
Ghimire, S., Castelino, R. L., Lioufas, N. M., Peterson, G. M., & Zaidi, S. T. R. (2015).
Nonadherence to medication therapy in haemodialysis patients: a systematic review. PloS
one, 10(12), e0144119.
Guarienti, M., Giacopuzzi, E., Gianoncelli, A., Sigala, S., Spano, P., Pecorelli, S., ... & Memo,
M. (2015). Computational and functional analysis of biopharmaceutical drugs in
zebrafish: Erythropoietin as a test model. Pharmacological research, 102, 12-21.
Jhund, P. S., & McMurray, J. J. (2016). The neprilysin pathway in heart failure: a review and
guide on the use of sacubitril/valsartan. Heart, 102(17), 1342-1347.
Johansen, K. L., Dalrymple, L. S., Delgado, C., Chertow, G. M., Segal, M. R., Chiang, J., ... &
Kaysen, G. A. (2017). Factors associated with frailty and its trajectory among patients on
hemodialysis. Clinical Journal of the American Society of Nephrology, 12(7), 1100-1108.
Levey, A. S., Becker, C., & Inker, L. A. (2015). Glomerular filtration rate and albuminuria for
detection and staging of acute and chronic kidney disease in adults: a systematic
review. Jama, 313(8), 837-846.
Levey, A. S., Inker, L. A., & Coresh, J. (2015). Chronic kidney disease in older
people. Jama, 314(6), 557-558.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10NURSING ASSIGNMENT
McCormack, P. L. (2016). Sacubitril/valsartan: a review in chronic heart failure with reduced
ejection fraction. Drugs, 76(3), 387-396.
Monseu, M., Gand, E., Saulnier, P. J., Ragot, S., Piguel, X., Zaoui, P., ... & Halimi, J. M. (2015).
Acute kidney injury predicts major adverse outcomes in diabetes: synergic impact with
low glomerular filtration rate and albuminuria. Diabetes Care, 38(12), 2333-2340.
Moreau, R., & Arroyo, V. (2015). Acute-on-chronic liver failure: a new clinical entity. Clinical
Gastroenterology and Hepatology, 13(5), 836-841.
Mushi, L., Marschall, P., & Fleßa, S. (2015). The cost of dialysis in low and middle-income
countries: a systematic review. BMC health services research, 15(1), 506.
Oh, M., Yoon, J., & Cho, D. Y. (2015). Pharmacokinetic and Pharmacodynamic Comparison of
Two Recombinant Human Erythropoietin Formulations, PDA10 and Eprex, in Healthy
Korean Male Volunteers: A Randomized, Double-Blinded, Single-Dose, Two-Period
Crossover Study. Clinical drug investigation, 35(10), 659-664.
Ramanathan, S., Kumar, D., Khanna, M., Al Heidous, M., Sheikh, A., Virmani, V., &
Palaniappan, Y. (2016). Multi-modality imaging review of congenital abnormalities of
kidney and upper urinary tract. World journal of radiology, 8(2), 132.
Shang, W., Li, L., Huang, S., Zeng, R., Huang, L., Ge, S., & Xu, G. (2016). Chronic kidney
disease and the risk of new-onset atrial fibrillation: a meta-analysis of prospective cohort
studies. PloS one, 11(5), e0155581.
Sharma, V., Ramesh Babu, C. S., & Gupta, O. P. (2015). Horseshoe kidney: A multidetector
computed tomography study. Int J Anat Res, 3(2), 1049-55.
McCormack, P. L. (2016). Sacubitril/valsartan: a review in chronic heart failure with reduced
ejection fraction. Drugs, 76(3), 387-396.
Monseu, M., Gand, E., Saulnier, P. J., Ragot, S., Piguel, X., Zaoui, P., ... & Halimi, J. M. (2015).
Acute kidney injury predicts major adverse outcomes in diabetes: synergic impact with
low glomerular filtration rate and albuminuria. Diabetes Care, 38(12), 2333-2340.
Moreau, R., & Arroyo, V. (2015). Acute-on-chronic liver failure: a new clinical entity. Clinical
Gastroenterology and Hepatology, 13(5), 836-841.
Mushi, L., Marschall, P., & Fleßa, S. (2015). The cost of dialysis in low and middle-income
countries: a systematic review. BMC health services research, 15(1), 506.
Oh, M., Yoon, J., & Cho, D. Y. (2015). Pharmacokinetic and Pharmacodynamic Comparison of
Two Recombinant Human Erythropoietin Formulations, PDA10 and Eprex, in Healthy
Korean Male Volunteers: A Randomized, Double-Blinded, Single-Dose, Two-Period
Crossover Study. Clinical drug investigation, 35(10), 659-664.
Ramanathan, S., Kumar, D., Khanna, M., Al Heidous, M., Sheikh, A., Virmani, V., &
Palaniappan, Y. (2016). Multi-modality imaging review of congenital abnormalities of
kidney and upper urinary tract. World journal of radiology, 8(2), 132.
Shang, W., Li, L., Huang, S., Zeng, R., Huang, L., Ge, S., & Xu, G. (2016). Chronic kidney
disease and the risk of new-onset atrial fibrillation: a meta-analysis of prospective cohort
studies. PloS one, 11(5), e0155581.
Sharma, V., Ramesh Babu, C. S., & Gupta, O. P. (2015). Horseshoe kidney: A multidetector
computed tomography study. Int J Anat Res, 3(2), 1049-55.

11NURSING ASSIGNMENT
Tsai, W. C., Wu, H. Y., Peng, Y. S., Ko, M. J., Wu, M. S., Hung, K. Y., ... & Chien, K. L.
(2016). Risk factors for development and progression of chronic kidney disease: a
systematic review and exploratory meta-analysis. Medicine, 95(11).
Tsai, W. C., Wu, H. Y., Peng, Y. S., Ko, M. J., Wu, M. S., Hung, K. Y., ... & Chien, K. L.
(2016). Risk factors for development and progression of chronic kidney disease: a
systematic review and exploratory meta-analysis. Medicine, 95(11).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





