Research Project: Telemedicine's Impact in Hougang, Singapore
VerifiedAdded on 2023/01/11
|38
|8235
|34
Report
AI Summary
This research project investigates the role of telemedicine in healthcare delivery within the Hougang area of Singapore. The study explores the awareness, reliability, and satisfaction levels of residents regarding telemedicine services. The research methodology includes a cross-sectional survey with a random sampling approach, collecting data through questionnaires. Key findings reveal that a majority of respondents are aware of telemedicine systems and report high reliability and satisfaction levels. The report delves into the benefits and disadvantages of telemedicine, providing a comprehensive analysis based on the collected data. The conclusion emphasizes the potential of telemedicine to enhance healthcare access and quality, especially in the context of promoting universal healthcare. Recommendations are provided to further improve and implement telemedicine services effectively in the Hougang area.

EXPLORING THE ROLE OF TELEMEDICINE IN HEALTH CARE DELIVERY IN
HOUGANG AREA, SINGAPORE
©April, 2019
HOUGANG AREA, SINGAPORE
©April, 2019
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
DECLARATION
I declare that research project is my original has been done to the best of my ability and
knowledge and it is my original work. It has never been submitted by any other person.
Signature...................................................... Date:..........................................................
The Supervisor Approval
This project has been submitted for examination with my approval as University Supervisor.
……………………………………………. ……………………………..
Signature Date
ii
I declare that research project is my original has been done to the best of my ability and
knowledge and it is my original work. It has never been submitted by any other person.
Signature...................................................... Date:..........................................................
The Supervisor Approval
This project has been submitted for examination with my approval as University Supervisor.
……………………………………………. ……………………………..
Signature Date
ii
TABLE OF CONTENTS
DECLARATION.......................................................................................................................................ii
TABLE OF CONTENTS.........................................................................................................................iii
LIST OF TABLES.....................................................................................................................................v
LIST OF FIGURES..................................................................................................................................vi
Figure 1: Conceptual framework……………………………………………………………...….5........vi
ABBREVIATIONS..................................................................................................................................vii
ABSTRACT............................................................................................................................................viii
SECTION 1................................................................................................................................................9
1.0 INTRODUCTION...............................................................................................................................9
1.1 Information Background....................................................................................................................9
1.2 Statement of the problem.................................................................................................................2
1.3 Study Objectives................................................................................................................................3
1.3.1 General objective........................................................................................................................3
1.3.2 Specific objectives.......................................................................................................................3
1.4 Research Questions...........................................................................................................................3
1.5 Hypothesis.........................................................................................................................................4
1.6 Conceptual Framework......................................................................................................................4
SECTION 2................................................................................................................................................5
2.0 LITERATURE REVIEW...................................................................................................................5
2.1. Theoretical Framework.....................................................................................................................5
2.1.1 Anderson’s Health Behaviour Model..........................................................................................5
2.2 Definition of Telemedicine.................................................................................................................6
2.3 History of Telemedicine.....................................................................................................................6
2.4 Health Information Technology and Telemedicine............................................................................7
2.5 Benefits of Telemedicine...................................................................................................................8
2.6. Disadvantages of Telemedicine......................................................................................................11
iii
DECLARATION.......................................................................................................................................ii
TABLE OF CONTENTS.........................................................................................................................iii
LIST OF TABLES.....................................................................................................................................v
LIST OF FIGURES..................................................................................................................................vi
Figure 1: Conceptual framework……………………………………………………………...….5........vi
ABBREVIATIONS..................................................................................................................................vii
ABSTRACT............................................................................................................................................viii
SECTION 1................................................................................................................................................9
1.0 INTRODUCTION...............................................................................................................................9
1.1 Information Background....................................................................................................................9
1.2 Statement of the problem.................................................................................................................2
1.3 Study Objectives................................................................................................................................3
1.3.1 General objective........................................................................................................................3
1.3.2 Specific objectives.......................................................................................................................3
1.4 Research Questions...........................................................................................................................3
1.5 Hypothesis.........................................................................................................................................4
1.6 Conceptual Framework......................................................................................................................4
SECTION 2................................................................................................................................................5
2.0 LITERATURE REVIEW...................................................................................................................5
2.1. Theoretical Framework.....................................................................................................................5
2.1.1 Anderson’s Health Behaviour Model..........................................................................................5
2.2 Definition of Telemedicine.................................................................................................................6
2.3 History of Telemedicine.....................................................................................................................6
2.4 Health Information Technology and Telemedicine............................................................................7
2.5 Benefits of Telemedicine...................................................................................................................8
2.6. Disadvantages of Telemedicine......................................................................................................11
iii
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
SECTION 3..............................................................................................................................................12
3.0 METHODOLOGY............................................................................................................................12
3.1 Research Design.............................................................................................................................13
3.2 Area of Study...................................................................................................................................13
The study was carried out in Hougang Area, Singapore (Figure 2).......................................................13
Figure 2: Map of study area (Source; Google map, 2019)....................................................................13
3.3 Study Population.............................................................................................................................14
The target population for this study was all the adult (above 18 years) resident of Hougang Area,
Singapore...............................................................................................................................................14
3.4 Sampling Techniques.......................................................................................................................14
3.4.1 Sample Size...............................................................................................................................14
A sample random sampling technique was used to select the 384 participants..................................14
3.4.2 Sample size determination.......................................................................................................14
3.4.3 Sampling Method.....................................................................................................................14
3.4.4 Recruitment Method................................................................................................................14
3.5 Data Collection Instrument..............................................................................................................15
3.6 Data Collection................................................................................................................................15
3.7 Data Analysis and Management......................................................................................................15
3.8 Ethical Considerations.....................................................................................................................15
SECTION 4..............................................................................................................................................16
4.0 ANALYSIS AND FINDINGS...........................................................................................................16
4.1 Response Rate.................................................................................................................................16
4.2 Personal Details of the Respondents...............................................................................................16
4.3 Usability of Telemedicine................................................................................................................18
SECTION 5..............................................................................................................................................19
5.0 DISCUSSION AND EVALUATION................................................................................................19
SECTION 6..............................................................................................................................................23
6.0 CONCLUSION & RECOMMENDATIONS...................................................................................23
6.1 CONCLUSION...................................................................................................................................23
6.2 RECOMMENDATIONS......................................................................................................................23
iv
3.0 METHODOLOGY............................................................................................................................12
3.1 Research Design.............................................................................................................................13
3.2 Area of Study...................................................................................................................................13
The study was carried out in Hougang Area, Singapore (Figure 2).......................................................13
Figure 2: Map of study area (Source; Google map, 2019)....................................................................13
3.3 Study Population.............................................................................................................................14
The target population for this study was all the adult (above 18 years) resident of Hougang Area,
Singapore...............................................................................................................................................14
3.4 Sampling Techniques.......................................................................................................................14
3.4.1 Sample Size...............................................................................................................................14
A sample random sampling technique was used to select the 384 participants..................................14
3.4.2 Sample size determination.......................................................................................................14
3.4.3 Sampling Method.....................................................................................................................14
3.4.4 Recruitment Method................................................................................................................14
3.5 Data Collection Instrument..............................................................................................................15
3.6 Data Collection................................................................................................................................15
3.7 Data Analysis and Management......................................................................................................15
3.8 Ethical Considerations.....................................................................................................................15
SECTION 4..............................................................................................................................................16
4.0 ANALYSIS AND FINDINGS...........................................................................................................16
4.1 Response Rate.................................................................................................................................16
4.2 Personal Details of the Respondents...............................................................................................16
4.3 Usability of Telemedicine................................................................................................................18
SECTION 5..............................................................................................................................................19
5.0 DISCUSSION AND EVALUATION................................................................................................19
SECTION 6..............................................................................................................................................23
6.0 CONCLUSION & RECOMMENDATIONS...................................................................................23
6.1 CONCLUSION...................................................................................................................................23
6.2 RECOMMENDATIONS......................................................................................................................23
iv
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
REFERENCES........................................................................................................................................24
APPENDICE............................................................................................................................................28
Appendix I: Consent for the Participant.................................................................................................28
Appendix II: Questionnaire....................................................................................................................29
LIST OF TABLES
Table 1: Sociodemographic data of the respondents……………………………………………16
Table 2: Usability of Telemedicine ……………………………………………………….…….17
v
APPENDICE............................................................................................................................................28
Appendix I: Consent for the Participant.................................................................................................28
Appendix II: Questionnaire....................................................................................................................29
LIST OF TABLES
Table 1: Sociodemographic data of the respondents……………………………………………16
Table 2: Usability of Telemedicine ……………………………………………………….…….17
v

LIST OF FIGURES
Figure 1: Conceptual framework……………………………………………………………...….5
Figure 2: Map of study area……………………………………..…………….…………………12
Figure 3: Distribution of respondents by gender…………………………………………..…….15
vi
Figure 1: Conceptual framework……………………………………………………………...….5
Figure 2: Map of study area……………………………………..…………….…………………12
Figure 3: Distribution of respondents by gender…………………………………………..…….15
vi
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
ABBREVIATIONS
ATA American Telemedicine Association
HIT Health Information Technologies
H0 Null Hypothesis
H1 Alternative Hypothesis
ICT Information, Communication Technology
IT Information Technology
SSN Statistics Singapore Newsletter
WHO World Health Organization
vii
ATA American Telemedicine Association
HIT Health Information Technologies
H0 Null Hypothesis
H1 Alternative Hypothesis
ICT Information, Communication Technology
IT Information Technology
SSN Statistics Singapore Newsletter
WHO World Health Organization
vii
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ABSTRACT
Telemedicine amalgamates communication over distance through telephones, telegrams,cables
and broadcast so as to make available use of medical information and Telemedicine is a fast
growing system. Telemedicine is widely used in health, learning and in administration sectors.
Telemedicine is of greatly assistance in integrating electronic medical records thus leading to the
decrease in the number of cases where doctors cannot access patient's records. It has also aided
in fast and delivering of quality service in health sector. The research adopts a cross-sectional
survey study and simple random sampling approach to recruit 370 respondents. Questionnaire
was the main tool for data collection and the collected data were keyed in EpiData (Version 3.1)
database, and then analysed with the SPSS software. The majority of interviewees were male
(62.2%) and most popular age group was 30-39 years (36.8%). Majority (75.3%) of the
respondents were also aware of telemedicine system. Further, majority of the respondents
reported that the system was more reliable and satisfy their needs. Thus, the success of
telemedicine implementation in Hougang Area, Singapore will enable majority of her population
to receive a faster health care services, hence this will help in propelling the idea of universal
health care.
viii
Telemedicine amalgamates communication over distance through telephones, telegrams,cables
and broadcast so as to make available use of medical information and Telemedicine is a fast
growing system. Telemedicine is widely used in health, learning and in administration sectors.
Telemedicine is of greatly assistance in integrating electronic medical records thus leading to the
decrease in the number of cases where doctors cannot access patient's records. It has also aided
in fast and delivering of quality service in health sector. The research adopts a cross-sectional
survey study and simple random sampling approach to recruit 370 respondents. Questionnaire
was the main tool for data collection and the collected data were keyed in EpiData (Version 3.1)
database, and then analysed with the SPSS software. The majority of interviewees were male
(62.2%) and most popular age group was 30-39 years (36.8%). Majority (75.3%) of the
respondents were also aware of telemedicine system. Further, majority of the respondents
reported that the system was more reliable and satisfy their needs. Thus, the success of
telemedicine implementation in Hougang Area, Singapore will enable majority of her population
to receive a faster health care services, hence this will help in propelling the idea of universal
health care.
viii
SECTION 1
1.0 INTRODUCTION
1.1 Information Background.
Health informatics and communication applications have positively impacted the healthcare
industry worldwide. The ICT revolution of the late 1990s, lead to the resurfaced of
Telemedicine, an invention that was likely to play a vital part in revolution and changes in health
informatics systems in the coming years. Telemedicine innovation is an important element in
health sector and technology. It covers also social and economic sectors, Telemedicine systems
are problem solvers for daily challenges faced in health sector and the high demand of health
information among individuals (Novillo-Ortiz, 2016).
Telemedicine system is of importance to medical experts and patients who cannot go to health
facilities because of no means of transport or being busy with other commitments, practicality or
any other issue that may play out (Sarhan, 2009). The telemedicine use in many areas shows that
quality management of health care for long term and patients being satisfied ,in several areas has
proved thus enabling enable patients access to quality health care and equipped with right
information to managed sickness. Telemedicine provides information flow between health
experts and patients, this increases quality of service delivery and high output. There is no need
patient and expert to meet physically most of communication and experts direction are done on
telemedine system. Health management systems encourages patients to manage and monitor
ix
1.0 INTRODUCTION
1.1 Information Background.
Health informatics and communication applications have positively impacted the healthcare
industry worldwide. The ICT revolution of the late 1990s, lead to the resurfaced of
Telemedicine, an invention that was likely to play a vital part in revolution and changes in health
informatics systems in the coming years. Telemedicine innovation is an important element in
health sector and technology. It covers also social and economic sectors, Telemedicine systems
are problem solvers for daily challenges faced in health sector and the high demand of health
information among individuals (Novillo-Ortiz, 2016).
Telemedicine system is of importance to medical experts and patients who cannot go to health
facilities because of no means of transport or being busy with other commitments, practicality or
any other issue that may play out (Sarhan, 2009). The telemedicine use in many areas shows that
quality management of health care for long term and patients being satisfied ,in several areas has
proved thus enabling enable patients access to quality health care and equipped with right
information to managed sickness. Telemedicine provides information flow between health
experts and patients, this increases quality of service delivery and high output. There is no need
patient and expert to meet physically most of communication and experts direction are done on
telemedine system. Health management systems encourages patients to manage and monitor
ix
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
their health condition for a system detecting pressure level and application detecting insulin
levels of diabetes patients. This systems are cheap and cost friendly even poor people can afford
and are user-friendly to use .Telemedicine systems ensures patients get quality services and are
easy to get soft wares which encourages the patients to responsible of their health. Telemedicine
systems has helped healthcare experts to respond to patients health state fast, provides patients in
rural areas with quality health information local and cost friendly services , makes health service
available and easy to access information, ensure after discharge care to know status of patients
and healing progress, improves accuracy and integrity of health records for patien (Alvandi,
2017).
Telemedicine system is of great importance during transfer of useful medical related
data .Medical expert can communicate with other experts from other countries on telemedicine
system(Rangasamy et al., 2011). With the numerous issues arising in medical sector ,emerging
of complicated diseases telemedicine plays vital role in promoting faster learning and this
helps in saving patients’ lives by minimizing health problems .Telemedicine system can be
applicable in military. For example when soldiers are at war where there is no near by health
centres or facilities telemedicine application can be of great help to them.Soldiers can use
telemedice to diagnose diseases .Telemedicine system can be used everywhere and in every part
of the world. (Rangasamy et al., 2011).
1.2 Statement of the problem.
The growth of telemedicine use globally is to improve quality of health sector. Telemedicine
help to improve in treatment of people and enable patients in rural areas to access health services
easily. There has been use of traditional way of communicating using telephone, messenger and
x
levels of diabetes patients. This systems are cheap and cost friendly even poor people can afford
and are user-friendly to use .Telemedicine systems ensures patients get quality services and are
easy to get soft wares which encourages the patients to responsible of their health. Telemedicine
systems has helped healthcare experts to respond to patients health state fast, provides patients in
rural areas with quality health information local and cost friendly services , makes health service
available and easy to access information, ensure after discharge care to know status of patients
and healing progress, improves accuracy and integrity of health records for patien (Alvandi,
2017).
Telemedicine system is of great importance during transfer of useful medical related
data .Medical expert can communicate with other experts from other countries on telemedicine
system(Rangasamy et al., 2011). With the numerous issues arising in medical sector ,emerging
of complicated diseases telemedicine plays vital role in promoting faster learning and this
helps in saving patients’ lives by minimizing health problems .Telemedicine system can be
applicable in military. For example when soldiers are at war where there is no near by health
centres or facilities telemedicine application can be of great help to them.Soldiers can use
telemedice to diagnose diseases .Telemedicine system can be used everywhere and in every part
of the world. (Rangasamy et al., 2011).
1.2 Statement of the problem.
The growth of telemedicine use globally is to improve quality of health sector. Telemedicine
help to improve in treatment of people and enable patients in rural areas to access health services
easily. There has been use of traditional way of communicating using telephone, messenger and
x
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
fax. Telemedicine system uses current innovation. To benefit from telemedicine applications, the
application be used by patients and health care providers.
McClellan and colleagues (2008) reported that health care effective cost and great quality action
taken to improve health care are not effective utilized locally, nationally and globally. This leads
to wastage and underutilization of hospital resources. (Heinzelmann et al, 2006). In Hougang
Area, Singapore, a few studies concerning the roll out rate of telemedicine have been conducted
but none have been carried out to determine the wider role played by telemedicine and its
acceptance level, hence this necessitated this present study.
1.3 Study Objectives
This study has objectives below.
1.3.1 General objective
To explore telemedicine roles in health sector service delivering in Hougang Area, Singapore.
1.3.2 Specific objectives
i. To determines awareness level of telemedicine delivery as a particular approach to health
care in Hougang Area, Singapore.
ii. To determine the reliability of telemedicine as a method of health care delivery among
residents of Hougang Area, Singapore.
iii. To determine satisfaction level and future use of telemedicine as a method of health care
delivery among residents of Hougang Area, Singapore.
1.4 Research Questions
i. How to know awareness levels in telemedicine delivery as a particular approach to health
care in Hougang Area, Singapore?
xi
application be used by patients and health care providers.
McClellan and colleagues (2008) reported that health care effective cost and great quality action
taken to improve health care are not effective utilized locally, nationally and globally. This leads
to wastage and underutilization of hospital resources. (Heinzelmann et al, 2006). In Hougang
Area, Singapore, a few studies concerning the roll out rate of telemedicine have been conducted
but none have been carried out to determine the wider role played by telemedicine and its
acceptance level, hence this necessitated this present study.
1.3 Study Objectives
This study has objectives below.
1.3.1 General objective
To explore telemedicine roles in health sector service delivering in Hougang Area, Singapore.
1.3.2 Specific objectives
i. To determines awareness level of telemedicine delivery as a particular approach to health
care in Hougang Area, Singapore.
ii. To determine the reliability of telemedicine as a method of health care delivery among
residents of Hougang Area, Singapore.
iii. To determine satisfaction level and future use of telemedicine as a method of health care
delivery among residents of Hougang Area, Singapore.
1.4 Research Questions
i. How to know awareness levels in telemedicine delivery as a particular approach to health
care in Hougang Area, Singapore?
xi
ii. Is telemedicine a reliable method of health care delivery among residents of Hougang
Area, Singapore?
iii. What are the satisfaction levels and future usage of telemedicine as a method of health
care delivery among residents of Hougang Area, Singapore
1.5 Hypothesis
H0: Telemedicine is not the actor in delivery of health care in Hougang Area, Singapore
H1: Telemedicine is the actor in delivery of health care Hougang Area, Singapore
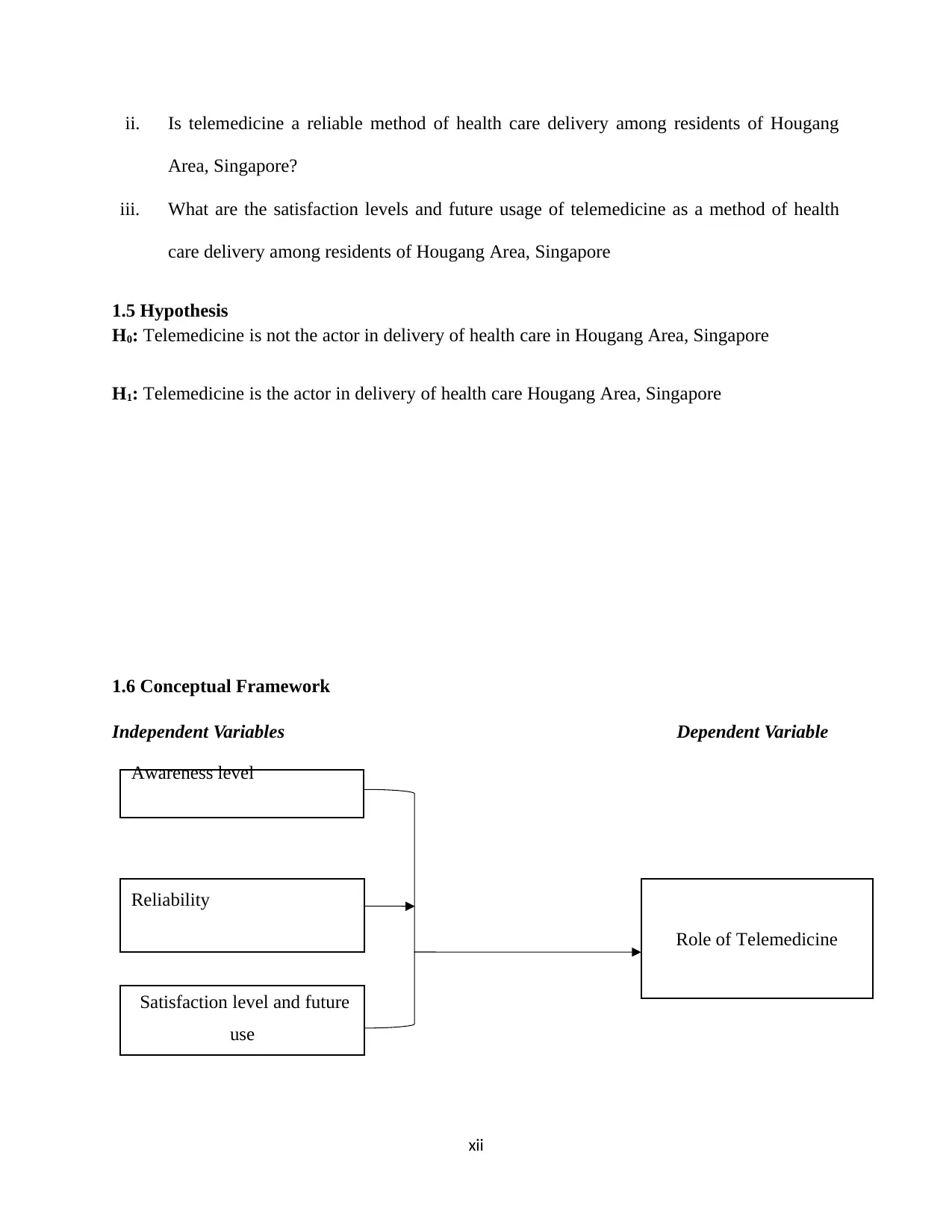
1.6 Conceptual Framework
Independent Variables Dependent Variable
xii
Role of Telemedicine
Awareness level
Reliability
Satisfaction level and future
use
Area, Singapore?
iii. What are the satisfaction levels and future usage of telemedicine as a method of health
care delivery among residents of Hougang Area, Singapore
1.5 Hypothesis
H0: Telemedicine is not the actor in delivery of health care in Hougang Area, Singapore
H1: Telemedicine is the actor in delivery of health care Hougang Area, Singapore
1.6 Conceptual Framework
Independent Variables Dependent Variable
xii
Role of Telemedicine
Awareness level
Reliability
Satisfaction level and future
use
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 38
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





