Wound Management of Pin Sites Post Hospital Discharge
VerifiedAdded on 2022/10/12
|14
|2932
|341
AI Summary
This study deals with wrong medicinal intervention and erroneous pharmaceutical events in the care of the percutaneous pin sites wound management, leading to adverse effects which are at times even life threatening. Read more about the best practice guidelines for wound management of pin sites in patients having external fixation frames after discharge from the hospital.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: WOUND MANAGEMENT OF PIN SITES POST HOSPITAL DISCHARGE
WOUND MANAGEMENT OF PIN SITES POST HOSPITAL DISCHARGE
Name of the Student
Name of the University
Author’s Note
WOUND MANAGEMENT OF PIN SITES POST HOSPITAL DISCHARGE
Name of the Student
Name of the University
Author’s Note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

1WOUND MANAGEMENT OF PIN SITES POST HOSPITAL DISCHARGE
Executive Summary
Pin site percutaneous wounds are common in orthopedic procedures while treating patients
with fractures or broken bones. Due to the presence of wires, screws and other external
fixture holding devices, the wounds do not heal till the time they are removed and thereby
making the wound care of the percutaneous pin sites very critical. The study deals with
wrong medicinal intervention and erroneous pharmaceutical events in the care of the
percutaneous pin sites wound management, leading to adverse effects which are at times even
life threatening. The case study includes systemic review of an academic article which
encompasses events of the effect of pharmacists’ interventions on medically significant
medication errors post discharge from the hospital. This article successfully highlights the
gross error in medical interventions which also leads to readmission with critical issues.
Executive Summary
Pin site percutaneous wounds are common in orthopedic procedures while treating patients
with fractures or broken bones. Due to the presence of wires, screws and other external
fixture holding devices, the wounds do not heal till the time they are removed and thereby
making the wound care of the percutaneous pin sites very critical. The study deals with
wrong medicinal intervention and erroneous pharmaceutical events in the care of the
percutaneous pin sites wound management, leading to adverse effects which are at times even
life threatening. The case study includes systemic review of an academic article which
encompasses events of the effect of pharmacists’ interventions on medically significant
medication errors post discharge from the hospital. This article successfully highlights the
gross error in medical interventions which also leads to readmission with critical issues.
2WOUND MANAGEMENT OF PIN SITES POST HOSPITAL DISCHARGE
Table of Contents
Introduction................................................................................................................................3
Background............................................................................................................................3
PICOT question......................................................................................................................4
Strategy proposal....................................................................................................................4
Literature critique.......................................................................................................................5
Article reviewed.....................................................................................................................5
Methodology used..................................................................................................................6
Author’s derivation................................................................................................................7
Limitations of the study.......................................................................................................10
Conclusion................................................................................................................................11
References................................................................................................................................12
Table of Contents
Introduction................................................................................................................................3
Background............................................................................................................................3
PICOT question......................................................................................................................4
Strategy proposal....................................................................................................................4
Literature critique.......................................................................................................................5
Article reviewed.....................................................................................................................5
Methodology used..................................................................................................................6
Author’s derivation................................................................................................................7
Limitations of the study.......................................................................................................10
Conclusion................................................................................................................................11
References................................................................................................................................12
3WOUND MANAGEMENT OF PIN SITES POST HOSPITAL DISCHARGE
Introduction
Background
Pin site wound issues are a prevalent orthopedic concern that occurs from
percutaneous insertion of wires, screws or cables (Kazmers, Fragomen & Rozbruch, 2016).
These set complicated hurdles for the usage of skeletal based traction pins, fracture pinning
done percutaneously along with external fixation that are the basic techniques used during
orthopedic fixation of broken or fractured bones (Park et al., 2015). Pin sites locations are
prone to infection due to disruption of the skin barrier. Most infections at the pin sites are
treatable and curable with regular medical intervention along with a basic oral antibiotic
course for a short period of time along with proper wound care (Andersen, 2019). Infections
which are deep tissue seated with the addition of osteomyelitis might occur in around 4% of
the cases that might lead to severe complications. Increased pain leading to loosening of pin,
use of medications for pain control along with delayed mobilization might follow due to
improper wound management of the pin sites. The removal of pins also might be required in
cases that are severe and fail to act in response to the treatment with antibiotics (Bernardo,
2001).
Given the elevated incidences of infections at the pin site locations amongst the
patients undergoing the external fixation and orthopedic surgeries, physicians must educate
the concerned patients ways to identify and recognize signs and pin site infections’ symptoms
in order to instigate treatment and initiate follow up promptly as required (Bibbo &
Brueggeman, 2017). A spectrum of infections at the pin site locations must be alottedand
distinguished by the orthopaedic surgeons to categorize patients based on risk along with
Introduction
Background
Pin site wound issues are a prevalent orthopedic concern that occurs from
percutaneous insertion of wires, screws or cables (Kazmers, Fragomen & Rozbruch, 2016).
These set complicated hurdles for the usage of skeletal based traction pins, fracture pinning
done percutaneously along with external fixation that are the basic techniques used during
orthopedic fixation of broken or fractured bones (Park et al., 2015). Pin sites locations are
prone to infection due to disruption of the skin barrier. Most infections at the pin sites are
treatable and curable with regular medical intervention along with a basic oral antibiotic
course for a short period of time along with proper wound care (Andersen, 2019). Infections
which are deep tissue seated with the addition of osteomyelitis might occur in around 4% of
the cases that might lead to severe complications. Increased pain leading to loosening of pin,
use of medications for pain control along with delayed mobilization might follow due to
improper wound management of the pin sites. The removal of pins also might be required in
cases that are severe and fail to act in response to the treatment with antibiotics (Bernardo,
2001).
Given the elevated incidences of infections at the pin site locations amongst the
patients undergoing the external fixation and orthopedic surgeries, physicians must educate
the concerned patients ways to identify and recognize signs and pin site infections’ symptoms
in order to instigate treatment and initiate follow up promptly as required (Bibbo &
Brueggeman, 2017). A spectrum of infections at the pin site locations must be alottedand
distinguished by the orthopaedic surgeons to categorize patients based on risk along with
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4WOUND MANAGEMENT OF PIN SITES POST HOSPITAL DISCHARGE
anticipating detrimental complications that might arise from a simple infection at the pin site
locations (Kazmers, Fragomen & Rozbruch, 2016).
Patients after discharge from the hospital must be comprehensive protocols in a
handout explaining the procedure for pin location care along with details of the
pharmaceutical drugs required for the medical management of the wound (Ip et al., 2018).
Although, discharge summary with all the drugs and protocols mentioned is an efficient
method of communicating with members of the household about the percutaneous pin wound
care, there has been reports of erroneous medical intervention from the pharmacists which
lead to poor wound management (Bell et al., 2016). The following case study highlights the
incidences of clinically important medication inaccuracies due to intervention by the
pharmacist after hospital discharge and addresses the best procedure to care for pin site
wounds in patient with external fixation frames after discharge from the healthcare center or
hospital (Kripalani et al., 2012).
PICOT question
The questions composed in the PICOT question format is a dependable and consistent
formula to generate answers addressing major criteria and therefore makes the process of
reaching the answers more reachable and better at evaluating the evidences (Echevarria &
Walker, 2014). The PICOT format encompasses P: Population or patient identity, I:
Intervention or indicator, C: Comparison or control, O: Outcome along with T: Time taken
to arrive at an outcome or the time for which the participants are observed.
The PICOT question composed for the assignment is “What are the best practice
guidelines for wound management of pin sites in patient having an external fixation frames
after discharge from the hospital?”
anticipating detrimental complications that might arise from a simple infection at the pin site
locations (Kazmers, Fragomen & Rozbruch, 2016).
Patients after discharge from the hospital must be comprehensive protocols in a
handout explaining the procedure for pin location care along with details of the
pharmaceutical drugs required for the medical management of the wound (Ip et al., 2018).
Although, discharge summary with all the drugs and protocols mentioned is an efficient
method of communicating with members of the household about the percutaneous pin wound
care, there has been reports of erroneous medical intervention from the pharmacists which
lead to poor wound management (Bell et al., 2016). The following case study highlights the
incidences of clinically important medication inaccuracies due to intervention by the
pharmacist after hospital discharge and addresses the best procedure to care for pin site
wounds in patient with external fixation frames after discharge from the healthcare center or
hospital (Kripalani et al., 2012).
PICOT question
The questions composed in the PICOT question format is a dependable and consistent
formula to generate answers addressing major criteria and therefore makes the process of
reaching the answers more reachable and better at evaluating the evidences (Echevarria &
Walker, 2014). The PICOT format encompasses P: Population or patient identity, I:
Intervention or indicator, C: Comparison or control, O: Outcome along with T: Time taken
to arrive at an outcome or the time for which the participants are observed.
The PICOT question composed for the assignment is “What are the best practice
guidelines for wound management of pin sites in patient having an external fixation frames
after discharge from the hospital?”
5WOUND MANAGEMENT OF PIN SITES POST HOSPITAL DISCHARGE
Strategy proposal
The strategy taken to address of the PICOT question comprises of systemic review of
articles to evaluate the effect of medication error due to pharmacist intervention after hospital
discharge and addresses the best procedure for treating pin site wounds in patients with
external fixing frames post hospital care. The peer reviewed articles were gathered from
Google Scholar along with the article DOI (digital object identifier) for easy access.
Literature critique
Article reviewed
Following hospital discharge, clinically imperative medication errors are common.
These include preventable adverse drug incidents along with drug discrepancies and cases of
non-adherence with the prescribed care plan which is potential for damage in the future
(potential negative drug events). The article chosen from the given list for this assignment is
“Effect of a Pharmacist Intervention on Clinically Important Medication Errors after Hospital
Discharge. Annals of Internal Medicine (Kripalani et al.,2012). The article has been published
in Annals of Internal Medicine which is a highly esteemed peer reviewed journal with a
current impact factor of 19.315). Annals of Internal Medicine journal is one of the most cited
internal general medicine academic journal along with being an influential journal in the field
of medicine.
Usually patients have issues with their drug regimen and many experience negative
results after discharge. The adverse drug events (ADEs) identified as substance injury, affect
11-17% of the patients within the initial few weeks after release from the hospital. Previously
conducted research suggests that many of preventable ADEs could have been managed.
Many others are not completely preventable, but their length or seriousness could be
Strategy proposal
The strategy taken to address of the PICOT question comprises of systemic review of
articles to evaluate the effect of medication error due to pharmacist intervention after hospital
discharge and addresses the best procedure for treating pin site wounds in patients with
external fixing frames post hospital care. The peer reviewed articles were gathered from
Google Scholar along with the article DOI (digital object identifier) for easy access.
Literature critique
Article reviewed
Following hospital discharge, clinically imperative medication errors are common.
These include preventable adverse drug incidents along with drug discrepancies and cases of
non-adherence with the prescribed care plan which is potential for damage in the future
(potential negative drug events). The article chosen from the given list for this assignment is
“Effect of a Pharmacist Intervention on Clinically Important Medication Errors after Hospital
Discharge. Annals of Internal Medicine (Kripalani et al.,2012). The article has been published
in Annals of Internal Medicine which is a highly esteemed peer reviewed journal with a
current impact factor of 19.315). Annals of Internal Medicine journal is one of the most cited
internal general medicine academic journal along with being an influential journal in the field
of medicine.
Usually patients have issues with their drug regimen and many experience negative
results after discharge. The adverse drug events (ADEs) identified as substance injury, affect
11-17% of the patients within the initial few weeks after release from the hospital. Previously
conducted research suggests that many of preventable ADEs could have been managed.
Many others are not completely preventable, but their length or seriousness could be
6WOUND MANAGEMENT OF PIN SITES POST HOSPITAL DISCHARGE
decreased (amendable ADEs). Besides, medication-related issues might also be present after
discharge in relation to ADEs, which have not yet caused injury but may cause damage if not
fixed in the future. These prospective ADEs include discrepancies or incidents of non-
adherence to the patient's medication plan. Together, improved or preventable ADEs and
probable ADEs include medication errors that are clinically essential, a significant goal for
patient safety measures. Some people, including the seniors, those with poor mental structure
or poor hygiene, or those recommended high-risk medicines tend to be at greater stake for
such medically significant mistakes.
In general, interventions with pharmacists are efficient in decreasing drug mistakes
and adverse incidents amongst clients. Investigation is required to establish the level to which
an action by a pharmacist could diminish errors in medication that are clinically essential
during the sensitive period after discharge from the hospital, especially in an age where
restoration via medication is limited (Kripalani et al.,2012).
Methodology used
The Pharmacist Intervention for Low Literacy in Cardiovascular Disease (PILL-
CVD) research was conducted in order to evaluate the impact of tailored action on the
amount of clinically significant errors in medication after discharge from the hospital,
composed of pharmacist-assisted understanding, in-patient pharmacist counseling, low-level
compliance support and individualized telephone follow-up. PILL-CVD was randomized
monitored trial which was conducted at two separate medical facilities.
The participants were randomized for experimentation, in order to receive ordinary
care or regular care with additional intervention. In permuted clusters of two to six
individuals, randomization was stratified by research location and disease through a computer
program that kept the distribution concealed. One unblinded investigation coordinator
decreased (amendable ADEs). Besides, medication-related issues might also be present after
discharge in relation to ADEs, which have not yet caused injury but may cause damage if not
fixed in the future. These prospective ADEs include discrepancies or incidents of non-
adherence to the patient's medication plan. Together, improved or preventable ADEs and
probable ADEs include medication errors that are clinically essential, a significant goal for
patient safety measures. Some people, including the seniors, those with poor mental structure
or poor hygiene, or those recommended high-risk medicines tend to be at greater stake for
such medically significant mistakes.
In general, interventions with pharmacists are efficient in decreasing drug mistakes
and adverse incidents amongst clients. Investigation is required to establish the level to which
an action by a pharmacist could diminish errors in medication that are clinically essential
during the sensitive period after discharge from the hospital, especially in an age where
restoration via medication is limited (Kripalani et al.,2012).
Methodology used
The Pharmacist Intervention for Low Literacy in Cardiovascular Disease (PILL-
CVD) research was conducted in order to evaluate the impact of tailored action on the
amount of clinically significant errors in medication after discharge from the hospital,
composed of pharmacist-assisted understanding, in-patient pharmacist counseling, low-level
compliance support and individualized telephone follow-up. PILL-CVD was randomized
monitored trial which was conducted at two separate medical facilities.
The participants were randomized for experimentation, in order to receive ordinary
care or regular care with additional intervention. In permuted clusters of two to six
individuals, randomization was stratified by research location and disease through a computer
program that kept the distribution concealed. One unblinded investigation coordinator
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7WOUND MANAGEMENT OF PIN SITES POST HOSPITAL DISCHARGE
administered the randomization per medical facility. The unblended coordinator contacted
pharmacists from study who then went on to deliver the intervention to the eligible patients
participating along with monitoring individualized follow-ups. All the other researchers,
evaluators of the result and statisticians were blinded.
Author’s derivation
The authors thereby discovered that clinically significant errors in medication were
prevalent in this randomized study which was crucially monitored, and the erroneous
intervention influenced 50.8 percent of clients during the first 30 days after hospital
discharge. Overall, the research clinics did not substantially decrease clinically significant
drug mistakes or ADEs through patient literacy-sensitive pharmacist interference.
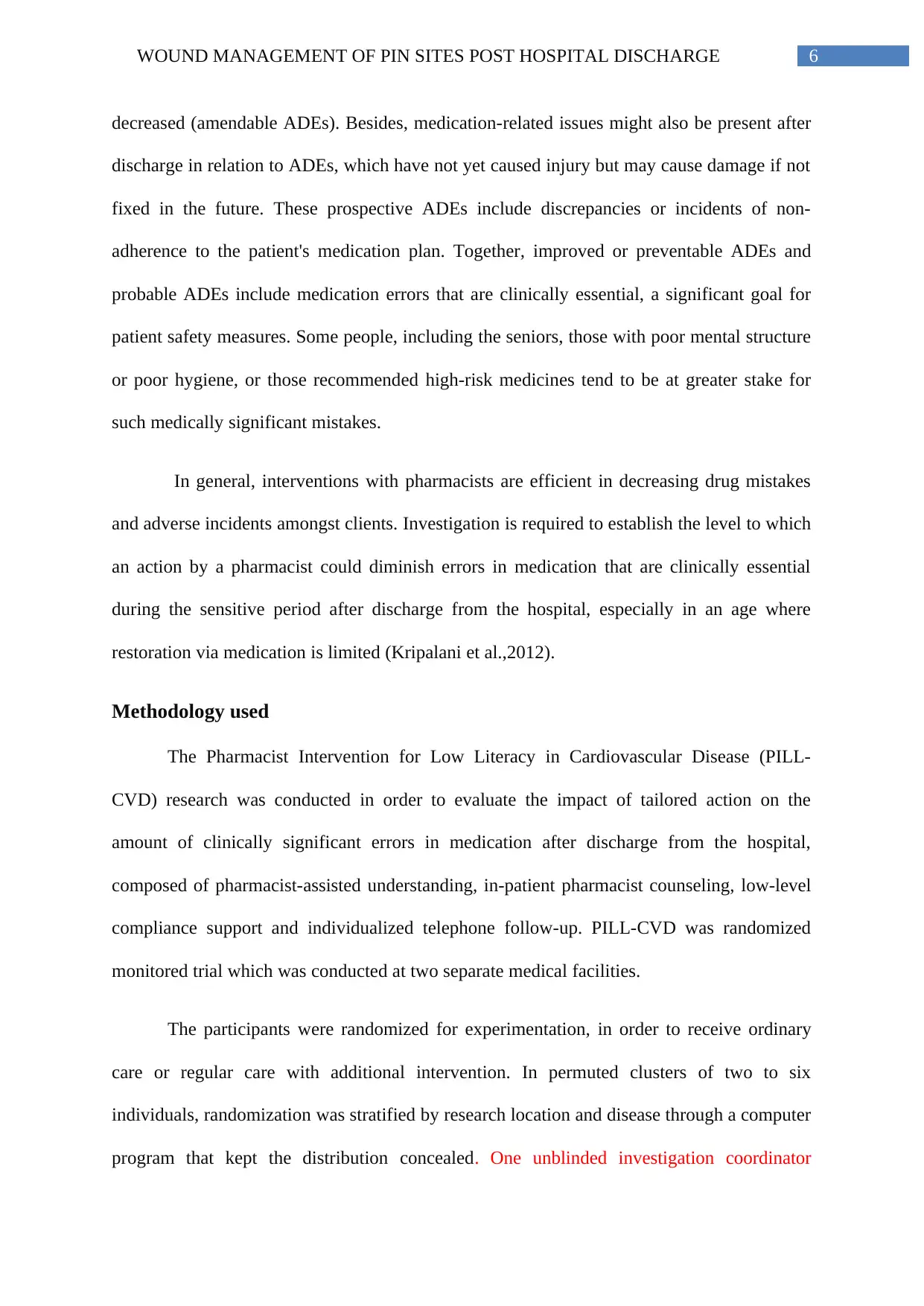
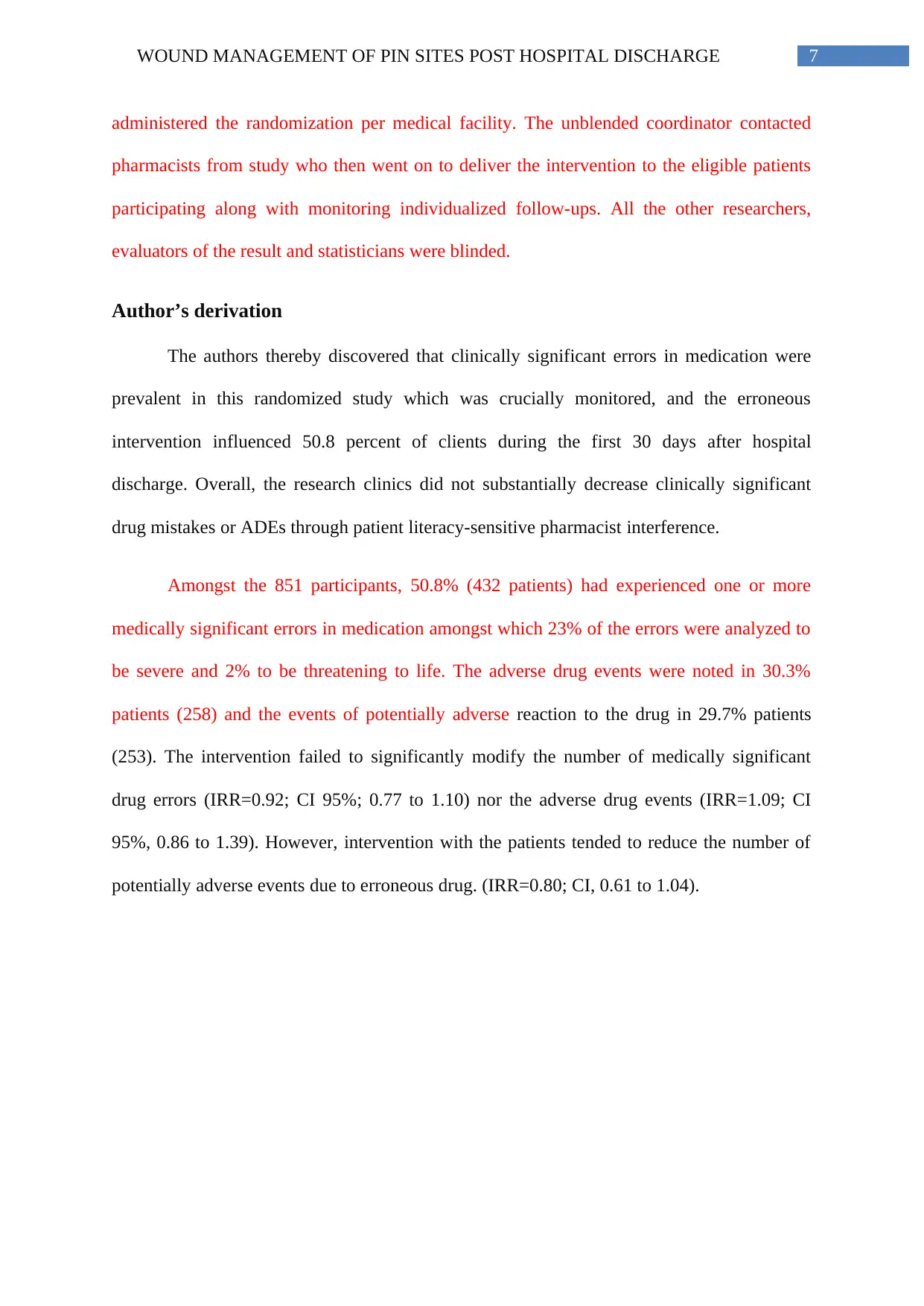
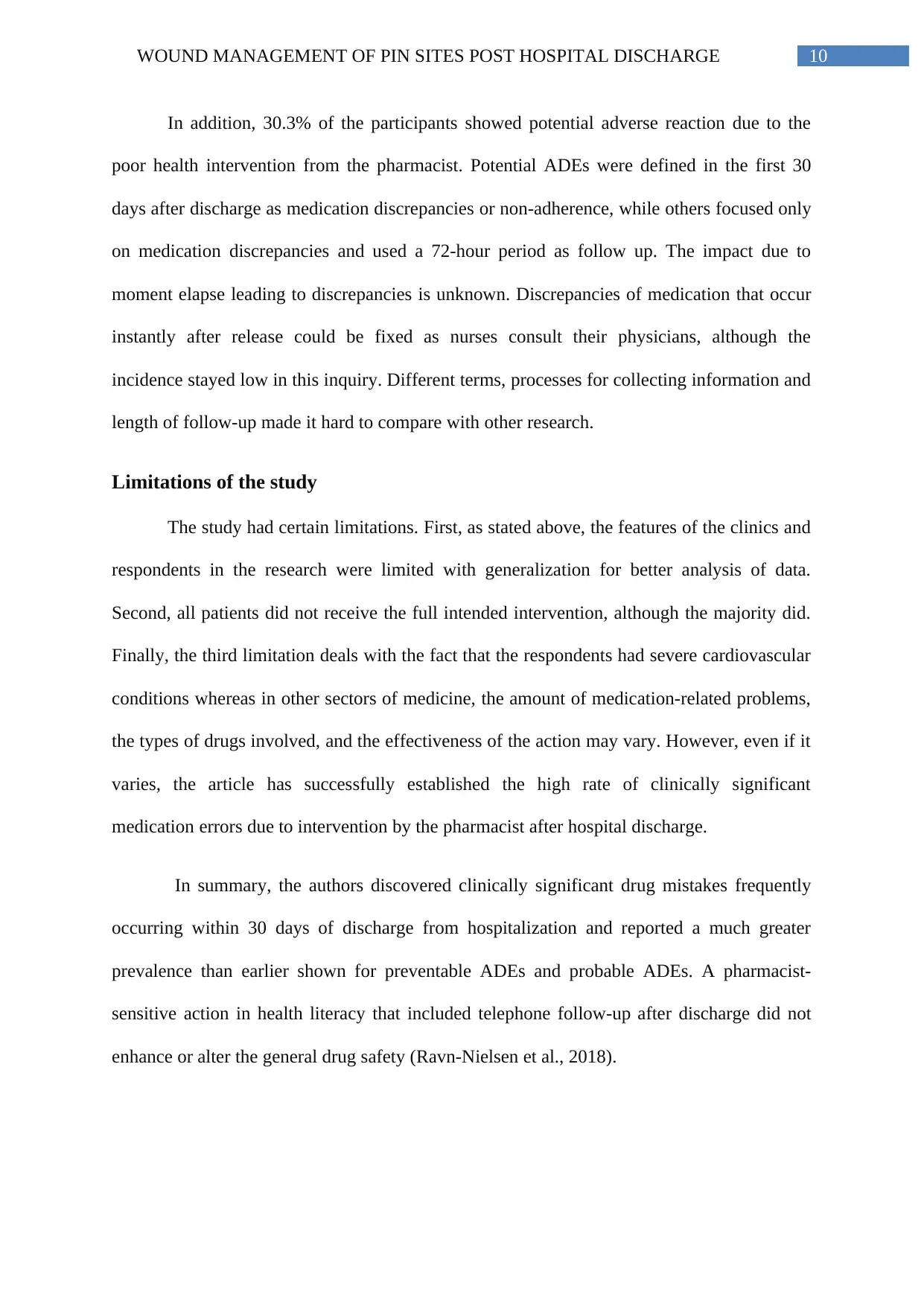
Amongst the 851 participants, 50.8% (432 patients) had experienced one or more
medically significant errors in medication amongst which 23% of the errors were analyzed to
be severe and 2% to be threatening to life. The adverse drug events were noted in 30.3%
patients (258) and the events of potentially adverse reaction to the drug in 29.7% patients
(253). The intervention failed to significantly modify the number of medically significant
drug errors (IRR=0.92; CI 95%; 0.77 to 1.10) nor the adverse drug events (IRR=1.09; CI
95%, 0.86 to 1.39). However, intervention with the patients tended to reduce the number of
potentially adverse events due to erroneous drug. (IRR=0.80; CI, 0.61 to 1.04).
administered the randomization per medical facility. The unblended coordinator contacted
pharmacists from study who then went on to deliver the intervention to the eligible patients
participating along with monitoring individualized follow-ups. All the other researchers,
evaluators of the result and statisticians were blinded.
Author’s derivation
The authors thereby discovered that clinically significant errors in medication were
prevalent in this randomized study which was crucially monitored, and the erroneous
intervention influenced 50.8 percent of clients during the first 30 days after hospital
discharge. Overall, the research clinics did not substantially decrease clinically significant
drug mistakes or ADEs through patient literacy-sensitive pharmacist interference.
Amongst the 851 participants, 50.8% (432 patients) had experienced one or more
medically significant errors in medication amongst which 23% of the errors were analyzed to
be severe and 2% to be threatening to life. The adverse drug events were noted in 30.3%
patients (258) and the events of potentially adverse reaction to the drug in 29.7% patients
(253). The intervention failed to significantly modify the number of medically significant
drug errors (IRR=0.92; CI 95%; 0.77 to 1.10) nor the adverse drug events (IRR=1.09; CI
95%, 0.86 to 1.39). However, intervention with the patients tended to reduce the number of
potentially adverse events due to erroneous drug. (IRR=0.80; CI, 0.61 to 1.04).
8WOUND MANAGEMENT OF PIN SITES POST HOSPITAL DISCHARGE
Percentage of affected patients
0.00%
10.00%
20.00%
30.00%
40.00%
50.00%
60.00%
Percentage of affected
patients
More than one clinically significant drug error
Adverse drug event
Potential adverse drug reaction
Source: Kripalani et al.,2012
Potential ADEs continued to decrease, but statistically this impact was not important.
During the shift from hospital to house, these findings show the trouble of enhancing
medication safety. The level to which its findings are generalized to other environments is the
main issue in understanding the outcomes of this adverse test. Indeed, as clinics are
increasingly implementing and evaluating programs to enhance patient movements,
understanding contextual variables that may influence outcomes is critical as there are
instances of both beneficial and negative research.
Another element influencing generalization was that the research respondents were all
well educated (14 years of schooling on average), good cognitive health (88%), and had a
comparatively small incidence of insufficient hygiene literacy (10%). PILL-CVD operation,
intended to suit clients with poor health literacy or cognitive impairment requires, may be
Percentage of affected patients
0.00%
10.00%
20.00%
30.00%
40.00%
50.00%
60.00%
Percentage of affected
patients
More than one clinically significant drug error
Adverse drug event
Potential adverse drug reaction
Source: Kripalani et al.,2012
Potential ADEs continued to decrease, but statistically this impact was not important.
During the shift from hospital to house, these findings show the trouble of enhancing
medication safety. The level to which its findings are generalized to other environments is the
main issue in understanding the outcomes of this adverse test. Indeed, as clinics are
increasingly implementing and evaluating programs to enhance patient movements,
understanding contextual variables that may influence outcomes is critical as there are
instances of both beneficial and negative research.
Another element influencing generalization was that the research respondents were all
well educated (14 years of schooling on average), good cognitive health (88%), and had a
comparatively small incidence of insufficient hygiene literacy (10%). PILL-CVD operation,
intended to suit clients with poor health literacy or cognitive impairment requires, may be
9WOUND MANAGEMENT OF PIN SITES POST HOSPITAL DISCHARGE
more efficient among these communities. The action had no impact after release on the
amount of ADEs. Part of this conclusion contains some intrinsic subjectivity in the
adjudication method. In particular, the patients learning through intervention about the side
effects can report symptoms so that adjudication as ADEs are more likely, consequently
varying the apparent effect of the intervention.
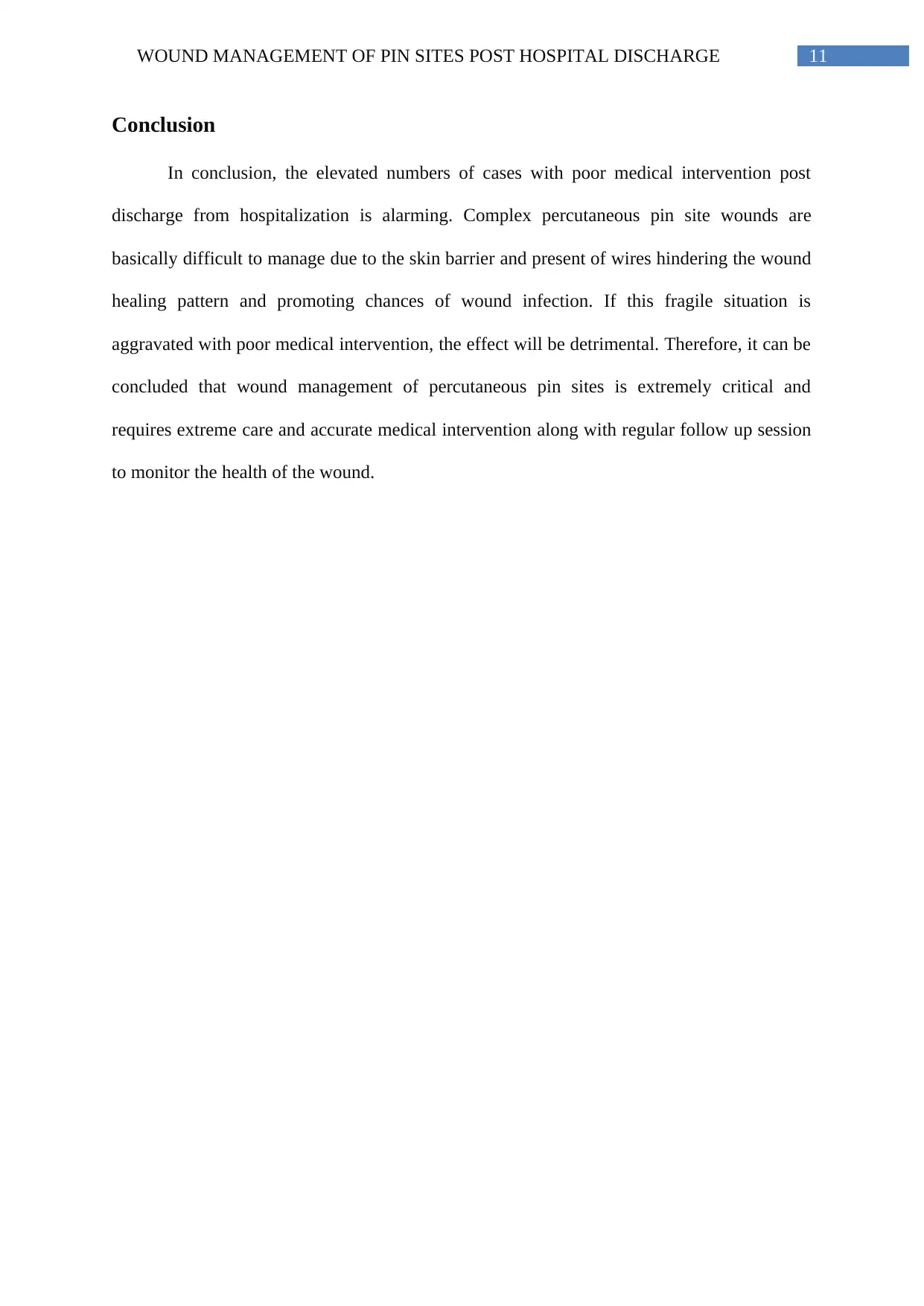
There were a higher amount of substantial ADEs (i.e., symptom-only) amongst the
clients participating in this research. Additionally, reducing preventable or improved ADEs
may involve distinct measures than those assessed here, such as nearer surveillance after
release, clinic-based help, or house trips. Despite comparable adjudication processes, the
recorded rate of preventable ADEs (30.3%) is more than double that was previously
recorded. Possible reasons include the current survey with a mildly shorter follow-up span
(30 days vs. a 24-day average), evaluation of electronic records of diagnostic health reports
for analysis, and more comprehensive examination of external medical records.
No issues noted,
49%
More than one significant
error
19%
Potential adverse
reaction
30.3%
Llife threatening effect
2%
Clinically significant medicine error noted
Source: Kripalani et al.,2012
more efficient among these communities. The action had no impact after release on the
amount of ADEs. Part of this conclusion contains some intrinsic subjectivity in the
adjudication method. In particular, the patients learning through intervention about the side
effects can report symptoms so that adjudication as ADEs are more likely, consequently
varying the apparent effect of the intervention.
There were a higher amount of substantial ADEs (i.e., symptom-only) amongst the
clients participating in this research. Additionally, reducing preventable or improved ADEs
may involve distinct measures than those assessed here, such as nearer surveillance after
release, clinic-based help, or house trips. Despite comparable adjudication processes, the
recorded rate of preventable ADEs (30.3%) is more than double that was previously
recorded. Possible reasons include the current survey with a mildly shorter follow-up span
(30 days vs. a 24-day average), evaluation of electronic records of diagnostic health reports
for analysis, and more comprehensive examination of external medical records.
No issues noted,
49%
More than one significant
error
19%
Potential adverse
reaction
30.3%
Llife threatening effect
2%
Clinically significant medicine error noted
Source: Kripalani et al.,2012
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10WOUND MANAGEMENT OF PIN SITES POST HOSPITAL DISCHARGE
In addition, 30.3% of the participants showed potential adverse reaction due to the
poor health intervention from the pharmacist. Potential ADEs were defined in the first 30
days after discharge as medication discrepancies or non-adherence, while others focused only
on medication discrepancies and used a 72-hour period as follow up. The impact due to
moment elapse leading to discrepancies is unknown. Discrepancies of medication that occur
instantly after release could be fixed as nurses consult their physicians, although the
incidence stayed low in this inquiry. Different terms, processes for collecting information and
length of follow-up made it hard to compare with other research.
Limitations of the study
The study had certain limitations. First, as stated above, the features of the clinics and
respondents in the research were limited with generalization for better analysis of data.
Second, all patients did not receive the full intended intervention, although the majority did.
Finally, the third limitation deals with the fact that the respondents had severe cardiovascular
conditions whereas in other sectors of medicine, the amount of medication-related problems,
the types of drugs involved, and the effectiveness of the action may vary. However, even if it
varies, the article has successfully established the high rate of clinically significant
medication errors due to intervention by the pharmacist after hospital discharge.
In summary, the authors discovered clinically significant drug mistakes frequently
occurring within 30 days of discharge from hospitalization and reported a much greater
prevalence than earlier shown for preventable ADEs and probable ADEs. A pharmacist-
sensitive action in health literacy that included telephone follow-up after discharge did not
enhance or alter the general drug safety (Ravn-Nielsen et al., 2018).
In addition, 30.3% of the participants showed potential adverse reaction due to the
poor health intervention from the pharmacist. Potential ADEs were defined in the first 30
days after discharge as medication discrepancies or non-adherence, while others focused only
on medication discrepancies and used a 72-hour period as follow up. The impact due to
moment elapse leading to discrepancies is unknown. Discrepancies of medication that occur
instantly after release could be fixed as nurses consult their physicians, although the
incidence stayed low in this inquiry. Different terms, processes for collecting information and
length of follow-up made it hard to compare with other research.
Limitations of the study
The study had certain limitations. First, as stated above, the features of the clinics and
respondents in the research were limited with generalization for better analysis of data.
Second, all patients did not receive the full intended intervention, although the majority did.
Finally, the third limitation deals with the fact that the respondents had severe cardiovascular
conditions whereas in other sectors of medicine, the amount of medication-related problems,
the types of drugs involved, and the effectiveness of the action may vary. However, even if it
varies, the article has successfully established the high rate of clinically significant
medication errors due to intervention by the pharmacist after hospital discharge.
In summary, the authors discovered clinically significant drug mistakes frequently
occurring within 30 days of discharge from hospitalization and reported a much greater
prevalence than earlier shown for preventable ADEs and probable ADEs. A pharmacist-
sensitive action in health literacy that included telephone follow-up after discharge did not
enhance or alter the general drug safety (Ravn-Nielsen et al., 2018).
11WOUND MANAGEMENT OF PIN SITES POST HOSPITAL DISCHARGE
Conclusion
In conclusion, the elevated numbers of cases with poor medical intervention post
discharge from hospitalization is alarming. Complex percutaneous pin site wounds are
basically difficult to manage due to the skin barrier and present of wires hindering the wound
healing pattern and promoting chances of wound infection. If this fragile situation is
aggravated with poor medical intervention, the effect will be detrimental. Therefore, it can be
concluded that wound management of percutaneous pin sites is extremely critical and
requires extreme care and accurate medical intervention along with regular follow up session
to monitor the health of the wound.
Conclusion
In conclusion, the elevated numbers of cases with poor medical intervention post
discharge from hospitalization is alarming. Complex percutaneous pin site wounds are
basically difficult to manage due to the skin barrier and present of wires hindering the wound
healing pattern and promoting chances of wound infection. If this fragile situation is
aggravated with poor medical intervention, the effect will be detrimental. Therefore, it can be
concluded that wound management of percutaneous pin sites is extremely critical and
requires extreme care and accurate medical intervention along with regular follow up session
to monitor the health of the wound.
12WOUND MANAGEMENT OF PIN SITES POST HOSPITAL DISCHARGE
References
Andersen, B. M. (2019). Care of Wound Drainages. In Prevention and Control of Infections
in Hospitals (pp. 495-499). Springer. DOI: 10.1007/978-3-319-99921-0_37
Bell, S. P., Schnipper, J. L., Goggins, K., Bian, A., Shintani, A., Roumie, C. L., ... & Gandhi,
T. K. (2016). Effect of pharmacist counseling intervention on health care utilization
following hospital discharge: a randomized control trial. Journal of general internal
medicine, 31(5), 470-477. DOI: 10.10072Fs11606-016-3596-3
Bernardo, L. M. (2001). Evidence-based practice for pin site care in injured
children. Orthopaedic Nursing, 20(5), 29-34.
Bibbo, C., & Brueggeman, J. (2017). Prevention and management of complications arising
from external fixation pin sites. The Journal of Foot and Ankle Surgery, 49(1), 87-92.
doi: 10.1007/s11751-016-0256-4
Echevarria, I. M., & Walker, S. (2014). To make your case, start with a PICOT
question. Nursing2019, 44(2), 18-19. DOI: 10.1097/01.NURSE.0000442594.00242.f9
Ip, R., Tenney, J., Chu, A., Chu, P., & Young, G. (2018). Pharmacist Clinical Interventions
and Discharge Counseling in Medical Rehabilitation Wards in a Local Hospital: A
Prospective Trial. Geriatrics, 3(3), 53. DOI: https://doi.org/10.3390/geriatrics3030053
Kazmers, N. H., Fragomen, A. T., & Rozbruch, S. R. (2016). Prevention of pin site infection
in external fixation: a review of the literature. Strategies in Trauma and Limb
Reconstruction, 11(2), 75-85. DOI: 10.1007/s11751-016-0256-4
Kripalani, S., Roumie, C. L., Dalal, A. K., Cawthon, C., Businger, A., Eden, S. K., ... &
Huang, R. L. (2012). Effect of a pharmacist intervention on clinically important
References
Andersen, B. M. (2019). Care of Wound Drainages. In Prevention and Control of Infections
in Hospitals (pp. 495-499). Springer. DOI: 10.1007/978-3-319-99921-0_37
Bell, S. P., Schnipper, J. L., Goggins, K., Bian, A., Shintani, A., Roumie, C. L., ... & Gandhi,
T. K. (2016). Effect of pharmacist counseling intervention on health care utilization
following hospital discharge: a randomized control trial. Journal of general internal
medicine, 31(5), 470-477. DOI: 10.10072Fs11606-016-3596-3
Bernardo, L. M. (2001). Evidence-based practice for pin site care in injured
children. Orthopaedic Nursing, 20(5), 29-34.
Bibbo, C., & Brueggeman, J. (2017). Prevention and management of complications arising
from external fixation pin sites. The Journal of Foot and Ankle Surgery, 49(1), 87-92.
doi: 10.1007/s11751-016-0256-4
Echevarria, I. M., & Walker, S. (2014). To make your case, start with a PICOT
question. Nursing2019, 44(2), 18-19. DOI: 10.1097/01.NURSE.0000442594.00242.f9
Ip, R., Tenney, J., Chu, A., Chu, P., & Young, G. (2018). Pharmacist Clinical Interventions
and Discharge Counseling in Medical Rehabilitation Wards in a Local Hospital: A
Prospective Trial. Geriatrics, 3(3), 53. DOI: https://doi.org/10.3390/geriatrics3030053
Kazmers, N. H., Fragomen, A. T., & Rozbruch, S. R. (2016). Prevention of pin site infection
in external fixation: a review of the literature. Strategies in Trauma and Limb
Reconstruction, 11(2), 75-85. DOI: 10.1007/s11751-016-0256-4
Kripalani, S., Roumie, C. L., Dalal, A. K., Cawthon, C., Businger, A., Eden, S. K., ... &
Huang, R. L. (2012). Effect of a pharmacist intervention on clinically important
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13WOUND MANAGEMENT OF PIN SITES POST HOSPITAL DISCHARGE
medication errors after hospital discharge: a randomized trial. Annals of internal
medicine, 157(1), 1-10. doi:10.7326/0003-4819-157-1-201207030-00003.
Park, P., Lodhia, K. R., Eden, S. V., Lewandrowski, K. U., & McGillicuddy, J. E. (2015).
Pin-site myiasis: a rare complication of halo orthosis. Spinal cord, 43(11), 684. DOI:
1362-4393/05
Ravn-Nielsen, L. V., Duckert, M. L., Lund, M. L., Henriksen, J. P., Nielsen, M. L., Eriksen,
C. S & Hallas, J. (2018). Effect of an in-hospital multifaceted clinical pharmacist
intervention on the risk of readmission: a randomized clinical trial. JAMA internal
medicine, 178(3), 375-382. DOI: 10.1001/jamainternmed.2017.8274
medication errors after hospital discharge: a randomized trial. Annals of internal
medicine, 157(1), 1-10. doi:10.7326/0003-4819-157-1-201207030-00003.
Park, P., Lodhia, K. R., Eden, S. V., Lewandrowski, K. U., & McGillicuddy, J. E. (2015).
Pin-site myiasis: a rare complication of halo orthosis. Spinal cord, 43(11), 684. DOI:
1362-4393/05
Ravn-Nielsen, L. V., Duckert, M. L., Lund, M. L., Henriksen, J. P., Nielsen, M. L., Eriksen,
C. S & Hallas, J. (2018). Effect of an in-hospital multifaceted clinical pharmacist
intervention on the risk of readmission: a randomized clinical trial. JAMA internal
medicine, 178(3), 375-382. DOI: 10.1001/jamainternmed.2017.8274
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.




