Wilms Tumour: A Detailed Report on Diagnosis, Treatment Options
VerifiedAdded on 2023/04/24
|15
|3349
|138
Report
AI Summary
This report provides a comprehensive overview of Wilms Tumour, a type of childhood kidney cancer. It covers the epidemiology and aetiology, noting its prevalence and genetic factors. The pathogenesis of the disease, including the two-hit theory and the role of tumour suppressor genes, is discussed. The report details the stages of Wilms Tumour, diagnostic methods such as abdominal ultrasounds, CT scans, and MRIs, and current treatment options including surgery, chemotherapy, and radiation therapy. Potential future treatments and the late effects of current treatments are also addressed, along with the concept of personalized medicine in managing Wilms Tumour. The report emphasizes the importance of early diagnosis and the advancements in treatment that have improved survival rates for children with Wilms Tumour.

Running Head: WILMS TUMOUR 0
Wilms Tumour
[Document subtitle]
[DATE]
Wilms Tumour
[Document subtitle]
[DATE]
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
WILMS TUMOUR 1
Table of Contents
Introduction.................................................................................................................................................2
Epidemiology and aetiology....................................................................................................................2
Pathogenesis...........................................................................................................................................3
Prognosis and diagnosis...........................................................................................................................4
Diagnosis.................................................................................................................................................5
Treatment................................................................................................................................................7
Current treatment...............................................................................................................................7
Potential treatments...........................................................................................................................8
Late effects of the treatment...............................................................................................................9
Personalized medicine.......................................................................................................................10
Conclusion.................................................................................................................................................10
References.................................................................................................................................................12
Table of Contents
Introduction.................................................................................................................................................2
Epidemiology and aetiology....................................................................................................................2
Pathogenesis...........................................................................................................................................3
Prognosis and diagnosis...........................................................................................................................4
Diagnosis.................................................................................................................................................5
Treatment................................................................................................................................................7
Current treatment...............................................................................................................................7
Potential treatments...........................................................................................................................8
Late effects of the treatment...............................................................................................................9
Personalized medicine.......................................................................................................................10
Conclusion.................................................................................................................................................10
References.................................................................................................................................................12
WILMS TUMOUR 2
Introduction
Cancer is the life threatening disease that generally caused with the uncontrolled growth and
multiplication of the tumour cells in the body. Wilms tumour is one of the types of cancer that
affects specifically children. Wilms tumour also known as the nephro-blastoma is the kind of
childhood cancer that begins in the renal part of the body. It is considered as the most usual type
of cancer associated with the kidneys in kids. It is commonly occurs in single kidney only, and
rarely found in both f kidneys. The symptoms associated with this health condition includes
abdominal swelling, abdominal pain, fever, blood come in the urine, constipation, nausea or
vomiting, loss of appetitive, increase blood pressure, and breathing issues (Vujanić, and
Sandstedt, 2010). The cause of this type of cancer is not very clear but in some cases hereditary
and race might play a role in causing this disease. In this particular assessment report the
epidemiology, aetiology, pathogenesis, prognosis, diagnosis, and its treatment options will be
discussed. The contribution of the knowledge of molecular genetics in diagnosis, treatment,
assessment or prognosis of this health condition will also be discussed (Chu, et al., 2010).
Epidemiology and aetiology
It has been estimated that this health conditions affects nearly 80-85 children every in years in
the United Kingdom and most commonly affect the children’s aged 7 years old. It affects one in
10000 kids and thankfully it is curable in 90 per cent of the cases. The incidence of the
occurrence of this health issues is 7 in 1,000, 00 kids under the age of sixteen (Kidney cancer
UK, 2017). It is the second most usual intra-abdominal malignancy of childhood and considered
5th most paediatric cancer overall. There only three per cent adults affected by this type of cancer.
In 5 to 10 per cent patients both the kidneys are affected with this cancer at the same time
(Faranoush, et al, 2009).
Introduction
Cancer is the life threatening disease that generally caused with the uncontrolled growth and
multiplication of the tumour cells in the body. Wilms tumour is one of the types of cancer that
affects specifically children. Wilms tumour also known as the nephro-blastoma is the kind of
childhood cancer that begins in the renal part of the body. It is considered as the most usual type
of cancer associated with the kidneys in kids. It is commonly occurs in single kidney only, and
rarely found in both f kidneys. The symptoms associated with this health condition includes
abdominal swelling, abdominal pain, fever, blood come in the urine, constipation, nausea or
vomiting, loss of appetitive, increase blood pressure, and breathing issues (Vujanić, and
Sandstedt, 2010). The cause of this type of cancer is not very clear but in some cases hereditary
and race might play a role in causing this disease. In this particular assessment report the
epidemiology, aetiology, pathogenesis, prognosis, diagnosis, and its treatment options will be
discussed. The contribution of the knowledge of molecular genetics in diagnosis, treatment,
assessment or prognosis of this health condition will also be discussed (Chu, et al., 2010).
Epidemiology and aetiology
It has been estimated that this health conditions affects nearly 80-85 children every in years in
the United Kingdom and most commonly affect the children’s aged 7 years old. It affects one in
10000 kids and thankfully it is curable in 90 per cent of the cases. The incidence of the
occurrence of this health issues is 7 in 1,000, 00 kids under the age of sixteen (Kidney cancer
UK, 2017). It is the second most usual intra-abdominal malignancy of childhood and considered
5th most paediatric cancer overall. There only three per cent adults affected by this type of cancer.
In 5 to 10 per cent patients both the kidneys are affected with this cancer at the same time
(Faranoush, et al, 2009).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
WILMS TUMOUR 3
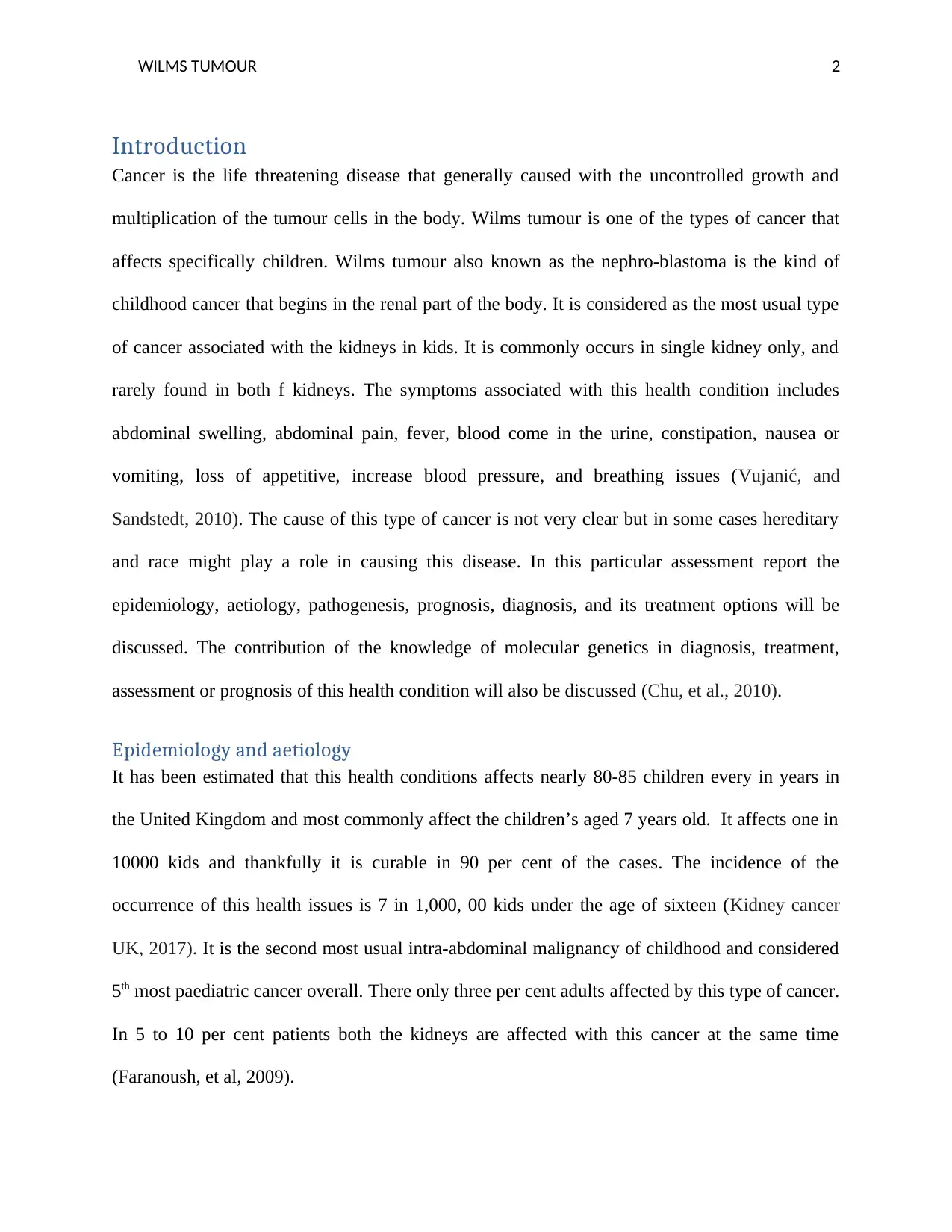
The Wilms' tumour is the genetically heterogeneous neoplasm. It might be caused by inheritance
or occurs sporadically. Some of the genes like WT1 present at the locus of 11p13 and WT2 at
11p15 plays an important role in the general development of this health conditions (Davidoff,
2009). In the evolution of Wilms’ tumour the inactivation of these genes is the initial genetic
event. The secondary events of Wilms’ tumour formations which includes loss of heterozygosity
at the 1p and sixteen p (Fukuzawa, et al., 2010). The risk of growth of this tumour is enhanced in
some overproduction of some syndrome like Beckwith-Wiedmann, hemi hypertrophy, Simpson-
golabi-behman, and Perlman Syndrome. Various studies have tried to identify that the parental
environmental factors like parent’s occupation, their exposure to pesticides, caffeine, hair dye
items, and ionizing radiation. However those studies were not fully conclusive (Huff, 2011).
Figure 1 chromocal aetiology of WT (description; the picture depicting that one segment from normal chromosome 11 is
deleted)
Pathogenesis
The pathogenesis of this kind of cancer is multistage process and considered to be initiated with
the premalignant phase. The first phase of genetic model of Wilms’ tumour is two-hit-theory,
which assumes that the kids who develop this hereditary cancer are born with the mutated
The Wilms' tumour is the genetically heterogeneous neoplasm. It might be caused by inheritance
or occurs sporadically. Some of the genes like WT1 present at the locus of 11p13 and WT2 at
11p15 plays an important role in the general development of this health conditions (Davidoff,
2009). In the evolution of Wilms’ tumour the inactivation of these genes is the initial genetic
event. The secondary events of Wilms’ tumour formations which includes loss of heterozygosity
at the 1p and sixteen p (Fukuzawa, et al., 2010). The risk of growth of this tumour is enhanced in
some overproduction of some syndrome like Beckwith-Wiedmann, hemi hypertrophy, Simpson-
golabi-behman, and Perlman Syndrome. Various studies have tried to identify that the parental
environmental factors like parent’s occupation, their exposure to pesticides, caffeine, hair dye
items, and ionizing radiation. However those studies were not fully conclusive (Huff, 2011).
Figure 1 chromocal aetiology of WT (description; the picture depicting that one segment from normal chromosome 11 is
deleted)
Pathogenesis
The pathogenesis of this kind of cancer is multistage process and considered to be initiated with
the premalignant phase. The first phase of genetic model of Wilms’ tumour is two-hit-theory,
which assumes that the kids who develop this hereditary cancer are born with the mutated
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

WILMS TUMOUR 4
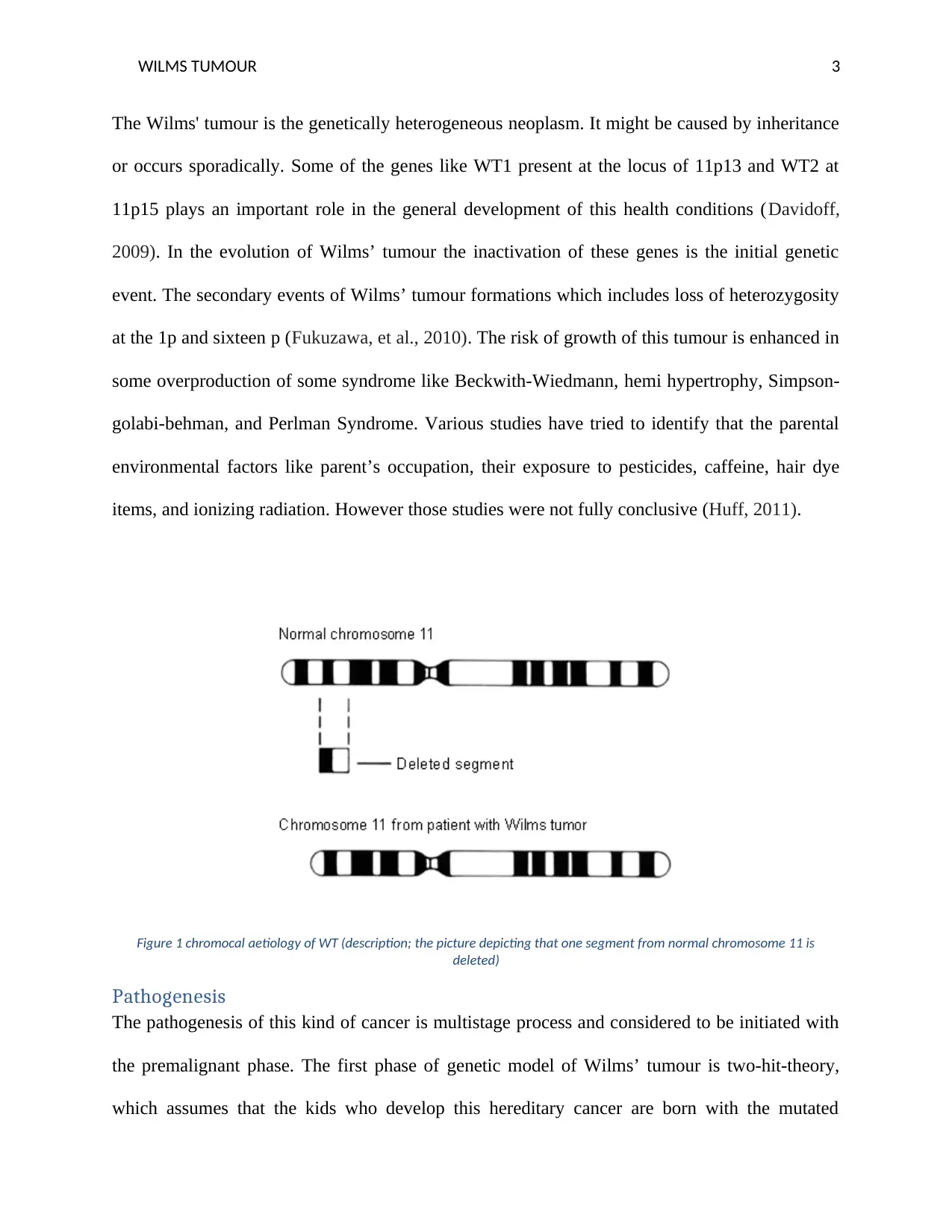
constitutional pre-zygotic DNA in single allele of the gene; this event followed by more genetic
events and ultimately leads to tumour progression (Szychot, Apps, and Pritchard-Jones, 2014).
The putative tumour suppressor genes on particular regions are linked to both sporadic and
hereditary Wilms’ tumour. Some of the regions include 11p13, 11p15, 17q, 19q, 16q, 1p, 5q14,
22q12, Xp22, 11q14, and 17p. Some of the investigators believed that the apparent expression of
oncogene named IGF-11 cause form the imprinting loos of a maternal IGF-11 gene might be
linked to the common epigenetic changes in the Wilms’ tumour (Davidoff, 2012).
Figure 2 pathogenesis of Wilms’ tumour (description; there are four different mutant genes are showed, in the mutant WT1 ½
releases AKH which attaches to the TET 2 and causes deletion to the DNA fragment) (Rampal, and Figueroa, 2016)
Histology
Wilm's tumor also called nephroblastoma is recognised as the most shared malicious pediatric
renal tumor typically appears at the age of 2-5 years. The malignant tumour is typically known to
constitutional pre-zygotic DNA in single allele of the gene; this event followed by more genetic
events and ultimately leads to tumour progression (Szychot, Apps, and Pritchard-Jones, 2014).
The putative tumour suppressor genes on particular regions are linked to both sporadic and
hereditary Wilms’ tumour. Some of the regions include 11p13, 11p15, 17q, 19q, 16q, 1p, 5q14,
22q12, Xp22, 11q14, and 17p. Some of the investigators believed that the apparent expression of
oncogene named IGF-11 cause form the imprinting loos of a maternal IGF-11 gene might be
linked to the common epigenetic changes in the Wilms’ tumour (Davidoff, 2012).
Figure 2 pathogenesis of Wilms’ tumour (description; there are four different mutant genes are showed, in the mutant WT1 ½
releases AKH which attaches to the TET 2 and causes deletion to the DNA fragment) (Rampal, and Figueroa, 2016)
Histology
Wilm's tumor also called nephroblastoma is recognised as the most shared malicious pediatric
renal tumor typically appears at the age of 2-5 years. The malignant tumour is typically known to
WILMS TUMOUR 5
comprise three histologic constituents counting blastema, epithelial components, and stromal
components. Though, the malignant tumour might be biphasic or infrequently monophasic
Prognosis and diagnosis
LOH used for DNA markers on the chromosomes 1p and 16q is associated with the increased
rate of repetition and inferior prognosis in kids with satisfactory histology in Wilms’ tumour.
Having more fragment of chromosome might also be linked with the increased chance of
reappearance. An illustration of this is the addition of a segment of chromosome termed 1q
(Wills, Kast, Stewart, Sullivan, Rabah, Poulik, Pandya, Auner, and Klein, 2009).
Stages of WT
Stage 1 comprises a contained tumour in the renal part, which can be removed surgically.
This is frequently done by the chemotherapy regimen and radiotherapy to decrease threat
of deterioration (Dome, and Huff, 2016).
Stage 2 tumours are restricted to the renal part but sometimes reached an additional
advanced phase. This similarly involves operating nephrectomy and preventative
chemotherapy and radiotherapy.
Stage 3 tumours are still restricted to the renal part or kidney but have proceeded to an
additional advanced phase. Management includes radiotherapy, surgical nephrectomy,
and chemotherapy and, with four-year survival degree from 53 per cent.
Stage 4 tumours have typically metastasized to further areas all over the body.
Management comprises radiotherapy, nephrectomy, and chemotherapy and, with four-
year of survival degree from 44 per cent (Szychot, Apps, and Pritchard-Jones, 2014).
comprise three histologic constituents counting blastema, epithelial components, and stromal
components. Though, the malignant tumour might be biphasic or infrequently monophasic
Prognosis and diagnosis
LOH used for DNA markers on the chromosomes 1p and 16q is associated with the increased
rate of repetition and inferior prognosis in kids with satisfactory histology in Wilms’ tumour.
Having more fragment of chromosome might also be linked with the increased chance of
reappearance. An illustration of this is the addition of a segment of chromosome termed 1q
(Wills, Kast, Stewart, Sullivan, Rabah, Poulik, Pandya, Auner, and Klein, 2009).
Stages of WT
Stage 1 comprises a contained tumour in the renal part, which can be removed surgically.
This is frequently done by the chemotherapy regimen and radiotherapy to decrease threat
of deterioration (Dome, and Huff, 2016).
Stage 2 tumours are restricted to the renal part but sometimes reached an additional
advanced phase. This similarly involves operating nephrectomy and preventative
chemotherapy and radiotherapy.
Stage 3 tumours are still restricted to the renal part or kidney but have proceeded to an
additional advanced phase. Management includes radiotherapy, surgical nephrectomy,
and chemotherapy and, with four-year survival degree from 53 per cent.
Stage 4 tumours have typically metastasized to further areas all over the body.
Management comprises radiotherapy, nephrectomy, and chemotherapy and, with four-
year of survival degree from 44 per cent (Szychot, Apps, and Pritchard-Jones, 2014).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
WILMS TUMOUR 6
Stage 5 tumours now metastasized to new areas all the way through the body and
extended a progressive stage. Treatment includes bilateral renal biopsy, radiotherapy,
nephrectomy, and chemotherapy. The 4-year survival rate is 42 percent (Davidoff, 2009).
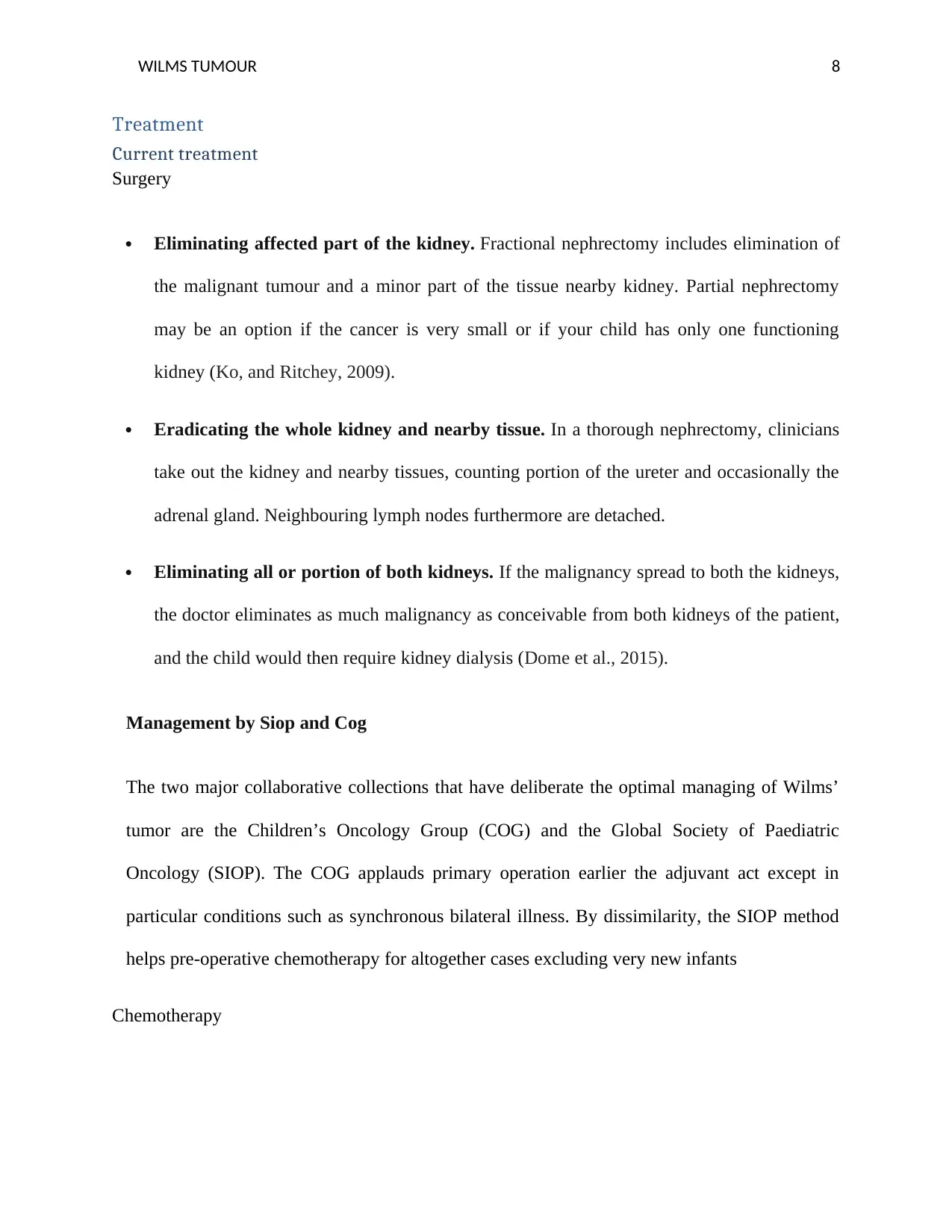
Diagnosis
Wilms’’’ tumour frequently does not disturb child’s well-being. The early diagnosis is attained
by using abdominal ultrasound to check the existence of a crucial mass. Afterward getting the
evidence of the availability of the malignant tumour, the CT examination or MRI to the
stomach can be used. Chest CT examination must be done as the malignant tumour might
cause metastasis problem into the lung in about 20 percent of children. A biopsy for the tumour
is not naturally implemented due to the threat of making trashes of malignance tissue and
spreading them to the abdomen (Szychot, Apps, and Pritchard-Jones, 2014).
Table 1 diagnostic test for WT and results
Tests Results
CBC Common and haemoglobin is less than 11
g/dL
Renal function test Usual or reduced creatinine clearance/
enhanced serum creatinine
LFTs Normal or increased AST, ALT and the serum
bilirubin
Urinalysis Clear or red colour, red blood cells higher than
3/high power field, and protein is higher than
Stage 5 tumours now metastasized to new areas all the way through the body and
extended a progressive stage. Treatment includes bilateral renal biopsy, radiotherapy,
nephrectomy, and chemotherapy. The 4-year survival rate is 42 percent (Davidoff, 2009).
Diagnosis
Wilms’’’ tumour frequently does not disturb child’s well-being. The early diagnosis is attained
by using abdominal ultrasound to check the existence of a crucial mass. Afterward getting the
evidence of the availability of the malignant tumour, the CT examination or MRI to the
stomach can be used. Chest CT examination must be done as the malignant tumour might
cause metastasis problem into the lung in about 20 percent of children. A biopsy for the tumour
is not naturally implemented due to the threat of making trashes of malignance tissue and
spreading them to the abdomen (Szychot, Apps, and Pritchard-Jones, 2014).
Table 1 diagnostic test for WT and results
Tests Results
CBC Common and haemoglobin is less than 11
g/dL
Renal function test Usual or reduced creatinine clearance/
enhanced serum creatinine
LFTs Normal or increased AST, ALT and the serum
bilirubin
Urinalysis Clear or red colour, red blood cells higher than
3/high power field, and protein is higher than
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
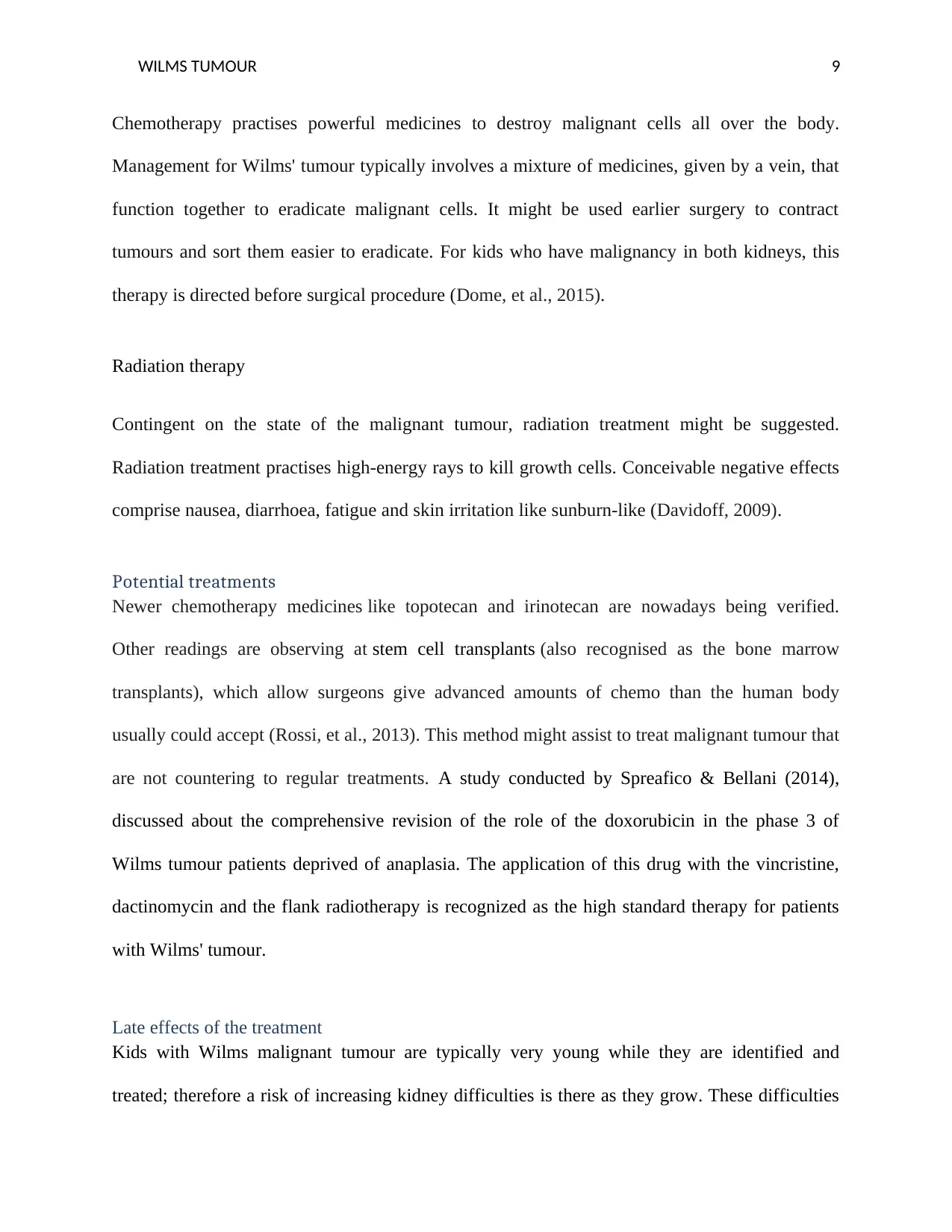
WILMS TUMOUR 7
thirty mg/dL
Serum complete protein or albumin Usual or low
Coagulation investigations Normal or extended aPTT
Level of serum and calcium Normal or increased
Ultrasound of abdomen with Doppler Heterogeneous, evenly echogenic, specially
compact mass arising from the renal part with
or deprived of cystic mass (Vujanić, and
Sandstedt, 2010)
X-ray of chest Hilar and mediastinal broadening because of
lymphadenopathy might be recognized (Wills,
et al., 2009)
CT or MRI abdomen Renal mass including heterogeneous
augmentation; extra renal lesions linked with
the metastatic disorder
CR or MRI chest Extra renal ass linked with the metastatic
disorders
Biopsy Confirms the identification or diagnosis with
pathologic presences (Szychot, Apps, and
Pritchard-Jones, 2014)
thirty mg/dL
Serum complete protein or albumin Usual or low
Coagulation investigations Normal or extended aPTT
Level of serum and calcium Normal or increased
Ultrasound of abdomen with Doppler Heterogeneous, evenly echogenic, specially
compact mass arising from the renal part with
or deprived of cystic mass (Vujanić, and
Sandstedt, 2010)
X-ray of chest Hilar and mediastinal broadening because of
lymphadenopathy might be recognized (Wills,
et al., 2009)
CT or MRI abdomen Renal mass including heterogeneous
augmentation; extra renal lesions linked with
the metastatic disorder
CR or MRI chest Extra renal ass linked with the metastatic
disorders
Biopsy Confirms the identification or diagnosis with
pathologic presences (Szychot, Apps, and
Pritchard-Jones, 2014)
WILMS TUMOUR 8
Treatment
Current treatment
Surgery
Eliminating affected part of the kidney. Fractional nephrectomy includes elimination of
the malignant tumour and a minor part of the tissue nearby kidney. Partial nephrectomy
may be an option if the cancer is very small or if your child has only one functioning
kidney (Ko, and Ritchey, 2009).
Eradicating the whole kidney and nearby tissue. In a thorough nephrectomy, clinicians
take out the kidney and nearby tissues, counting portion of the ureter and occasionally the
adrenal gland. Neighbouring lymph nodes furthermore are detached.
Eliminating all or portion of both kidneys. If the malignancy spread to both the kidneys,
the doctor eliminates as much malignancy as conceivable from both kidneys of the patient,
and the child would then require kidney dialysis (Dome et al., 2015).
Management by Siop and Cog
The two major collaborative collections that have deliberate the optimal managing of Wilms’
tumor are the Children’s Oncology Group (COG) and the Global Society of Paediatric
Oncology (SIOP). The COG applauds primary operation earlier the adjuvant act except in
particular conditions such as synchronous bilateral illness. By dissimilarity, the SIOP method
helps pre-operative chemotherapy for altogether cases excluding very new infants
Chemotherapy
Treatment
Current treatment
Surgery
Eliminating affected part of the kidney. Fractional nephrectomy includes elimination of
the malignant tumour and a minor part of the tissue nearby kidney. Partial nephrectomy
may be an option if the cancer is very small or if your child has only one functioning
kidney (Ko, and Ritchey, 2009).
Eradicating the whole kidney and nearby tissue. In a thorough nephrectomy, clinicians
take out the kidney and nearby tissues, counting portion of the ureter and occasionally the
adrenal gland. Neighbouring lymph nodes furthermore are detached.
Eliminating all or portion of both kidneys. If the malignancy spread to both the kidneys,
the doctor eliminates as much malignancy as conceivable from both kidneys of the patient,
and the child would then require kidney dialysis (Dome et al., 2015).
Management by Siop and Cog
The two major collaborative collections that have deliberate the optimal managing of Wilms’
tumor are the Children’s Oncology Group (COG) and the Global Society of Paediatric
Oncology (SIOP). The COG applauds primary operation earlier the adjuvant act except in
particular conditions such as synchronous bilateral illness. By dissimilarity, the SIOP method
helps pre-operative chemotherapy for altogether cases excluding very new infants
Chemotherapy
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
WILMS TUMOUR 9
Chemotherapy practises powerful medicines to destroy malignant cells all over the body.
Management for Wilms' tumour typically involves a mixture of medicines, given by a vein, that
function together to eradicate malignant cells. It might be used earlier surgery to contract
tumours and sort them easier to eradicate. For kids who have malignancy in both kidneys, this
therapy is directed before surgical procedure (Dome, et al., 2015).
Radiation therapy
Contingent on the state of the malignant tumour, radiation treatment might be suggested.
Radiation treatment practises high-energy rays to kill growth cells. Conceivable negative effects
comprise nausea, diarrhoea, fatigue and skin irritation like sunburn-like (Davidoff, 2009).
Potential treatments
Newer chemotherapy medicines like topotecan and irinotecan are nowadays being verified.
Other readings are observing at stem cell transplants (also recognised as the bone marrow
transplants), which allow surgeons give advanced amounts of chemo than the human body
usually could accept (Rossi, et al., 2013). This method might assist to treat malignant tumour that
are not countering to regular treatments. A study conducted by Spreafico & Bellani (2014),
discussed about the comprehensive revision of the role of the doxorubicin in the phase 3 of
Wilms tumour patients deprived of anaplasia. The application of this drug with the vincristine,
dactinomycin and the flank radiotherapy is recognized as the high standard therapy for patients
with Wilms' tumour.
Late effects of the treatment
Kids with Wilms malignant tumour are typically very young while they are identified and
treated; therefore a risk of increasing kidney difficulties is there as they grow. These difficulties
Chemotherapy practises powerful medicines to destroy malignant cells all over the body.
Management for Wilms' tumour typically involves a mixture of medicines, given by a vein, that
function together to eradicate malignant cells. It might be used earlier surgery to contract
tumours and sort them easier to eradicate. For kids who have malignancy in both kidneys, this
therapy is directed before surgical procedure (Dome, et al., 2015).
Radiation therapy
Contingent on the state of the malignant tumour, radiation treatment might be suggested.
Radiation treatment practises high-energy rays to kill growth cells. Conceivable negative effects
comprise nausea, diarrhoea, fatigue and skin irritation like sunburn-like (Davidoff, 2009).
Potential treatments
Newer chemotherapy medicines like topotecan and irinotecan are nowadays being verified.
Other readings are observing at stem cell transplants (also recognised as the bone marrow
transplants), which allow surgeons give advanced amounts of chemo than the human body
usually could accept (Rossi, et al., 2013). This method might assist to treat malignant tumour that
are not countering to regular treatments. A study conducted by Spreafico & Bellani (2014),
discussed about the comprehensive revision of the role of the doxorubicin in the phase 3 of
Wilms tumour patients deprived of anaplasia. The application of this drug with the vincristine,
dactinomycin and the flank radiotherapy is recognized as the high standard therapy for patients
with Wilms' tumour.
Late effects of the treatment
Kids with Wilms malignant tumour are typically very young while they are identified and
treated; therefore a risk of increasing kidney difficulties is there as they grow. These difficulties
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
WILMS TUMOUR 10
comprise proteinuria (extra protein existence in the urine) and hypertension. Kidney failure can
also be a late consequence for kids who have Wilms malignant tumour in both kidneys. Kids
with the WAGR syndrome likewise have a greater threat for failure of kidney. Children cured
with stomach surgical treatment can grow scar tissue that upsurges the threat of bowel
obstruction later in life. Symptoms of bowel barrier include stomach pain and vomiting. Some
chemotherapy medicines used to address Wilms tumour, like doxorubicin may have a late
negative impacts on the heart like cardiomyopathy or left ventricular dysfunction. Radiation
treatment to the upper body (chest) can cause difficulties like pulmonary fibrosis and radiation
pneumonitis. Children may develop and grow sluggish (slow) or less than other kids (Wright,
Green, and Daw, 2009).
Personalized medicine
Personalised medicine includes using knowledge about an individual’s cancer to support
diagnose, cure and analyse how fine treatment is functioning (Ko, and Ritchey, 2009). P- Drug is
the global combined project. It targets to enable the shift to adapted/individualised well-being
care delivery through the safe incorporation of pseudonymised medical (Graf et al., 2012),
radiological and rudimentary science datasets and by constructing multi-scale methods and
models (in silico oncology) of malignant tumour. Personalised drug is, in philosophy, evidence-
based and provides individualised drug at the correct time to the correct patient subsequent in
quantifiable improvements in results and a decrease in health care expenses (Ko, and Ritchey,
2009).
Conclusion
Wilms tumour is a type of cancer that affects mostly children. The malignant tumour grows in
one or sometime in bot kidneys of the kids. The main cause of this health condition is genetic
and it passes from parents to children. Approximately 80 to 85 kids affected by this type of
comprise proteinuria (extra protein existence in the urine) and hypertension. Kidney failure can
also be a late consequence for kids who have Wilms malignant tumour in both kidneys. Kids
with the WAGR syndrome likewise have a greater threat for failure of kidney. Children cured
with stomach surgical treatment can grow scar tissue that upsurges the threat of bowel
obstruction later in life. Symptoms of bowel barrier include stomach pain and vomiting. Some
chemotherapy medicines used to address Wilms tumour, like doxorubicin may have a late
negative impacts on the heart like cardiomyopathy or left ventricular dysfunction. Radiation
treatment to the upper body (chest) can cause difficulties like pulmonary fibrosis and radiation
pneumonitis. Children may develop and grow sluggish (slow) or less than other kids (Wright,
Green, and Daw, 2009).
Personalized medicine
Personalised medicine includes using knowledge about an individual’s cancer to support
diagnose, cure and analyse how fine treatment is functioning (Ko, and Ritchey, 2009). P- Drug is
the global combined project. It targets to enable the shift to adapted/individualised well-being
care delivery through the safe incorporation of pseudonymised medical (Graf et al., 2012),
radiological and rudimentary science datasets and by constructing multi-scale methods and
models (in silico oncology) of malignant tumour. Personalised drug is, in philosophy, evidence-
based and provides individualised drug at the correct time to the correct patient subsequent in
quantifiable improvements in results and a decrease in health care expenses (Ko, and Ritchey,
2009).
Conclusion
Wilms tumour is a type of cancer that affects mostly children. The malignant tumour grows in
one or sometime in bot kidneys of the kids. The main cause of this health condition is genetic
and it passes from parents to children. Approximately 80 to 85 kids affected by this type of
WILMS TUMOUR 11
cancer every year in UK. Genes like WT1 exist at the locus 11p13 and WT2 at the 11p15 are
associated with the occurrence of this type of malignancy. Overproduction of syndrome like
Perlman syndrome, also beckwith-Wiedmann also results in the disease progression. The
children affected by this tumour are born with the genetically altered constitutional pre-zygotic
DNA in the gene. The disease prognosis includes five different stages including the tumour
restricted to kidney, progressed tumour, more advanced progression, spread to other parts of the
body, and progression to new areas of the body with more advanced malignancy. It can be
diagnosed by CT scan, MRI, and biopsy. The treatment option available includes surgery,
chemotherapy, and radiation therapy. The potential treatments include stem cell transplants, and
use of doxorubicin. Late effects of Wilms tumour include kidney failure, bowel obstruction,
pulmonary fibrosis, and slow body growth. Personalized medicine is the concept in order to deal
with Wilms tumour it comprises the knowledge of the patient to help in diagnosis, treats, and
examine whether the treatment was successful or not.
cancer every year in UK. Genes like WT1 exist at the locus 11p13 and WT2 at the 11p15 are
associated with the occurrence of this type of malignancy. Overproduction of syndrome like
Perlman syndrome, also beckwith-Wiedmann also results in the disease progression. The
children affected by this tumour are born with the genetically altered constitutional pre-zygotic
DNA in the gene. The disease prognosis includes five different stages including the tumour
restricted to kidney, progressed tumour, more advanced progression, spread to other parts of the
body, and progression to new areas of the body with more advanced malignancy. It can be
diagnosed by CT scan, MRI, and biopsy. The treatment option available includes surgery,
chemotherapy, and radiation therapy. The potential treatments include stem cell transplants, and
use of doxorubicin. Late effects of Wilms tumour include kidney failure, bowel obstruction,
pulmonary fibrosis, and slow body growth. Personalized medicine is the concept in order to deal
with Wilms tumour it comprises the knowledge of the patient to help in diagnosis, treats, and
examine whether the treatment was successful or not.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 15
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.


