GP Trainer Journey Essay
VerifiedAdded on 2019/09/25
|11
|5481
|389
Essay
AI Summary
This essay chronicles the author's journey to becoming a GP trainer. It focuses on three key aspects: reflection, perseverance, and negotiation and decision-making. The author details their experiences as a GDMO supervisor in the army, highlighting the importance of teaching methods, feedback, and assessment. They discuss challenges in establishing a training practice, including navigating resistance from superiors and colleagues. The essay also explores the use of reflective practices like Gibbs' reflective cycle and the importance of continuous professional development. The author emphasizes the significance of perseverance in overcoming obstacles and achieving long-term goals. The narrative includes experiences with significant event analysis, patient satisfaction questionnaires, and 360-degree feedback. The author also discusses the importance of negotiation skills in various contexts, from patient consultations to practice management. The essay concludes with reflections on the author's experiences and lessons learned, emphasizing the importance of feedback, support, and perseverance in achieving success in medical training and practice management.

Assignment – Journey of becoming a trainer, rescuing a practice under
threat and maintaining good quality of care.
My essay is about the journey of becoming a GP trainer. Throughout this journey I would like to
comment on 3 main facets of learning, Reflection, perseverance, negotiation and decision
making.
Reflection:
This journey started when I was working as a GP in the army. I was very keen to become a GP
trainer as I was a General Duty Medical officer (GDMO) supervisor at that point. General Duty
Medical officers are trainee doctors in the army. They have completed their Foundation year
training and before they start their speciality training they have to do general duties in the army
for 2 yrs. As these doctors are not fully qualified general practitioners, they should work under
the supervision of a GDMO supervisor. GDMO supervisor is a GP in the army who has had
training. Which involves attending the 3 day course - introduction to medical education. During
this course I learnt about who are GDMOs and their role in the army. Teaching methods, giving
feedback, assessing the trainees. We engaged in group work and role playing.
As a GDMO supervisor you will be supervising up to 2 trainees at a time. I had 2 trainees at the
time. Before they arrive I will arrange them an induction package which will include
introduction to the building, to the computer system, and all the areas of the medical centre,
the reception, pharmacy treatment room and clinics. During the induction I encourage them to
sit with all GPs in the practice in order for them to see their consultation styles.
“1Bad consultations result from having insufficient clinical knowledge, from failing to relate to
patients or from failing to understand the patient's behaviour, his perception of his illness or its
context“
It is paramount to have a consultation style that works for the doctor and also works for the
patient as well, to deliver excellent clinical care. As GPs we all consult in slightly different ways
and it is good to observe and learn. Following this we will have joint clinics. After each
consultation we will discuss about what went well, and is there anything that could have done
better. During the consultation, if I felt there is something that would have affected patient care
I would intervene at that time. Following joint clinics, they will start their own clinics. During
their training I will encourage them to attend sessions with the regional occupational health
team where they conduct medical boards for patients. Also they will attend sessions with
physiotherapy department, community mental health department and regional rehabilitation
unit. We will also have weekly tutorials. Tutorials will be interactive and will be on a topic that
the trainee would like to discuss or anything that I feel trainee’s learning need. We will also
have case based discussions sometimes during a tutorial. During their stay in the practice I will
1JGR Howie (1985)
threat and maintaining good quality of care.
My essay is about the journey of becoming a GP trainer. Throughout this journey I would like to
comment on 3 main facets of learning, Reflection, perseverance, negotiation and decision
making.
Reflection:
This journey started when I was working as a GP in the army. I was very keen to become a GP
trainer as I was a General Duty Medical officer (GDMO) supervisor at that point. General Duty
Medical officers are trainee doctors in the army. They have completed their Foundation year
training and before they start their speciality training they have to do general duties in the army
for 2 yrs. As these doctors are not fully qualified general practitioners, they should work under
the supervision of a GDMO supervisor. GDMO supervisor is a GP in the army who has had
training. Which involves attending the 3 day course - introduction to medical education. During
this course I learnt about who are GDMOs and their role in the army. Teaching methods, giving
feedback, assessing the trainees. We engaged in group work and role playing.
As a GDMO supervisor you will be supervising up to 2 trainees at a time. I had 2 trainees at the
time. Before they arrive I will arrange them an induction package which will include
introduction to the building, to the computer system, and all the areas of the medical centre,
the reception, pharmacy treatment room and clinics. During the induction I encourage them to
sit with all GPs in the practice in order for them to see their consultation styles.
“1Bad consultations result from having insufficient clinical knowledge, from failing to relate to
patients or from failing to understand the patient's behaviour, his perception of his illness or its
context“
It is paramount to have a consultation style that works for the doctor and also works for the
patient as well, to deliver excellent clinical care. As GPs we all consult in slightly different ways
and it is good to observe and learn. Following this we will have joint clinics. After each
consultation we will discuss about what went well, and is there anything that could have done
better. During the consultation, if I felt there is something that would have affected patient care
I would intervene at that time. Following joint clinics, they will start their own clinics. During
their training I will encourage them to attend sessions with the regional occupational health
team where they conduct medical boards for patients. Also they will attend sessions with
physiotherapy department, community mental health department and regional rehabilitation
unit. We will also have weekly tutorials. Tutorials will be interactive and will be on a topic that
the trainee would like to discuss or anything that I feel trainee’s learning need. We will also
have case based discussions sometimes during a tutorial. During their stay in the practice I will
1JGR Howie (1985)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
encourage them to do a full circle audit, a patient satisfaction questionnaire and a 360
feedback. They can successfully conduct these as they will be in the surgery for 2 yrs. Also we
will discuss any significant events, complaints or compliments.
I really enjoyed supervising these trainees. As they have already had their foundation year
training they did have very good clinical skills. They also had other expertise that we as a whole
practice could benefit from. Once one of my trainees were an Advanced Life Support (ALS)
provider. So we managed to use his expertise to arrange a Basic Life Support training for the
practice. I found doing joint clinics were very rewarding. It has always been a 2 way learning
experience. Once, one of my trainees had a very polite manner of consulting. Even he had a
higher rank than most of the patients he will always call them very politely and respectfully. He
will always shake hands with patients before a consultation and give them enough time to
express themselves. I thought this is a really good way of having a good rapport with patients.
Part of military general practice did involve occupational health i.e. grading patients
appropriately so that they will be employed appropriately. During joint clinical sessions,
conducting medical boards I found very useful for me as a trainer/Supervisor. In this situation
doctors need to have extremely good communication and negotiation skills. Patients do not like
to be down-graded due to medical problems as it will affect their promotions and development.
On the other hand, chain of command and their line managers wants us to down grade them
appropriately so that they can employ their soldiers accordingly. In this situation we have to
explain to the patient in a way that they understand and agree and then without breeching
confidentiality, give as much information as possible to the chain of command so that they can
employ them appropriately. In the mean time we have to discuss with the regional occupational
health team as well, making sure we have done the right thing. I could see initially in some of
my trainees that they didn’t have adequate negotiating and communicating skills, specially with
their military background and they thought this is a challenging situation. It was a pleasure to
guide them through these skills and to see them flourish. I can remember once, one of my
trainees explained the medical situation and the grading process to a patient and then he
realised he had given too much information too soon to the patient. Then he apologized and
discussed again.
For these trainee we had to provide 6 monthly reports recording their progress of learning and
development. Every 6 months we will have a meeting and discuss their experience, concerns,
learning needs. We will agree on a personal development plan. I will give them feed-back on
their progress.
Our Senior Medical Officer at this time was also very supportive and the teaching experience I
gained during this period was great. Also we had the opportunity to have regular discussions
about teaching and supervising. This experience encouraged me to explore the opportunity of
becoming a GP trainer.
After discussing with the clinical lead for GP training I was given permission to attend the
prospective trainers course. This is how I started my journey. Here I am now after almost 3yrs.
later working in an NHS practice, becoming the senior partner of the practice and hoping to
continue as a GP trainer. I was not expecting this extraordinary journey, overcoming greatest
difficulties that I never expected and at the same time taking me through an extraordinary
steep learning curve.
feedback. They can successfully conduct these as they will be in the surgery for 2 yrs. Also we
will discuss any significant events, complaints or compliments.
I really enjoyed supervising these trainees. As they have already had their foundation year
training they did have very good clinical skills. They also had other expertise that we as a whole
practice could benefit from. Once one of my trainees were an Advanced Life Support (ALS)
provider. So we managed to use his expertise to arrange a Basic Life Support training for the
practice. I found doing joint clinics were very rewarding. It has always been a 2 way learning
experience. Once, one of my trainees had a very polite manner of consulting. Even he had a
higher rank than most of the patients he will always call them very politely and respectfully. He
will always shake hands with patients before a consultation and give them enough time to
express themselves. I thought this is a really good way of having a good rapport with patients.
Part of military general practice did involve occupational health i.e. grading patients
appropriately so that they will be employed appropriately. During joint clinical sessions,
conducting medical boards I found very useful for me as a trainer/Supervisor. In this situation
doctors need to have extremely good communication and negotiation skills. Patients do not like
to be down-graded due to medical problems as it will affect their promotions and development.
On the other hand, chain of command and their line managers wants us to down grade them
appropriately so that they can employ their soldiers accordingly. In this situation we have to
explain to the patient in a way that they understand and agree and then without breeching
confidentiality, give as much information as possible to the chain of command so that they can
employ them appropriately. In the mean time we have to discuss with the regional occupational
health team as well, making sure we have done the right thing. I could see initially in some of
my trainees that they didn’t have adequate negotiating and communicating skills, specially with
their military background and they thought this is a challenging situation. It was a pleasure to
guide them through these skills and to see them flourish. I can remember once, one of my
trainees explained the medical situation and the grading process to a patient and then he
realised he had given too much information too soon to the patient. Then he apologized and
discussed again.
For these trainee we had to provide 6 monthly reports recording their progress of learning and
development. Every 6 months we will have a meeting and discuss their experience, concerns,
learning needs. We will agree on a personal development plan. I will give them feed-back on
their progress.
Our Senior Medical Officer at this time was also very supportive and the teaching experience I
gained during this period was great. Also we had the opportunity to have regular discussions
about teaching and supervising. This experience encouraged me to explore the opportunity of
becoming a GP trainer.
After discussing with the clinical lead for GP training I was given permission to attend the
prospective trainers course. This is how I started my journey. Here I am now after almost 3yrs.
later working in an NHS practice, becoming the senior partner of the practice and hoping to
continue as a GP trainer. I was not expecting this extraordinary journey, overcoming greatest
difficulties that I never expected and at the same time taking me through an extraordinary
steep learning curve.
Perseverance:
So I felt so happy with the opportunity of doing the prospective trainers course and managed to
successfully complete the course soon after. Unfortunately, the military medical center I
worked at that time wasn’t a training practice. So I had to use GDMOs as my trainees.
I was really keen to make that practice a training practice. In the meantime, unfortunately our
senior medical officer, who was very keen on making that practice a training practice, was
posted. His successor was not a GP trainer and wasn't keen to have GP trainees. So my efforts
unfortunately became to no avail. So I requested a transfer to another practice which was
already a training practice. This wasn’t going to happen either. I became very frustrated. This
was my first job as a qualified GP. By then I had worked there for 7 yrs.
When I started in this practice there were six GPs. But unfortunately there were no continuous
professional development (CPD) events happening in this practice and all the doctors were
carrying out their normal day-to-day work. There were no clinical meetings or dedicated
professional development time. We didn't have any trainees either. During this time I was doing
my membership exam and I was very keen on having continuous professional development
activities in the practice. I encouraged other doctors to get involved. We had a Senior Medical
Officer (SMO)who was just posted and a GP trainer. He was also very keen on professional
development and training.
With his help I initiated the lunch time clinical meetings. We had a rotation that all of us
participated in presenting an important topic every week.
In the mean-time, I was very keen to bring in Significant Event Analysis (SEA) and Audits to the
practice. I could remember for the first time ever when we had a SEA meeting, one of the
doctors took it very personally and became very angry towards all of us. We reiterated several
times it was all about learning from our mistakes in order to find out what we could do
differently for a better outcome for our patients.
Gibbs reflective cycle:
The reflective cycle (Gibbs 1988)
So I felt so happy with the opportunity of doing the prospective trainers course and managed to
successfully complete the course soon after. Unfortunately, the military medical center I
worked at that time wasn’t a training practice. So I had to use GDMOs as my trainees.
I was really keen to make that practice a training practice. In the meantime, unfortunately our
senior medical officer, who was very keen on making that practice a training practice, was
posted. His successor was not a GP trainer and wasn't keen to have GP trainees. So my efforts
unfortunately became to no avail. So I requested a transfer to another practice which was
already a training practice. This wasn’t going to happen either. I became very frustrated. This
was my first job as a qualified GP. By then I had worked there for 7 yrs.
When I started in this practice there were six GPs. But unfortunately there were no continuous
professional development (CPD) events happening in this practice and all the doctors were
carrying out their normal day-to-day work. There were no clinical meetings or dedicated
professional development time. We didn't have any trainees either. During this time I was doing
my membership exam and I was very keen on having continuous professional development
activities in the practice. I encouraged other doctors to get involved. We had a Senior Medical
Officer (SMO)who was just posted and a GP trainer. He was also very keen on professional
development and training.
With his help I initiated the lunch time clinical meetings. We had a rotation that all of us
participated in presenting an important topic every week.
In the mean-time, I was very keen to bring in Significant Event Analysis (SEA) and Audits to the
practice. I could remember for the first time ever when we had a SEA meeting, one of the
doctors took it very personally and became very angry towards all of us. We reiterated several
times it was all about learning from our mistakes in order to find out what we could do
differently for a better outcome for our patients.
Gibbs reflective cycle:
The reflective cycle (Gibbs 1988)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
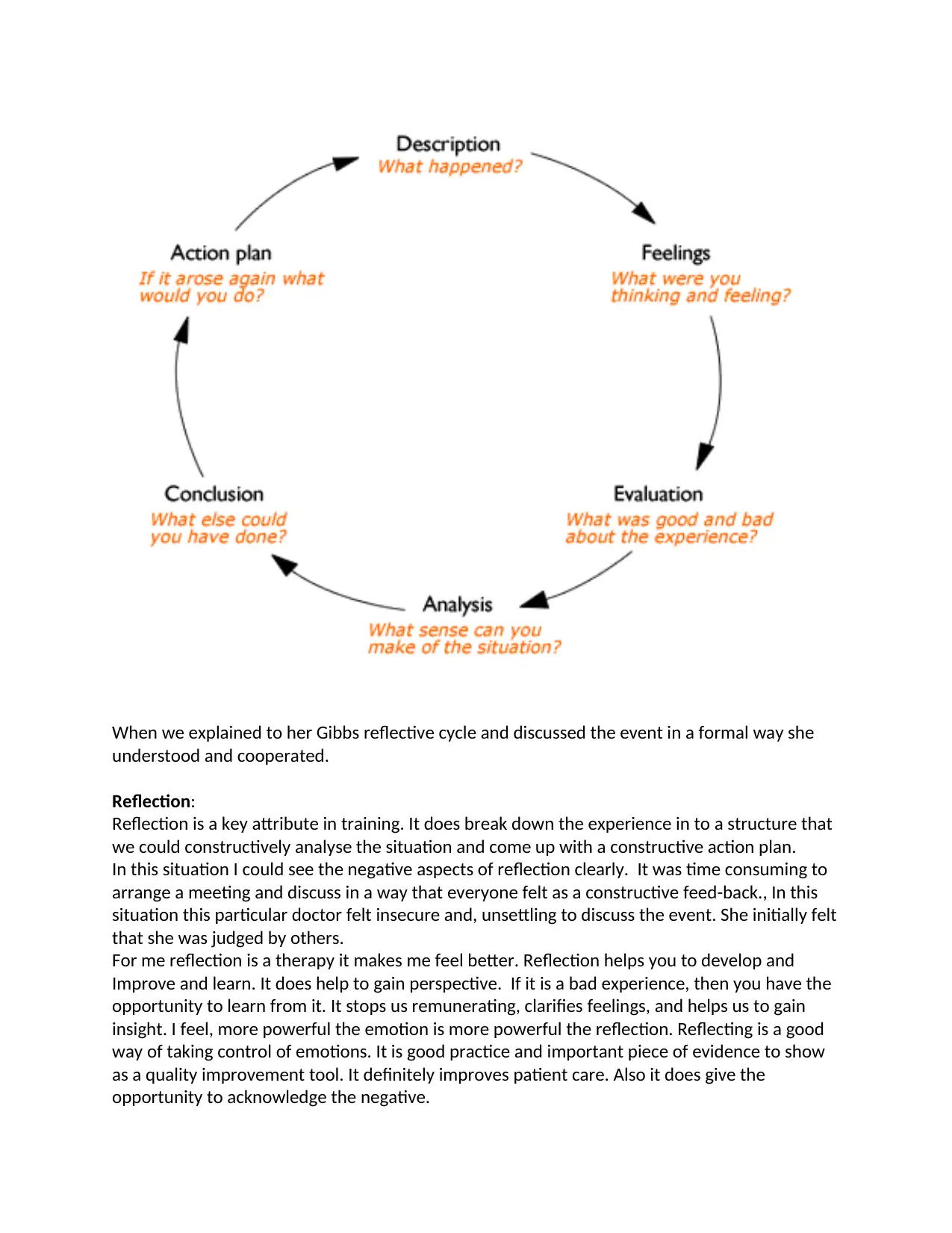
When we explained to her Gibbs reflective cycle and discussed the event in a formal way she
understood and cooperated.
Reflection:
Reflection is a key attribute in training. It does break down the experience in to a structure that
we could constructively analyse the situation and come up with a constructive action plan.
In this situation I could see the negative aspects of reflection clearly. It was time consuming to
arrange a meeting and discuss in a way that everyone felt as a constructive feed-back., In this
situation this particular doctor felt insecure and, unsettling to discuss the event. She initially felt
that she was judged by others.
For me reflection is a therapy it makes me feel better. Reflection helps you to develop and
Improve and learn. It does help to gain perspective. If it is a bad experience, then you have the
opportunity to learn from it. It stops us remunerating, clarifies feelings, and helps us to gain
insight. I feel, more powerful the emotion is more powerful the reflection. Reflecting is a good
way of taking control of emotions. It is good practice and important piece of evidence to show
as a quality improvement tool. It definitely improves patient care. Also it does give the
opportunity to acknowledge the negative.
understood and cooperated.
Reflection:
Reflection is a key attribute in training. It does break down the experience in to a structure that
we could constructively analyse the situation and come up with a constructive action plan.
In this situation I could see the negative aspects of reflection clearly. It was time consuming to
arrange a meeting and discuss in a way that everyone felt as a constructive feed-back., In this
situation this particular doctor felt insecure and, unsettling to discuss the event. She initially felt
that she was judged by others.
For me reflection is a therapy it makes me feel better. Reflection helps you to develop and
Improve and learn. It does help to gain perspective. If it is a bad experience, then you have the
opportunity to learn from it. It stops us remunerating, clarifies feelings, and helps us to gain
insight. I feel, more powerful the emotion is more powerful the reflection. Reflecting is a good
way of taking control of emotions. It is good practice and important piece of evidence to show
as a quality improvement tool. It definitely improves patient care. Also it does give the
opportunity to acknowledge the negative.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
This experience gave me the opportunity to develop as a trainer. It shows me how difficult it is
to give constructive feed-back to someone if that person has had less exposure on getting feed-
back. It will be even harder if that person is not used to reflecting either. This encouraged me to
give constructive feed-back to my trainees as early as possible. Also encouraging them to seek
feed-back from other colleagues, patients etc. Also teaching them to reflect on their actions.
I feel significant event analysis are a very good way of reflecting and learning from our
mistakes.
Gibbs cycle can be used in many ways as a trainer. It can be used to explore any incident that
you would like to discuss and evaluate in a structured way. It gives the opportunity to speak up
your feelings helping to be self-aware. It gives the opportunity to discuss and evaluate among
group of people. It helps to make a judgement about what happened and consider what had
gone well, and what had gone not so well. Then analyse the situation in several parts, what
went well, what did you do well, what others did well, what went wrong, in what way did you
or others contributed to this. Then the synthesis stage where you would develop an insight into
every bodies behaviour. Detailed analysis and honest exploration will lead for you to realise
what could have done better bringing you to an action plan.
Perseverance:
At this time the revalidation process had started officially and we all realised the importance of
having comprehensive appraisals. Before revalidation, appraisals happened in the army
according to a military protocol and was usually a discussion with a military appraiser. I always
reiterated the importance of doing Patient Satisfaction questionnaires (PSQ) and 360
feedbacks. 360 feed-back is a multi- source feedback which includes colleague and self-
assessment questionnaires. It gives you valuable information about your performance that are
difficult to quantify. It gives you a good opportunity to reflect and change your behaviour for
the best.
“Feedback about professionalism is necessary to change practice and behaviour. This technique
focuses on multiple perspectives and levels of evaluation leading to results that are considered
to be highly credible and a powerful tool to change behaviour.” 2
Following study had looked at how leaders reacted to feed back.
“For leaders with low ratings, those who agreed with others about their ratings were less
motivated than those who received low ratings and over rated themselves. For leaders with high
ratings, agreement between self and other did not influence their motivation. Individuals with
more favorable attitudes toward using feedback were more motivated following feedback.”3
I feel these results are very interesting and useful.
2 360-degree Feedback: Possibilities for Assessment of the ACGME Core Competencies for
Emergency Medicine Residents Kevin G. Rodgers, MD, Craig Manifold, DO
3 Antecedents and consequences of reactions to developmental 360° feedback ☆
Leanne E. Atwater, , Joan F. Brett
to give constructive feed-back to someone if that person has had less exposure on getting feed-
back. It will be even harder if that person is not used to reflecting either. This encouraged me to
give constructive feed-back to my trainees as early as possible. Also encouraging them to seek
feed-back from other colleagues, patients etc. Also teaching them to reflect on their actions.
I feel significant event analysis are a very good way of reflecting and learning from our
mistakes.
Gibbs cycle can be used in many ways as a trainer. It can be used to explore any incident that
you would like to discuss and evaluate in a structured way. It gives the opportunity to speak up
your feelings helping to be self-aware. It gives the opportunity to discuss and evaluate among
group of people. It helps to make a judgement about what happened and consider what had
gone well, and what had gone not so well. Then analyse the situation in several parts, what
went well, what did you do well, what others did well, what went wrong, in what way did you
or others contributed to this. Then the synthesis stage where you would develop an insight into
every bodies behaviour. Detailed analysis and honest exploration will lead for you to realise
what could have done better bringing you to an action plan.
Perseverance:
At this time the revalidation process had started officially and we all realised the importance of
having comprehensive appraisals. Before revalidation, appraisals happened in the army
according to a military protocol and was usually a discussion with a military appraiser. I always
reiterated the importance of doing Patient Satisfaction questionnaires (PSQ) and 360
feedbacks. 360 feed-back is a multi- source feedback which includes colleague and self-
assessment questionnaires. It gives you valuable information about your performance that are
difficult to quantify. It gives you a good opportunity to reflect and change your behaviour for
the best.
“Feedback about professionalism is necessary to change practice and behaviour. This technique
focuses on multiple perspectives and levels of evaluation leading to results that are considered
to be highly credible and a powerful tool to change behaviour.” 2
Following study had looked at how leaders reacted to feed back.
“For leaders with low ratings, those who agreed with others about their ratings were less
motivated than those who received low ratings and over rated themselves. For leaders with high
ratings, agreement between self and other did not influence their motivation. Individuals with
more favorable attitudes toward using feedback were more motivated following feedback.”3
I feel these results are very interesting and useful.
2 360-degree Feedback: Possibilities for Assessment of the ACGME Core Competencies for
Emergency Medicine Residents Kevin G. Rodgers, MD, Craig Manifold, DO
3 Antecedents and consequences of reactions to developmental 360° feedback ☆
Leanne E. Atwater, , Joan F. Brett
I always encourage my trainees to involve in these quality improvement activities if they are
going to be in the same practice for a reasonable length of time. As this study has shown it is
interesting to know if you rated yourself high and others rated you lower than that, you are
more motivated to change in behaviour. It gives you some self awareness.
Even though I showed lot of interest in quality improvement activities in the practice and
encouraged other clinicians in many ways, unfortunately, the Senior Medical Officer was not
interested in going through the process for accreditation.
So I had to believe I will never be able to proceed any further in my career in this practice. So
with difficulty I decided to try and find a different practice, NHS practice as I have never had
experience in working in an NHS practice at this stage.
Subsequently I managed to join a local NHS practice.
Few months in to the post as a salaried GP in this practice, I reaslised that there was no hope to
become a trainer or becoming a partner in this practice.
So I continued to work in the NHS with no trainee.
“Grit - Defined as perseverance and passion for long-term goals. Grit did not relate positively to
IQ but was highly correlated with Big Five Conscientiousness. Grit nonetheless demonstrated
incremental predictive validity of success measures over and beyond IQ and conscientiousness.
Collectively, these findings suggest that the achievement of difficult goals entails not only talent
but also the sustained and focused application of talent over time.”4
This quote is about grit which defined as perseverance and passion for long term goals- which is
a noncognitive trait that predict success. In this study Grit demonstrated incremental predictive
validity of success measures over and beyond IQ and conscientiousness. Also findings suggested
that the achievement of difficult goals entails not only talent but also the sustained and focused
application of talent over time. This means that there is evidence that perseverance will help
you to achieve your long term goals.
I certainly had a passion to achieve the goal of becoming a trainer for a long period of time. I’d
been extremely determined to persevere with my journey but I couldn’t even find a training
practice to work so that I could continue with my training.
So I started to explore again and kept applying for GP partnership posts.
Eventually, I was successful twice.
One was a training practice, there were 2 trainers and they did have trainees.
So I felt so happy. Finally, I will get a chance to pursue with what I wanted.
So I left my salaried post and join this practice as a part time partner.
My extraordinary journey started from here.
Just before entering the partnership I realised that out of 2 trainers one has decided to take an
early retirement.
I felt still content as there was one trainer with a trainee and he was not nearing retirement.
I wanted to learn more about the business side of the partnership as I had no experience
before.
4 (PsycINFO Database Record (c) 2015 APA
going to be in the same practice for a reasonable length of time. As this study has shown it is
interesting to know if you rated yourself high and others rated you lower than that, you are
more motivated to change in behaviour. It gives you some self awareness.
Even though I showed lot of interest in quality improvement activities in the practice and
encouraged other clinicians in many ways, unfortunately, the Senior Medical Officer was not
interested in going through the process for accreditation.
So I had to believe I will never be able to proceed any further in my career in this practice. So
with difficulty I decided to try and find a different practice, NHS practice as I have never had
experience in working in an NHS practice at this stage.
Subsequently I managed to join a local NHS practice.
Few months in to the post as a salaried GP in this practice, I reaslised that there was no hope to
become a trainer or becoming a partner in this practice.
So I continued to work in the NHS with no trainee.
“Grit - Defined as perseverance and passion for long-term goals. Grit did not relate positively to
IQ but was highly correlated with Big Five Conscientiousness. Grit nonetheless demonstrated
incremental predictive validity of success measures over and beyond IQ and conscientiousness.
Collectively, these findings suggest that the achievement of difficult goals entails not only talent
but also the sustained and focused application of talent over time.”4
This quote is about grit which defined as perseverance and passion for long term goals- which is
a noncognitive trait that predict success. In this study Grit demonstrated incremental predictive
validity of success measures over and beyond IQ and conscientiousness. Also findings suggested
that the achievement of difficult goals entails not only talent but also the sustained and focused
application of talent over time. This means that there is evidence that perseverance will help
you to achieve your long term goals.
I certainly had a passion to achieve the goal of becoming a trainer for a long period of time. I’d
been extremely determined to persevere with my journey but I couldn’t even find a training
practice to work so that I could continue with my training.
So I started to explore again and kept applying for GP partnership posts.
Eventually, I was successful twice.
One was a training practice, there were 2 trainers and they did have trainees.
So I felt so happy. Finally, I will get a chance to pursue with what I wanted.
So I left my salaried post and join this practice as a part time partner.
My extraordinary journey started from here.
Just before entering the partnership I realised that out of 2 trainers one has decided to take an
early retirement.
I felt still content as there was one trainer with a trainee and he was not nearing retirement.
I wanted to learn more about the business side of the partnership as I had no experience
before.
4 (PsycINFO Database Record (c) 2015 APA
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
So I attended a modular course arranged by the RCGP – The Business of General practice.
Module 1 - was about understanding accounts, partnership liabilities and the profiles of high
and low earners. Developing an understanding about accounts. Following this session, I
understood about income per patient, then about GMS/PMS contracts. Dealing with cash flow
issues.
Understood PMS is a local contract unlike GMS which is a national contract. Discussed about
Merging, pros and cons.
Found the theme going for gold is an eye opener.
Signs of practice of low earners. – When partners have disputes, staffing inadequacy, badly
organized, not understanding what is important and what is urgent.
High earners – would think practice as a business. Importance of working closely with CCGs and
other local organizations.
Most important and interesting thing I learnt during this module is how the patients will judge
you. “Reality is what you Perceive”. 5 important areas to consider
1. Assurance
2. Tangibility
3. Responsiveness
4. Empathy
5. Reliability
Detailed discussion about legal obligations like partnership act 1890. Learning about relation
with outside agencies.
Importance of having a legal agreement about premises as well as a well written partnership
agreement.
(This is a section from my learning journal)
Through this module I could gain valuable knowledge about accounts, liabilities and going for
gold
Negotiation and decision making:
Module 2 was about decision making, GP federations and negotiating skills.
We had a really good work shop about decision making and using the model of 6 different
thinking hats. Thinking in different angles, firstly neutral and objective – concerned with facts
and figures, secondly emotional view, next cautious and careful thinking and looks for
weaknesses. Then being optimistic and looks for benefits, creativity and new ideas, lastly the
hat that controls the thinking and use of the other hats.
Then basic ways of using the hat, in a sequence or singly.
(This is from my learning journal)
As a GP partner or a trainer, decision making and negotiating are very important attributes. This
exercise did help me to think differently which will help in decision making. This is a good
exercise that I could experiment with my trainees.
As a GP we will have many decisions to make. Starting from your consultation up to the level of
management as a partner. Once you get used to think in different ways, like using the model of
6 different hats, it will not be a daunting experience.
Module 1 - was about understanding accounts, partnership liabilities and the profiles of high
and low earners. Developing an understanding about accounts. Following this session, I
understood about income per patient, then about GMS/PMS contracts. Dealing with cash flow
issues.
Understood PMS is a local contract unlike GMS which is a national contract. Discussed about
Merging, pros and cons.
Found the theme going for gold is an eye opener.
Signs of practice of low earners. – When partners have disputes, staffing inadequacy, badly
organized, not understanding what is important and what is urgent.
High earners – would think practice as a business. Importance of working closely with CCGs and
other local organizations.
Most important and interesting thing I learnt during this module is how the patients will judge
you. “Reality is what you Perceive”. 5 important areas to consider
1. Assurance
2. Tangibility
3. Responsiveness
4. Empathy
5. Reliability
Detailed discussion about legal obligations like partnership act 1890. Learning about relation
with outside agencies.
Importance of having a legal agreement about premises as well as a well written partnership
agreement.
(This is a section from my learning journal)
Through this module I could gain valuable knowledge about accounts, liabilities and going for
gold
Negotiation and decision making:
Module 2 was about decision making, GP federations and negotiating skills.
We had a really good work shop about decision making and using the model of 6 different
thinking hats. Thinking in different angles, firstly neutral and objective – concerned with facts
and figures, secondly emotional view, next cautious and careful thinking and looks for
weaknesses. Then being optimistic and looks for benefits, creativity and new ideas, lastly the
hat that controls the thinking and use of the other hats.
Then basic ways of using the hat, in a sequence or singly.
(This is from my learning journal)
As a GP partner or a trainer, decision making and negotiating are very important attributes. This
exercise did help me to think differently which will help in decision making. This is a good
exercise that I could experiment with my trainees.
As a GP we will have many decisions to make. Starting from your consultation up to the level of
management as a partner. Once you get used to think in different ways, like using the model of
6 different hats, it will not be a daunting experience.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
As a trainer I have to evaluate my trainees, understand them and help them to improve in their
career. Also I have a duty of care to my patients that their health is not compromised. It is also
my duty to identify poorly performing and unsafe trainees and take action to make sure that
the patients are not put at risk. That is why I believe decision making is imperative. So that I can
make an early decision about my trainee and then decide on a management plan as a trainer. If
the trainee is a high performing good trainee, I should have a challenging training plan and on
the other hand if the trainee is under performing then I should have a constructive supportive
training plan to help the trainee to improve. But also making sure that the trainee is safe to
practice.
Next important facet of learning during this session was negotiating skills. Negotiation deals
with conflict, depends upon a mutual motivation to reach agreement and involves trying for
agreement. This is one aspect that helped me immensely later when I had to deal with massive
problems in my partnership.
In my opinion, negotiation is a key aspect of communication in general practice and a must
have skill. Starting from your consultation, negotiating with your patients about managing their
illnesses, engaging them in their treatment plan then negotiating with other agencies to
arrange care for your patients. As you have to work with lot of other agencies, I feel this is a
must have skill and as a trainer I have to help my trainees to develop this.
Perseverance:
Twelve months in to this partnership, both other partners wanted to leave one after the other
due to personal reasons. So I was left to deal with everything in six months. This put me under
huge pressure. I couldn’t get my head around this. So I thought I should seek some help. First
thing came to my mind was asking some advice from a web based GP group –called Resilient
GP. I put a little notice on this group. There were overwhelming response. One GP who works
for a Local Medical Council (LMC) offered me to come and see her over a week end. So I went
to see her and she offered extremely good advice.
So basically, within six months, I had to either recruit and carry on, work together or merge
with another practice or think about handing in the contract.
Then I had to advertise to try and recruit. There were only 3 applicants. Only one of them
wanted a partnership other 2 just offered services as locum doctors.
I was exploring my opportunities, seeking help every possible way, discussing with local
authorities, local practices to find a way to carry on. I had meetings with LMC. Discussed about
what options I have.
I discussed with local GPs. They were happy to work together. But had their own problems to
prevent from merging. One practice offered us to engage in their training and teaching
programs. Like -wise I offered them to have joint tutorials.
Subsequently our FY2 trainee and me attended couple of their training sessions. It was
rewarding as we could meet other local GPs and also meet local consultants.
We are a training practice providing a good service. In the mean time we had trainees and we
were continuing with our training programme. Regular tutorials, case base discussions, Direct
observation tools, joint clinics etc.
career. Also I have a duty of care to my patients that their health is not compromised. It is also
my duty to identify poorly performing and unsafe trainees and take action to make sure that
the patients are not put at risk. That is why I believe decision making is imperative. So that I can
make an early decision about my trainee and then decide on a management plan as a trainer. If
the trainee is a high performing good trainee, I should have a challenging training plan and on
the other hand if the trainee is under performing then I should have a constructive supportive
training plan to help the trainee to improve. But also making sure that the trainee is safe to
practice.
Next important facet of learning during this session was negotiating skills. Negotiation deals
with conflict, depends upon a mutual motivation to reach agreement and involves trying for
agreement. This is one aspect that helped me immensely later when I had to deal with massive
problems in my partnership.
In my opinion, negotiation is a key aspect of communication in general practice and a must
have skill. Starting from your consultation, negotiating with your patients about managing their
illnesses, engaging them in their treatment plan then negotiating with other agencies to
arrange care for your patients. As you have to work with lot of other agencies, I feel this is a
must have skill and as a trainer I have to help my trainees to develop this.
Perseverance:
Twelve months in to this partnership, both other partners wanted to leave one after the other
due to personal reasons. So I was left to deal with everything in six months. This put me under
huge pressure. I couldn’t get my head around this. So I thought I should seek some help. First
thing came to my mind was asking some advice from a web based GP group –called Resilient
GP. I put a little notice on this group. There were overwhelming response. One GP who works
for a Local Medical Council (LMC) offered me to come and see her over a week end. So I went
to see her and she offered extremely good advice.
So basically, within six months, I had to either recruit and carry on, work together or merge
with another practice or think about handing in the contract.
Then I had to advertise to try and recruit. There were only 3 applicants. Only one of them
wanted a partnership other 2 just offered services as locum doctors.
I was exploring my opportunities, seeking help every possible way, discussing with local
authorities, local practices to find a way to carry on. I had meetings with LMC. Discussed about
what options I have.
I discussed with local GPs. They were happy to work together. But had their own problems to
prevent from merging. One practice offered us to engage in their training and teaching
programs. Like -wise I offered them to have joint tutorials.
Subsequently our FY2 trainee and me attended couple of their training sessions. It was
rewarding as we could meet other local GPs and also meet local consultants.
We are a training practice providing a good service. In the mean time we had trainees and we
were continuing with our training programme. Regular tutorials, case base discussions, Direct
observation tools, joint clinics etc.
Soon after we joined we had a denary visit for our senior partner. The Dean was happy to have
me in the practice as well and we had discussion about best way to complete my training and
having a trainee soon.
Unfortunately, few months later when my senior partner gave notice, I contacted the Dean. I
wanted to discuss the situation with her face to face, about rescuing the practice and
maintaining as a training practice. She was very understanding, subsequently we arranged a
meeting and discussed about best way to proceed. She will arrange a visit soon and I will be
prepared. I will have a video ready for them to view of a teaching session. Then I will be
allocated a FY2 trainee for the first year.
Reflection:
As planned I attended all the sessions of the new trainers course. I found this extremely useful.
The discussions we had were so important. They all had trainees and they had different levels
of performance. Some had extremely good trainees but interestingly one had a trainee who
was underperforming and what she thought was unsafe to practice. We learnt a lot from her
experience. I felt better to learn through someone’s real experience. As a trainer with the first
trainee it is very difficult to understand if you are doing the right thing. Last thing you want to
do is to put your trainee’s life in a difficult situation, at the same time you have to make sure
that you don’t put your patients at risk. We discussed about giving feedback.
I wrote in my learning log several times about giving feedback. This is what I liked most;
Good feedback should be PROMPTED.
P –Precise
R-Relevant
O-Outcome
M-Measurable
P-Possible
T-Time determined
E-Encouraging
D-Descriptive
(From my learning log)
This is easy to remember and I could use it for my trainees as well as for other staff, including
nurses, HCAs and Reception staff even.
We discussed how she should give this under- performing trainee a constructive feed-back. We
talked about better ways of giving negative feed-back. We talked about arranging educational
walks with trainees which I think is a very clever idea. Also while driving, going for a home visit
with your trainee and you could break bad news while not directly looking at your trainee.
I was the only one who didn’t have a trainee at the course. This made me feel sad at times as I
couldn’t always practice what we discuss. We had a trainee in the practice always but as I am
part time as well we didn’t have lot of time together to practice what I have learnt. But I
managed to have few tutorials and many case based discussions with our trainees. I managed
to keep in touch.
With our last trainee I did have some combined clinics. During these clinics I was able to assess
his communication skills, examination skills, coming up with an appropriate management plan,
negotiating with patients and also other agencies as needed and also making sure he is aware
me in the practice as well and we had discussion about best way to complete my training and
having a trainee soon.
Unfortunately, few months later when my senior partner gave notice, I contacted the Dean. I
wanted to discuss the situation with her face to face, about rescuing the practice and
maintaining as a training practice. She was very understanding, subsequently we arranged a
meeting and discussed about best way to proceed. She will arrange a visit soon and I will be
prepared. I will have a video ready for them to view of a teaching session. Then I will be
allocated a FY2 trainee for the first year.
Reflection:
As planned I attended all the sessions of the new trainers course. I found this extremely useful.
The discussions we had were so important. They all had trainees and they had different levels
of performance. Some had extremely good trainees but interestingly one had a trainee who
was underperforming and what she thought was unsafe to practice. We learnt a lot from her
experience. I felt better to learn through someone’s real experience. As a trainer with the first
trainee it is very difficult to understand if you are doing the right thing. Last thing you want to
do is to put your trainee’s life in a difficult situation, at the same time you have to make sure
that you don’t put your patients at risk. We discussed about giving feedback.
I wrote in my learning log several times about giving feedback. This is what I liked most;
Good feedback should be PROMPTED.
P –Precise
R-Relevant
O-Outcome
M-Measurable
P-Possible
T-Time determined
E-Encouraging
D-Descriptive
(From my learning log)
This is easy to remember and I could use it for my trainees as well as for other staff, including
nurses, HCAs and Reception staff even.
We discussed how she should give this under- performing trainee a constructive feed-back. We
talked about better ways of giving negative feed-back. We talked about arranging educational
walks with trainees which I think is a very clever idea. Also while driving, going for a home visit
with your trainee and you could break bad news while not directly looking at your trainee.
I was the only one who didn’t have a trainee at the course. This made me feel sad at times as I
couldn’t always practice what we discuss. We had a trainee in the practice always but as I am
part time as well we didn’t have lot of time together to practice what I have learnt. But I
managed to have few tutorials and many case based discussions with our trainees. I managed
to keep in touch.
With our last trainee I did have some combined clinics. During these clinics I was able to assess
his communication skills, examination skills, coming up with an appropriate management plan,
negotiating with patients and also other agencies as needed and also making sure he is aware
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
of local and national guidelines. I felt this trainee was very thorough. He was very good at
following his patients. He will keep a record and even did phone them time to time to find out
their progression. He will always seek advice if there are any doubts. I can remember once he
had this elderly patient who came with shortness of breath, and then he found out he had a
slow heart rate. This was at the very end of the day but he didn’t hesitate to do an ECG by
himself and found out that the patient had a heart block. So he arranged his transfer to the
hospital and waited with the patient until the ambulance arrived. We discussed this as a case
based discussion. We discussed about what went well, what didn’t go so well and what would
have done differently next time. He was very happy with all the support he received from the
practice team. The ambulance took a while to arrive as he ordered one within the hour rather
than blue light. So we discussed about pros and cons of this as well.
We also had few tutorials together, I found it very productive when he came prepared and we
had an interactive session. Tutorial we did about HRT and Menopause was very interesting and
productive. Our nurse practitioner also participated in this tutorial. At the beginning when I
asked him if he had any patients with these issues he came up with a very good example, at the
end we managed to use her for learning most aspects of HRT and menopause. Trainer
experience is a key element during tutorials.
About the good tutorials:
Before: Preparation – what, how, when, where and why
During: Roleplay /Video /RCA – random case analysis/Relevant/Interesting. Joint surgeries,
observing, consulting feed-back.
After: Having a diary to log, plan next tutorial, write 1-2 own learning needs.
(This is from my learning journal)
End of each day, we went through all of his consultations together. Then I noticed that he tends
to say “no further concerns” at the end of the consultation rather than safety netting. Then he
explained to me that it means he had gone through all the concerns of the patient on that day.
Then we discussed about the importance of safety netting and asking the patient to call back if
any further concerns.
Perseverance and negotiation:
During recruitment of new partners, I managed to recruit 2 new part time partners. Towards
the end one decided not to join.
My plans were destroyed again. But I wanted to survive and reach my goal. Making my practice
survive and continue as a training practice.
I found another group of GPs nearer to my practice interested in working together.
I had numerous meetings with them discussing options.But unfortunately, their final decision
was not favourable for us. They decided not to proceed due to logistic issues.
Another big blow to my effort. I felt very sad and lost. Do I give up? I joined this practice
thinking it will help me to finish my GP training and complete my assignment with some advice
and guidance from existing trainers, but now I have to build up the practice and maintain a high
standard first of all before even thinking about finishing my training.
With great effort and support from my family and friends I decided to carry on.
following his patients. He will keep a record and even did phone them time to time to find out
their progression. He will always seek advice if there are any doubts. I can remember once he
had this elderly patient who came with shortness of breath, and then he found out he had a
slow heart rate. This was at the very end of the day but he didn’t hesitate to do an ECG by
himself and found out that the patient had a heart block. So he arranged his transfer to the
hospital and waited with the patient until the ambulance arrived. We discussed this as a case
based discussion. We discussed about what went well, what didn’t go so well and what would
have done differently next time. He was very happy with all the support he received from the
practice team. The ambulance took a while to arrive as he ordered one within the hour rather
than blue light. So we discussed about pros and cons of this as well.
We also had few tutorials together, I found it very productive when he came prepared and we
had an interactive session. Tutorial we did about HRT and Menopause was very interesting and
productive. Our nurse practitioner also participated in this tutorial. At the beginning when I
asked him if he had any patients with these issues he came up with a very good example, at the
end we managed to use her for learning most aspects of HRT and menopause. Trainer
experience is a key element during tutorials.
About the good tutorials:
Before: Preparation – what, how, when, where and why
During: Roleplay /Video /RCA – random case analysis/Relevant/Interesting. Joint surgeries,
observing, consulting feed-back.
After: Having a diary to log, plan next tutorial, write 1-2 own learning needs.
(This is from my learning journal)
End of each day, we went through all of his consultations together. Then I noticed that he tends
to say “no further concerns” at the end of the consultation rather than safety netting. Then he
explained to me that it means he had gone through all the concerns of the patient on that day.
Then we discussed about the importance of safety netting and asking the patient to call back if
any further concerns.
Perseverance and negotiation:
During recruitment of new partners, I managed to recruit 2 new part time partners. Towards
the end one decided not to join.
My plans were destroyed again. But I wanted to survive and reach my goal. Making my practice
survive and continue as a training practice.
I found another group of GPs nearer to my practice interested in working together.
I had numerous meetings with them discussing options.But unfortunately, their final decision
was not favourable for us. They decided not to proceed due to logistic issues.
Another big blow to my effort. I felt very sad and lost. Do I give up? I joined this practice
thinking it will help me to finish my GP training and complete my assignment with some advice
and guidance from existing trainers, but now I have to build up the practice and maintain a high
standard first of all before even thinking about finishing my training.
With great effort and support from my family and friends I decided to carry on.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5People who achieve success have done so through hard work, diligence, dreaming and
persevering through all obstacles that have come their way. Individuals who fail and then never
try anything difficult again, will not be sitting at the top of the ladder of success. That top seat is
reserved for the people who see the value in, and know how to persevere.
Word count 4772-425 = 4347
5 5 Facts That Prove Perseverance Can Get You Far in Your Career
by Joanne Troppello
persevering through all obstacles that have come their way. Individuals who fail and then never
try anything difficult again, will not be sitting at the top of the ladder of success. That top seat is
reserved for the people who see the value in, and know how to persevere.
Word count 4772-425 = 4347
5 5 Facts That Prove Perseverance Can Get You Far in Your Career
by Joanne Troppello
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





