Leadership and Innovation: Planned Change in Hospital Ward, Singapore
VerifiedAdded on 2023/04/08
|15
|4499
|288
Essay
AI Summary
This essay delves into the concept of planned change within a hospital setting, specifically focusing on updating patient information within one hour of admission to improve patient satisfaction and quality care. It explores the role of leadership, particularly transformational and transactional leadership theories, in implementing such changes, highlighting the importance of leaders in fostering collaboration, managing stakeholder expectations, and adapting to value-based healthcare. The essay also examines the influence of innovation and environmental factors on change implementation, utilizing SWOT analysis to assess strengths, weaknesses, opportunities, and threats. Furthermore, it discusses change management theories, including Lewin's and Roger's change theories, emphasizing the need to overcome resistant forces and facilitate the adoption of new policies and procedures within the healthcare organization. This document is a student contribution and available on Desklib.
Leadership and Innovation
1
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1.Introduction:
In this essay, planned change in the hospital would be discussed. Planned change is updating
information to the patients within one hour of admission to the ward. Implementation of this
change is necessary in the ward because it is helpful in improving overall patient satisfaction
and providing quality care to the patients. In this essay, suitable leadership theory which is
necessary for implementing change would be discussed. Role of innovation and influence of
environmental factors on implementing change also would be discussed. Change can be
implemented through validated policies and procedures. Hence, specific change theories
would be assessed for implementing planned change in the hospital. Nurse should not only be
well versed with the nursing skills but also be aware of other skills like communication skills,
leadership skills, interpersonal skills and innovative thinking skills.
2. Discussion
2a. Leadership:
Leadership is important aspect to implement proposed change in the healthcare sector
because leaders can bring together different professionals and departments to work together
to bring change. It is important to bring these stakeholders together because different
stakeholders might have different ideas to implement proposed change. Leaders are capable
to understand changes and are sensitive to the needs and requirements of the different
professionals working in the healthcare sector. Leaders are capable to monitor and regulate
the change because excessive change can be exhaustive to the workers and organisation
(Lega, Prenestini, and Rosso, 2017). Leaders can change mindset of workers to adapt to
change in the healthcare sector. Leaders can effectively switch healthcare services to value
based to volume based and can bring wider changes in the organisation. Idea of change can
produce nervousness in the workers; hence, leaders can show effective path to achieve big
goal (Nelson-Brantley and Ford, 2017).
Transformational leadership theory:
Transformational leadership theory is widely accepted and supported leadership theory for
the healthcare sector. This theory states that more than one individual involve in such a
manner that both leaders and subordinates promote each other to the advanced stage of
motivation and morality. According to the transformational leadership theory, leaders
promote excelling in self-interests of their sub-ordinates, raising their requirement for the
2
In this essay, planned change in the hospital would be discussed. Planned change is updating
information to the patients within one hour of admission to the ward. Implementation of this
change is necessary in the ward because it is helpful in improving overall patient satisfaction
and providing quality care to the patients. In this essay, suitable leadership theory which is
necessary for implementing change would be discussed. Role of innovation and influence of
environmental factors on implementing change also would be discussed. Change can be
implemented through validated policies and procedures. Hence, specific change theories
would be assessed for implementing planned change in the hospital. Nurse should not only be
well versed with the nursing skills but also be aware of other skills like communication skills,
leadership skills, interpersonal skills and innovative thinking skills.
2. Discussion
2a. Leadership:
Leadership is important aspect to implement proposed change in the healthcare sector
because leaders can bring together different professionals and departments to work together
to bring change. It is important to bring these stakeholders together because different
stakeholders might have different ideas to implement proposed change. Leaders are capable
to understand changes and are sensitive to the needs and requirements of the different
professionals working in the healthcare sector. Leaders are capable to monitor and regulate
the change because excessive change can be exhaustive to the workers and organisation
(Lega, Prenestini, and Rosso, 2017). Leaders can change mindset of workers to adapt to
change in the healthcare sector. Leaders can effectively switch healthcare services to value
based to volume based and can bring wider changes in the organisation. Idea of change can
produce nervousness in the workers; hence, leaders can show effective path to achieve big
goal (Nelson-Brantley and Ford, 2017).
Transformational leadership theory:
Transformational leadership theory is widely accepted and supported leadership theory for
the healthcare sector. This theory states that more than one individual involve in such a
manner that both leaders and subordinates promote each other to the advanced stage of
motivation and morality. According to the transformational leadership theory, leaders
promote excelling in self-interests of their sub-ordinates, raising their requirement for the
2
organisation and make them realise their responsibility of larger organisational goal. It is
useful in bringing change like providing information to the patients within one hour of
admission. For bringing this type change, healthcare workers those who works very closely
with patients need to provide information to the patients. It is useful in the overall
development of the total workforce in the organisation which is necessary to bring change in
the organisation (Vaismoradi, Griffiths, Turunen, and Jordan, 2016). Transformational
leaders possess certain special traits. These traits include vision, self-confidence and self-
awareness which are useful in developing multidisciplinary team necessary to bring change in
the healthcare organisation. For providing information to the patients within first hour,
multidisciplinary team need to work in integrated manner. Transformational leaders provide
opportunity to the subordinates to exercise leadership which would be helpful in improving
confidence of the subordinates to achieve aim of bringing change in the healthcare
organisation. Transformational leadership is considered as catalyst for bringing new and
innovative model in the healthcare organisation which indicates usefulness of this theory in
bringing change (Liukka, Hupli, and Turunen, 2018).
Collaboration, interpersonal skills and personal contacts are the prominent traits of
transformation leadership which are necessary for communication to the patients in the first
hour of admission to the hospital. Transformational leadership is also helpful for subordinates
for developing new ideas and improving aspirations for improvement and bringing change in
the healthcare organisation. Despite having all the beneficial qualities for bringing change in
the organisation, transformational theory is associated with certain drawbacks.
Transformational theory alone in the long run can be harmful to the organisation. It has also
been proved that transformational leaders might fail without traditional management skills. It
is highly possible that without specific plan and vision; transformational leaders would fail in
bringing change in the organisation (Fischer, 2016).
Transactional leadership theory:
Transactional leadership theory is built on the exercising leadership due to management
position according to the organisational hierarchy. According to this theory, leaders identify
needs of the subordinates and transact with them. This theory has social aspect which is based
on the power and reward system. This theory is useful in achieving goal of the organisation
through providing better healthcare services to the patients. Providing information to the
patients within first hour of admission would be helpful in providing relevant intervention
3
useful in bringing change like providing information to the patients within one hour of
admission. For bringing this type change, healthcare workers those who works very closely
with patients need to provide information to the patients. It is useful in the overall
development of the total workforce in the organisation which is necessary to bring change in
the organisation (Vaismoradi, Griffiths, Turunen, and Jordan, 2016). Transformational
leaders possess certain special traits. These traits include vision, self-confidence and self-
awareness which are useful in developing multidisciplinary team necessary to bring change in
the healthcare organisation. For providing information to the patients within first hour,
multidisciplinary team need to work in integrated manner. Transformational leaders provide
opportunity to the subordinates to exercise leadership which would be helpful in improving
confidence of the subordinates to achieve aim of bringing change in the healthcare
organisation. Transformational leadership is considered as catalyst for bringing new and
innovative model in the healthcare organisation which indicates usefulness of this theory in
bringing change (Liukka, Hupli, and Turunen, 2018).
Collaboration, interpersonal skills and personal contacts are the prominent traits of
transformation leadership which are necessary for communication to the patients in the first
hour of admission to the hospital. Transformational leadership is also helpful for subordinates
for developing new ideas and improving aspirations for improvement and bringing change in
the healthcare organisation. Despite having all the beneficial qualities for bringing change in
the organisation, transformational theory is associated with certain drawbacks.
Transformational theory alone in the long run can be harmful to the organisation. It has also
been proved that transformational leaders might fail without traditional management skills. It
is highly possible that without specific plan and vision; transformational leaders would fail in
bringing change in the organisation (Fischer, 2016).
Transactional leadership theory:
Transactional leadership theory is built on the exercising leadership due to management
position according to the organisational hierarchy. According to this theory, leaders identify
needs of the subordinates and transact with them. This theory has social aspect which is based
on the power and reward system. This theory is useful in achieving goal of the organisation
through providing better healthcare services to the patients. Providing information to the
patients within first hour of admission would be helpful in providing relevant intervention
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
and quality care to the patients. Transactional leaders play their leadership roles by
maintaining equilibrium and harmony through following policies and procedures (Smith,
2015). It would be helpful in the improving loyalty and performance of the subordinates.
Hence, these leaders can totally depend on subordinate nurses for providing useful
information to the patients. Moreover, subordinate nurses follow necessary procedures and
policies for providing necessary information to the patients. Transactional leaders give away
performance-based rewards to the subordinates. Subordinates should have proper direction
and behaviour for bringing change in the healthcare organisation which can be effectively
provided by the transactional leaders. Though, this theory is useful in bringing change in the
healthcare organisation; it has been stated that this theory lacks vision. Hence, this leadership
theory along with transformational theory needs to be implemented in the organisation for
bringing effective change to provide required information to the patients within one hour of
admission to the hospital. Moreover, it has also been stated that transactional theory has
narrow focus and most of the organisational activities are based on the self interest of the
leader. However, these drawbacks of this theory can be effectively managed based on the
individual traits of the leader (Saravo, Netzel, and Kiesewetter, 2017; Xenikou, 2017).
Change in the healthcare organisation can be effectively brought by working in the hierarchy
environment. Leaders need to develop and implement effective hierarchical model to train the
nurses in middle management related to change in the healthcare organisation. All the clinical
information which is necessary to pass on to the bedside nurses should be given by the nurses
in the middle level. Nurse in the middle level should act as connecting link between the
leaders and nurses at the bedside need to provide relevant information to the patients within
first hour of admission to the hospital. Moreover, leaders should ensure that all the clinical
information should be given to the patients. Leaders should discus among team members and
come to the consequence for deciding on which type of information should not be given to
the patients (Cope and Murray, 2017).
2b. Innovation in healthcare:
Innovation is related to bringing new ideas to the actual practice. Hence, nurse need to use
clinical judgment, expertise and experience to communicate with the patients to provide
relevant clinical information within first hour of admission to the hospital. Usually, it has
been considered that bringing innovation in the healthcare organisation is difficult. Changes
need to be made in the behaviours of healthcare workers including nurses and current medical
4
maintaining equilibrium and harmony through following policies and procedures (Smith,
2015). It would be helpful in the improving loyalty and performance of the subordinates.
Hence, these leaders can totally depend on subordinate nurses for providing useful
information to the patients. Moreover, subordinate nurses follow necessary procedures and
policies for providing necessary information to the patients. Transactional leaders give away
performance-based rewards to the subordinates. Subordinates should have proper direction
and behaviour for bringing change in the healthcare organisation which can be effectively
provided by the transactional leaders. Though, this theory is useful in bringing change in the
healthcare organisation; it has been stated that this theory lacks vision. Hence, this leadership
theory along with transformational theory needs to be implemented in the organisation for
bringing effective change to provide required information to the patients within one hour of
admission to the hospital. Moreover, it has also been stated that transactional theory has
narrow focus and most of the organisational activities are based on the self interest of the
leader. However, these drawbacks of this theory can be effectively managed based on the
individual traits of the leader (Saravo, Netzel, and Kiesewetter, 2017; Xenikou, 2017).
Change in the healthcare organisation can be effectively brought by working in the hierarchy
environment. Leaders need to develop and implement effective hierarchical model to train the
nurses in middle management related to change in the healthcare organisation. All the clinical
information which is necessary to pass on to the bedside nurses should be given by the nurses
in the middle level. Nurse in the middle level should act as connecting link between the
leaders and nurses at the bedside need to provide relevant information to the patients within
first hour of admission to the hospital. Moreover, leaders should ensure that all the clinical
information should be given to the patients. Leaders should discus among team members and
come to the consequence for deciding on which type of information should not be given to
the patients (Cope and Murray, 2017).
2b. Innovation in healthcare:
Innovation is related to bringing new ideas to the actual practice. Hence, nurse need to use
clinical judgment, expertise and experience to communicate with the patients to provide
relevant clinical information within first hour of admission to the hospital. Usually, it has
been considered that bringing innovation in the healthcare organisation is difficult. Changes
need to be made in the behaviours of healthcare workers including nurses and current medical
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
practices to bring innovation in the healthcare organisation. However, it is risky to bring
changes in these aspects because these are directly related to patient care and overall outcome
of the healthcare organisation. Changes in the healthcare organisation can also influence
financial, social and ethical issues. Despite these hurdles, innovation in healthcare sector is
necessary to bring changes in the healthcare organisation (Snowdon, 2017).
Both internal and external environment can influence implementation of change in the
healthcare organisation. Internal environment comprises of healthcare provider in the
organisation and external environment comprises of other healthcare organisations. However,
in this case of bringing change by providing information within one hour of hospital
admission; internal environment influence change in the healthcare organisation (Romaniuk
and Szromek, 2016). In this planned change, SWOT analysis would be more useful in
identifying effects of working environment on the planned change. PESTLE model would not
be useful in this planned change because PESTEL model is associated with most of the
external factors which can influence change in the environment (Slatyer, Coventry, Twigg,
and Davis, 2016).
SWOT analysis is mainly associated with the positive and negative factors to bring the
change in the organisation. SWOT analysis is based on the strengths, weaknesses,
opportunities and threats of the change. Strengths of the organisation to bring changes include
specialised expertise to bring change, well accepted reputation of the leader, lower cost,
available technology and advantage for the healthcare organisation by providing quality care
to the patients through giving relevant information in the first hour of hospital admission.
Weaknesses to bring these changes include limited manpower to implement change and
management of the existing healthcare staff to bring change. Existing healthcare staff in the
organisation is well adopted to the existing system of the hospital. Hence, it is difficult to
convince and mange them for the planned change. Opportunities include development and
implementation of new technologies and methods and attracting a greater number of patients.
Threats to the planned change include overburden of work on the existing staff to develop
and implement new policies and procedures, lack of energy by the existing staff and lack of
management’s willingness to bring the change (Briggs, Fisher, , and Rob, 2015).
2c. Change and change management:
Lewin’s change theory is widely used in the nursing profession. This change theory can be
implemented in three stages like unfreezing stage, moving stage and refreezing stage (Shirey,
5
changes in these aspects because these are directly related to patient care and overall outcome
of the healthcare organisation. Changes in the healthcare organisation can also influence
financial, social and ethical issues. Despite these hurdles, innovation in healthcare sector is
necessary to bring changes in the healthcare organisation (Snowdon, 2017).
Both internal and external environment can influence implementation of change in the
healthcare organisation. Internal environment comprises of healthcare provider in the
organisation and external environment comprises of other healthcare organisations. However,
in this case of bringing change by providing information within one hour of hospital
admission; internal environment influence change in the healthcare organisation (Romaniuk
and Szromek, 2016). In this planned change, SWOT analysis would be more useful in
identifying effects of working environment on the planned change. PESTLE model would not
be useful in this planned change because PESTEL model is associated with most of the
external factors which can influence change in the environment (Slatyer, Coventry, Twigg,
and Davis, 2016).
SWOT analysis is mainly associated with the positive and negative factors to bring the
change in the organisation. SWOT analysis is based on the strengths, weaknesses,
opportunities and threats of the change. Strengths of the organisation to bring changes include
specialised expertise to bring change, well accepted reputation of the leader, lower cost,
available technology and advantage for the healthcare organisation by providing quality care
to the patients through giving relevant information in the first hour of hospital admission.
Weaknesses to bring these changes include limited manpower to implement change and
management of the existing healthcare staff to bring change. Existing healthcare staff in the
organisation is well adopted to the existing system of the hospital. Hence, it is difficult to
convince and mange them for the planned change. Opportunities include development and
implementation of new technologies and methods and attracting a greater number of patients.
Threats to the planned change include overburden of work on the existing staff to develop
and implement new policies and procedures, lack of energy by the existing staff and lack of
management’s willingness to bring the change (Briggs, Fisher, , and Rob, 2015).
2c. Change and change management:
Lewin’s change theory is widely used in the nursing profession. This change theory can be
implemented in three stages like unfreezing stage, moving stage and refreezing stage (Shirey,
5

2013). Unfreezing stage related to the getting ready to change. It can be achieved by
understanding benefits of change and readiness through getting away from the comfort zone.
Moving stage demonstrates that change is not an even; however, it is a process. Second stage
is helpful in bringing necessary changes. Freezing stage provides stability to the implemented
change. Lewin’s change theory is one of the most relevant theories for bringing change in the
healthcare organisation and most of the other theories are based on the Lewin’s change
theory. Lewin’s change theory is based on the driving and resistant forces (Shirey, 2013).
Identification of the driving forces is necessary to facilitate change in the health care
organisation. Knowledge of resistant forces is also important because effective action can be
taken to circumvent resistant forces. In this planned change, leaders can be considered as the
driving force because leaders are well versed with the policies and procedures to bring
change in the organisation through providing information to the patients in the first hour of
hospital admission. In this planned change, nurses along with other healthcare workers and
patients can be considered as the resistant forces (King, Gerard, and Rapp, 2018).
Nurses and other healthcare workers might not be willing to bring this change because it
might produce additional workload on them in addition to the routine work. Moreover, due to
lack of experience to bring change; nurses might be with low confidence to adopt new
policies and procedures. Moreover, patients also might not be willing to listen to clinical
information to be provided by the nurses. Patients might not be willing to listen to clinical
information because they might not be comfortable with medical technologies. Driving forces
need to be dominant over resistant forces to implement Lewin’s change theory in this planned
change (Manchester et al., 2014; King, Gerard, and Rapp, 2018).
Another change theory which is useful for bringing change in the nursing profession is
Roger’s change theory. Roger’s change theory is the modified form of Lewin’s change
theory. Roger’s change theory is based on five stages like awareness, interest, evaluation,
implementation and adoption. Roger’s change theory is specifically useful in bringing long-
term changes in the healthcare organisations (Barlow, 2016). Planned change like providing
information within first hour of hospital admission is also a long-term change. Hence,
Roger’s change theory is relevant to the planned change. This theory proved more useful in
the nurses, those who rejected the change process in the initial stage; however, accepted the
change after proper training (Barlow, 2016; King, Gerard, and Rapp, 2018).
6
understanding benefits of change and readiness through getting away from the comfort zone.
Moving stage demonstrates that change is not an even; however, it is a process. Second stage
is helpful in bringing necessary changes. Freezing stage provides stability to the implemented
change. Lewin’s change theory is one of the most relevant theories for bringing change in the
healthcare organisation and most of the other theories are based on the Lewin’s change
theory. Lewin’s change theory is based on the driving and resistant forces (Shirey, 2013).
Identification of the driving forces is necessary to facilitate change in the health care
organisation. Knowledge of resistant forces is also important because effective action can be
taken to circumvent resistant forces. In this planned change, leaders can be considered as the
driving force because leaders are well versed with the policies and procedures to bring
change in the organisation through providing information to the patients in the first hour of
hospital admission. In this planned change, nurses along with other healthcare workers and
patients can be considered as the resistant forces (King, Gerard, and Rapp, 2018).
Nurses and other healthcare workers might not be willing to bring this change because it
might produce additional workload on them in addition to the routine work. Moreover, due to
lack of experience to bring change; nurses might be with low confidence to adopt new
policies and procedures. Moreover, patients also might not be willing to listen to clinical
information to be provided by the nurses. Patients might not be willing to listen to clinical
information because they might not be comfortable with medical technologies. Driving forces
need to be dominant over resistant forces to implement Lewin’s change theory in this planned
change (Manchester et al., 2014; King, Gerard, and Rapp, 2018).
Another change theory which is useful for bringing change in the nursing profession is
Roger’s change theory. Roger’s change theory is the modified form of Lewin’s change
theory. Roger’s change theory is based on five stages like awareness, interest, evaluation,
implementation and adoption. Roger’s change theory is specifically useful in bringing long-
term changes in the healthcare organisations (Barlow, 2016). Planned change like providing
information within first hour of hospital admission is also a long-term change. Hence,
Roger’s change theory is relevant to the planned change. This theory proved more useful in
the nurses, those who rejected the change process in the initial stage; however, accepted the
change after proper training (Barlow, 2016; King, Gerard, and Rapp, 2018).
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Integrated Lewin’s Theory with Lean’s System Approach is the useful change management
model for bringing change in the healthcare organisation. Collaborating work and
interprofessional problem solving abilities are necessary for implementing planned change.
Each professional in the healthcare organisation has influence to bring planned change and
every professional has own perspective to bring planned change. Hence, integrated efforts by
all the healthcare professionals need to be taken to implement planned change. Integrated
Lewin’s Theory with Lean’s System Approach is useful in putting integrated efforts to being
planned change (King, Gerard, and Rapp, 2018). Unfreezing, moving and refreezing are the
three stages of Lewin’s theory. Unfreezing stage is useful in improving awareness of the
nurse through education and demonstrating issues or problems. Leaders need to educate
about benefits and demonstrate problems associated with providing information to the
patients within 1 hour of hospital admission. It would be helpful in improving confidence of
nurses to work in the direction of planned change. Moving stage is associated with the
pursuing probable alternatives and minimising forces which would affect change negatively.
Brainstorming, coaching and training are the important aspects of the moving stage.
Brainstorming among nurses and leaders is necessary to plan the process of planned change.
Leaders need to train the subordinate nurses to provide clinical information to the patients
within one hour of hospital admission. Refreezing integrate all the processes in the planned
change and stabilize the new system in healthcare organisation. Refreezing includes
celebrating success and monitoring key performance indicators. Celebrating success is the
indication of promoting and accepting the change. Monitoring key performance indicators
would be helpful in ensuring successful long-term implementation of the planned change
(Manchester et al., 2014).
Lean systems approach is useful improving the process and supporting the people to bring
planned change. Lean process model facilitates improved process flow and empower
healthcare staff to perform activities at all the stages. Hence, lean process is useful in
implementing planned change because there should be simplified process and all the staff
members should have freedom to perform activities to provide information to the patients
(Wojciechowski, Pearsall, Murphy, and French, 2016; King, Gerard, and Rapp, 2018).
Being a change agent, nurse need to perform major functions in the planned change. Nurse
need to work more closely with the patients; hence, nurse should provide information to the
patient in the first hour of hospital admission. Nurse can understand the patient’s perspectives
in a better way. As a change agent nurse should have characteristics like clear vision, patient
7
model for bringing change in the healthcare organisation. Collaborating work and
interprofessional problem solving abilities are necessary for implementing planned change.
Each professional in the healthcare organisation has influence to bring planned change and
every professional has own perspective to bring planned change. Hence, integrated efforts by
all the healthcare professionals need to be taken to implement planned change. Integrated
Lewin’s Theory with Lean’s System Approach is useful in putting integrated efforts to being
planned change (King, Gerard, and Rapp, 2018). Unfreezing, moving and refreezing are the
three stages of Lewin’s theory. Unfreezing stage is useful in improving awareness of the
nurse through education and demonstrating issues or problems. Leaders need to educate
about benefits and demonstrate problems associated with providing information to the
patients within 1 hour of hospital admission. It would be helpful in improving confidence of
nurses to work in the direction of planned change. Moving stage is associated with the
pursuing probable alternatives and minimising forces which would affect change negatively.
Brainstorming, coaching and training are the important aspects of the moving stage.
Brainstorming among nurses and leaders is necessary to plan the process of planned change.
Leaders need to train the subordinate nurses to provide clinical information to the patients
within one hour of hospital admission. Refreezing integrate all the processes in the planned
change and stabilize the new system in healthcare organisation. Refreezing includes
celebrating success and monitoring key performance indicators. Celebrating success is the
indication of promoting and accepting the change. Monitoring key performance indicators
would be helpful in ensuring successful long-term implementation of the planned change
(Manchester et al., 2014).
Lean systems approach is useful improving the process and supporting the people to bring
planned change. Lean process model facilitates improved process flow and empower
healthcare staff to perform activities at all the stages. Hence, lean process is useful in
implementing planned change because there should be simplified process and all the staff
members should have freedom to perform activities to provide information to the patients
(Wojciechowski, Pearsall, Murphy, and French, 2016; King, Gerard, and Rapp, 2018).
Being a change agent, nurse need to perform major functions in the planned change. Nurse
need to work more closely with the patients; hence, nurse should provide information to the
patient in the first hour of hospital admission. Nurse can understand the patient’s perspectives
in a better way. As a change agent nurse should have characteristics like clear vision, patient
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
yet persistent, able to ask tough questions and knowledgeable and leads by example. Nurse
can be considered as the most suitable change agent in this planned change because nurse can
exploit all the acquired education and training for providing clinical information to the
patients. Moreover, patients also feel more comfortable with the nurses while providing
information to them (Wall, 2014). Nurses are well trained for effective healthcare delivery
and can play significant role in the health-related decision making. Nurse has the ability to
look at the planned change in different ways and nurses can effectively assess the impact of
change on the healthcare system. Nurse can help peers to bring the planned change in the
healthcare organisation. Nurse understands holistic care of the patients; hence, nurses can
effectively work to bring the planned change (Eads and Maruzzella, 2016).
2d. Use of Evidence to support change:
Providing information is one of the most important needs of the patient and family members.
However, nurses should not be in dilemma whether to provide true information or give hope.
Such dilemma might lead to ethical issue. Most of the patients and family members remain in
the stress and anxiety due to inadequate information about the prognosis and treatment.
Hence, change could be helpful in reducing stress and anxiety in patients and family
members. In the initial period, most of the patients might not be able to disclose all their
complications to the nurses. However, updating patient in the first hour would be helpful in
establishing open communication among nurse with patient and family members (Schnock et
al., 2017).
It has been established that change is also useful in giving emotional support to the patient
and family members. It is also evident that updating to patients would be helpful in the
improving their knowledge about disease and management. Hence, patients would be able to
take care of themselves whenever possible. It is necessary that nurse should give complete
and understandable information because it is evident that incomplete information would lead
to misunderstanding and misinterpretation by the patients (Tandon and Kaushik, 2015;
Vertino, 2014). It would lead to more disappointment or more hopefulness in the patient and
family members. It is also evident that communication needs to be improved between the
nurse and physician to update patient within first hour of admission (Hamrosi, Raynor, and
Aslani, 2013; Kim, Han, and Kim, 2017). Nurse leaders need to visit patients within one hour
of admission and welcome them, provide relevant information and assure them healthcare
workers would be with them during their stay in the hospital. Evidence-based system is
8
can be considered as the most suitable change agent in this planned change because nurse can
exploit all the acquired education and training for providing clinical information to the
patients. Moreover, patients also feel more comfortable with the nurses while providing
information to them (Wall, 2014). Nurses are well trained for effective healthcare delivery
and can play significant role in the health-related decision making. Nurse has the ability to
look at the planned change in different ways and nurses can effectively assess the impact of
change on the healthcare system. Nurse can help peers to bring the planned change in the
healthcare organisation. Nurse understands holistic care of the patients; hence, nurses can
effectively work to bring the planned change (Eads and Maruzzella, 2016).
2d. Use of Evidence to support change:
Providing information is one of the most important needs of the patient and family members.
However, nurses should not be in dilemma whether to provide true information or give hope.
Such dilemma might lead to ethical issue. Most of the patients and family members remain in
the stress and anxiety due to inadequate information about the prognosis and treatment.
Hence, change could be helpful in reducing stress and anxiety in patients and family
members. In the initial period, most of the patients might not be able to disclose all their
complications to the nurses. However, updating patient in the first hour would be helpful in
establishing open communication among nurse with patient and family members (Schnock et
al., 2017).
It has been established that change is also useful in giving emotional support to the patient
and family members. It is also evident that updating to patients would be helpful in the
improving their knowledge about disease and management. Hence, patients would be able to
take care of themselves whenever possible. It is necessary that nurse should give complete
and understandable information because it is evident that incomplete information would lead
to misunderstanding and misinterpretation by the patients (Tandon and Kaushik, 2015;
Vertino, 2014). It would lead to more disappointment or more hopefulness in the patient and
family members. It is also evident that communication needs to be improved between the
nurse and physician to update patient within first hour of admission (Hamrosi, Raynor, and
Aslani, 2013; Kim, Han, and Kim, 2017). Nurse leaders need to visit patients within one hour
of admission and welcome them, provide relevant information and assure them healthcare
workers would be with them during their stay in the hospital. Evidence-based system is
8
finding the evidence and applying the evidence in making clinical decisions. High level
evidence is helpful in grading and making recommendations. Articles from the RCTs need to
be selected as the evidence because RCT data is more robust data and RCTs answer the
specific question. Observational studies can also be considered as valid evidence; however,
these studies should be properly planned. High level evidence needs to be used because this
type of evidence is useful in interpreting the results in better manner. High of evidence is also
helpful in translating the research in actual clinical practice (Kourkouta and Papathanasiou,
2014; McCarthy et al., 2013; Newell and Jordan, 2015).
3. Conclusion:
Change in the hospital functioning is useful in improving quality of care to the patients.
Update of information to the patients within one hour of ward admission proved helpful not
only in improving healthcare services to patients; however, it is also helpful in improving
leadership qualities, facilitating innovation and brining change in the hospital. Effective
leadership is necessary for the bringing change in the hospital and specific leadership theories
like transformational and transactional leadership theories need to implemented in the
healthcare facility. Change theories like Lewin’s change theory and Roger’s change theory
are useful in implementing planned change in the hospital. Since, multiple professionals need
to be incorporated in implementing planned change; integrated model of Lewin’s Theory
with Lean’s System Approach proved helpful in bringing planned change. SWOT analysis is
the suitable technique to evaluate factors affecting the planned change. Valid and high-level
evidence is useful in implementing planned change. After successful implementation of the
planned change in the ward; this change needs to be implemented in other departments
including departments with critical patients.
9
evidence is helpful in grading and making recommendations. Articles from the RCTs need to
be selected as the evidence because RCT data is more robust data and RCTs answer the
specific question. Observational studies can also be considered as valid evidence; however,
these studies should be properly planned. High level evidence needs to be used because this
type of evidence is useful in interpreting the results in better manner. High of evidence is also
helpful in translating the research in actual clinical practice (Kourkouta and Papathanasiou,
2014; McCarthy et al., 2013; Newell and Jordan, 2015).
3. Conclusion:
Change in the hospital functioning is useful in improving quality of care to the patients.
Update of information to the patients within one hour of ward admission proved helpful not
only in improving healthcare services to patients; however, it is also helpful in improving
leadership qualities, facilitating innovation and brining change in the hospital. Effective
leadership is necessary for the bringing change in the hospital and specific leadership theories
like transformational and transactional leadership theories need to implemented in the
healthcare facility. Change theories like Lewin’s change theory and Roger’s change theory
are useful in implementing planned change in the hospital. Since, multiple professionals need
to be incorporated in implementing planned change; integrated model of Lewin’s Theory
with Lean’s System Approach proved helpful in bringing planned change. SWOT analysis is
the suitable technique to evaluate factors affecting the planned change. Valid and high-level
evidence is useful in implementing planned change. After successful implementation of the
planned change in the ward; this change needs to be implemented in other departments
including departments with critical patients.
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
References:
Barlow, J. (2016). Managing Innovation in Healthcare. World Scientific Publishing
Company. Singapore.
Briggs, A. D. M., Fisher, P. A., and Rob F. Practising Public Health: A Guide to
Examinations and Workplace Application. 1st Eds. CRC Press. Florida, United States.
Cope, V., and Murray, M. (2017). Leadership styles in nursing. Nursing Standard, 31(43),
61-70.
Eads, V., and Maruzzella, G. (2016). The Clinical Nurse as an Agent of Change. MEDSURG
Nursing, 25(3), 173-5.
Fischer, S.A. (2016). Transformational leadership in nursing: a concept analysis. Journal of
Advanced Nursing, 72(11), 2644-2653.
Hamrosi, K.K., Raynor, D.K., and Aslani, P. (2013). Pharmacist and general practitioner
ambivalence about providing written medicine information to patients-a qualitative
study. Research in Social and Administrative Pharmacy, 9(5), 517-30.
Kim, K., Han, Y., and Kim, J.S. (2017). Nurses' and patients' perceptions of privacy
protection behaviours and information provision. Nursing Ethics, 24(5), 598-611.
King, C. R., Gerard, S., and Rapp, C. G. (2018). Essential Knowledge for CNL and APRN
Nurse Leaders. Springer Publishing Company. New York City, United States.
Kourkouta, L., and Papathanasiou, I. V. (2014). Communication in Nursing Practice. Materia
Socio-Medica, 26(1), pp. 65–67.
Lega, F., Prenestini, A., and Rosso, M. (2017). Leadership research in healthcare: A realist
review. Health Services Management Research, 30(2), 94-104.
Liukka, M., Hupli, M., and Turunen, H. (2018). How transformational leadership appears in
action with adverse events? A study for Finnish nurse manager. Journal of Nursing
Management, 26(6), 639-646.
Manchester, J., Gray-Miceli, D.L., Metcalf, J.A., Paolini, C.A., Napier, A.H., Coogle, C.L.,…
and Owens, M.G. (2014). Facilitating Lewin's change model with collaborative
evaluation in promoting evidence-based practices of health professionals. Evaluation
and Program Planning, 47, 82-90.
McCarthy, D.M., Buckley, B.A., Engel, K.G., Forth, V.E., Adams, J.G.,..Cameron, K.A.
(2013). Understanding patient-provider conversations: what are we talking about?
Academic Emergency Medicine, 20(5), 441–8.
Nelson-Brantley, H.V., and Ford, D.J. (2017). Leading change: a concept analysis. Journal of
Advanced Nursing, 73(4), 834-846.
Newell, S., and Jordan, Z. (2015). The patient experience of patient-centered communication
with nurses in the hospital setting: a qualitative systematic review protocol. JBI
Database of Systematic Reviews and Implementation Reports, 13(1), 76-87.
10
Barlow, J. (2016). Managing Innovation in Healthcare. World Scientific Publishing
Company. Singapore.
Briggs, A. D. M., Fisher, P. A., and Rob F. Practising Public Health: A Guide to
Examinations and Workplace Application. 1st Eds. CRC Press. Florida, United States.
Cope, V., and Murray, M. (2017). Leadership styles in nursing. Nursing Standard, 31(43),
61-70.
Eads, V., and Maruzzella, G. (2016). The Clinical Nurse as an Agent of Change. MEDSURG
Nursing, 25(3), 173-5.
Fischer, S.A. (2016). Transformational leadership in nursing: a concept analysis. Journal of
Advanced Nursing, 72(11), 2644-2653.
Hamrosi, K.K., Raynor, D.K., and Aslani, P. (2013). Pharmacist and general practitioner
ambivalence about providing written medicine information to patients-a qualitative
study. Research in Social and Administrative Pharmacy, 9(5), 517-30.
Kim, K., Han, Y., and Kim, J.S. (2017). Nurses' and patients' perceptions of privacy
protection behaviours and information provision. Nursing Ethics, 24(5), 598-611.
King, C. R., Gerard, S., and Rapp, C. G. (2018). Essential Knowledge for CNL and APRN
Nurse Leaders. Springer Publishing Company. New York City, United States.
Kourkouta, L., and Papathanasiou, I. V. (2014). Communication in Nursing Practice. Materia
Socio-Medica, 26(1), pp. 65–67.
Lega, F., Prenestini, A., and Rosso, M. (2017). Leadership research in healthcare: A realist
review. Health Services Management Research, 30(2), 94-104.
Liukka, M., Hupli, M., and Turunen, H. (2018). How transformational leadership appears in
action with adverse events? A study for Finnish nurse manager. Journal of Nursing
Management, 26(6), 639-646.
Manchester, J., Gray-Miceli, D.L., Metcalf, J.A., Paolini, C.A., Napier, A.H., Coogle, C.L.,…
and Owens, M.G. (2014). Facilitating Lewin's change model with collaborative
evaluation in promoting evidence-based practices of health professionals. Evaluation
and Program Planning, 47, 82-90.
McCarthy, D.M., Buckley, B.A., Engel, K.G., Forth, V.E., Adams, J.G.,..Cameron, K.A.
(2013). Understanding patient-provider conversations: what are we talking about?
Academic Emergency Medicine, 20(5), 441–8.
Nelson-Brantley, H.V., and Ford, D.J. (2017). Leading change: a concept analysis. Journal of
Advanced Nursing, 73(4), 834-846.
Newell, S., and Jordan, Z. (2015). The patient experience of patient-centered communication
with nurses in the hospital setting: a qualitative systematic review protocol. JBI
Database of Systematic Reviews and Implementation Reports, 13(1), 76-87.
10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Romaniuk, P., and Szromek, A.R. (2016). The evolution of the health system outcomes in
Central and Eastern Europe and their association with social, economic and political
factors: an analysis of 25 years of transition. BMC Health Services Research, 16, 95.
doi: 10.1186/s12913-016-1344-3.
Saravo, B., Netzel, J., and Kiesewetter, J. (2017). The need for strong clinical leaders -
Transformational and transactional leadership as a framework for resident leadership
training. PLoS One, 12(8), e0183019. doi: 10.1371/journal.pone.0183019.
Schnock, K.O., Ravindran, S.S, Fladger, A., Leone, K., Williams, D.M., Dwyer, C.L.,…and
Gazarian, P. (2017). Identifying Information Resources for Patients in the Intensive
Care Unit and Their Families. Critical Care Nurse, 37(6), e10-e16.
Shirey, M.R. (2013). Lewin's Theory of Planned Change as a strategic resource. Journal of
Nursing Administration, 43(2), 69-72.
Slatyer, S., Coventry, L.L., Twigg, D., and Davis, S. (2016). Professional practice models for
nursing: a review of the literature and synthesis of key components. Journal of
Nursing Management, 24(2), 139-50.
Smith, P.O. (2015). Leadership in Academic Health Centers: Transactional and
Transformational Leadership. Journal of Clinical Psychology in Medical Settings,
22(4), 228-31.
Snowdon, A.W. (2017). A Blueprint for Innovation to Achieve Health System
Transformation. Healthcare Papers, 16(3), 8-11.
Tandon, R., and Kaushik, P. (2015). Quality of Life and Interpersonal Communication among
Nursing Professionals. International Journal of Nursing Studies, 3(3), 25-329.
Vaismoradi, M., Griffiths, P., Turunen, H., and Jordan, S. (2016). Transformational
leadership in nursing and medication safety education: a discussion paper. Journal of
Nursing Management, 24(7), 970-980.
Vertino, K.A. (2014). Effective Interpersonal Communication: A Practical Guide to Improve
Your Life. Online journal of issues in nursing, 19(3), 1.
Wall, S. (2014). Self-employed nurses as change agents in healthcare: strategies,
consequences, and possibilities. Journal of Health Organization and Management,
28(4), 511-31.
Wojciechowski, E., Pearsall, T., Murphy, P., and French, E. A. (2016). Case Review:
Integrating Lewin’s Theory with Lean’s System Approach for Change. Online
journal of issues in nursing, 21(2), 4. doi: 10.3912/OJIN.Vol21No02Man04.
Xenikou, A. (2017). Transformational Leadership, Transactional Contingent Reward, and
Organizational Identification: The Mediating Effect of Perceived Innovation and Goal
Culture Orientations. Frontiers in Psychology, 8, 1754. doi:
10.3389/fpsyg.2017.01754.
11
Central and Eastern Europe and their association with social, economic and political
factors: an analysis of 25 years of transition. BMC Health Services Research, 16, 95.
doi: 10.1186/s12913-016-1344-3.
Saravo, B., Netzel, J., and Kiesewetter, J. (2017). The need for strong clinical leaders -
Transformational and transactional leadership as a framework for resident leadership
training. PLoS One, 12(8), e0183019. doi: 10.1371/journal.pone.0183019.
Schnock, K.O., Ravindran, S.S, Fladger, A., Leone, K., Williams, D.M., Dwyer, C.L.,…and
Gazarian, P. (2017). Identifying Information Resources for Patients in the Intensive
Care Unit and Their Families. Critical Care Nurse, 37(6), e10-e16.
Shirey, M.R. (2013). Lewin's Theory of Planned Change as a strategic resource. Journal of
Nursing Administration, 43(2), 69-72.
Slatyer, S., Coventry, L.L., Twigg, D., and Davis, S. (2016). Professional practice models for
nursing: a review of the literature and synthesis of key components. Journal of
Nursing Management, 24(2), 139-50.
Smith, P.O. (2015). Leadership in Academic Health Centers: Transactional and
Transformational Leadership. Journal of Clinical Psychology in Medical Settings,
22(4), 228-31.
Snowdon, A.W. (2017). A Blueprint for Innovation to Achieve Health System
Transformation. Healthcare Papers, 16(3), 8-11.
Tandon, R., and Kaushik, P. (2015). Quality of Life and Interpersonal Communication among
Nursing Professionals. International Journal of Nursing Studies, 3(3), 25-329.
Vaismoradi, M., Griffiths, P., Turunen, H., and Jordan, S. (2016). Transformational
leadership in nursing and medication safety education: a discussion paper. Journal of
Nursing Management, 24(7), 970-980.
Vertino, K.A. (2014). Effective Interpersonal Communication: A Practical Guide to Improve
Your Life. Online journal of issues in nursing, 19(3), 1.
Wall, S. (2014). Self-employed nurses as change agents in healthcare: strategies,
consequences, and possibilities. Journal of Health Organization and Management,
28(4), 511-31.
Wojciechowski, E., Pearsall, T., Murphy, P., and French, E. A. (2016). Case Review:
Integrating Lewin’s Theory with Lean’s System Approach for Change. Online
journal of issues in nursing, 21(2), 4. doi: 10.3912/OJIN.Vol21No02Man04.
Xenikou, A. (2017). Transformational Leadership, Transactional Contingent Reward, and
Organizational Identification: The Mediating Effect of Perceived Innovation and Goal
Culture Orientations. Frontiers in Psychology, 8, 1754. doi:
10.3389/fpsyg.2017.01754.
11
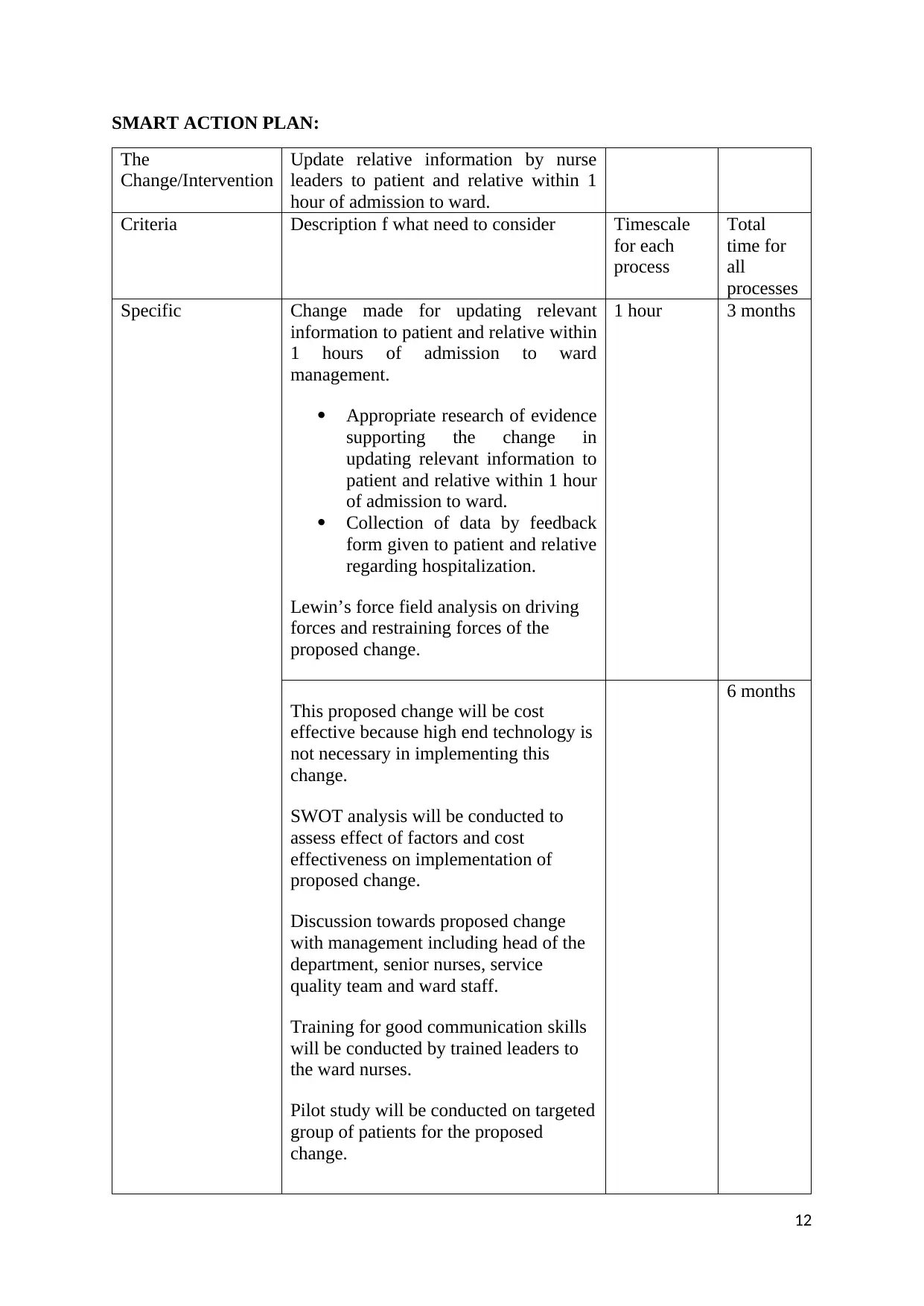
SMART ACTION PLAN:
The
Change/Intervention
Update relative information by nurse
leaders to patient and relative within 1
hour of admission to ward.
Criteria Description f what need to consider Timescale
for each
process
Total
time for
all
processes
Specific Change made for updating relevant
information to patient and relative within
1 hours of admission to ward
management.
Appropriate research of evidence
supporting the change in
updating relevant information to
patient and relative within 1 hour
of admission to ward.
Collection of data by feedback
form given to patient and relative
regarding hospitalization.
Lewin’s force field analysis on driving
forces and restraining forces of the
proposed change.
1 hour 3 months
This proposed change will be cost
effective because high end technology is
not necessary in implementing this
change.
SWOT analysis will be conducted to
assess effect of factors and cost
effectiveness on implementation of
proposed change.
Discussion towards proposed change
with management including head of the
department, senior nurses, service
quality team and ward staff.
Training for good communication skills
will be conducted by trained leaders to
the ward nurses.
Pilot study will be conducted on targeted
group of patients for the proposed
change.
6 months
12
The
Change/Intervention
Update relative information by nurse
leaders to patient and relative within 1
hour of admission to ward.
Criteria Description f what need to consider Timescale
for each
process
Total
time for
all
processes
Specific Change made for updating relevant
information to patient and relative within
1 hours of admission to ward
management.
Appropriate research of evidence
supporting the change in
updating relevant information to
patient and relative within 1 hour
of admission to ward.
Collection of data by feedback
form given to patient and relative
regarding hospitalization.
Lewin’s force field analysis on driving
forces and restraining forces of the
proposed change.
1 hour 3 months
This proposed change will be cost
effective because high end technology is
not necessary in implementing this
change.
SWOT analysis will be conducted to
assess effect of factors and cost
effectiveness on implementation of
proposed change.
Discussion towards proposed change
with management including head of the
department, senior nurses, service
quality team and ward staff.
Training for good communication skills
will be conducted by trained leaders to
the ward nurses.
Pilot study will be conducted on targeted
group of patients for the proposed
change.
6 months
12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





