A Randomised Controlled Trial: CBT vs. Antidepressants for Depression
VerifiedAdded on 2023/06/10
|7
|2141
|437
Project
AI Summary
This research proposal outlines a randomized controlled single-blind trial comparing the effectiveness of cognitive behavioral therapy (CBT) versus antidepressants (fluoxetine) in treating adults diagnosed with mild to moderate major depressive disorder. The study aims to recruit 200 participants, aged 18 and above, with a MADRS score of >18, excluding those currently on antidepressant or CBT treatment, or with comorbid conditions. Participants will be randomly assigned to either the CBT or pharmacotherapy group. CBT will involve 12 sessions focusing on behavioral activation and cognitive restructuring, while the pharmacotherapy group will receive fluoxetine, with dosage adjustments based on clinical response. Primary outcomes include assessing depressive symptoms and suicidal ideation using the Hamilton Rating Scale and Beck Depression Inventory. Secondary outcomes involve assessing functional status. Statistical analysis will be performed using SPSS 21.0, employing logistic regression, χ2, random effects linear regression, and ANOVA to compare treatment effects. The study's strategic importance lies in its potential to inform clinical practice and improve patient outcomes by identifying the more effective intervention for depression treatment.

Running head: RESEARCH PROPOSAL
Treatment of Depression, Cognitive therapy VS anti-depressants a randomised controlled
single blind trial on adults
Name of the Student
Name of the University
Author Note
Treatment of Depression, Cognitive therapy VS anti-depressants a randomised controlled
single blind trial on adults
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1RESEARCH PROPOSAL
Table of Contents
Section 1.....................................................................................................................................2
Introduction............................................................................................................................2
Research hypothesis...............................................................................................................2
Background............................................................................................................................2
Research objectives................................................................................................................2
Section 2.....................................................................................................................................2
Participant selection...............................................................................................................2
Sample recruitment................................................................................................................3
Ethical approval.....................................................................................................................3
Randomisation........................................................................................................................3
Pharmacotherapy....................................................................................................................3
Cognitive Behavioural Therapy.............................................................................................3
Primary outcome....................................................................................................................4
Secondary outcome................................................................................................................4
Statistical analysis..................................................................................................................4
Section 3.....................................................................................................................................4
Strategic importance...............................................................................................................4
Section 4.....................................................................................................................................4
References..................................................................................................................................5
Table of Contents
Section 1.....................................................................................................................................2
Introduction............................................................................................................................2
Research hypothesis...............................................................................................................2
Background............................................................................................................................2
Research objectives................................................................................................................2
Section 2.....................................................................................................................................2
Participant selection...............................................................................................................2
Sample recruitment................................................................................................................3
Ethical approval.....................................................................................................................3
Randomisation........................................................................................................................3
Pharmacotherapy....................................................................................................................3
Cognitive Behavioural Therapy.............................................................................................3
Primary outcome....................................................................................................................4
Secondary outcome................................................................................................................4
Statistical analysis..................................................................................................................4
Section 3.....................................................................................................................................4
Strategic importance...............................................................................................................4
Section 4.....................................................................................................................................4
References..................................................................................................................................5
2RESEARCH PROPOSAL
Section 1
Introduction
Depression, commonly known as major depressive disorder are characterised by
persistent low mood that is manifested by the affected individual in most situations. This
condition is generally accompanies by loss of interest, low self-esteem, pain, and low energy
(Snyder, 2013). This psychological condition most often creates negative impacts on the
personal, and professional life of the affected person and also affects the eating and sleeping
habits, thereby lowering the general health status.
Research hypothesis
Cognitive behavioural therapy is more effective than antidepressants in the treatment
of major depressive disorder
Background
Cognitive therapy is directed towards solving presenting mental problems of clients
and also teach the clients to bring about modifications in their behaviour and dysfunctional
thinking (van der Velden et al., 2015). On the other hand, antidepressants are drugs used for
the treatment of depression and other comorbid conditions such as, anxiety disorders,
dysthymia, and seasonal affective disorder (McGrath et al., 2013). Selective serotonin
reuptake inhibitors are the mainstay of treating depression owing to their mild side effects
and less toxicity, when administered in overdose, in comparison to other antidepressants
(Cipriani et al., 2016). On the other hand, studies have also shown that cognitive therapy
effectively treats depression and its effectiveness is comparable to that of psychodynamic
therapy and antidepressants (Hollon et al., 2014).
Research objectives
To determine the effectiveness of antidepressant (fluoxetine) on reducing depression
associated mood and behaviour- Antidepressants have been identified as best
pharmacotherapy options for treating people with a history of moderate to severe
depression
To determine the effectiveness of cognitive therapy on lowering symptoms associated
with depression- It has been recommended for patients suffering from moderate to
chronic unipolar depression
To compare between the two interventions and identify the better treatment option-
Comparing between the two options will pave the way for new clinical applications
and improve patient outcomes
Section 2
Participant selection
Eligibility criteria will include participants, aged 18 years or more, who have been
diagnosed with mild depression, based on the DSM-V diagnostic criteria (Uher et al., 2014).
A total of 200 participants will be recruited over a period of six months. The inclusion criteria
will comprise of individuals who will score more than 18 in the Montgomery–Åsberg
Depression Rating Scale (MADRS) (Kjærgaard et al., 2014). They should be of normal
intelligence and in good health. However, patients who are on fluoxetine or cognitive therapy
treatment will be excluded from the study. Exclusion criteria will include those with a
concurrent diagnosis of bipolar disorder, known systemic medical disorder, and clinical
diagnosis of any substance use disorder.
Section 1
Introduction
Depression, commonly known as major depressive disorder are characterised by
persistent low mood that is manifested by the affected individual in most situations. This
condition is generally accompanies by loss of interest, low self-esteem, pain, and low energy
(Snyder, 2013). This psychological condition most often creates negative impacts on the
personal, and professional life of the affected person and also affects the eating and sleeping
habits, thereby lowering the general health status.
Research hypothesis
Cognitive behavioural therapy is more effective than antidepressants in the treatment
of major depressive disorder
Background
Cognitive therapy is directed towards solving presenting mental problems of clients
and also teach the clients to bring about modifications in their behaviour and dysfunctional
thinking (van der Velden et al., 2015). On the other hand, antidepressants are drugs used for
the treatment of depression and other comorbid conditions such as, anxiety disorders,
dysthymia, and seasonal affective disorder (McGrath et al., 2013). Selective serotonin
reuptake inhibitors are the mainstay of treating depression owing to their mild side effects
and less toxicity, when administered in overdose, in comparison to other antidepressants
(Cipriani et al., 2016). On the other hand, studies have also shown that cognitive therapy
effectively treats depression and its effectiveness is comparable to that of psychodynamic
therapy and antidepressants (Hollon et al., 2014).
Research objectives
To determine the effectiveness of antidepressant (fluoxetine) on reducing depression
associated mood and behaviour- Antidepressants have been identified as best
pharmacotherapy options for treating people with a history of moderate to severe
depression
To determine the effectiveness of cognitive therapy on lowering symptoms associated
with depression- It has been recommended for patients suffering from moderate to
chronic unipolar depression
To compare between the two interventions and identify the better treatment option-
Comparing between the two options will pave the way for new clinical applications
and improve patient outcomes
Section 2
Participant selection
Eligibility criteria will include participants, aged 18 years or more, who have been
diagnosed with mild depression, based on the DSM-V diagnostic criteria (Uher et al., 2014).
A total of 200 participants will be recruited over a period of six months. The inclusion criteria
will comprise of individuals who will score more than 18 in the Montgomery–Åsberg
Depression Rating Scale (MADRS) (Kjærgaard et al., 2014). They should be of normal
intelligence and in good health. However, patients who are on fluoxetine or cognitive therapy
treatment will be excluded from the study. Exclusion criteria will include those with a
concurrent diagnosis of bipolar disorder, known systemic medical disorder, and clinical
diagnosis of any substance use disorder.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3RESEARCH PROPOSAL
Sample recruitment
Private psychiatrists, general practitioners and local psychiatric inpatient units will be
contacted for recruitment. Pamphlets will also be distributed in university campuses, waiting
rooms and community centres.
Ethical approval
Approval to conduct the RCT will be collected from the Human Research Ethics
Committee. Following participant selection, an envelope will be sent to all of them, stating
the purpose, benefits and use of the research. This will be followed by obtaining a written
informed consent from each of them.
Randomisation
Individuals who will qualify for the research will be randomly assigned to one of the
two study conditions, namely, cognitive therapy and antidepressant pharmacotherapy. This
will be done after matching every subject in one particular group with the counterpart in the
other. This will reduce chance of skewing results due to some influential variable.
Randomisation process will be conducted by research staff, blinded to the treatment
condition, until the end of the study. All therapists will provide the treatment in both the
intervention groups. Patients assigned to the antidepressant treatment group will be made to
attend one week long sessions with a trained psychiatrist.
Pharmacotherapy
All participants will be examined at the beginning of the study, at 6 weeks, and 12
weeks. The medication sessions will have a duration of 30-60 minutes and will also include a
vital signs assessment and measurement of the adverse effects of drugs, their safety dosage,
and symptomatic response. This will occur weekly, for the first month, and every alternate
week thereafter. The dosage of the SSRI (fluoxetine) will be 10mg/day for the first week,
followed by 20mg/day for weeks 2 to 6. There will be an option to increase the dosage to
40mg/day on observing insufficient clinical improvements among the patients, based on the
Clinical Global Impressions-Severity subscale. The maximum dosage of fluoxetine that will
be allowed. Following any adverse effects after increase in dosage of the medication, it will
be lowered to 20mg of fluoxetine.
During the follow-up period, fluoxetine administration will continue. However, there
will be face-to-face meetings. Booster sessions will be held that will focus on clinical
management. The treatment will be focused on the following: (1) pharmacotherapy
management that will involve providing education to the patients about the medication,
dosage adjustment and schedules and potential side effects, (2) clinical management that will
involve assessing the functioning of the participants in major life activities, limited advice
giving and support counselling.
Cognitive Behavioural Therapy
The CBT will comprise of behavioural activation and modification of dysfunctional
thoughts, in addition to incorporating structural modification and identification of core beliefs
that are presumed to result in depressive thoughts in the participants. This therapy will
comprise of 12 sessions, each for a duration of 60-90 minutes during the first 12 weeks of the
intervention. Of these, weeks 3-6 will comprise of family sessions, which will be aimed at
identifying the roots of major depressive disorder among the participants. The family session
will also assist all family members to behave and think more adaptively, thereby allowing the
family members to demonstrate respect, empathy, and care towards the affected individuals.
The treatment will be administered in a progressive manner that will facilitate the
recognition and modification of core and intermediate beliefs. While the first week sessions
Sample recruitment
Private psychiatrists, general practitioners and local psychiatric inpatient units will be
contacted for recruitment. Pamphlets will also be distributed in university campuses, waiting
rooms and community centres.
Ethical approval
Approval to conduct the RCT will be collected from the Human Research Ethics
Committee. Following participant selection, an envelope will be sent to all of them, stating
the purpose, benefits and use of the research. This will be followed by obtaining a written
informed consent from each of them.
Randomisation
Individuals who will qualify for the research will be randomly assigned to one of the
two study conditions, namely, cognitive therapy and antidepressant pharmacotherapy. This
will be done after matching every subject in one particular group with the counterpart in the
other. This will reduce chance of skewing results due to some influential variable.
Randomisation process will be conducted by research staff, blinded to the treatment
condition, until the end of the study. All therapists will provide the treatment in both the
intervention groups. Patients assigned to the antidepressant treatment group will be made to
attend one week long sessions with a trained psychiatrist.
Pharmacotherapy
All participants will be examined at the beginning of the study, at 6 weeks, and 12
weeks. The medication sessions will have a duration of 30-60 minutes and will also include a
vital signs assessment and measurement of the adverse effects of drugs, their safety dosage,
and symptomatic response. This will occur weekly, for the first month, and every alternate
week thereafter. The dosage of the SSRI (fluoxetine) will be 10mg/day for the first week,
followed by 20mg/day for weeks 2 to 6. There will be an option to increase the dosage to
40mg/day on observing insufficient clinical improvements among the patients, based on the
Clinical Global Impressions-Severity subscale. The maximum dosage of fluoxetine that will
be allowed. Following any adverse effects after increase in dosage of the medication, it will
be lowered to 20mg of fluoxetine.
During the follow-up period, fluoxetine administration will continue. However, there
will be face-to-face meetings. Booster sessions will be held that will focus on clinical
management. The treatment will be focused on the following: (1) pharmacotherapy
management that will involve providing education to the patients about the medication,
dosage adjustment and schedules and potential side effects, (2) clinical management that will
involve assessing the functioning of the participants in major life activities, limited advice
giving and support counselling.
Cognitive Behavioural Therapy
The CBT will comprise of behavioural activation and modification of dysfunctional
thoughts, in addition to incorporating structural modification and identification of core beliefs
that are presumed to result in depressive thoughts in the participants. This therapy will
comprise of 12 sessions, each for a duration of 60-90 minutes during the first 12 weeks of the
intervention. Of these, weeks 3-6 will comprise of family sessions, which will be aimed at
identifying the roots of major depressive disorder among the participants. The family session
will also assist all family members to behave and think more adaptively, thereby allowing the
family members to demonstrate respect, empathy, and care towards the affected individuals.
The treatment will be administered in a progressive manner that will facilitate the
recognition and modification of core and intermediate beliefs. While the first week sessions
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4RESEARCH PROPOSAL
would focus on establishing a rapport, reviewing the problem, and providing a general outline
for the therapy, the following weeks will encompass relaxation training, problem solving,
personalisation, fallacy control and overgeneralisation.
Primary outcome
Presence of depressive symptoms and suicidal ideations will be the primary outcomes
based on the Hamilton Rating Scale for Depression and Suicide Ideation Questionnaire-Jr.
Self-reported depression will also be measured by the Beck Depression Inventory II scale.
Secondary outcome
Assessing the functional status of the participants will be the secondary outcome.
Statistical analysis
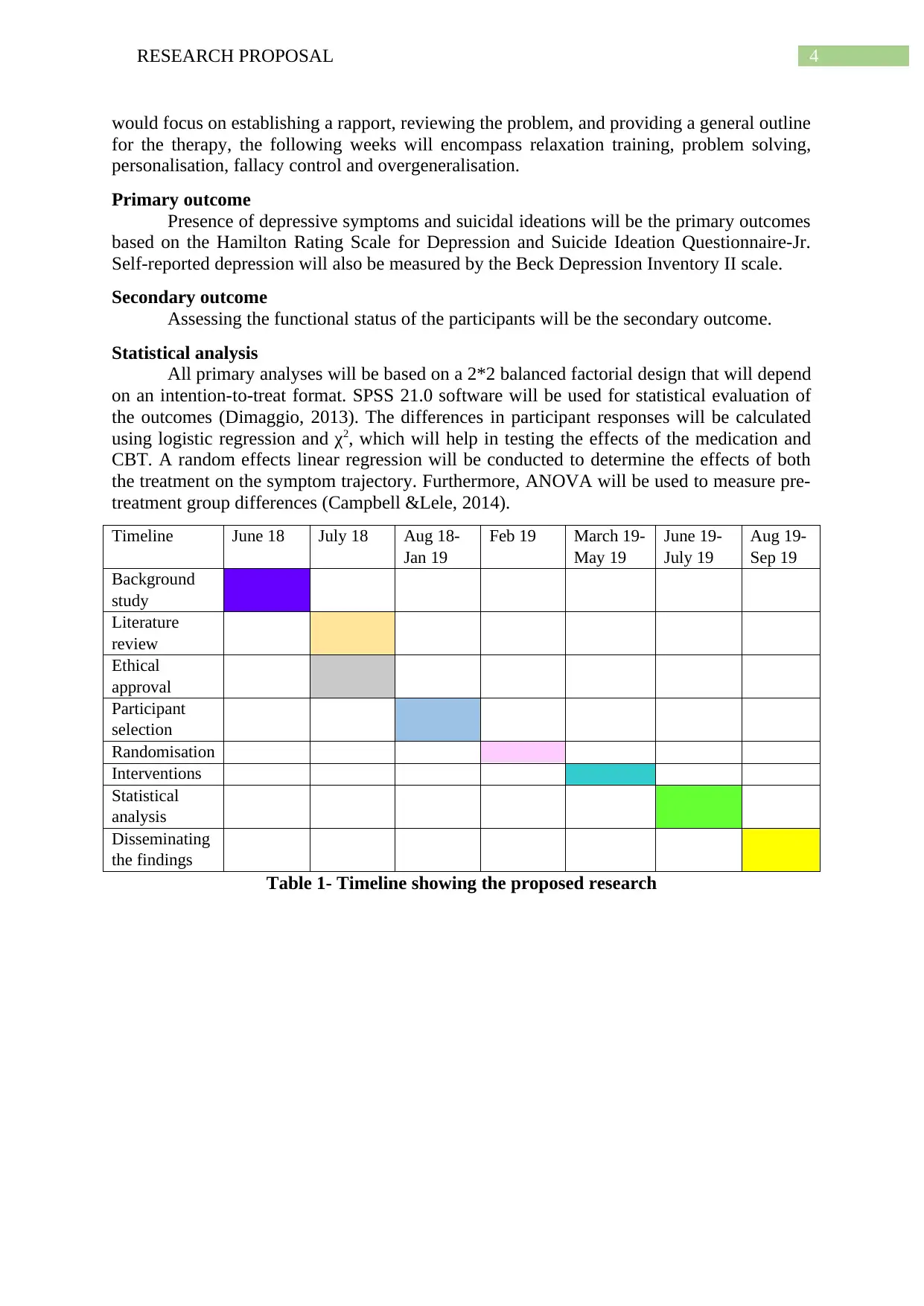
All primary analyses will be based on a 2*2 balanced factorial design that will depend
on an intention-to-treat format. SPSS 21.0 software will be used for statistical evaluation of
the outcomes (Dimaggio, 2013). The differences in participant responses will be calculated
using logistic regression and χ2, which will help in testing the effects of the medication and
CBT. A random effects linear regression will be conducted to determine the effects of both
the treatment on the symptom trajectory. Furthermore, ANOVA will be used to measure pre-
treatment group differences (Campbell &Lele, 2014).
Timeline June 18 July 18 Aug 18-
Jan 19
Feb 19 March 19-
May 19
June 19-
July 19
Aug 19-
Sep 19
Background
study
Literature
review
Ethical
approval
Participant
selection
Randomisation
Interventions
Statistical
analysis
Disseminating
the findings
Table 1- Timeline showing the proposed research
would focus on establishing a rapport, reviewing the problem, and providing a general outline
for the therapy, the following weeks will encompass relaxation training, problem solving,
personalisation, fallacy control and overgeneralisation.
Primary outcome
Presence of depressive symptoms and suicidal ideations will be the primary outcomes
based on the Hamilton Rating Scale for Depression and Suicide Ideation Questionnaire-Jr.
Self-reported depression will also be measured by the Beck Depression Inventory II scale.
Secondary outcome
Assessing the functional status of the participants will be the secondary outcome.
Statistical analysis
All primary analyses will be based on a 2*2 balanced factorial design that will depend
on an intention-to-treat format. SPSS 21.0 software will be used for statistical evaluation of
the outcomes (Dimaggio, 2013). The differences in participant responses will be calculated
using logistic regression and χ2, which will help in testing the effects of the medication and
CBT. A random effects linear regression will be conducted to determine the effects of both
the treatment on the symptom trajectory. Furthermore, ANOVA will be used to measure pre-
treatment group differences (Campbell &Lele, 2014).
Timeline June 18 July 18 Aug 18-
Jan 19
Feb 19 March 19-
May 19
June 19-
July 19
Aug 19-
Sep 19
Background
study
Literature
review
Ethical
approval
Participant
selection
Randomisation
Interventions
Statistical
analysis
Disseminating
the findings
Table 1- Timeline showing the proposed research

5RESEARCH PROPOSAL
Section 3
Strategic importance
Owing to fact that one in six adults had been diagnosed with common mental
disorders at a point in their lives by the 2012/13 New Zealand Health Survey, there is a need
to effectively disseminate the findings of the RCT (Mental Health Foundation, 2018).
Following an analysis of the outcomes, the study will help in gaining a sound understanding
of the better intervention for treating depression, the evidence of which can be utilised by
clinicians and therapists for reducing the prevalence rates of the disorder in New Zealand.
Section 4
Expected outcomes that focus on a greater reduction in depression and suicidal
thoughts upon CBT administration will be disseminated by presenting an article and sending
it for publication in an international journal. Conference presentations will be held with the
key stakeholders such as, public health officials, patients, healthcare providers, research
committees, and health organisations. An effective presentation of the findings might be
successful in gaining government funding for future research.
Section 3
Strategic importance
Owing to fact that one in six adults had been diagnosed with common mental
disorders at a point in their lives by the 2012/13 New Zealand Health Survey, there is a need
to effectively disseminate the findings of the RCT (Mental Health Foundation, 2018).
Following an analysis of the outcomes, the study will help in gaining a sound understanding
of the better intervention for treating depression, the evidence of which can be utilised by
clinicians and therapists for reducing the prevalence rates of the disorder in New Zealand.
Section 4
Expected outcomes that focus on a greater reduction in depression and suicidal
thoughts upon CBT administration will be disseminated by presenting an article and sending
it for publication in an international journal. Conference presentations will be held with the
key stakeholders such as, public health officials, patients, healthcare providers, research
committees, and health organisations. An effective presentation of the findings might be
successful in gaining government funding for future research.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6RESEARCH PROPOSAL
References
Campbell, D., &Lele, S. (2014). An ANOVA test for parameter estimability using data
cloning with application to statistical inference for dynamic systems. Computational
Statistics & Data Analysis, 70, 257-267.
Cipriani, A., Zhou, X., Del Giovane, C., Hetrick, S. E., Qin, B., Whittington, C., ...&Cuijpers,
P. (2016). Comparative efficacy and tolerability of antidepressants for major
depressive disorder in children and adolescents: a network meta-analysis. The
Lancet, 388(10047), 881-890.
Dimaggio, C. (2013). Introduction. In SAS for Epidemiologists(pp. 1-5). Springer, New York,
NY.
Hollon, S. D., DeRubeis, R. J., Fawcett, J., Amsterdam, J. D., Shelton, R. C., Zajecka, J., ... &
Gallop, R. (2014). Effect of cognitive therapy with antidepressant medications vs
antidepressants alone on the rate of recovery in major depressive disorder: a
randomized clinical trial. JAMA psychiatry, 71(10), 1157-1164.
Kjærgaard, M., Arfwedson Wang, C. E., Waterloo, K., &Jorde, R. (2014). A study of the
psychometric properties of the Beck Depression Inventory‐II, the Montgomery and
Åsberg Depression Rating Scale, and the Hospital Anxiety and Depression Scale in a
sample from a healthy population. Scandinavian journal of psychology, 55(1), 83-89.
McGrath, C. L., Kelley, M. E., Holtzheimer, P. E., Dunlop, B. W., Craighead, W. E., Franco,
A. R., ... &Mayberg, H. S. (2013). Toward a neuroimaging treatment selection
biomarker for major depressive disorder. JAMA psychiatry, 70(8), 821-829.
Mental Health Foundation. (2018). Quick Facts and Stats 2014. Retrieved from
https://www.mentalhealth.org.nz/assets/Uploads/MHF-Quick-facts-and-stats-
FINAL.pdf
Snyder, H. R. (2013). Major depressive disorder is associated with broad impairments on
neuropsychological measures of executive function: a meta-analysis and
review. Psychological bulletin, 139(1), 81.
Uher, R., Payne, J. L., Pavlova, B., & Perlis, R. H. (2014). Major depressive disorder in
DSM‐5: Implications for clinical practice and research of changes from DSM‐
IV. Depression and anxiety, 31(6), 459-471.
van der Velden, A. M., Kuyken, W., Wattar, U., Crane, C., Pallesen, K. J., Dahlgaard, J., ... &
Piet, J. (2015). A systematic review of mechanisms of change in mindfulness-based
cognitive therapy in the treatment of recurrent major depressive disorder. Clinical
psychology review, 37, 26-39.
References
Campbell, D., &Lele, S. (2014). An ANOVA test for parameter estimability using data
cloning with application to statistical inference for dynamic systems. Computational
Statistics & Data Analysis, 70, 257-267.
Cipriani, A., Zhou, X., Del Giovane, C., Hetrick, S. E., Qin, B., Whittington, C., ...&Cuijpers,
P. (2016). Comparative efficacy and tolerability of antidepressants for major
depressive disorder in children and adolescents: a network meta-analysis. The
Lancet, 388(10047), 881-890.
Dimaggio, C. (2013). Introduction. In SAS for Epidemiologists(pp. 1-5). Springer, New York,
NY.
Hollon, S. D., DeRubeis, R. J., Fawcett, J., Amsterdam, J. D., Shelton, R. C., Zajecka, J., ... &
Gallop, R. (2014). Effect of cognitive therapy with antidepressant medications vs
antidepressants alone on the rate of recovery in major depressive disorder: a
randomized clinical trial. JAMA psychiatry, 71(10), 1157-1164.
Kjærgaard, M., Arfwedson Wang, C. E., Waterloo, K., &Jorde, R. (2014). A study of the
psychometric properties of the Beck Depression Inventory‐II, the Montgomery and
Åsberg Depression Rating Scale, and the Hospital Anxiety and Depression Scale in a
sample from a healthy population. Scandinavian journal of psychology, 55(1), 83-89.
McGrath, C. L., Kelley, M. E., Holtzheimer, P. E., Dunlop, B. W., Craighead, W. E., Franco,
A. R., ... &Mayberg, H. S. (2013). Toward a neuroimaging treatment selection
biomarker for major depressive disorder. JAMA psychiatry, 70(8), 821-829.
Mental Health Foundation. (2018). Quick Facts and Stats 2014. Retrieved from
https://www.mentalhealth.org.nz/assets/Uploads/MHF-Quick-facts-and-stats-
FINAL.pdf
Snyder, H. R. (2013). Major depressive disorder is associated with broad impairments on
neuropsychological measures of executive function: a meta-analysis and
review. Psychological bulletin, 139(1), 81.
Uher, R., Payne, J. L., Pavlova, B., & Perlis, R. H. (2014). Major depressive disorder in
DSM‐5: Implications for clinical practice and research of changes from DSM‐
IV. Depression and anxiety, 31(6), 459-471.
van der Velden, A. M., Kuyken, W., Wattar, U., Crane, C., Pallesen, K. J., Dahlgaard, J., ... &
Piet, J. (2015). A systematic review of mechanisms of change in mindfulness-based
cognitive therapy in the treatment of recurrent major depressive disorder. Clinical
psychology review, 37, 26-39.
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.



