Chronic Kidney Disease and Diabetic Nephropathy
VerifiedAdded on 2023/01/19
|10
|1365
|80
AI Summary
This document discusses the causes, risk factors, and treatment options for chronic kidney disease (CKD) and diabetic nephropathy. It explains how obesity, hypertension, and diabetes contribute to the development of CKD and the impact of hyperkalemia and metabolic acidosis on kidney function. The document also explores pharmacological and non-pharmacological treatment options for managing CKD and diabetic nephropathy. References to relevant books and journals are provided for further reading.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
ASSESSMENT 2: TRIMESTER 2,
2019
2019
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
TABLE OF CONTENTS
REFERENCES................................................................................................................................5
REFERENCES................................................................................................................................5
3
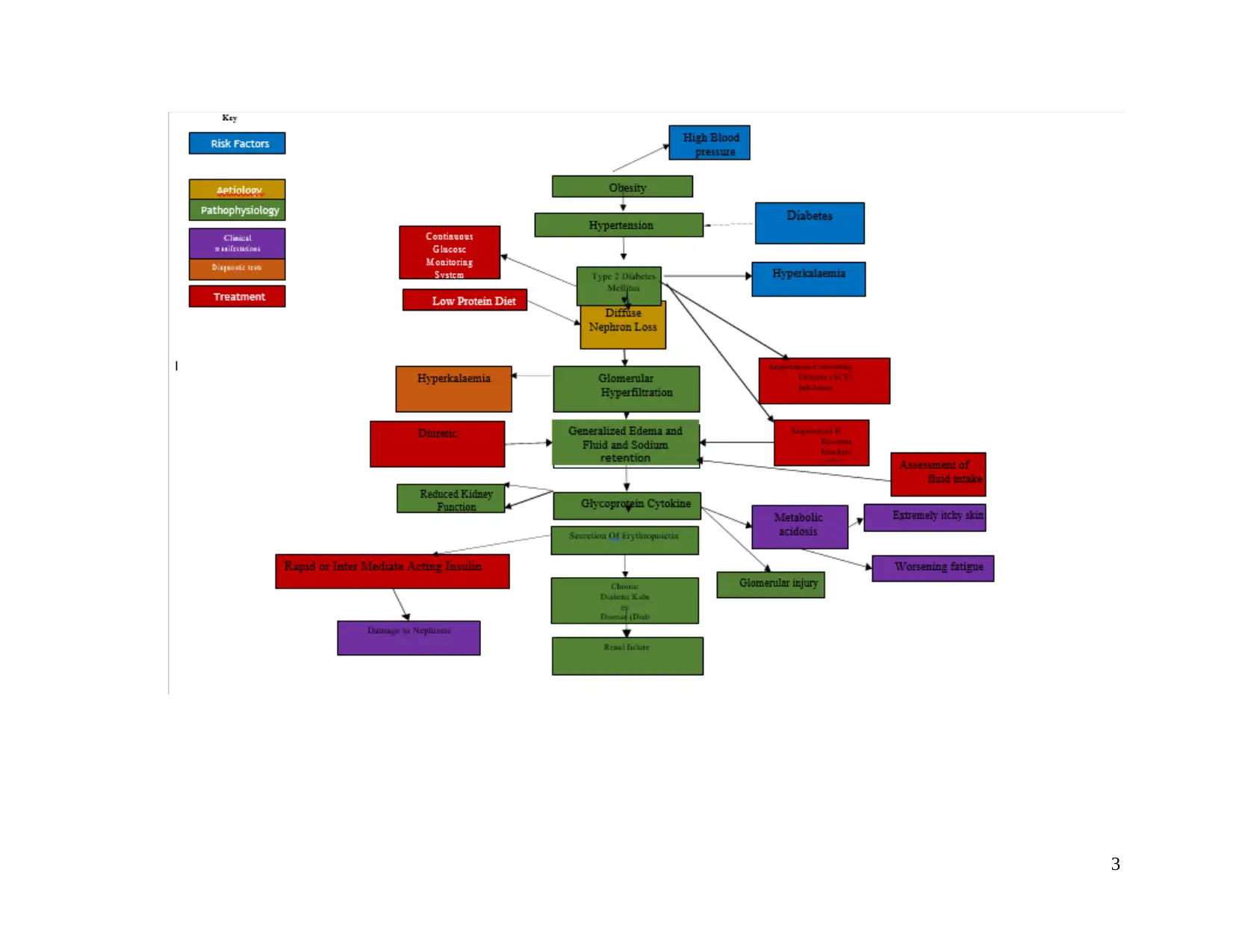
Steve McManus, and obese man with pitting oedema, is diagnosed with chronic kidney
disease due to diffuse nephron loss. Chronic kidney disease (CKD) is a long-standing disease
which causes damage where kidneys fails to filter waste fluid from blood (Papadopoulou &
et.al., 2015). However, loss of nephron is counterbalanced by adaptive increase in secretory rate
of Potassium ion (K+) in remaining nephrons. In accordance with case scenario it can be
articulated that patient is at risk of diabetic kidney disease that is diabetic nephropathy.
Risk factors for the patient comprise hypertension, type 2 diabetes mellitus and obesity.
As per the view of Porrini & et.al., 2015, increase in obesity is major developing risk factor for
CKD because it comprises cause of hypertension and Diabetes. Diabetes occur when the blood
sugar level of body is high. Excessive glucose in blood causes damage to filters of kidneys. On
the other hand, high blood pressure cause damage to blood vessels in kidneys due to which
kidneys become unable to remove extra fluid and waste from body (Causes of Chronic Kidney
Disease, 2019).
From the physical examination of patient, it is identified that the patient has
hyperkalaemia and metabolic acidosis. As per observation, it can be said that potassium and acid
excretion are the common reasons behind hyperkalaemia and metabolic acidosis. According to
Thomas & et.al., 2015, chronic hyperglycaemias is a primary cause of diabetic nephropathy. In
this transmembrane glucose transporters (GLUT) receptors stop facilitation of intracellular
glucose transport in kidneys. This occurs due to activation of mechanism like direct effect of
hyperglycaemia, secretion of cytokine, advanced glycosylation of end products and glomerular
hyperfiltration.
In accordance with patient condition that is swollen legs is evident to activation of
glomerular hyperfiltration has been found out which is mediated via dilation the afferent
arteriole which causes rise in Glomerular filtration rate (GFR). As per Toth-Manikowski & Atta,
2015, Glomeruli are tiny filters in kidneys which filters waste from the blood. Hyperfiltration can
be recorded as GFR ≥150 mL/min/1.73 m 2. GFR activation leads to generalized edema which is
reflected in swelling, and occurs due to water retention because of loss GFR which leads to fluid
and sodium retention. However, worsening fatigue denotes Anaemia which occurs due to
activation of glycoprotein cytokine which causes secretion of Erythropoietin (EPO) from
kidneys. Lim, 2014, stated that elevations in vascular endothelial growth factor (VEGF) is a
growth factor for profibrotic proteins and beta (TFG-β) which causes damage to nephrons at
4
disease due to diffuse nephron loss. Chronic kidney disease (CKD) is a long-standing disease
which causes damage where kidneys fails to filter waste fluid from blood (Papadopoulou &
et.al., 2015). However, loss of nephron is counterbalanced by adaptive increase in secretory rate
of Potassium ion (K+) in remaining nephrons. In accordance with case scenario it can be
articulated that patient is at risk of diabetic kidney disease that is diabetic nephropathy.
Risk factors for the patient comprise hypertension, type 2 diabetes mellitus and obesity.
As per the view of Porrini & et.al., 2015, increase in obesity is major developing risk factor for
CKD because it comprises cause of hypertension and Diabetes. Diabetes occur when the blood
sugar level of body is high. Excessive glucose in blood causes damage to filters of kidneys. On
the other hand, high blood pressure cause damage to blood vessels in kidneys due to which
kidneys become unable to remove extra fluid and waste from body (Causes of Chronic Kidney
Disease, 2019).
From the physical examination of patient, it is identified that the patient has
hyperkalaemia and metabolic acidosis. As per observation, it can be said that potassium and acid
excretion are the common reasons behind hyperkalaemia and metabolic acidosis. According to
Thomas & et.al., 2015, chronic hyperglycaemias is a primary cause of diabetic nephropathy. In
this transmembrane glucose transporters (GLUT) receptors stop facilitation of intracellular
glucose transport in kidneys. This occurs due to activation of mechanism like direct effect of
hyperglycaemia, secretion of cytokine, advanced glycosylation of end products and glomerular
hyperfiltration.
In accordance with patient condition that is swollen legs is evident to activation of
glomerular hyperfiltration has been found out which is mediated via dilation the afferent
arteriole which causes rise in Glomerular filtration rate (GFR). As per Toth-Manikowski & Atta,
2015, Glomeruli are tiny filters in kidneys which filters waste from the blood. Hyperfiltration can
be recorded as GFR ≥150 mL/min/1.73 m 2. GFR activation leads to generalized edema which is
reflected in swelling, and occurs due to water retention because of loss GFR which leads to fluid
and sodium retention. However, worsening fatigue denotes Anaemia which occurs due to
activation of glycoprotein cytokine which causes secretion of Erythropoietin (EPO) from
kidneys. Lim, 2014, stated that elevations in vascular endothelial growth factor (VEGF) is a
growth factor for profibrotic proteins and beta (TFG-β) which causes damage to nephrons at
4
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

different levels. Further, activation of hyperkalemia impacts ability of kidneys to secret
potassium in urine which in case of Steve McManus is because of uncontrolled type 2 diabetes
mellitus which diminish capacity of kidneys to excrete potassium into urine. Thus, severity of
GFR mechanism leads to Glomerulonephritis which causes Glomerular injury which causes
chronic kidney diseases. According to Rossignol, 2015, Glomerulonephritis leads to high blood
pressure because of reduced kidney function and influence ability of kidney to handle sodium
which causes chronic diabetic kidney disease (diabetic nephropathy). This stage of illness leads
to long term kidney disease and end stage renal diseases.
According to Wong, 2012, risk of diabetes mellitus increases by increase in obesity and
therefore Diabetic nephropathy is most significant complication of type ii diabetes mellitus
which leads to end stage kidney diseases. Pharmacological treatment for treating Steve
McManus can be angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor
blockers (ARBs) which given to treat high blood pressure. Further, diuretic can be given relieve
swelling, it is a class of drug which aid in increasing urine production by increasing excretion of
liquid from body (Gallagher & Suckling, 2016). In addition, rapid or inter mediate acting insulin
medication can be given for controlling increasing risk of hypoglycaemia (Mulay & Anders,
2017). Apparently, end stage treat for kidney disease can be dialysis or kidney transplant.
However, non-pharmacological treatment continuously measuring glucose levels by
Continuous Glucose Monitoring Systems (CGMS) can aid the nurse in detecting downward and
upward trend in glucose. As per the views of Ahmad, 2015, it is important to note amount of
fluid intake in case of Steve McManus will aid in stabilizing fluid volume, weight an d signs of
edema. In addition, nurse will assess appetite of Steve McManus to ensure low protein diet to
decrease waste products from blood. Terami, 2014, articulated that restricting protein diet helps
in managing progression of kidney disease because protein intake affects renal hemodynamic by
raising GFR.
5
potassium in urine which in case of Steve McManus is because of uncontrolled type 2 diabetes
mellitus which diminish capacity of kidneys to excrete potassium into urine. Thus, severity of
GFR mechanism leads to Glomerulonephritis which causes Glomerular injury which causes
chronic kidney diseases. According to Rossignol, 2015, Glomerulonephritis leads to high blood
pressure because of reduced kidney function and influence ability of kidney to handle sodium
which causes chronic diabetic kidney disease (diabetic nephropathy). This stage of illness leads
to long term kidney disease and end stage renal diseases.
According to Wong, 2012, risk of diabetes mellitus increases by increase in obesity and
therefore Diabetic nephropathy is most significant complication of type ii diabetes mellitus
which leads to end stage kidney diseases. Pharmacological treatment for treating Steve
McManus can be angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor
blockers (ARBs) which given to treat high blood pressure. Further, diuretic can be given relieve
swelling, it is a class of drug which aid in increasing urine production by increasing excretion of
liquid from body (Gallagher & Suckling, 2016). In addition, rapid or inter mediate acting insulin
medication can be given for controlling increasing risk of hypoglycaemia (Mulay & Anders,
2017). Apparently, end stage treat for kidney disease can be dialysis or kidney transplant.
However, non-pharmacological treatment continuously measuring glucose levels by
Continuous Glucose Monitoring Systems (CGMS) can aid the nurse in detecting downward and
upward trend in glucose. As per the views of Ahmad, 2015, it is important to note amount of
fluid intake in case of Steve McManus will aid in stabilizing fluid volume, weight an d signs of
edema. In addition, nurse will assess appetite of Steve McManus to ensure low protein diet to
decrease waste products from blood. Terami, 2014, articulated that restricting protein diet helps
in managing progression of kidney disease because protein intake affects renal hemodynamic by
raising GFR.
5
REFERENCES
Books and Journals
Ahmad, J. (2015). Management of diabetic nephropathy: recent progress and future
perspective. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 9(4). 343-
358.
Gallagher, H., & Suckling, R. J. (2016). Diabetic nephropathy: where are we on the journey from
pathophysiology to treatment? Diabetes, Obesity and Metabolism. 18(7). 641-647.
Lim, A. K. (2014). Diabetic nephropathy–complications and treatment. International journal of
nephrology and renovascular disease. 7. 361.
Mulay, S. R., & Anders, H. J. (2017). Crystal nephropathies: mechanisms of crystal-induced
kidney injury. Nature Reviews Nephrology. 13(4). 226.
Papadopoulou, E., Varouktsi, A., Lazaridis, A., Boutari, C., & Doumas, M. (2015). Erectile
dysfunction in chronic kidney disease: From pathophysiology to management. World
journal of nephrology. 4(3). 379.
Porrini, E., Ruggenenti, P., Mogensen, C. E., Barlovic, D. P., Praga, M., Cruzado, J. M., ... &
ERA-EDTA Diabesity Working Group. (2015). Non-proteinuric pathways in loss of renal
function in patients with type 2 diabetes. The Lancet Diabetes & Endocrinology. 3(5).
382-391.
Rossignol, P., Massy, Z. A., Azizi, M., Bakris, G., Ritz, E., Covic, A., ... & Mallamaci, F.
(2015). The double challenge of resistant hypertension and chronic kidney disease. The
Lancet. 386(10003). 1588-1598.
Terami, N., Ogawa, D., Tachibana, H., Hatanaka, T., Wada, J., Nakatsuka, A., ... & Takei, K.
(2014). Long-term treatment with the sodium glucose cotransporter 2 inhibitor,
dapagliflozin, ameliorates glucose homeostasis and diabetic nephropathy in db/db
mice. PloS one. 9(6). e100777.
Thomas, M. C., Brownlee, M., Susztak, K., Sharma, K., Jandeleit-Dahm, K. A., Zoungas, S., ...
& Cooper, M. E. (2015). Diabetic kidney disease. Nature Reviews Disease Primers. 1.
15018.
Toth-Manikowski, S., & Atta, M. G. (2015). Diabetic kidney disease: pathophysiology and
therapeutic targets. Journal of diabetes research. 2015.
Online
6
Books and Journals
Ahmad, J. (2015). Management of diabetic nephropathy: recent progress and future
perspective. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 9(4). 343-
358.
Gallagher, H., & Suckling, R. J. (2016). Diabetic nephropathy: where are we on the journey from
pathophysiology to treatment? Diabetes, Obesity and Metabolism. 18(7). 641-647.
Lim, A. K. (2014). Diabetic nephropathy–complications and treatment. International journal of
nephrology and renovascular disease. 7. 361.
Mulay, S. R., & Anders, H. J. (2017). Crystal nephropathies: mechanisms of crystal-induced
kidney injury. Nature Reviews Nephrology. 13(4). 226.
Papadopoulou, E., Varouktsi, A., Lazaridis, A., Boutari, C., & Doumas, M. (2015). Erectile
dysfunction in chronic kidney disease: From pathophysiology to management. World
journal of nephrology. 4(3). 379.
Porrini, E., Ruggenenti, P., Mogensen, C. E., Barlovic, D. P., Praga, M., Cruzado, J. M., ... &
ERA-EDTA Diabesity Working Group. (2015). Non-proteinuric pathways in loss of renal
function in patients with type 2 diabetes. The Lancet Diabetes & Endocrinology. 3(5).
382-391.
Rossignol, P., Massy, Z. A., Azizi, M., Bakris, G., Ritz, E., Covic, A., ... & Mallamaci, F.
(2015). The double challenge of resistant hypertension and chronic kidney disease. The
Lancet. 386(10003). 1588-1598.
Terami, N., Ogawa, D., Tachibana, H., Hatanaka, T., Wada, J., Nakatsuka, A., ... & Takei, K.
(2014). Long-term treatment with the sodium glucose cotransporter 2 inhibitor,
dapagliflozin, ameliorates glucose homeostasis and diabetic nephropathy in db/db
mice. PloS one. 9(6). e100777.
Thomas, M. C., Brownlee, M., Susztak, K., Sharma, K., Jandeleit-Dahm, K. A., Zoungas, S., ...
& Cooper, M. E. (2015). Diabetic kidney disease. Nature Reviews Disease Primers. 1.
15018.
Toth-Manikowski, S., & Atta, M. G. (2015). Diabetic kidney disease: pathophysiology and
therapeutic targets. Journal of diabetes research. 2015.
Online
6
Causes of Chronic Kidney Disease. (2019). [Online]. Available through: <
https://www.niddk.nih.gov/health-information/kidney-disease/chronic-kidney-disease-
ckd/causes >.
Wong, W. (2012). CHRONIC KIDNEY DISEASE (CKD. [Online]. Available through: <
http://www.pathophys.org/ckd/#Pathophysiology >.
7
https://www.niddk.nih.gov/health-information/kidney-disease/chronic-kidney-disease-
ckd/causes >.
Wong, W. (2012). CHRONIC KIDNEY DISEASE (CKD. [Online]. Available through: <
http://www.pathophys.org/ckd/#Pathophysiology >.
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

8

9

10
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





