Cardiovascular & Respiratory Response to Aerobic Exercise - University
VerifiedAdded on 2023/04/11
|10
|2316
|146
Report
AI Summary
This report assesses the cardiovascular and respiratory responses to aerobic exercise in a 25-year-old female subject. The study utilizes spirometry, vitalograph, and ECG to measure lung function, electrical activity of the heart, and blood pressure changes during exercise. The results indicate that aerobic activity significantly impacts lung capacity, heart function, and blood pressure. Spirometry results show changes in expiratory and inspiratory volumes, while ECG displays variations in P wave, QRS complex, ST segment, and T wave during aerobic activity. The study highlights the importance of understanding these physiological changes to assess an individual's response to exercise. Desklib provides access to similar reports and study resources.
Assessment of Cardiovascular and Respiratory response during aerobic exercises
University
Name
Tutor
University
Name
Tutor
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2
Abstract
Aerobic activity has the ability to produce a significant effect on the cardiovascular and
respiratory responses. The investigation into the various phases of exercise shows a varied
activity of the chest and electro cadium waves displayed. Aerobic exercise entails intake and
exhalation of oxygen from the body, hence signifying various wave patterns. This study
displayed various activity forms of electro cadium activity and cardiovascular and respiratory
processes.
Introduction
Response to physiological processes often depends on the intensity, duration and the exercise
frequency coupled with environment presence. During exercise engagement, the needs of
oxygen tend to rise and the skeletal substrate increase, with the removal of metabolites and
carbon dioxide. The resulting mechanical and thermal effects alter metabolic, ventilator and
cardiovascular functions so as to meet the increased demands (Epstein et al., 2014). Physical
exercise elevation is associated with an increase in the metabolic activity of the
cardiovascular system in order to accommodate the resulting cardiac output. In this process,
various mechanisms take center stage. These include heart rate, vascular vasodilation,
ventilation functions, contractility of the heart and venous return.
Participation and engagement of physical exercise are often central and peripheral to
cardiovascular adaptations which enable the generation of large and sustained cardiac output.
Increase in cardiac output is key to generate stroke output. The cardiovascular system change
during exercise has an effect on the function of the skeletal muscles (Rivera-Brown et al.,
2012). They increase the requirement of substrate and oxygen requirements above resting
requirements. Resting blood flow linked to muscles is usually 2-4 mls/100 g ml/min is
elevated to almost 100ml/100gof muscle. The blood flow increase on the muscle and coroner,
the cerebral blood is often maintained with constant and splanchnic flow diminishing
(Porcelli et al., 2014).
Increased blood flow of to the muscles requires an elevated cardiac output which is direct
proportion to the increase in oxygen consumption. The output of the cardiac is increased
through the heart rate stroke volume which is attributed to the emptying of the systolic
contraction.
Abstract
Aerobic activity has the ability to produce a significant effect on the cardiovascular and
respiratory responses. The investigation into the various phases of exercise shows a varied
activity of the chest and electro cadium waves displayed. Aerobic exercise entails intake and
exhalation of oxygen from the body, hence signifying various wave patterns. This study
displayed various activity forms of electro cadium activity and cardiovascular and respiratory
processes.
Introduction
Response to physiological processes often depends on the intensity, duration and the exercise
frequency coupled with environment presence. During exercise engagement, the needs of
oxygen tend to rise and the skeletal substrate increase, with the removal of metabolites and
carbon dioxide. The resulting mechanical and thermal effects alter metabolic, ventilator and
cardiovascular functions so as to meet the increased demands (Epstein et al., 2014). Physical
exercise elevation is associated with an increase in the metabolic activity of the
cardiovascular system in order to accommodate the resulting cardiac output. In this process,
various mechanisms take center stage. These include heart rate, vascular vasodilation,
ventilation functions, contractility of the heart and venous return.
Participation and engagement of physical exercise are often central and peripheral to
cardiovascular adaptations which enable the generation of large and sustained cardiac output.
Increase in cardiac output is key to generate stroke output. The cardiovascular system change
during exercise has an effect on the function of the skeletal muscles (Rivera-Brown et al.,
2012). They increase the requirement of substrate and oxygen requirements above resting
requirements. Resting blood flow linked to muscles is usually 2-4 mls/100 g ml/min is
elevated to almost 100ml/100gof muscle. The blood flow increase on the muscle and coroner,
the cerebral blood is often maintained with constant and splanchnic flow diminishing
(Porcelli et al., 2014).
Increased blood flow of to the muscles requires an elevated cardiac output which is direct
proportion to the increase in oxygen consumption. The output of the cardiac is increased
through the heart rate stroke volume which is attributed to the emptying of the systolic
contraction.
3
Spirometry assessment is essential in measuring lung function ability. Forced Vital Capacity
–FVC and Forced Expiratory Capacity are essential aspects of exercise assessment. The long
duration of aerobic exercise improve the aerobic capacity and lead to good lung function. The
respiratory system ventilation increases during resting exercise. The resting value is 5-6 liters
per minute to about more than 100litres per minute. Ventilation process increases with an
increase in the work rate submaximal intensity level. An average resting oxygen intake is
about 250ml/min while in endurance exercise especially in athletes rises to 5000ml/min. The
elevated increase in the ventilation process of the pulmonary is linked to the increase of tidal
volume and respiratory rate which is linked to increased oxygen intake and output of oxygen.
Spirometry thus measures the volume moving out and into the respiratory system. It assessed
the mechanical function of the lungs, chest wall and respiratory muscles, it asses the total
lung capacity to the maximal expiration (Dwyer et al., 2014).
Ventilation process increases initially on the exercise level then followed on a gradual
increase. The elevated level of ventilation at the onset of exercise affects various activities.
The mechanism affects the arterial oxygen and carbon dioxide which are not abnormal to
stimulate respiration during exercise. Studies have indicated that the sensitivity of peripheral
chemoreceptors with respect to oscillations of Pao2 and Paco2 are linked to increased
ventilation while the absolute values remain. The central chemoreceptors are thus adjusted to
increase the ventilation level. Other explanations have been offered on the link of body
temperature role through the neurogenic impulses arising from motor cortex to location of
active muscles and joints stimulating brain stem and respiratory centre (Rivera-Brown et al.,
2012).
ECG tests refer to the standards used in the measurement of heart condition and abnormalities
associated. The tests show causing the display on the screen. Abnormal tests subject is in
producing an increase in heart arteries and blood pressure. ECG has been useful; in assessing
Ischemic in assessing prognostic signs. In ischemic ST-segment produces wave plateau
which slopes downwards. The flat depression is more than 0.1 mV which can persist in
longer times. Thus basically ECG expresses the visual representation of electrical activity
taking place on the heart. The construction and the pulse are stimulated with a natural signal
which is assessed using an ECG tests system. Exercise levels have shown an effect on the
ECG assessment levels (Molmen-Hansen et al., 2012).
Measurement of Blood Pressure and Heart Rate during exercise has shown a positive
Spirometry assessment is essential in measuring lung function ability. Forced Vital Capacity
–FVC and Forced Expiratory Capacity are essential aspects of exercise assessment. The long
duration of aerobic exercise improve the aerobic capacity and lead to good lung function. The
respiratory system ventilation increases during resting exercise. The resting value is 5-6 liters
per minute to about more than 100litres per minute. Ventilation process increases with an
increase in the work rate submaximal intensity level. An average resting oxygen intake is
about 250ml/min while in endurance exercise especially in athletes rises to 5000ml/min. The
elevated increase in the ventilation process of the pulmonary is linked to the increase of tidal
volume and respiratory rate which is linked to increased oxygen intake and output of oxygen.
Spirometry thus measures the volume moving out and into the respiratory system. It assessed
the mechanical function of the lungs, chest wall and respiratory muscles, it asses the total
lung capacity to the maximal expiration (Dwyer et al., 2014).
Ventilation process increases initially on the exercise level then followed on a gradual
increase. The elevated level of ventilation at the onset of exercise affects various activities.
The mechanism affects the arterial oxygen and carbon dioxide which are not abnormal to
stimulate respiration during exercise. Studies have indicated that the sensitivity of peripheral
chemoreceptors with respect to oscillations of Pao2 and Paco2 are linked to increased
ventilation while the absolute values remain. The central chemoreceptors are thus adjusted to
increase the ventilation level. Other explanations have been offered on the link of body
temperature role through the neurogenic impulses arising from motor cortex to location of
active muscles and joints stimulating brain stem and respiratory centre (Rivera-Brown et al.,
2012).
ECG tests refer to the standards used in the measurement of heart condition and abnormalities
associated. The tests show causing the display on the screen. Abnormal tests subject is in
producing an increase in heart arteries and blood pressure. ECG has been useful; in assessing
Ischemic in assessing prognostic signs. In ischemic ST-segment produces wave plateau
which slopes downwards. The flat depression is more than 0.1 mV which can persist in
longer times. Thus basically ECG expresses the visual representation of electrical activity
taking place on the heart. The construction and the pulse are stimulated with a natural signal
which is assessed using an ECG tests system. Exercise levels have shown an effect on the
ECG assessment levels (Molmen-Hansen et al., 2012).
Measurement of Blood Pressure and Heart Rate during exercise has shown a positive
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4
association. Heart rate increases the rate action during exercise especially due to cordial vagal
action initiation which is increases over time. The relationship of a rise in heart rate and
blood pressure increase is not plausible. Blood vessels get dilated to allow more blood to flow
and move easily. During the exercise, the heart rate speeds up more blood to reach the
muscles. Heart rate increases over time during physical exercise. The higher interest in
exercise increases the heart rate more (Molmen-Hansen et al., 2012).
With this overview, assessment of the physiological process underlying aerobic exercise is
essential. The key aspects entailing cardiovascular, respiratory and cardiac output levels are
enduring exercise activity. This study aims at investigating the response activities of
respiratory, cardiovascular and ventilator engagement during aerobic exercises.
Materials and methods
This assessment focuses on a female subject aged 25 years, with 58.6 kg and a height of 1.67
m. The heart rate monitor entails death rate of 68beats per minute, systolic pressure is 116mm
Hg while the diastolic pressure is 73mm Hg.
Respiratory and cardiovascular physiology
In the assessment of respiratory and cardiovascular parameters, the following materials were
useful; spirometry, vitalograph, ECG lab chart, heart rate, and blood pressure digital monitors
and Douglas bag to measure expired air.
Clean mouth piece filter was used at the end of clear plastic tubing on the opening of the
subjects. The tests were initiated with normal breathing and assessment of spirometry was
initiated. Handheld peak flow meters and the pneumotographs was used to compare the
results obtained. During the connection of the electrocardium, the electrodes were connected
on the electrodes. The right procedure was followed; the electrode run was placed in software
to run the series.
Assessment of blood pressure and pulse rate was connected into an automatic blood pressure
monitor and placed on the brachial artery. The arm position was placed on the arterial
brachial. The arm was adjusted to place the hand on the heart. The systolic and diastolic
pressures were recorded on the table.
association. Heart rate increases the rate action during exercise especially due to cordial vagal
action initiation which is increases over time. The relationship of a rise in heart rate and
blood pressure increase is not plausible. Blood vessels get dilated to allow more blood to flow
and move easily. During the exercise, the heart rate speeds up more blood to reach the
muscles. Heart rate increases over time during physical exercise. The higher interest in
exercise increases the heart rate more (Molmen-Hansen et al., 2012).
With this overview, assessment of the physiological process underlying aerobic exercise is
essential. The key aspects entailing cardiovascular, respiratory and cardiac output levels are
enduring exercise activity. This study aims at investigating the response activities of
respiratory, cardiovascular and ventilator engagement during aerobic exercises.
Materials and methods
This assessment focuses on a female subject aged 25 years, with 58.6 kg and a height of 1.67
m. The heart rate monitor entails death rate of 68beats per minute, systolic pressure is 116mm
Hg while the diastolic pressure is 73mm Hg.
Respiratory and cardiovascular physiology
In the assessment of respiratory and cardiovascular parameters, the following materials were
useful; spirometry, vitalograph, ECG lab chart, heart rate, and blood pressure digital monitors
and Douglas bag to measure expired air.
Clean mouth piece filter was used at the end of clear plastic tubing on the opening of the
subjects. The tests were initiated with normal breathing and assessment of spirometry was
initiated. Handheld peak flow meters and the pneumotographs was used to compare the
results obtained. During the connection of the electrocardium, the electrodes were connected
on the electrodes. The right procedure was followed; the electrode run was placed in software
to run the series.
Assessment of blood pressure and pulse rate was connected into an automatic blood pressure
monitor and placed on the brachial artery. The arm position was placed on the arterial
brachial. The arm was adjusted to place the hand on the heart. The systolic and diastolic
pressures were recorded on the table.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5
Analysis of Expired Air during Quiet Breathing using a Douglas Bag
The process of collecting expired air as initiate with the assembly of expired air. The
connection was undertaken and ensured that the bag is ready for collecting the expired air.
Before the collection process, the bag was checked if correcting assembling done and
collection initiated.
The air composition was analyzed through the usage of the gas analyzer, with baseline
recordings of the CO2% and O2%. The process was repeated while taking note of the
readings. The air in the Douglas bag was assessed and measured with key findings being
recorded and tabulated on a table.
Results
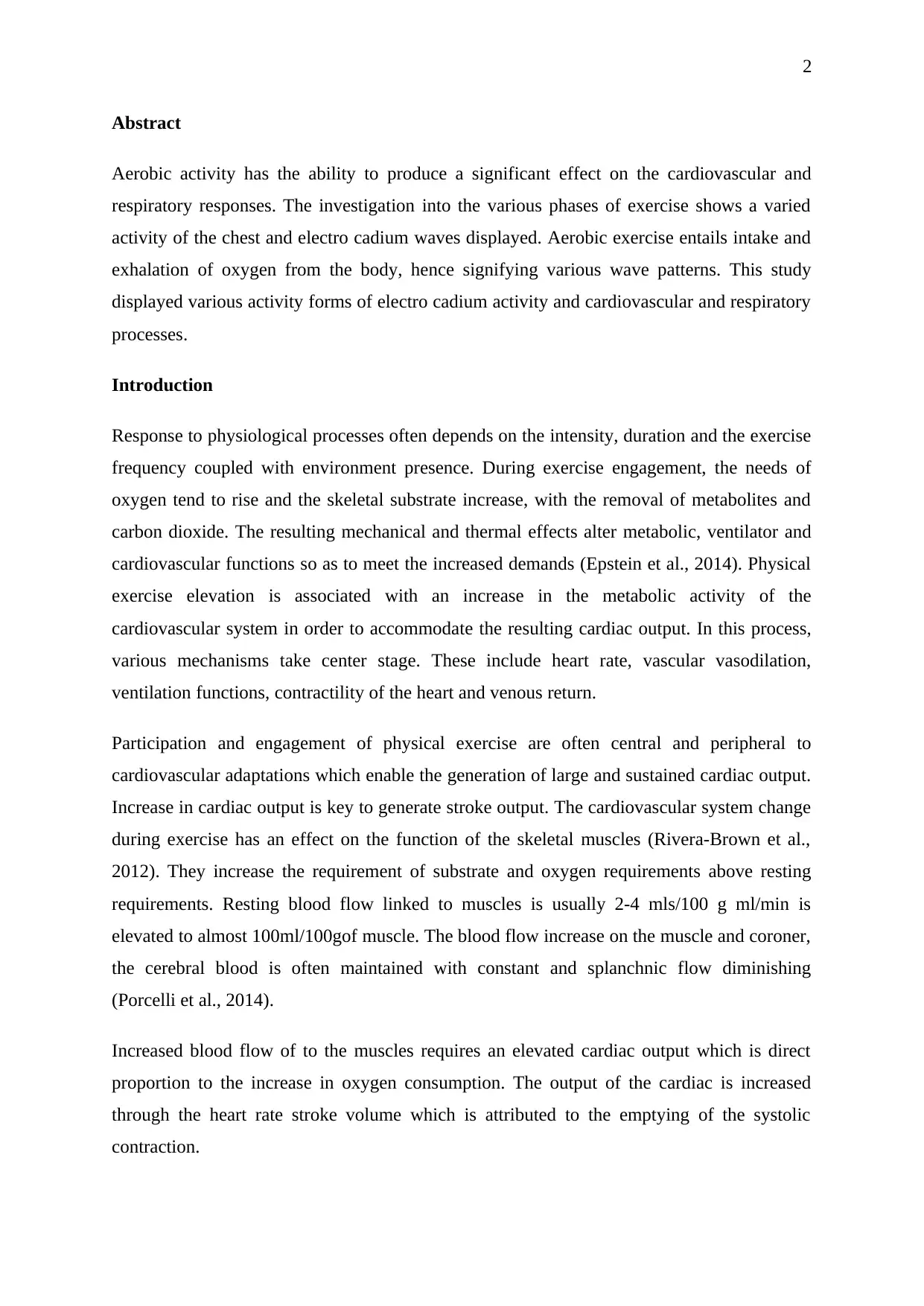
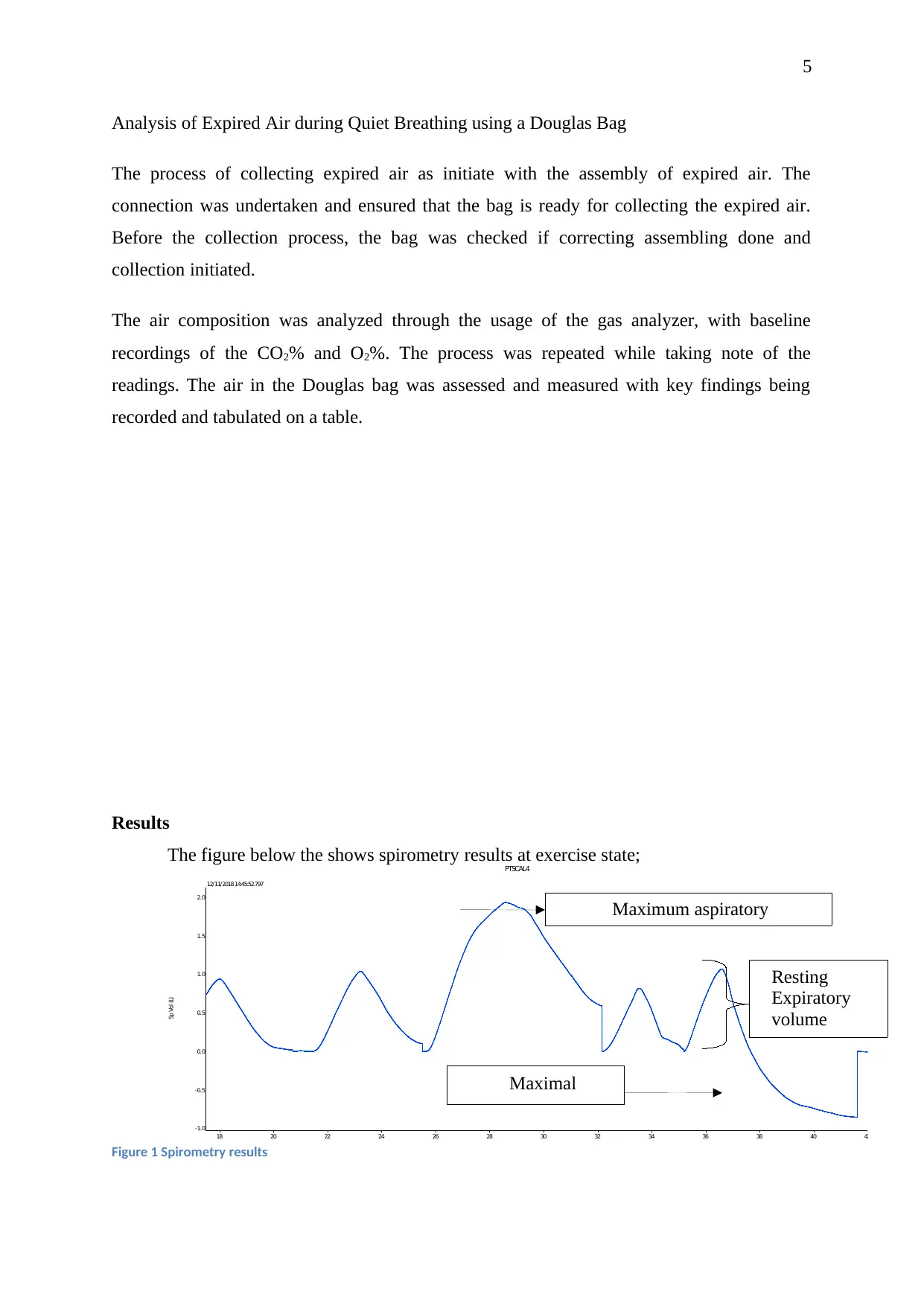
The figure below the shows spirometry results at exercise state;
PTSCAL4
Sp Vol (L)
-1.0
-0.5
0.0
0.5
1.0
1.5
2.0
18 20 22 24 26 28 30 32 34 36 38 40 42
12/11/2018 14:45:52.797
Figure 1 Spirometry results
Maximum aspiratory
Resting
Expiratory
volume
Maximal
expiratory
Analysis of Expired Air during Quiet Breathing using a Douglas Bag
The process of collecting expired air as initiate with the assembly of expired air. The
connection was undertaken and ensured that the bag is ready for collecting the expired air.
Before the collection process, the bag was checked if correcting assembling done and
collection initiated.
The air composition was analyzed through the usage of the gas analyzer, with baseline
recordings of the CO2% and O2%. The process was repeated while taking note of the
readings. The air in the Douglas bag was assessed and measured with key findings being
recorded and tabulated on a table.
Results
The figure below the shows spirometry results at exercise state;
PTSCAL4
Sp Vol (L)
-1.0
-0.5
0.0
0.5
1.0
1.5
2.0
18 20 22 24 26 28 30 32 34 36 38 40 42
12/11/2018 14:45:52.797
Figure 1 Spirometry results
Maximum aspiratory
Resting
Expiratory
volume
Maximal
expiratory
6
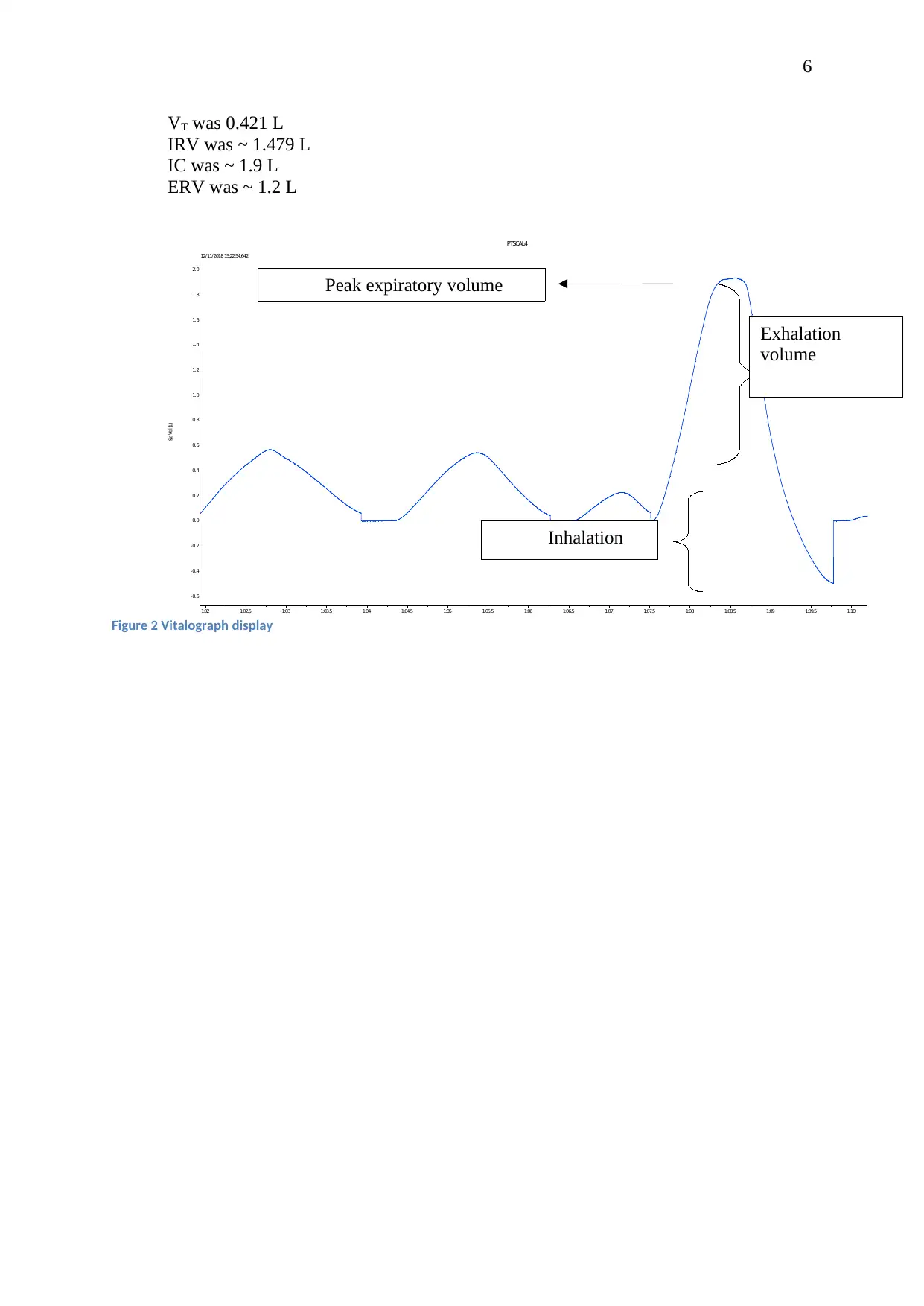
VT was 0.421 L
IRV was ~ 1.479 L
IC was ~ 1.9 L
ERV was ~ 1.2 L
PTSCAL4
Sp Vol (L)
-0.6
-0.4
-0.2
0.0
0.2
0.4
0.6
0.8
1.0
1.2
1.4
1.6
1.8
2.0
1:02 1:02.5 1:03 1:03.5 1:04 1:04.5 1:05 1:05.5 1:06 1:06.5 1:07 1:07.5 1:08 1:08.5 1:09 1:09.5 1:10
12/11/2018 15:22:54.642
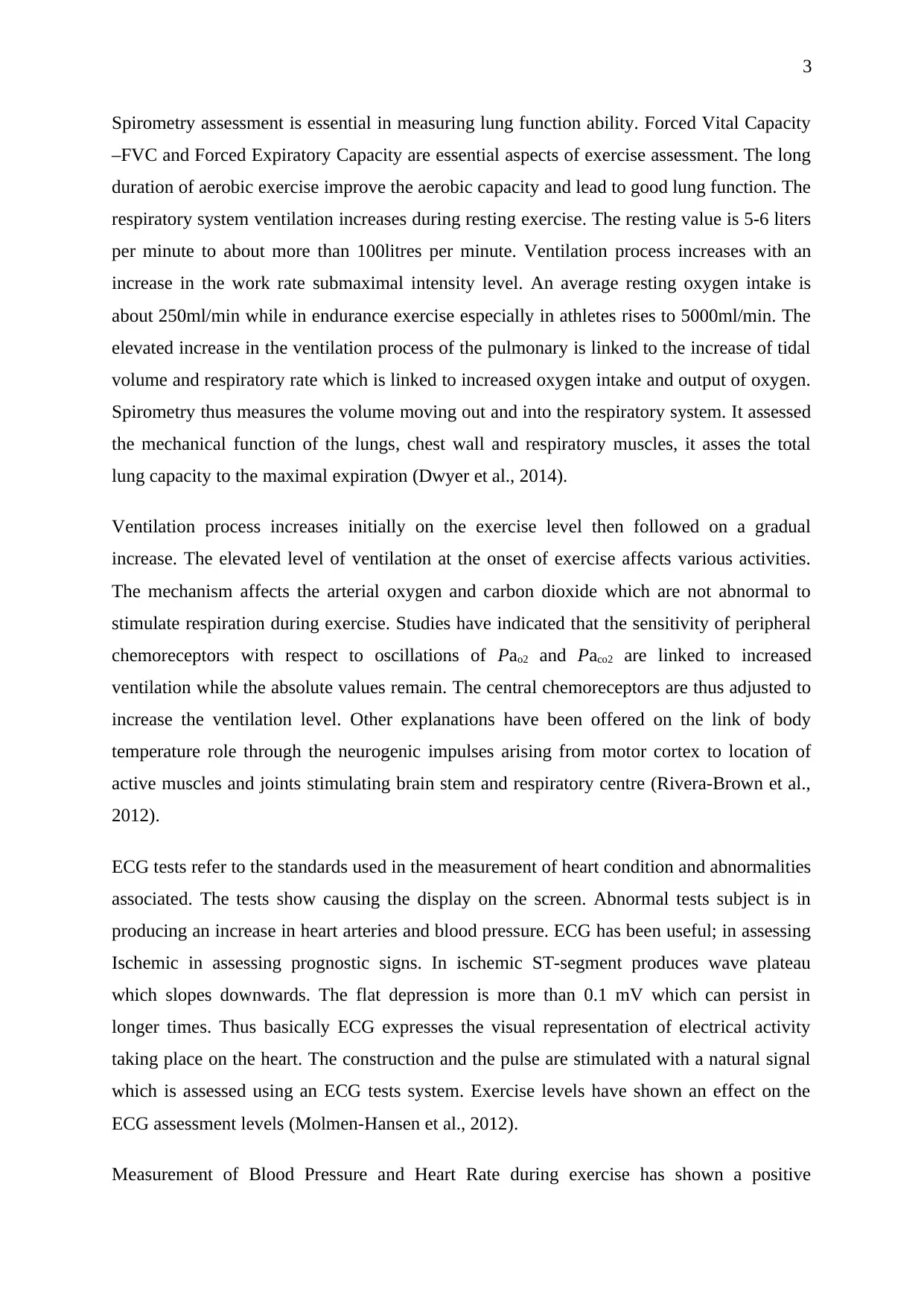
Figure 2 Vitalograph display
Peak expiratory volume
Inhalation
Exhalation
volume
VT was 0.421 L
IRV was ~ 1.479 L
IC was ~ 1.9 L
ERV was ~ 1.2 L
PTSCAL4
Sp Vol (L)
-0.6
-0.4
-0.2
0.0
0.2
0.4
0.6
0.8
1.0
1.2
1.4
1.6
1.8
2.0
1:02 1:02.5 1:03 1:03.5 1:04 1:04.5 1:05 1:05.5 1:06 1:06.5 1:07 1:07.5 1:08 1:08.5 1:09 1:09.5 1:10
12/11/2018 15:22:54.642
Figure 2 Vitalograph display
Peak expiratory volume
Inhalation
Exhalation
volume
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
PTSCAL4
EC
G
(
m
V)
-1.0
-0.8
-0.6
-0.4
-0.2
0.0
0.2
0.4
0.6
0.8
1.0
1.2
57.5 58
7
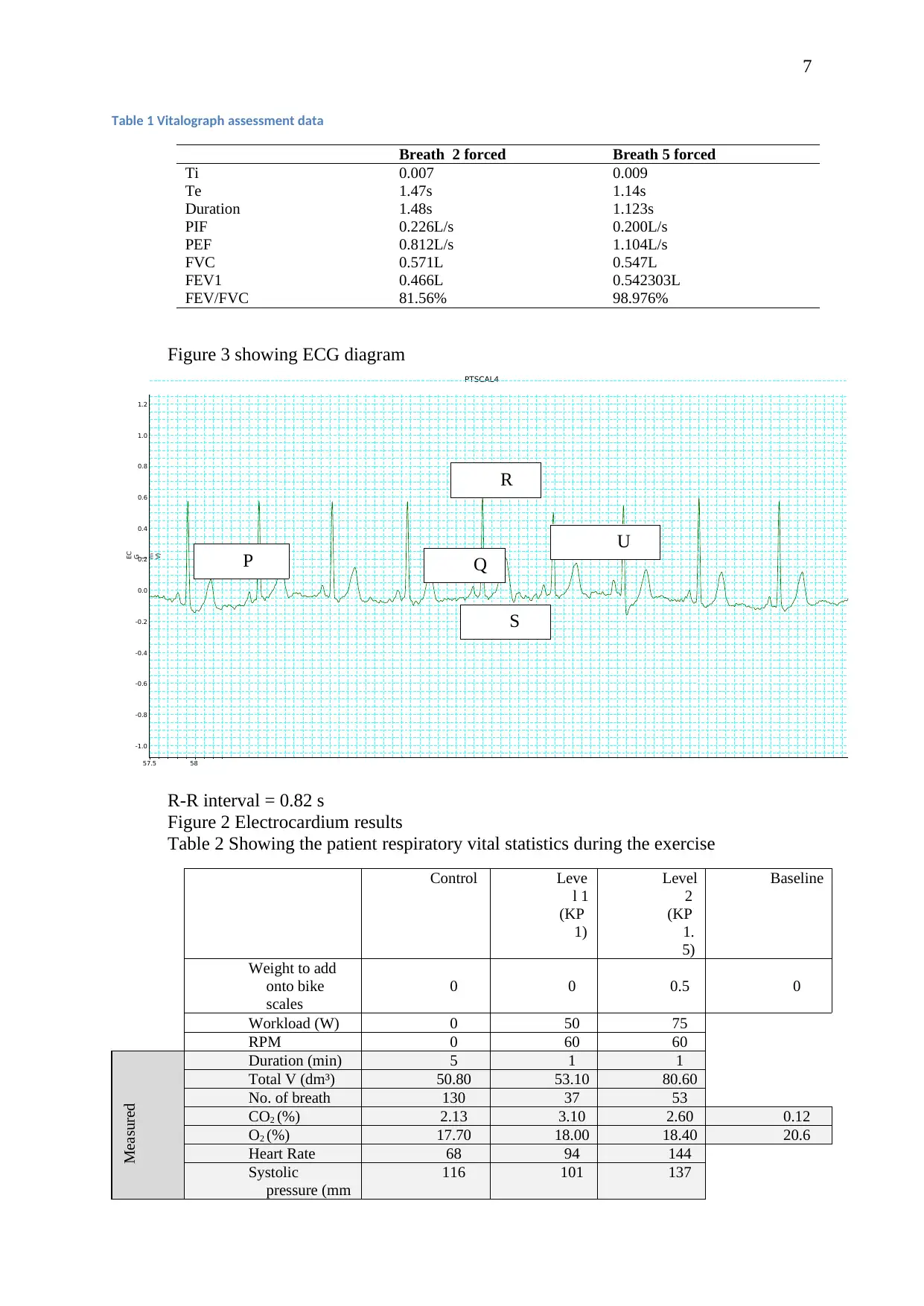
Table 1 Vitalograph assessment data
Breath 2 forced Breath 5 forced
Ti 0.007 0.009
Te 1.47s 1.14s
Duration 1.48s 1.123s
PIF 0.226L/s 0.200L/s
PEF 0.812L/s 1.104L/s
FVC 0.571L 0.547L
FEV1 0.466L 0.542303L
FEV/FVC 81.56% 98.976%
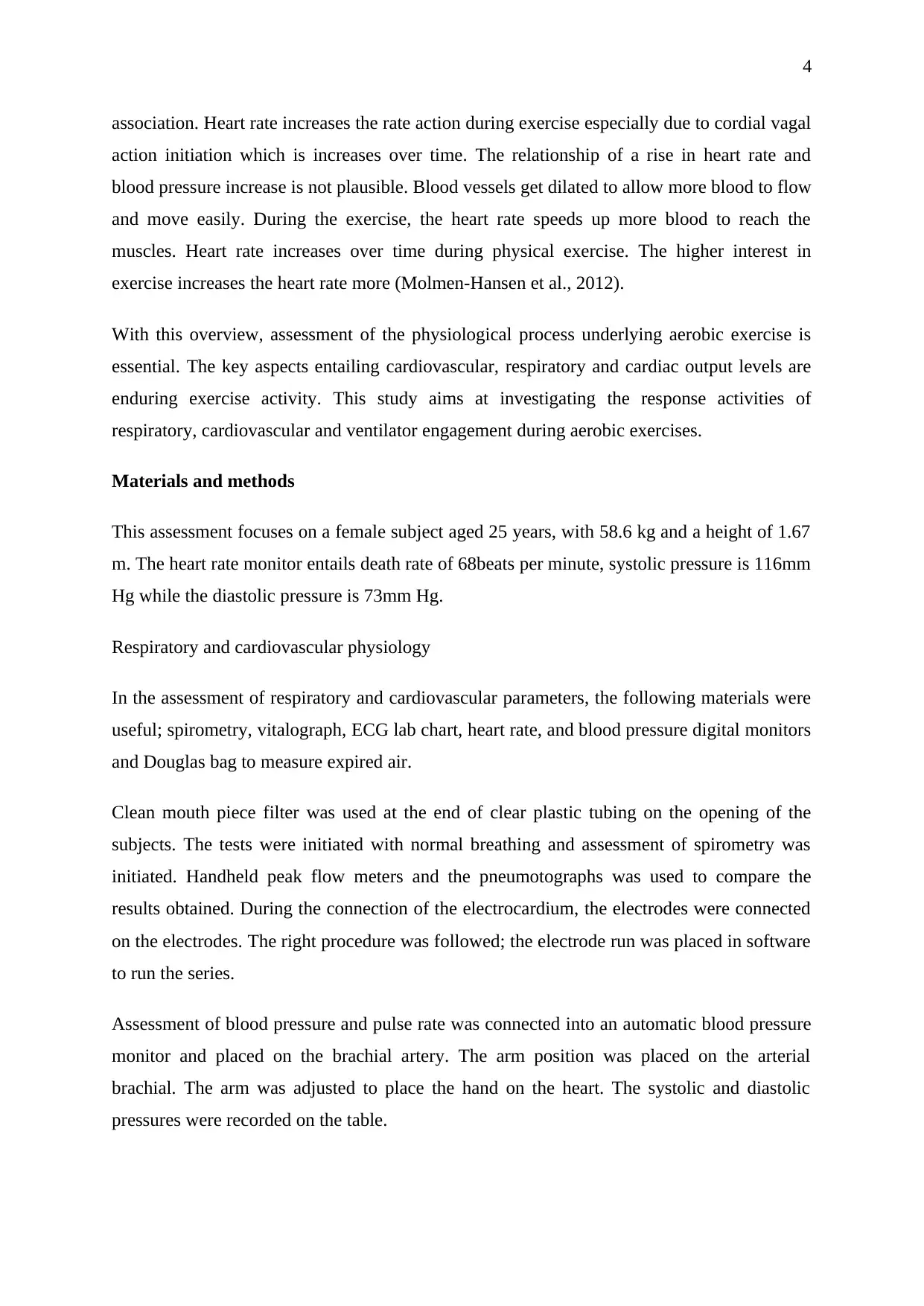
Figure 3 showing ECG diagram
R-R interval = 0.82 s
Figure 2 Electrocardium results
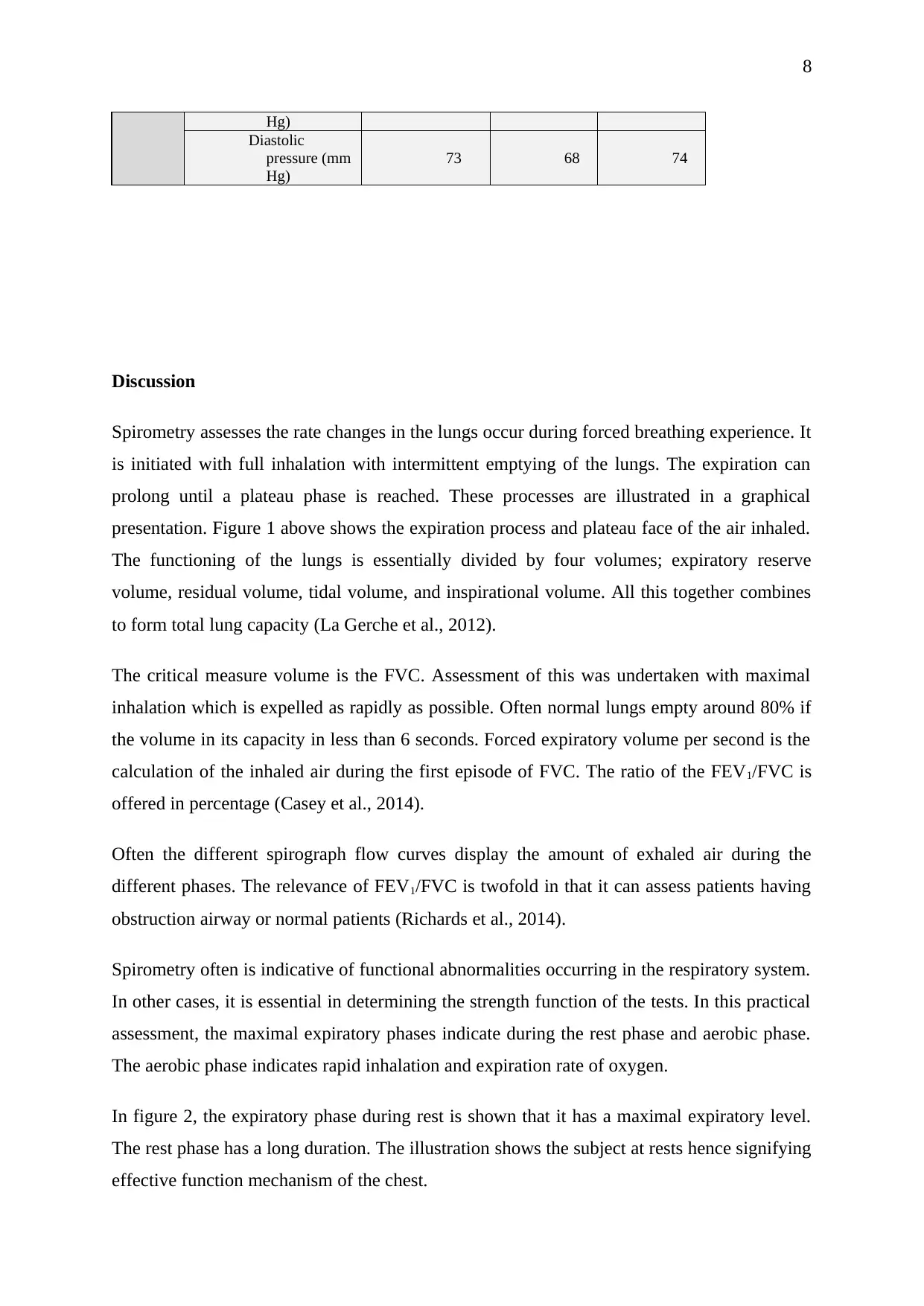
Table 2 Showing the patient respiratory vital statistics during the exercise
Control Leve
l 1
(KP
1)
Level
2
(KP
1.
5)
Baseline
Weight to add
onto bike
scales
0 0 0.5 0
Workload (W) 0 50 75
RPM 0 60 60
Measured
Duration (min) 5 1 1
Total V (dm³) 50.80 53.10 80.60
No. of breath 130 37 53
CO2 (%) 2.13 3.10 2.60 0.12
O2 (%) 17.70 18.00 18.40 20.6
Heart Rate 68 94 144
Systolic
pressure (mm
116 101 137
P Q
S
U
R
EC
G
(
m
V)
-1.0
-0.8
-0.6
-0.4
-0.2
0.0
0.2
0.4
0.6
0.8
1.0
1.2
57.5 58
7
Table 1 Vitalograph assessment data
Breath 2 forced Breath 5 forced
Ti 0.007 0.009
Te 1.47s 1.14s
Duration 1.48s 1.123s
PIF 0.226L/s 0.200L/s
PEF 0.812L/s 1.104L/s
FVC 0.571L 0.547L
FEV1 0.466L 0.542303L
FEV/FVC 81.56% 98.976%
Figure 3 showing ECG diagram
R-R interval = 0.82 s
Figure 2 Electrocardium results
Table 2 Showing the patient respiratory vital statistics during the exercise
Control Leve
l 1
(KP
1)
Level
2
(KP
1.
5)
Baseline
Weight to add
onto bike
scales
0 0 0.5 0
Workload (W) 0 50 75
RPM 0 60 60
Measured
Duration (min) 5 1 1
Total V (dm³) 50.80 53.10 80.60
No. of breath 130 37 53
CO2 (%) 2.13 3.10 2.60 0.12
O2 (%) 17.70 18.00 18.40 20.6
Heart Rate 68 94 144
Systolic
pressure (mm
116 101 137
P Q
S
U
R
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8
Hg)
Diastolic
pressure (mm
Hg)
73 68 74
Discussion
Spirometry assesses the rate changes in the lungs occur during forced breathing experience. It
is initiated with full inhalation with intermittent emptying of the lungs. The expiration can
prolong until a plateau phase is reached. These processes are illustrated in a graphical
presentation. Figure 1 above shows the expiration process and plateau face of the air inhaled.
The functioning of the lungs is essentially divided by four volumes; expiratory reserve
volume, residual volume, tidal volume, and inspirational volume. All this together combines
to form total lung capacity (La Gerche et al., 2012).
The critical measure volume is the FVC. Assessment of this was undertaken with maximal
inhalation which is expelled as rapidly as possible. Often normal lungs empty around 80% if
the volume in its capacity in less than 6 seconds. Forced expiratory volume per second is the
calculation of the inhaled air during the first episode of FVC. The ratio of the FEV1/FVC is
offered in percentage (Casey et al., 2014).
Often the different spirograph flow curves display the amount of exhaled air during the
different phases. The relevance of FEV1/FVC is twofold in that it can assess patients having
obstruction airway or normal patients (Richards et al., 2014).
Spirometry often is indicative of functional abnormalities occurring in the respiratory system.
In other cases, it is essential in determining the strength function of the tests. In this practical
assessment, the maximal expiratory phases indicate during the rest phase and aerobic phase.
The aerobic phase indicates rapid inhalation and expiration rate of oxygen.
In figure 2, the expiratory phase during rest is shown that it has a maximal expiratory level.
The rest phase has a long duration. The illustration shows the subject at rests hence signifying
effective function mechanism of the chest.
Hg)
Diastolic
pressure (mm
Hg)
73 68 74
Discussion
Spirometry assesses the rate changes in the lungs occur during forced breathing experience. It
is initiated with full inhalation with intermittent emptying of the lungs. The expiration can
prolong until a plateau phase is reached. These processes are illustrated in a graphical
presentation. Figure 1 above shows the expiration process and plateau face of the air inhaled.
The functioning of the lungs is essentially divided by four volumes; expiratory reserve
volume, residual volume, tidal volume, and inspirational volume. All this together combines
to form total lung capacity (La Gerche et al., 2012).
The critical measure volume is the FVC. Assessment of this was undertaken with maximal
inhalation which is expelled as rapidly as possible. Often normal lungs empty around 80% if
the volume in its capacity in less than 6 seconds. Forced expiratory volume per second is the
calculation of the inhaled air during the first episode of FVC. The ratio of the FEV1/FVC is
offered in percentage (Casey et al., 2014).
Often the different spirograph flow curves display the amount of exhaled air during the
different phases. The relevance of FEV1/FVC is twofold in that it can assess patients having
obstruction airway or normal patients (Richards et al., 2014).
Spirometry often is indicative of functional abnormalities occurring in the respiratory system.
In other cases, it is essential in determining the strength function of the tests. In this practical
assessment, the maximal expiratory phases indicate during the rest phase and aerobic phase.
The aerobic phase indicates rapid inhalation and expiration rate of oxygen.
In figure 2, the expiratory phase during rest is shown that it has a maximal expiratory level.
The rest phase has a long duration. The illustration shows the subject at rests hence signifying
effective function mechanism of the chest.
9
ECG assessment displays the electrical activity of the heart. The waveform components
indicate the electrical events of the heartbeat. With waveforms of P, Q, R, S, T and U, figure
3 above indicate a quick recession of the electrical conducts. The aerobic activity of the ECG
changes of the P wave, QRS complex, and the ST segment and T wave analyzed indicated
that the maximal P wave is shifting downwards. The Q wave amplitude is negative while the
R amplitude focus rises sharply. The QRS vectors show shifts in the right and posterior
position. The ST amplitude shifts upward exponentially. The magnitude of T lessons during
the aerobic state. After the assessment of all the measurements, there is a gradual return to the
normal resting point (La et al., 2013).
Thus it is essential that the cardiovascular changes on the rates of exercise. The spirometry
levels during exercise indicate the lung capacity to inhale and exhale exercise during aerobic
activity. The FVC is critical in assessing the activity of exercise. The maximal exhaled
volume and inhalation phases depict the respiration activity occurring during the level of
exercise activity. Thus, during exercise their changes which occur on the cardiovascular and
respiratory systems signifying elevated levels of gaseous exchange activity.
Bibliography
Casey, D.P., Treichler, D.P., Ganger IV, C.T., Schneider IV, A.C. and Ueda, K., 2014. Acute
dietary nitrate supplementation enhances compensatory vasodilation during hypoxic exercise
in older adults. American Journal of Physiology-Heart and Circulatory Physiology.
Dwyer, D.J., Belenky, P.A., Yang, J.H., MacDonald, I.C., Martell, J.D., Takahashi, N., Chan,
C.T., Lobritz, M.A., Braff, D., Schwarz, E.G. and Jonathan, D.Y., 2014. Antibiotics induce
redox-related physiological alterations as part of their lethality. Proceedings of the National
Academy of Sciences, 111(20), pp.E2100-E2109.
ECG assessment displays the electrical activity of the heart. The waveform components
indicate the electrical events of the heartbeat. With waveforms of P, Q, R, S, T and U, figure
3 above indicate a quick recession of the electrical conducts. The aerobic activity of the ECG
changes of the P wave, QRS complex, and the ST segment and T wave analyzed indicated
that the maximal P wave is shifting downwards. The Q wave amplitude is negative while the
R amplitude focus rises sharply. The QRS vectors show shifts in the right and posterior
position. The ST amplitude shifts upward exponentially. The magnitude of T lessons during
the aerobic state. After the assessment of all the measurements, there is a gradual return to the
normal resting point (La et al., 2013).
Thus it is essential that the cardiovascular changes on the rates of exercise. The spirometry
levels during exercise indicate the lung capacity to inhale and exhale exercise during aerobic
activity. The FVC is critical in assessing the activity of exercise. The maximal exhaled
volume and inhalation phases depict the respiration activity occurring during the level of
exercise activity. Thus, during exercise their changes which occur on the cardiovascular and
respiratory systems signifying elevated levels of gaseous exchange activity.
Bibliography
Casey, D.P., Treichler, D.P., Ganger IV, C.T., Schneider IV, A.C. and Ueda, K., 2014. Acute
dietary nitrate supplementation enhances compensatory vasodilation during hypoxic exercise
in older adults. American Journal of Physiology-Heart and Circulatory Physiology.
Dwyer, D.J., Belenky, P.A., Yang, J.H., MacDonald, I.C., Martell, J.D., Takahashi, N., Chan,
C.T., Lobritz, M.A., Braff, D., Schwarz, E.G. and Jonathan, D.Y., 2014. Antibiotics induce
redox-related physiological alterations as part of their lethality. Proceedings of the National
Academy of Sciences, 111(20), pp.E2100-E2109.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
10
Epstein, T., Xu, L., Gillies, R.J. and Gatenby, R.A., 2014. Separation of metabolic supply and
demand: aerobic glycolysis as a normal physiological response to fluctuating energetic
demands in the membrane. Cancer & metabolism, 2(1), p.7.
La, A.G., Claessen, G., de Bruaene Van, A., Pattyn, N., Van, J.C., Gewillig, M., Bogaert, J.,
Dymarkowski, S., Claus, P. and Heidbuchel, H., 2013. Cardiac MRI: a new gold standard for
ventricular volume quantification during high-intensity exercise. Circulation. Cardiovascular
imaging, 6(2), pp.329-338.
Molmen-Hansen, H.E., Stolen, T., Tjonna, A.E., Aamot, I.L., Ekeberg, I.S., Tyldum, G.A.,
Wisloff, U., Ingul, C.B. and Stoylen, A., 2012. Aerobic interval training reduces blood
pressure and improves myocardial function in hypertensive patients. European journal of
preventive cardiology, 19(2), pp.151-160.
Richards, J.C., Luckasen, G.J., Larson, D.G. and Dinenno, F.A., 2014. Role of α‐adrenergic
vasoconstriction in regulating skeletal muscle blood flow and vascular conductance during
forearm exercise in ageing humans. The Journal of physiology, 592(21), pp.4775-4788.
Rivera-Brown, A.M. and Frontera, W.R., 2012. Principles of exercise physiology: responses
to acute exercise and long-term adaptations to training. Pm&r, 4(11), pp.797-804.
Rivera-Brown, A.M. and Frontera, W.R., 2012. Principles of exercise physiology: responses
to acute exercise and long-term adaptations to training. Pm&r, 4(11), pp.797-804.
Thanassoulis, G., Lyass, A., Benjamin, E.J., Larson, M.G., Vita, J.A., Levy, D., Hamburg,
N.M., Widlansky, M.E., O'Donnell, C.J., Mitchell, G.F. and Vasan, R.S., 2012. Relations of
exercise blood pressure response to cardiovascular risk factors and vascular function in the
Framingham Heart Study. Circulation, 125(23), pp.2836-2843.
Epstein, T., Xu, L., Gillies, R.J. and Gatenby, R.A., 2014. Separation of metabolic supply and
demand: aerobic glycolysis as a normal physiological response to fluctuating energetic
demands in the membrane. Cancer & metabolism, 2(1), p.7.
La, A.G., Claessen, G., de Bruaene Van, A., Pattyn, N., Van, J.C., Gewillig, M., Bogaert, J.,
Dymarkowski, S., Claus, P. and Heidbuchel, H., 2013. Cardiac MRI: a new gold standard for
ventricular volume quantification during high-intensity exercise. Circulation. Cardiovascular
imaging, 6(2), pp.329-338.
Molmen-Hansen, H.E., Stolen, T., Tjonna, A.E., Aamot, I.L., Ekeberg, I.S., Tyldum, G.A.,
Wisloff, U., Ingul, C.B. and Stoylen, A., 2012. Aerobic interval training reduces blood
pressure and improves myocardial function in hypertensive patients. European journal of
preventive cardiology, 19(2), pp.151-160.
Richards, J.C., Luckasen, G.J., Larson, D.G. and Dinenno, F.A., 2014. Role of α‐adrenergic
vasoconstriction in regulating skeletal muscle blood flow and vascular conductance during
forearm exercise in ageing humans. The Journal of physiology, 592(21), pp.4775-4788.
Rivera-Brown, A.M. and Frontera, W.R., 2012. Principles of exercise physiology: responses
to acute exercise and long-term adaptations to training. Pm&r, 4(11), pp.797-804.
Rivera-Brown, A.M. and Frontera, W.R., 2012. Principles of exercise physiology: responses
to acute exercise and long-term adaptations to training. Pm&r, 4(11), pp.797-804.
Thanassoulis, G., Lyass, A., Benjamin, E.J., Larson, M.G., Vita, J.A., Levy, D., Hamburg,
N.M., Widlansky, M.E., O'Donnell, C.J., Mitchell, G.F. and Vasan, R.S., 2012. Relations of
exercise blood pressure response to cardiovascular risk factors and vascular function in the
Framingham Heart Study. Circulation, 125(23), pp.2836-2843.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





