Caboolture/Kilcoy Hospitals Wound Care Program Assignment
VerifiedAdded on 2023/06/08
|42
|8291
|494
Homework Assignment
AI Summary
This assignment solution addresses the Caboolture/Kilcoy Hospitals and Woodford Corrections Health Service Acute Care Transition Support Program's Introduction to Wound Care. The assignment requires the classification of wound types (acute and chronic) based on healing intentions (primary, delayed primary, and secondary). It includes patient case studies, detailing wound assessment, including subjective and objective data, factors affecting tissue integrity, and the aetiology of wounds. Furthermore, the solution covers the review of facility-specific wound management procedures, clinical decision-making frameworks, and the identification of treatment and management goals. The assignment also requires the completion of a wound classification table, detailing clinical appearances like granulation, epithelialization, slough, necrosis, hypergranulation, and exudate types, providing a comprehensive overview of wound care principles and practices.

Caboolture / Kilcoy Hospitals and Woodford Corrections Health Service
Acute Care Transition
Support Program
Introduction to Wound
Care Answer Template
Acute Care Transition
Support Program
Introduction to Wound
Care Answer Template
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Statement of Copyright
© THE STATE OF QUEENSLAND (QUEENSLAND HEALTH) 2019
Statement of Indemnity
Version Control
Authors
Developed by: Kylie Hillier, Nurse Educator Caboolture Hospital
Beth McCauley, Acting Nurse Educator, Royal Brisbane and Women’s
Hospital
Additional support and editing: Kerrie Coleman, Nurse Practitioner, Skin Integrity Services, Royal Brisbane
and Women’s Hospital
Acute Care Transition Support Program Editorial Group
© THE STATE OF QUEENSLAND (QUEENSLAND HEALTH) 2019
Statement of Indemnity
Version Control
Authors
Developed by: Kylie Hillier, Nurse Educator Caboolture Hospital
Beth McCauley, Acting Nurse Educator, Royal Brisbane and Women’s
Hospital
Additional support and editing: Kerrie Coleman, Nurse Practitioner, Skin Integrity Services, Royal Brisbane
and Women’s Hospital
Acute Care Transition Support Program Editorial Group

Unit 1 – Overview of Wound Healing
Modes of Wound Healing
Activity 1
1.1. Discuss and document the different types of wounds that would be
classified as healing by primary intention, delayed primary intention
and secondary intention.
1.2. Select two patients in your care that suit the following requirements:
Patient One: Requires a dressing to a wound that is healing by primary
intention.
Patient 1 : patient 1 is male and 52 years old and he is suffering from the
hypertension from last few year. He has a surgical wound on right hand which
becomes now a ulcer.
Patient Two: Requires a dressing to a wound that is healing by
delayed primary intention or secondary intention.
Patient 2 is male and he is 60 years old. He is also suffering from
diabetes since last several years. He has backbone surgical wound on
his back due to road accident which takes long time to cure.
1.3. Complete Appendix 1, Section One for each patient: Identify and
justify the phase of wound healing that applies to your patient’s wound.
1.4. Complete Appendix 1, Section Two for each patient: Identify and
justify the mode of healing that applies to your patient’s wound.
If access to your allocated patients is limited, or they have been discharged after your
initial assessment, you may draw from past experience or the literature to inform your
case study.
1.1Type answers here
There are two kinds of wounds and are classified on the basis of nature of the wound. The two
kinds of wounds are mentioned below-
Acute wound – it is a type of surgical wound which heals by primary intention. The
traumatic wound heals by secondary intention also comes under acute wounds. It is
caused by trauma and causes damage in tissue. The causes of acute wounds include
heat, electricity, friction, chemical exposure, projectiles and blunt force. Acute wounds do
not need any kind of surgery it can be managed by normal healing and this normal healing
causes closure of wound.
Chronic wound – it is developed when the healing processes don not cause recovery. It
is defined as the wound that is not recovered by the normal healing process. It get stuck in
the inflammation phase. It is caused by poor blood circulation or due to weak immune
system. It develops due to disruption in the normal wound healing cycle. A chronic wound
may be infectious, ischemic, surgical and radiation poisoning.
1.3 and 1.4 Type answers here
PATIENT: 1
Modes of Wound Healing
Activity 1
1.1. Discuss and document the different types of wounds that would be
classified as healing by primary intention, delayed primary intention
and secondary intention.
1.2. Select two patients in your care that suit the following requirements:
Patient One: Requires a dressing to a wound that is healing by primary
intention.
Patient 1 : patient 1 is male and 52 years old and he is suffering from the
hypertension from last few year. He has a surgical wound on right hand which
becomes now a ulcer.
Patient Two: Requires a dressing to a wound that is healing by
delayed primary intention or secondary intention.
Patient 2 is male and he is 60 years old. He is also suffering from
diabetes since last several years. He has backbone surgical wound on
his back due to road accident which takes long time to cure.
1.3. Complete Appendix 1, Section One for each patient: Identify and
justify the phase of wound healing that applies to your patient’s wound.
1.4. Complete Appendix 1, Section Two for each patient: Identify and
justify the mode of healing that applies to your patient’s wound.
If access to your allocated patients is limited, or they have been discharged after your
initial assessment, you may draw from past experience or the literature to inform your
case study.
1.1Type answers here
There are two kinds of wounds and are classified on the basis of nature of the wound. The two
kinds of wounds are mentioned below-
Acute wound – it is a type of surgical wound which heals by primary intention. The
traumatic wound heals by secondary intention also comes under acute wounds. It is
caused by trauma and causes damage in tissue. The causes of acute wounds include
heat, electricity, friction, chemical exposure, projectiles and blunt force. Acute wounds do
not need any kind of surgery it can be managed by normal healing and this normal healing
causes closure of wound.
Chronic wound – it is developed when the healing processes don not cause recovery. It
is defined as the wound that is not recovered by the normal healing process. It get stuck in
the inflammation phase. It is caused by poor blood circulation or due to weak immune
system. It develops due to disruption in the normal wound healing cycle. A chronic wound
may be infectious, ischemic, surgical and radiation poisoning.
1.3 and 1.4 Type answers here
PATIENT: 1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

PATIENT: 2
Include
subjective/objective data
SECTION ONE
Identify and justify the
phase of wound healing
that applies to your
patient’s wound. List anyInflammation □ Justify your assessment: In case of patient 2 Requires a dressing to
a wound that is healing by delayed primary intention or secondary
intention. Patient feel pain and marked redness as well just after the
injury .
Reconstruction
and Regeneration
□ Reconstruction and regeneration process is a healing process in formation
of new tissue occurs but in case of my patient this process is too slow.
Maturation □ In patient 2, at maturation stage the wound was completely closed as the
collagen in the skin is remolded. The collagen are responsible for the
reconstruction of the skin and the skin becomes uneven and thick.
SECTION TWO
Identify and justify the mode
of healing that applies to
Primary Intention □ Justify your assessment:
Delayed Primary
Intention
□
Secondary
intention
□ Patient's wound left open. The wound is left for healing process. The wound
is allowed for healing, filling and closing up naturally. The patient was
treated with regular dressing to the area of injury and after six weeks she
got recovered.
Include
subjective/objective data
SECTION ONE
Identify and justify the
phase of wound healing
that applies to your
patient’s wound. List anyInflammation □ Justify your assessment: In case of patient 2 Requires a dressing to
a wound that is healing by delayed primary intention or secondary
intention. Patient feel pain and marked redness as well just after the
injury .
Reconstruction
and Regeneration
□ Reconstruction and regeneration process is a healing process in formation
of new tissue occurs but in case of my patient this process is too slow.
Maturation □ In patient 2, at maturation stage the wound was completely closed as the
collagen in the skin is remolded. The collagen are responsible for the
reconstruction of the skin and the skin becomes uneven and thick.
SECTION TWO
Identify and justify the mode
of healing that applies to
Primary Intention □ Justify your assessment:
Delayed Primary
Intention
□
Secondary
intention
□ Patient's wound left open. The wound is left for healing process. The wound
is allowed for healing, filling and closing up naturally. The patient was
treated with regular dressing to the area of injury and after six weeks she
got recovered.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Unit 2 – Patient/Wound Assessment
Introduction
Activity 2
2.1 Complete Appendix 1 – Section Three for each patient: Discuss with
your patient their reason for admission and aetiology of their wound.
Document your findings.
2.2 Complete Appendix 1 – Section Four for each patient: List the specific factors
that may affect the tissue integrity and wound healing of each patient.
PATIENT: 1
Include
subjective/objective data
Patient 1 is a 52 years old male .
Who is suffering with
hypertension and also suffering
from the the surgical wound on
his back. Since his wound now
become a ulcer so he required a
good treatment and for this
SECTION THREE
Discuss the reason for
admission with each
patient and the aetiology ofWounds are commonly occurred
due to injury. In case of patient 1
the injury was cause by a minor
accident in which his right hand
gets some cut and scar which
Requires a dressing to a wound
that is healing by primary
intention. in case of patient 2 the
back bone injury caused due to
road accident.
SECTION FOUR
List the specific factors
that may affect the tissue
integrity and wound
Factors: Justification:
Age of the patient My patient was fifty two years old. The older age people have delayed
wound healing where as in young ones healing process takes place rapidly.
In older age people the inflammation response gets decreased.
Introduction
Activity 2
2.1 Complete Appendix 1 – Section Three for each patient: Discuss with
your patient their reason for admission and aetiology of their wound.
Document your findings.
2.2 Complete Appendix 1 – Section Four for each patient: List the specific factors
that may affect the tissue integrity and wound healing of each patient.
PATIENT: 1
Include
subjective/objective data
Patient 1 is a 52 years old male .
Who is suffering with
hypertension and also suffering
from the the surgical wound on
his back. Since his wound now
become a ulcer so he required a
good treatment and for this
SECTION THREE
Discuss the reason for
admission with each
patient and the aetiology ofWounds are commonly occurred
due to injury. In case of patient 1
the injury was cause by a minor
accident in which his right hand
gets some cut and scar which
Requires a dressing to a wound
that is healing by primary
intention. in case of patient 2 the
back bone injury caused due to
road accident.
SECTION FOUR
List the specific factors
that may affect the tissue
integrity and wound
Factors: Justification:
Age of the patient My patient was fifty two years old. The older age people have delayed
wound healing where as in young ones healing process takes place rapidly.
In older age people the inflammation response gets decreased.

Type of wound In patient 1 wound was caused due to road accident and it heals rapidly
because it the minor surgery on his right hand . Types of wound also affect
the speed of recovery. Larger and severe wound takes time for healing
where as wounds caused by small cut or injury heal faster. Circular wound
heals slowest and linear wounds heal faster.
Infection Skin breaks causes bacteria enter into the skin specially at the site of the
injury. My patient's injury was completely covered so the chances of
bacterial infection is negligible.
Chronic diseases My patient was also suffering from diabetes so the healing process got
delayed .
Poor nutrition patient was not taking the diet properly and this made healing delayed.
PATIENT: 2
Include
subjective/objective data
SECTION THREE
Discuss the reason for
admission with each
patient and the aetiology ofIn case of patient 2 the back injury
caused due to road accident by
motorcycle. Due to road accident
the surgical wound is deeper and
severe and it is left open to heal
by itself.
SECTION FOUR
List the specific factors
that may affect the tissue
integrity and wound
Factors: Justification:
because it the minor surgery on his right hand . Types of wound also affect
the speed of recovery. Larger and severe wound takes time for healing
where as wounds caused by small cut or injury heal faster. Circular wound
heals slowest and linear wounds heal faster.
Infection Skin breaks causes bacteria enter into the skin specially at the site of the
injury. My patient's injury was completely covered so the chances of
bacterial infection is negligible.
Chronic diseases My patient was also suffering from diabetes so the healing process got
delayed .
Poor nutrition patient was not taking the diet properly and this made healing delayed.
PATIENT: 2
Include
subjective/objective data
SECTION THREE
Discuss the reason for
admission with each
patient and the aetiology ofIn case of patient 2 the back injury
caused due to road accident by
motorcycle. Due to road accident
the surgical wound is deeper and
severe and it is left open to heal
by itself.
SECTION FOUR
List the specific factors
that may affect the tissue
integrity and wound
Factors: Justification:
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

Age factor Patient 2 was younger and healing becomes easier in younger ones as the
inflammation response is faster.
Poor nutrition As my patient was eating oily and sugary food so wound developed pus and
started paining.
Type of wound As the patient met with road accident the injury was severe and so the
healing may take time.
Infection In case of patient 2 the wound left to heal by itself so there is possibility of
bacterial infection
Chronic disease As patient was healthy there was nothing to worry
Activity 3 3.1 Review the Wound Management Procedure and Wound Management/Assessment
Tool/Pathway for your facility. Discuss the procedure and the tool with your
Preceptor/CN/CF/NE/CNC/NUM. Does your facility have a dedicated wound
management/skin integrity team? If so, review and document their role within the
organisation.
3.1 Complete Appendix 2 for each patient: Undertake a review of each patient and
their medical history and complete the Clinical Decision Making Framework.
PATIENT: 1
Objective Data
Vital Signs: Patient’s Observations
Heart Rate 120 beats per minute
Respiratory Rate 19 breaths per minute
Blood Pressure 90/80 mmHg
Temperature 35 degree Celsius
Oxygen Saturations 92.00%
Relevant
Laboratory/D
Test Results
inflammation response is faster.
Poor nutrition As my patient was eating oily and sugary food so wound developed pus and
started paining.
Type of wound As the patient met with road accident the injury was severe and so the
healing may take time.
Infection In case of patient 2 the wound left to heal by itself so there is possibility of
bacterial infection
Chronic disease As patient was healthy there was nothing to worry
Activity 3 3.1 Review the Wound Management Procedure and Wound Management/Assessment
Tool/Pathway for your facility. Discuss the procedure and the tool with your
Preceptor/CN/CF/NE/CNC/NUM. Does your facility have a dedicated wound
management/skin integrity team? If so, review and document their role within the
organisation.
3.1 Complete Appendix 2 for each patient: Undertake a review of each patient and
their medical history and complete the Clinical Decision Making Framework.
PATIENT: 1
Objective Data
Vital Signs: Patient’s Observations
Heart Rate 120 beats per minute
Respiratory Rate 19 breaths per minute
Blood Pressure 90/80 mmHg
Temperature 35 degree Celsius
Oxygen Saturations 92.00%
Relevant
Laboratory/D
Test Results
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

WBC test: patient WBC count- 3500
normal WBC count- 4500 to
Cholesterol test: patient HDL level- 140
mg/dL
Sugar level: patient glucose level- 130 mg/dL
normal glucose level- 100 mg/dL
Subjective Data Patient one is suffering from hypertension
and a accidental wound on his right hand.
Pain Assessment Pain score of patient 1 is 4 /10 on pain scale.
He feel pain in only surrounding to the
wound and no itching around his wound.
Wound Assessment There are minor cut on patient right hand
from which a liquid exudates ooze out.
Patient/Relative/Carer Reports Patient 1 is suffering from hypertension.
Any additional relevant assessment
data
No
PATIENT: 2
Objective Data
Vital Signs: Patient’s
Observations
Normal Parameters
for patients age
Heart Rate 95 beats per minute 100 beats per minute
Respiratory Rate 18 breaths per minute 20 breaths per minute
Blood Pressure 110/70 mmHg 120/80 mmHg
Temperature 35 degree Celsius 37 degree Celsius
Oxygen Saturations 95.00% 95.00% 95.00%
Relevant Laboratory/Diagnostic Tests
Test Results Normal Parameters
for patients age
WBC test: patient WBC count- 4200
normal WBC count- 4500 to 11000
Cholesterol test: patient HDL level- 132mg/dL
normal HDL level – less than 130 mg/dL
normal WBC count- 4500 to
Cholesterol test: patient HDL level- 140
mg/dL
Sugar level: patient glucose level- 130 mg/dL
normal glucose level- 100 mg/dL
Subjective Data Patient one is suffering from hypertension
and a accidental wound on his right hand.
Pain Assessment Pain score of patient 1 is 4 /10 on pain scale.
He feel pain in only surrounding to the
wound and no itching around his wound.
Wound Assessment There are minor cut on patient right hand
from which a liquid exudates ooze out.
Patient/Relative/Carer Reports Patient 1 is suffering from hypertension.
Any additional relevant assessment
data
No
PATIENT: 2
Objective Data
Vital Signs: Patient’s
Observations
Normal Parameters
for patients age
Heart Rate 95 beats per minute 100 beats per minute
Respiratory Rate 18 breaths per minute 20 breaths per minute
Blood Pressure 110/70 mmHg 120/80 mmHg
Temperature 35 degree Celsius 37 degree Celsius
Oxygen Saturations 95.00% 95.00% 95.00%
Relevant Laboratory/Diagnostic Tests
Test Results Normal Parameters
for patients age
WBC test: patient WBC count- 4200
normal WBC count- 4500 to 11000
Cholesterol test: patient HDL level- 132mg/dL
normal HDL level – less than 130 mg/dL
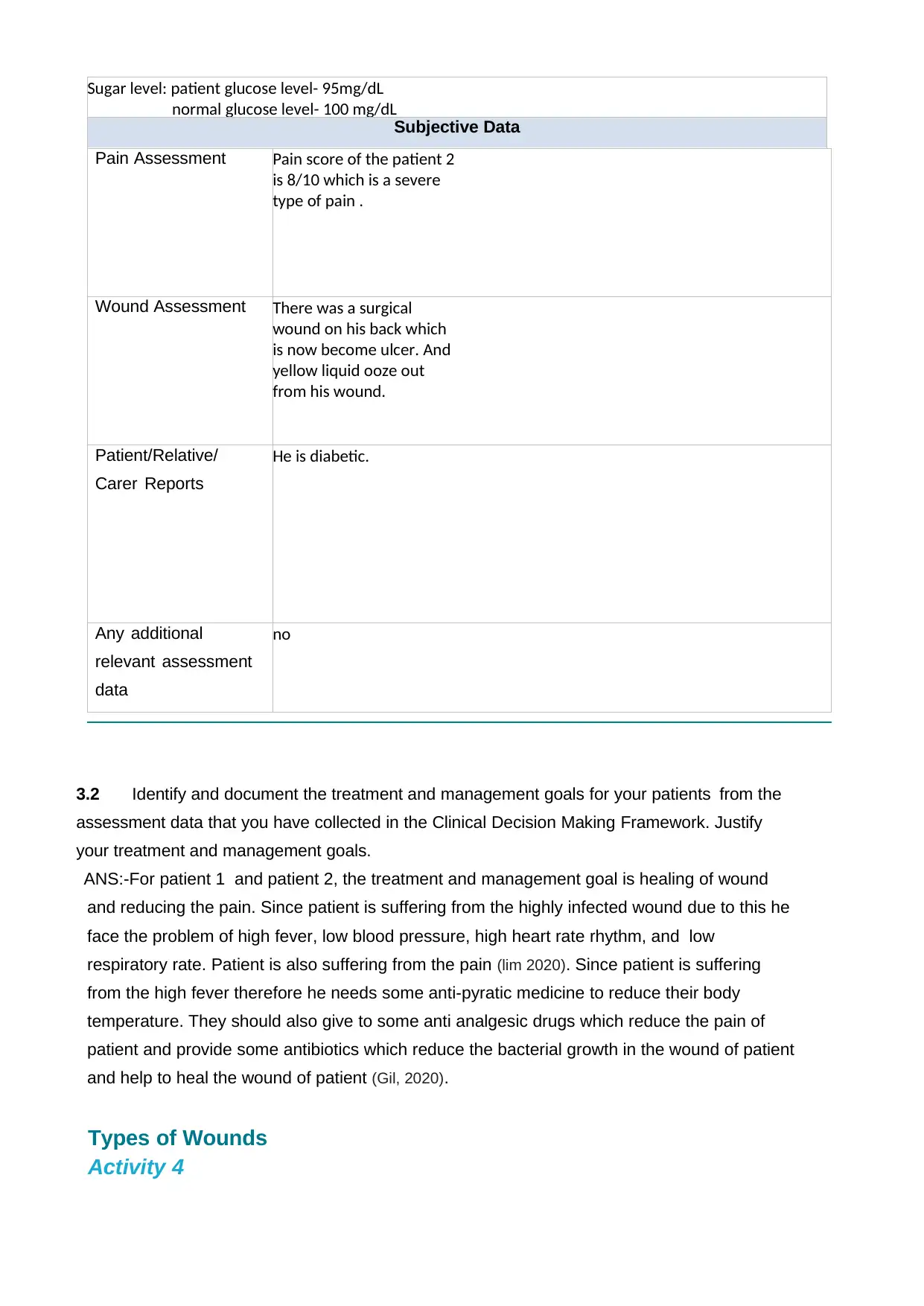
Sugar level: patient glucose level- 95mg/dL
normal glucose level- 100 mg/dL
Subjective Data
Pain Assessment Pain score of the patient 2
is 8/10 which is a severe
type of pain .
Wound Assessment There was a surgical
wound on his back which
is now become ulcer. And
yellow liquid ooze out
from his wound.
Patient/Relative/
Carer Reports
He is diabetic.
Any additional
relevant assessment
data
no
3.2 Identify and document the treatment and management goals for your patients from the
assessment data that you have collected in the Clinical Decision Making Framework. Justify
your treatment and management goals.
ANS:-For patient 1 and patient 2, the treatment and management goal is healing of wound
and reducing the pain. Since patient is suffering from the highly infected wound due to this he
face the problem of high fever, low blood pressure, high heart rate rhythm, and low
respiratory rate. Patient is also suffering from the pain (lim 2020). Since patient is suffering
from the high fever therefore he needs some anti-pyratic medicine to reduce their body
temperature. They should also give to some anti analgesic drugs which reduce the pain of
patient and provide some antibiotics which reduce the bacterial growth in the wound of patient
and help to heal the wound of patient (Gil, 2020).
Types of Wounds
Activity 4
normal glucose level- 100 mg/dL
Subjective Data
Pain Assessment Pain score of the patient 2
is 8/10 which is a severe
type of pain .
Wound Assessment There was a surgical
wound on his back which
is now become ulcer. And
yellow liquid ooze out
from his wound.
Patient/Relative/
Carer Reports
He is diabetic.
Any additional
relevant assessment
data
no
3.2 Identify and document the treatment and management goals for your patients from the
assessment data that you have collected in the Clinical Decision Making Framework. Justify
your treatment and management goals.
ANS:-For patient 1 and patient 2, the treatment and management goal is healing of wound
and reducing the pain. Since patient is suffering from the highly infected wound due to this he
face the problem of high fever, low blood pressure, high heart rate rhythm, and low
respiratory rate. Patient is also suffering from the pain (lim 2020). Since patient is suffering
from the high fever therefore he needs some anti-pyratic medicine to reduce their body
temperature. They should also give to some anti analgesic drugs which reduce the pain of
patient and provide some antibiotics which reduce the bacterial growth in the wound of patient
and help to heal the wound of patient (Gil, 2020).
Types of Wounds
Activity 4
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

4.1 Based on your reading, complete the Wound Classification table. If the Wound
Management/Assessment Tool/Pathway at your facility has different/more
descriptive sections, then please include them.
Table 1 - Wound Classification
Clinical Appearance Description
Granulation A granulation tissue which is healthy is pink or red in color, which is
a good indicator of healing. Unhealthy granulation is dusky red, dark,
bleeds easily and may indicates the presence of wound infection.
Epithelialisation It is the final phase of proliferation stage of wound healing, or
epithelial cells resurface or injury.
Slough It refers to white or yellow material in the wound bed. It is generally
wet but may be dry. Consist dead cells which accumulate in the
wound exudation.
Necrosis There are different types of necrotic tissue which is present in the
form of eschar and slough. Slough is characterized as being tan,
green, yellow or brown colour which may be loose, moist and stringy
in appearance. Eschar presents as thick, dry leathery tissue which is
Hypergranulation Excess granulation is also known as proud flesh or hypergranulation.
The wound tissue will evident above the normal bed of wound. It is
generally friable and bleeds.
Management/Assessment Tool/Pathway at your facility has different/more
descriptive sections, then please include them.
Table 1 - Wound Classification
Clinical Appearance Description
Granulation A granulation tissue which is healthy is pink or red in color, which is
a good indicator of healing. Unhealthy granulation is dusky red, dark,
bleeds easily and may indicates the presence of wound infection.
Epithelialisation It is the final phase of proliferation stage of wound healing, or
epithelial cells resurface or injury.
Slough It refers to white or yellow material in the wound bed. It is generally
wet but may be dry. Consist dead cells which accumulate in the
wound exudation.
Necrosis There are different types of necrotic tissue which is present in the
form of eschar and slough. Slough is characterized as being tan,
green, yellow or brown colour which may be loose, moist and stringy
in appearance. Eschar presents as thick, dry leathery tissue which is
Hypergranulation Excess granulation is also known as proud flesh or hypergranulation.
The wound tissue will evident above the normal bed of wound. It is
generally friable and bleeds.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Exudate Type
Serous Any semisolid fluid which has oozed out of a damaged tissue or its
capillaries, it is very specifically because it is characterized by high
protein and the white blood cells. It is secreted through the inflamed
Haemoserous It is the type of drainage of watery, pink colored fluid, drainage of a
thin composed of serum and blood. This kind of ooze of any wounds
Sanguineous Sanguineous exudate is the indication of trauma to blood vessels. A
bleeding which is fresh, seen in full thickness wound and in ddep
partial wound.
Purulent It is a opaque and thick exudate which is tan , green,yellow or brown
in color.
Haemopurulent It is Thin, watery and cloudy and yellow in color.
Wound Edge Description
Normal Indicate wound completely heal.
Colour Pink edges indicates growth of new tissue
Raised Indicate hyper-granulation.
Rolled Indicate hyper-granulation.
Contraction Coming together indicate healing process
Sensation Increased pain or absence of sensation lead further treatment.
Surrounding Skin Description
Erythema It indicates healing process occur. Redness process.
Serous Any semisolid fluid which has oozed out of a damaged tissue or its
capillaries, it is very specifically because it is characterized by high
protein and the white blood cells. It is secreted through the inflamed
Haemoserous It is the type of drainage of watery, pink colored fluid, drainage of a
thin composed of serum and blood. This kind of ooze of any wounds
Sanguineous Sanguineous exudate is the indication of trauma to blood vessels. A
bleeding which is fresh, seen in full thickness wound and in ddep
partial wound.
Purulent It is a opaque and thick exudate which is tan , green,yellow or brown
in color.
Haemopurulent It is Thin, watery and cloudy and yellow in color.
Wound Edge Description
Normal Indicate wound completely heal.
Colour Pink edges indicates growth of new tissue
Raised Indicate hyper-granulation.
Rolled Indicate hyper-granulation.
Contraction Coming together indicate healing process
Sensation Increased pain or absence of sensation lead further treatment.
Surrounding Skin Description
Erythema It indicates healing process occur. Redness process.

Oedematous Tissue with excess of interstitial fluid.
Macerated Soften the tissue indicates healing process.
Cellulitis It is common , serious ,potential bacterial skin infectious wounds.
Fragile/Thin Porous tissue which becomes permeable for exudates
Dry/Scaly Indicates wound healing process occur.
Dermatitis/Eczema It is broken tissue wound treated by the topical steroid.
Induration Abnormal hardening of tissue which is caused due to the
consolidation of the edema.
Skin Tears
Activity 5 5.1 Locate the STAR tool in your work area. Using the tool, categories the
following skin tears and describe their features.
thi
Category 1a
This is category 1a type skin tear where the edges of
wound can be realigned to the normal anatomical
position without undue stretching and the skin flap color
is not pale dusky or darkened.
Macerated Soften the tissue indicates healing process.
Cellulitis It is common , serious ,potential bacterial skin infectious wounds.
Fragile/Thin Porous tissue which becomes permeable for exudates
Dry/Scaly Indicates wound healing process occur.
Dermatitis/Eczema It is broken tissue wound treated by the topical steroid.
Induration Abnormal hardening of tissue which is caused due to the
consolidation of the edema.
Skin Tears
Activity 5 5.1 Locate the STAR tool in your work area. Using the tool, categories the
following skin tears and describe their features.
thi
Category 1a
This is category 1a type skin tear where the edges of
wound can be realigned to the normal anatomical
position without undue stretching and the skin flap color
is not pale dusky or darkened.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 42
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





