Health Care
VerifiedAdded on 2023/04/21
|18
|4403
|234
AI Summary
This document discusses the public health problems related to smoking and the interventions for smoking prevention. It highlights the needs and priorities for smoking prevention in the UK, sets aims and objectives, and discusses the methods and interventions for smoking prevention. It also evaluates the evidence-based approaches and resources required for implementation, and provides an analysis of critical factors for successful intervention.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: HEALTH CARE
Health Care
Name of the Student
Name of the University
Author Note
Health Care
Name of the Student
Name of the University
Author Note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1
HEALTH CARE
Context and Overview of the Public Health Problems
The use of tobacco is common throughout the world in spite of being a leading cause
behind the development of a number of chronic diseases like cancer, pulmonary disease and
cardio-vascular diseases (1). According to the Public Health England ,smoking is a leading
cause of the preventable illness and premature death in England (2). During the tenure of
2016, around 78,000 deaths occurred in England and it is attributable to smoking. This
presents 16% of all deaths occurring in the UK. The adult smoking in England however have
decline during the progression of the year. For example, at the of year 2017 recorded 14.9%
of the adult smoking in England (18 years and above) and this amounted to 6.1 million
people in comparison to 16% smoking rates in 2016. Though this percentage is still alarming
but keeping into consideration this rate of decrease in smoking, it can be concluded that the
by the end of 2023, the rate of smoking along the adults might get reduced to a permissible
range that is 8.5% to 11.7%. Public Health England is vouching for long term smoking
prevention plan by the end of 2030 under the collaboration of NHS in order to reduced the
smoking rate among adult by 5% (2). According to the reports published by the Surgeon
General during 2010, there is no low limit of tobacco smoking and there are no so-called safe
tobacco products. Centers for Disease Control and Prevention (2010) are of the opinion both
active and passive smoking leads to the development of cardiovascular complications. The
“tar phase” and the “gas phase of the cigarette hampers the inter-action of the cardio-vascular
and the pulmonary pathways giving rise to several complications [2]. Smoking during the
early phase of life also leads to the development of the pulmonary complications like
development of the asthmatic attack during the later stages of life. Smoking of tobacco also
increases the pre-disposition of developing type-2 diabetes mellitus (4). The decrease in the
overall rate of smoking in England is mainly successful among the middle and high income
HEALTH CARE
Context and Overview of the Public Health Problems
The use of tobacco is common throughout the world in spite of being a leading cause
behind the development of a number of chronic diseases like cancer, pulmonary disease and
cardio-vascular diseases (1). According to the Public Health England ,smoking is a leading
cause of the preventable illness and premature death in England (2). During the tenure of
2016, around 78,000 deaths occurred in England and it is attributable to smoking. This
presents 16% of all deaths occurring in the UK. The adult smoking in England however have
decline during the progression of the year. For example, at the of year 2017 recorded 14.9%
of the adult smoking in England (18 years and above) and this amounted to 6.1 million
people in comparison to 16% smoking rates in 2016. Though this percentage is still alarming
but keeping into consideration this rate of decrease in smoking, it can be concluded that the
by the end of 2023, the rate of smoking along the adults might get reduced to a permissible
range that is 8.5% to 11.7%. Public Health England is vouching for long term smoking
prevention plan by the end of 2030 under the collaboration of NHS in order to reduced the
smoking rate among adult by 5% (2). According to the reports published by the Surgeon
General during 2010, there is no low limit of tobacco smoking and there are no so-called safe
tobacco products. Centers for Disease Control and Prevention (2010) are of the opinion both
active and passive smoking leads to the development of cardiovascular complications. The
“tar phase” and the “gas phase of the cigarette hampers the inter-action of the cardio-vascular
and the pulmonary pathways giving rise to several complications [2]. Smoking during the
early phase of life also leads to the development of the pulmonary complications like
development of the asthmatic attack during the later stages of life. Smoking of tobacco also
increases the pre-disposition of developing type-2 diabetes mellitus (4). The decrease in the
overall rate of smoking in England is mainly successful among the middle and high income
2
HEALTH CARE
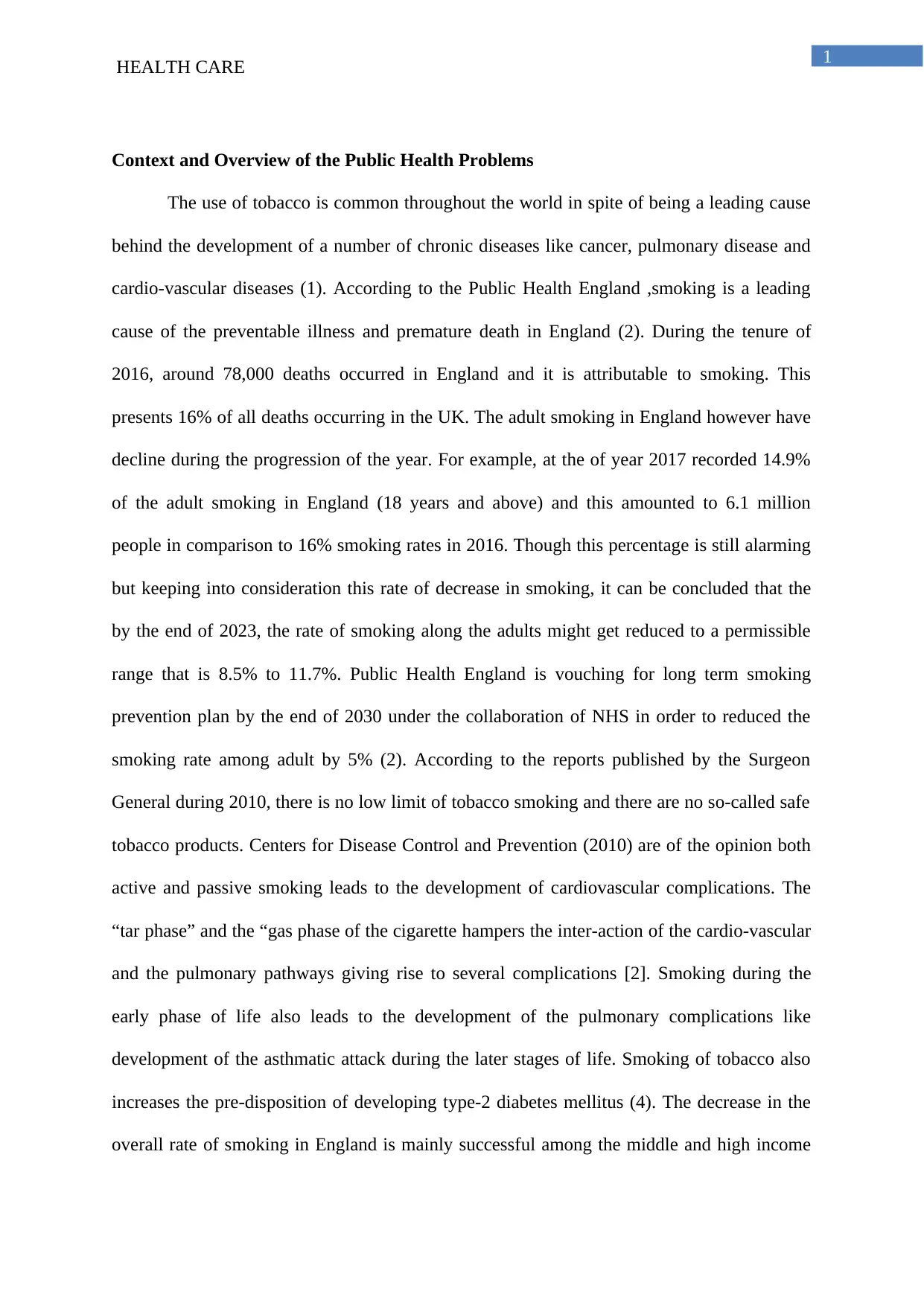
groups. Thus increase in the health-inequalities is the main socio-economic cause behind the
increase in the rate of smoking from the low income groups (4). According to the World
Health Organisation (WHO) poor socio-economic condition shape up the money, power and
the availability of the resources at the national or the local levels and this lead to increase in
the tendency of smoking among the adults to hails from the low socio-economic groups (4).
The survey done by the Office of the National Statistics showed that smoking varies with the
socio-economic status like people who earn daily wages or are unemployed are more
addicted towards smoking (5). Moreover, illiterate people are more prone towards
uncontrollable smoking in comparison to the educated adults.
(Source: Office of the National Health Statistics 2018)
HEALTH CARE
groups. Thus increase in the health-inequalities is the main socio-economic cause behind the
increase in the rate of smoking from the low income groups (4). According to the World
Health Organisation (WHO) poor socio-economic condition shape up the money, power and
the availability of the resources at the national or the local levels and this lead to increase in
the tendency of smoking among the adults to hails from the low socio-economic groups (4).
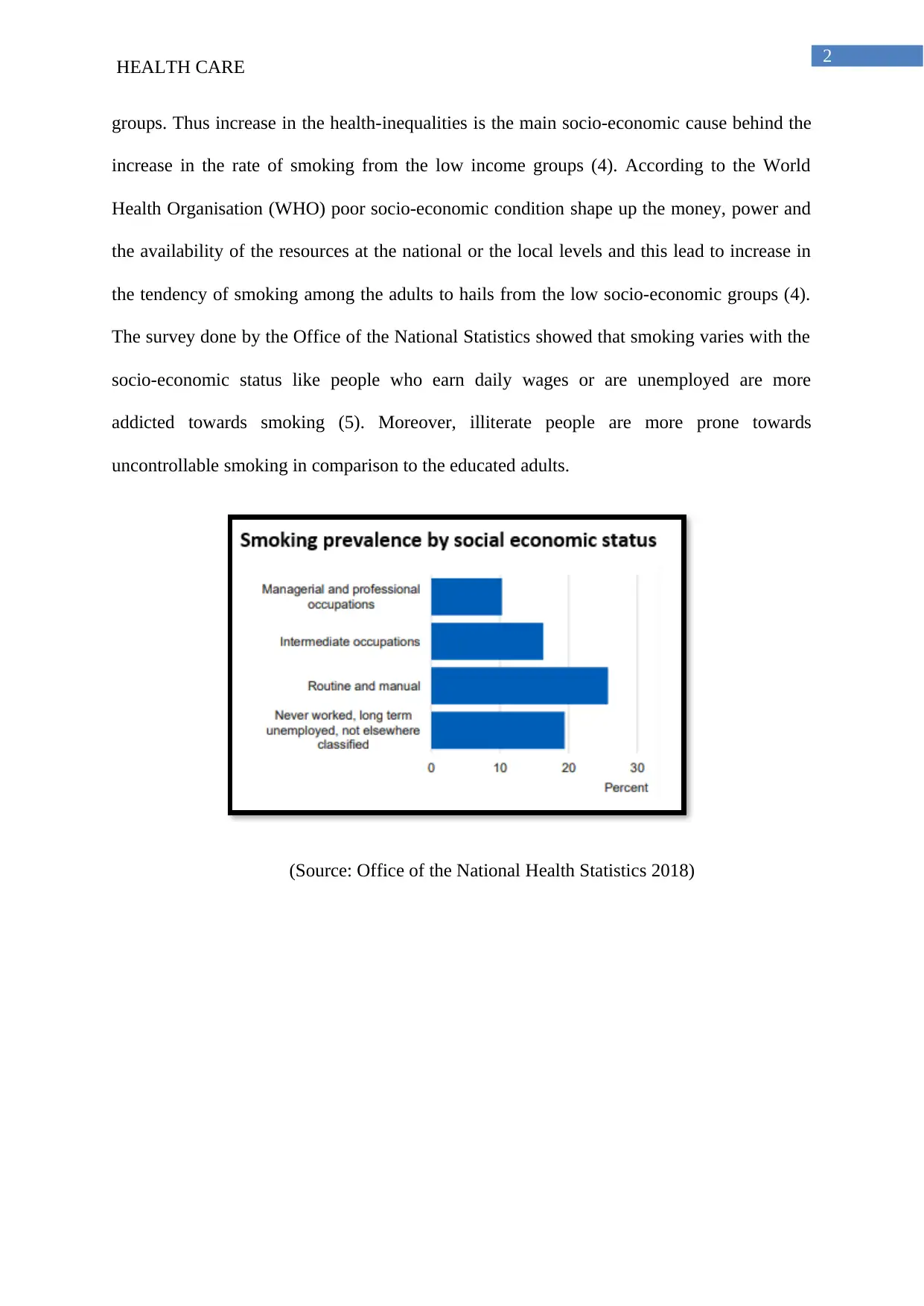
The survey done by the Office of the National Statistics showed that smoking varies with the
socio-economic status like people who earn daily wages or are unemployed are more
addicted towards smoking (5). Moreover, illiterate people are more prone towards
uncontrollable smoking in comparison to the educated adults.
(Source: Office of the National Health Statistics 2018)
3
HEALTH CARE
(Source: Office of the National Health Statistics 2018)
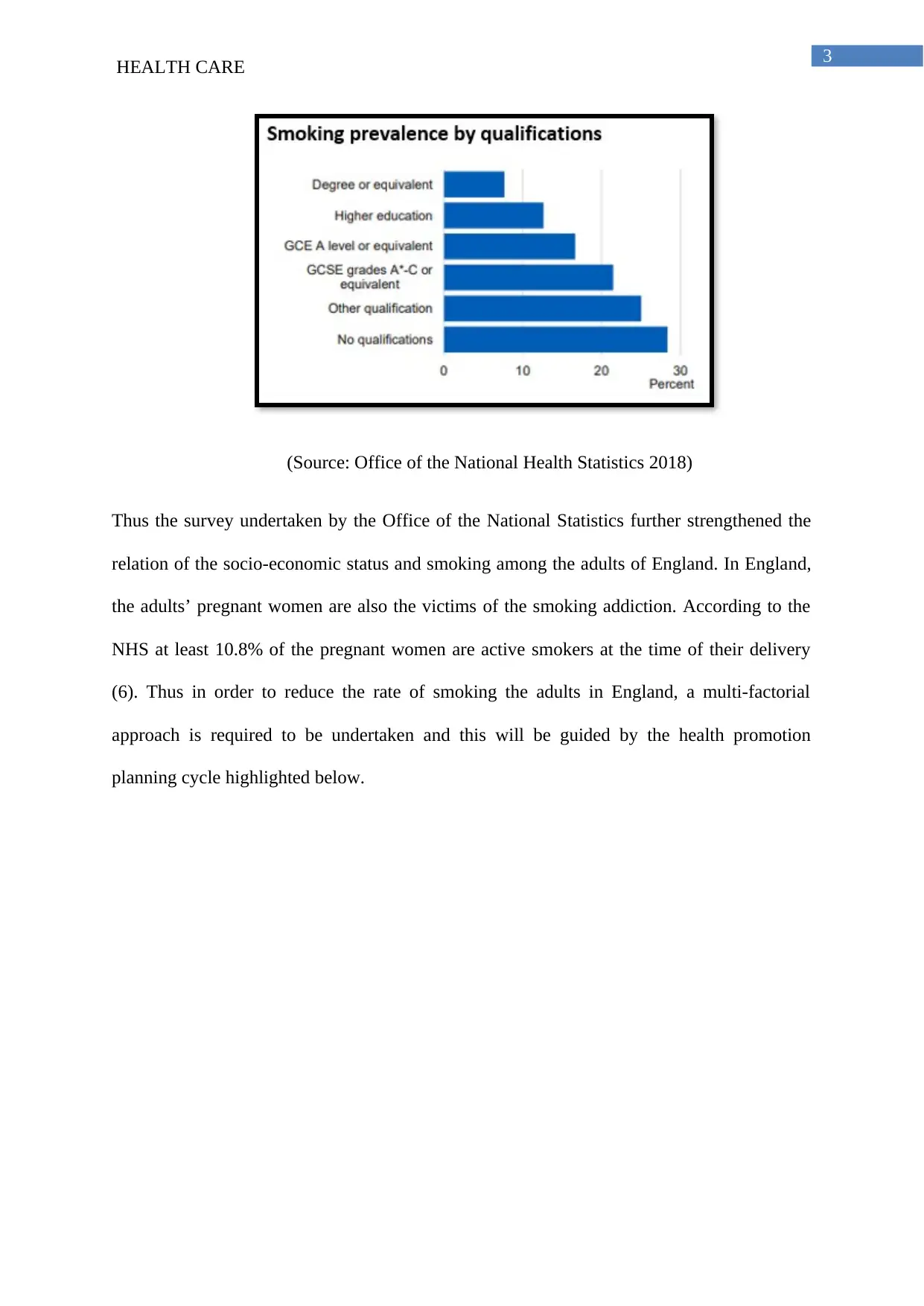
Thus the survey undertaken by the Office of the National Statistics further strengthened the
relation of the socio-economic status and smoking among the adults of England. In England,
the adults’ pregnant women are also the victims of the smoking addiction. According to the
NHS at least 10.8% of the pregnant women are active smokers at the time of their delivery
(6). Thus in order to reduce the rate of smoking the adults in England, a multi-factorial
approach is required to be undertaken and this will be guided by the health promotion
planning cycle highlighted below.
HEALTH CARE
(Source: Office of the National Health Statistics 2018)
Thus the survey undertaken by the Office of the National Statistics further strengthened the
relation of the socio-economic status and smoking among the adults of England. In England,
the adults’ pregnant women are also the victims of the smoking addiction. According to the
NHS at least 10.8% of the pregnant women are active smokers at the time of their delivery
(6). Thus in order to reduce the rate of smoking the adults in England, a multi-factorial
approach is required to be undertaken and this will be guided by the health promotion
planning cycle highlighted below.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4
HEALTH CARE
Health Promotion Planning
(Source: Grosios, Gahan and Burbidge 2010)
Section: B: Plan for the Smoking Prevention Intervention
Needs and Priorities
The main needs and priorities of the smoking prevention in the UK is the reduction in
the health-equalities at the socio-economic level in order to reduce the level of high level of
smoking among the people who belongs to the socio-economically backward group. The
second priority of the smoking reduction is restricting the young adults to indulge in the
intoxication in smoking. The third priority of the smoking prevention is decreasing the
smoking tendency among the pregnant women and thereby reducing adverse pregnancy
related outcome. The forth priority is increasing he smoking related awareness among the
mass through community level approach (2).
HEALTH CARE
Health Promotion Planning
(Source: Grosios, Gahan and Burbidge 2010)
Section: B: Plan for the Smoking Prevention Intervention
Needs and Priorities
The main needs and priorities of the smoking prevention in the UK is the reduction in
the health-equalities at the socio-economic level in order to reduce the level of high level of
smoking among the people who belongs to the socio-economically backward group. The
second priority of the smoking reduction is restricting the young adults to indulge in the
intoxication in smoking. The third priority of the smoking prevention is decreasing the
smoking tendency among the pregnant women and thereby reducing adverse pregnancy
related outcome. The forth priority is increasing he smoking related awareness among the
mass through community level approach (2).
5
HEALTH CARE
Setting Aims and Objectives
Thus the main aim for the health promotion intervention to reduce the prevalence of
smoking among adults of England is to reduce the smoking related ill-health.
The main objectives include
To increase public awareness regarding the consequences of smoking
To promote smoking cessation among smokers aged 18 years and older in England
Attitude changes regarding the consequences of smoking
Methods and Interventions
In order to increase the public health awareness towards smoking and to reduce the
addiction towards smoking both behavioural and the pharmacological approaches must be
taken under prime consideration. Stead and Lancaster conducted a systematic review in order
to analyze the effectiveness of the pharmacotherapy and behavioural interventions for the
prevention of smoking. The main behavioural approach that was taken under consideration
for this systematic review was brief advice and thorough counselling and pharmacotherapy
selected was nicotine replacement therapy and therapy by bupropion and varenicline(7). The
review also aims towards identifying the size f the treatment effect with various combinations
and under different healthcare and population settings. Stead and Lancaster mainly selected
randomised control trails and quasi-randomised control trails for the conduction of the
systematic review (7). The trails with the focus group o the pregnant women and the young
adults were mainly included in the study with six months of follow-up. The analysis of the
results highlighted that the combination of the behavioural and the pharmacological
intervention is effective in reducing the tendency of smoking in comparison to single
approach. However, the behavioural support must be provided by trained professionals in
four to eight sessions for duration of 30 minutes.
HEALTH CARE
Setting Aims and Objectives
Thus the main aim for the health promotion intervention to reduce the prevalence of
smoking among adults of England is to reduce the smoking related ill-health.
The main objectives include
To increase public awareness regarding the consequences of smoking
To promote smoking cessation among smokers aged 18 years and older in England
Attitude changes regarding the consequences of smoking
Methods and Interventions
In order to increase the public health awareness towards smoking and to reduce the
addiction towards smoking both behavioural and the pharmacological approaches must be
taken under prime consideration. Stead and Lancaster conducted a systematic review in order
to analyze the effectiveness of the pharmacotherapy and behavioural interventions for the
prevention of smoking. The main behavioural approach that was taken under consideration
for this systematic review was brief advice and thorough counselling and pharmacotherapy
selected was nicotine replacement therapy and therapy by bupropion and varenicline(7). The
review also aims towards identifying the size f the treatment effect with various combinations
and under different healthcare and population settings. Stead and Lancaster mainly selected
randomised control trails and quasi-randomised control trails for the conduction of the
systematic review (7). The trails with the focus group o the pregnant women and the young
adults were mainly included in the study with six months of follow-up. The analysis of the
results highlighted that the combination of the behavioural and the pharmacological
intervention is effective in reducing the tendency of smoking in comparison to single
approach. However, the behavioural support must be provided by trained professionals in
four to eight sessions for duration of 30 minutes.
6
HEALTH CARE
Cahill et al. conducted the meta-analysis in order analyze the effectiveness of the
combination of the different pharmacological technologies towards the prevention of the
smoking. The pharmacological interventions which are selected for the study are nicotine
replacement therapy (NRT), anti-depressants (nortriptyline and bupropion), nicotine receptor
partial agonists (cytosine and varenicline), caanbinoid receptor antagonists, anxiolytics,
dianicline, lobeline and other nicotine vaccines (9). The main focus groups who are taken
under the prime focus for the analysis of the effectiveness of the intervention included
pregnant women. The meta-analysis was conducted from 267 studies with 12 different
treatments. The analysis of the results by the meta-analysis highlighted that NRT bupropion,
cystisine and varenicline are found to improve the overall condition of prevention of
smoking. The effectiveness increases with combination was done with NRT and varenicline.
Nortriptyline also shown to produce positive improvements in increasing the tendency of
quitting smoke along with the reduction of the withdrawal effects (9).
Lancaster and Stead conducted a review with an objective to study how individual
counselling promotes smoking cessation in comparison to no treatment. The study also
attempted to compare how individual counselling is effective than self-help material and less
intensive interventions towards promotion of the smoking cessation (8). The review was
undertaken by specific selection of the randomised control trails and quasi-randomised trials
where one intervention was face-to-face interview or counselling and no routine clinical care
along with a follow-up of 6 months. 49 trials were identified with around 19,00 participants.
The analysis of the results concluded that individually-delivered smoking cessation
counselling can help the chain smokers to quit smoking. The evidenced-based practise
suggested that for the best benefit the individual face-to-face counselling must be coupled
with proper pharmacotherapy in order to accelerates the overall outcome (8).
HEALTH CARE
Cahill et al. conducted the meta-analysis in order analyze the effectiveness of the
combination of the different pharmacological technologies towards the prevention of the
smoking. The pharmacological interventions which are selected for the study are nicotine
replacement therapy (NRT), anti-depressants (nortriptyline and bupropion), nicotine receptor
partial agonists (cytosine and varenicline), caanbinoid receptor antagonists, anxiolytics,
dianicline, lobeline and other nicotine vaccines (9). The main focus groups who are taken
under the prime focus for the analysis of the effectiveness of the intervention included
pregnant women. The meta-analysis was conducted from 267 studies with 12 different
treatments. The analysis of the results by the meta-analysis highlighted that NRT bupropion,
cystisine and varenicline are found to improve the overall condition of prevention of
smoking. The effectiveness increases with combination was done with NRT and varenicline.
Nortriptyline also shown to produce positive improvements in increasing the tendency of
quitting smoke along with the reduction of the withdrawal effects (9).
Lancaster and Stead conducted a review with an objective to study how individual
counselling promotes smoking cessation in comparison to no treatment. The study also
attempted to compare how individual counselling is effective than self-help material and less
intensive interventions towards promotion of the smoking cessation (8). The review was
undertaken by specific selection of the randomised control trails and quasi-randomised trials
where one intervention was face-to-face interview or counselling and no routine clinical care
along with a follow-up of 6 months. 49 trials were identified with around 19,00 participants.
The analysis of the results concluded that individually-delivered smoking cessation
counselling can help the chain smokers to quit smoking. The evidenced-based practise
suggested that for the best benefit the individual face-to-face counselling must be coupled
with proper pharmacotherapy in order to accelerates the overall outcome (8).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
HEALTH CARE
Evidence Based Evaluation
The review of the literature and the evidence based approach highlighted that the
combination of both face-to-face counselling and pharmacotherapy is effective in inflicting
the tendency of quitting the smoking habits by overcoming the withdrawal symptoms.
Similar approach was highlighted in the guidelines published by the National Institute of
Care and Excellence (NICE)(10). As per the NICE guidelines, which is based on the
systematic review of different studies the combination of the pharmaco-therapy and
behavioural interventions are effective in reducing the smoking habits and outcome can be
reviewed 6-months after the implementation of the interventions.
The Hurdles and Resources Required for the Implementation
The main hurdle for the implementation of the intervention and to achieve
comprehensive outcome is abstinence during the tenure of the 6 months of follow-up (11). In
order to overcome such barrier, motivational enhancement can be proved to be effective. This
comes under the domain of the psychosocial interventions as highlighted by the review
conducted by Stanton and Grimshaw over the young adults (12). The psychological
interventions for the motivational approach can be done with the procurement of the financial
incentives. The financial incentives are found to be effective in order to increase the
participation of the people who resides under the poor socio-economic determinants (13).
The main resources that will be required for the process of assisting the adults in the
topic of quitting smoking is psychological counselling expert for face-face counselling at the
community level. The psychological counselling experts will be assisted by the clinical nurse
and the healthcare physicals for the procurement of the pharmaco-therapy (10). According to
National Institute for Health and Care Excellence ,the effective mode of the implementation
of the intervention will be done through behavioural support (individual and group) this will
be followed by bupropion, nicotine replacement therapy (NRT) [short acting], vareniciline
HEALTH CARE
Evidence Based Evaluation
The review of the literature and the evidence based approach highlighted that the
combination of both face-to-face counselling and pharmacotherapy is effective in inflicting
the tendency of quitting the smoking habits by overcoming the withdrawal symptoms.
Similar approach was highlighted in the guidelines published by the National Institute of
Care and Excellence (NICE)(10). As per the NICE guidelines, which is based on the
systematic review of different studies the combination of the pharmaco-therapy and
behavioural interventions are effective in reducing the smoking habits and outcome can be
reviewed 6-months after the implementation of the interventions.
The Hurdles and Resources Required for the Implementation
The main hurdle for the implementation of the intervention and to achieve
comprehensive outcome is abstinence during the tenure of the 6 months of follow-up (11). In
order to overcome such barrier, motivational enhancement can be proved to be effective. This
comes under the domain of the psychosocial interventions as highlighted by the review
conducted by Stanton and Grimshaw over the young adults (12). The psychological
interventions for the motivational approach can be done with the procurement of the financial
incentives. The financial incentives are found to be effective in order to increase the
participation of the people who resides under the poor socio-economic determinants (13).
The main resources that will be required for the process of assisting the adults in the
topic of quitting smoking is psychological counselling expert for face-face counselling at the
community level. The psychological counselling experts will be assisted by the clinical nurse
and the healthcare physicals for the procurement of the pharmaco-therapy (10). According to
National Institute for Health and Care Excellence ,the effective mode of the implementation
of the intervention will be done through behavioural support (individual and group) this will
be followed by bupropion, nicotine replacement therapy (NRT) [short acting], vareniciline
8
HEALTH CARE
(brief and active). Text messaging can also be considered as a medium of the behavioural
support and this can help to increase the provision of individuals’ consultation and
maintenance of privacy and confidentiality (14). The designing of the pharmacological
therapy will initiate with a agreed quite date of smoking within first 2 weeks of bupropion
treatment and within 1 to 2 weeks of varenicline treatment NRT therapy is mainly proposed
for the young adults who are dependent on tobacco along with the behavioural support
(National Institute for Health and Care Excellence 2018). All the resources and the
approaches that are recommended for the application of these interventions are cost-effective
and cost-saving under the settings of both NHS and other local authorities. Another important
aspect of this collaborative intervention is the drugs which are recommended for quitting
smoke do not have any severe side-effects. Moreover, for the groups of the individuals who
are hailing from the disadvantaged backgrounds, behavioural support if successful might
provide confidence and skills which will act as a buffer against poor social determinant of
health and thus facilitating positive behavioural change (13).
Evaluation of the outcome
The evaluation of the outcome can be done with the help of the periodic follow up of
the participants of the interventions at the community health set-up. The evaluation will be
based on the self-reported tendency of quitting the tobacco or other tobacco related products.
However, Thomas et al. are of the opinion that the self-reported levels at times might be
biased or erroneous (15). Thus in order to overcome such biased outcomes. The evaluation
approach will also be based on the evaluation of the improvement of the overall quality of life
of the participations in terms of dietary habits and feeding habits. The mental health
professionals will also be recruited in order to take a note of the improvement of the level of
depression among the people who are from the poor socio-economic status (14). According to
Hitsman et al. fighting against depression is one of the driving factors behind the high rate of
HEALTH CARE
(brief and active). Text messaging can also be considered as a medium of the behavioural
support and this can help to increase the provision of individuals’ consultation and
maintenance of privacy and confidentiality (14). The designing of the pharmacological
therapy will initiate with a agreed quite date of smoking within first 2 weeks of bupropion
treatment and within 1 to 2 weeks of varenicline treatment NRT therapy is mainly proposed
for the young adults who are dependent on tobacco along with the behavioural support
(National Institute for Health and Care Excellence 2018). All the resources and the
approaches that are recommended for the application of these interventions are cost-effective
and cost-saving under the settings of both NHS and other local authorities. Another important
aspect of this collaborative intervention is the drugs which are recommended for quitting
smoke do not have any severe side-effects. Moreover, for the groups of the individuals who
are hailing from the disadvantaged backgrounds, behavioural support if successful might
provide confidence and skills which will act as a buffer against poor social determinant of
health and thus facilitating positive behavioural change (13).
Evaluation of the outcome
The evaluation of the outcome can be done with the help of the periodic follow up of
the participants of the interventions at the community health set-up. The evaluation will be
based on the self-reported tendency of quitting the tobacco or other tobacco related products.
However, Thomas et al. are of the opinion that the self-reported levels at times might be
biased or erroneous (15). Thus in order to overcome such biased outcomes. The evaluation
approach will also be based on the evaluation of the improvement of the overall quality of life
of the participations in terms of dietary habits and feeding habits. The mental health
professionals will also be recruited in order to take a note of the improvement of the level of
depression among the people who are from the poor socio-economic status (14). According to
Hitsman et al. fighting against depression is one of the driving factors behind the high rate of
9
HEALTH CARE
smoking among the people who resides under the poor social determinants of health.
Furthermore, follow-up counselling will also help to ascertain the change in the attitude of
the people towards smoking (16).
Analysis of the critical factors for the successful implementation of the intervention
A health promotion program is pivotal in the cessation of smoking among the age
group 18 years and above, in the United Kingdom. As stated earlier, one of the main reasons
for the prevalence of smoking among the young adults, is lack of education about the harmful
effect of tobacco (18). Before carrying out any interventions it is necessary for the target
group to understand why the intervention should be carried out. Peer education is needed, that
involves sharing of the information in small groups, such that they can educate themselves
and their peers as of why education about the health promotion is required. Before,
application of the pharmacological therapy, it is necessary to teach them about the importance
of the pharmacological therapy in smoking cessation. In order to spread awareness about the
health promotion an effective media platform is required for disseminating the messages
related to the good health. Media advocacy is required to frame a particular issue and
advocate the issue using media as the platform. Information has to be disseminated through
the media with a view to alter the minds of the public (18). Hence mass media campaigns
should be used widely in order to make a successful implementation of the smoking
interventions. Success of a health promotion program entirely depends upon whether the
intervention is applicable to the generalised population. The wave of the interventions might
not reach to the remotest communities due to lack of communication and remoteness of the
communities. Hence the stakeholders and the campaigners should reach out to the remotest
communities and set up regular check-ups and educate them about smoking cessation.
Smoking cessation in the rural communities can be challenging in comparison to the urban
HEALTH CARE
smoking among the people who resides under the poor social determinants of health.
Furthermore, follow-up counselling will also help to ascertain the change in the attitude of
the people towards smoking (16).
Analysis of the critical factors for the successful implementation of the intervention
A health promotion program is pivotal in the cessation of smoking among the age
group 18 years and above, in the United Kingdom. As stated earlier, one of the main reasons
for the prevalence of smoking among the young adults, is lack of education about the harmful
effect of tobacco (18). Before carrying out any interventions it is necessary for the target
group to understand why the intervention should be carried out. Peer education is needed, that
involves sharing of the information in small groups, such that they can educate themselves
and their peers as of why education about the health promotion is required. Before,
application of the pharmacological therapy, it is necessary to teach them about the importance
of the pharmacological therapy in smoking cessation. In order to spread awareness about the
health promotion an effective media platform is required for disseminating the messages
related to the good health. Media advocacy is required to frame a particular issue and
advocate the issue using media as the platform. Information has to be disseminated through
the media with a view to alter the minds of the public (18). Hence mass media campaigns
should be used widely in order to make a successful implementation of the smoking
interventions. Success of a health promotion program entirely depends upon whether the
intervention is applicable to the generalised population. The wave of the interventions might
not reach to the remotest communities due to lack of communication and remoteness of the
communities. Hence the stakeholders and the campaigners should reach out to the remotest
communities and set up regular check-ups and educate them about smoking cessation.
Smoking cessation in the rural communities can be challenging in comparison to the urban
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10
HEALTH CARE
areas by the fact , that there are unique social and cultural factors that can affect the use of
tobacco (19). Some rural communities might have some social norms supportive of the use of
tobacco, or remain exposed to the tobacco industry marketing campaign. Again proximity to
the tobacco growing areas in the rural area also acts as a factor to tobacco use among the age
group 18 and above. Hence before chalking out the interventions it is necessary to assess and
evaluate all these factors (20).
It is necessary to involve the stakeholders and the community partners for the success
of any tobacco cessation program and the prevention activities. Stakeholders should also be
involved in the evaluation of the results; hence the input in the evaluation process is
important. For the successful intervention of the program, the stakeholders include people or
organisation with an interest in outcomes like those engaged in the programs, like the health
care providers, the health educators, the department of health, the program managers and the
staffs and the funders (21). Stakeholders also includes the one that will be benefitted by the
program, such as the young adults , their families, the local organisation and those who would
use the evaluation results for a taking actions such as the clinics, the health care providers, the
health system, the federal state , the tribal or the territorial government.
Again, for the successful implementation of a health promotion plan it is necessary to
get an accurate data of the exact rate of smoking among the young adults to estimate the scale
of the intervention and the funding of the health promotion (21). For the successful health
promotion it is necessary to consider the different models of health behaviour such as the
health belief model, which states that the particular behaviour of an individual is guided by
several factors. Hence, while developing an intervention program, it is necessary to address
the triggering factors of the behaviour (smoking). This model can be a framework for
motivating the people to adopt positive health actions and avoid the negative health actions.
HEALTH CARE
areas by the fact , that there are unique social and cultural factors that can affect the use of
tobacco (19). Some rural communities might have some social norms supportive of the use of
tobacco, or remain exposed to the tobacco industry marketing campaign. Again proximity to
the tobacco growing areas in the rural area also acts as a factor to tobacco use among the age
group 18 and above. Hence before chalking out the interventions it is necessary to assess and
evaluate all these factors (20).
It is necessary to involve the stakeholders and the community partners for the success
of any tobacco cessation program and the prevention activities. Stakeholders should also be
involved in the evaluation of the results; hence the input in the evaluation process is
important. For the successful intervention of the program, the stakeholders include people or
organisation with an interest in outcomes like those engaged in the programs, like the health
care providers, the health educators, the department of health, the program managers and the
staffs and the funders (21). Stakeholders also includes the one that will be benefitted by the
program, such as the young adults , their families, the local organisation and those who would
use the evaluation results for a taking actions such as the clinics, the health care providers, the
health system, the federal state , the tribal or the territorial government.
Again, for the successful implementation of a health promotion plan it is necessary to
get an accurate data of the exact rate of smoking among the young adults to estimate the scale
of the intervention and the funding of the health promotion (21). For the successful health
promotion it is necessary to consider the different models of health behaviour such as the
health belief model, which states that the particular behaviour of an individual is guided by
several factors. Hence, while developing an intervention program, it is necessary to address
the triggering factors of the behaviour (smoking). This model can be a framework for
motivating the people to adopt positive health actions and avoid the negative health actions.
11
HEALTH CARE
Young people often might find it awkward to sit for a face to face counselling with
the counsellor and discuss about their smoking habits, hence it is necessary to make a careful
choice of the stakeholders needed for the health promotion interventions. It is necessary to
involve the schools in the smoking cessation campaigns (22). On the other hand have argued
that ,students might find it “cool” to discuss openly about smoking to the teachers and might
smoke more in the campus without any hesitation as before. It has been stated before that
face to face counselling might be effective in understanding the behaviour behind a particular
practice (smoking). Counselling such as motivational interviewing is a client focussed
directive approach that stimulates positive behaviour change and resolve the ambivalence
(18). Important guiding principle of counselling is empathy, supporting self efficacy rolling
with the resistance. It has been demonstrated about the effectiveness motivational interview
based intervention given by the clinical staffs versus normal advice to quit smoking. Higher
rate of smoking abstinence has been noticed in person receiving MI based interventions (18).
One of the main factors behind the successful implementation of a health promotion is
the involvement of the government funding. Identification of the health objectives and the
targets, assessing the needs of the people and allocating the resources is the main role of the
government. A government should first assess the prevalence and the large scale implication
of the condition before the allocation of the funds (20). A fully funded tobacco prevention
program and cessation program is required as the Tobacco cessation programs are cost
effective and according to a study ,it has been found that California’s tobacco control
program has saved over $56 in health care sector for every $1 invested since 1990 to 2008.
Hence it is evident, that fewer people would smoke for due to the health interventions taken
(19).
Smoking among the age group of 18 and above, is a serious public health challenge
across the world. The dimension of this epidemic is resulting in enormous disease, disability
HEALTH CARE
Young people often might find it awkward to sit for a face to face counselling with
the counsellor and discuss about their smoking habits, hence it is necessary to make a careful
choice of the stakeholders needed for the health promotion interventions. It is necessary to
involve the schools in the smoking cessation campaigns (22). On the other hand have argued
that ,students might find it “cool” to discuss openly about smoking to the teachers and might
smoke more in the campus without any hesitation as before. It has been stated before that
face to face counselling might be effective in understanding the behaviour behind a particular
practice (smoking). Counselling such as motivational interviewing is a client focussed
directive approach that stimulates positive behaviour change and resolve the ambivalence
(18). Important guiding principle of counselling is empathy, supporting self efficacy rolling
with the resistance. It has been demonstrated about the effectiveness motivational interview
based intervention given by the clinical staffs versus normal advice to quit smoking. Higher
rate of smoking abstinence has been noticed in person receiving MI based interventions (18).
One of the main factors behind the successful implementation of a health promotion is
the involvement of the government funding. Identification of the health objectives and the
targets, assessing the needs of the people and allocating the resources is the main role of the
government. A government should first assess the prevalence and the large scale implication
of the condition before the allocation of the funds (20). A fully funded tobacco prevention
program and cessation program is required as the Tobacco cessation programs are cost
effective and according to a study ,it has been found that California’s tobacco control
program has saved over $56 in health care sector for every $1 invested since 1990 to 2008.
Hence it is evident, that fewer people would smoke for due to the health interventions taken
(19).
Smoking among the age group of 18 and above, is a serious public health challenge
across the world. The dimension of this epidemic is resulting in enormous disease, disability
12
HEALTH CARE
and death. The tobacco use attributed to about 5 million preventable deaths all around the
world and death at this rate is expected to double by 2020. Interventions like
pharmacotherapy like nicotine replacement therapy have been chosen for tobacco cessation
among the target group. Apart from the pharmacological therapy, behavioral therapies such
as one-to-one counseling and educations were also some of the proposed interventions.
However, the paper had also discussed about the resources required for the successful
implementation of the resources. However, it has also been stated that factors as peer
education, involvement of mass media, access to the rural communities and proper funding
by the government is necessary for the ideal implementation of the program.
HEALTH CARE
and death. The tobacco use attributed to about 5 million preventable deaths all around the
world and death at this rate is expected to double by 2020. Interventions like
pharmacotherapy like nicotine replacement therapy have been chosen for tobacco cessation
among the target group. Apart from the pharmacological therapy, behavioral therapies such
as one-to-one counseling and educations were also some of the proposed interventions.
However, the paper had also discussed about the resources required for the successful
implementation of the resources. However, it has also been stated that factors as peer
education, involvement of mass media, access to the rural communities and proper funding
by the government is necessary for the ideal implementation of the program.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13
HEALTH CARE
References
1. World Health Organisation.. Tobacco and inequities Guidance for addressing inequities
in tobacco-related harm 2014. Access date: 10th of Jan 2019. Retrieved from:
http://www.euro.who.int/__data/assets/pdf_file/0005/247640/tobacco-090514.pdf
2. Public Health England.. Health matters: smoking and quitting in England. 2015. Access
date: 10th of Jan 2019. Retrieved from:
https://www.gov.uk/government/publications/health-matters-smoking-and-quitting-in-
england/smoking-and-quitting-in-england
3. Public Health England.. Health matters: stopping smoking - what works?. 2018. Access
date: 10th of Jan 2019. Retrieved from:
https://www.gov.uk/government/publications/health-matters-stopping-smoking-what-
works/health-matters-stopping-smoking-what-works
4. Centers for Disease Control and Prevention. Introduction, Evaluation of Evidence on
Mechanisms of Disease Production, and Summary. In How Tobacco Smoke Causes
Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report
of the Surgeon General. Centers for Disease Control and Prevention (US).2010
5. Office of the National Statistics. Statistics on Smoking England: 2018. Access date: 10th
of Jan 2019. Retrieved from: https://files.digital.nhs.uk/0C/95F481/stat-smok-eng-2018-
rep.pdf
6. National Health Statistics. 2018. Statistics on Smoking England (2018). Access date: 10th
of Jan 2019. Retrieved from: https://files.digital.nhs.uk/0C/95F481/stat-smok-eng-2018-
rep.pdf
HEALTH CARE
References
1. World Health Organisation.. Tobacco and inequities Guidance for addressing inequities
in tobacco-related harm 2014. Access date: 10th of Jan 2019. Retrieved from:
http://www.euro.who.int/__data/assets/pdf_file/0005/247640/tobacco-090514.pdf
2. Public Health England.. Health matters: smoking and quitting in England. 2015. Access
date: 10th of Jan 2019. Retrieved from:
https://www.gov.uk/government/publications/health-matters-smoking-and-quitting-in-
england/smoking-and-quitting-in-england
3. Public Health England.. Health matters: stopping smoking - what works?. 2018. Access
date: 10th of Jan 2019. Retrieved from:
https://www.gov.uk/government/publications/health-matters-stopping-smoking-what-
works/health-matters-stopping-smoking-what-works
4. Centers for Disease Control and Prevention. Introduction, Evaluation of Evidence on
Mechanisms of Disease Production, and Summary. In How Tobacco Smoke Causes
Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report
of the Surgeon General. Centers for Disease Control and Prevention (US).2010
5. Office of the National Statistics. Statistics on Smoking England: 2018. Access date: 10th
of Jan 2019. Retrieved from: https://files.digital.nhs.uk/0C/95F481/stat-smok-eng-2018-
rep.pdf
6. National Health Statistics. 2018. Statistics on Smoking England (2018). Access date: 10th
of Jan 2019. Retrieved from: https://files.digital.nhs.uk/0C/95F481/stat-smok-eng-2018-
rep.pdf
14
HEALTH CARE
7. Stead LF, Lancaster T. Combined pharmacotherapy and behavioural interventions for
smoking cessation. Cochrane Database of Systematic Reviews. 2012(10). Access date:
11th of Jan 2019. Retrieved from : https://www.ncbi.nlm.nih.gov/pubmed/27009521
8. Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation.
Cochrane database of systematic reviews. 2017(3). Access date: 11th of Jan 2019.
Retrieved from : https://www.ncbi.nlm.nih.gov/pubmed/28361496
9. Cahill K, Stevens S, Perera R, Lancaster T. Pharmacological interventions for smoking
cessation: an overview of reviews. Cochrane database of systematic reviews. 2013(5).
Access date: 11th of Jan 2019. Retrieved from :
https://www.ncbi.nlm.nih.gov/pubmed/23728690
10. National Institute for Health and Care Excellence. Smoking cessation interventions and
services. 2018 Access date: 11th of Jan 2019. Retrieved from :
https://www.nice.org.uk/guidance/ng92/evidence/b-interventions-to-aid-smoking-
cessation-behavioural-support-and-pharmacotherapy-pdf-4788920847
11. Mdege ND, Chindove S. Effectiveness of tobacco use cessation interventions delivered
by pharmacy personnel: a systematic review. Research in Social and Administrative
Pharmacy. 2014 Jan 1;10(1):21-44. Access date: 11th of Jan 2019. Retrieved from :
https://www.ncbi.nlm.nih.gov/pubmed/23743504
12. Stanton A, Grimshaw G. Tobacco cessation interventions for young people. Cochrane
Database of Systematic Reviews. 2013(8). Access date: 11th of Jan 2019. Retrieved from :
https://www.ncbi.nlm.nih.gov/pubmed/23975659
13. Giles EL, Robalino S, McColl E, Sniehotta FF, Adams J. The effectiveness of financial
incentives for health behaviour change: systematic review and meta-analysis. PloS one.
HEALTH CARE
7. Stead LF, Lancaster T. Combined pharmacotherapy and behavioural interventions for
smoking cessation. Cochrane Database of Systematic Reviews. 2012(10). Access date:
11th of Jan 2019. Retrieved from : https://www.ncbi.nlm.nih.gov/pubmed/27009521
8. Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation.
Cochrane database of systematic reviews. 2017(3). Access date: 11th of Jan 2019.
Retrieved from : https://www.ncbi.nlm.nih.gov/pubmed/28361496
9. Cahill K, Stevens S, Perera R, Lancaster T. Pharmacological interventions for smoking
cessation: an overview of reviews. Cochrane database of systematic reviews. 2013(5).
Access date: 11th of Jan 2019. Retrieved from :
https://www.ncbi.nlm.nih.gov/pubmed/23728690
10. National Institute for Health and Care Excellence. Smoking cessation interventions and
services. 2018 Access date: 11th of Jan 2019. Retrieved from :
https://www.nice.org.uk/guidance/ng92/evidence/b-interventions-to-aid-smoking-
cessation-behavioural-support-and-pharmacotherapy-pdf-4788920847
11. Mdege ND, Chindove S. Effectiveness of tobacco use cessation interventions delivered
by pharmacy personnel: a systematic review. Research in Social and Administrative
Pharmacy. 2014 Jan 1;10(1):21-44. Access date: 11th of Jan 2019. Retrieved from :
https://www.ncbi.nlm.nih.gov/pubmed/23743504
12. Stanton A, Grimshaw G. Tobacco cessation interventions for young people. Cochrane
Database of Systematic Reviews. 2013(8). Access date: 11th of Jan 2019. Retrieved from :
https://www.ncbi.nlm.nih.gov/pubmed/23975659
13. Giles EL, Robalino S, McColl E, Sniehotta FF, Adams J. The effectiveness of financial
incentives for health behaviour change: systematic review and meta-analysis. PloS one.
15
HEALTH CARE
2014 Mar 11;9(3):e90347. Access date: 11th of Jan 2019. Retrieved from :
https://doi.org/10.1371/journal.pone.0090347
14. Abroms LC, Boal AL, Simmens SJ, Mendel JA, Windsor RA. A randomized trial of
Text2Quit: a text messaging program for smoking cessation. American journal of
preventive medicine. 2014 Sep 1;47(3):242-50. Access date: 11th of Jan 2019. Retrieved
from :
15. Thomas KH, Martin RM, Davies NM, Metcalfe C, Windmeijer F, Gunnell D. Smoking
cessation treatment and risk of depression, suicide, and self harm in the Clinical Practice
Research Datalink: prospective cohort study. Bmj. 2013 Oct 11;347:f5704. Access date:
11th of Jan 2019. Retrieved from : https://www.ncbi.nlm.nih.gov/pubmed/24913220
16. Hitsman B, Papandonatos GD, McChargue DE, DeMott A, Herrera MJ, Spring B,
Borrelli B, Niaura R. Past major depression and smoking cessation outcome: a systematic
review and meta‐analysis update. Addiction. 2013 Feb;108(2):294-306. Access date: 11th
of Jan 2019. Retrieved from : doi: 10.1111/add.12009
17. Grosios K, Gahan PB, Burbidge J. Overview of healthcare in the UK. EPMA Journal.
2010 Dec 1;1(4):529-34. Access date: 11th of Jan 2019. Retrieved from :
doi: 10.1111/add.12009
18. Golechha M. Health promotion methods for smoking prevention and cessation: A
comprehensive review of effectiveness and the way forward. International journal of
HEALTH CARE
2014 Mar 11;9(3):e90347. Access date: 11th of Jan 2019. Retrieved from :
https://doi.org/10.1371/journal.pone.0090347
14. Abroms LC, Boal AL, Simmens SJ, Mendel JA, Windsor RA. A randomized trial of
Text2Quit: a text messaging program for smoking cessation. American journal of
preventive medicine. 2014 Sep 1;47(3):242-50. Access date: 11th of Jan 2019. Retrieved
from :
15. Thomas KH, Martin RM, Davies NM, Metcalfe C, Windmeijer F, Gunnell D. Smoking
cessation treatment and risk of depression, suicide, and self harm in the Clinical Practice
Research Datalink: prospective cohort study. Bmj. 2013 Oct 11;347:f5704. Access date:
11th of Jan 2019. Retrieved from : https://www.ncbi.nlm.nih.gov/pubmed/24913220
16. Hitsman B, Papandonatos GD, McChargue DE, DeMott A, Herrera MJ, Spring B,
Borrelli B, Niaura R. Past major depression and smoking cessation outcome: a systematic
review and meta‐analysis update. Addiction. 2013 Feb;108(2):294-306. Access date: 11th
of Jan 2019. Retrieved from : doi: 10.1111/add.12009
17. Grosios K, Gahan PB, Burbidge J. Overview of healthcare in the UK. EPMA Journal.
2010 Dec 1;1(4):529-34. Access date: 11th of Jan 2019. Retrieved from :
doi: 10.1111/add.12009
18. Golechha M. Health promotion methods for smoking prevention and cessation: A
comprehensive review of effectiveness and the way forward. International journal of
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
16
HEALTH CARE
preventive medicine. 2016;7. Access date: 11th of Jan 2019. Retrieved from :
doi: 10.4103/2008-7802.173797
19. Butler KM, Hedgecock S, Record RA, Derifield S, McGinn C, Murray D, Hahn EJ. An
evidence-based cessation strategy using rural smokers’ experiences with tobacco. Nursing
Clinics. 2012 Mar 1;47(1):31-43. Access date: 11th of Jan 2019. Retrieved from :
doi: 10.1111/add.12009
20. Frieden TR. Government's role in protecting health and safety. New England Journal of
Medicine. 2013 May 16;368(20):1857-9. Access date: 11th of Jan 2019. Retrieved from :
DOI:10.1056/NEJMp1303819
21. Harris J, Croot L, Thompson J, Springett J. How stakeholder participation can contribute
to systematic reviews of complex interventions. J Epidemiol Community Health. 2016
Feb 1;70(2):207-1. Access date: 11th of Jan 2019. Retrieved from : doi: 10.1136/jech-
2015-205701
HEALTH CARE
preventive medicine. 2016;7. Access date: 11th of Jan 2019. Retrieved from :
doi: 10.4103/2008-7802.173797
19. Butler KM, Hedgecock S, Record RA, Derifield S, McGinn C, Murray D, Hahn EJ. An
evidence-based cessation strategy using rural smokers’ experiences with tobacco. Nursing
Clinics. 2012 Mar 1;47(1):31-43. Access date: 11th of Jan 2019. Retrieved from :
doi: 10.1111/add.12009
20. Frieden TR. Government's role in protecting health and safety. New England Journal of
Medicine. 2013 May 16;368(20):1857-9. Access date: 11th of Jan 2019. Retrieved from :
DOI:10.1056/NEJMp1303819
21. Harris J, Croot L, Thompson J, Springett J. How stakeholder participation can contribute
to systematic reviews of complex interventions. J Epidemiol Community Health. 2016
Feb 1;70(2):207-1. Access date: 11th of Jan 2019. Retrieved from : doi: 10.1136/jech-
2015-205701

17
HEALTH CARE
HEALTH CARE
1 out of 18
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





