NSN431 Health Service Analysis: Independent Nursing Practice Model
VerifiedAdded on 2023/06/15
|24
|6412
|458
Report
AI Summary
This report provides a comprehensive analysis of the Independent Nursing Practice (INP) model within the healthcare sector, focusing on its application in an aged residential care setting. It evaluates the strengths and weaknesses of the model, explores opportunities for collaboration with other healthcare professionals, and addresses barriers to change. The analysis considers patient demographics, factors influencing consumer care provision, and the social determinants of health impacting elderly patients. Strategies for improvement are proposed, including enhancing patient experience and fostering strategic cultural alignment, while also acknowledging challenges such as time constraints, cost of care, and resistance from general physicians. The report highlights the potential of INP to improve access to quality care, promote health education, and enhance the overall healthcare infrastructure through effective collaboration and a patient-centric approach. Desklib offers a platform to access this and many other solved assignments and past papers.

Running head: Transforming Healthcare Services
Transforming Healthcare Services
-An approach towards Independent Nursing Practitioners
Name of the Student
Name of the University
Author Note
Transforming Healthcare Services
-An approach towards Independent Nursing Practitioners
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1Transforming Healthcare Services
Abstract:
Advanced nursing practice (APN) comprises of roles like nursing midwifery, clinical
nurse specialist, nurse anesthetist and nurse practitioners. Independent Nursing Practice (INP)
is a form of nursing practitioner profession, in which the nurses can work independently, but
with collaboration, with other healthcare professionals like general physicians,
pharmacologists, social care workers and other professionals from a multidisciplinary
healthcare team. The INP is required to be highly mobile, and deliver care in various setups
ranging from patient’s homes to various healthcare and daycare facilities. The profession
faces different challenges in its implementation, and the aim of this report is to analyze the
strengths and weaknesses of the model, and explore the opportunities for collaboration with
other healthcare professionals, keeping in mind that through effective collaborations, the
model can be further improved. The barriers and challenges towards the implementation of
change are also discussed in the report. The strengths of the model include flexibility of
practice, does not require physician supervision, can allow the nurses to act as teachers and
counselors for the patients. However several healthcare organizations do not have sufficient
trust on the competencies of independent nursing practice that can merit its utilization,
independent of general physicians. Provision for support is offered by Nursing and
Midwifery board though endorsements for advanced clinical nursing practice. Other strengths
include the ability of the practice being conducted in different settings, which increases
accessibility to healthcare services and increase the range of healthcare setups supported by
healthcare organizations. INP can also be effective model for the care of elderly patients,
considering how the practice can address the needs identified through the social determinants
of health. INP also fosters the development of active collaboration within a multidisciplinary
healthcare team and develops a culture where the quality of care can be constantly developed.
Abstract:
Advanced nursing practice (APN) comprises of roles like nursing midwifery, clinical
nurse specialist, nurse anesthetist and nurse practitioners. Independent Nursing Practice (INP)
is a form of nursing practitioner profession, in which the nurses can work independently, but
with collaboration, with other healthcare professionals like general physicians,
pharmacologists, social care workers and other professionals from a multidisciplinary
healthcare team. The INP is required to be highly mobile, and deliver care in various setups
ranging from patient’s homes to various healthcare and daycare facilities. The profession
faces different challenges in its implementation, and the aim of this report is to analyze the
strengths and weaknesses of the model, and explore the opportunities for collaboration with
other healthcare professionals, keeping in mind that through effective collaborations, the
model can be further improved. The barriers and challenges towards the implementation of
change are also discussed in the report. The strengths of the model include flexibility of
practice, does not require physician supervision, can allow the nurses to act as teachers and
counselors for the patients. However several healthcare organizations do not have sufficient
trust on the competencies of independent nursing practice that can merit its utilization,
independent of general physicians. Provision for support is offered by Nursing and
Midwifery board though endorsements for advanced clinical nursing practice. Other strengths
include the ability of the practice being conducted in different settings, which increases
accessibility to healthcare services and increase the range of healthcare setups supported by
healthcare organizations. INP can also be effective model for the care of elderly patients,
considering how the practice can address the needs identified through the social determinants
of health. INP also fosters the development of active collaboration within a multidisciplinary
healthcare team and develops a culture where the quality of care can be constantly developed.
2Transforming Healthcare Services
The strategies of improvement in the existing model can be implemented at two levels:
patient experience and strategic cultural alignment. The steps can be divided into four stages:
complex care, development of partnership network and value based care and incorporating
strategic enablers like branding of services, technology, facility planning, etc. However, the
different factors that affect services should also be considered. Strengths and weaknesses of
service can also be measured through the value of services, calculated by the equation device
by UK healthcare. INP also allows access to quality care in a coordinated and patient centric
manner, it fosters health promotion through health education and training, and it also
improves affordability of healthcare services, as well as improves the overall health
infrastructure. Collaboration of care can also be developed through leadership and
commitment, attributed in nursing profession, apart from fostering health literacy and
improving access to affordable and high quality care. Different barriers to the practice
includes the providence of adequate time, and time lost in the regular travelling, the cost of
care as well as resistance from general physicians in acknowledging INP as a credible
healthcare option. However an effective collaboration such barriers can be overcome, and
ensure that the nursing profession flourishes further.
The strategies of improvement in the existing model can be implemented at two levels:
patient experience and strategic cultural alignment. The steps can be divided into four stages:
complex care, development of partnership network and value based care and incorporating
strategic enablers like branding of services, technology, facility planning, etc. However, the
different factors that affect services should also be considered. Strengths and weaknesses of
service can also be measured through the value of services, calculated by the equation device
by UK healthcare. INP also allows access to quality care in a coordinated and patient centric
manner, it fosters health promotion through health education and training, and it also
improves affordability of healthcare services, as well as improves the overall health
infrastructure. Collaboration of care can also be developed through leadership and
commitment, attributed in nursing profession, apart from fostering health literacy and
improving access to affordable and high quality care. Different barriers to the practice
includes the providence of adequate time, and time lost in the regular travelling, the cost of
care as well as resistance from general physicians in acknowledging INP as a credible
healthcare option. However an effective collaboration such barriers can be overcome, and
ensure that the nursing profession flourishes further.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3Transforming Healthcare Services
Contents
ABSTRACT:..............................................................................................................................1
Introduction:...............................................................................................................................4
Description of the current service:.............................................................................................4
Patient Demographics:...............................................................................................................5
Factors Influencing Consumer Care Provision or Access..........................................................5
Current Model of Care:..............................................................................................................8
Strengths and Weaknesses of Health Service:.........................................................................13
Proposed NP Model:................................................................................................................14
Conclusion:..............................................................................................................................15
Recommendations:...................................................................................................................16
References:...............................................................................................................................18
Contents
ABSTRACT:..............................................................................................................................1
Introduction:...............................................................................................................................4
Description of the current service:.............................................................................................4
Patient Demographics:...............................................................................................................5
Factors Influencing Consumer Care Provision or Access..........................................................5
Current Model of Care:..............................................................................................................8
Strengths and Weaknesses of Health Service:.........................................................................13
Proposed NP Model:................................................................................................................14
Conclusion:..............................................................................................................................15
Recommendations:...................................................................................................................16
References:...............................................................................................................................18
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4Transforming Healthcare Services
Introduction:
Advanced Practice Registered Nursing (APRN) comprises of four roles which are
nurse mid-wife, clinical nurse specialist, nurse anaesthetist and nurse practitioner. Nursing
practitioners are registered nurses with an accredited graduate degree and specialization
certifications reflecting the area of expertise (Nursing.upenn.edu, 2018). Independent Nursing
Practice allows the nurses to carryout work independent of other healthcare professionals,
and also allows collaboration whenever required. This means that the nursing practitioners
can practice and prescribe medications independently (Rigolosi & Salmond, 2014).The
Independent nursing practice model comprises of models that are small business or private
and are very mobile, which means that the nurses often have to travel to client’s locations.
This model combines the functions of a small business ownership and a professional practice,
which raises are significant challenge in respect to the combination of responsibilities
associated with each of these functions (Hamric et al., 2013).
In the current context, the Independent Nursing Practice model will be critically
analysed and evaluated to identify the strengths and weaknesses in the model. Opportunities
for collaboration with other professionals in order to support the service model shall also be
discussed, which can allow improvement in the model. Furthermore, the different barriers
and challenges for improvement will also be analysed which can help nib the development of
improvement strategies for the model.
The setup for the independent practice is setup in an aged residential care centre (Blue
Care) which houses about 100 residents of ages 70 to 100 years.
Description of the current service:
Introduction:
Advanced Practice Registered Nursing (APRN) comprises of four roles which are
nurse mid-wife, clinical nurse specialist, nurse anaesthetist and nurse practitioner. Nursing
practitioners are registered nurses with an accredited graduate degree and specialization
certifications reflecting the area of expertise (Nursing.upenn.edu, 2018). Independent Nursing
Practice allows the nurses to carryout work independent of other healthcare professionals,
and also allows collaboration whenever required. This means that the nursing practitioners
can practice and prescribe medications independently (Rigolosi & Salmond, 2014).The
Independent nursing practice model comprises of models that are small business or private
and are very mobile, which means that the nurses often have to travel to client’s locations.
This model combines the functions of a small business ownership and a professional practice,
which raises are significant challenge in respect to the combination of responsibilities
associated with each of these functions (Hamric et al., 2013).
In the current context, the Independent Nursing Practice model will be critically
analysed and evaluated to identify the strengths and weaknesses in the model. Opportunities
for collaboration with other professionals in order to support the service model shall also be
discussed, which can allow improvement in the model. Furthermore, the different barriers
and challenges for improvement will also be analysed which can help nib the development of
improvement strategies for the model.
The setup for the independent practice is setup in an aged residential care centre (Blue
Care) which houses about 100 residents of ages 70 to 100 years.
Description of the current service:
5Transforming Healthcare Services
Independent Nursing Practice involves the providence of differential services
depending upon the local demand as well as the scope of the nursing practitioner, showing a
lot of flexibility in practice. This entails the independent practice to be conducted at different
service environments. Independent NP can provide non acute care in a home setup (MacPhee
& Borram, 2012). The types of care provided can include: regular monitoring of blood
glucose, blood pressure, and blood clotting; regular health checkups; care for wound;
treatment for upper respiratory system, continence care, assessing the medication provided,
assessment for falls and also provide referral for other services.
Patient Demographics:
In the present scenario, the selected population comprises of elderly patients.
Factors Influencing Consumer Care Provision or Access
Independent NP enables the nursing practice to be conducted without the
supervision of a physician. This helps the nurses to gain independence and autonomy as they
are able to provide medical care without management or oversight of the physician (Antohe
et al., 2016). A ‘full practice’ status of an NP is a provision that enables independent
assessment, diagnosis, interpretation of diagnostic tests, and prescription of medicines
(Moran et al., 2016). Licensed Independent Nurse Practitioners can conduct their practice in
different setups like: ambulatory, acute, long term care and also function as primary or
speciality care providers. They can assess, diagnose, treat and manage both chronic
conditions as well as acute episodic conditions. Therefore the practitioners need to be adept
with health promotion and disease prevention. They can also order, conduct, supervise as
well as interpret laboratory and diagnostic results, provide prescriptions for pharmacological
substances and non-pharmacological therapies. Moreover, the independent nurses can also be
involved in teaching and counselling of the patients. Hain and Fleck (2014) however pointed
Independent Nursing Practice involves the providence of differential services
depending upon the local demand as well as the scope of the nursing practitioner, showing a
lot of flexibility in practice. This entails the independent practice to be conducted at different
service environments. Independent NP can provide non acute care in a home setup (MacPhee
& Borram, 2012). The types of care provided can include: regular monitoring of blood
glucose, blood pressure, and blood clotting; regular health checkups; care for wound;
treatment for upper respiratory system, continence care, assessing the medication provided,
assessment for falls and also provide referral for other services.
Patient Demographics:
In the present scenario, the selected population comprises of elderly patients.
Factors Influencing Consumer Care Provision or Access
Independent NP enables the nursing practice to be conducted without the
supervision of a physician. This helps the nurses to gain independence and autonomy as they
are able to provide medical care without management or oversight of the physician (Antohe
et al., 2016). A ‘full practice’ status of an NP is a provision that enables independent
assessment, diagnosis, interpretation of diagnostic tests, and prescription of medicines
(Moran et al., 2016). Licensed Independent Nurse Practitioners can conduct their practice in
different setups like: ambulatory, acute, long term care and also function as primary or
speciality care providers. They can assess, diagnose, treat and manage both chronic
conditions as well as acute episodic conditions. Therefore the practitioners need to be adept
with health promotion and disease prevention. They can also order, conduct, supervise as
well as interpret laboratory and diagnostic results, provide prescriptions for pharmacological
substances and non-pharmacological therapies. Moreover, the independent nurses can also be
involved in teaching and counselling of the patients. Hain and Fleck (2014) however pointed
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6Transforming Healthcare Services
out that many professional healthcare organizations do not support independent nursing
practice as they believe that physicians have better competency in medical care compared to
Nursing Practitioners due to their rigorous training, and hence NP are incapable of providing
care within the same quality and safety parameters as physicians (Hain & Fleck, 2014).
According to the Australian Department of Health, endorsement from Nursing and
Midwifery Board of Australia is required to work as a nurse practitioner. The endorsement
can be received on the merit of several factors like a general registration as a registered nurse
with no restriction on practice; advanced practice in clinical leadership in the area of
expertise in the last 5 years and complemented with research, education and management;
showing competence in the competency standards set by the Nursing and Midwifery Board
of Australia, and completion of the required qualification as mandated by Nursing and
Midwifery Board of Australia. Such factors can ensure the development of competency,
expertise and knowledge of the nurses to independently conduct their practice
(nursingmidwiferyboard.gov.au, 2018).
The practitioners can work with individuals, families or communities in different
care settings like hospitals, community health settings and private practice. However, there
isn’t any limit on where an independent nursing practitioner can work, and currently in
Australia Nursing Practitioners are involved in speciality areas like: aged care, emergency,
drug and alcohol, private practice, surgical, medical, women’s health, rural and remote setup,
mental healthcare facilities, communities, chronic and complex care centre as well as
paediatric units (Nursing.upenn.edu, 2018). This also increases accessibility to healthcare
services, as well as increase the range of care settings that can be supported by healthcare
organizations.
out that many professional healthcare organizations do not support independent nursing
practice as they believe that physicians have better competency in medical care compared to
Nursing Practitioners due to their rigorous training, and hence NP are incapable of providing
care within the same quality and safety parameters as physicians (Hain & Fleck, 2014).
According to the Australian Department of Health, endorsement from Nursing and
Midwifery Board of Australia is required to work as a nurse practitioner. The endorsement
can be received on the merit of several factors like a general registration as a registered nurse
with no restriction on practice; advanced practice in clinical leadership in the area of
expertise in the last 5 years and complemented with research, education and management;
showing competence in the competency standards set by the Nursing and Midwifery Board
of Australia, and completion of the required qualification as mandated by Nursing and
Midwifery Board of Australia. Such factors can ensure the development of competency,
expertise and knowledge of the nurses to independently conduct their practice
(nursingmidwiferyboard.gov.au, 2018).
The practitioners can work with individuals, families or communities in different
care settings like hospitals, community health settings and private practice. However, there
isn’t any limit on where an independent nursing practitioner can work, and currently in
Australia Nursing Practitioners are involved in speciality areas like: aged care, emergency,
drug and alcohol, private practice, surgical, medical, women’s health, rural and remote setup,
mental healthcare facilities, communities, chronic and complex care centre as well as
paediatric units (Nursing.upenn.edu, 2018). This also increases accessibility to healthcare
services, as well as increase the range of care settings that can be supported by healthcare
organizations.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7Transforming Healthcare Services
In each of such settings, the consumer population needs, social determinants of health
and primary healthcare principles can differ. In an aged care centre, the NP needs to deal with
elderly patients. The health needs of the elderly population are underlined by the higher
prevalence of chronic conditions, physical disabilities, mental health conditions, and
related co-morbidities. Shrivastava et al. (2013) suggested that the health needs of the
elderly patients cannot be viewed in isolation. This is because of different inter-related factors
that can be attributed to the various health problems seen among them. Several determinants
of health that affects the well being of the elderly has been identified by different authors, and
includes: social factors (isolation of the patients, due to their children moving out in search
for occupation), mistreatment of the elderly, lack of awareness about the risk factors, dietary
and nutritional needs, psycho-emotional factors (like mental stress and isolation), financial
factors (reduction of income after retirement thereby challenging the access to basic needs
like proper nutrition, shelter and clothing), factors attributed to healthcare systems (healthcare
insurance for elderly and government care facilities) and physical determinants. These factors
can significantly affect the medical problems of the elderly, and also have an impact on the
quality of life experienced by them (Song et al., 2013; Braz et al., 2012). INP can ensure
provision of care that spans across several of these social determinants, providing a multi-
dimensional care for the patient.
Shrivastava et al. (2013) proposed that prevention and control of health issues among
the elderly populace requires a multidimensional approach that requires an active
collaboration of different sectors like healthcare, social welfare, urban/rural development
and legal, which can be a significant challenge considering the diverse range of professional
skills required to maintain communication with them. Also, a lack of comprehensive policy
that addresses the determinants of health is a weakness of this service. A community or a
home based care program for the elderly patient’s needs to begin with the development of a
In each of such settings, the consumer population needs, social determinants of health
and primary healthcare principles can differ. In an aged care centre, the NP needs to deal with
elderly patients. The health needs of the elderly population are underlined by the higher
prevalence of chronic conditions, physical disabilities, mental health conditions, and
related co-morbidities. Shrivastava et al. (2013) suggested that the health needs of the
elderly patients cannot be viewed in isolation. This is because of different inter-related factors
that can be attributed to the various health problems seen among them. Several determinants
of health that affects the well being of the elderly has been identified by different authors, and
includes: social factors (isolation of the patients, due to their children moving out in search
for occupation), mistreatment of the elderly, lack of awareness about the risk factors, dietary
and nutritional needs, psycho-emotional factors (like mental stress and isolation), financial
factors (reduction of income after retirement thereby challenging the access to basic needs
like proper nutrition, shelter and clothing), factors attributed to healthcare systems (healthcare
insurance for elderly and government care facilities) and physical determinants. These factors
can significantly affect the medical problems of the elderly, and also have an impact on the
quality of life experienced by them (Song et al., 2013; Braz et al., 2012). INP can ensure
provision of care that spans across several of these social determinants, providing a multi-
dimensional care for the patient.
Shrivastava et al. (2013) proposed that prevention and control of health issues among
the elderly populace requires a multidimensional approach that requires an active
collaboration of different sectors like healthcare, social welfare, urban/rural development
and legal, which can be a significant challenge considering the diverse range of professional
skills required to maintain communication with them. Also, a lack of comprehensive policy
that addresses the determinants of health is a weakness of this service. A community or a
home based care program for the elderly patient’s needs to begin with the development of a

8Transforming Healthcare Services
comprehensive policy that can include the other determinants of health apart from the
medical aspects. A strong sense of commitment and social action is needed for the proper
implementation of the care model at the basic level. Improving the knowledge of the elderly
about health and risk factors is an important measure, as pointed out by Song et al.
(2013).Other measures include social measures that involves creating a culture where care of
the elderly is also participated by their children; involving regulatory strategies that enables
members of society to care for their aged parents developing health insurance policies for the
elderly to cover their healthcare needs; developing pension schemes; development of elder
friendly houses and roads; promoting primary prevention strategies like healthy lifestyle;
providence of education, information and communication for the elderly, middle aged
(individuals who will move on towards elderly age group in the near future) and the youth
(acting as caregiver for the elderly) about issues related to hygiene, physical exercise,
nutrition, avoiding alcohol and tobacco, accident prevention and developing awareness about
the early signs of geriatric problems (Song et al., 2013). Training of medical professionals to
understand the specialized needs of the elderly, provision of medical aids, setting up
gerontology units, ensuring proper communication with the patients can also be implemented
in the primary care policies for effective care (Shrivastava et al., 2013).
Current Model of Care:
Different strategies have been identified that can improve the healthcare service for
the elderly. These strategies have been embodied in different care plans globally, which shall
be discussed next.
The UK Healthcare Strategic Plan (2015-2020) aims the development of Patient
Centered Care, and considers two aspects of improvement: Patient Experience and
Strategic cultural alignment. The plan necessitates the involvement of patient experience
comprehensive policy that can include the other determinants of health apart from the
medical aspects. A strong sense of commitment and social action is needed for the proper
implementation of the care model at the basic level. Improving the knowledge of the elderly
about health and risk factors is an important measure, as pointed out by Song et al.
(2013).Other measures include social measures that involves creating a culture where care of
the elderly is also participated by their children; involving regulatory strategies that enables
members of society to care for their aged parents developing health insurance policies for the
elderly to cover their healthcare needs; developing pension schemes; development of elder
friendly houses and roads; promoting primary prevention strategies like healthy lifestyle;
providence of education, information and communication for the elderly, middle aged
(individuals who will move on towards elderly age group in the near future) and the youth
(acting as caregiver for the elderly) about issues related to hygiene, physical exercise,
nutrition, avoiding alcohol and tobacco, accident prevention and developing awareness about
the early signs of geriatric problems (Song et al., 2013). Training of medical professionals to
understand the specialized needs of the elderly, provision of medical aids, setting up
gerontology units, ensuring proper communication with the patients can also be implemented
in the primary care policies for effective care (Shrivastava et al., 2013).
Current Model of Care:
Different strategies have been identified that can improve the healthcare service for
the elderly. These strategies have been embodied in different care plans globally, which shall
be discussed next.
The UK Healthcare Strategic Plan (2015-2020) aims the development of Patient
Centered Care, and considers two aspects of improvement: Patient Experience and
Strategic cultural alignment. The plan necessitates the involvement of patient experience
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9Transforming Healthcare Services
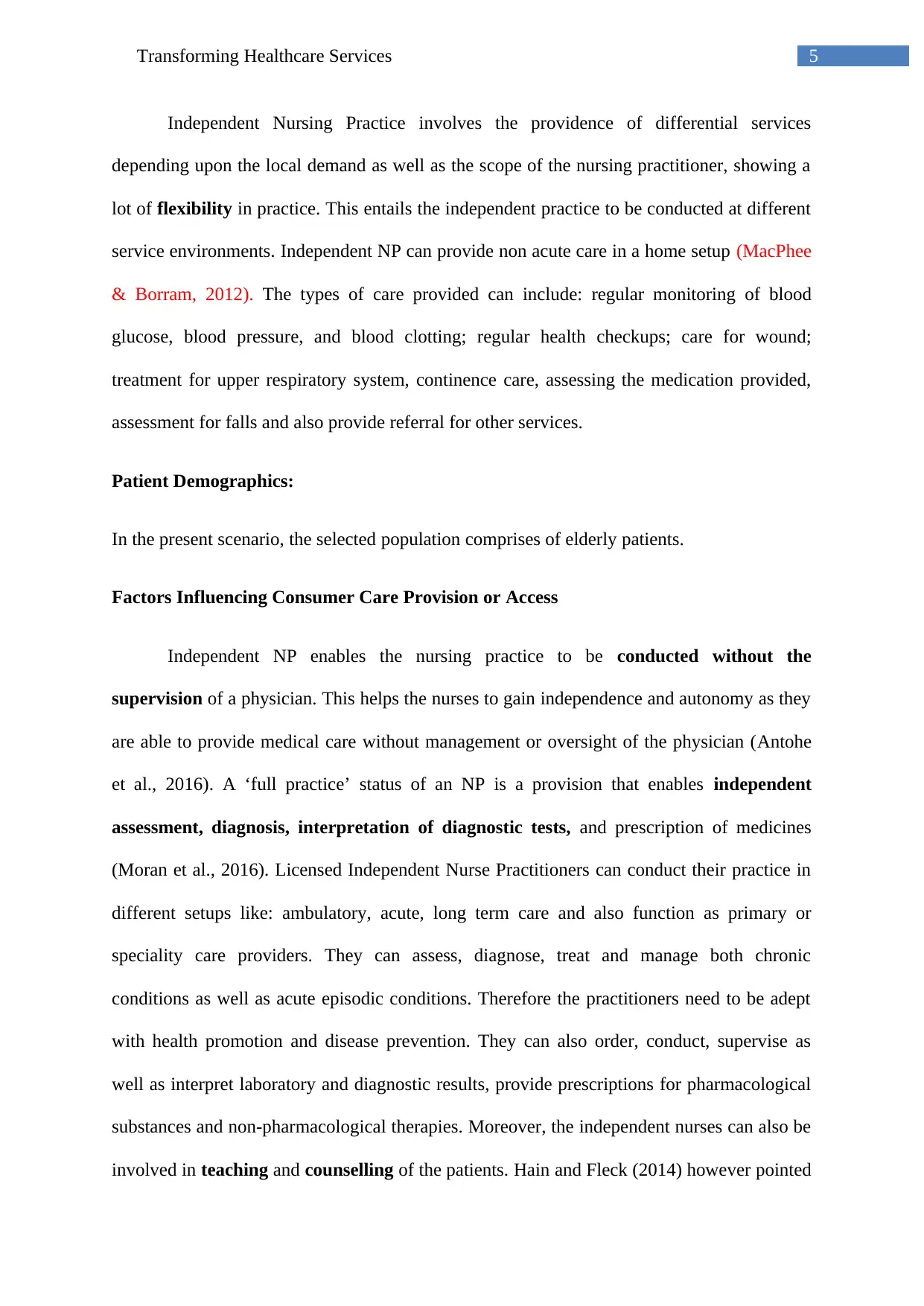
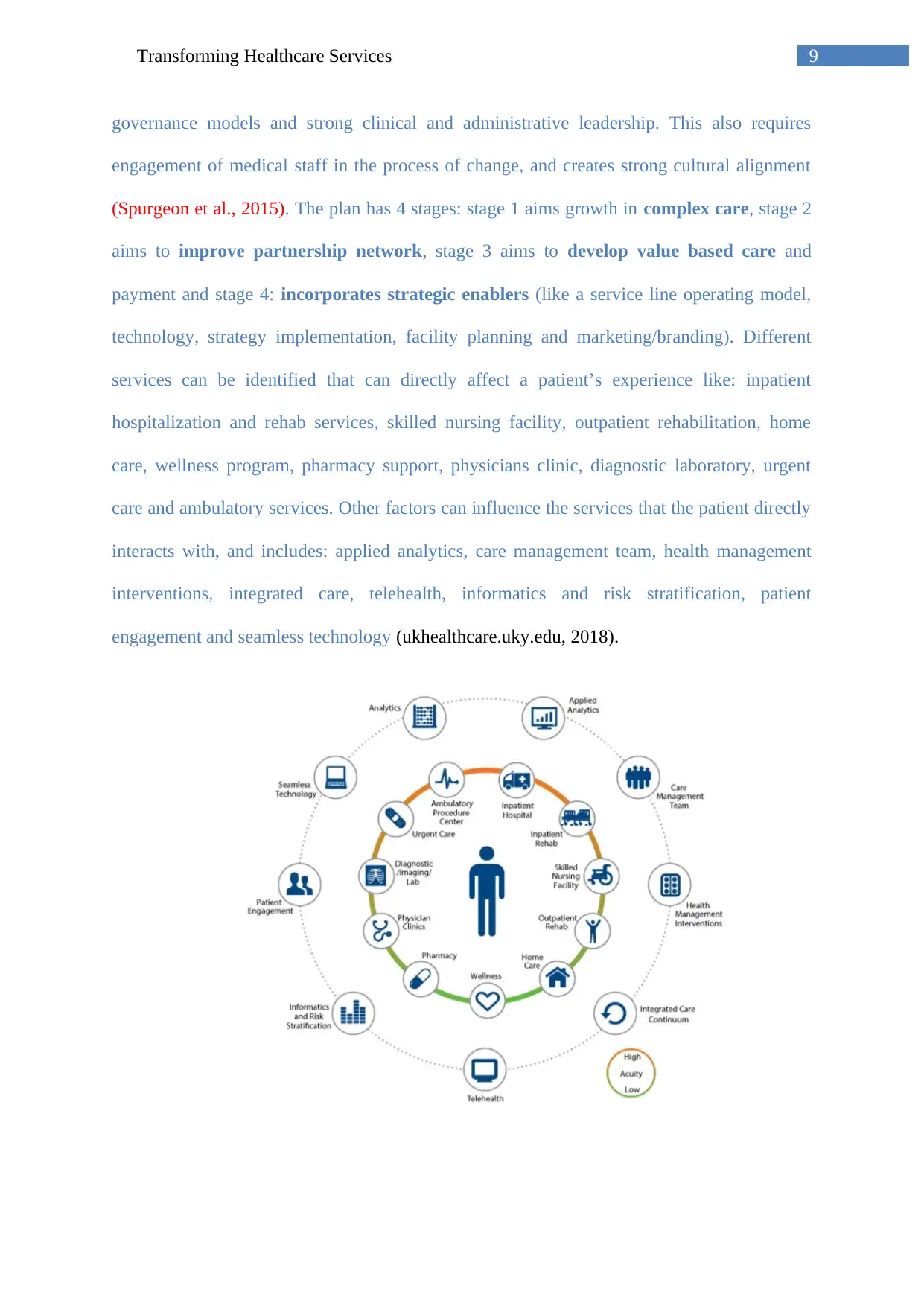
governance models and strong clinical and administrative leadership. This also requires
engagement of medical staff in the process of change, and creates strong cultural alignment
(Spurgeon et al., 2015). The plan has 4 stages: stage 1 aims growth in complex care, stage 2
aims to improve partnership network, stage 3 aims to develop value based care and
payment and stage 4: incorporates strategic enablers (like a service line operating model,
technology, strategy implementation, facility planning and marketing/branding). Different
services can be identified that can directly affect a patient’s experience like: inpatient
hospitalization and rehab services, skilled nursing facility, outpatient rehabilitation, home
care, wellness program, pharmacy support, physicians clinic, diagnostic laboratory, urgent
care and ambulatory services. Other factors can influence the services that the patient directly
interacts with, and includes: applied analytics, care management team, health management
interventions, integrated care, telehealth, informatics and risk stratification, patient
engagement and seamless technology (ukhealthcare.uky.edu, 2018).
governance models and strong clinical and administrative leadership. This also requires
engagement of medical staff in the process of change, and creates strong cultural alignment
(Spurgeon et al., 2015). The plan has 4 stages: stage 1 aims growth in complex care, stage 2
aims to improve partnership network, stage 3 aims to develop value based care and
payment and stage 4: incorporates strategic enablers (like a service line operating model,
technology, strategy implementation, facility planning and marketing/branding). Different
services can be identified that can directly affect a patient’s experience like: inpatient
hospitalization and rehab services, skilled nursing facility, outpatient rehabilitation, home
care, wellness program, pharmacy support, physicians clinic, diagnostic laboratory, urgent
care and ambulatory services. Other factors can influence the services that the patient directly
interacts with, and includes: applied analytics, care management team, health management
interventions, integrated care, telehealth, informatics and risk stratification, patient
engagement and seamless technology (ukhealthcare.uky.edu, 2018).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

10Transforming Healthcare Services
Figure 1: Alignment of services to ensure patient centered care; source:
(ukhealthcare.uky.edu, 2018).
Figure 2: Strengthening of partnership networks; source: (ukhealthcare.uky.edu, 2018).
Figure 3: Calculating value of care as a factor of quality, service, access to care and cost;
source: (ukhealthcare.uky.edu, 2018).
Figure 1 and 2 above shows how services can be strategically aligned to the needs of
the patient, and help to support other services in order to strengthen and improve care through
the development of partnership networks. Figure 3 shows how the value of a service model;
can be analysed from individual components like the sum quality of care, service, and
accessibility to it over the cost of care (ukhealthcare.uky.edu, 2018).
The partnership HealthPlan of California suggests that community based approaches
can be developed through an improved access to primary care, improve access to alcohol and
Figure 1: Alignment of services to ensure patient centered care; source:
(ukhealthcare.uky.edu, 2018).
Figure 2: Strengthening of partnership networks; source: (ukhealthcare.uky.edu, 2018).
Figure 3: Calculating value of care as a factor of quality, service, access to care and cost;
source: (ukhealthcare.uky.edu, 2018).
Figure 1 and 2 above shows how services can be strategically aligned to the needs of
the patient, and help to support other services in order to strengthen and improve care through
the development of partnership networks. Figure 3 shows how the value of a service model;
can be analysed from individual components like the sum quality of care, service, and
accessibility to it over the cost of care (ukhealthcare.uky.edu, 2018).
The partnership HealthPlan of California suggests that community based approaches
can be developed through an improved access to primary care, improve access to alcohol and
11Transforming Healthcare Services
drug treatment, developing comprehensive care plan for elderly, supporting the recruitment
of providers and commitment to the development of health information exchange and clinical
data repository. The plan identifies partnership of 4 pillars (providers, employees, public
resources, and community partners) on which a health of individuals can be promoted
(Partnershiphp.org, 2018).
Central Health strategic plan incorporates four aspects in the improvement of
healthcare model: 1. Improving healthcare through the access of high quality, patient
centric coordinated clinical service. 2. Health Promotion through the alignment of health
education policies to foster the ability of patients to improve their own health conditions as
well as that of their families. 3. Improving health coverage through affordable healthcare
products and enrolment to healthcare services that can improve accessibility to care. 4.
Developing health infrastructure by ensuring necessary services being in place and
accessible by the patient. INP allows all such factors to be considered in the service.
The various aspects identified above can be utilised in the designing of a strategic plan that
can improve the healthcare service model of independent nursing practice (centralhealth.net,
2018).
Keeping the patient’s experience central to the service
Help in the development of complex care
Develop partnership network
Develop value based care
Using strategic enablers
Health education
Improving accessibility to care
Implementation of health promotion and wellness programs
drug treatment, developing comprehensive care plan for elderly, supporting the recruitment
of providers and commitment to the development of health information exchange and clinical
data repository. The plan identifies partnership of 4 pillars (providers, employees, public
resources, and community partners) on which a health of individuals can be promoted
(Partnershiphp.org, 2018).
Central Health strategic plan incorporates four aspects in the improvement of
healthcare model: 1. Improving healthcare through the access of high quality, patient
centric coordinated clinical service. 2. Health Promotion through the alignment of health
education policies to foster the ability of patients to improve their own health conditions as
well as that of their families. 3. Improving health coverage through affordable healthcare
products and enrolment to healthcare services that can improve accessibility to care. 4.
Developing health infrastructure by ensuring necessary services being in place and
accessible by the patient. INP allows all such factors to be considered in the service.
The various aspects identified above can be utilised in the designing of a strategic plan that
can improve the healthcare service model of independent nursing practice (centralhealth.net,
2018).
Keeping the patient’s experience central to the service
Help in the development of complex care
Develop partnership network
Develop value based care
Using strategic enablers
Health education
Improving accessibility to care
Implementation of health promotion and wellness programs
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 24
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





