Chronic Illness Management - Strategies, Treatment, and Complications
VerifiedAdded on 2023/06/10
|9
|1779
|330
AI Summary
This teaching session covers chronic illness management, including strategies for slowing disease progression, treatment options, and complications. It focuses on chronic kidney disease, discussing the different stages and the dietary restrictions required. The session also covers the complications that require immediate attention and the importance of early diagnosis and treatment. The teaching sources used include studies on fragmented care, whole-person illness, and the development of primary care-based interventions for patients with multimorbidity.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: CHRONIC ILLNESS
Chronic Illness Management
Name of Student
Name of Institution
1
Chronic Illness Management
Name of Student
Name of Institution
1
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
CHRONIC ILLNESS
Chronic Illness Management
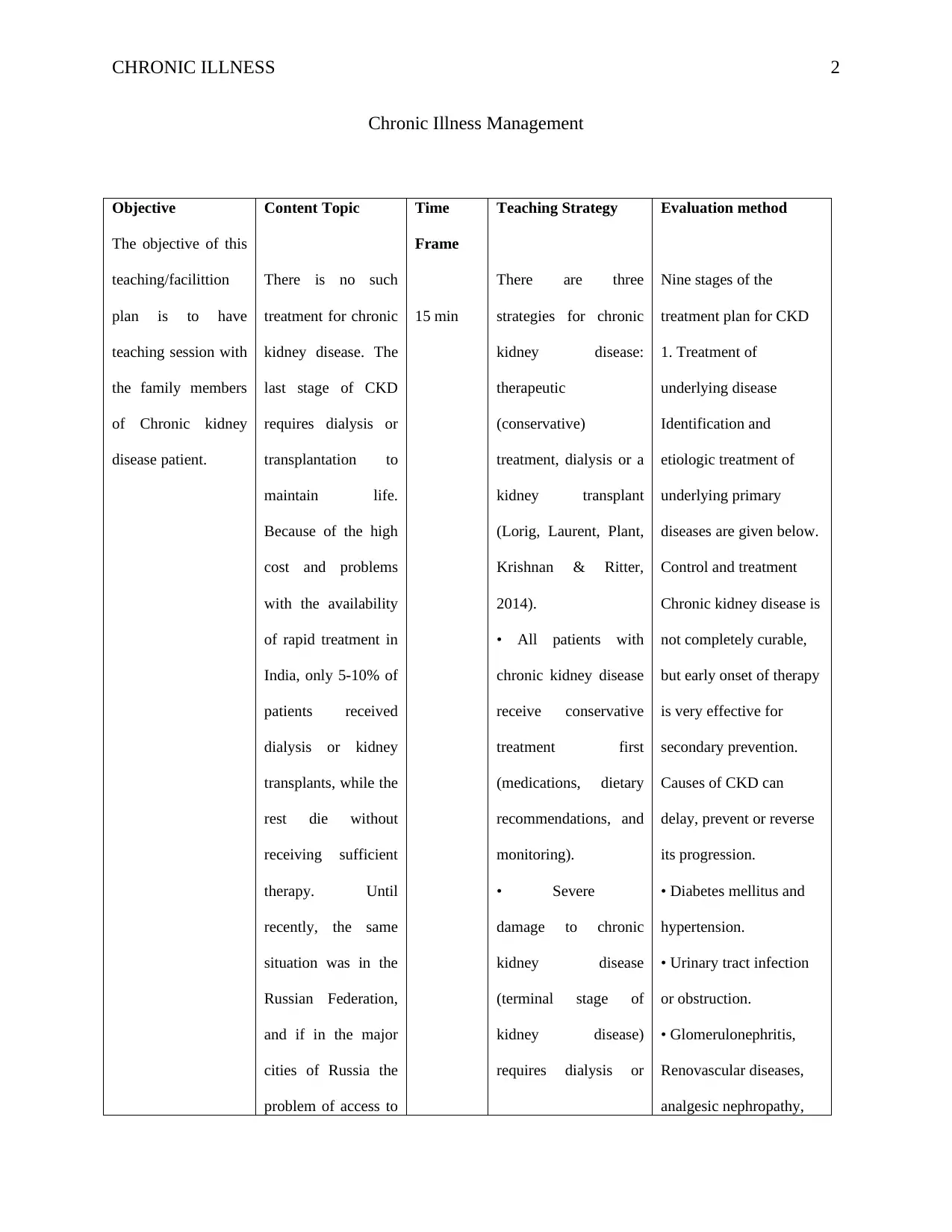
Objective
The objective of this
teaching/facilittion
plan is to have
teaching session with
the family members
of Chronic kidney
disease patient.
Content Topic
There is no such
treatment for chronic
kidney disease. The
last stage of CKD
requires dialysis or
transplantation to
maintain life.
Because of the high
cost and problems
with the availability
of rapid treatment in
India, only 5-10% of
patients received
dialysis or kidney
transplants, while the
rest die without
receiving sufficient
therapy. Until
recently, the same
situation was in the
Russian Federation,
and if in the major
cities of Russia the
problem of access to
Time
Frame
15 min
Teaching Strategy
There are three
strategies for chronic
kidney disease:
therapeutic
(conservative)
treatment, dialysis or a
kidney transplant
(Lorig, Laurent, Plant,
Krishnan & Ritter,
2014).
• All patients with
chronic kidney disease
receive conservative
treatment first
(medications, dietary
recommendations, and
monitoring).
• Severe
damage to chronic
kidney disease
(terminal stage of
kidney disease)
requires dialysis or
Evaluation method
Nine stages of the
treatment plan for CKD
1. Treatment of
underlying disease
Identification and
etiologic treatment of
underlying primary
diseases are given below.
Control and treatment
Chronic kidney disease is
not completely curable,
but early onset of therapy
is very effective for
secondary prevention.
Causes of CKD can
delay, prevent or reverse
its progression.
• Diabetes mellitus and
hypertension.
• Urinary tract infection
or obstruction.
• Glomerulonephritis,
Renovascular diseases,
analgesic nephropathy,
2
Chronic Illness Management
Objective
The objective of this
teaching/facilittion
plan is to have
teaching session with
the family members
of Chronic kidney
disease patient.
Content Topic
There is no such
treatment for chronic
kidney disease. The
last stage of CKD
requires dialysis or
transplantation to
maintain life.
Because of the high
cost and problems
with the availability
of rapid treatment in
India, only 5-10% of
patients received
dialysis or kidney
transplants, while the
rest die without
receiving sufficient
therapy. Until
recently, the same
situation was in the
Russian Federation,
and if in the major
cities of Russia the
problem of access to
Time
Frame
15 min
Teaching Strategy
There are three
strategies for chronic
kidney disease:
therapeutic
(conservative)
treatment, dialysis or a
kidney transplant
(Lorig, Laurent, Plant,
Krishnan & Ritter,
2014).
• All patients with
chronic kidney disease
receive conservative
treatment first
(medications, dietary
recommendations, and
monitoring).
• Severe
damage to chronic
kidney disease
(terminal stage of
kidney disease)
requires dialysis or
Evaluation method
Nine stages of the
treatment plan for CKD
1. Treatment of
underlying disease
Identification and
etiologic treatment of
underlying primary
diseases are given below.
Control and treatment
Chronic kidney disease is
not completely curable,
but early onset of therapy
is very effective for
secondary prevention.
Causes of CKD can
delay, prevent or reverse
its progression.
• Diabetes mellitus and
hypertension.
• Urinary tract infection
or obstruction.
• Glomerulonephritis,
Renovascular diseases,
analgesic nephropathy,
2
CHRONIC ILLNESS
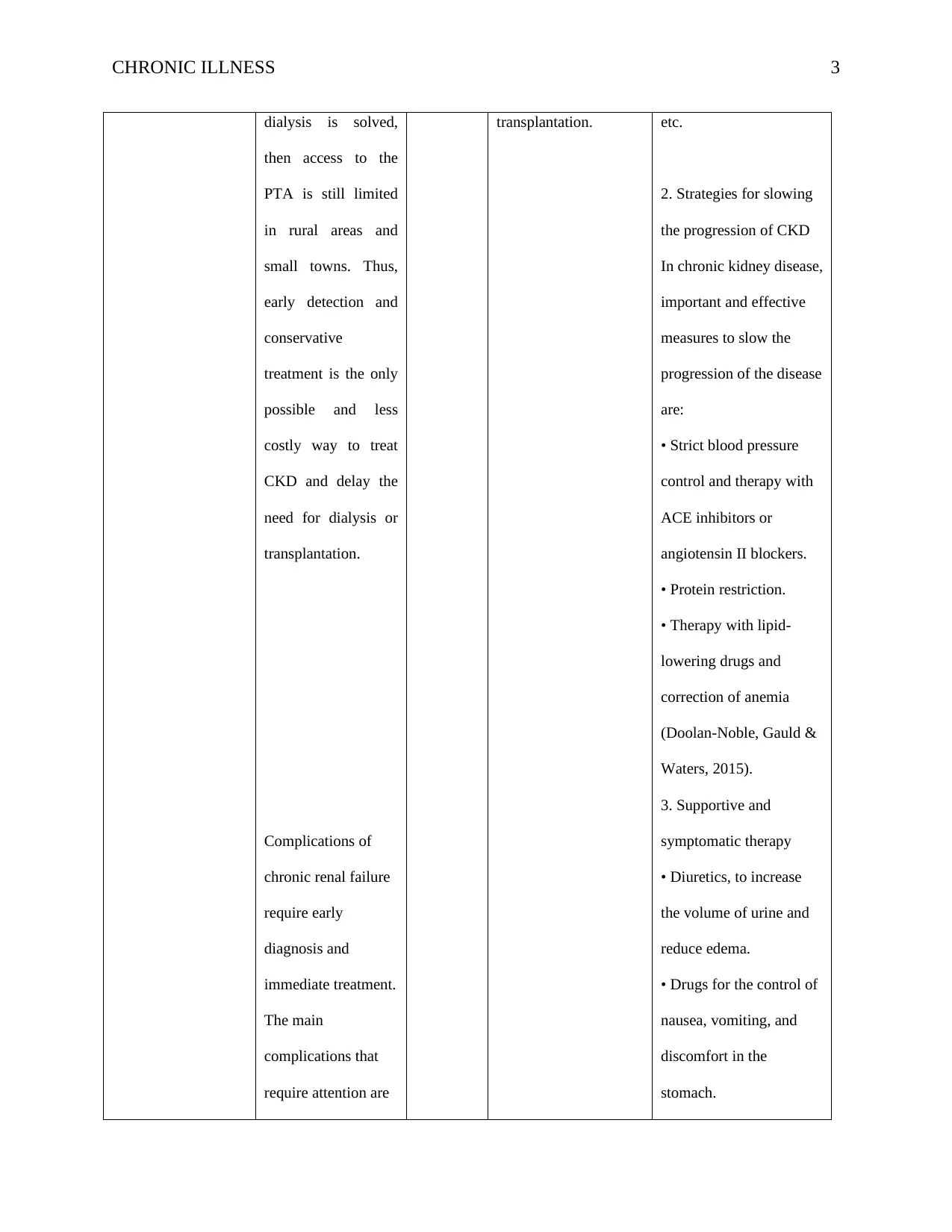
dialysis is solved,
then access to the
PTA is still limited
in rural areas and
small towns. Thus,
early detection and
conservative
treatment is the only
possible and less
costly way to treat
CKD and delay the
need for dialysis or
transplantation.
Complications of
chronic renal failure
require early
diagnosis and
immediate treatment.
The main
complications that
require attention are
transplantation. etc.
2. Strategies for slowing
the progression of CKD
In chronic kidney disease,
important and effective
measures to slow the
progression of the disease
are:
• Strict blood pressure
control and therapy with
ACE inhibitors or
angiotensin II blockers.
• Protein restriction.
• Therapy with lipid-
lowering drugs and
correction of anemia
(Doolan-Noble, Gauld &
Waters, 2015).
3. Supportive and
symptomatic therapy
• Diuretics, to increase
the volume of urine and
reduce edema.
• Drugs for the control of
nausea, vomiting, and
discomfort in the
stomach.
3
dialysis is solved,
then access to the
PTA is still limited
in rural areas and
small towns. Thus,
early detection and
conservative
treatment is the only
possible and less
costly way to treat
CKD and delay the
need for dialysis or
transplantation.
Complications of
chronic renal failure
require early
diagnosis and
immediate treatment.
The main
complications that
require attention are
transplantation. etc.
2. Strategies for slowing
the progression of CKD
In chronic kidney disease,
important and effective
measures to slow the
progression of the disease
are:
• Strict blood pressure
control and therapy with
ACE inhibitors or
angiotensin II blockers.
• Protein restriction.
• Therapy with lipid-
lowering drugs and
correction of anemia
(Doolan-Noble, Gauld &
Waters, 2015).
3. Supportive and
symptomatic therapy
• Diuretics, to increase
the volume of urine and
reduce edema.
• Drugs for the control of
nausea, vomiting, and
discomfort in the
stomach.
3
CHRONIC ILLNESS
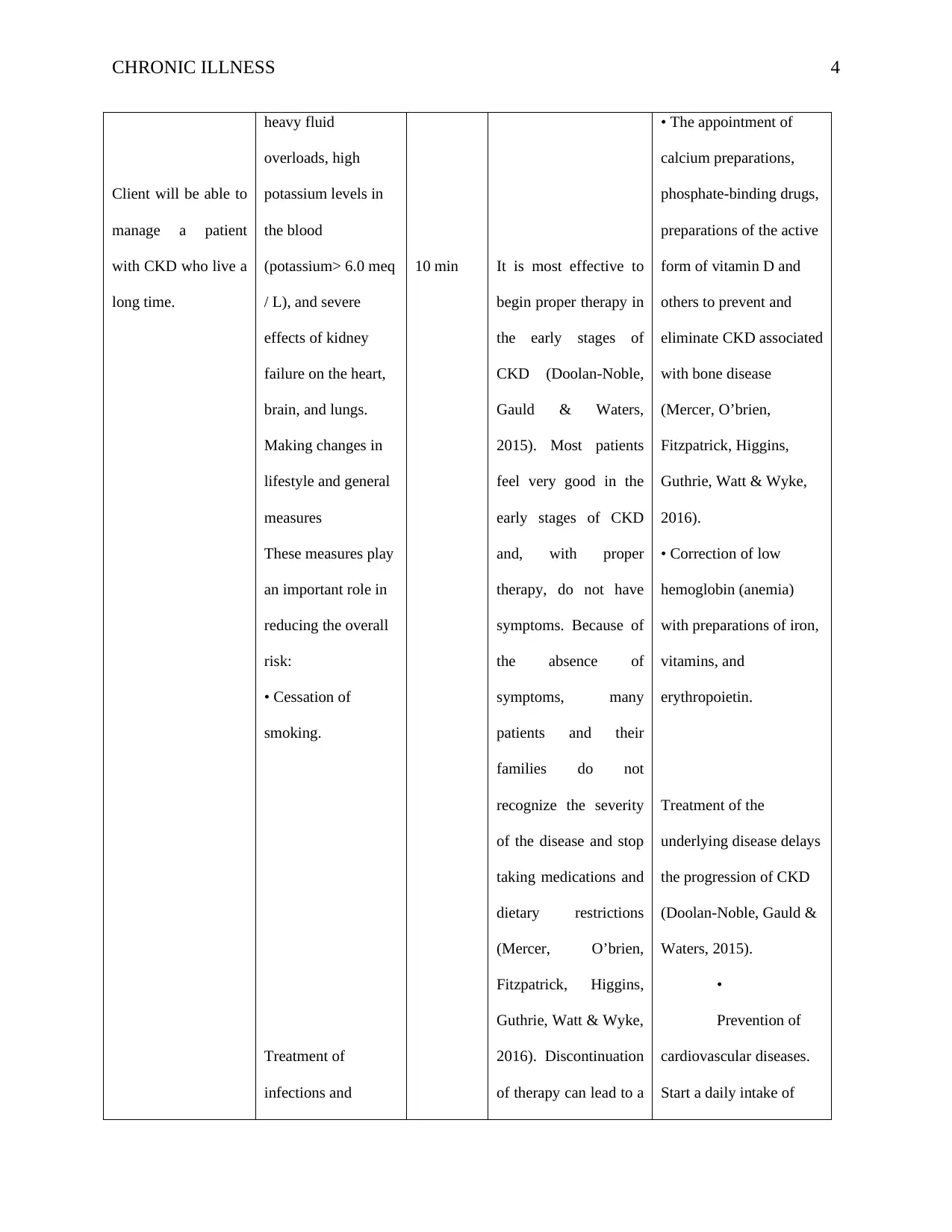
Client will be able to
manage a patient
with CKD who live a
long time.
heavy fluid
overloads, high
potassium levels in
the blood
(potassium> 6.0 meq
/ L), and severe
effects of kidney
failure on the heart,
brain, and lungs.
Making changes in
lifestyle and general
measures
These measures play
an important role in
reducing the overall
risk:
• Cessation of
smoking.
Treatment of
infections and
10 min It is most effective to
begin proper therapy in
the early stages of
CKD (Doolan-Noble,
Gauld & Waters,
2015). Most patients
feel very good in the
early stages of CKD
and, with proper
therapy, do not have
symptoms. Because of
the absence of
symptoms, many
patients and their
families do not
recognize the severity
of the disease and stop
taking medications and
dietary restrictions
(Mercer, O’brien,
Fitzpatrick, Higgins,
Guthrie, Watt & Wyke,
2016). Discontinuation
of therapy can lead to a
• The appointment of
calcium preparations,
phosphate-binding drugs,
preparations of the active
form of vitamin D and
others to prevent and
eliminate CKD associated
with bone disease
(Mercer, O’brien,
Fitzpatrick, Higgins,
Guthrie, Watt & Wyke,
2016).
• Correction of low
hemoglobin (anemia)
with preparations of iron,
vitamins, and
erythropoietin.
Treatment of the
underlying disease delays
the progression of CKD
(Doolan-Noble, Gauld &
Waters, 2015).
•
Prevention of
cardiovascular diseases.
Start a daily intake of
4
Client will be able to
manage a patient
with CKD who live a
long time.
heavy fluid
overloads, high
potassium levels in
the blood
(potassium> 6.0 meq
/ L), and severe
effects of kidney
failure on the heart,
brain, and lungs.
Making changes in
lifestyle and general
measures
These measures play
an important role in
reducing the overall
risk:
• Cessation of
smoking.
Treatment of
infections and
10 min It is most effective to
begin proper therapy in
the early stages of
CKD (Doolan-Noble,
Gauld & Waters,
2015). Most patients
feel very good in the
early stages of CKD
and, with proper
therapy, do not have
symptoms. Because of
the absence of
symptoms, many
patients and their
families do not
recognize the severity
of the disease and stop
taking medications and
dietary restrictions
(Mercer, O’brien,
Fitzpatrick, Higgins,
Guthrie, Watt & Wyke,
2016). Discontinuation
of therapy can lead to a
• The appointment of
calcium preparations,
phosphate-binding drugs,
preparations of the active
form of vitamin D and
others to prevent and
eliminate CKD associated
with bone disease
(Mercer, O’brien,
Fitzpatrick, Higgins,
Guthrie, Watt & Wyke,
2016).
• Correction of low
hemoglobin (anemia)
with preparations of iron,
vitamins, and
erythropoietin.
Treatment of the
underlying disease delays
the progression of CKD
(Doolan-Noble, Gauld &
Waters, 2015).
•
Prevention of
cardiovascular diseases.
Start a daily intake of
4
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
CHRONIC ILLNESS
Client will be able to
change lifestyle and
important measures
to reduce risk of
CKD patient.
depletion of the
volume is very
useful in chronic
kidney disease.
• Maintain a
healthy weight,
regular exercise and
physical activity on a
regular basis.
• Restriction of
alcohol consumption.
• Compliance with
the principle of
healthy eating and
reducing salt intake.
• Reception
of prescribed
medications.
Adjusting the dose of
the drug taking into
account the severity
of renal failure.
• Continuous
adherence to
treatment by the
directions of the
nephrologist.
30 min
rapid deterioration in
kidney damage and in
a short time such
patients may need such
expensive treatment as
dialysis or a kidney
transplant (Allen et al.,
2015).
Chronic kidney disease
is a progressive
condition that can not
be cured. The goals of
conservative therapy
are:
1. The slowdown of
disease progression.
2. Treatment of
the causes that led to
the disease and
provoking factors.
3. Relieving
symptoms and treating
aspirin if it is prescribed
by a doctor.
4. Control over
reversible states
It is necessary to search
for and treat reversible
conditions, which can
aggravate the degree of
renal failure (McKinlay,
McBain & Gray, 2009).
5
Client will be able to
change lifestyle and
important measures
to reduce risk of
CKD patient.
depletion of the
volume is very
useful in chronic
kidney disease.
• Maintain a
healthy weight,
regular exercise and
physical activity on a
regular basis.
• Restriction of
alcohol consumption.
• Compliance with
the principle of
healthy eating and
reducing salt intake.
• Reception
of prescribed
medications.
Adjusting the dose of
the drug taking into
account the severity
of renal failure.
• Continuous
adherence to
treatment by the
directions of the
nephrologist.
30 min
rapid deterioration in
kidney damage and in
a short time such
patients may need such
expensive treatment as
dialysis or a kidney
transplant (Allen et al.,
2015).
Chronic kidney disease
is a progressive
condition that can not
be cured. The goals of
conservative therapy
are:
1. The slowdown of
disease progression.
2. Treatment of
the causes that led to
the disease and
provoking factors.
3. Relieving
symptoms and treating
aspirin if it is prescribed
by a doctor.
4. Control over
reversible states
It is necessary to search
for and treat reversible
conditions, which can
aggravate the degree of
renal failure (McKinlay,
McBain & Gray, 2009).
5
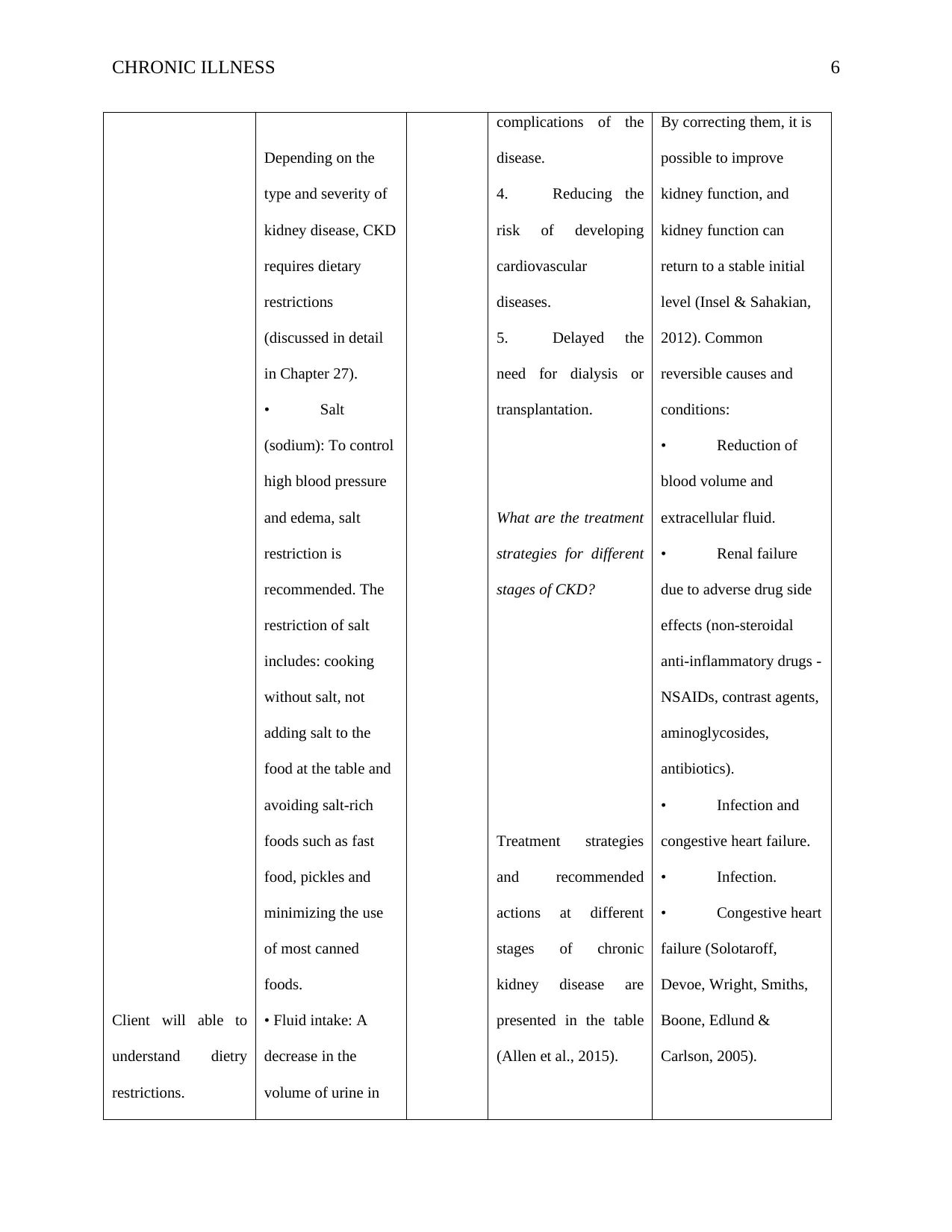
CHRONIC ILLNESS
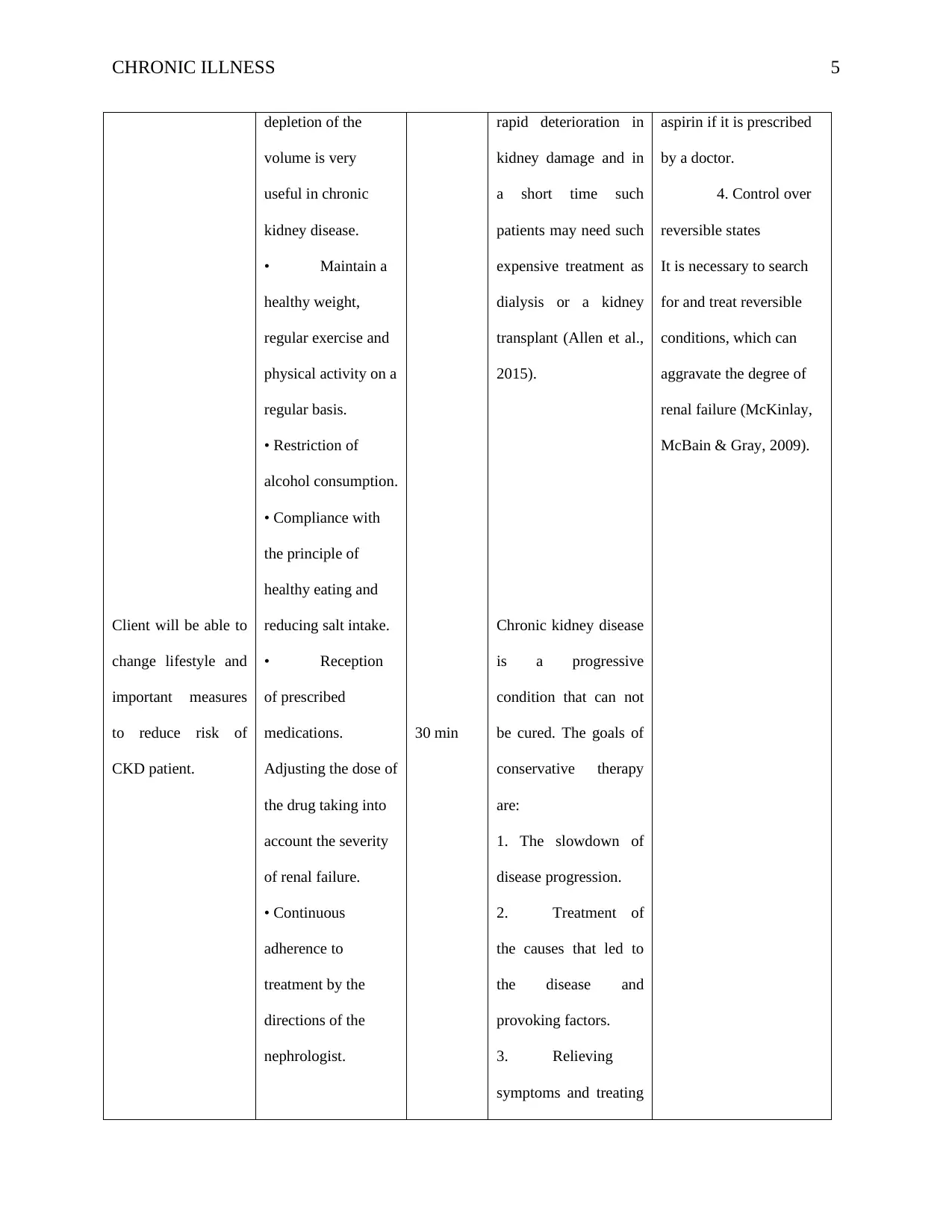
Client will able to
understand dietry
restrictions.
Depending on the
type and severity of
kidney disease, CKD
requires dietary
restrictions
(discussed in detail
in Chapter 27).
• Salt
(sodium): To control
high blood pressure
and edema, salt
restriction is
recommended. The
restriction of salt
includes: cooking
without salt, not
adding salt to the
food at the table and
avoiding salt-rich
foods such as fast
food, pickles and
minimizing the use
of most canned
foods.
• Fluid intake: A
decrease in the
volume of urine in
complications of the
disease.
4. Reducing the
risk of developing
cardiovascular
diseases.
5. Delayed the
need for dialysis or
transplantation.
What are the treatment
strategies for different
stages of CKD?
Treatment strategies
and recommended
actions at different
stages of chronic
kidney disease are
presented in the table
(Allen et al., 2015).
By correcting them, it is
possible to improve
kidney function, and
kidney function can
return to a stable initial
level (Insel & Sahakian,
2012). Common
reversible causes and
conditions:
• Reduction of
blood volume and
extracellular fluid.
• Renal failure
due to adverse drug side
effects (non-steroidal
anti-inflammatory drugs -
NSAIDs, contrast agents,
aminoglycosides,
antibiotics).
• Infection and
congestive heart failure.
• Infection.
• Congestive heart
failure (Solotaroff,
Devoe, Wright, Smiths,
Boone, Edlund &
Carlson, 2005).
6
Client will able to
understand dietry
restrictions.
Depending on the
type and severity of
kidney disease, CKD
requires dietary
restrictions
(discussed in detail
in Chapter 27).
• Salt
(sodium): To control
high blood pressure
and edema, salt
restriction is
recommended. The
restriction of salt
includes: cooking
without salt, not
adding salt to the
food at the table and
avoiding salt-rich
foods such as fast
food, pickles and
minimizing the use
of most canned
foods.
• Fluid intake: A
decrease in the
volume of urine in
complications of the
disease.
4. Reducing the
risk of developing
cardiovascular
diseases.
5. Delayed the
need for dialysis or
transplantation.
What are the treatment
strategies for different
stages of CKD?
Treatment strategies
and recommended
actions at different
stages of chronic
kidney disease are
presented in the table
(Allen et al., 2015).
By correcting them, it is
possible to improve
kidney function, and
kidney function can
return to a stable initial
level (Insel & Sahakian,
2012). Common
reversible causes and
conditions:
• Reduction of
blood volume and
extracellular fluid.
• Renal failure
due to adverse drug side
effects (non-steroidal
anti-inflammatory drugs -
NSAIDs, contrast agents,
aminoglycosides,
antibiotics).
• Infection and
congestive heart failure.
• Infection.
• Congestive heart
failure (Solotaroff,
Devoe, Wright, Smiths,
Boone, Edlund &
Carlson, 2005).
6
CHRONIC ILLNESS
patients with CKD
can cause swelling
and in severe cases
even shortness of
breath. Thus, fluid
restriction is
recommended for all
patients with CKD
with edema. •
Potassium: A high
level of potassium is
a common problem
in patients with
CKD. In turn, it can
have a serious
impact on the
function of the heart.
To prevent this limit
the consumption of
food
30
7
patients with CKD
can cause swelling
and in severe cases
even shortness of
breath. Thus, fluid
restriction is
recommended for all
patients with CKD
with edema. •
Potassium: A high
level of potassium is
a common problem
in patients with
CKD. In turn, it can
have a serious
impact on the
function of the heart.
To prevent this limit
the consumption of
food
30
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CHRONIC ILLNESS
References
FOLLOWING SOURCES ARE USED AS TEACHING SOURCES:
Allen, D., Badro, V., Denyer-Willis, L., Ellen Macdonald, M., Paré, A., Hutchinson, T., …
Cohen, S. R. (2015). Fragmented care and whole-person illness: Decision-making for
people with chronic end-stage kidney disease. Chronic Illness, 11(1), 44–55.
https://doi.org/10.1177/1742395314562974
Doolan-Noble, F., Gauld, R., & Waters, D. L. (2015). Are nurses more likely to report providing
care plans for chronic disease patients than doctors? Findings from a New Zealand study.
Chronic Illness, 11(3), 210–217. https://doi.org/10.1177/1742395314567479
Lorig, K., Laurent, D. D., Plant, K., Krishnan, E., & Ritter, P. L. (2014). The components of
action planning and their associations with behavior and health outcomes. Chronic
Illness, 10(1), 50–59. https://doi.org/10.1177/1742395313495572
Mercer, S. W., O'brien, R., Fitzpatrick, B., Higgins, M., Guthrie, B., Watt, G., & Wyke, S.
(2016). The development and optimization of a primary care-based whole system
complex intervention (CARE Plus) for patients with multimorbidity living in areas of
high socioeconomic deprivation. Chronic Illness, 12(3), 165–181.
https://doi.org/10.1177/1742395316644304
FOLLOWING SOURCES USED IN OTHER SECTIONS:
Insel, T. R., & Sahakian, B. J. (2012). A plan for mental illness. Nature.
https://doi.org/10.1038/483269a
McKinlay, E., McBain, L., & Gray, B. (2009). Teaching and learning about chronic conditions
management for undergraduate medical students: Utilizing the patient-as-teacher
approach. Chronic Illness, 5(3), 209–218. https://doi.org/10.1177/1742395309343812
8
References
FOLLOWING SOURCES ARE USED AS TEACHING SOURCES:
Allen, D., Badro, V., Denyer-Willis, L., Ellen Macdonald, M., Paré, A., Hutchinson, T., …
Cohen, S. R. (2015). Fragmented care and whole-person illness: Decision-making for
people with chronic end-stage kidney disease. Chronic Illness, 11(1), 44–55.
https://doi.org/10.1177/1742395314562974
Doolan-Noble, F., Gauld, R., & Waters, D. L. (2015). Are nurses more likely to report providing
care plans for chronic disease patients than doctors? Findings from a New Zealand study.
Chronic Illness, 11(3), 210–217. https://doi.org/10.1177/1742395314567479
Lorig, K., Laurent, D. D., Plant, K., Krishnan, E., & Ritter, P. L. (2014). The components of
action planning and their associations with behavior and health outcomes. Chronic
Illness, 10(1), 50–59. https://doi.org/10.1177/1742395313495572
Mercer, S. W., O'brien, R., Fitzpatrick, B., Higgins, M., Guthrie, B., Watt, G., & Wyke, S.
(2016). The development and optimization of a primary care-based whole system
complex intervention (CARE Plus) for patients with multimorbidity living in areas of
high socioeconomic deprivation. Chronic Illness, 12(3), 165–181.
https://doi.org/10.1177/1742395316644304
FOLLOWING SOURCES USED IN OTHER SECTIONS:
Insel, T. R., & Sahakian, B. J. (2012). A plan for mental illness. Nature.
https://doi.org/10.1038/483269a
McKinlay, E., McBain, L., & Gray, B. (2009). Teaching and learning about chronic conditions
management for undergraduate medical students: Utilizing the patient-as-teacher
approach. Chronic Illness, 5(3), 209–218. https://doi.org/10.1177/1742395309343812
8
CHRONIC ILLNESS
Solotaroff, R., Devoe, J., Wright, B. J., Smith, J., Boone, J., Edlund, T., & Carlson, M. J. (2005).
Medicaid programme changes and the chronically ill: Early results from a prospective
cohort study of the Oregon Health Plan. Chronic Illness, 1(3), 191–205.
https://doi.org/10.1177/17423953050010030301
Solotaroff, R., Devoe, J., Wright, B. J., Smiths, J., Boone, J., Edlund, T., & Carlson, M. J.
(2005). Medicaid programme changes and the chronically ill: early results from a
prospective cohort study of the Oregon Health Plan. Chronic Illness, 1(3), 191–205.
9
Solotaroff, R., Devoe, J., Wright, B. J., Smith, J., Boone, J., Edlund, T., & Carlson, M. J. (2005).
Medicaid programme changes and the chronically ill: Early results from a prospective
cohort study of the Oregon Health Plan. Chronic Illness, 1(3), 191–205.
https://doi.org/10.1177/17423953050010030301
Solotaroff, R., Devoe, J., Wright, B. J., Smiths, J., Boone, J., Edlund, T., & Carlson, M. J.
(2005). Medicaid programme changes and the chronically ill: early results from a
prospective cohort study of the Oregon Health Plan. Chronic Illness, 1(3), 191–205.
9
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





