Case Study: Chronic Kidney Disease, Diagnosis, Symptoms, and Treatment
VerifiedAdded on 2022/10/19
|5
|1570
|166
Case Study
AI Summary
This case study focuses on a patient diagnosed with chronic kidney disease (CKD) due to diffuse nephron loss, with a medical history of type 2 diabetes and hypertension. The analysis explores the pathophysiology, risk factors, and aetiology of CKD, highlighting symptoms such as fatigue, itchy skin, and swollen legs. Diagnostic tests, including blood and urine tests, are discussed, along with treatment modalities like medications to reduce blood pressure, statins, and supplements like erythropoietin and calcium. The study also covers the role of dietary interventions, regenerative medicine, and the importance of managing diabetes to slow disease progression. The patient's condition is linked to poor management of underlying conditions, emphasizing the impact of high blood pressure and elevated blood sugar on kidney health, and the importance of regular monitoring and proactive treatment strategies. References to supporting literature are included.
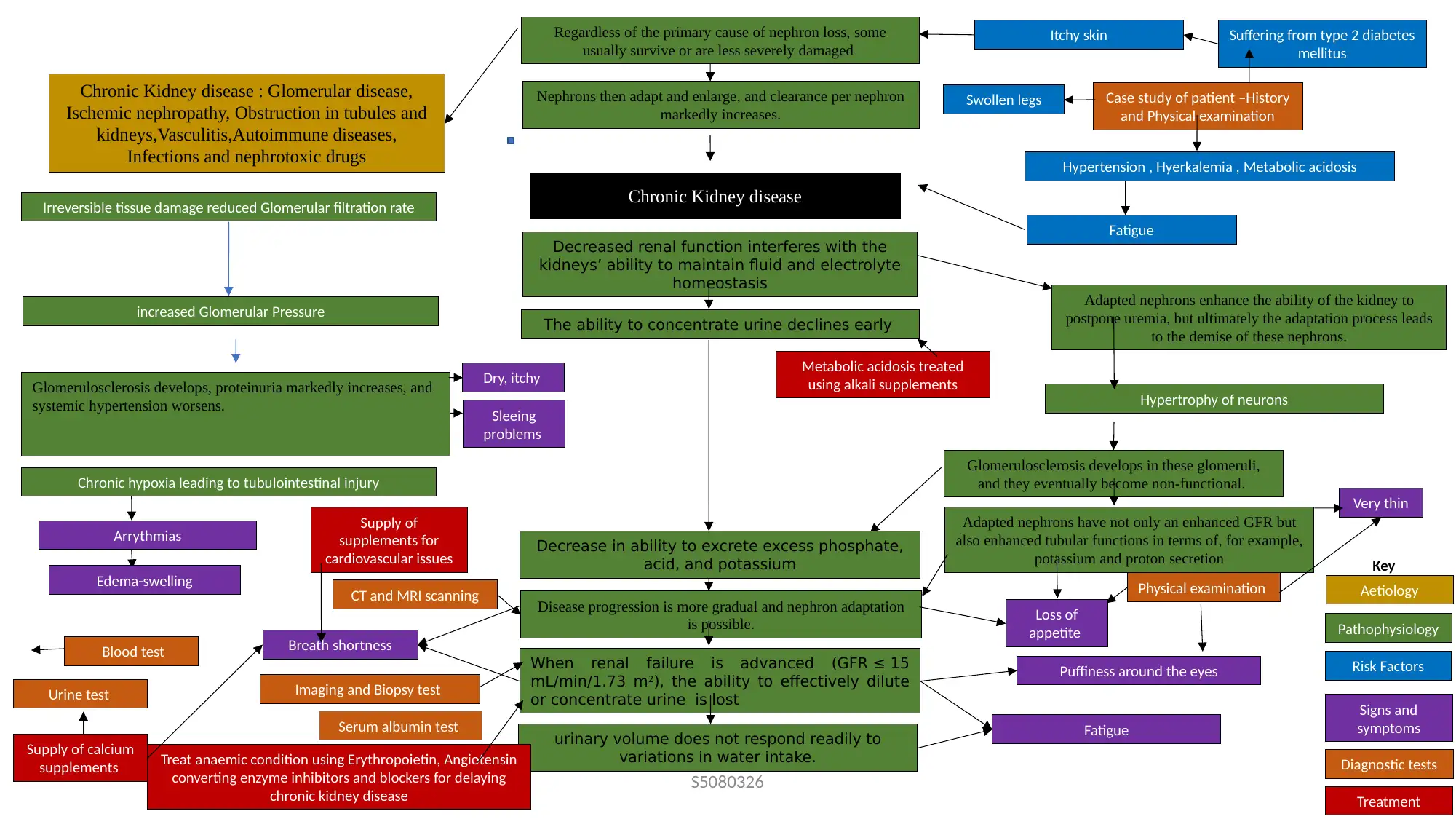
Glomerulosclerosis develops, proteinuria markedly increases, and
systemic hypertension worsens.
Irreversible tissue damage reduced Glomerular filtration rate
Suffering from type 2 diabetes
mellitus
Hypertension , Hyerkalemia , Metabolic acidosis
The ability to concentrate urine declines early
Puffiness around the eyes
Chronic Kidney disease : Glomerular disease,
Ischemic nephropathy, Obstruction in tubules and
kidneys,Vasculitis,Autoimmune diseases,
Infections and nephrotoxic drugs
Breath shortness
Treatment
Disease progression is more gradual and nephron adaptation
is possible.
Adapted nephrons enhance the ability of the kidney to
postpone uremia, but ultimately the adaptation process leads
to the demise of these nephrons.
When renal failure is advanced (GFR ≤ 15
mL/min/1.73 m2), the ability to effectively dilute
or concentrate urine is lost
Supply of
supplements for
cardiovascular issues
Loss of
appetite
Glomerulosclerosis develops in these glomeruli,
and they eventually become non-functional.
Case study of patient –History
and Physical examination
Key
Arrythmias
Regardless of the primary cause of nephron loss, some
usually survive or are less severely damaged
Decreased renal function interferes with the
kidneys’ ability to maintain fluid and electrolyte
homeostasis
Swollen legs
Pathophysiology
Risk Factors
Aetiology
Signs and
symptoms
Diagnostic tests
Fatigue
CT and MRI scanning
Very thin
Fatigue
increased Glomerular Pressure
Nephrons then adapt and enlarge, and clearance per nephron
markedly increases.
Physical examination
Adapted nephrons have not only an enhanced GFR but
also enhanced tubular functions in terms of, for example,
potassium and proton secretion
Hypertrophy of neurons
Urine test
Itchy skin
Metabolic acidosis treated
using alkali supplements
Decrease in ability to excrete excess phosphate,
acid, and potassium
Supply of calcium
supplements
Chronic hypoxia leading to tubulointestinal injury
Edema-swelling
Sleeing
problems
Dry, itchy
urinary volume does not respond readily to
variations in water intake.
Imaging and Biopsy test
Treat anaemic condition using Erythropoietin, Angiotensin
converting enzyme inhibitors and blockers for delaying
chronic kidney disease
Serum albumin test
Blood test
S5080326
Chronic Kidney disease
systemic hypertension worsens.
Irreversible tissue damage reduced Glomerular filtration rate
Suffering from type 2 diabetes
mellitus
Hypertension , Hyerkalemia , Metabolic acidosis
The ability to concentrate urine declines early
Puffiness around the eyes
Chronic Kidney disease : Glomerular disease,
Ischemic nephropathy, Obstruction in tubules and
kidneys,Vasculitis,Autoimmune diseases,
Infections and nephrotoxic drugs
Breath shortness
Treatment
Disease progression is more gradual and nephron adaptation
is possible.
Adapted nephrons enhance the ability of the kidney to
postpone uremia, but ultimately the adaptation process leads
to the demise of these nephrons.
When renal failure is advanced (GFR ≤ 15
mL/min/1.73 m2), the ability to effectively dilute
or concentrate urine is lost
Supply of
supplements for
cardiovascular issues
Loss of
appetite
Glomerulosclerosis develops in these glomeruli,
and they eventually become non-functional.
Case study of patient –History
and Physical examination
Key
Arrythmias
Regardless of the primary cause of nephron loss, some
usually survive or are less severely damaged
Decreased renal function interferes with the
kidneys’ ability to maintain fluid and electrolyte
homeostasis
Swollen legs
Pathophysiology
Risk Factors
Aetiology
Signs and
symptoms
Diagnostic tests
Fatigue
CT and MRI scanning
Very thin
Fatigue
increased Glomerular Pressure
Nephrons then adapt and enlarge, and clearance per nephron
markedly increases.
Physical examination
Adapted nephrons have not only an enhanced GFR but
also enhanced tubular functions in terms of, for example,
potassium and proton secretion
Hypertrophy of neurons
Urine test
Itchy skin
Metabolic acidosis treated
using alkali supplements
Decrease in ability to excrete excess phosphate,
acid, and potassium
Supply of calcium
supplements
Chronic hypoxia leading to tubulointestinal injury
Edema-swelling
Sleeing
problems
Dry, itchy
urinary volume does not respond readily to
variations in water intake.
Imaging and Biopsy test
Treat anaemic condition using Erythropoietin, Angiotensin
converting enzyme inhibitors and blockers for delaying
chronic kidney disease
Serum albumin test
Blood test
S5080326
Chronic Kidney disease
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Chronic Kidney disease-Case study &Discussion
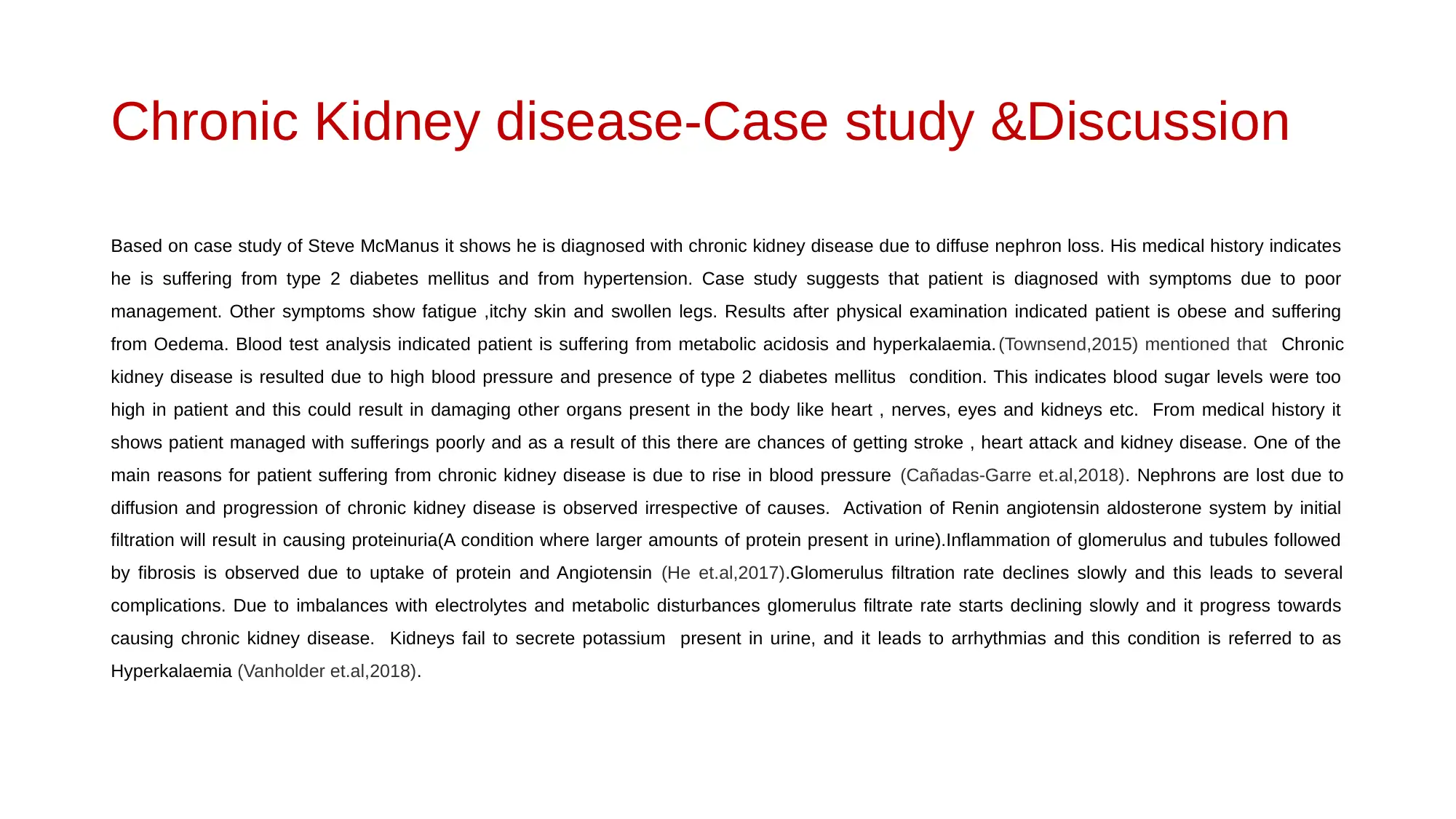
Based on case study of Steve McManus it shows he is diagnosed with chronic kidney disease due to diffuse nephron loss. His medical history indicates
he is suffering from type 2 diabetes mellitus and from hypertension. Case study suggests that patient is diagnosed with symptoms due to poor
management. Other symptoms show fatigue ,itchy skin and swollen legs. Results after physical examination indicated patient is obese and suffering
from Oedema. Blood test analysis indicated patient is suffering from metabolic acidosis and hyperkalaemia. (Townsend,2015) mentioned that Chronic
kidney disease is resulted due to high blood pressure and presence of type 2 diabetes mellitus condition. This indicates blood sugar levels were too
high in patient and this could result in damaging other organs present in the body like heart , nerves, eyes and kidneys etc. From medical history it
shows patient managed with sufferings poorly and as a result of this there are chances of getting stroke , heart attack and kidney disease. One of the
main reasons for patient suffering from chronic kidney disease is due to rise in blood pressure (Cañadas-Garre et.al,2018). Nephrons are lost due to
diffusion and progression of chronic kidney disease is observed irrespective of causes. Activation of Renin angiotensin aldosterone system by initial
filtration will result in causing proteinuria(A condition where larger amounts of protein present in urine).Inflammation of glomerulus and tubules followed
by fibrosis is observed due to uptake of protein and Angiotensin (He et.al,2017).Glomerulus filtration rate declines slowly and this leads to several
complications. Due to imbalances with electrolytes and metabolic disturbances glomerulus filtrate rate starts declining slowly and it progress towards
causing chronic kidney disease. Kidneys fail to secrete potassium present in urine, and it leads to arrhythmias and this condition is referred to as
Hyperkalaemia (Vanholder et.al,2018).
Based on case study of Steve McManus it shows he is diagnosed with chronic kidney disease due to diffuse nephron loss. His medical history indicates
he is suffering from type 2 diabetes mellitus and from hypertension. Case study suggests that patient is diagnosed with symptoms due to poor
management. Other symptoms show fatigue ,itchy skin and swollen legs. Results after physical examination indicated patient is obese and suffering
from Oedema. Blood test analysis indicated patient is suffering from metabolic acidosis and hyperkalaemia. (Townsend,2015) mentioned that Chronic
kidney disease is resulted due to high blood pressure and presence of type 2 diabetes mellitus condition. This indicates blood sugar levels were too
high in patient and this could result in damaging other organs present in the body like heart , nerves, eyes and kidneys etc. From medical history it
shows patient managed with sufferings poorly and as a result of this there are chances of getting stroke , heart attack and kidney disease. One of the
main reasons for patient suffering from chronic kidney disease is due to rise in blood pressure (Cañadas-Garre et.al,2018). Nephrons are lost due to
diffusion and progression of chronic kidney disease is observed irrespective of causes. Activation of Renin angiotensin aldosterone system by initial
filtration will result in causing proteinuria(A condition where larger amounts of protein present in urine).Inflammation of glomerulus and tubules followed
by fibrosis is observed due to uptake of protein and Angiotensin (He et.al,2017).Glomerulus filtration rate declines slowly and this leads to several
complications. Due to imbalances with electrolytes and metabolic disturbances glomerulus filtrate rate starts declining slowly and it progress towards
causing chronic kidney disease. Kidneys fail to secrete potassium present in urine, and it leads to arrhythmias and this condition is referred to as
Hyperkalaemia (Vanholder et.al,2018).
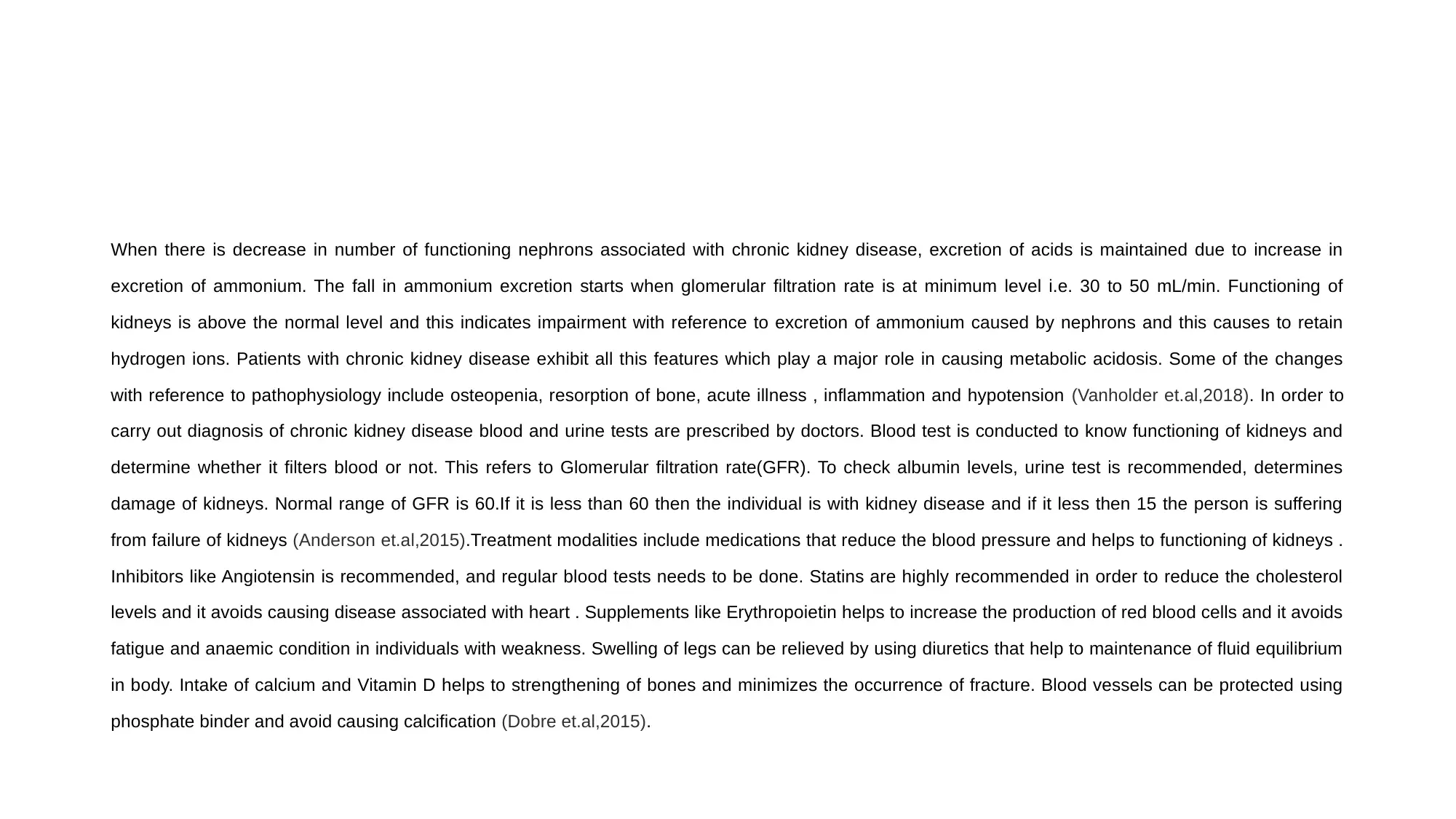
When there is decrease in number of functioning nephrons associated with chronic kidney disease, excretion of acids is maintained due to increase in
excretion of ammonium. The fall in ammonium excretion starts when glomerular filtration rate is at minimum level i.e. 30 to 50 mL/min. Functioning of
kidneys is above the normal level and this indicates impairment with reference to excretion of ammonium caused by nephrons and this causes to retain
hydrogen ions. Patients with chronic kidney disease exhibit all this features which play a major role in causing metabolic acidosis. Some of the changes
with reference to pathophysiology include osteopenia, resorption of bone, acute illness , inflammation and hypotension (Vanholder et.al,2018). In order to
carry out diagnosis of chronic kidney disease blood and urine tests are prescribed by doctors. Blood test is conducted to know functioning of kidneys and
determine whether it filters blood or not. This refers to Glomerular filtration rate(GFR). To check albumin levels, urine test is recommended, determines
damage of kidneys. Normal range of GFR is 60.If it is less than 60 then the individual is with kidney disease and if it less then 15 the person is suffering
from failure of kidneys (Anderson et.al,2015).Treatment modalities include medications that reduce the blood pressure and helps to functioning of kidneys .
Inhibitors like Angiotensin is recommended, and regular blood tests needs to be done. Statins are highly recommended in order to reduce the cholesterol
levels and it avoids causing disease associated with heart . Supplements like Erythropoietin helps to increase the production of red blood cells and it avoids
fatigue and anaemic condition in individuals with weakness. Swelling of legs can be relieved by using diuretics that help to maintenance of fluid equilibrium
in body. Intake of calcium and Vitamin D helps to strengthening of bones and minimizes the occurrence of fracture. Blood vessels can be protected using
phosphate binder and avoid causing calcification (Dobre et.al,2015).
excretion of ammonium. The fall in ammonium excretion starts when glomerular filtration rate is at minimum level i.e. 30 to 50 mL/min. Functioning of
kidneys is above the normal level and this indicates impairment with reference to excretion of ammonium caused by nephrons and this causes to retain
hydrogen ions. Patients with chronic kidney disease exhibit all this features which play a major role in causing metabolic acidosis. Some of the changes
with reference to pathophysiology include osteopenia, resorption of bone, acute illness , inflammation and hypotension (Vanholder et.al,2018). In order to
carry out diagnosis of chronic kidney disease blood and urine tests are prescribed by doctors. Blood test is conducted to know functioning of kidneys and
determine whether it filters blood or not. This refers to Glomerular filtration rate(GFR). To check albumin levels, urine test is recommended, determines
damage of kidneys. Normal range of GFR is 60.If it is less than 60 then the individual is with kidney disease and if it less then 15 the person is suffering
from failure of kidneys (Anderson et.al,2015).Treatment modalities include medications that reduce the blood pressure and helps to functioning of kidneys .
Inhibitors like Angiotensin is recommended, and regular blood tests needs to be done. Statins are highly recommended in order to reduce the cholesterol
levels and it avoids causing disease associated with heart . Supplements like Erythropoietin helps to increase the production of red blood cells and it avoids
fatigue and anaemic condition in individuals with weakness. Swelling of legs can be relieved by using diuretics that help to maintenance of fluid equilibrium
in body. Intake of calcium and Vitamin D helps to strengthening of bones and minimizes the occurrence of fracture. Blood vessels can be protected using
phosphate binder and avoid causing calcification (Dobre et.al,2015).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
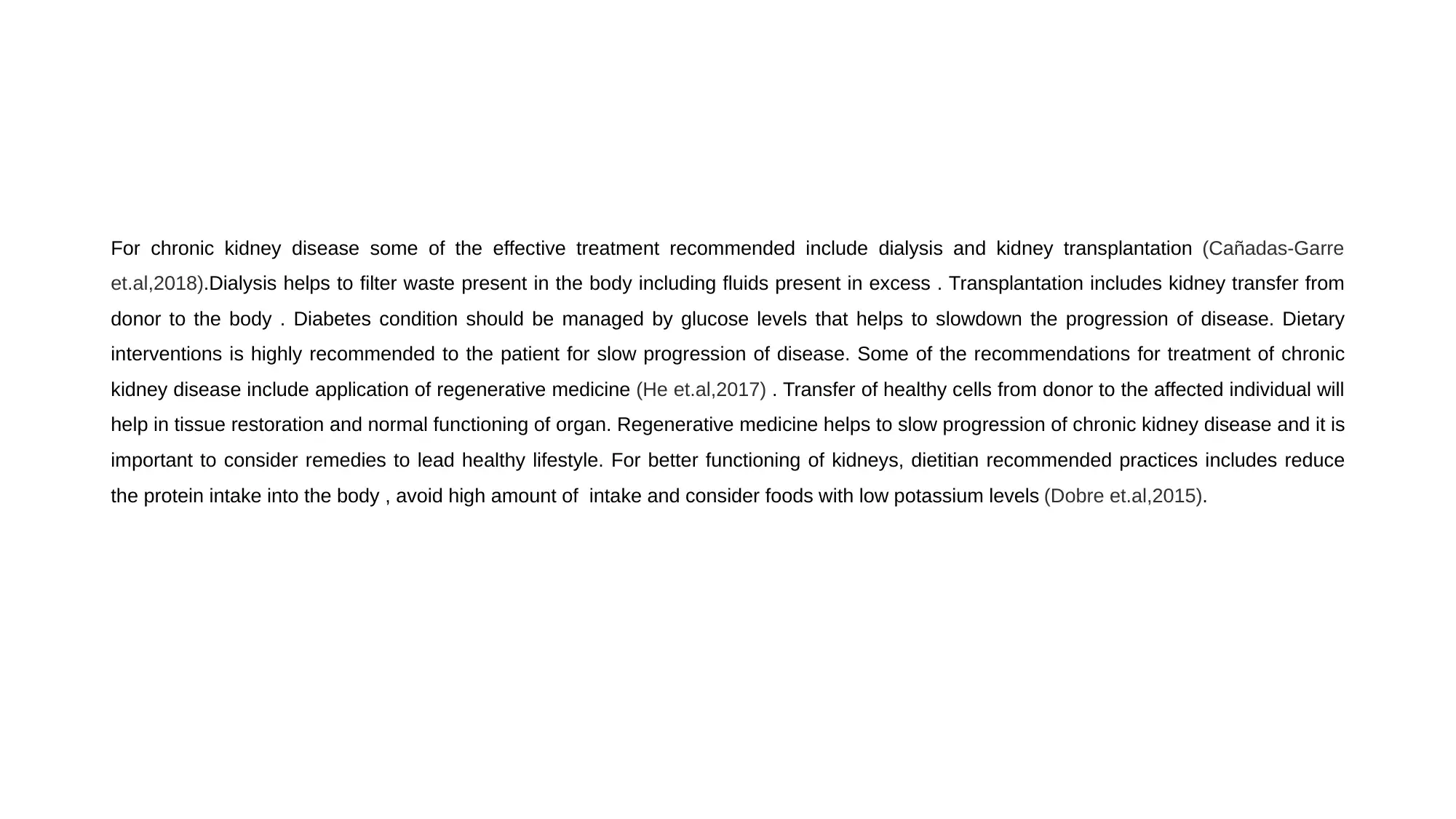
For chronic kidney disease some of the effective treatment recommended include dialysis and kidney transplantation (Cañadas-Garre
et.al,2018).Dialysis helps to filter waste present in the body including fluids present in excess . Transplantation includes kidney transfer from
donor to the body . Diabetes condition should be managed by glucose levels that helps to slowdown the progression of disease. Dietary
interventions is highly recommended to the patient for slow progression of disease. Some of the recommendations for treatment of chronic
kidney disease include application of regenerative medicine (He et.al,2017) . Transfer of healthy cells from donor to the affected individual will
help in tissue restoration and normal functioning of organ. Regenerative medicine helps to slow progression of chronic kidney disease and it is
important to consider remedies to lead healthy lifestyle. For better functioning of kidneys, dietitian recommended practices includes reduce
the protein intake into the body , avoid high amount of intake and consider foods with low potassium levels (Dobre et.al,2015).
et.al,2018).Dialysis helps to filter waste present in the body including fluids present in excess . Transplantation includes kidney transfer from
donor to the body . Diabetes condition should be managed by glucose levels that helps to slowdown the progression of disease. Dietary
interventions is highly recommended to the patient for slow progression of disease. Some of the recommendations for treatment of chronic
kidney disease include application of regenerative medicine (He et.al,2017) . Transfer of healthy cells from donor to the affected individual will
help in tissue restoration and normal functioning of organ. Regenerative medicine helps to slow progression of chronic kidney disease and it is
important to consider remedies to lead healthy lifestyle. For better functioning of kidneys, dietitian recommended practices includes reduce
the protein intake into the body , avoid high amount of intake and consider foods with low potassium levels (Dobre et.al,2015).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
References
• Townsend R. R. (2015). Arterial stiffness and chronic kidney disease: lessons from the Chronic Renal
Insufficiency Cohort study. Current opinion in nephrology and hypertension, 24(1), 47–53.
doi:10.1097/MNH.0000000000000086
• He, J., Shlipak, M., Anderson, A., Roy, J. A., Feldman, H. I., Kallem, R. R., … CRIC (Chronic Renal Insufficiency
Cohort) Investigators (2017). Risk Factors for Heart Failure in Patients With Chronic Kidney Disease: The CRIC
(Chronic Renal Insufficiency Cohort) Study. Journal of the American Heart Association, 6(5), e005336.
doi:10.1161/JAHA.116.005336
• Vanholder, R., Van Laecke, S., Glorieux, G., Verbeke, F., Castillo-Rodriguez, E., & Ortiz, A. (2018). Deleting
Death and Dialysis: Conservative Care of Cardio-Vascular Risk and Kidney Function Loss in Chronic Kidney
Disease (CKD). Toxins, 10(6), 237. doi:10.3390/toxins10060237
• Anderson, A. H., Yang, W., Townsend, R. R., Pan, Q., Chertow, G. M., Kusek, J. W., … Chronic Renal
Insufficiency Cohort Study Investigators (2015). Time-updated systolic blood pressure and the progression of
chronic kidney disease: a cohort study. Annals of internal medicine, 162(4), 258–265. doi:10.7326/M14-0488
• Cañadas-Garre, M., Anderson, K., McGoldrick, J., Maxwell, A. P., & McKnight, A. J. (2018). Genomic
approaches in the search for molecular biomarkers in chronic kidney disease. Journal of translational
medicine, 16(1), 292. doi:10.1186/s12967-018-1664-7
• Dobre, M., Yang, W., Pan, Q., Appel, L., Bellovich, K., Chen, J., … CRIC Study Investigators (2015). Persistent
high serum bicarbonate and the risk of heart failure in patients with chronic kidney disease (CKD): A report from
the Chronic Renal Insufficiency Cohort (CRIC) study. Journal of the American Heart Association, 4(4), e001599.
doi:10.1161/JAHA.114.001599
• Townsend R. R. (2015). Arterial stiffness and chronic kidney disease: lessons from the Chronic Renal
Insufficiency Cohort study. Current opinion in nephrology and hypertension, 24(1), 47–53.
doi:10.1097/MNH.0000000000000086
• He, J., Shlipak, M., Anderson, A., Roy, J. A., Feldman, H. I., Kallem, R. R., … CRIC (Chronic Renal Insufficiency
Cohort) Investigators (2017). Risk Factors for Heart Failure in Patients With Chronic Kidney Disease: The CRIC
(Chronic Renal Insufficiency Cohort) Study. Journal of the American Heart Association, 6(5), e005336.
doi:10.1161/JAHA.116.005336
• Vanholder, R., Van Laecke, S., Glorieux, G., Verbeke, F., Castillo-Rodriguez, E., & Ortiz, A. (2018). Deleting
Death and Dialysis: Conservative Care of Cardio-Vascular Risk and Kidney Function Loss in Chronic Kidney
Disease (CKD). Toxins, 10(6), 237. doi:10.3390/toxins10060237
• Anderson, A. H., Yang, W., Townsend, R. R., Pan, Q., Chertow, G. M., Kusek, J. W., … Chronic Renal
Insufficiency Cohort Study Investigators (2015). Time-updated systolic blood pressure and the progression of
chronic kidney disease: a cohort study. Annals of internal medicine, 162(4), 258–265. doi:10.7326/M14-0488
• Cañadas-Garre, M., Anderson, K., McGoldrick, J., Maxwell, A. P., & McKnight, A. J. (2018). Genomic
approaches in the search for molecular biomarkers in chronic kidney disease. Journal of translational
medicine, 16(1), 292. doi:10.1186/s12967-018-1664-7
• Dobre, M., Yang, W., Pan, Q., Appel, L., Bellovich, K., Chen, J., … CRIC Study Investigators (2015). Persistent
high serum bicarbonate and the risk of heart failure in patients with chronic kidney disease (CKD): A report from
the Chronic Renal Insufficiency Cohort (CRIC) study. Journal of the American Heart Association, 4(4), e001599.
doi:10.1161/JAHA.114.001599
1 out of 5
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





