Wound Healing Assessment Chart: Developing a Structured Wound Measurement Tool
VerifiedAdded on 2023/06/03
|17
|4672
|334
AI Summary
This article discusses the importance of wound assessment in wound management and the development of a wound healing assessment chart. It includes the professional team involved, the inclusion and exclusion criteria, and the TIME acronym for wound bed assessment. The article also emphasizes the importance of pain assessment and the cost-effectiveness of evidence-based interventions.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running Header; WOUND HEALING ASSESSMENT CHART.
1
WOUND HEALING ASSESSMENT CHART.
Student’s name
Institutional affiliation
Course name
Date
1
WOUND HEALING ASSESSMENT CHART.
Student’s name
Institutional affiliation
Course name
Date
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
.
WOUND HEALING ASSESSMENT CHART.
2
Introduction
Skin is the largest organ of the body. It makes up to 16% of the body’s weight. It serves
several vital functions: immune function, temperature regulation sensation, synthesis of vitamin
D. The skin is a dynamic organ that is constantly changing. It constantly sheds off and gets
replaced by the inner layer. A wound develops when the skin tissue gets damaged by trauma.
This compromises its functioning (Menna, 2017). Wound assessment plays an important role in
wound management as it facilitates in identifying factors that may be preventing wounds from
healing. However, wound assessments are often subjective and is practitioner reliant, the
information collected can vary dependent on skill and education of the individual. In wound
assessment consistency can be difficult as assessments such as pain, size of the wound, exudate
and odor can vary between clinicians (Fletcher, 2007). A structured wound measurement tool
can remove imprecise terms and measurement techniques.
This assignment will focus on developing a wound assessment chart. This charts’
appropriateness will be described in terms of the workplace, the patient group and the size of the
work setting. Secondly, a description of the professional group working at the setting and its
consideration in developing the chart. Thirdly, a justification of developing the wound
assessment chart. Fourthly, consideration of the documentation, can it stand by its own or is it
part of the hospital. Fifthly, ensure that the chart is user friendly. Sixthly, come up with a
rationale of the inclusion and the exclusion of each characteristic when developing the chart.
That is a discuss on the inclusion and exclusion criteria of a wound assessment chart used in a
private podiatry practice (Krasner, 1992). Lastly, a summary of the assignment.
WOUND HEALING ASSESSMENT CHART.
2
Introduction
Skin is the largest organ of the body. It makes up to 16% of the body’s weight. It serves
several vital functions: immune function, temperature regulation sensation, synthesis of vitamin
D. The skin is a dynamic organ that is constantly changing. It constantly sheds off and gets
replaced by the inner layer. A wound develops when the skin tissue gets damaged by trauma.
This compromises its functioning (Menna, 2017). Wound assessment plays an important role in
wound management as it facilitates in identifying factors that may be preventing wounds from
healing. However, wound assessments are often subjective and is practitioner reliant, the
information collected can vary dependent on skill and education of the individual. In wound
assessment consistency can be difficult as assessments such as pain, size of the wound, exudate
and odor can vary between clinicians (Fletcher, 2007). A structured wound measurement tool
can remove imprecise terms and measurement techniques.
This assignment will focus on developing a wound assessment chart. This charts’
appropriateness will be described in terms of the workplace, the patient group and the size of the
work setting. Secondly, a description of the professional group working at the setting and its
consideration in developing the chart. Thirdly, a justification of developing the wound
assessment chart. Fourthly, consideration of the documentation, can it stand by its own or is it
part of the hospital. Fifthly, ensure that the chart is user friendly. Sixthly, come up with a
rationale of the inclusion and the exclusion of each characteristic when developing the chart.
That is a discuss on the inclusion and exclusion criteria of a wound assessment chart used in a
private podiatry practice (Krasner, 1992). Lastly, a summary of the assignment.
.
WOUND HEALING ASSESSMENT CHART.
3
The professional team.
Podiatrist treat foot and lower limb conditions including diabetic and foot ulcers (QUT
website). Podiatrists in a multidisciplinary team are involved in primary prevention and
management of diabetes related foot complications including foot ulcers (Lazzarini, 2014).
Evidence has shown that early prevention, education for patient and staff, treatment from a
multidisciplinary team can reduce amputation rates by 49-85% (Andrews, Houdek, & Kiemele,
2015). Management strategies that are often implemented by podiatrist include sharps
debridement, dressing changes and offloading the pressures on the wounded foot (Gibson et al,
2013). A variation of disciplines makes up a multidisciplinary team, those involved typically are
vascular surgeons, endocrinologist, orthopaedic surgeons, nurse specialist, podiatrist and
orthotists (Buggy & Moore, 2017). It is therefore important to have a reliable assessment tool
with consistent language to assist in the share care and collaboration of health professionals.
New chart/improving on existing chart
The Queensland High Risk Foot Form (QHRFF) was a tool developed to capture risk
factors, assess foot wounds, and analyse patient outcomes in a hospital setting. The QHRFF
assessment tool showed majority of the criteria to be moderate in validity and reliability,
however, the authors states that a systematic literature review was not performed and was limited
to podiatrists only to test the inter-reliability of the tool.
For podiatrist in private clinics, often working on their own and can be limited with time
and funding an assessment tool was improved to suit their needs. The assessment tool needed to
be time efficient and had instruction on how to assess high risk foot, improve so as to suit private
WOUND HEALING ASSESSMENT CHART.
3
The professional team.
Podiatrist treat foot and lower limb conditions including diabetic and foot ulcers (QUT
website). Podiatrists in a multidisciplinary team are involved in primary prevention and
management of diabetes related foot complications including foot ulcers (Lazzarini, 2014).
Evidence has shown that early prevention, education for patient and staff, treatment from a
multidisciplinary team can reduce amputation rates by 49-85% (Andrews, Houdek, & Kiemele,
2015). Management strategies that are often implemented by podiatrist include sharps
debridement, dressing changes and offloading the pressures on the wounded foot (Gibson et al,
2013). A variation of disciplines makes up a multidisciplinary team, those involved typically are
vascular surgeons, endocrinologist, orthopaedic surgeons, nurse specialist, podiatrist and
orthotists (Buggy & Moore, 2017). It is therefore important to have a reliable assessment tool
with consistent language to assist in the share care and collaboration of health professionals.
New chart/improving on existing chart
The Queensland High Risk Foot Form (QHRFF) was a tool developed to capture risk
factors, assess foot wounds, and analyse patient outcomes in a hospital setting. The QHRFF
assessment tool showed majority of the criteria to be moderate in validity and reliability,
however, the authors states that a systematic literature review was not performed and was limited
to podiatrists only to test the inter-reliability of the tool.
For podiatrist in private clinics, often working on their own and can be limited with time
and funding an assessment tool was improved to suit their needs. The assessment tool needed to
be time efficient and had instruction on how to assess high risk foot, improve so as to suit private
.
WOUND HEALING ASSESSMENT CHART.
4
practice, stand on its on in documentation and have instructions on how to use the chart
(Greatrix-White & Moxey 2015).
The wound healing assessment chart.
Greatrix-White & Moxey (2015) study reported that nurses are not confident in
developing a wound management plan and executing it out. The study suggested that for best
practice in wound management, nurses required a structured assessment tool and educational
guidelines with a clear guideline.
The inclusion/exclusion
Patient’s details/ medical history
The primary/basic level in contact with the patient, the patient’s details are important in
identification purpose. They match the patient and the wound assessment to be done. Secondly,
the wound assessment is a holistic assessment and in order to ensure that its holistic the patients
detail and condition are important. The patient’s comorbidities that could affect the wound
healing should be recorded. This will allow the healthcare to put them into consideration when
planning their wound management (Menna, 2017).
The site and the size of the wound.
Grey et al., (2006) identification and recording the wound site is important, especially if
there is more than one area of skin breakdown. In addition to this, the site of wound is important
in the diagnosis of an underlying ailment that could be associated with the wound development.
WOUND HEALING ASSESSMENT CHART.
4
practice, stand on its on in documentation and have instructions on how to use the chart
(Greatrix-White & Moxey 2015).
The wound healing assessment chart.
Greatrix-White & Moxey (2015) study reported that nurses are not confident in
developing a wound management plan and executing it out. The study suggested that for best
practice in wound management, nurses required a structured assessment tool and educational
guidelines with a clear guideline.
The inclusion/exclusion
Patient’s details/ medical history
The primary/basic level in contact with the patient, the patient’s details are important in
identification purpose. They match the patient and the wound assessment to be done. Secondly,
the wound assessment is a holistic assessment and in order to ensure that its holistic the patients
detail and condition are important. The patient’s comorbidities that could affect the wound
healing should be recorded. This will allow the healthcare to put them into consideration when
planning their wound management (Menna, 2017).
The site and the size of the wound.
Grey et al., (2006) identification and recording the wound site is important, especially if
there is more than one area of skin breakdown. In addition to this, the site of wound is important
in the diagnosis of an underlying ailment that could be associated with the wound development.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
.
WOUND HEALING ASSESSMENT CHART.
5
In the case of diabetic foot ulcer, they arise in the areas of abnormal distribution of pressure
while the venous ulcers develop in the gaiter area of the leg.
Every wound needs to be reassessed and measured each time it gets dressed. Since it is a
nursing procedure documentation of the findings should be recorded. To assess the depth of the
wound, the measurements starts from the epidermis to the part that is deepest. Grey et al., (2006)
suggested that to get the margins of the wounds a transparent acetate sheets and estimate the
surface area. This should be done every time the wound is dressed. It forms the baseline to be
referred for wound healing progresses.
Factors affecting wound healing.
I. Nutritional assessment
The following factors influences wound healing: nutrition status of the patient, present
medication of the patient and the aetiology of the wound. Good nutritional support promotes the
healing of the wound. When the patient is malnourished there is delays, complicates and inhibits
the healing process (Williams & Leaper 2010). It is therefore important to assess the nutritional
status of the patient with a wound and it should be recorded. In case of inadequacy, health
promotion should be offered and also the patient should be referred to a dietitian. The tools to
assess nutritional status includes the malnutrition universal screening tool (MUST), body mass
index (BMI).
WOUND HEALING ASSESSMENT CHART.
5
In the case of diabetic foot ulcer, they arise in the areas of abnormal distribution of pressure
while the venous ulcers develop in the gaiter area of the leg.
Every wound needs to be reassessed and measured each time it gets dressed. Since it is a
nursing procedure documentation of the findings should be recorded. To assess the depth of the
wound, the measurements starts from the epidermis to the part that is deepest. Grey et al., (2006)
suggested that to get the margins of the wounds a transparent acetate sheets and estimate the
surface area. This should be done every time the wound is dressed. It forms the baseline to be
referred for wound healing progresses.
Factors affecting wound healing.
I. Nutritional assessment
The following factors influences wound healing: nutrition status of the patient, present
medication of the patient and the aetiology of the wound. Good nutritional support promotes the
healing of the wound. When the patient is malnourished there is delays, complicates and inhibits
the healing process (Williams & Leaper 2010). It is therefore important to assess the nutritional
status of the patient with a wound and it should be recorded. In case of inadequacy, health
promotion should be offered and also the patient should be referred to a dietitian. The tools to
assess nutritional status includes the malnutrition universal screening tool (MUST), body mass
index (BMI).
.
WOUND HEALING ASSESSMENT CHART.
6
II. Medication
The anti-coagulants and anti-platelets drugs interferes with the clotting process which negatively
affects the wound healing process. medications such as non-steroidal anti-inflammatory drugs
(NSAIDs), corticosteroids, and disease modifying anti-rheumatic drugs (DMARDs) they lowers
the immunity levels which increases the infection rates affecting the healing process (Fletcher,
2010).
III. Etiology of the wound.
Etiology of the wound is important in planning the care of the wound and in assessing its healing
progress. In case the wound is as a result of diabetes mellitus the healing progress is expected to
increase slowly and gradually and its management includes controlling the blood sugars. In case
it’s as a result of sickle cell/sickle ulcers, the management revolves around managing sickle cell
disease (Fletcher, 2010).
Exudate
An infected wound produces purulent discharge. For effective wound healing, this discharge has
to be controlled. The wound environment has to be kept warm and moist so as to ensure effective
healing (Winter 2012) and also prevent skin maceration. A healthy exudate is normally clear and
amber colored and has no odor. It becomes malodorous as the wound bacterial infection
increases.
The changes in the characteristics of the exudate should be reported. Increase in protein content
is associated with infection and also it is associated with the exudate being sticky and thick.
WOUND HEALING ASSESSMENT CHART.
6
II. Medication
The anti-coagulants and anti-platelets drugs interferes with the clotting process which negatively
affects the wound healing process. medications such as non-steroidal anti-inflammatory drugs
(NSAIDs), corticosteroids, and disease modifying anti-rheumatic drugs (DMARDs) they lowers
the immunity levels which increases the infection rates affecting the healing process (Fletcher,
2010).
III. Etiology of the wound.
Etiology of the wound is important in planning the care of the wound and in assessing its healing
progress. In case the wound is as a result of diabetes mellitus the healing progress is expected to
increase slowly and gradually and its management includes controlling the blood sugars. In case
it’s as a result of sickle cell/sickle ulcers, the management revolves around managing sickle cell
disease (Fletcher, 2010).
Exudate
An infected wound produces purulent discharge. For effective wound healing, this discharge has
to be controlled. The wound environment has to be kept warm and moist so as to ensure effective
healing (Winter 2012) and also prevent skin maceration. A healthy exudate is normally clear and
amber colored and has no odor. It becomes malodorous as the wound bacterial infection
increases.
The changes in the characteristics of the exudate should be reported. Increase in protein content
is associated with infection and also it is associated with the exudate being sticky and thick.
.
WOUND HEALING ASSESSMENT CHART.
7
When the exudate is thin and runny, it may be as a result of low protein content which is
associated with venous congestion, cardiac disease or malnutrition (White & Cutting, 2016).
It is therefore important for the health practitioner assessing the wound healing to assess the
exudate; colour, consistency, odor and the amount. Measuring and recording the amount of the
exudate of a wound at times is difficult. To make it easy, the dressing used should be assessed in
terms of being soiled. The observations made can be indicative of exudate levels increasing,
remaining static or decreasing (White & Cutting, 2016).
For effective wound treatment, the nursing management should focus on finding out the
etiology of the wound. Secondly, identify the comorbidities or/and complications that would
contribute to the wound development or delayed wound healing. Thirdly, assessing the status of
the wound. Lastly, develop a wound management plan (White & Cutting, 2016).
Wound bed appearance.
To assess this the international advisory board on wound bed assessment formulated the
TIME acronym to aid the health care providers with a tool that enables the systematic approach
to the wound management. The acronym is important as it optimizes the wound bed by reducing
the exudate and moisture which reduces the bacterial burden and corrects any abnormalities that
may be present (Williams & Leaper 2010). The acronym TIME:
a) Tissue
The wound bed tissue should be assessed and identified, where the tissue is deficient and
non-viable there is delayed in healing. The removal of this tissue is vital in facilitating wound
WOUND HEALING ASSESSMENT CHART.
7
When the exudate is thin and runny, it may be as a result of low protein content which is
associated with venous congestion, cardiac disease or malnutrition (White & Cutting, 2016).
It is therefore important for the health practitioner assessing the wound healing to assess the
exudate; colour, consistency, odor and the amount. Measuring and recording the amount of the
exudate of a wound at times is difficult. To make it easy, the dressing used should be assessed in
terms of being soiled. The observations made can be indicative of exudate levels increasing,
remaining static or decreasing (White & Cutting, 2016).
For effective wound treatment, the nursing management should focus on finding out the
etiology of the wound. Secondly, identify the comorbidities or/and complications that would
contribute to the wound development or delayed wound healing. Thirdly, assessing the status of
the wound. Lastly, develop a wound management plan (White & Cutting, 2016).
Wound bed appearance.
To assess this the international advisory board on wound bed assessment formulated the
TIME acronym to aid the health care providers with a tool that enables the systematic approach
to the wound management. The acronym is important as it optimizes the wound bed by reducing
the exudate and moisture which reduces the bacterial burden and corrects any abnormalities that
may be present (Williams & Leaper 2010). The acronym TIME:
a) Tissue
The wound bed tissue should be assessed and identified, where the tissue is deficient and
non-viable there is delayed in healing. The removal of this tissue is vital in facilitating wound
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
.
WOUND HEALING ASSESSMENT CHART.
8
healing. In addition to this, devitalized tissue not only does it prevent the wound healing but it
also increases the wound infection. In case of necrotic tissues, (eschars) they should be removed
so as to facilitate healing. Lastly, slough a yellow fibrinous tissues which contains fibrin, pus and
dead cells lengthens the process of inflammation and it prevents the proliferative phase of wound
healing (Stephen-Hayes & Thompson, 2017). To promote healing the slough should be removed.
b) Infection/ inflammation
If the wound is infected the wound requires treatment and also the wound healing process is
delayed. It causes pain and discomfort to the patient. Through critical colonization all wounds
contain bacterial infection. Cooper (2015) reported that the diagnosis of bacterial wound
infection is a task for a clinical skill. The microbiology data obtained should be used to aid in
formulating the clinical diagnosis. The wound swabs should be taken and appropriate antibiotics
administered.
c) Moisture imbalance
Moisture is important in wound healing as it enhances the autolytic process. It also acts as a
medium for the transport of the growth factors that are essential during the epithelization phase
of wound healing (Cutting & Tong 2014). When the wound dries, a scab forms which causes
wound contraction that delays the wound healing. When the wound gets so wet, the exudate
damages the peri-wound skin that causes maceration. The choice of the wound dressing material
so as to have the correct amount of moisture retained is important so as to enhance wound
dressing.
WOUND HEALING ASSESSMENT CHART.
8
healing. In addition to this, devitalized tissue not only does it prevent the wound healing but it
also increases the wound infection. In case of necrotic tissues, (eschars) they should be removed
so as to facilitate healing. Lastly, slough a yellow fibrinous tissues which contains fibrin, pus and
dead cells lengthens the process of inflammation and it prevents the proliferative phase of wound
healing (Stephen-Hayes & Thompson, 2017). To promote healing the slough should be removed.
b) Infection/ inflammation
If the wound is infected the wound requires treatment and also the wound healing process is
delayed. It causes pain and discomfort to the patient. Through critical colonization all wounds
contain bacterial infection. Cooper (2015) reported that the diagnosis of bacterial wound
infection is a task for a clinical skill. The microbiology data obtained should be used to aid in
formulating the clinical diagnosis. The wound swabs should be taken and appropriate antibiotics
administered.
c) Moisture imbalance
Moisture is important in wound healing as it enhances the autolytic process. It also acts as a
medium for the transport of the growth factors that are essential during the epithelization phase
of wound healing (Cutting & Tong 2014). When the wound dries, a scab forms which causes
wound contraction that delays the wound healing. When the wound gets so wet, the exudate
damages the peri-wound skin that causes maceration. The choice of the wound dressing material
so as to have the correct amount of moisture retained is important so as to enhance wound
dressing.
.
WOUND HEALING ASSESSMENT CHART.
9
d) Edge of the wound
The failure of the wound to heal can be deduced through the lack of improvement on the
wound dimensions. Secondly, the failure of the edges of epidermal improve as times goes by. An
undermined margin of the wound is indicative of wound infection or as a result of critical
colonization. If this is the case the wound requires reassessment and the current treatment should
have reassessed too. In addition, the patient can be referred to a tissue viable specialist for
appropriate advice on the wound management (White & Cutting 2016).
Pain
Patients with wounds suffers with pain. Solowiej et al., (2010) they experience different
type of pain that occurs resulting from the chronic wound, this includes neuropathic pain, the
pain as a result of the treatment of the wound and the anticipatory pain. It is important to assess
the patient’s pain as it is essential in planning the patient’s care as it provides the health care
provider with the baseline information important in selecting the management strategies that are
appropriate and the appropriate dressing products.
Unresolved pain causes stress to the patient that results in delays in wound healing
(Reddy et al., 2013). Psychological stress has been found to have negative impacts on healing in
different settings and wound types. The studies have shown psychological stress impair wound
healing by decreasing local pro-inflammatory cytokines. The health care provider should explain
all procedures to the patients so as to alleviate the patients stress/anxiety. During dressing
procedure, the patient should only feel some sensation. The aim of this is to limit both the pain
and the discomfort to its minimum and also to ensure that the patient is involved in their care
WOUND HEALING ASSESSMENT CHART.
9
d) Edge of the wound
The failure of the wound to heal can be deduced through the lack of improvement on the
wound dimensions. Secondly, the failure of the edges of epidermal improve as times goes by. An
undermined margin of the wound is indicative of wound infection or as a result of critical
colonization. If this is the case the wound requires reassessment and the current treatment should
have reassessed too. In addition, the patient can be referred to a tissue viable specialist for
appropriate advice on the wound management (White & Cutting 2016).
Pain
Patients with wounds suffers with pain. Solowiej et al., (2010) they experience different
type of pain that occurs resulting from the chronic wound, this includes neuropathic pain, the
pain as a result of the treatment of the wound and the anticipatory pain. It is important to assess
the patient’s pain as it is essential in planning the patient’s care as it provides the health care
provider with the baseline information important in selecting the management strategies that are
appropriate and the appropriate dressing products.
Unresolved pain causes stress to the patient that results in delays in wound healing
(Reddy et al., 2013). Psychological stress has been found to have negative impacts on healing in
different settings and wound types. The studies have shown psychological stress impair wound
healing by decreasing local pro-inflammatory cytokines. The health care provider should explain
all procedures to the patients so as to alleviate the patients stress/anxiety. During dressing
procedure, the patient should only feel some sensation. The aim of this is to limit both the pain
and the discomfort to its minimum and also to ensure that the patient is involved in their care
.
WOUND HEALING ASSESSMENT CHART.
10
plan. The assessment includes; initial assessment, background pain and review assessment. The
pain levels of the patient should be recorded so as to be able to identify the pain patterns.
Evaluation
Posnett & Franks, (2017) the wound care is a costly area of treatment, it costs the
National Health Services (NHS) between 2 and 3 billion a year. It is important to understand the
wound assessment and management as it is important in ensuring that the care is cost-effective
and evidence based interventions. The nurses need to develop accurate wound assessment and be
able to identify the related areas of care that requires attention (Harding et al., 2008). The wound
assessment should be holistic. Accurate wound assessment is an essential skill that should be
acquired by the health care providers so as to effectively plan, implement and evaluate care for
patients.
In addition, Greatrix-White & Moxey (2015) study reported that nurses are not confident in
developing a wound management plan and executing it out. The study suggested that for best
practice in wound management, nurses required a structured assessment tool and educational
guidelines with a clear guideline.
Discussion
As started above the wound healing assessment chart ensures that the assessment ensures
that there is holistic care. This is obtained by not only focusing on the wound but by focusing on
the patient as an individual (Cooper, 2015). The chart inclusion includes; the patient history, the
size and site of wound, the factors affecting wound healing, the patients pain, and the wound bed
appearance. The patient history is important in patient identification. It is also important in the
WOUND HEALING ASSESSMENT CHART.
10
plan. The assessment includes; initial assessment, background pain and review assessment. The
pain levels of the patient should be recorded so as to be able to identify the pain patterns.
Evaluation
Posnett & Franks, (2017) the wound care is a costly area of treatment, it costs the
National Health Services (NHS) between 2 and 3 billion a year. It is important to understand the
wound assessment and management as it is important in ensuring that the care is cost-effective
and evidence based interventions. The nurses need to develop accurate wound assessment and be
able to identify the related areas of care that requires attention (Harding et al., 2008). The wound
assessment should be holistic. Accurate wound assessment is an essential skill that should be
acquired by the health care providers so as to effectively plan, implement and evaluate care for
patients.
In addition, Greatrix-White & Moxey (2015) study reported that nurses are not confident in
developing a wound management plan and executing it out. The study suggested that for best
practice in wound management, nurses required a structured assessment tool and educational
guidelines with a clear guideline.
Discussion
As started above the wound healing assessment chart ensures that the assessment ensures
that there is holistic care. This is obtained by not only focusing on the wound but by focusing on
the patient as an individual (Cooper, 2015). The chart inclusion includes; the patient history, the
size and site of wound, the factors affecting wound healing, the patients pain, and the wound bed
appearance. The patient history is important in patient identification. It is also important in the
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
.
WOUND HEALING ASSESSMENT CHART.
11
holistic care. The size and the site of the patient’s wound is important in assessing the wound
healing. The factors affecting wound healing are important to assess as they help in
understanding the wound healing progress and in planning the wound management as they can
be eliminated. In addition, the wound bed appearance is important in assessing the patient’s
wound healing. Lastly, the former is important as it helps in identifying the dressing materials
and regime. All the above are important as they trace the wound healing progress and the
outcome (Menna Lloyd, 2017).
Conclusion.
In conclusion the wound healing assessment chart includes a lot of documentation,
therefore it can stand alone. The chart is also detailed and it ensures that the patient care is
holistic. The wound healing assessment chart includes; the patient history, the size and site of
wound, the factors affecting wound healing, the patients pain, and the wound bed appearance.
The patient history is important in patient identification. The size and the site of the patient’s
wound is important in assessing the wound healing. The factors affecting wound healing are
important to assess as they help in understanding the wound healing progress and in planning the
wound management as they can be eliminated. The chart can also be interpreted by different
health care providers therefore it friendly. Lastly, it entails a detailed documentation which
makes it qualify as a document that can stand by itself.
WOUND HEALING ASSESSMENT CHART.
11
holistic care. The size and the site of the patient’s wound is important in assessing the wound
healing. The factors affecting wound healing are important to assess as they help in
understanding the wound healing progress and in planning the wound management as they can
be eliminated. In addition, the wound bed appearance is important in assessing the patient’s
wound healing. Lastly, the former is important as it helps in identifying the dressing materials
and regime. All the above are important as they trace the wound healing progress and the
outcome (Menna Lloyd, 2017).
Conclusion.
In conclusion the wound healing assessment chart includes a lot of documentation,
therefore it can stand alone. The chart is also detailed and it ensures that the patient care is
holistic. The wound healing assessment chart includes; the patient history, the size and site of
wound, the factors affecting wound healing, the patients pain, and the wound bed appearance.
The patient history is important in patient identification. The size and the site of the patient’s
wound is important in assessing the wound healing. The factors affecting wound healing are
important to assess as they help in understanding the wound healing progress and in planning the
wound management as they can be eliminated. The chart can also be interpreted by different
health care providers therefore it friendly. Lastly, it entails a detailed documentation which
makes it qualify as a document that can stand by itself.
.
WOUND HEALING ASSESSMENT CHART.
12
References
Cooper R., (2015). Identifying Criteria for Wound Infection. Medical Education Partnership Ltd,
London.
Cutting K, Tong A (2013). Wound Physiology and Moist Wound Healing. Medical
Communications Ltd, Holsworthy.
European Wound Management Association (2008.) Hard-to-Heal Wounds: A Holistic Approach.
http://tiny.cc/pjvcc (accessed 28 April 2011)
Fletcher J (2010). Development of a new wound assessment form. Wounds UK 6(1): 92–9
Grey JE, Enoch S, Harding K (2006). Wound assessment. BMJ, 332(7536): 285–8
Harding KG et al (2018) Best Practice Statement. Optimising Wound Care. http://tiny.cc/7jwgp
(accessed 9 April 2011).
Maylor M (2012) Are wound care assessments real or imaginary and what can be done? Br J
Nurs11(12): S5
McIntosh C, Ousey K (2008) A survey of nurses’ and podiatrists’ attitudes, skills and knowledge
of lower extremity wound care. Wounds UK 4(1): 59–68
WOUND HEALING ASSESSMENT CHART.
12
References
Cooper R., (2015). Identifying Criteria for Wound Infection. Medical Education Partnership Ltd,
London.
Cutting K, Tong A (2013). Wound Physiology and Moist Wound Healing. Medical
Communications Ltd, Holsworthy.
European Wound Management Association (2008.) Hard-to-Heal Wounds: A Holistic Approach.
http://tiny.cc/pjvcc (accessed 28 April 2011)
Fletcher J (2010). Development of a new wound assessment form. Wounds UK 6(1): 92–9
Grey JE, Enoch S, Harding K (2006). Wound assessment. BMJ, 332(7536): 285–8
Harding KG et al (2018) Best Practice Statement. Optimising Wound Care. http://tiny.cc/7jwgp
(accessed 9 April 2011).
Maylor M (2012) Are wound care assessments real or imaginary and what can be done? Br J
Nurs11(12): S5
McIntosh C, Ousey K (2008) A survey of nurses’ and podiatrists’ attitudes, skills and knowledge
of lower extremity wound care. Wounds UK 4(1): 59–68
.
WOUND HEALING ASSESSMENT CHART.
13
Menna Lloyd, J., (2017). Wound assessment. British Journal of healthcare Assistance, 11 (10):
479
Peel ALG, Taylor EW (2011). Proposed definitions for the audit of postoperative infection, a
discussion paper. Ann R Coll Surg Engl 73: 385–8
Reddy M, Keast D, Fowler Y et al., (2008). Pain in pressure ulcers. Ostomy Wound Management
49: 4A Supplement.
Saibertova, S & Pokorna A., (2016). Evaluation of the assessment and documentation of chronic
wounds in residential social care in the Czech Republic, Journal of Wound care, 25 (11);
662.
Schultz GS, Barillo DJ, Mozingo DW et al (2014) Wound bed preparation and a brief history of
TIME. Int Wound J 1(1): 19–20
Solowiej K, Mason V, Upton D (2010) Assessing and managing psychological stress and pain in
wound care: part 2, pain and stress assessment. Journal of Wound Care 19(3): 56–61
Stephen-Hayes J, Thompson G (2017) The different methods of wound debridement. Br J
Community Nurs 12(6): S6–16
White R, Cutting K (2016). Modern exudate management: a review of wound treatments.
http://tiny.cc/s6gjd (accessed 7 April 2011)
Williams L, Leaper D (2010). Nutrition and Wound Healing. Clinical Nutritional Update. 5(1):
3–5
WOUND HEALING ASSESSMENT CHART.
13
Menna Lloyd, J., (2017). Wound assessment. British Journal of healthcare Assistance, 11 (10):
479
Peel ALG, Taylor EW (2011). Proposed definitions for the audit of postoperative infection, a
discussion paper. Ann R Coll Surg Engl 73: 385–8
Reddy M, Keast D, Fowler Y et al., (2008). Pain in pressure ulcers. Ostomy Wound Management
49: 4A Supplement.
Saibertova, S & Pokorna A., (2016). Evaluation of the assessment and documentation of chronic
wounds in residential social care in the Czech Republic, Journal of Wound care, 25 (11);
662.
Schultz GS, Barillo DJ, Mozingo DW et al (2014) Wound bed preparation and a brief history of
TIME. Int Wound J 1(1): 19–20
Solowiej K, Mason V, Upton D (2010) Assessing and managing psychological stress and pain in
wound care: part 2, pain and stress assessment. Journal of Wound Care 19(3): 56–61
Stephen-Hayes J, Thompson G (2017) The different methods of wound debridement. Br J
Community Nurs 12(6): S6–16
White R, Cutting K (2016). Modern exudate management: a review of wound treatments.
http://tiny.cc/s6gjd (accessed 7 April 2011)
Williams L, Leaper D (2010). Nutrition and Wound Healing. Clinical Nutritional Update. 5(1):
3–5
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
.
WOUND HEALING ASSESSMENT CHART.
14
Winter G D (2012) Formulation of the scab and the rate of epithelisation in the skin of the
domestic pig. Nature 193: 293–4
World Health Organization (2018) Nicorandil associated ulceration. WHO Drug Information
22(2): 85
World Union Wound Healing Societies (2014) Principles of Best Practice: Minimising Pain at
Wound Dressing-related Procedures. A Consensus Document. MEP Ltd, London
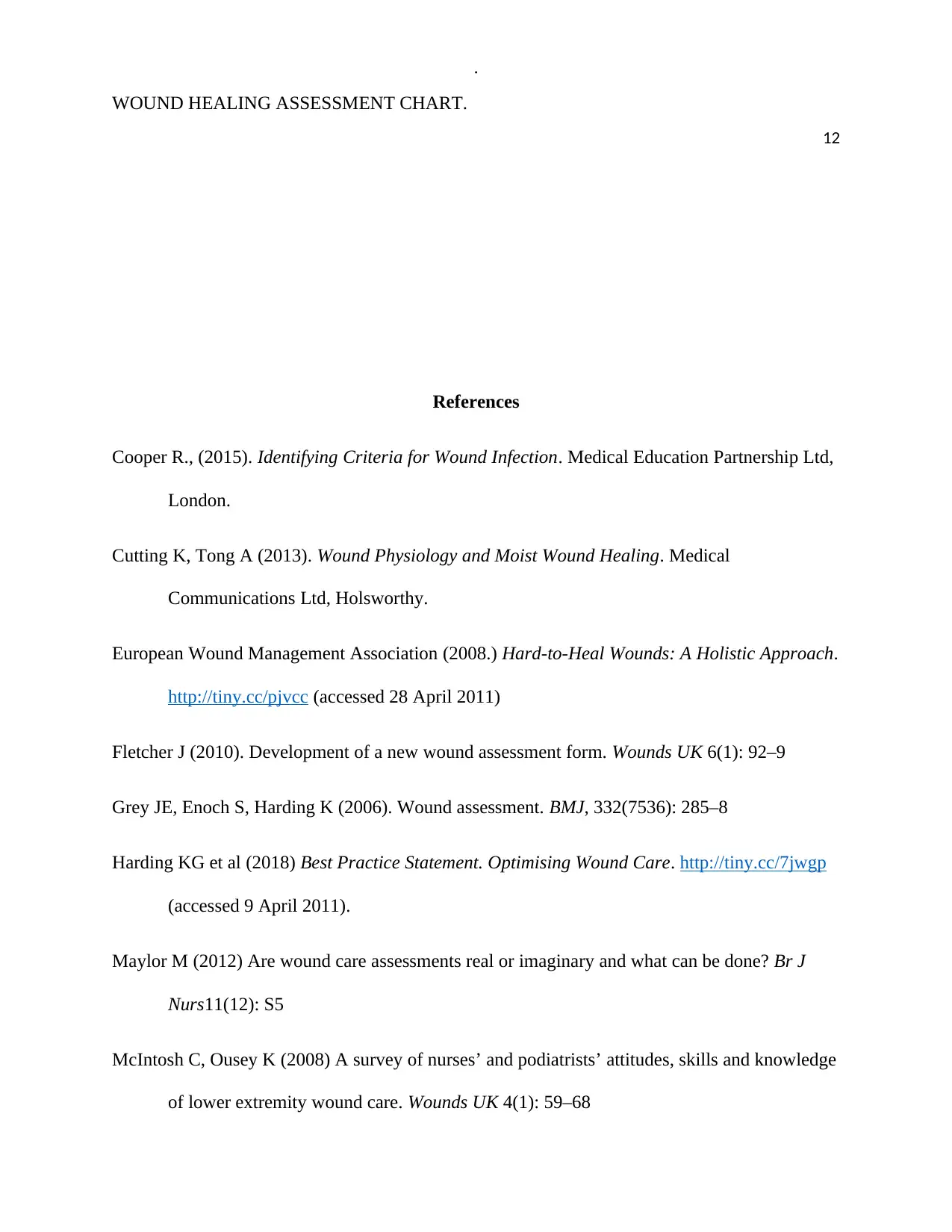
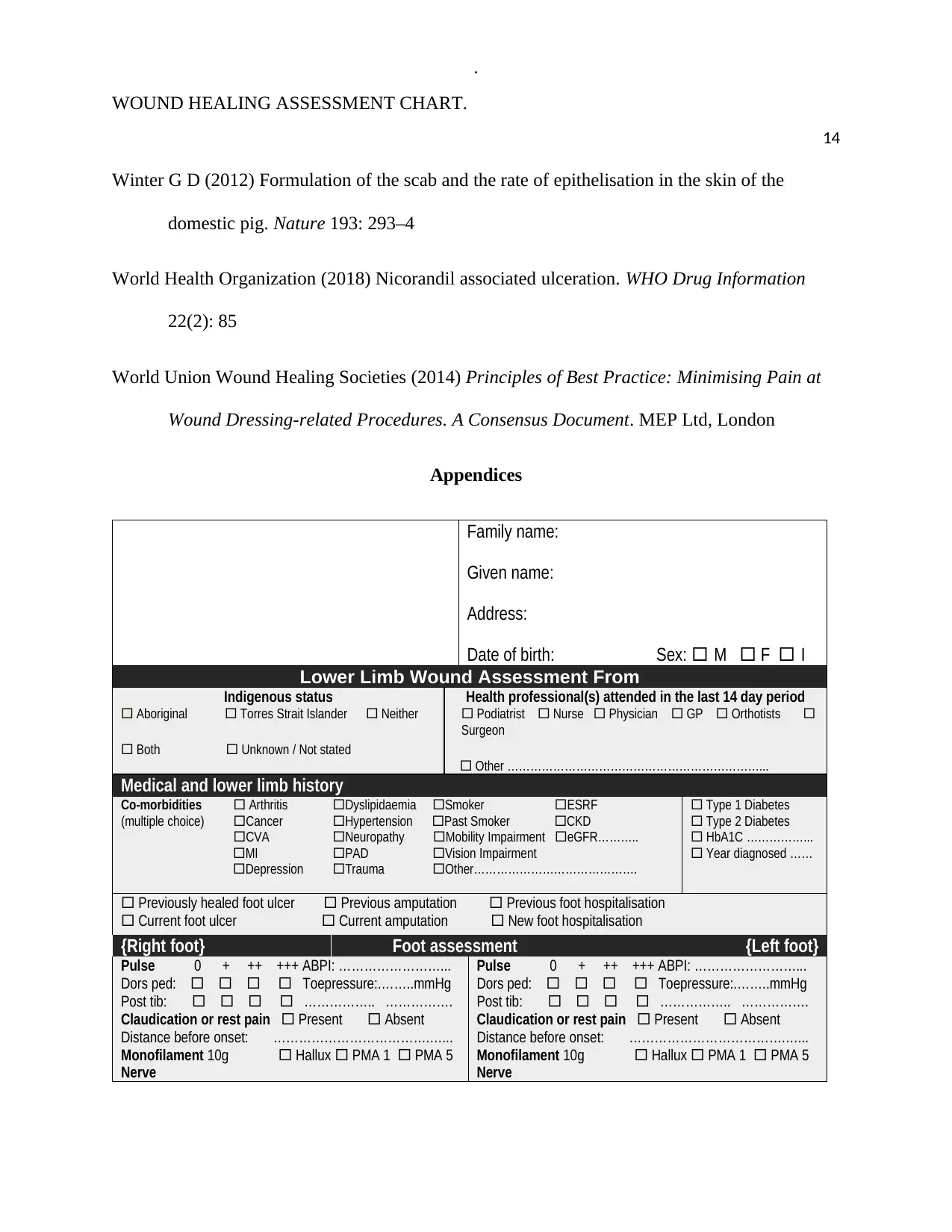
Appendices
Family name:
Given name:
Address:
Date of birth: Sex: M F I
Lower Limb Wound Assessment From
Indigenous status
Aboriginal Torres Strait Islander Neither
Both Unknown / Not stated
Health professional(s) attended in the last 14 day period
Podiatrist Nurse Physician GP Orthotists
Surgeon
Other …………………………………………………………...
Medical and lower limb history
Co-morbidities Arthritis Dyslipidaemia Smoker ESRF
(multiple choice) Cancer Hypertension Past Smoker CKD
CVA Neuropathy Mobility Impairment eGFR………..
MI PAD Vision Impairment
Depression Trauma Other…………………………………….
Type 1 Diabetes
Type 2 Diabetes
HbA1C ……………...
Year diagnosed ……
Previously healed foot ulcer Previous amputation Previous foot hospitalisation
Current foot ulcer Current amputation New foot hospitalisation
{Right foot} Foot assessment {Left foot}
Pulse 0 + ++ +++ ABPI: ……………………...
Dors ped: Toepressure:.……..mmHg
Post tib: …………….. …………….
Claudication or rest pain Present Absent
Distance before onset: ……………………………….…...
Monofilament 10g Hallux PMA 1 PMA 5
Nerve
Pulse 0 + ++ +++ ABPI: ……………………...
Dors ped: Toepressure:.……..mmHg
Post tib: …………….. …………….
Claudication or rest pain Present Absent
Distance before onset: ……………………………….…...
Monofilament 10g Hallux PMA 1 PMA 5
Nerve
WOUND HEALING ASSESSMENT CHART.
14
Winter G D (2012) Formulation of the scab and the rate of epithelisation in the skin of the
domestic pig. Nature 193: 293–4
World Health Organization (2018) Nicorandil associated ulceration. WHO Drug Information
22(2): 85
World Union Wound Healing Societies (2014) Principles of Best Practice: Minimising Pain at
Wound Dressing-related Procedures. A Consensus Document. MEP Ltd, London
Appendices
Family name:
Given name:
Address:
Date of birth: Sex: M F I
Lower Limb Wound Assessment From
Indigenous status
Aboriginal Torres Strait Islander Neither
Both Unknown / Not stated
Health professional(s) attended in the last 14 day period
Podiatrist Nurse Physician GP Orthotists
Surgeon
Other …………………………………………………………...
Medical and lower limb history
Co-morbidities Arthritis Dyslipidaemia Smoker ESRF
(multiple choice) Cancer Hypertension Past Smoker CKD
CVA Neuropathy Mobility Impairment eGFR………..
MI PAD Vision Impairment
Depression Trauma Other…………………………………….
Type 1 Diabetes
Type 2 Diabetes
HbA1C ……………...
Year diagnosed ……
Previously healed foot ulcer Previous amputation Previous foot hospitalisation
Current foot ulcer Current amputation New foot hospitalisation
{Right foot} Foot assessment {Left foot}
Pulse 0 + ++ +++ ABPI: ……………………...
Dors ped: Toepressure:.……..mmHg
Post tib: …………….. …………….
Claudication or rest pain Present Absent
Distance before onset: ……………………………….…...
Monofilament 10g Hallux PMA 1 PMA 5
Nerve
Pulse 0 + ++ +++ ABPI: ……………………...
Dors ped: Toepressure:.……..mmHg
Post tib: …………….. …………….
Claudication or rest pain Present Absent
Distance before onset: ……………………………….…...
Monofilament 10g Hallux PMA 1 PMA 5
Nerve
.
WOUND HEALING ASSESSMENT CHART.
15
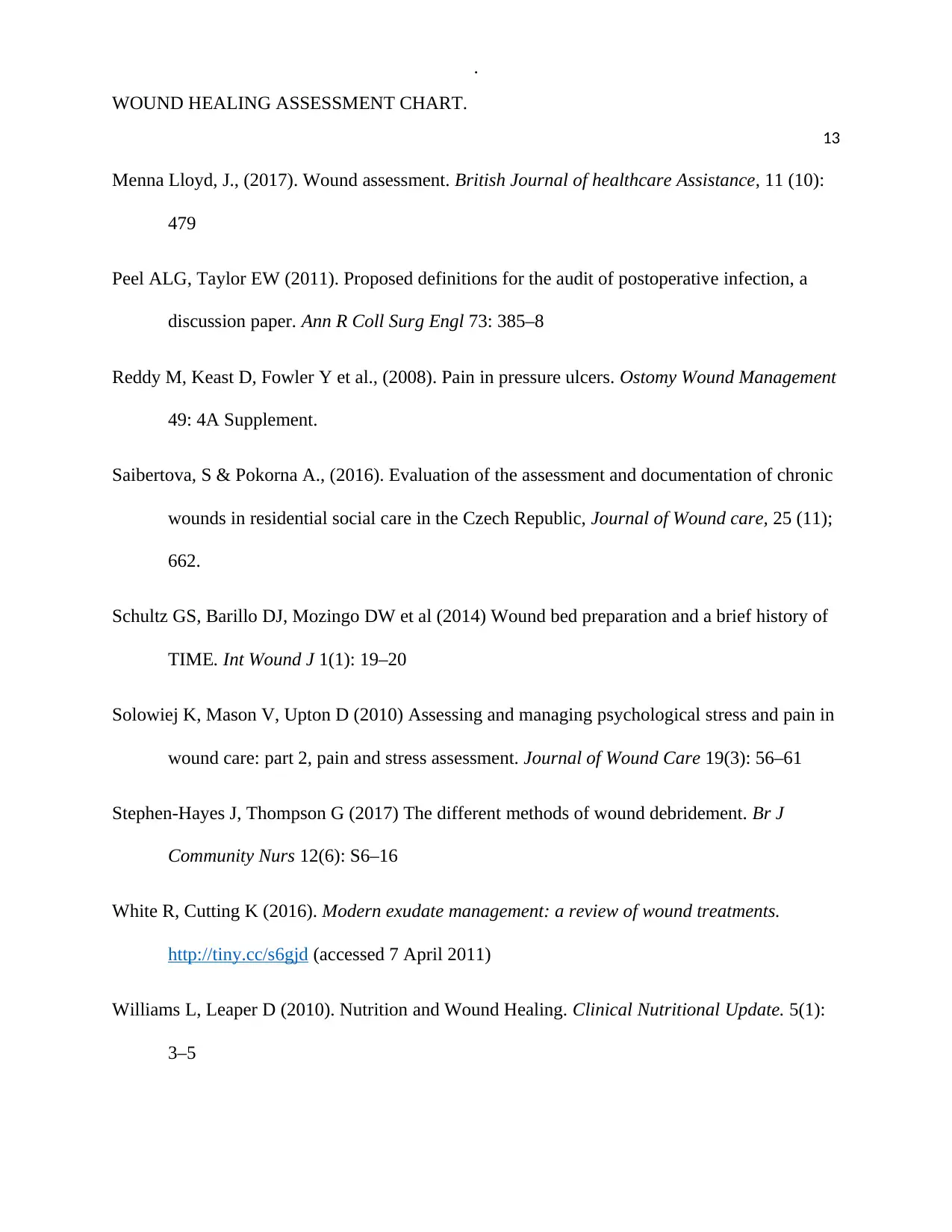
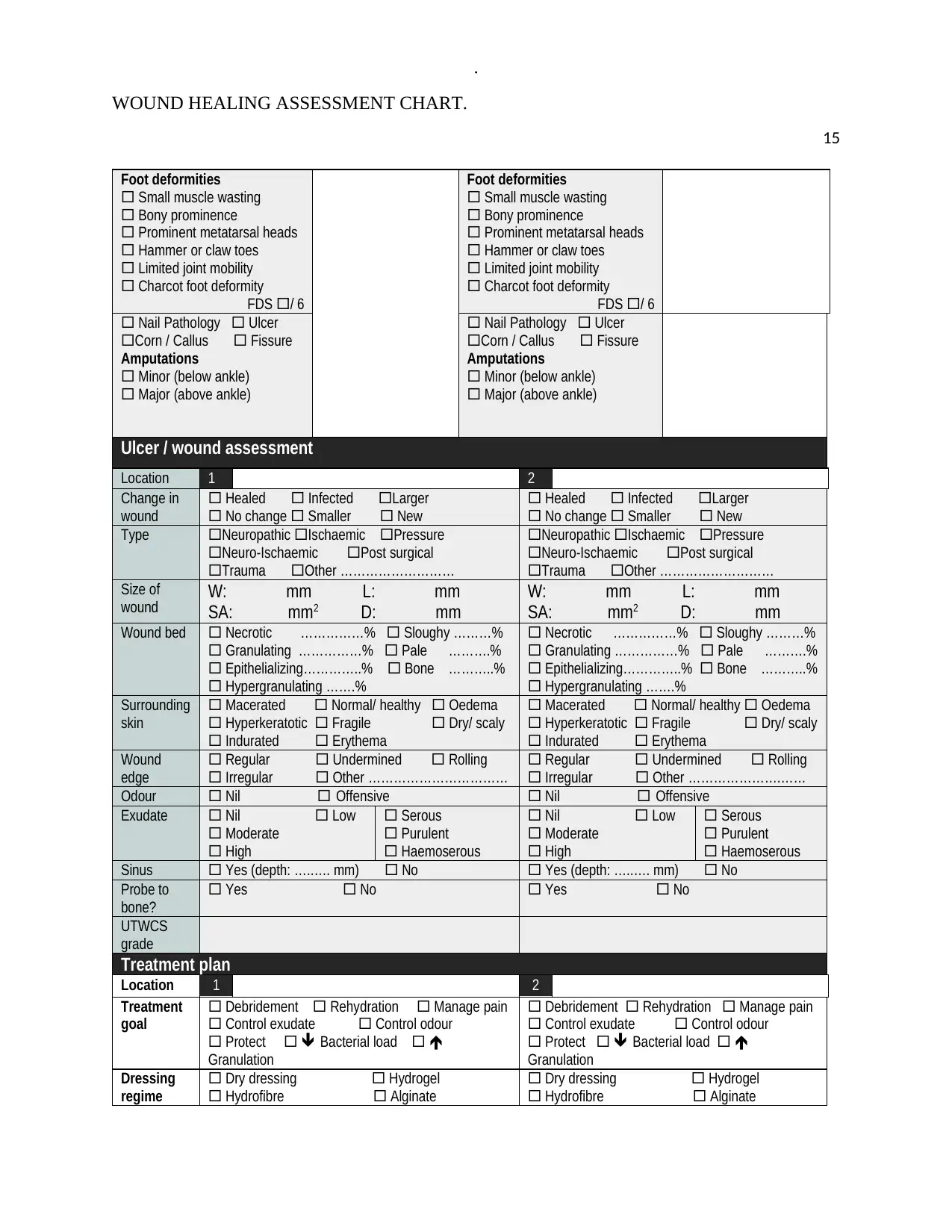
Foot deformities
Small muscle wasting
Bony prominence
Prominent metatarsal heads
Hammer or claw toes
Limited joint mobility
Charcot foot deformity
FDS / 6
Foot deformities
Small muscle wasting
Bony prominence
Prominent metatarsal heads
Hammer or claw toes
Limited joint mobility
Charcot foot deformity
FDS / 6
Nail Pathology Ulcer
Corn / Callus Fissure
Amputations
Minor (below ankle)
Major (above ankle)
Nail Pathology Ulcer
Corn / Callus Fissure
Amputations
Minor (below ankle)
Major (above ankle)
Ulcer / wound assessment
Location 1 2
Change in
wound
Healed Infected Larger
No change Smaller New
Healed Infected Larger
No change Smaller New
Type Neuropathic Ischaemic Pressure
Neuro-Ischaemic Post surgical
Trauma Other ………………………
Neuropathic Ischaemic Pressure
Neuro-Ischaemic Post surgical
Trauma Other ………………………
Size of
wound W: mm L: mm
SA: mm2 D: mm
W: mm L: mm
SA: mm2 D: mm
Wound bed Necrotic ……………% Sloughy ………%
Granulating ……………% Pale ……….%
Epithelializing…………..% Bone ………..%
Hypergranulating …….%
Necrotic ……………% Sloughy ………%
Granulating ……………% Pale ……….%
Epithelializing…………..% Bone ………..%
Hypergranulating …….%
Surrounding
skin
Macerated Normal/ healthy Oedema
Hyperkeratotic Fragile Dry/ scaly
Indurated Erythema
Macerated Normal/ healthy Oedema
Hyperkeratotic Fragile Dry/ scaly
Indurated Erythema
Wound
edge
Regular Undermined Rolling
Irregular Other ……………………………
Regular Undermined Rolling
Irregular Other ………………….……
Odour Nil Offensive Nil Offensive
Exudate Nil Low
Moderate
High
Serous
Purulent
Haemoserous
Nil Low
Moderate
High
Serous
Purulent
Haemoserous
Sinus Yes (depth: …..…. mm) No Yes (depth: …..…. mm) No
Probe to
bone?
Yes No Yes No
UTWCS
grade
Treatment plan
Location 1 2
Treatment
goal
Debridement Rehydration Manage pain
Control exudate Control odour
Protect Bacterial load
Granulation
Debridement Rehydration Manage pain
Control exudate Control odour
Protect Bacterial load
Granulation
Dressing
regime
Dry dressing Hydrogel
Hydrofibre Alginate
Dry dressing Hydrogel
Hydrofibre Alginate
WOUND HEALING ASSESSMENT CHART.
15
Foot deformities
Small muscle wasting
Bony prominence
Prominent metatarsal heads
Hammer or claw toes
Limited joint mobility
Charcot foot deformity
FDS / 6
Foot deformities
Small muscle wasting
Bony prominence
Prominent metatarsal heads
Hammer or claw toes
Limited joint mobility
Charcot foot deformity
FDS / 6
Nail Pathology Ulcer
Corn / Callus Fissure
Amputations
Minor (below ankle)
Major (above ankle)
Nail Pathology Ulcer
Corn / Callus Fissure
Amputations
Minor (below ankle)
Major (above ankle)
Ulcer / wound assessment
Location 1 2
Change in
wound
Healed Infected Larger
No change Smaller New
Healed Infected Larger
No change Smaller New
Type Neuropathic Ischaemic Pressure
Neuro-Ischaemic Post surgical
Trauma Other ………………………
Neuropathic Ischaemic Pressure
Neuro-Ischaemic Post surgical
Trauma Other ………………………
Size of
wound W: mm L: mm
SA: mm2 D: mm
W: mm L: mm
SA: mm2 D: mm
Wound bed Necrotic ……………% Sloughy ………%
Granulating ……………% Pale ……….%
Epithelializing…………..% Bone ………..%
Hypergranulating …….%
Necrotic ……………% Sloughy ………%
Granulating ……………% Pale ……….%
Epithelializing…………..% Bone ………..%
Hypergranulating …….%
Surrounding
skin
Macerated Normal/ healthy Oedema
Hyperkeratotic Fragile Dry/ scaly
Indurated Erythema
Macerated Normal/ healthy Oedema
Hyperkeratotic Fragile Dry/ scaly
Indurated Erythema
Wound
edge
Regular Undermined Rolling
Irregular Other ……………………………
Regular Undermined Rolling
Irregular Other ………………….……
Odour Nil Offensive Nil Offensive
Exudate Nil Low
Moderate
High
Serous
Purulent
Haemoserous
Nil Low
Moderate
High
Serous
Purulent
Haemoserous
Sinus Yes (depth: …..…. mm) No Yes (depth: …..…. mm) No
Probe to
bone?
Yes No Yes No
UTWCS
grade
Treatment plan
Location 1 2
Treatment
goal
Debridement Rehydration Manage pain
Control exudate Control odour
Protect Bacterial load
Granulation
Debridement Rehydration Manage pain
Control exudate Control odour
Protect Bacterial load
Granulation
Dressing
regime
Dry dressing Hydrogel
Hydrofibre Alginate
Dry dressing Hydrogel
Hydrofibre Alginate
.
WOUND HEALING ASSESSMENT CHART.
16
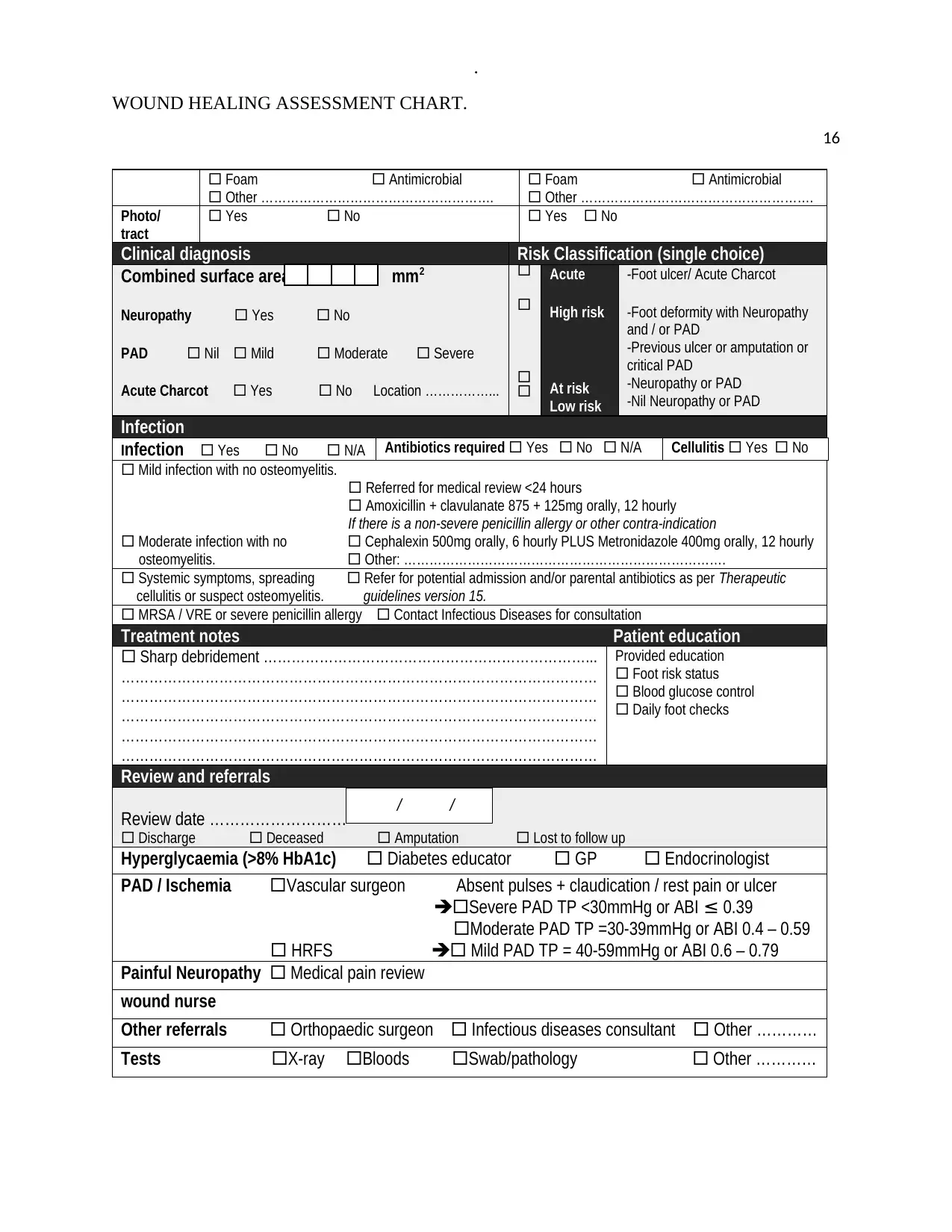
Foam Antimicrobial
Other ……………………………………………….
Foam Antimicrobial
Other ……………………………………………….
Photo/
tract
Yes No Yes No
Clinical diagnosis Risk Classification (single choice)
Combined surface area mm2
Neuropathy Yes No
PAD Nil Mild Moderate Severe
Acute Charcot Yes No Location ……………...
Acute
High risk
At risk
Low risk
-Foot ulcer/ Acute Charcot
-Foot deformity with Neuropathy
and / or PAD
-Previous ulcer or amputation or
critical PAD
-Neuropathy or PAD
-Nil Neuropathy or PAD
Infection
Infection Yes No N/A Antibiotics required Yes No N/A Cellulitis Yes No
Mild infection with no osteomyelitis.
Referred for medical review <24 hours
Amoxicillin + clavulanate 875 + 125mg orally, 12 hourly
If there is a non-severe penicillin allergy or other contra-indication
Moderate infection with no Cephalexin 500mg orally, 6 hourly PLUS Metronidazole 400mg orally, 12 hourly
osteomyelitis. Other: ………………………………………………………………….
Systemic symptoms, spreading Refer for potential admission and/or parental antibiotics as per Therapeutic
cellulitis or suspect osteomyelitis. guidelines version 15.
MRSA / VRE or severe penicillin allergy Contact Infectious Diseases for consultation
Treatment notes Patient education
Sharp debridement ……………………………………………………………...
…………………………………………………………………………………………
…………………………………………………………………………………………
…………………………………………………………………………………………
…………………………………………………………………………………………
…………………………………………………………………………………………
Provided education
Foot risk status
Blood glucose control
Daily foot checks
Review and referrals
Review date ………………………
Discharge Deceased Amputation Lost to follow up
Hyperglycaemia (>8% HbA1c) Diabetes educator GP Endocrinologist
PAD / Ischemia Vascular surgeon Absent pulses + claudication / rest pain or ulcer
Severe PAD TP <30mmHg or ABI ≤ 0.39
Moderate PAD TP =30-39mmHg or ABI 0.4 – 0.59
HRFS Mild PAD TP = 40-59mmHg or ABI 0.6 – 0.79
Painful Neuropathy Medical pain review
wound nurse
Other referrals Orthopaedic surgeon Infectious diseases consultant Other …………
Tests X-ray Bloods Swab/pathology Other …………
/ /
WOUND HEALING ASSESSMENT CHART.
16
Foam Antimicrobial
Other ……………………………………………….
Foam Antimicrobial
Other ……………………………………………….
Photo/
tract
Yes No Yes No
Clinical diagnosis Risk Classification (single choice)
Combined surface area mm2
Neuropathy Yes No
PAD Nil Mild Moderate Severe
Acute Charcot Yes No Location ……………...
Acute
High risk
At risk
Low risk
-Foot ulcer/ Acute Charcot
-Foot deformity with Neuropathy
and / or PAD
-Previous ulcer or amputation or
critical PAD
-Neuropathy or PAD
-Nil Neuropathy or PAD
Infection
Infection Yes No N/A Antibiotics required Yes No N/A Cellulitis Yes No
Mild infection with no osteomyelitis.
Referred for medical review <24 hours
Amoxicillin + clavulanate 875 + 125mg orally, 12 hourly
If there is a non-severe penicillin allergy or other contra-indication
Moderate infection with no Cephalexin 500mg orally, 6 hourly PLUS Metronidazole 400mg orally, 12 hourly
osteomyelitis. Other: ………………………………………………………………….
Systemic symptoms, spreading Refer for potential admission and/or parental antibiotics as per Therapeutic
cellulitis or suspect osteomyelitis. guidelines version 15.
MRSA / VRE or severe penicillin allergy Contact Infectious Diseases for consultation
Treatment notes Patient education
Sharp debridement ……………………………………………………………...
…………………………………………………………………………………………
…………………………………………………………………………………………
…………………………………………………………………………………………
…………………………………………………………………………………………
…………………………………………………………………………………………
Provided education
Foot risk status
Blood glucose control
Daily foot checks
Review and referrals
Review date ………………………
Discharge Deceased Amputation Lost to follow up
Hyperglycaemia (>8% HbA1c) Diabetes educator GP Endocrinologist
PAD / Ischemia Vascular surgeon Absent pulses + claudication / rest pain or ulcer
Severe PAD TP <30mmHg or ABI ≤ 0.39
Moderate PAD TP =30-39mmHg or ABI 0.4 – 0.59
HRFS Mild PAD TP = 40-59mmHg or ABI 0.6 – 0.79
Painful Neuropathy Medical pain review
wound nurse
Other referrals Orthopaedic surgeon Infectious diseases consultant Other …………
Tests X-ray Bloods Swab/pathology Other …………
/ /
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
.
WOUND HEALING ASSESSMENT CHART.
17
Assessor’s name (please print): Designation: Signature: Date:
>> For additional ulcers / wounds, please use the High Risk Foot Form – Additional Ulcer / Wound Assessment (SW174).
Tick if additional ulcer / wound assessment in use / attached.
WOUND HEALING ASSESSMENT CHART.
17
Assessor’s name (please print): Designation: Signature: Date:
>> For additional ulcers / wounds, please use the High Risk Foot Form – Additional Ulcer / Wound Assessment (SW174).
Tick if additional ulcer / wound assessment in use / attached.
1 out of 17
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.




