Primary Health Care Improvement: Report on Global Stakeholder Meeting
VerifiedAdded on 2023/06/12
|25
|9855
|325
Report
AI Summary
This report summarizes the key discussions and outcomes of the Primary Health Care Improvement Global Stakeholder Meeting held on 6-8 April 2016. The meeting focused on improving primary health care (PHC) performance through better measurement, knowledge management, and collaborative action. It highlights the importance of strong PHC systems in achieving better health outcomes equitably and cost-effectively, emphasizing domains such as access, comprehensiveness, continuity, coordination, people-centeredness, and quality. The report outlines efforts by initiatives like the Primary Health Care Performance Initiative (PHCPI) and the Health Data Collaborative (HDC) to enhance PHC measurement and data utilization. It addresses common causes of poor PHC performance and proposes strategies for improvement, including the WHO Global Challenge on Primary Health Care Improvement. The report serves as a roadmap for stakeholders to support country-level PHC measurement and improvement efforts, aiming to advance evidence-informed decision-making and overall performance enhancement in primary health care systems globally.

Primary Health Care Improveme
Global Stakeholder Meetin
6-8 April 2016
Global Stakeholder Meetin
6-8 April 2016
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

| P a g e 2
| P a g e 3
Table of Contents
Table of Contents ........................................................................................................................ 3
Key Messages ............................................................................................................................. 4
Acronym Index ............................................................................................................................ 5
Purpose ...................................................................................................................................... 7
Background ................................................................................................................................. 7
Measurement ............................................................................................................................. 9
Monitoring and Evaluation Framework ................................................................................................. 9
Establishing priorities for PHC measurement ....................................................................................... 10
Health Data Collaborative ................................................................................................................... 13
From Measurement to Improvement ........................................................................................ 15
Accelerating the process of using measurement to drive improvement ............................................... 15
Knowledge Management .................................................................................................................... 16
Action for Improvement ............................................................................................................ 18
Common causes of poor PHC performance .......................................................................................... 18
Strategies for PHC improvement ......................................................................................................... 19
PHC improvement activities (current and future) ................................................................................ 20
Global Challenge for Primary Health Care Improvement ...................................................................... 21
Annex 1: Situation Analysis Measurement ................................................................................ 23
Annex 2: PHCPI Vital Signs ........................................................................................................ 24
This report contains the collective views of an international group of experts, and does not necessarily
represent the decisions or the stated policy of the World Health Organization.
Table of Contents
Table of Contents ........................................................................................................................ 3
Key Messages ............................................................................................................................. 4
Acronym Index ............................................................................................................................ 5
Purpose ...................................................................................................................................... 7
Background ................................................................................................................................. 7
Measurement ............................................................................................................................. 9
Monitoring and Evaluation Framework ................................................................................................. 9
Establishing priorities for PHC measurement ....................................................................................... 10
Health Data Collaborative ................................................................................................................... 13
From Measurement to Improvement ........................................................................................ 15
Accelerating the process of using measurement to drive improvement ............................................... 15
Knowledge Management .................................................................................................................... 16
Action for Improvement ............................................................................................................ 18
Common causes of poor PHC performance .......................................................................................... 18
Strategies for PHC improvement ......................................................................................................... 19
PHC improvement activities (current and future) ................................................................................ 20
Global Challenge for Primary Health Care Improvement ...................................................................... 21
Annex 1: Situation Analysis Measurement ................................................................................ 23
Annex 2: PHCPI Vital Signs ........................................................................................................ 24
This report contains the collective views of an international group of experts, and does not necessarily
represent the decisions or the stated policy of the World Health Organization.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
| P a g e 4
Key Messages
1. Health systems based on high-performing primary health care (PHC) are able to achieve better health
outcomes, more equitably, and at lower relative cost than health systems that over emphasize disease-
specific and/or hospital-based care.
2. Little is known about the performance of PHC, particularly in domains of service delivery: access,
comprehensiveness, continuity, coordination, people-centeredness and quality. Challenges exist across
the measurement spectrum from data collection, analysis, visualization and use for improvement.
3. Recent efforts by international agencies, including the Primary Health Care Performance Initiative
(PHCPI) and the Health Data Collaborative (HDC), offer an opportunity for stakeholders to collaborate
and complement country investments in the area of PHC measurement for improvement.
4. The Primary Health Care Performance Initiative (PHCPI) seeks to catalyze improvements in PHC in low-
and middle-income countries by developing better measurement of PHC-relevant domains, increasing
data availability and sharing knowledge.
5. The Health Data Collaborative (HDC) aims to address disparate funding and fragmented sources of
health data that lead to the current inadequacy of data for reliable, timely decision-making. The output
of HDC is more collaborative and efficient investment in country information systems and monitoring
and evaluation plans.
6. This meeting seeks to inform these stakeholder efforts and provide a common work plan for (1)
improved PHC performance measurement including research and development of less measured
domains of quality PHC and incorporation of these measures into existing measurement platforms and
(2) PHC improvement efforts including relevant guidance and tools and the WHO Global Challenge on
Primary Health Care Improvement.
Key Messages
1. Health systems based on high-performing primary health care (PHC) are able to achieve better health
outcomes, more equitably, and at lower relative cost than health systems that over emphasize disease-
specific and/or hospital-based care.
2. Little is known about the performance of PHC, particularly in domains of service delivery: access,
comprehensiveness, continuity, coordination, people-centeredness and quality. Challenges exist across
the measurement spectrum from data collection, analysis, visualization and use for improvement.
3. Recent efforts by international agencies, including the Primary Health Care Performance Initiative
(PHCPI) and the Health Data Collaborative (HDC), offer an opportunity for stakeholders to collaborate
and complement country investments in the area of PHC measurement for improvement.
4. The Primary Health Care Performance Initiative (PHCPI) seeks to catalyze improvements in PHC in low-
and middle-income countries by developing better measurement of PHC-relevant domains, increasing
data availability and sharing knowledge.
5. The Health Data Collaborative (HDC) aims to address disparate funding and fragmented sources of
health data that lead to the current inadequacy of data for reliable, timely decision-making. The output
of HDC is more collaborative and efficient investment in country information systems and monitoring
and evaluation plans.
6. This meeting seeks to inform these stakeholder efforts and provide a common work plan for (1)
improved PHC performance measurement including research and development of less measured
domains of quality PHC and incorporation of these measures into existing measurement platforms and
(2) PHC improvement efforts including relevant guidance and tools and the WHO Global Challenge on
Primary Health Care Improvement.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
| P a g e 5
Acronym Index
AeHIN Asia eHealth Information Network
ASSD Africa Symposium on Statistical Development
BMGF
CoP
CQI
The Bill and Melinda Gates Foundation
Community of practice
Continuous quality improvement
CRVS Civil registration and vital statistics
DHIS District Health Information System
GAVI Global Alliance for Vaccines and Immunization
GFATM The Global Fund to Fight AIDS, Tuberculosis and Malaria
GFF Global Financing Facility in Support of Every Woman Every Child
GIZ German Corporation for International Cooperation
HDC Health data collaborative
HMIS Health management information system
IHP+ The international health partnership
IPCHS Integrated, people-centred health services
JICA Japan International Cooperation Agency
LMIC Low and Middle Income Countries
M&E Monitoring and evaluation
NHA National health accounts
NORAD Norwegian Agency for Development Cooperation
OECD Organisation for Economic Co-operation and Development
PEPFAR The United States President's Emergency Plan for AIDS Relief
PHC Primary health care
PHCPI Primary health care performance initiative
RBF Results based financing
SARA Service Availability and Readiness Assessment
SDG Sustainable development goal
SDI Service Delivery Indicators
SPA Service Provision Assessment
UHC Universal health coverage
UNFPA United Nations Population Fund
UNICEF United Nations Children's Fund
UNSD United Nations Statistical Division
USAID United States Agency for International Development
WBG World Bank Group
WHO World Health Organization
Acronym Index
AeHIN Asia eHealth Information Network
ASSD Africa Symposium on Statistical Development
BMGF
CoP
CQI
The Bill and Melinda Gates Foundation
Community of practice
Continuous quality improvement
CRVS Civil registration and vital statistics
DHIS District Health Information System
GAVI Global Alliance for Vaccines and Immunization
GFATM The Global Fund to Fight AIDS, Tuberculosis and Malaria
GFF Global Financing Facility in Support of Every Woman Every Child
GIZ German Corporation for International Cooperation
HDC Health data collaborative
HMIS Health management information system
IHP+ The international health partnership
IPCHS Integrated, people-centred health services
JICA Japan International Cooperation Agency
LMIC Low and Middle Income Countries
M&E Monitoring and evaluation
NHA National health accounts
NORAD Norwegian Agency for Development Cooperation
OECD Organisation for Economic Co-operation and Development
PEPFAR The United States President's Emergency Plan for AIDS Relief
PHC Primary health care
PHCPI Primary health care performance initiative
RBF Results based financing
SARA Service Availability and Readiness Assessment
SDG Sustainable development goal
SDI Service Delivery Indicators
SPA Service Provision Assessment
UHC Universal health coverage
UNFPA United Nations Population Fund
UNICEF United Nations Children's Fund
UNSD United Nations Statistical Division
USAID United States Agency for International Development
WBG World Bank Group
WHO World Health Organization

| P a g e 6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
| P a g e 7
Purpose
This document provides background on situation, challenges, and opportunities in the field of
measurement for improvement in primary health care (PHC). It then describes current, relevant multi-
stakeholder efforts to address these challenges and opportunities, followed by key questions for
consideration and potential deliverables for the global stakeholder community. These deliverables (some
underway, some proposed) are offered as a draft roadmap toward a collaborative process for supporting
country PHC measurement and improvement efforts. This document will undergo significant revision with
inputs from the PHC Improvement Global Stakeholder Meeting on 6-8 April to develop a work plan for (1)
improved PHC performance measurement including research and development of less measured domains of
quality PHC and incorporation of these measures into existing measurement platforms and (2) PHC
improvement efforts including the development of relevant guidance and tools and the WHO Global
Challenge on Primary Health Care Improvement.
Background
The highest attainable standard of health, including access to timely, acceptable, affordable, and high-
quality health care is a fundamental right of every human being. Primary health care (PHC), as a regular site
of first-access and on-going care with the capacity to address the majority of health problems, has long been
recognized as critical to attaining health for all.1 Numerous international reviews have bolstered this claim,
demonstrating that health systems based on high-performing PHC are able to achieve better health
outcomes, more equitably (even equilibrating the negative impact of social determinants of health), and at
lower relative cost than health systems that over emphasize selective disease-specific and/or hospital-based
care. 2,3,4,5
It is undeniable that strong PHC is foundational to achieving health for all, particularly the most
marginalized and vulnerable. In addition, strong PHC is essential to attaining today’s leading global health
objectives including Universal Health Coverage (UHC), Integrated People-centred Health Services (IPCHS)6,
and health related Sustainable Development Goals (SDGs). Yet, too often the potential of PHC for dramatic
improvements in the health of populations and function of health systems is undermined by lack of
1 Recognizing that primary care has variable definitions, this paper is grounded in the historical approach of primary health care established at
Alma Ata while emphasising health system and service delivery reforms relevant to primary care. We adopt a definition from the World Health
Report 2008: Primary health care – now more than ever: care that exhibits features of person-centeredness, comprehensiveness, integration,
continuity of care, participation of patients, families and communities. This requires health services that are organized with close-to-client
multidisciplinary teams responsible for a defined population, collaborate with social services and other sectors, and coordinate the contributions of
specialists and community organizations.
2 Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457-502
3 Kruk, Margaret Elizabeth, et al. "The Contribution of Primary Care to Health and Health Systems in Low-and Middle-Income Countries: a critical
review of major primary care initiatives." Social science & medicine 70.6 (2010): 904-911.
4 Starfield B. Policy relevant determinants of health: an international perspective. Health Policy, 2002, 60:201-218.
5 Rohde J, et al 30 years after Alma-Ata: has primary health care worked in countries?, The Lancet, Volume 372, Issue 9642, 13–19 September
2008, 950-961
6 WHO Framework on integrated people-centred health services was recently adopted by the 138th Session of the Executive Board, and will be
discussed at this year’s World Health Assembly. The framework proposes five interdependent strategies (including reorienting the model of care
around primary-care based systems) for health services to become more integrated and people-centred. The proposed resolution includes a request
for research and development on indicators to trace global progress on integrated people-centered health services; as well as technical support and
guidance to Member States for the implementation, national adaptation and operationalization of the framework.
http://apps.who.int/gb/ebwha/pdf_files/EB138/B138_37-en.pdf
Purpose
This document provides background on situation, challenges, and opportunities in the field of
measurement for improvement in primary health care (PHC). It then describes current, relevant multi-
stakeholder efforts to address these challenges and opportunities, followed by key questions for
consideration and potential deliverables for the global stakeholder community. These deliverables (some
underway, some proposed) are offered as a draft roadmap toward a collaborative process for supporting
country PHC measurement and improvement efforts. This document will undergo significant revision with
inputs from the PHC Improvement Global Stakeholder Meeting on 6-8 April to develop a work plan for (1)
improved PHC performance measurement including research and development of less measured domains of
quality PHC and incorporation of these measures into existing measurement platforms and (2) PHC
improvement efforts including the development of relevant guidance and tools and the WHO Global
Challenge on Primary Health Care Improvement.
Background
The highest attainable standard of health, including access to timely, acceptable, affordable, and high-
quality health care is a fundamental right of every human being. Primary health care (PHC), as a regular site
of first-access and on-going care with the capacity to address the majority of health problems, has long been
recognized as critical to attaining health for all.1 Numerous international reviews have bolstered this claim,
demonstrating that health systems based on high-performing PHC are able to achieve better health
outcomes, more equitably (even equilibrating the negative impact of social determinants of health), and at
lower relative cost than health systems that over emphasize selective disease-specific and/or hospital-based
care. 2,3,4,5
It is undeniable that strong PHC is foundational to achieving health for all, particularly the most
marginalized and vulnerable. In addition, strong PHC is essential to attaining today’s leading global health
objectives including Universal Health Coverage (UHC), Integrated People-centred Health Services (IPCHS)6,
and health related Sustainable Development Goals (SDGs). Yet, too often the potential of PHC for dramatic
improvements in the health of populations and function of health systems is undermined by lack of
1 Recognizing that primary care has variable definitions, this paper is grounded in the historical approach of primary health care established at
Alma Ata while emphasising health system and service delivery reforms relevant to primary care. We adopt a definition from the World Health
Report 2008: Primary health care – now more than ever: care that exhibits features of person-centeredness, comprehensiveness, integration,
continuity of care, participation of patients, families and communities. This requires health services that are organized with close-to-client
multidisciplinary teams responsible for a defined population, collaborate with social services and other sectors, and coordinate the contributions of
specialists and community organizations.
2 Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457-502
3 Kruk, Margaret Elizabeth, et al. "The Contribution of Primary Care to Health and Health Systems in Low-and Middle-Income Countries: a critical
review of major primary care initiatives." Social science & medicine 70.6 (2010): 904-911.
4 Starfield B. Policy relevant determinants of health: an international perspective. Health Policy, 2002, 60:201-218.
5 Rohde J, et al 30 years after Alma-Ata: has primary health care worked in countries?, The Lancet, Volume 372, Issue 9642, 13–19 September
2008, 950-961
6 WHO Framework on integrated people-centred health services was recently adopted by the 138th Session of the Executive Board, and will be
discussed at this year’s World Health Assembly. The framework proposes five interdependent strategies (including reorienting the model of care
around primary-care based systems) for health services to become more integrated and people-centred. The proposed resolution includes a request
for research and development on indicators to trace global progress on integrated people-centered health services; as well as technical support and
guidance to Member States for the implementation, national adaptation and operationalization of the framework.
http://apps.who.int/gb/ebwha/pdf_files/EB138/B138_37-en.pdf
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
| P a g e 8
emphasis and underinvestment. As a result, PHC implementation has lagged far behind its aspirational
objectives: continuing to focus on the delivery of a basic package of health interventions for selected priority
diseases rather than comprehensive care, ineffective decentralization that impedes PHC from responding to
local conditions, failing to focus on improved coordination between providers and levels of care, missing out
on the benefits of multidisciplinary care, limiting access hours of PHC facilities, and under-emphasising
health work force development and retention resulting in overworked and under-supported staff.
In most countries, little is known about the performance of PHC, particularly in service delivery domains
that are critical to its effectiveness but often not well measured: access7, comprehensiveness8, continuity9,
coordination10, people-centeredness11 (family and community orientation), and quality (both technical and
interpersonal). These domains characterize high-quality primary care (as first contact care) and help explain
performance variation across country contexts, in all settings from low- to high-income countries. While
there are numerous typologies of primary care, not all of them lead to desirable outcomes and impact.
Measuring these domains of high quality PHC acknowledges their importance in explaining performance
variation and can lead to critical reforms. Increased and improved measurement of PHC performance, with
measures relevant to community, facility, district and national processes, is needed to promote
accountability and guide improvement efforts at each level of the health system. There is tremendous
opportunity to have a major impact on health through targeted measurement of what drives strong primary
health care systems and better utilization of these data for improvement by stakeholders at all levels of the
health system.
Several recent collaborative efforts by international development agencies have drawn further attention
to this area including the Health Data Collaborative (HDC)12 and the Primary Health Care Performance
Initiative (PHCPI). 13 HDC seeks to facilitate and accelerate progress in strengthening country systems for
monitoring progress and performance for accountability and transparency within the context of the health
related SDGs. PHCPI brings together partners to improve PHC in low- and middle-income countries through
better measurement to inform and accelerate national and sub-national PHC progress and knowledge-
sharing.
As a key next step, this meeting serves to engage leadership of Member States, partner organizations,
international development associations, academic partners and WHO to move toward a common roadmap
for strengthened PHC measurement and improvement. Stakeholder input obtained through this meeting will
be used to shape the concrete steps needed to advance the measurement and improvement agenda,
including: (1) improved performance measurement (2) research and development for under-measured
domains (3) improved transparency and accountability (4) and evidence-informed decision making all
leading to (5) performance improvement.
7 Access: Available, affordable services in close proximity to people. Primary care serves as the entry point into the health care system and the
first and regular source of care for most health needs.
8 Comprehensiveness: Delivers a broad spectrum of preventive, promotive, curative and palliative care across the life-course
9 Continuity: Individuals have a relationship with same provider and team over time, health information is available over time, and health
management plans are continuous.
10 Coordination: Primary care offers a hub from which people are guided through the health system, managing care across levels, referring to
specialists as needed and effectively following-up to monitor health progress.
11People-centeredness: an approach to care that consciously adopts individuals’, carers’, families’ and communities’ perspectives as
participants in, and beneficiaries of, trusted health systems that are organized around the comprehensive needs of people rather than individual
diseases, and respects their preferences. People-centred care also requires that patients have the education and support they need to make
decisions and participate in their own care and that carers are able to attain maximal function within a supportive working environment. People-
centred care is broader than patient and person-centred care, encompassing not only clinical encounters, but also including attention to the health of
people in their communities and their crucial role in shaping health policy and health services.
12 Health Data Collaborative www.healthdatacollaborative.org
13 Primary Health Care Performance Initiative www.phcperformanceinitiative.org
emphasis and underinvestment. As a result, PHC implementation has lagged far behind its aspirational
objectives: continuing to focus on the delivery of a basic package of health interventions for selected priority
diseases rather than comprehensive care, ineffective decentralization that impedes PHC from responding to
local conditions, failing to focus on improved coordination between providers and levels of care, missing out
on the benefits of multidisciplinary care, limiting access hours of PHC facilities, and under-emphasising
health work force development and retention resulting in overworked and under-supported staff.
In most countries, little is known about the performance of PHC, particularly in service delivery domains
that are critical to its effectiveness but often not well measured: access7, comprehensiveness8, continuity9,
coordination10, people-centeredness11 (family and community orientation), and quality (both technical and
interpersonal). These domains characterize high-quality primary care (as first contact care) and help explain
performance variation across country contexts, in all settings from low- to high-income countries. While
there are numerous typologies of primary care, not all of them lead to desirable outcomes and impact.
Measuring these domains of high quality PHC acknowledges their importance in explaining performance
variation and can lead to critical reforms. Increased and improved measurement of PHC performance, with
measures relevant to community, facility, district and national processes, is needed to promote
accountability and guide improvement efforts at each level of the health system. There is tremendous
opportunity to have a major impact on health through targeted measurement of what drives strong primary
health care systems and better utilization of these data for improvement by stakeholders at all levels of the
health system.
Several recent collaborative efforts by international development agencies have drawn further attention
to this area including the Health Data Collaborative (HDC)12 and the Primary Health Care Performance
Initiative (PHCPI). 13 HDC seeks to facilitate and accelerate progress in strengthening country systems for
monitoring progress and performance for accountability and transparency within the context of the health
related SDGs. PHCPI brings together partners to improve PHC in low- and middle-income countries through
better measurement to inform and accelerate national and sub-national PHC progress and knowledge-
sharing.
As a key next step, this meeting serves to engage leadership of Member States, partner organizations,
international development associations, academic partners and WHO to move toward a common roadmap
for strengthened PHC measurement and improvement. Stakeholder input obtained through this meeting will
be used to shape the concrete steps needed to advance the measurement and improvement agenda,
including: (1) improved performance measurement (2) research and development for under-measured
domains (3) improved transparency and accountability (4) and evidence-informed decision making all
leading to (5) performance improvement.
7 Access: Available, affordable services in close proximity to people. Primary care serves as the entry point into the health care system and the
first and regular source of care for most health needs.
8 Comprehensiveness: Delivers a broad spectrum of preventive, promotive, curative and palliative care across the life-course
9 Continuity: Individuals have a relationship with same provider and team over time, health information is available over time, and health
management plans are continuous.
10 Coordination: Primary care offers a hub from which people are guided through the health system, managing care across levels, referring to
specialists as needed and effectively following-up to monitor health progress.
11People-centeredness: an approach to care that consciously adopts individuals’, carers’, families’ and communities’ perspectives as
participants in, and beneficiaries of, trusted health systems that are organized around the comprehensive needs of people rather than individual
diseases, and respects their preferences. People-centred care also requires that patients have the education and support they need to make
decisions and participate in their own care and that carers are able to attain maximal function within a supportive working environment. People-
centred care is broader than patient and person-centred care, encompassing not only clinical encounters, but also including attention to the health of
people in their communities and their crucial role in shaping health policy and health services.
12 Health Data Collaborative www.healthdatacollaborative.org
13 Primary Health Care Performance Initiative www.phcperformanceinitiative.org
| P a g e 9
Measurement
In order to improve primary health care performance, countries, districts, and facilities first need
information about how their systems are performing and what barriers are preventing them from delivering
high-quality, patient-centered primary care services. The last decade saw progress in many low- and middle-
income countries toward producing, using, and sharing health data; yet, most country health information
systems still do not meet current data demands.
In many countries data collection is not harmonized around the needs of planners and managers, but
rather numerous reporting tools to meet the stated objectives of multiple implementers and stakeholders.
This lack of coordination requires an enormous data collection effort from already overburdened human
resources. At times country HMIS efforts are siloed or lack interoperability, missing out on opportunities for
analysis of complex, crosscutting problems. Far too often, there are limited resources for HMIS reforms.
Even where coordinated, high-functioning systems exist, data quality assurance can remain challenging.
Traditionally, measures of PHC performance have focused on quantifying the inputs—human resources,
facilities, and financing, for example—and describing service delivery volume and outcomes, including
disease-specific morbidity and mortality. Measurement of quality service delivery has been largely
neglected, as has the experience of patients, health workers, and communities in seeking, accessing and
delivering health services. Most countries, districts, and facilities lack data on many of the core functions of
quality PHC (first contact accessibility, continuity, coordination, and comprehensiveness), patient-
centeredness and responsiveness, and primary care organization and management. This lack of data and
knowledge about which components of service delivery and organization need strengthening impedes the
ability of actors at all levels of the health system to take action for improvement.
Ideally, measurement of PHC functions and service delivery should be occurring in a coordinated way at
the community and facility, subnational and national levels. In such a system, actors at each level of the
system - national planners and policy makers, sub-national managers, and providers and communities -
would be able to access and use standardized and interoperable data collection platforms to track key
performance indicators to continually assess the quality and effectiveness of care delivered and proactively
plan for future service delivery needs as well as identify areas where change in existing systems and policies
are needed.
Data needs for these activities range from measurement of the local burden of disease to drug and
supply availability and from health worker performance and motivation to experiential quality and results of
care delivery. Subnational-level decision makers need access to this information from facilities in their
catchment area in order to track trends in performance and outcomes over time, quickly detect and act
upon emerging issues and gaps, and identify positive outliers to extract and spread promising practices. The
same is true at the national level, where timely information from districts is converted to knowledge to drive
action for improvement and used to inform future practices, policies and strategic planning. At the global
level, measurement informs global surveillance efforts, donor investment priorities, and international
policies. At all levels, measurement is a tool for enabling comparability, identifying promising practices for
sharing, and creating accountable and transparent systems that are responsive to the needs of their
constituents.
Monitoring and Evaluation Framework
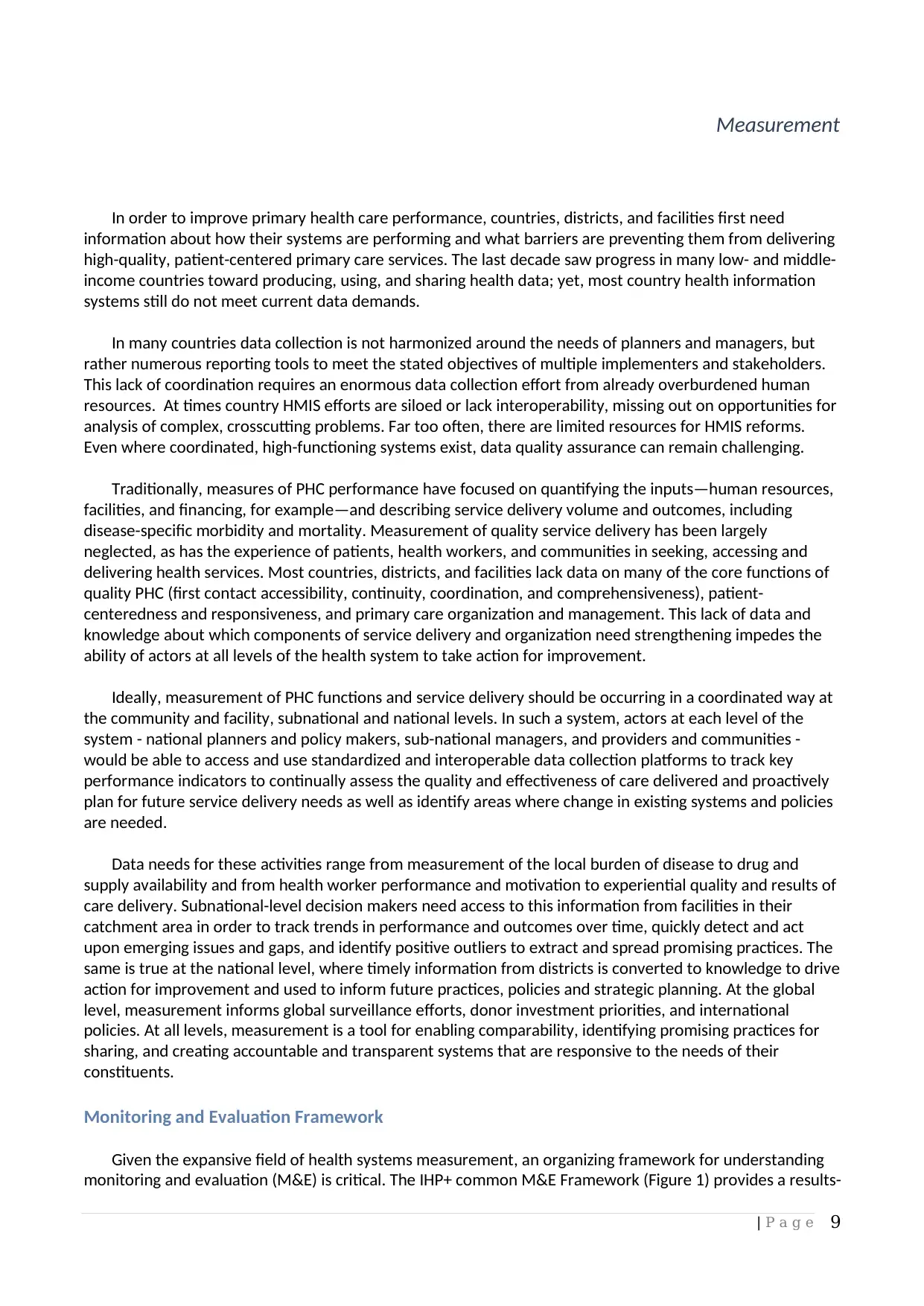
Given the expansive field of health systems measurement, an organizing framework for understanding
monitoring and evaluation (M&E) is critical. The IHP+ common M&E Framework (Figure 1) provides a results-
Measurement
In order to improve primary health care performance, countries, districts, and facilities first need
information about how their systems are performing and what barriers are preventing them from delivering
high-quality, patient-centered primary care services. The last decade saw progress in many low- and middle-
income countries toward producing, using, and sharing health data; yet, most country health information
systems still do not meet current data demands.
In many countries data collection is not harmonized around the needs of planners and managers, but
rather numerous reporting tools to meet the stated objectives of multiple implementers and stakeholders.
This lack of coordination requires an enormous data collection effort from already overburdened human
resources. At times country HMIS efforts are siloed or lack interoperability, missing out on opportunities for
analysis of complex, crosscutting problems. Far too often, there are limited resources for HMIS reforms.
Even where coordinated, high-functioning systems exist, data quality assurance can remain challenging.
Traditionally, measures of PHC performance have focused on quantifying the inputs—human resources,
facilities, and financing, for example—and describing service delivery volume and outcomes, including
disease-specific morbidity and mortality. Measurement of quality service delivery has been largely
neglected, as has the experience of patients, health workers, and communities in seeking, accessing and
delivering health services. Most countries, districts, and facilities lack data on many of the core functions of
quality PHC (first contact accessibility, continuity, coordination, and comprehensiveness), patient-
centeredness and responsiveness, and primary care organization and management. This lack of data and
knowledge about which components of service delivery and organization need strengthening impedes the
ability of actors at all levels of the health system to take action for improvement.
Ideally, measurement of PHC functions and service delivery should be occurring in a coordinated way at
the community and facility, subnational and national levels. In such a system, actors at each level of the
system - national planners and policy makers, sub-national managers, and providers and communities -
would be able to access and use standardized and interoperable data collection platforms to track key
performance indicators to continually assess the quality and effectiveness of care delivered and proactively
plan for future service delivery needs as well as identify areas where change in existing systems and policies
are needed.
Data needs for these activities range from measurement of the local burden of disease to drug and
supply availability and from health worker performance and motivation to experiential quality and results of
care delivery. Subnational-level decision makers need access to this information from facilities in their
catchment area in order to track trends in performance and outcomes over time, quickly detect and act
upon emerging issues and gaps, and identify positive outliers to extract and spread promising practices. The
same is true at the national level, where timely information from districts is converted to knowledge to drive
action for improvement and used to inform future practices, policies and strategic planning. At the global
level, measurement informs global surveillance efforts, donor investment priorities, and international
policies. At all levels, measurement is a tool for enabling comparability, identifying promising practices for
sharing, and creating accountable and transparent systems that are responsive to the needs of their
constituents.
Monitoring and Evaluation Framework
Given the expansive field of health systems measurement, an organizing framework for understanding
monitoring and evaluation (M&E) is critical. The IHP+ common M&E Framework (Figure 1) provides a results-
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
| P a g e 10
chain representation of the key components of a national M&E strategy. It identifies four major indicator
domains: system inputs and processes, outputs, outcomes, and impact. The framework demonstrates how
inputs to the system and processes result in outputs, outcomes and impact. The framework facilitates the
identification of core indicators along the results chain, while also identifying key data collection methods.
The framework also highlights the need for analysis and synthesis of data from multiple sources, including
data quality assessment; and demonstrates how the data need to be communicated and used to inform
decision-making at different levels.
Figure 1. IHP+ common M&E framework14
Establishing priorities for PHC measurement
The above framework addresses the key components of a monitoring and evaluation strategy; however,
current monitoring and evaluation efforts have overemphasized inputs, outcomes and impact without
sufficiently focusing on crosscutting processes at various levels of service delivery – including information on
clinical quality and safety. Several efforts at PHC performance assessment frameworks have been
undertaken historically; however, due to difficult/costly methodologies, lack of integration into routine data
collection efforts, and under emphasis of crosscutting issues, few have had sufficient uptake and integration
into national monitoring and evaluation strategies to have sustainable impact.
Despite the vast array of surveys and facility assessment conducted in LMICs, many core PHC service
delivery concepts are not routinely measured effectively. For example, existing data collection
methodologies in use in LMICs do not adequately capture indicators of the four functions of PHC—first
contact accessibility, continuity, comprehensiveness, and coordination. Although the centrality of these
functions to primary care is consistent across high, middle, and low-income settings, most existing measures
14 WHO. Monitoring, evaluation and review of national health strategies: a country-led platform for information and accountability. 2011.
http://www.internationalhealthpartnership.net/fileadmin/uploads/ihp/Documents/Tools/M_E_Framework/M%26E.framework.2011.pdf
chain representation of the key components of a national M&E strategy. It identifies four major indicator
domains: system inputs and processes, outputs, outcomes, and impact. The framework demonstrates how
inputs to the system and processes result in outputs, outcomes and impact. The framework facilitates the
identification of core indicators along the results chain, while also identifying key data collection methods.
The framework also highlights the need for analysis and synthesis of data from multiple sources, including
data quality assessment; and demonstrates how the data need to be communicated and used to inform
decision-making at different levels.
Figure 1. IHP+ common M&E framework14
Establishing priorities for PHC measurement
The above framework addresses the key components of a monitoring and evaluation strategy; however,
current monitoring and evaluation efforts have overemphasized inputs, outcomes and impact without
sufficiently focusing on crosscutting processes at various levels of service delivery – including information on
clinical quality and safety. Several efforts at PHC performance assessment frameworks have been
undertaken historically; however, due to difficult/costly methodologies, lack of integration into routine data
collection efforts, and under emphasis of crosscutting issues, few have had sufficient uptake and integration
into national monitoring and evaluation strategies to have sustainable impact.
Despite the vast array of surveys and facility assessment conducted in LMICs, many core PHC service
delivery concepts are not routinely measured effectively. For example, existing data collection
methodologies in use in LMICs do not adequately capture indicators of the four functions of PHC—first
contact accessibility, continuity, comprehensiveness, and coordination. Although the centrality of these
functions to primary care is consistent across high, middle, and low-income settings, most existing measures
14 WHO. Monitoring, evaluation and review of national health strategies: a country-led platform for information and accountability. 2011.
http://www.internationalhealthpartnership.net/fileadmin/uploads/ihp/Documents/Tools/M_E_Framework/M%26E.framework.2011.pdf
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
| P a g e 11
are currently validated and used in only high-income countries. Expert consensus is that these measures are
not applicable to most LMICs, particularly fragile states. This leads to the paradoxical situation of many low
and middle-income countries in which countries are overwhelmed by data and reporting requirements, but
lack critical data for decision-making and improvement efforts.
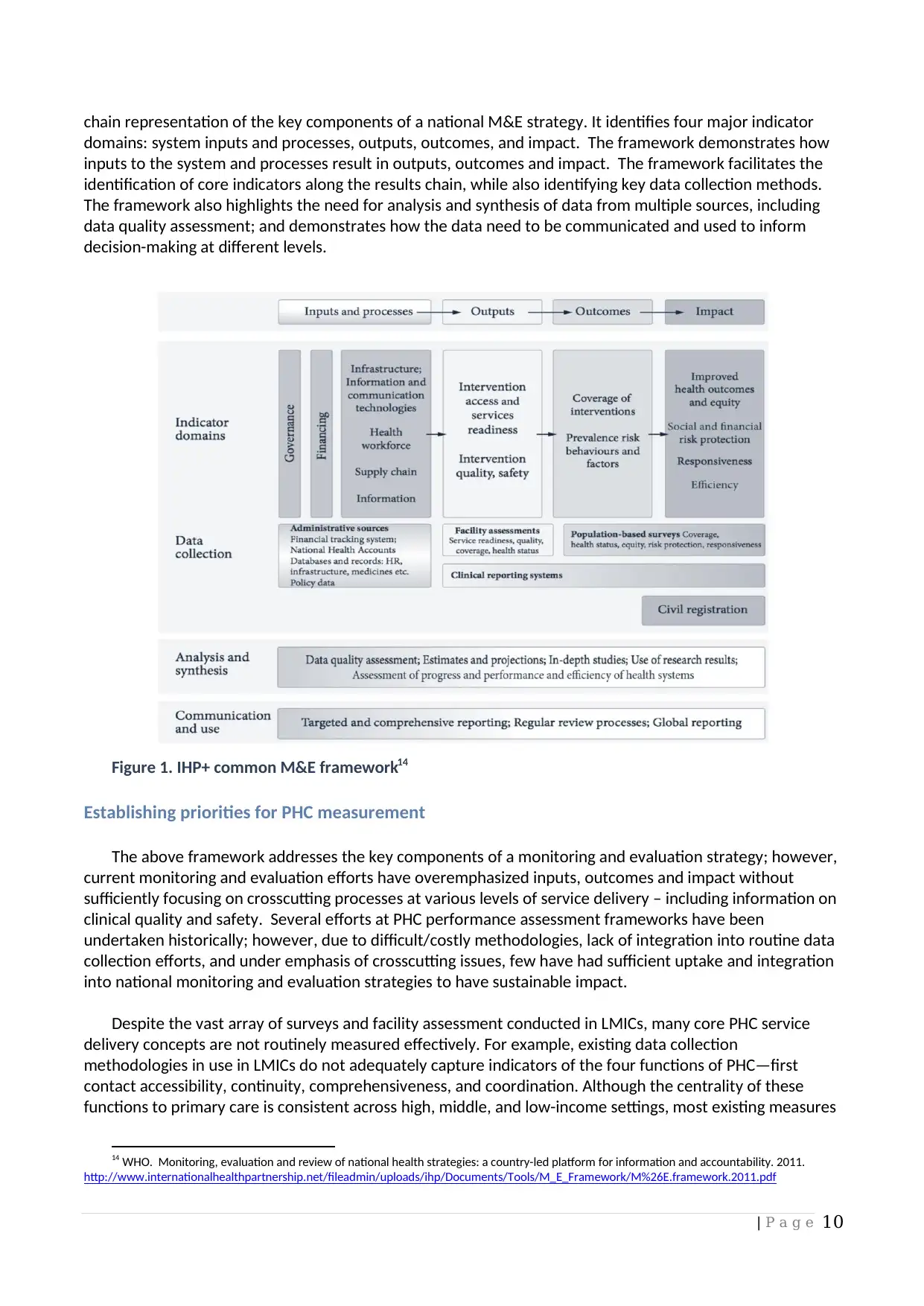
The Primary Health Care Performance Initiative (PHCPI) 15 framework (Figure 2) attempts to address
these challenges by more explicitly articulating the key inputs, functionalities, and desired goals of an
effective PHC system. This framework draws from other measurement frameworks while offering a novel
focus on the intersection between service delivery and the core functions of PHC as key drivers of
performance variation. The PHCPI Conceptual Framework highlights people- and community-centered care,
supply and demand functions, and integrated service delivery through effective organization and
management.
Figure 2. Primary Health Care Performance Initiative Framework
Based on an extensive review of the scientific literature and consultations with international experts and
health systems practitioners across the globe, PHCPI also identified and selected indicators to assess the
performance of country primary health care systems, understand the root causes of primary health care
performance and give countries more clarity on what and how to improve.
Using a rigorous process, a core set of internationally comparable indicators and an expanded set of
indicators were selected to help countries assess overall primary health care system performance (Core set:
Vital Signs indicators – See Annex 3) and identify performance determinants (Expanded set: Diagnostic
indicators), while recognizing that each country will collect a unique set of indicators based upon country
priorities in each domain. The chosen Vital Signs indicators align and complement the Global Reference List
of 100 Core Health Indicators16 by focusing on important service delivery processes that are crucial for
15 The Primary Health Care Performance Initiative (PHCPI) is a new partnership that brings together country policymakers, health system
managers, practitioners, advocates and other development partners to catalyze improvements in primary health care (PHC) in low- and middle-
income countries through better measurement and knowledge sharing. PHCPI was officially launched by the Bill & Melinda Gates Foundation, World
Bank Group, and World Health Organization on the sidelines of the UN General Assembly in September 2015. www.phcperformanceinitiative.org
16 Developed through technical consultation of the Interagency Working Group on Indicators and Reporting Burden in 2013 and updated in
2015, the Global Reference List of 100 Core Health Indicators is a standard set of 100 core indicators prioritized by the global community to provide
concise information on the health situation and trends including responses at national and global levels.
http://www.who.int/healthinfo/indicators/2015/en/
are currently validated and used in only high-income countries. Expert consensus is that these measures are
not applicable to most LMICs, particularly fragile states. This leads to the paradoxical situation of many low
and middle-income countries in which countries are overwhelmed by data and reporting requirements, but
lack critical data for decision-making and improvement efforts.
The Primary Health Care Performance Initiative (PHCPI) 15 framework (Figure 2) attempts to address
these challenges by more explicitly articulating the key inputs, functionalities, and desired goals of an
effective PHC system. This framework draws from other measurement frameworks while offering a novel
focus on the intersection between service delivery and the core functions of PHC as key drivers of
performance variation. The PHCPI Conceptual Framework highlights people- and community-centered care,
supply and demand functions, and integrated service delivery through effective organization and
management.
Figure 2. Primary Health Care Performance Initiative Framework
Based on an extensive review of the scientific literature and consultations with international experts and
health systems practitioners across the globe, PHCPI also identified and selected indicators to assess the
performance of country primary health care systems, understand the root causes of primary health care
performance and give countries more clarity on what and how to improve.
Using a rigorous process, a core set of internationally comparable indicators and an expanded set of
indicators were selected to help countries assess overall primary health care system performance (Core set:
Vital Signs indicators – See Annex 3) and identify performance determinants (Expanded set: Diagnostic
indicators), while recognizing that each country will collect a unique set of indicators based upon country
priorities in each domain. The chosen Vital Signs indicators align and complement the Global Reference List
of 100 Core Health Indicators16 by focusing on important service delivery processes that are crucial for
15 The Primary Health Care Performance Initiative (PHCPI) is a new partnership that brings together country policymakers, health system
managers, practitioners, advocates and other development partners to catalyze improvements in primary health care (PHC) in low- and middle-
income countries through better measurement and knowledge sharing. PHCPI was officially launched by the Bill & Melinda Gates Foundation, World
Bank Group, and World Health Organization on the sidelines of the UN General Assembly in September 2015. www.phcperformanceinitiative.org
16 Developed through technical consultation of the Interagency Working Group on Indicators and Reporting Burden in 2013 and updated in
2015, the Global Reference List of 100 Core Health Indicators is a standard set of 100 core indicators prioritized by the global community to provide
concise information on the health situation and trends including responses at national and global levels.
http://www.who.int/healthinfo/indicators/2015/en/
| P a g e 12
achieving universal health coverage and other global priorities. Diagnostic indicators, which provide more
detailed information to identify performance gaps are, by nature, less internationally comparable, and will
need to be tailored to country context and health management information system (HMIS) capacities.
Currently available information on LMIC performance related to the Vital Signs can be found on the PHCPI
website at www.phcperformanceintiative.org.
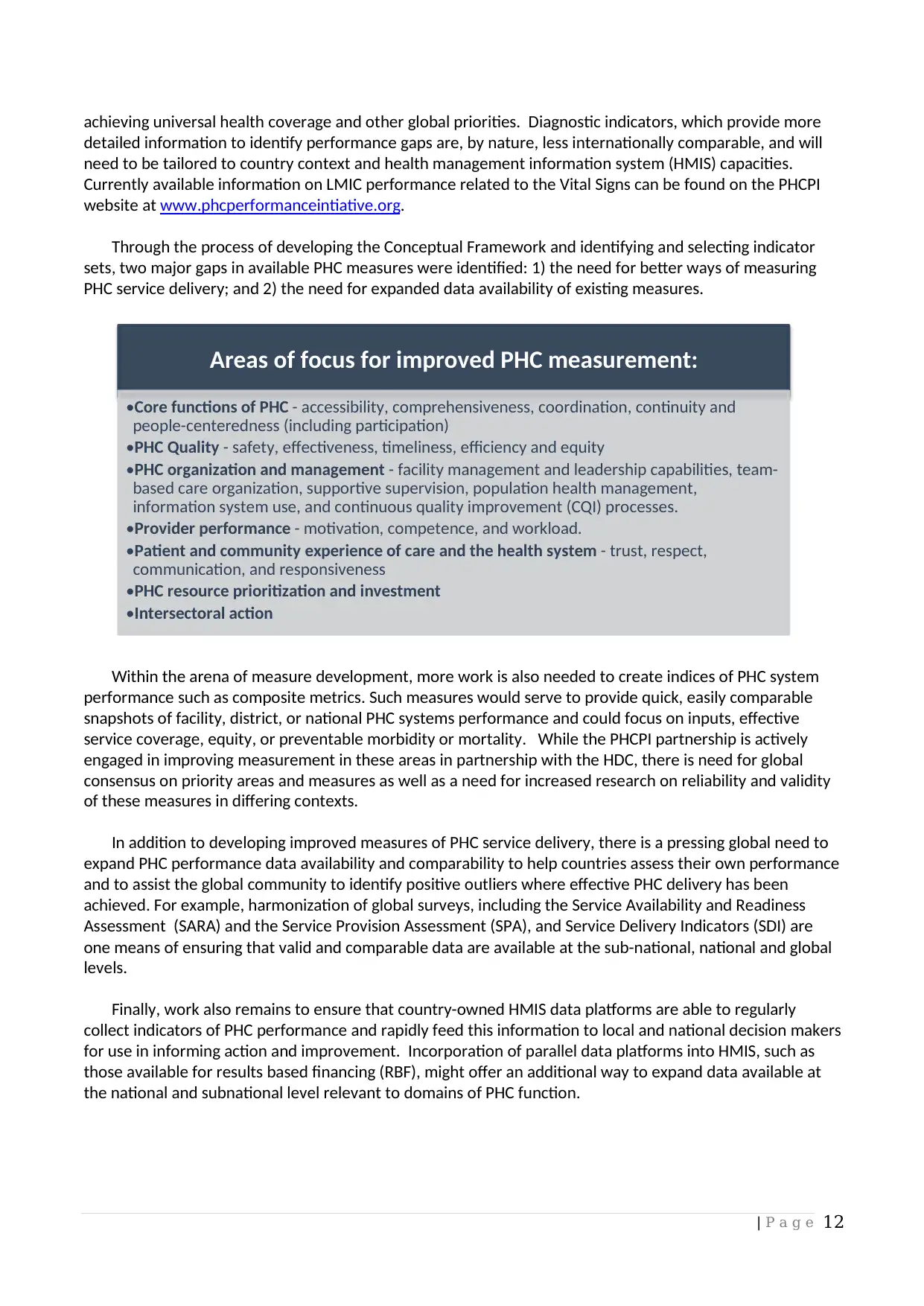
Through the process of developing the Conceptual Framework and identifying and selecting indicator
sets, two major gaps in available PHC measures were identified: 1) the need for better ways of measuring
PHC service delivery; and 2) the need for expanded data availability of existing measures.
Within the arena of measure development, more work is also needed to create indices of PHC system
performance such as composite metrics. Such measures would serve to provide quick, easily comparable
snapshots of facility, district, or national PHC systems performance and could focus on inputs, effective
service coverage, equity, or preventable morbidity or mortality. While the PHCPI partnership is actively
engaged in improving measurement in these areas in partnership with the HDC, there is need for global
consensus on priority areas and measures as well as a need for increased research on reliability and validity
of these measures in differing contexts.
In addition to developing improved measures of PHC service delivery, there is a pressing global need to
expand PHC performance data availability and comparability to help countries assess their own performance
and to assist the global community to identify positive outliers where effective PHC delivery has been
achieved. For example, harmonization of global surveys, including the Service Availability and Readiness
Assessment (SARA) and the Service Provision Assessment (SPA), and Service Delivery Indicators (SDI) are
one means of ensuring that valid and comparable data are available at the sub-national, national and global
levels.
Finally, work also remains to ensure that country-owned HMIS data platforms are able to regularly
collect indicators of PHC performance and rapidly feed this information to local and national decision makers
for use in informing action and improvement. Incorporation of parallel data platforms into HMIS, such as
those available for results based financing (RBF), might offer an additional way to expand data available at
the national and subnational level relevant to domains of PHC function.
Areas of focus for improved PHC measurement:
•Core functions of PHC - accessibility, comprehensiveness, coordination, continuity and
people-centeredness (including participation)
•PHC Quality - safety, effectiveness, timeliness, efficiency and equity
•PHC organization and management - facility management and leadership capabilities, team-
based care organization, supportive supervision, population health management,
information system use, and continuous quality improvement (CQI) processes.
•Provider performance - motivation, competence, and workload.
•Patient and community experience of care and the health system - trust, respect,
communication, and responsiveness
•PHC resource prioritization and investment
•Intersectoral action
achieving universal health coverage and other global priorities. Diagnostic indicators, which provide more
detailed information to identify performance gaps are, by nature, less internationally comparable, and will
need to be tailored to country context and health management information system (HMIS) capacities.
Currently available information on LMIC performance related to the Vital Signs can be found on the PHCPI
website at www.phcperformanceintiative.org.
Through the process of developing the Conceptual Framework and identifying and selecting indicator
sets, two major gaps in available PHC measures were identified: 1) the need for better ways of measuring
PHC service delivery; and 2) the need for expanded data availability of existing measures.
Within the arena of measure development, more work is also needed to create indices of PHC system
performance such as composite metrics. Such measures would serve to provide quick, easily comparable
snapshots of facility, district, or national PHC systems performance and could focus on inputs, effective
service coverage, equity, or preventable morbidity or mortality. While the PHCPI partnership is actively
engaged in improving measurement in these areas in partnership with the HDC, there is need for global
consensus on priority areas and measures as well as a need for increased research on reliability and validity
of these measures in differing contexts.
In addition to developing improved measures of PHC service delivery, there is a pressing global need to
expand PHC performance data availability and comparability to help countries assess their own performance
and to assist the global community to identify positive outliers where effective PHC delivery has been
achieved. For example, harmonization of global surveys, including the Service Availability and Readiness
Assessment (SARA) and the Service Provision Assessment (SPA), and Service Delivery Indicators (SDI) are
one means of ensuring that valid and comparable data are available at the sub-national, national and global
levels.
Finally, work also remains to ensure that country-owned HMIS data platforms are able to regularly
collect indicators of PHC performance and rapidly feed this information to local and national decision makers
for use in informing action and improvement. Incorporation of parallel data platforms into HMIS, such as
those available for results based financing (RBF), might offer an additional way to expand data available at
the national and subnational level relevant to domains of PHC function.
Areas of focus for improved PHC measurement:
•Core functions of PHC - accessibility, comprehensiveness, coordination, continuity and
people-centeredness (including participation)
•PHC Quality - safety, effectiveness, timeliness, efficiency and equity
•PHC organization and management - facility management and leadership capabilities, team-
based care organization, supportive supervision, population health management,
information system use, and continuous quality improvement (CQI) processes.
•Provider performance - motivation, competence, and workload.
•Patient and community experience of care and the health system - trust, respect,
communication, and responsiveness
•PHC resource prioritization and investment
•Intersectoral action
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 25
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




