Types of Pacemakers for Treating Cardiovascular Disorders
VerifiedAdded on 2022/12/28
|19
|5856
|2
AI Summary
This mini-review discusses the different types of pacemakers used to treat various cardiovascular disorders, including single chamber pacemakers, dual chamber pacemakers, and biventricular pacemakers. It explores their utility and associated health outcomes.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: HEALTH ASSIGNMENT
HEALTH ASSIGNMENT
Name of the Student:
Name of the University:
Author Note:
HEALTH ASSIGNMENT
Name of the Student:
Name of the University:
Author Note:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1HEALTH ASSIGNMENT
Abstract:
Statistical data collected from the
Department of Health, Australia suggests
that cardiovascular disorders are the
leading causes that attribute to an
overwhelming proportion of death. The
most common cardiovascular conditions
include, stroke, arrhythmias and heart
block. Pacemakers can be broadly defined
as medical devices that help to monitor
and regulate the heart-beat so as to ensure
normal functioning of the heart. The
correct choice of the pacemaker type can
help to acquire positive patient outcome.
The paper critically mentions about the
three types of pacemakers that include,
single chamber pacemaker, dual chamber
pacemaker and Biventricular pacemakers
and discusses about their utility and
associated health outcome.
Introduction:
Pacemakers can be defined as
miniature devices that are placed
underneath the skin of the chest so as to
effectively regulate the heart-beat.
Pacemakers are usually used in order to
treat issues pertaining to irregular heart
beat which is also known as arrhythmia.
Research studies in this regard mention
that implantation of pacemakers within the
chest requires an extensive surgical
procedure (Nazif et al. 2015). It has further
been suggested that implantation of
pacemakers can cumulatively improve
patient outcome.
According to the Department of
Health Australia (2019), it has been
mentioned that cardiovascular disorder
form one of the leading causes of death
within the Australian territory. Statistical
evidence suggests that between the year
2014-2015, on an average 4.2 million
Australian adults which formed 18.3% of
the Australian population presented
problems related to cardiovascular
problems (Sahle et al. 2016). Out of the
predicted statistical data, 1.2 million of the
affected individuals were reported to suffer
from cardiovascular conditions such as
Abstract:
Statistical data collected from the
Department of Health, Australia suggests
that cardiovascular disorders are the
leading causes that attribute to an
overwhelming proportion of death. The
most common cardiovascular conditions
include, stroke, arrhythmias and heart
block. Pacemakers can be broadly defined
as medical devices that help to monitor
and regulate the heart-beat so as to ensure
normal functioning of the heart. The
correct choice of the pacemaker type can
help to acquire positive patient outcome.
The paper critically mentions about the
three types of pacemakers that include,
single chamber pacemaker, dual chamber
pacemaker and Biventricular pacemakers
and discusses about their utility and
associated health outcome.
Introduction:
Pacemakers can be defined as
miniature devices that are placed
underneath the skin of the chest so as to
effectively regulate the heart-beat.
Pacemakers are usually used in order to
treat issues pertaining to irregular heart
beat which is also known as arrhythmia.
Research studies in this regard mention
that implantation of pacemakers within the
chest requires an extensive surgical
procedure (Nazif et al. 2015). It has further
been suggested that implantation of
pacemakers can cumulatively improve
patient outcome.
According to the Department of
Health Australia (2019), it has been
mentioned that cardiovascular disorder
form one of the leading causes of death
within the Australian territory. Statistical
evidence suggests that between the year
2014-2015, on an average 4.2 million
Australian adults which formed 18.3% of
the Australian population presented
problems related to cardiovascular
problems (Sahle et al. 2016). Out of the
predicted statistical data, 1.2 million of the
affected individuals were reported to suffer
from cardiovascular conditions such as
2HEALTH ASSIGNMENT
heart disease and one episode of stroke. In
addition to this, as reported by the
Australian Bureau of Statistics, 2.6 million
Australians have presented physical health
problems related to hypertension (Sahle et
al. 2016). Also, 430,000 individuals have
been reported to suffer an episode of
myocardial infarction (Heart Attack)
(www.health.gov.au 2019). Further, in the
year 2015, 29% of the total deaths were
attributed due to cardiovascular diseases
(www.health.gov.au 2019). Further,
approximately, 69,000 members of the
Aboriginal and Torres Islander community
were reported to suffer from
cardiovascular disorders
(www.health.gov.au 2019). Within the
year 2014 to 2015, 15.7% of the
indigenous population base was predicted
to suffer from cardiovascular disorders
which had culminated thrice the incidence
rate within the indigenous community
members (Sahle et al. 2016). Therefore, on
the basis of the available statistical data it
can be stated that cardiovascular diseases
have emerged as a disease burden which
has limited the quality of life of the people.
As stated by Greason et al. (2017),
cardiovascular disorders such as
bradycardia, arrhythmia, Long QT
syndrome and cardiac blockage can be
effectively treated with the help of
pacemaker implantation. Hence, in this
regard it can be mentioned that pacemaker
implantation is the single effective
intervention that can help to alleviate the
disease burden and can subsequently
improve the quality of life of the patients.
Thus, on account of the available
background information about the disease
prevalence, conducting an exhaustive
research on the use of pacemakers as an
effective treatment can be considered
relevant. This accounts for the reason why
this mini-review paper focuses on the use
of pacemakers as a treatment option for
ensuring positive health outcome in
patients suffering from cardiovascular
disorders.
heart disease and one episode of stroke. In
addition to this, as reported by the
Australian Bureau of Statistics, 2.6 million
Australians have presented physical health
problems related to hypertension (Sahle et
al. 2016). Also, 430,000 individuals have
been reported to suffer an episode of
myocardial infarction (Heart Attack)
(www.health.gov.au 2019). Further, in the
year 2015, 29% of the total deaths were
attributed due to cardiovascular diseases
(www.health.gov.au 2019). Further,
approximately, 69,000 members of the
Aboriginal and Torres Islander community
were reported to suffer from
cardiovascular disorders
(www.health.gov.au 2019). Within the
year 2014 to 2015, 15.7% of the
indigenous population base was predicted
to suffer from cardiovascular disorders
which had culminated thrice the incidence
rate within the indigenous community
members (Sahle et al. 2016). Therefore, on
the basis of the available statistical data it
can be stated that cardiovascular diseases
have emerged as a disease burden which
has limited the quality of life of the people.
As stated by Greason et al. (2017),
cardiovascular disorders such as
bradycardia, arrhythmia, Long QT
syndrome and cardiac blockage can be
effectively treated with the help of
pacemaker implantation. Hence, in this
regard it can be mentioned that pacemaker
implantation is the single effective
intervention that can help to alleviate the
disease burden and can subsequently
improve the quality of life of the patients.
Thus, on account of the available
background information about the disease
prevalence, conducting an exhaustive
research on the use of pacemakers as an
effective treatment can be considered
relevant. This accounts for the reason why
this mini-review paper focuses on the use
of pacemakers as a treatment option for
ensuring positive health outcome in
patients suffering from cardiovascular
disorders.
3HEALTH ASSIGNMENT
Comparison with pros/cons and how
future devices might address the issues:
According to Mohananey et al.
(2017), pacemaker can be defined as a
miniature medical device that is integrated
within the chest or the abdomen in order to
control the abnormal heart beats. The
medical device makes use of electrical
pulses in order to ensure that the heart
beats at a normal rate. Pacemakers are also
used for the treatment of arrhythmias or
cardiovascular issues that causes the heart
to beat irregularly (Mohananey et al.
2017). Arrhythmias are cardiac issues that
causes abnormality with the beating
pattern of the heart. It has been reported
that arrhythmia can either cause the heart
to either beat too fast or too slow with an
irregular cardiac rhythm (Greason et al.
2017). It should be noted in this regard that
an accelerated heart beat is referred to as
tachycardia and a slower heart beat is
referred to as bradycardia (Mohananey et
al. 2017).
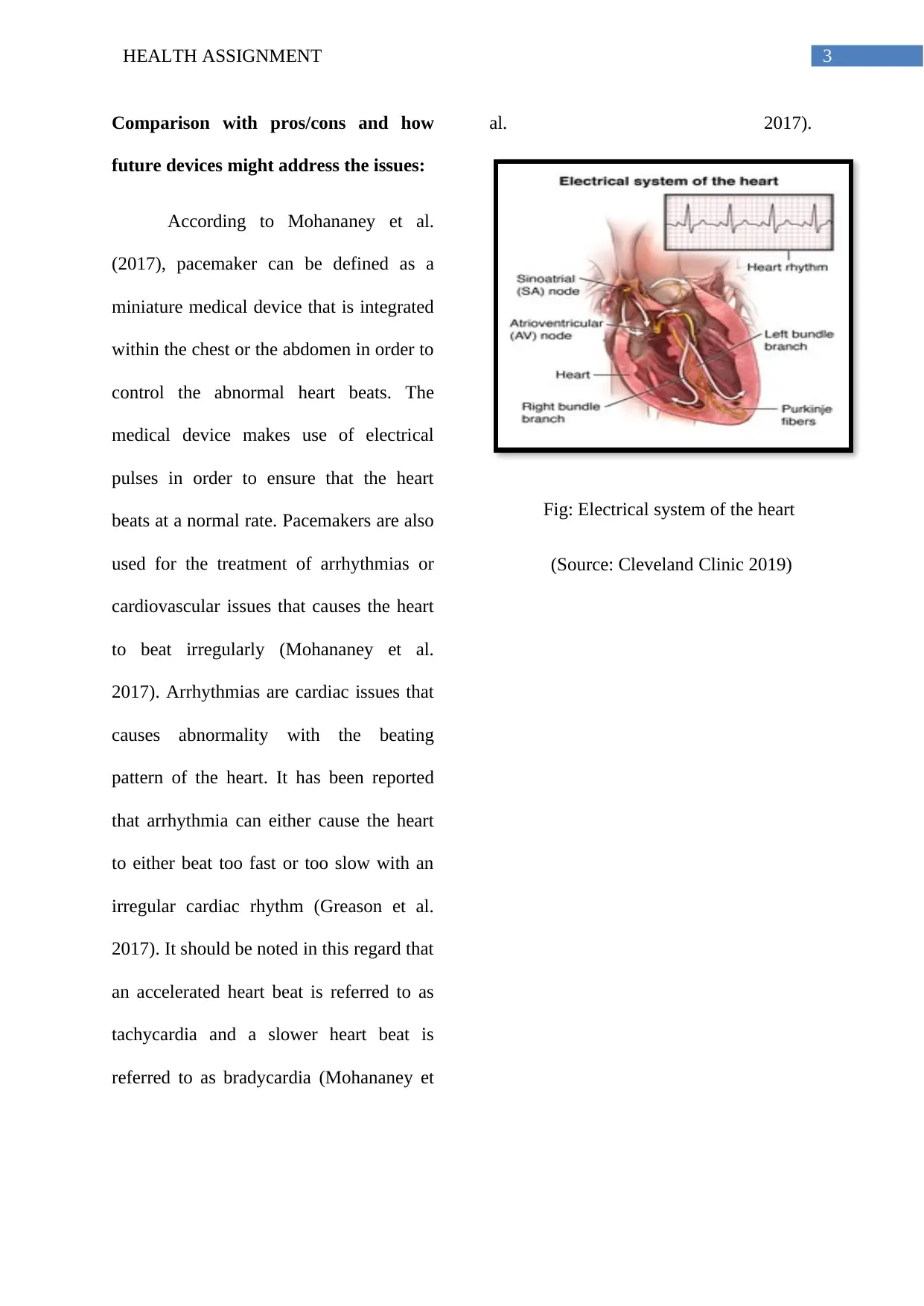
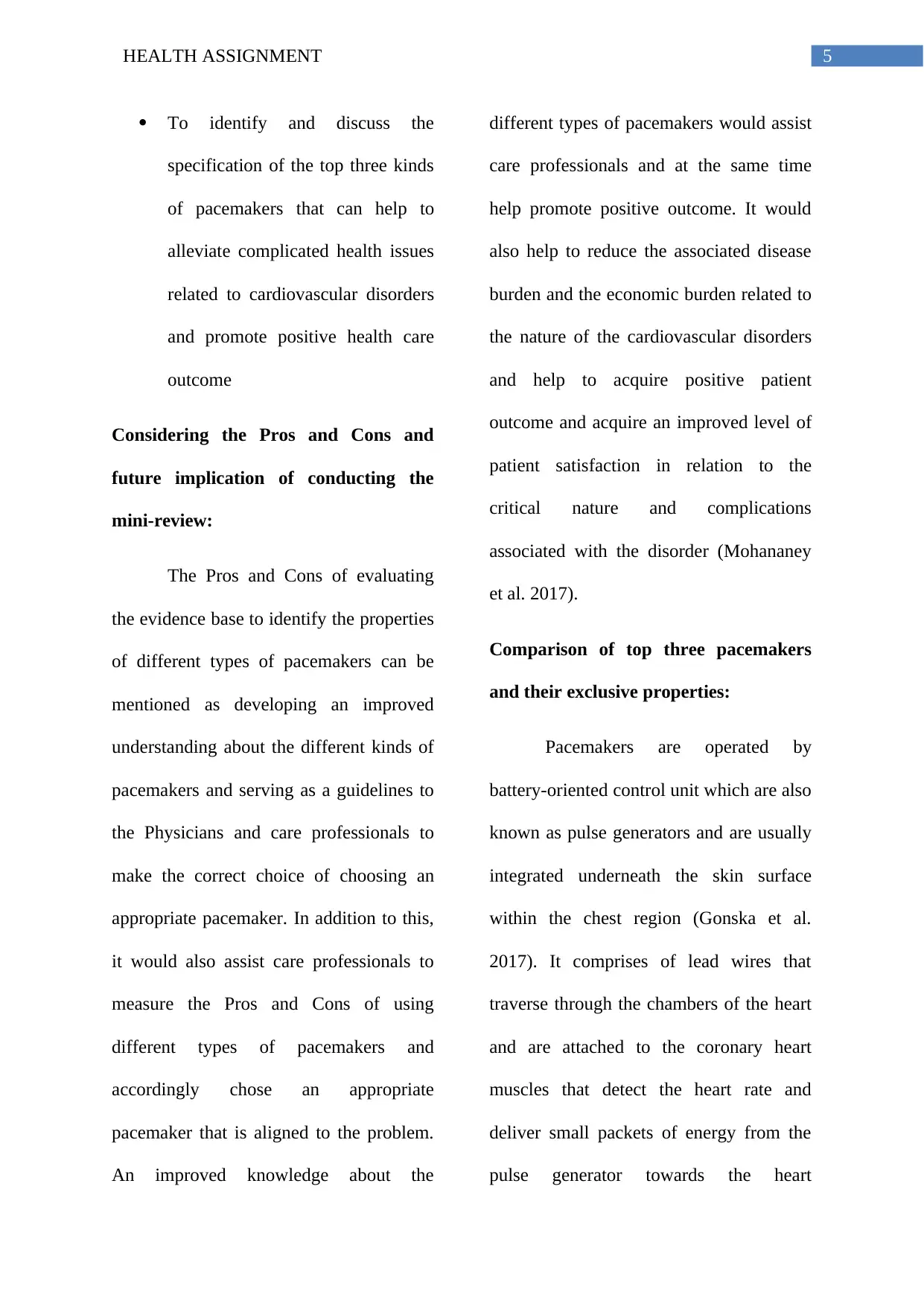
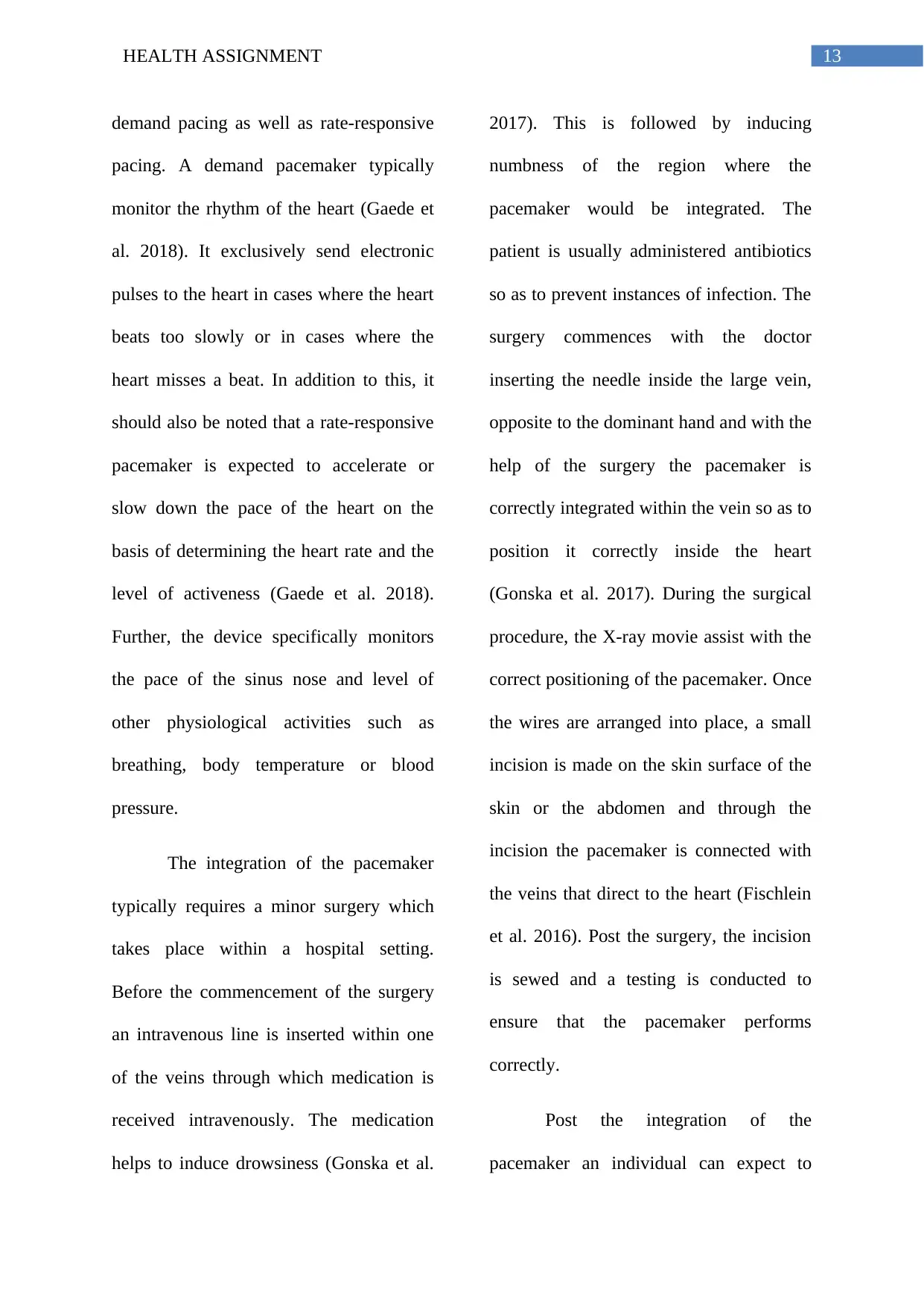
Fig: Electrical system of the heart
(Source: Cleveland Clinic 2019)
Comparison with pros/cons and how
future devices might address the issues:
According to Mohananey et al.
(2017), pacemaker can be defined as a
miniature medical device that is integrated
within the chest or the abdomen in order to
control the abnormal heart beats. The
medical device makes use of electrical
pulses in order to ensure that the heart
beats at a normal rate. Pacemakers are also
used for the treatment of arrhythmias or
cardiovascular issues that causes the heart
to beat irregularly (Mohananey et al.
2017). Arrhythmias are cardiac issues that
causes abnormality with the beating
pattern of the heart. It has been reported
that arrhythmia can either cause the heart
to either beat too fast or too slow with an
irregular cardiac rhythm (Greason et al.
2017). It should be noted in this regard that
an accelerated heart beat is referred to as
tachycardia and a slower heart beat is
referred to as bradycardia (Mohananey et
al. 2017).
Fig: Electrical system of the heart
(Source: Cleveland Clinic 2019)
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4HEALTH ASSIGNMENT
In cases of arrhythmia, the heart
vessels are unable to pump sufficient blood
for the body as a result, the body is
deprived of sufficient blood supply. This
leads to symptoms such as fatigue,
tiredness or even shortness of breath
(Fisclein, Gersak and Pfeiffer 2016). In
addition to this, research studies have
stated that severe intensity of arrhythmia’s
can impair the normal functioning of the
vital organs of the body. This might lead to
unconsciousness or even death. It is in
such case that a pacemaker can alleviate
the symptoms of arrhythmia and effective
treat the symptoms of fatigue or
unconsciousness (Gonska et al. 2017). The
use of pacemaker typically helps to
maintain a normal heart rhythm and assists
a person to lead a normal life style.
However, it should be noted in this context
that the choice of a correct pacemaker is
extremely important as different
cardiovascular issues require the use of
specialised pacemakers that can
appropriately address the ambiguity of the
heart-beat.
Upon evaluation of the evidence
base, a research gap was identified in
terms of a concise stipulated review that
could focus on the different types of
pacemakers that are used in cases of
different cardiovascular disorders. Based
on the retrieved background information,
this mini review intends to address the
articulated research question:
What are the different kinds of
pacemakers that are used to treat
different types of cardiovascular
abnormalities?
On the basis of the articulated
research question, the following research
objectives can be articulated:
To identify the different types of
pacemakers and analyse their
utility in different cardiovascular
disorders
To understand the mechanism of a
pacemaker
In cases of arrhythmia, the heart
vessels are unable to pump sufficient blood
for the body as a result, the body is
deprived of sufficient blood supply. This
leads to symptoms such as fatigue,
tiredness or even shortness of breath
(Fisclein, Gersak and Pfeiffer 2016). In
addition to this, research studies have
stated that severe intensity of arrhythmia’s
can impair the normal functioning of the
vital organs of the body. This might lead to
unconsciousness or even death. It is in
such case that a pacemaker can alleviate
the symptoms of arrhythmia and effective
treat the symptoms of fatigue or
unconsciousness (Gonska et al. 2017). The
use of pacemaker typically helps to
maintain a normal heart rhythm and assists
a person to lead a normal life style.
However, it should be noted in this context
that the choice of a correct pacemaker is
extremely important as different
cardiovascular issues require the use of
specialised pacemakers that can
appropriately address the ambiguity of the
heart-beat.
Upon evaluation of the evidence
base, a research gap was identified in
terms of a concise stipulated review that
could focus on the different types of
pacemakers that are used in cases of
different cardiovascular disorders. Based
on the retrieved background information,
this mini review intends to address the
articulated research question:
What are the different kinds of
pacemakers that are used to treat
different types of cardiovascular
abnormalities?
On the basis of the articulated
research question, the following research
objectives can be articulated:
To identify the different types of
pacemakers and analyse their
utility in different cardiovascular
disorders
To understand the mechanism of a
pacemaker
5HEALTH ASSIGNMENT
To identify and discuss the
specification of the top three kinds
of pacemakers that can help to
alleviate complicated health issues
related to cardiovascular disorders
and promote positive health care
outcome
Considering the Pros and Cons and
future implication of conducting the
mini-review:
The Pros and Cons of evaluating
the evidence base to identify the properties
of different types of pacemakers can be
mentioned as developing an improved
understanding about the different kinds of
pacemakers and serving as a guidelines to
the Physicians and care professionals to
make the correct choice of choosing an
appropriate pacemaker. In addition to this,
it would also assist care professionals to
measure the Pros and Cons of using
different types of pacemakers and
accordingly chose an appropriate
pacemaker that is aligned to the problem.
An improved knowledge about the
different types of pacemakers would assist
care professionals and at the same time
help promote positive outcome. It would
also help to reduce the associated disease
burden and the economic burden related to
the nature of the cardiovascular disorders
and help to acquire positive patient
outcome and acquire an improved level of
patient satisfaction in relation to the
critical nature and complications
associated with the disorder (Mohananey
et al. 2017).
Comparison of top three pacemakers
and their exclusive properties:
Pacemakers are operated by
battery-oriented control unit which are also
known as pulse generators and are usually
integrated underneath the skin surface
within the chest region (Gonska et al.
2017). It comprises of lead wires that
traverse through the chambers of the heart
and are attached to the coronary heart
muscles that detect the heart rate and
deliver small packets of energy from the
pulse generator towards the heart
To identify and discuss the
specification of the top three kinds
of pacemakers that can help to
alleviate complicated health issues
related to cardiovascular disorders
and promote positive health care
outcome
Considering the Pros and Cons and
future implication of conducting the
mini-review:
The Pros and Cons of evaluating
the evidence base to identify the properties
of different types of pacemakers can be
mentioned as developing an improved
understanding about the different kinds of
pacemakers and serving as a guidelines to
the Physicians and care professionals to
make the correct choice of choosing an
appropriate pacemaker. In addition to this,
it would also assist care professionals to
measure the Pros and Cons of using
different types of pacemakers and
accordingly chose an appropriate
pacemaker that is aligned to the problem.
An improved knowledge about the
different types of pacemakers would assist
care professionals and at the same time
help promote positive outcome. It would
also help to reduce the associated disease
burden and the economic burden related to
the nature of the cardiovascular disorders
and help to acquire positive patient
outcome and acquire an improved level of
patient satisfaction in relation to the
critical nature and complications
associated with the disorder (Mohananey
et al. 2017).
Comparison of top three pacemakers
and their exclusive properties:
Pacemakers are operated by
battery-oriented control unit which are also
known as pulse generators and are usually
integrated underneath the skin surface
within the chest region (Gonska et al.
2017). It comprises of lead wires that
traverse through the chambers of the heart
and are attached to the coronary heart
muscles that detect the heart rate and
deliver small packets of energy from the
pulse generator towards the heart
6HEALTH ASSIGNMENT
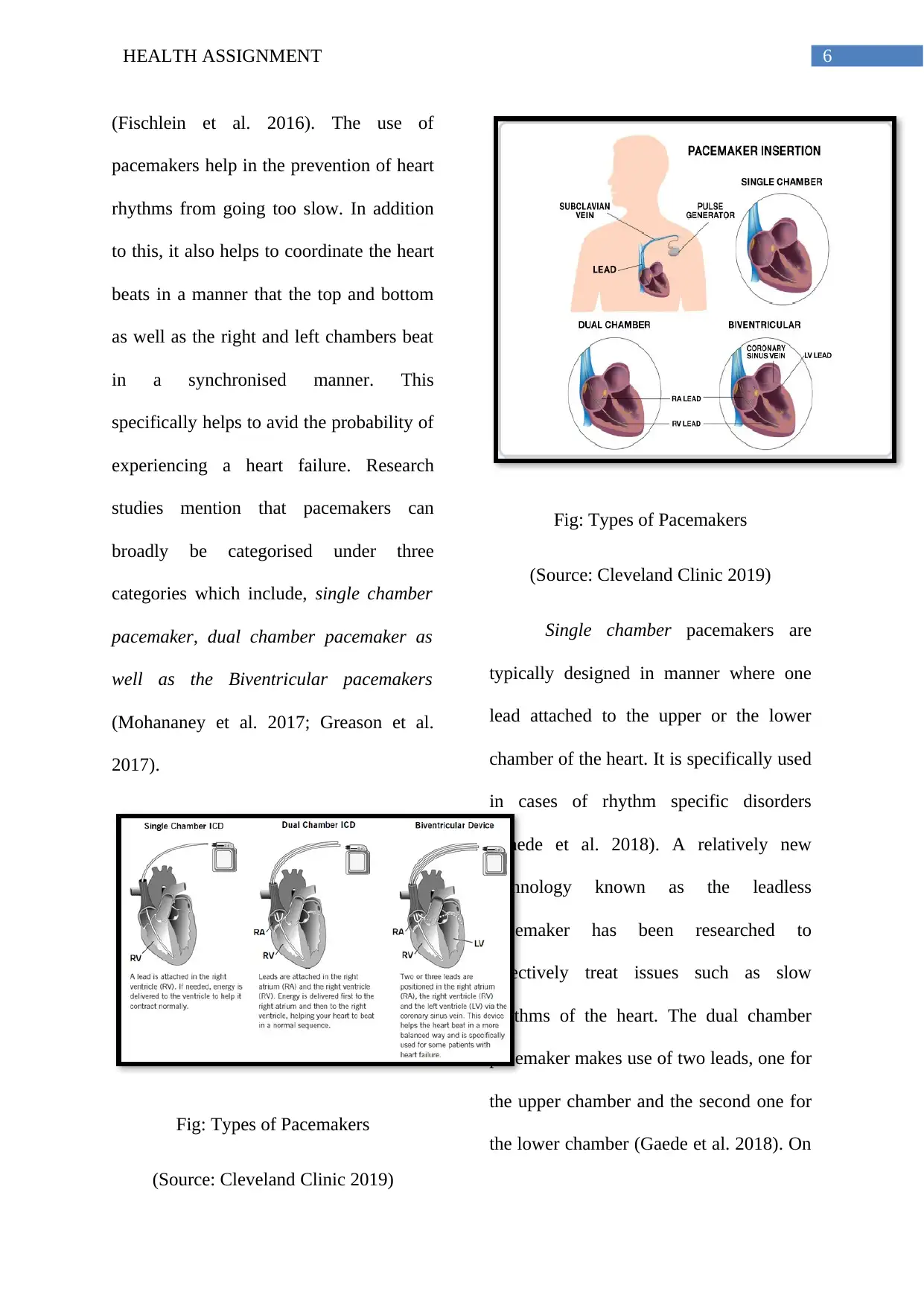
(Fischlein et al. 2016). The use of
pacemakers help in the prevention of heart
rhythms from going too slow. In addition
to this, it also helps to coordinate the heart
beats in a manner that the top and bottom
as well as the right and left chambers beat
in a synchronised manner. This
specifically helps to avid the probability of
experiencing a heart failure. Research
studies mention that pacemakers can
broadly be categorised under three
categories which include, single chamber
pacemaker, dual chamber pacemaker as
well as the Biventricular pacemakers
(Mohananey et al. 2017; Greason et al.
2017).
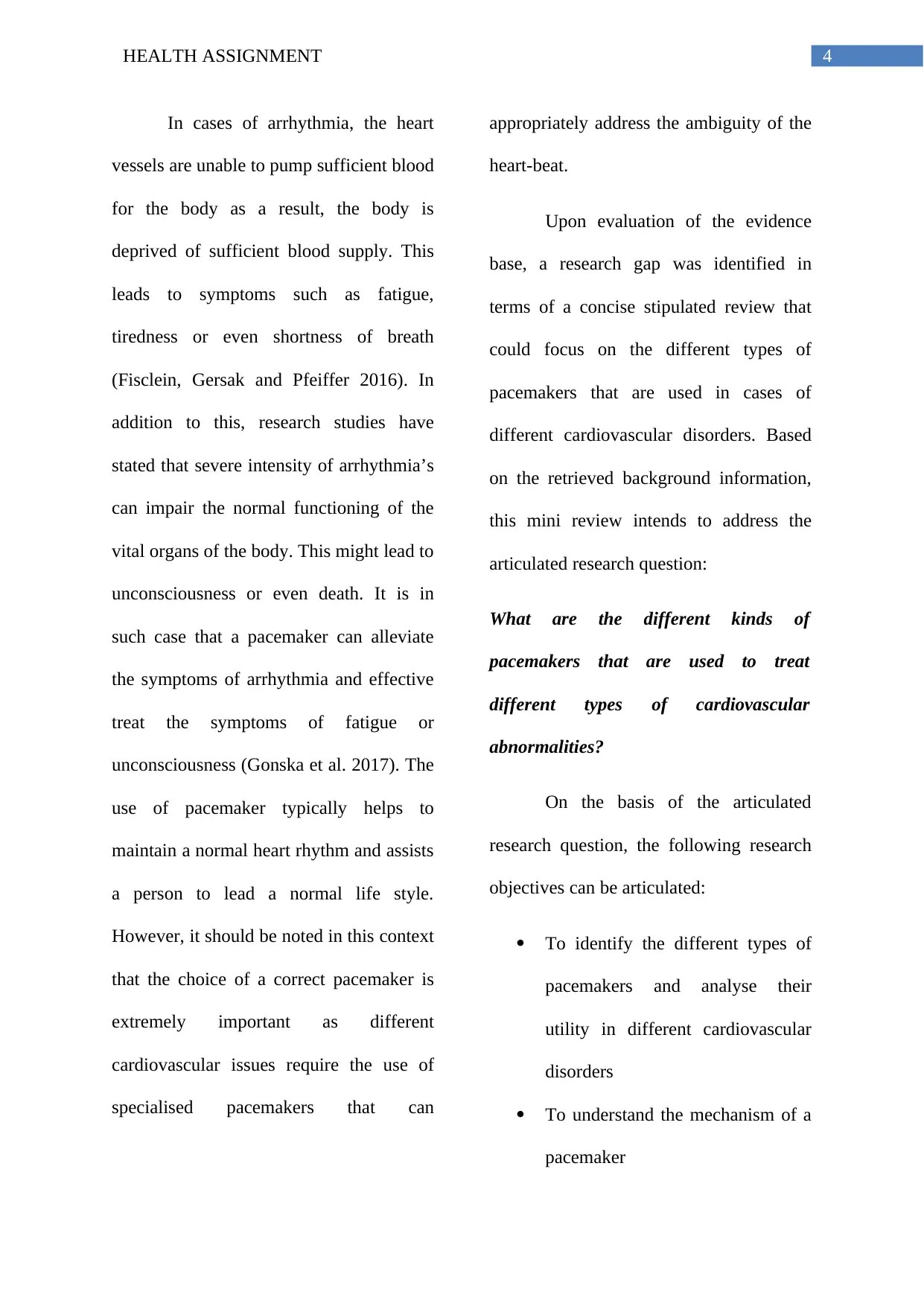
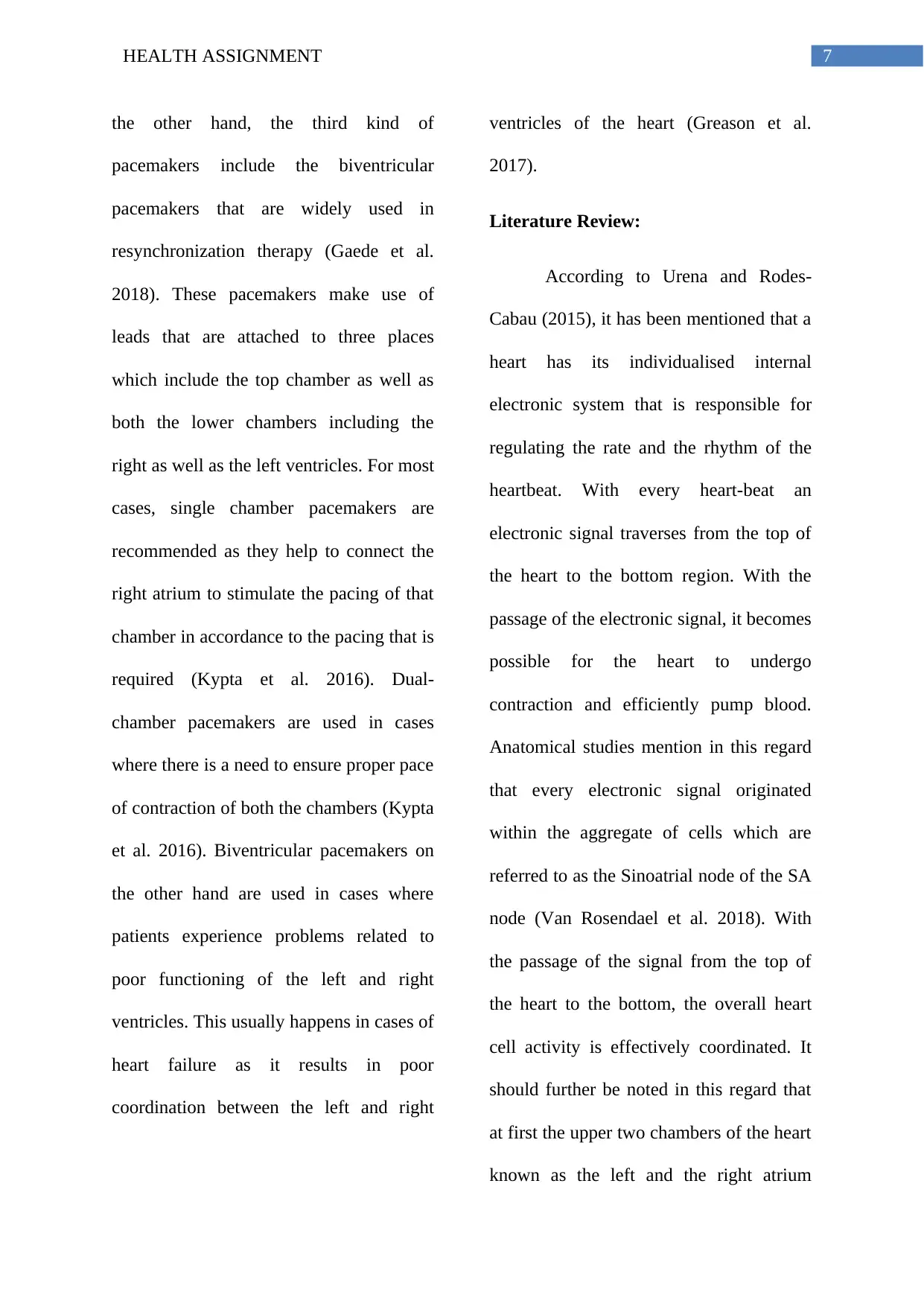
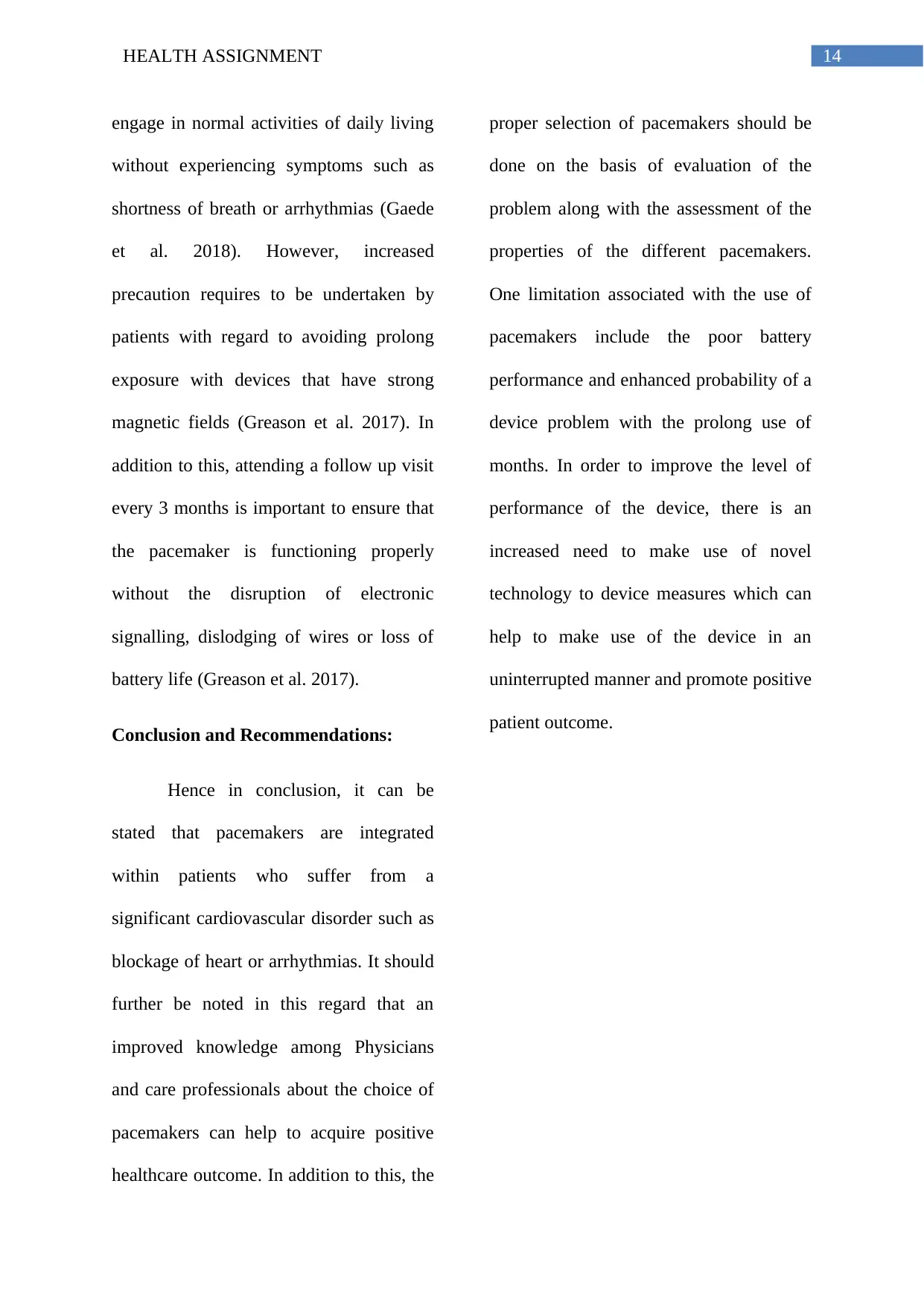
Fig: Types of Pacemakers
(Source: Cleveland Clinic 2019)
Fig: Types of Pacemakers
(Source: Cleveland Clinic 2019)
Single chamber pacemakers are
typically designed in manner where one
lead attached to the upper or the lower
chamber of the heart. It is specifically used
in cases of rhythm specific disorders
(Gaede et al. 2018). A relatively new
technology known as the leadless
pacemaker has been researched to
effectively treat issues such as slow
rhythms of the heart. The dual chamber
pacemaker makes use of two leads, one for
the upper chamber and the second one for
the lower chamber (Gaede et al. 2018). On
(Fischlein et al. 2016). The use of
pacemakers help in the prevention of heart
rhythms from going too slow. In addition
to this, it also helps to coordinate the heart
beats in a manner that the top and bottom
as well as the right and left chambers beat
in a synchronised manner. This
specifically helps to avid the probability of
experiencing a heart failure. Research
studies mention that pacemakers can
broadly be categorised under three
categories which include, single chamber
pacemaker, dual chamber pacemaker as
well as the Biventricular pacemakers
(Mohananey et al. 2017; Greason et al.
2017).
Fig: Types of Pacemakers
(Source: Cleveland Clinic 2019)
Fig: Types of Pacemakers
(Source: Cleveland Clinic 2019)
Single chamber pacemakers are
typically designed in manner where one
lead attached to the upper or the lower
chamber of the heart. It is specifically used
in cases of rhythm specific disorders
(Gaede et al. 2018). A relatively new
technology known as the leadless
pacemaker has been researched to
effectively treat issues such as slow
rhythms of the heart. The dual chamber
pacemaker makes use of two leads, one for
the upper chamber and the second one for
the lower chamber (Gaede et al. 2018). On
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7HEALTH ASSIGNMENT
the other hand, the third kind of
pacemakers include the biventricular
pacemakers that are widely used in
resynchronization therapy (Gaede et al.
2018). These pacemakers make use of
leads that are attached to three places
which include the top chamber as well as
both the lower chambers including the
right as well as the left ventricles. For most
cases, single chamber pacemakers are
recommended as they help to connect the
right atrium to stimulate the pacing of that
chamber in accordance to the pacing that is
required (Kypta et al. 2016). Dual-
chamber pacemakers are used in cases
where there is a need to ensure proper pace
of contraction of both the chambers (Kypta
et al. 2016). Biventricular pacemakers on
the other hand are used in cases where
patients experience problems related to
poor functioning of the left and right
ventricles. This usually happens in cases of
heart failure as it results in poor
coordination between the left and right
ventricles of the heart (Greason et al.
2017).
Literature Review:
According to Urena and Rodes-
Cabau (2015), it has been mentioned that a
heart has its individualised internal
electronic system that is responsible for
regulating the rate and the rhythm of the
heartbeat. With every heart-beat an
electronic signal traverses from the top of
the heart to the bottom region. With the
passage of the electronic signal, it becomes
possible for the heart to undergo
contraction and efficiently pump blood.
Anatomical studies mention in this regard
that every electronic signal originated
within the aggregate of cells which are
referred to as the Sinoatrial node of the SA
node (Van Rosendael et al. 2018). With
the passage of the signal from the top of
the heart to the bottom, the overall heart
cell activity is effectively coordinated. It
should further be noted in this regard that
at first the upper two chambers of the heart
known as the left and the right atrium
the other hand, the third kind of
pacemakers include the biventricular
pacemakers that are widely used in
resynchronization therapy (Gaede et al.
2018). These pacemakers make use of
leads that are attached to three places
which include the top chamber as well as
both the lower chambers including the
right as well as the left ventricles. For most
cases, single chamber pacemakers are
recommended as they help to connect the
right atrium to stimulate the pacing of that
chamber in accordance to the pacing that is
required (Kypta et al. 2016). Dual-
chamber pacemakers are used in cases
where there is a need to ensure proper pace
of contraction of both the chambers (Kypta
et al. 2016). Biventricular pacemakers on
the other hand are used in cases where
patients experience problems related to
poor functioning of the left and right
ventricles. This usually happens in cases of
heart failure as it results in poor
coordination between the left and right
ventricles of the heart (Greason et al.
2017).
Literature Review:
According to Urena and Rodes-
Cabau (2015), it has been mentioned that a
heart has its individualised internal
electronic system that is responsible for
regulating the rate and the rhythm of the
heartbeat. With every heart-beat an
electronic signal traverses from the top of
the heart to the bottom region. With the
passage of the electronic signal, it becomes
possible for the heart to undergo
contraction and efficiently pump blood.
Anatomical studies mention in this regard
that every electronic signal originated
within the aggregate of cells which are
referred to as the Sinoatrial node of the SA
node (Van Rosendael et al. 2018). With
the passage of the signal from the top of
the heart to the bottom, the overall heart
cell activity is effectively coordinated. It
should further be noted in this regard that
at first the upper two chambers of the heart
known as the left and the right atrium
8HEALTH ASSIGNMENT
contract and this leads to the initiation of
the heart activity (Dizon et al. 2015). As a
result of this contraction, the heart pumps
the blood to the lower chambers or the
ventricles of the heart. Upon contraction,
the ventricles pump the blood to different
areas of the body. Therefore, a heartbeat is
a result of the combination of the
contraction of the atria and the ventricles
of the heart (Dizon et al. 2015).
In this regard, it is integral to note
that any faulty electronic signalling of the
heart can lead to arrhythmias. The
pacemakers make use of electronic pulses
that are low in energy so as to overcome
the faulty electronic signalling (Fujita et al.
2016). As a result, this helps to efficiently
improve the functioning of the heartbeat.
According to Fujita et al. (2016),
pacemakers can be used to perform a wide
range of functions such as accelerating or
de-accelerating a heartbeat. Further, it also
helps to control an abnormal or an
accelerated heart rhythm. The use of
pacemakers help to ensure that the atria are
contracting normally in a normal rhythmic
pattern instead of quivering. This condition
is extremely common in cases of atrial
fibrillation. Further, the integration of a
pacemaker in a heart helps to maintain the
effective coordination between the
electronic signalling occurring between the
two chambers of the heart (Vogt et al.
2015). Also, pacemakers help to ensure
that appropriate electronic signalling is
maintained between the two ventricles of
the heart. This is managed by the
pacemakers with the use of the cardiac
resynchronization therapy or the CRT
specialised devices. The evidence base
further suggests that the use of the CRT
devices helps to appropriately treat cardiac
failure (Vogt et al. 2015). Also, the use of
pacemakers help to prevent the occurrence
of arrhythmias that are caused due to long
QT syndrome (Vogt et al. 2015).
According to Maeno et al. (2017),
pacemakers are equipped with the property
to accurately record and monitor the
heartbeat. In fact, pacemakers can
contract and this leads to the initiation of
the heart activity (Dizon et al. 2015). As a
result of this contraction, the heart pumps
the blood to the lower chambers or the
ventricles of the heart. Upon contraction,
the ventricles pump the blood to different
areas of the body. Therefore, a heartbeat is
a result of the combination of the
contraction of the atria and the ventricles
of the heart (Dizon et al. 2015).
In this regard, it is integral to note
that any faulty electronic signalling of the
heart can lead to arrhythmias. The
pacemakers make use of electronic pulses
that are low in energy so as to overcome
the faulty electronic signalling (Fujita et al.
2016). As a result, this helps to efficiently
improve the functioning of the heartbeat.
According to Fujita et al. (2016),
pacemakers can be used to perform a wide
range of functions such as accelerating or
de-accelerating a heartbeat. Further, it also
helps to control an abnormal or an
accelerated heart rhythm. The use of
pacemakers help to ensure that the atria are
contracting normally in a normal rhythmic
pattern instead of quivering. This condition
is extremely common in cases of atrial
fibrillation. Further, the integration of a
pacemaker in a heart helps to maintain the
effective coordination between the
electronic signalling occurring between the
two chambers of the heart (Vogt et al.
2015). Also, pacemakers help to ensure
that appropriate electronic signalling is
maintained between the two ventricles of
the heart. This is managed by the
pacemakers with the use of the cardiac
resynchronization therapy or the CRT
specialised devices. The evidence base
further suggests that the use of the CRT
devices helps to appropriately treat cardiac
failure (Vogt et al. 2015). Also, the use of
pacemakers help to prevent the occurrence
of arrhythmias that are caused due to long
QT syndrome (Vogt et al. 2015).
According to Maeno et al. (2017),
pacemakers are equipped with the property
to accurately record and monitor the
heartbeat. In fact, pacemakers can
9HEALTH ASSIGNMENT
uniquely sense the electrical activity of the
heart and the existing heart rhythm. In
addition to this, it should also be noted that
advanced pacemakers have been designed
that are equipped with the property to
manage and monitor the vital signs of a
patient include, body temperature,
breathing rate, pulse rate or other vital
physiological functions (Maeno et al.
2017). In addition to this, pacemakers are
also equipped with the property to adjust
according the changes of the heart rate.
Research studies mention that depending
upon the utility, pacemakers can either be
temporary or permanent (Regueiro et al.
2016). While temporary pacemakers are
used during emergency conditions or while
treating temporary heart problems such as
slower heart-beat that us caused on
account of complications such as heart
surgery, heart attack or maybe an overdose
of medication. It should be noted in this
regard that the use of a temporary
pacemaker is widely restricted to
emergencies where a temporary condition
requires to be addressed (Regueiro et al.
2016). In cases, where a temporary
pacemaker is used, the patient is made to
stay within the hospital as long as the
temporary condition sustains within the
patient. In most of the cases, after a
temporary condition is tackled, the
physicians proceed with the use of the
permanent pacemakers (Regueiro et al.
2016). Permanent pacemakers are typically
used for the treatment of long-term
problems such as arrhythmias. In this
regard, it should be noted that the certain,
life-threatening arrhythmias are tackled
with the use of ICDs or Implanatable
Cardioverter Defibrillator (Maeno et al.
2017). In this case, it should be noted that
ICDs are similar medical devices as
pacemakers and make use of both low as
well as high electronic impulses in order
stabilise severe arrhythmias (Fadahunsi et
al. 2016).
As stated by Mauri et al. (2016),
pacemakers can be recommended for a
variety of reasons that include heart
uniquely sense the electrical activity of the
heart and the existing heart rhythm. In
addition to this, it should also be noted that
advanced pacemakers have been designed
that are equipped with the property to
manage and monitor the vital signs of a
patient include, body temperature,
breathing rate, pulse rate or other vital
physiological functions (Maeno et al.
2017). In addition to this, pacemakers are
also equipped with the property to adjust
according the changes of the heart rate.
Research studies mention that depending
upon the utility, pacemakers can either be
temporary or permanent (Regueiro et al.
2016). While temporary pacemakers are
used during emergency conditions or while
treating temporary heart problems such as
slower heart-beat that us caused on
account of complications such as heart
surgery, heart attack or maybe an overdose
of medication. It should be noted in this
regard that the use of a temporary
pacemaker is widely restricted to
emergencies where a temporary condition
requires to be addressed (Regueiro et al.
2016). In cases, where a temporary
pacemaker is used, the patient is made to
stay within the hospital as long as the
temporary condition sustains within the
patient. In most of the cases, after a
temporary condition is tackled, the
physicians proceed with the use of the
permanent pacemakers (Regueiro et al.
2016). Permanent pacemakers are typically
used for the treatment of long-term
problems such as arrhythmias. In this
regard, it should be noted that the certain,
life-threatening arrhythmias are tackled
with the use of ICDs or Implanatable
Cardioverter Defibrillator (Maeno et al.
2017). In this case, it should be noted that
ICDs are similar medical devices as
pacemakers and make use of both low as
well as high electronic impulses in order
stabilise severe arrhythmias (Fadahunsi et
al. 2016).
As stated by Mauri et al. (2016),
pacemakers can be recommended for a
variety of reasons that include heart
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10HEALTH ASSIGNMENT
blockage or bradycardia. Bradycardia is a
physiological condition where the
heartbeat is significantly lower than the
normal heart beat (Mauri et al. 2016) On
the other hand, blockage of the heart refers
to the condition where an electronic signal
is slowed down or disrupter as the signal
traverses through the heart. However, it is
essential to note in this regard, a
pacemaker might be recommended by the
physician for multiple other reasons as
well, which primarily include; Ageing
which diminishes the ability of the Sinus
nodes to set an appropriate pace for the
heart to beat appropriately (De Torres-
Alba et al. 2016). Such cases causes
slowing down of the heart-beat or gives
rise to long pauses between the heartbeats.
This gives rise to sick sinus syndrome and
can only be treated with the help of a
pacemaker. A pacemaker is widely
recommended in cases of atrial fibrillation
or arrhythmias. A pacemaker can also be
recommended in case of tackling the side
effect of consuming excessive beta
blockers that causes the slowing down of
the pace of the heart- beat (Reddy et al.
2015). In addition to this, pacemakers are
also recommended to patients that suffer
from long QT syndrome or experience a
loss of function of the artery that is
responsible for supplying the blood to the
brain from the heart and traverses through
the neck. In addition to this, patients who
suffer from a congenital heart disease or
undergo heart transplant surgeries are also
recommended to use pacemakers (Vogt et
al. 2015).
Prior to recommending a
pacemaker, few diagnostic tests are
ordered which help to evaluate the level of
arrhythmias. These diagnostic tests
include, an electrocardiogram,
echocardiography, Stress test, Holter and
Event Monitors as well as
Electrophysiology Study (Reddy et al.
2015). An electrocardiogram or an EKG is
known as a painless diagnostic tests that
helps to record the electric activity of the
heart. The test helps to assess the
blockage or bradycardia. Bradycardia is a
physiological condition where the
heartbeat is significantly lower than the
normal heart beat (Mauri et al. 2016) On
the other hand, blockage of the heart refers
to the condition where an electronic signal
is slowed down or disrupter as the signal
traverses through the heart. However, it is
essential to note in this regard, a
pacemaker might be recommended by the
physician for multiple other reasons as
well, which primarily include; Ageing
which diminishes the ability of the Sinus
nodes to set an appropriate pace for the
heart to beat appropriately (De Torres-
Alba et al. 2016). Such cases causes
slowing down of the heart-beat or gives
rise to long pauses between the heartbeats.
This gives rise to sick sinus syndrome and
can only be treated with the help of a
pacemaker. A pacemaker is widely
recommended in cases of atrial fibrillation
or arrhythmias. A pacemaker can also be
recommended in case of tackling the side
effect of consuming excessive beta
blockers that causes the slowing down of
the pace of the heart- beat (Reddy et al.
2015). In addition to this, pacemakers are
also recommended to patients that suffer
from long QT syndrome or experience a
loss of function of the artery that is
responsible for supplying the blood to the
brain from the heart and traverses through
the neck. In addition to this, patients who
suffer from a congenital heart disease or
undergo heart transplant surgeries are also
recommended to use pacemakers (Vogt et
al. 2015).
Prior to recommending a
pacemaker, few diagnostic tests are
ordered which help to evaluate the level of
arrhythmias. These diagnostic tests
include, an electrocardiogram,
echocardiography, Stress test, Holter and
Event Monitors as well as
Electrophysiology Study (Reddy et al.
2015). An electrocardiogram or an EKG is
known as a painless diagnostic tests that
helps to record the electric activity of the
heart. The test helps to assess the
11HEALTH ASSIGNMENT
steadiness or irregularity of the heart. The
test effectively helps to diagnose ab heart
block or a bradycardia (Reddy et al. 2015).
A Holter monitor is a wearable device that
typically documents the activity of the
heart for a period of 24 to 48 hours (Nazif
et al. 2015). The device helps to record the
activity of the heart for a longer duration
that the standard EKG test.
Echocardiography on the other hand
makes use of sound waves to create a
motion picture of the heart (Nazif et al.
2015). The test effectively shows the shape
as well as the size of the heart and that the
heart chambers as well as the valves are
efficiently working. In addition to this, an
echocardiogram also shows the areas that
receive poor supply of blood or areas that
do not contract normally (Mauri et al.
2016). It also helps to detect injuries to the
heart muscles that are caused on account
of poor blood flow. Further,
electrophysiology study test involves the
integration of flexible wire through a vein
in the groin area to the arm of the heart
(Fadahunsi et al. 2016). The wire is
responsible for recording the signals of the
heart. The wire is stimulated by the
physician which in order to track the
response of the heart to the induced
electrical impulse. Stress test includes
tracking the activity of heart while
performing a physically strenuous activity
(Fadahunsi et al. 2016). In such condition
a medicine could be administered to the
patient in order to elevate the heart beat
and record the same so as ti develop a
better understanding about the abnormality
of the heart-beat (Fadahunsi et al. 2016).
Research studies mention that a
pacemaker comprises of a battery and a
computerized generator that has wires and
sensors at the tip (Maeno et al. 2017; Vogt
et al. 2015). The sensors are referred to as
the electrodes and the battery that powers
to operate the generator is encased in a thin
metallic box. The wires effectively help to
connect the generator to the heart. The
pacemaker is widely responsible for
monitoring and regulating the heartbeat.
steadiness or irregularity of the heart. The
test effectively helps to diagnose ab heart
block or a bradycardia (Reddy et al. 2015).
A Holter monitor is a wearable device that
typically documents the activity of the
heart for a period of 24 to 48 hours (Nazif
et al. 2015). The device helps to record the
activity of the heart for a longer duration
that the standard EKG test.
Echocardiography on the other hand
makes use of sound waves to create a
motion picture of the heart (Nazif et al.
2015). The test effectively shows the shape
as well as the size of the heart and that the
heart chambers as well as the valves are
efficiently working. In addition to this, an
echocardiogram also shows the areas that
receive poor supply of blood or areas that
do not contract normally (Mauri et al.
2016). It also helps to detect injuries to the
heart muscles that are caused on account
of poor blood flow. Further,
electrophysiology study test involves the
integration of flexible wire through a vein
in the groin area to the arm of the heart
(Fadahunsi et al. 2016). The wire is
responsible for recording the signals of the
heart. The wire is stimulated by the
physician which in order to track the
response of the heart to the induced
electrical impulse. Stress test includes
tracking the activity of heart while
performing a physically strenuous activity
(Fadahunsi et al. 2016). In such condition
a medicine could be administered to the
patient in order to elevate the heart beat
and record the same so as ti develop a
better understanding about the abnormality
of the heart-beat (Fadahunsi et al. 2016).
Research studies mention that a
pacemaker comprises of a battery and a
computerized generator that has wires and
sensors at the tip (Maeno et al. 2017; Vogt
et al. 2015). The sensors are referred to as
the electrodes and the battery that powers
to operate the generator is encased in a thin
metallic box. The wires effectively help to
connect the generator to the heart. The
pacemaker is widely responsible for
monitoring and regulating the heartbeat.
12HEALTH ASSIGNMENT
The electrodes effectively detect the
electronic activity of the heart and
transmits data by means of the wires to the
integrated circuit within the generator
(Fujita et al. 2016).
In cases where the heart rhythm is
abnormal the integrated circuit would
signal the generator to transmit electronic
impulses to the heart. This would ensure
that the pulses travel through the wires to
reach towards the heart. It should be noted
in this regard that the use of new
pacemakers have been studied to regulate
the vital functions along with the heart
rhythm as well as the electrical activity of
the heart (Van Rosendael et al. 2018). The
obtained readings would be used to
effectively adjust the pacemakers in order
to ensure improved outcome.
The evidence base further stated
that pacemakers typically possess one or
three wires that are uniquely placed within
the different chambers of the heart. The
wires integrated within the single chamber
pacemaker are responsible for carrying
pulses from the generator to the right
ventricle of the heart that is situated within
the lower right hand side chamber of the
heart (Dizon et al. 2015). The wires
present within a dual-chamber pacemaker
carries the pulses from the generator to the
right atrium which is also considered as
the upper right chamber of the heart. These
pulses typically facilitate improved
coordination between the contraction of
the right atrium and the right ventricle
(Urena and Rodes-Cabau 2015). In case of
a biventricular pacemaker, the wires are
responsible for carrying pulses from the
generator to one atrium as well as to the
both ventricles (Kypta et al. 2016). The
pulses typically help to coordinate the
electrical signalling in between the two
ventricles. This kind of pacemaker is
popularly referred to as the
resynchronization therapy or the CRT
device (Mohananey et al. 2017).
Research studies mention in this
regard that the two major types of
programming for pacemakers require
The electrodes effectively detect the
electronic activity of the heart and
transmits data by means of the wires to the
integrated circuit within the generator
(Fujita et al. 2016).
In cases where the heart rhythm is
abnormal the integrated circuit would
signal the generator to transmit electronic
impulses to the heart. This would ensure
that the pulses travel through the wires to
reach towards the heart. It should be noted
in this regard that the use of new
pacemakers have been studied to regulate
the vital functions along with the heart
rhythm as well as the electrical activity of
the heart (Van Rosendael et al. 2018). The
obtained readings would be used to
effectively adjust the pacemakers in order
to ensure improved outcome.
The evidence base further stated
that pacemakers typically possess one or
three wires that are uniquely placed within
the different chambers of the heart. The
wires integrated within the single chamber
pacemaker are responsible for carrying
pulses from the generator to the right
ventricle of the heart that is situated within
the lower right hand side chamber of the
heart (Dizon et al. 2015). The wires
present within a dual-chamber pacemaker
carries the pulses from the generator to the
right atrium which is also considered as
the upper right chamber of the heart. These
pulses typically facilitate improved
coordination between the contraction of
the right atrium and the right ventricle
(Urena and Rodes-Cabau 2015). In case of
a biventricular pacemaker, the wires are
responsible for carrying pulses from the
generator to one atrium as well as to the
both ventricles (Kypta et al. 2016). The
pulses typically help to coordinate the
electrical signalling in between the two
ventricles. This kind of pacemaker is
popularly referred to as the
resynchronization therapy or the CRT
device (Mohananey et al. 2017).
Research studies mention in this
regard that the two major types of
programming for pacemakers require
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13HEALTH ASSIGNMENT
demand pacing as well as rate-responsive
pacing. A demand pacemaker typically
monitor the rhythm of the heart (Gaede et
al. 2018). It exclusively send electronic
pulses to the heart in cases where the heart
beats too slowly or in cases where the
heart misses a beat. In addition to this, it
should also be noted that a rate-responsive
pacemaker is expected to accelerate or
slow down the pace of the heart on the
basis of determining the heart rate and the
level of activeness (Gaede et al. 2018).
Further, the device specifically monitors
the pace of the sinus nose and level of
other physiological activities such as
breathing, body temperature or blood
pressure.
The integration of the pacemaker
typically requires a minor surgery which
takes place within a hospital setting.
Before the commencement of the surgery
an intravenous line is inserted within one
of the veins through which medication is
received intravenously. The medication
helps to induce drowsiness (Gonska et al.
2017). This is followed by inducing
numbness of the region where the
pacemaker would be integrated. The
patient is usually administered antibiotics
so as to prevent instances of infection. The
surgery commences with the doctor
inserting the needle inside the large vein,
opposite to the dominant hand and with the
help of the surgery the pacemaker is
correctly integrated within the vein so as to
position it correctly inside the heart
(Gonska et al. 2017). During the surgical
procedure, the X-ray movie assist with the
correct positioning of the pacemaker. Once
the wires are arranged into place, a small
incision is made on the skin surface of the
skin or the abdomen and through the
incision the pacemaker is connected with
the veins that direct to the heart (Fischlein
et al. 2016). Post the surgery, the incision
is sewed and a testing is conducted to
ensure that the pacemaker performs
correctly.
Post the integration of the
pacemaker an individual can expect to
demand pacing as well as rate-responsive
pacing. A demand pacemaker typically
monitor the rhythm of the heart (Gaede et
al. 2018). It exclusively send electronic
pulses to the heart in cases where the heart
beats too slowly or in cases where the
heart misses a beat. In addition to this, it
should also be noted that a rate-responsive
pacemaker is expected to accelerate or
slow down the pace of the heart on the
basis of determining the heart rate and the
level of activeness (Gaede et al. 2018).
Further, the device specifically monitors
the pace of the sinus nose and level of
other physiological activities such as
breathing, body temperature or blood
pressure.
The integration of the pacemaker
typically requires a minor surgery which
takes place within a hospital setting.
Before the commencement of the surgery
an intravenous line is inserted within one
of the veins through which medication is
received intravenously. The medication
helps to induce drowsiness (Gonska et al.
2017). This is followed by inducing
numbness of the region where the
pacemaker would be integrated. The
patient is usually administered antibiotics
so as to prevent instances of infection. The
surgery commences with the doctor
inserting the needle inside the large vein,
opposite to the dominant hand and with the
help of the surgery the pacemaker is
correctly integrated within the vein so as to
position it correctly inside the heart
(Gonska et al. 2017). During the surgical
procedure, the X-ray movie assist with the
correct positioning of the pacemaker. Once
the wires are arranged into place, a small
incision is made on the skin surface of the
skin or the abdomen and through the
incision the pacemaker is connected with
the veins that direct to the heart (Fischlein
et al. 2016). Post the surgery, the incision
is sewed and a testing is conducted to
ensure that the pacemaker performs
correctly.
Post the integration of the
pacemaker an individual can expect to
14HEALTH ASSIGNMENT
engage in normal activities of daily living
without experiencing symptoms such as
shortness of breath or arrhythmias (Gaede
et al. 2018). However, increased
precaution requires to be undertaken by
patients with regard to avoiding prolong
exposure with devices that have strong
magnetic fields (Greason et al. 2017). In
addition to this, attending a follow up visit
every 3 months is important to ensure that
the pacemaker is functioning properly
without the disruption of electronic
signalling, dislodging of wires or loss of
battery life (Greason et al. 2017).
Conclusion and Recommendations:
Hence in conclusion, it can be
stated that pacemakers are integrated
within patients who suffer from a
significant cardiovascular disorder such as
blockage of heart or arrhythmias. It should
further be noted in this regard that an
improved knowledge among Physicians
and care professionals about the choice of
pacemakers can help to acquire positive
healthcare outcome. In addition to this, the
proper selection of pacemakers should be
done on the basis of evaluation of the
problem along with the assessment of the
properties of the different pacemakers.
One limitation associated with the use of
pacemakers include the poor battery
performance and enhanced probability of a
device problem with the prolong use of
months. In order to improve the level of
performance of the device, there is an
increased need to make use of novel
technology to device measures which can
help to make use of the device in an
uninterrupted manner and promote positive
patient outcome.
engage in normal activities of daily living
without experiencing symptoms such as
shortness of breath or arrhythmias (Gaede
et al. 2018). However, increased
precaution requires to be undertaken by
patients with regard to avoiding prolong
exposure with devices that have strong
magnetic fields (Greason et al. 2017). In
addition to this, attending a follow up visit
every 3 months is important to ensure that
the pacemaker is functioning properly
without the disruption of electronic
signalling, dislodging of wires or loss of
battery life (Greason et al. 2017).
Conclusion and Recommendations:
Hence in conclusion, it can be
stated that pacemakers are integrated
within patients who suffer from a
significant cardiovascular disorder such as
blockage of heart or arrhythmias. It should
further be noted in this regard that an
improved knowledge among Physicians
and care professionals about the choice of
pacemakers can help to acquire positive
healthcare outcome. In addition to this, the
proper selection of pacemakers should be
done on the basis of evaluation of the
problem along with the assessment of the
properties of the different pacemakers.
One limitation associated with the use of
pacemakers include the poor battery
performance and enhanced probability of a
device problem with the prolong use of
months. In order to improve the level of
performance of the device, there is an
increased need to make use of novel
technology to device measures which can
help to make use of the device in an
uninterrupted manner and promote positive
patient outcome.
15HEALTH ASSIGNMENT
References:
Cleveland Clinic (2019). Implantable
Cardioverter Defibrillator (ICD) |
Cleveland clinic. [online] Cleveland
Clinic. Available at:
https://my.clevelandclinic.org/health/treat
ments/17123-implantable-cardioverter-
defibrillator-icd [Accessed 2 Sep. 2019].
De Torres-Alba, F., Kaleschke, G., Diller,
G.P., Vormbrock, J., Orwat, S., Radke, R.,
Reinke, F., Fischer, D., Reinecke, H. and
Baumgartner, H., 2016. Changes in the
pacemaker rate after transition from
Edwards SAPIEN XT to SAPIEN 3
transcatheter aortic valve implantation: the
critical role of valve implantation
height. JACC: Cardiovascular
Interventions, 9(8), pp.805-813.
Dizon, J.M., Nazif, T.M., Hess, P.L.,
Biviano, A., Garan, H., Douglas, P.S.,
Kapadia, S., Babaliaros, V., Herrmann,
H.C., Szeto, W.Y. and Jilaihawi, H., 2015.
Chronic pacing and adverse outcomes after
transcatheter aortic valve
implantation. Heart, 101(20), pp.1665-
1671.
Fadahunsi, O.O., Olowoyeye, A.,
Ukaigwe, A., Li, Z., Vora, A.N.,
Vemulapalli, S., Elgin, E. and Donato, A.,
2016. Incidence, predictors, and outcomes
of permanent pacemaker implantation
following transcatheter aortic valve
replacement: analysis from the US Society
of Thoracic Surgeons/American College of
Cardiology TVT Registry. JACC:
Cardiovascular Interventions, 9(21),
pp.2189-2199.
Fischlein, T., Gersak, B. and Pfeiffer, S.,
2016. How to prevent a pacemaker
implantation after sutureless
bioprosthesis. The Journal of thoracic and
cardiovascular surgery, 152(2), pp.635-
636.
Fujita, B., Kütting, M., Seiffert, M.,
Scholtz, S., Egron, S., Prashovikj, E.,
Börgermann, J., Schäfer, T., Scholtz, W.,
Preuss, R. and Gummert, J., 2016.
Calcium distribution patterns of the aortic
References:
Cleveland Clinic (2019). Implantable
Cardioverter Defibrillator (ICD) |
Cleveland clinic. [online] Cleveland
Clinic. Available at:
https://my.clevelandclinic.org/health/treat
ments/17123-implantable-cardioverter-
defibrillator-icd [Accessed 2 Sep. 2019].
De Torres-Alba, F., Kaleschke, G., Diller,
G.P., Vormbrock, J., Orwat, S., Radke, R.,
Reinke, F., Fischer, D., Reinecke, H. and
Baumgartner, H., 2016. Changes in the
pacemaker rate after transition from
Edwards SAPIEN XT to SAPIEN 3
transcatheter aortic valve implantation: the
critical role of valve implantation
height. JACC: Cardiovascular
Interventions, 9(8), pp.805-813.
Dizon, J.M., Nazif, T.M., Hess, P.L.,
Biviano, A., Garan, H., Douglas, P.S.,
Kapadia, S., Babaliaros, V., Herrmann,
H.C., Szeto, W.Y. and Jilaihawi, H., 2015.
Chronic pacing and adverse outcomes after
transcatheter aortic valve
implantation. Heart, 101(20), pp.1665-
1671.
Fadahunsi, O.O., Olowoyeye, A.,
Ukaigwe, A., Li, Z., Vora, A.N.,
Vemulapalli, S., Elgin, E. and Donato, A.,
2016. Incidence, predictors, and outcomes
of permanent pacemaker implantation
following transcatheter aortic valve
replacement: analysis from the US Society
of Thoracic Surgeons/American College of
Cardiology TVT Registry. JACC:
Cardiovascular Interventions, 9(21),
pp.2189-2199.
Fischlein, T., Gersak, B. and Pfeiffer, S.,
2016. How to prevent a pacemaker
implantation after sutureless
bioprosthesis. The Journal of thoracic and
cardiovascular surgery, 152(2), pp.635-
636.
Fujita, B., Kütting, M., Seiffert, M.,
Scholtz, S., Egron, S., Prashovikj, E.,
Börgermann, J., Schäfer, T., Scholtz, W.,
Preuss, R. and Gummert, J., 2016.
Calcium distribution patterns of the aortic
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
16HEALTH ASSIGNMENT
valve as a risk factor for the need of
permanent pacemaker implantation after
transcatheter aortic valve
implantation. European Journal of
Echocardiography, 17(12), pp.1385-1393.
Gaede, L., Kim, W.K., Liebetrau, C., Dörr,
O., Sperzel, J., Blumenstein, J.,
Berkowitsch, A., Walther, T., Hamm, C.,
Elsässer, A. and Nef, H., 2018. Pacemaker
implantation after TAVI: predictors of AV
block persistence. Clinical Research in
Cardiology, 107(1), pp.60-69.
Gonska, B., Seeger, J., Keßler, M., von
Keil, A., Rottbauer, W. and Wöhrle, J.,
2017. Predictors for permanent pacemaker
implantation in patients undergoing
transfemoral aortic valve implantation with
the Edwards Sapien 3 valve. Clinical
Research in Cardiology, 106(8), pp.590-
597.
Greason, K.L., Lahr, B.D., Stulak, J.M.,
Cha, Y.M., Rea, R.F., Schaff, H.V. and
Dearani, J.A., 2017. Long-term mortality
effect of early pacemaker implantation
after surgical aortic valve
replacement. The Annals of thoracic
surgery, 104(4), pp.1259-1264.
Kypta, A., Blessberger, H., Kammler, J.,
Lambert, T., Lichtenauer, M.,
Brandstaetter, W., Gabriel, M. and
Steinwender, C., 2016. Leadless cardiac
pacemaker implantation after lead
extraction in patients with severe device
infection. Journal of cardiovascular
electrophysiology, 27(9), pp.1067-1071.
Maeno, Y., Abramowitz, Y., Kawamori,
H., Kazuno, Y., Kubo, S., Takahashi, N.,
Mangat, G., Okuyama, K., Kashif, M.,
Chakravarty, T. and Nakamura, M., 2017.
A highly predictive risk model for
pacemaker implantation after
TAVR. JACC: Cardiovascular
Imaging, 10(10 Part A), pp.1139-1147.
Mauri, V., Reimann, A., Stern, D.,
Scherner, M., Kuhn, E., Rudolph, V.,
Rosenkranz, S., Eghbalzadeh, K.,
Friedrichs, K., Wahlers, T. and Baldus, S.,
2016. Predictors of permanent pacemaker
valve as a risk factor for the need of
permanent pacemaker implantation after
transcatheter aortic valve
implantation. European Journal of
Echocardiography, 17(12), pp.1385-1393.
Gaede, L., Kim, W.K., Liebetrau, C., Dörr,
O., Sperzel, J., Blumenstein, J.,
Berkowitsch, A., Walther, T., Hamm, C.,
Elsässer, A. and Nef, H., 2018. Pacemaker
implantation after TAVI: predictors of AV
block persistence. Clinical Research in
Cardiology, 107(1), pp.60-69.
Gonska, B., Seeger, J., Keßler, M., von
Keil, A., Rottbauer, W. and Wöhrle, J.,
2017. Predictors for permanent pacemaker
implantation in patients undergoing
transfemoral aortic valve implantation with
the Edwards Sapien 3 valve. Clinical
Research in Cardiology, 106(8), pp.590-
597.
Greason, K.L., Lahr, B.D., Stulak, J.M.,
Cha, Y.M., Rea, R.F., Schaff, H.V. and
Dearani, J.A., 2017. Long-term mortality
effect of early pacemaker implantation
after surgical aortic valve
replacement. The Annals of thoracic
surgery, 104(4), pp.1259-1264.
Kypta, A., Blessberger, H., Kammler, J.,
Lambert, T., Lichtenauer, M.,
Brandstaetter, W., Gabriel, M. and
Steinwender, C., 2016. Leadless cardiac
pacemaker implantation after lead
extraction in patients with severe device
infection. Journal of cardiovascular
electrophysiology, 27(9), pp.1067-1071.
Maeno, Y., Abramowitz, Y., Kawamori,
H., Kazuno, Y., Kubo, S., Takahashi, N.,
Mangat, G., Okuyama, K., Kashif, M.,
Chakravarty, T. and Nakamura, M., 2017.
A highly predictive risk model for
pacemaker implantation after
TAVR. JACC: Cardiovascular
Imaging, 10(10 Part A), pp.1139-1147.
Mauri, V., Reimann, A., Stern, D.,
Scherner, M., Kuhn, E., Rudolph, V.,
Rosenkranz, S., Eghbalzadeh, K.,
Friedrichs, K., Wahlers, T. and Baldus, S.,
2016. Predictors of permanent pacemaker
17HEALTH ASSIGNMENT
implantation after transcatheter aortic
valve replacement with the SAPIEN
3. JACC: Cardiovascular
Interventions, 9(21), pp.2200-2209.
Mohananey, D., Jobanputra, Y., Kumar,
A., Krishnaswamy, A., Mick, S., White,
J.M. and Kapadia, S.R., 2017. Clinical and
echocardiographic outcomes following
permanent pacemaker implantation after
transcatheter aortic valve replacement:
meta-analysis and meta-
regression. Circulation: Cardiovascular
Interventions, 10(7), p.e005046.
Nazif, T.M., Dizon, J.M., Hahn, R.T., Xu,
K., Babaliaros, V., Douglas, P.S., El-
Chami, M.F., Herrmann, H.C., Mack, M.,
Makkar, R.R. and Miller, D.C., 2015.
Predictors and clinical outcomes of
permanent pacemaker implantation after
transcatheter aortic valve replacement: the
PARTNER (Placement of AoRtic
TraNscathetER Valves) trial and
registry. JACC: Cardiovascular
Interventions, 8(1 Part A), pp.60-69.
Reddy, V.Y., Exner, D.V., Cantillon, D.J.,
Doshi, R., Bunch, T.J., Tomassoni, G.F.,
Friedman, P.A., Estes III, N.M., Ip, J.,
Niazi, I. and Plunkitt, K., 2015.
Percutaneous implantation of an entirely
intracardiac leadless pacemaker. New
England Journal of Medicine, 373(12),
pp.1125-1135.
Regueiro, A., Abdul-Jawad Altisent, O.,
Del Trigo, M., Campelo-Parada, F., Puri,
R., Urena, M., Philippon, F. and Rodés-
Cabau, J., 2016. Impact of new-onset left
bundle branch block and periprocedural
permanent pacemaker implantation on
clinical outcomes in patients undergoing
transcatheter aortic valve replacement: a
systematic review and meta-
analysis. Circulation: Cardiovascular
Interventions, 9(5), p.e003635.
Sahle, B.W., Owen, A.J., Mutowo, M.P.,
Krum, H. and Reid, C.M., 2016.
Prevalence of heart failure in Australia: a
systematic review. BMC cardiovascular
disorders, 16(1), p.32.
implantation after transcatheter aortic
valve replacement with the SAPIEN
3. JACC: Cardiovascular
Interventions, 9(21), pp.2200-2209.
Mohananey, D., Jobanputra, Y., Kumar,
A., Krishnaswamy, A., Mick, S., White,
J.M. and Kapadia, S.R., 2017. Clinical and
echocardiographic outcomes following
permanent pacemaker implantation after
transcatheter aortic valve replacement:
meta-analysis and meta-
regression. Circulation: Cardiovascular
Interventions, 10(7), p.e005046.
Nazif, T.M., Dizon, J.M., Hahn, R.T., Xu,
K., Babaliaros, V., Douglas, P.S., El-
Chami, M.F., Herrmann, H.C., Mack, M.,
Makkar, R.R. and Miller, D.C., 2015.
Predictors and clinical outcomes of
permanent pacemaker implantation after
transcatheter aortic valve replacement: the
PARTNER (Placement of AoRtic
TraNscathetER Valves) trial and
registry. JACC: Cardiovascular
Interventions, 8(1 Part A), pp.60-69.
Reddy, V.Y., Exner, D.V., Cantillon, D.J.,
Doshi, R., Bunch, T.J., Tomassoni, G.F.,
Friedman, P.A., Estes III, N.M., Ip, J.,
Niazi, I. and Plunkitt, K., 2015.
Percutaneous implantation of an entirely
intracardiac leadless pacemaker. New
England Journal of Medicine, 373(12),
pp.1125-1135.
Regueiro, A., Abdul-Jawad Altisent, O.,
Del Trigo, M., Campelo-Parada, F., Puri,
R., Urena, M., Philippon, F. and Rodés-
Cabau, J., 2016. Impact of new-onset left
bundle branch block and periprocedural
permanent pacemaker implantation on
clinical outcomes in patients undergoing
transcatheter aortic valve replacement: a
systematic review and meta-
analysis. Circulation: Cardiovascular
Interventions, 9(5), p.e003635.
Sahle, B.W., Owen, A.J., Mutowo, M.P.,
Krum, H. and Reid, C.M., 2016.
Prevalence of heart failure in Australia: a
systematic review. BMC cardiovascular
disorders, 16(1), p.32.

18HEALTH ASSIGNMENT
Urena, M. and Rodes-Cabau, J., 2015.
Managing heart block after transcatheter
aortic valve implantation: from monitoring
to device selection and pacemaker
indications. EuroIntervention: journal of
EuroPCR in collaboration with the
Working Group on Interventional
Cardiology of the European Society of
Cardiology, 11, pp.W101-5.
Van Rosendael, P.J., Delgado, V. and Bax,
J.J., 2018. Pacemaker implantation rate
after transcatheter aortic valve
implantation with early and new-
generation devices: a systematic
review. European heart journal, 39(21),
pp.2003-2013.
Vogt, F., Pfeiffer, S., Dell'Aquila, A.M.,
Fischlein, T. and Santarpino, G., 2015.
Sutureless aortic valve replacement with
Perceval bioprosthesis: are there predicting
factors for postoperative pacemaker
implantation?. Interactive cardiovascular
and thoracic surgery, 22(3), pp.253-258.
www.health.gov.au (2019). Department of
Health | Cardiovascular disease. [online]
Www1.health.gov.au. Available at:
https://www1.health.gov.au/internet/main/
publishing.nsf/Content/chronic-cardio
[Accessed 2 Sep. 2019].
Urena, M. and Rodes-Cabau, J., 2015.
Managing heart block after transcatheter
aortic valve implantation: from monitoring
to device selection and pacemaker
indications. EuroIntervention: journal of
EuroPCR in collaboration with the
Working Group on Interventional
Cardiology of the European Society of
Cardiology, 11, pp.W101-5.
Van Rosendael, P.J., Delgado, V. and Bax,
J.J., 2018. Pacemaker implantation rate
after transcatheter aortic valve
implantation with early and new-
generation devices: a systematic
review. European heart journal, 39(21),
pp.2003-2013.
Vogt, F., Pfeiffer, S., Dell'Aquila, A.M.,
Fischlein, T. and Santarpino, G., 2015.
Sutureless aortic valve replacement with
Perceval bioprosthesis: are there predicting
factors for postoperative pacemaker
implantation?. Interactive cardiovascular
and thoracic surgery, 22(3), pp.253-258.
www.health.gov.au (2019). Department of
Health | Cardiovascular disease. [online]
Www1.health.gov.au. Available at:
https://www1.health.gov.au/internet/main/
publishing.nsf/Content/chronic-cardio
[Accessed 2 Sep. 2019].
1 out of 19
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





