Acute Care Nursing: Diabetes Type 2 Assignment Report
VerifiedAdded on 2022/12/19
|13
|3437
|1
Report
AI Summary
This nursing assignment report delves into Type 2 diabetes, exploring its pathophysiology, which includes impaired insulin secretion and insulin resistance, and its causes, such as genetic and environmental factors like obesity, lack of exercise, and aging. The report examines the impact of these factors on patient health, with a case study of an individual named Bill. It also details potential management approaches, including controlling hypertension through pharmacological and non-pharmacological therapies. At the nursing level, the report recommends alcohol abstinence, dietary modifications, and increased physical activity. Moreover, the report outlines a patient education plan, emphasizing self-management, nutrition, emotional health, and the importance of healthcare provider consultations. The education plan includes key times for evaluation and adjustment, and a list of scenarios when patients should seek professional medical help.

Running Head: NURSING ASSIGNMENT. 1
Nursing assignment
Student’s Name
Institution Affiliation
Date
Nursing assignment
Student’s Name
Institution Affiliation
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING ASSIGNMENT. 2
Introduction
Diabetes is a category of disorders that occur metabolically and are featured by
hyperglycaemic conditions that result from an inadequate insulin action. The fundamental
pathophysiological characteristics of diabetes type 2 presenting a significant number of cases
worldwide are an appreciated insulin resistance as well as an impeded insulin secretion (Care,
2019). Progress of type 2 diabetes over some time is highlighted by the impediment of the
beta pancreatic cell function. Additionally, type 2 diabetes is brought about by some genetic
factors which are directly intertwined to appreciating insulin resistance and impending insulin
secretion and environmental elements which are overeating, obesity, stress, lack of exercise
and lastly aging.
Diabetes type 2 involves different extents of environmental factors as well as multiple genes.
Furthermore, the development of type 2 diabetes among many people has directly linked to
the same condition or maybe lesser diabetic conditions existing in the family line (Dunbar et
al., 2014). Type 2 diabetes is also presumed to associate with genetic abnormalities in
molecules interlinked with the glucose metabolism regulatory systems (Nolan, 2011). When
assessments of affected individual's genes are made while targeting at glucose-stimulated
insulin secretion of pancreatic beta cells as well as the molecules containing the molecular
operation for insulin action, genetic anomalies are defined and can be independent factors to
the type 2 diabetes such as those in mitochondrial genes, glucokinase genes as well as insulin
receptor genes.
Pathophysiology
Impending insulin secretion and appreciating insulin resistance results in the
development of type 2 diabetes as mentioned above. An impending insulin secretion means
depreciating responsiveness to glucose, so impaired glucose tolerance abbreviated as IGT is
Introduction
Diabetes is a category of disorders that occur metabolically and are featured by
hyperglycaemic conditions that result from an inadequate insulin action. The fundamental
pathophysiological characteristics of diabetes type 2 presenting a significant number of cases
worldwide are an appreciated insulin resistance as well as an impeded insulin secretion (Care,
2019). Progress of type 2 diabetes over some time is highlighted by the impediment of the
beta pancreatic cell function. Additionally, type 2 diabetes is brought about by some genetic
factors which are directly intertwined to appreciating insulin resistance and impending insulin
secretion and environmental elements which are overeating, obesity, stress, lack of exercise
and lastly aging.
Diabetes type 2 involves different extents of environmental factors as well as multiple genes.
Furthermore, the development of type 2 diabetes among many people has directly linked to
the same condition or maybe lesser diabetic conditions existing in the family line (Dunbar et
al., 2014). Type 2 diabetes is also presumed to associate with genetic abnormalities in
molecules interlinked with the glucose metabolism regulatory systems (Nolan, 2011). When
assessments of affected individual's genes are made while targeting at glucose-stimulated
insulin secretion of pancreatic beta cells as well as the molecules containing the molecular
operation for insulin action, genetic anomalies are defined and can be independent factors to
the type 2 diabetes such as those in mitochondrial genes, glucokinase genes as well as insulin
receptor genes.
Pathophysiology
Impending insulin secretion and appreciating insulin resistance results in the
development of type 2 diabetes as mentioned above. An impending insulin secretion means
depreciating responsiveness to glucose, so impaired glucose tolerance abbreviated as IGT is
NURSING ASSIGNMENT. 3
instigated by a diminish in glucose-responsive initial phase insulin secretion and a lessen in
surplus insulin secretion after having meals often causes postprandial hyperglycemia (Kahn,
2014). Individuals with obesity outlay an initial phase secretory response. A diminish in the
initial phase secretion is an essential segment in the prevalence of type 2 diabetes and is
considered an elemental pathophysiological dynamic during type 2 onset. Impeding insulin
secretion appears to be progressive, and a progression in itself means that lipo-toxicity, as
well as glucose toxicity, will be experienced.
Appreciating insulin resistance that the insulin in the body will not exert abundant
action with respect to the blood concentration. The stultification of insulin action in primary
target body organs, for instance, the muscles and the liver is a recurring pathophysiological
characteristic of type 2 diabetes. Insulin resistance grows and outstretches itself preceding the
onset of the disease. Insulin resistance is directly intertwined with environmental factors such
as free fatty acids, hyperglycemia, the inflammatory mechanism among others as well as
genetic factors.
It is also intertwined with genetic factors such as insulin receptors and insulin receptor
substrate abbreviated as IRS-1 gene polymorphisms. These do affect not only the insulin
signals but also change the polymorphisms of thrifty genes, for instance, the uncoupling
protein gene abbreviated as UCP and the beta3 adrenergic receptor gene which are auxiliary
with visceral obesity and enhance body insulin resistance. Additional elements that are
crucial to the impediment of insulin secretion and obstruction of insulin signalling are
inflammatory conciliators as well as glucolipotoxicity arbiters (Morris, 2012).
The leading causes of exceeding mortality rates in type 2 diabetes are cardiovascular
diseases as well as atherosclerosis diseases which are intertwined to metabolic syndrome as
well as hepatic insulin resistance. Increased production of very low-density lipoprotein causes
instigated by a diminish in glucose-responsive initial phase insulin secretion and a lessen in
surplus insulin secretion after having meals often causes postprandial hyperglycemia (Kahn,
2014). Individuals with obesity outlay an initial phase secretory response. A diminish in the
initial phase secretion is an essential segment in the prevalence of type 2 diabetes and is
considered an elemental pathophysiological dynamic during type 2 onset. Impeding insulin
secretion appears to be progressive, and a progression in itself means that lipo-toxicity, as
well as glucose toxicity, will be experienced.
Appreciating insulin resistance that the insulin in the body will not exert abundant
action with respect to the blood concentration. The stultification of insulin action in primary
target body organs, for instance, the muscles and the liver is a recurring pathophysiological
characteristic of type 2 diabetes. Insulin resistance grows and outstretches itself preceding the
onset of the disease. Insulin resistance is directly intertwined with environmental factors such
as free fatty acids, hyperglycemia, the inflammatory mechanism among others as well as
genetic factors.
It is also intertwined with genetic factors such as insulin receptors and insulin receptor
substrate abbreviated as IRS-1 gene polymorphisms. These do affect not only the insulin
signals but also change the polymorphisms of thrifty genes, for instance, the uncoupling
protein gene abbreviated as UCP and the beta3 adrenergic receptor gene which are auxiliary
with visceral obesity and enhance body insulin resistance. Additional elements that are
crucial to the impediment of insulin secretion and obstruction of insulin signalling are
inflammatory conciliators as well as glucolipotoxicity arbiters (Morris, 2012).
The leading causes of exceeding mortality rates in type 2 diabetes are cardiovascular
diseases as well as atherosclerosis diseases which are intertwined to metabolic syndrome as
well as hepatic insulin resistance. Increased production of very low-density lipoprotein causes
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NURSING ASSIGNMENT. 4
dense, small and atherogenic low-density lipoprotein (Ozougwu, 2013). The manifestation of
insulin resistance for type 2 diabetes is NAFLD which is the abbreviation for non-alcoholic
fatty liver disease. Glucagon and insulin secretion defects in type 2 diabetes are as defined
above. However, eliminating requires increased physical activity and avoiding obesity both
of which Bill did not explain his susceptibility to the disease as well as the symptoms he
would face.
As mentioned above, obesity, aging, lack of exercise meaning there is deficient
consumption of energy are the key factors to diabetes type 2. Other factors causing diabetes
type 2 include consuming alcohol as well as taking a smoke (Nolan, 2011). Bill fits in almost
all the factors attributing to his condition. His age is 58 years' old which depicts aging. He
would smoke 12775 packs of smoke every year for 35 years and has a history of heavy
consumption of alcohol. Calculating his body mass index from two years ago when he was so
active in the activities, he was obese with a BMI of 50.94.
Furthermore, his mother had been diagnosed with the same condition and passed on
from the disease. All these factors explain the prevalence of his type 2 diabetes. He was
obese, and with such a body mass index, he must have had visceral fat obesity and did not
engage in exercises which results in a depreciating muscle mass inducing his insulin
resistance. This has been noted to increase rapidly especially among high-aged individuals as
he is as well as middle-aged individuals. His sedentary lifestyle resulted in an increased
intake of sugars and a decreased fiber diet resulting in obesity which in turn factors in a
depreciation of glucose tolerance. Scientifically, mild obesity will lead to an increased risk of
acquiring diabetes especially if the visceral fat mass increases.
Potential management approaches.
dense, small and atherogenic low-density lipoprotein (Ozougwu, 2013). The manifestation of
insulin resistance for type 2 diabetes is NAFLD which is the abbreviation for non-alcoholic
fatty liver disease. Glucagon and insulin secretion defects in type 2 diabetes are as defined
above. However, eliminating requires increased physical activity and avoiding obesity both
of which Bill did not explain his susceptibility to the disease as well as the symptoms he
would face.
As mentioned above, obesity, aging, lack of exercise meaning there is deficient
consumption of energy are the key factors to diabetes type 2. Other factors causing diabetes
type 2 include consuming alcohol as well as taking a smoke (Nolan, 2011). Bill fits in almost
all the factors attributing to his condition. His age is 58 years' old which depicts aging. He
would smoke 12775 packs of smoke every year for 35 years and has a history of heavy
consumption of alcohol. Calculating his body mass index from two years ago when he was so
active in the activities, he was obese with a BMI of 50.94.
Furthermore, his mother had been diagnosed with the same condition and passed on
from the disease. All these factors explain the prevalence of his type 2 diabetes. He was
obese, and with such a body mass index, he must have had visceral fat obesity and did not
engage in exercises which results in a depreciating muscle mass inducing his insulin
resistance. This has been noted to increase rapidly especially among high-aged individuals as
he is as well as middle-aged individuals. His sedentary lifestyle resulted in an increased
intake of sugars and a decreased fiber diet resulting in obesity which in turn factors in a
depreciation of glucose tolerance. Scientifically, mild obesity will lead to an increased risk of
acquiring diabetes especially if the visceral fat mass increases.
Potential management approaches.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING ASSIGNMENT. 5
Failure to treat hypertension or treating it poorly can substantially result in an
accelerated progression or development of the macrovascular and microvascular
complications that lead to diabetes. Controlling truculent blood pressure results in an
improvement in the affected individual's health outcome as well as reduce the cost of
accessing health care. According to ADA, almost two-thirds of individuals worldwide do not
have their blood pressure readings as per the set target ranges (American Diabetes
Association, 2013). Effectual hypertensive administrations offer a maxim in non-
pharmacological therapies, diffuse the possible risks of medication interlinked after effects,
diminish the inauspicious impacts on glucose control and offer appropriate renal and cardiac
protection.
Depreciating blood pressure in persons with diabetic conditions as well as those with
hypertension decreases the prevalence rates to acquire microvascular and macrovascular
complications. At a medical level, clinical trials applying the use of antihypertensive
elements such as Empagliflozin (Barnett et al., 2014), have shown that self-effacing depletions
in blood pressure at a range of about nine to eleven millimetres mercury systolic and two to
nine millimetres mercury diastolic deplete cardiovascular disease events by almost thirty-five
percent to seventy percent and diminish microvascular hurdles which range from
nephropathy to retinopathy by twenty-five percent to forty-five percent in two to five years of
use (Tikkanen, 2015).
Nevertheless, clinical and medical attempts focusing on control of diabetic
hypertensive conditions have illustrated the significant improvement of cardiovascular
diseases as well as microvascular results with the desired range of diastolic blood pressure
clocking at less than eighty millimetres per mercury (Pecoits‐Filho, 2012). For the presaging
more severe systolic blood pressures, medical attempts to control diabetic hypertensive
conditions along with following observed data conducted by certified clinical trials have
Failure to treat hypertension or treating it poorly can substantially result in an
accelerated progression or development of the macrovascular and microvascular
complications that lead to diabetes. Controlling truculent blood pressure results in an
improvement in the affected individual's health outcome as well as reduce the cost of
accessing health care. According to ADA, almost two-thirds of individuals worldwide do not
have their blood pressure readings as per the set target ranges (American Diabetes
Association, 2013). Effectual hypertensive administrations offer a maxim in non-
pharmacological therapies, diffuse the possible risks of medication interlinked after effects,
diminish the inauspicious impacts on glucose control and offer appropriate renal and cardiac
protection.
Depreciating blood pressure in persons with diabetic conditions as well as those with
hypertension decreases the prevalence rates to acquire microvascular and macrovascular
complications. At a medical level, clinical trials applying the use of antihypertensive
elements such as Empagliflozin (Barnett et al., 2014), have shown that self-effacing depletions
in blood pressure at a range of about nine to eleven millimetres mercury systolic and two to
nine millimetres mercury diastolic deplete cardiovascular disease events by almost thirty-five
percent to seventy percent and diminish microvascular hurdles which range from
nephropathy to retinopathy by twenty-five percent to forty-five percent in two to five years of
use (Tikkanen, 2015).
Nevertheless, clinical and medical attempts focusing on control of diabetic
hypertensive conditions have illustrated the significant improvement of cardiovascular
diseases as well as microvascular results with the desired range of diastolic blood pressure
clocking at less than eighty millimetres per mercury (Pecoits‐Filho, 2012). For the presaging
more severe systolic blood pressures, medical attempts to control diabetic hypertensive
conditions along with following observed data conducted by certified clinical trials have
NURSING ASSIGNMENT. 6
shown that support enhanced cardiovascular diseases along with microvascular conditions for
a target systolic blood pressure lesser that one hundred and thirty for every eighty millimetres
mercury significantly improve. This explains why many local, national and international
measures and guidelines recommend a target blood pressure of one hundred and thirty for
every eighty millimetres mercury for persons with diabetic conditions.
Diabetic individuals with a complete urinary protein to creatinine and proteinuria ratio
of above grams per milligram; per the measures and guidelines offered by the National
Kidney Foundation (NKF), it recommends that a target systolic blood pressure of lesser than
one hundred and twenty-five for every hundred millimetres mercury should be retained. In
the case the blood pressure is lowered to smaller than one hundred and ten per hundred
millimetres mercury, then cardiovascular disease conditions, as well as renal conditions,
would only worsen rather than get better. The majority of persons with diabetic hypertensive
conditions and also have a conventional renal function need two to three combinations of
antihypertensive elements so that the blood pressure can lower to one hundred and thirty per
eighty millimetres mercury. For persons with collateral chronic kidney conditions, they might
need three or more antihypertensive elements (Pradeepa, 2013).
At the nursing level, management can be achieved by recommending alcohol abstinence or
restriction to only two drinks every day for men and only one bottle for ladies. Additionally,
recommendations of a better diet will significantly aid in managing the condition (Paterson et
al., 2016). That is, consuming a portion of food with about five fruits a day, five vegetables a
day, seven whole grains a day, an average of 1200mg of calcium daily, 505mg magnesium a
day, 4695 mg of potassium daily and lastly limiting cholesterol intake to 145mg and saturated
fat at only five percent daily. Additionally, advising the patient to engage in physical
activities for about forty minutes and stopping to smoke cigarettes will substantially aid the
shown that support enhanced cardiovascular diseases along with microvascular conditions for
a target systolic blood pressure lesser that one hundred and thirty for every eighty millimetres
mercury significantly improve. This explains why many local, national and international
measures and guidelines recommend a target blood pressure of one hundred and thirty for
every eighty millimetres mercury for persons with diabetic conditions.
Diabetic individuals with a complete urinary protein to creatinine and proteinuria ratio
of above grams per milligram; per the measures and guidelines offered by the National
Kidney Foundation (NKF), it recommends that a target systolic blood pressure of lesser than
one hundred and twenty-five for every hundred millimetres mercury should be retained. In
the case the blood pressure is lowered to smaller than one hundred and ten per hundred
millimetres mercury, then cardiovascular disease conditions, as well as renal conditions,
would only worsen rather than get better. The majority of persons with diabetic hypertensive
conditions and also have a conventional renal function need two to three combinations of
antihypertensive elements so that the blood pressure can lower to one hundred and thirty per
eighty millimetres mercury. For persons with collateral chronic kidney conditions, they might
need three or more antihypertensive elements (Pradeepa, 2013).
At the nursing level, management can be achieved by recommending alcohol abstinence or
restriction to only two drinks every day for men and only one bottle for ladies. Additionally,
recommendations of a better diet will significantly aid in managing the condition (Paterson et
al., 2016). That is, consuming a portion of food with about five fruits a day, five vegetables a
day, seven whole grains a day, an average of 1200mg of calcium daily, 505mg magnesium a
day, 4695 mg of potassium daily and lastly limiting cholesterol intake to 145mg and saturated
fat at only five percent daily. Additionally, advising the patient to engage in physical
activities for about forty minutes and stopping to smoke cigarettes will substantially aid the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NURSING ASSIGNMENT. 7
individuals affected to manage it and prevent others from obtaining the condition (Nolan,
2011).
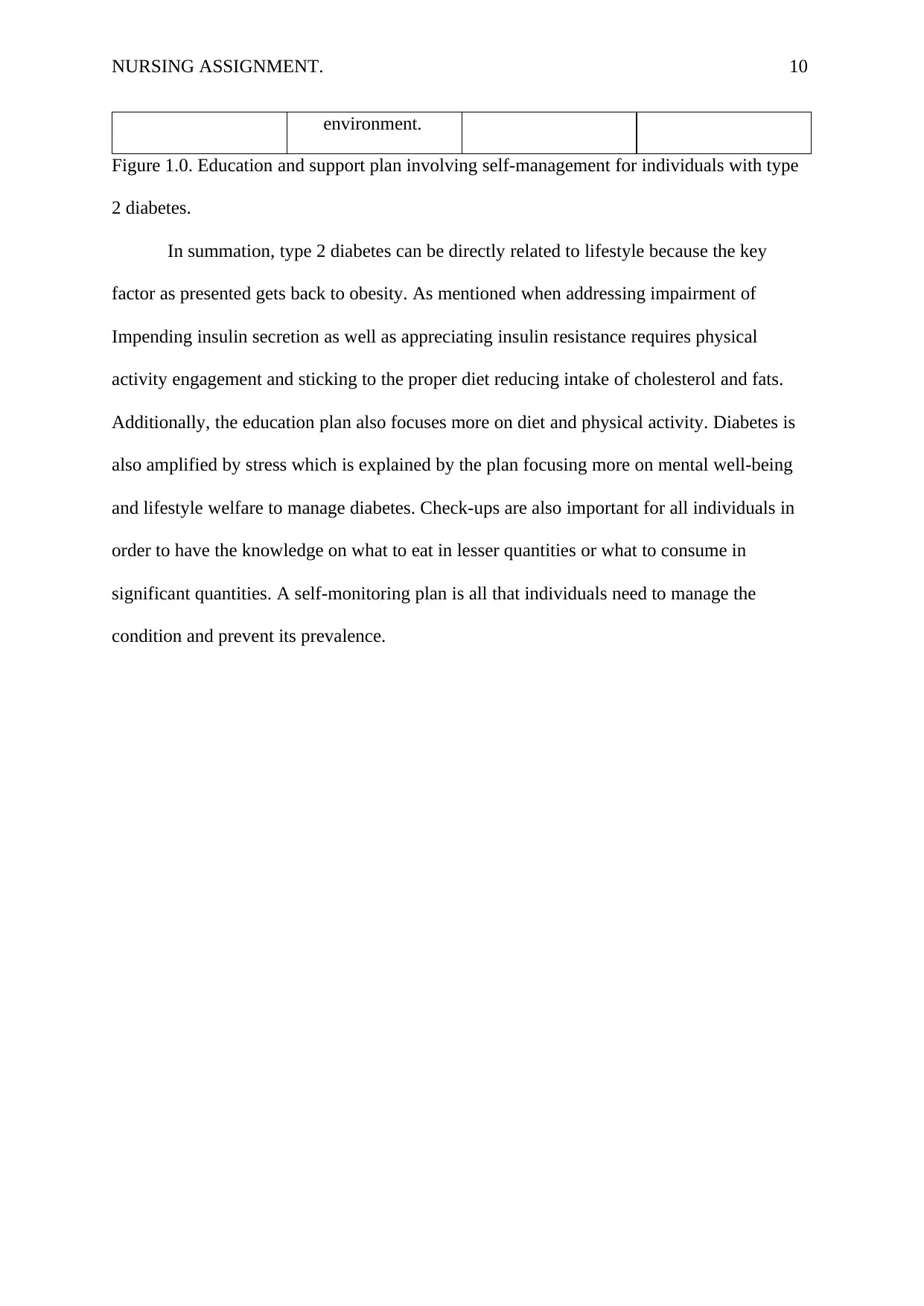
Education plan
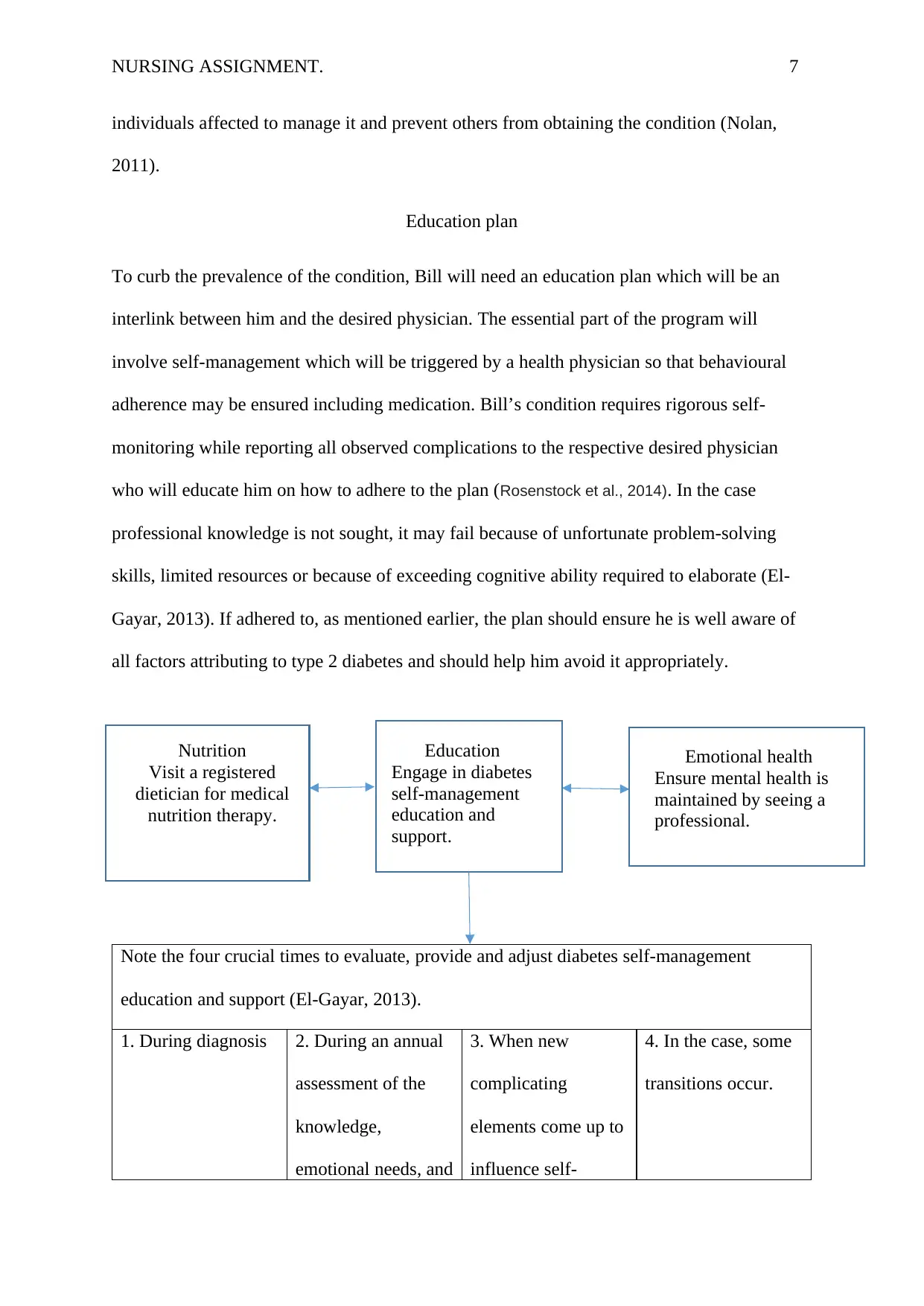
To curb the prevalence of the condition, Bill will need an education plan which will be an
interlink between him and the desired physician. The essential part of the program will
involve self-management which will be triggered by a health physician so that behavioural
adherence may be ensured including medication. Bill’s condition requires rigorous self-
monitoring while reporting all observed complications to the respective desired physician
who will educate him on how to adhere to the plan (Rosenstock et al., 2014). In the case
professional knowledge is not sought, it may fail because of unfortunate problem-solving
skills, limited resources or because of exceeding cognitive ability required to elaborate (El-
Gayar, 2013). If adhered to, as mentioned earlier, the plan should ensure he is well aware of
all factors attributing to type 2 diabetes and should help him avoid it appropriately.
Note the four crucial times to evaluate, provide and adjust diabetes self-management
education and support (El-Gayar, 2013).
1. During diagnosis 2. During an annual
assessment of the
knowledge,
emotional needs, and
3. When new
complicating
elements come up to
influence self-
4. In the case, some
transitions occur.
Nutrition
Visit a registered
dietician for medical
nutrition therapy.
Education
Engage in diabetes
self-management
education and
support.
Emotional health
Ensure mental health is
maintained by seeing a
professional.
individuals affected to manage it and prevent others from obtaining the condition (Nolan,
2011).
Education plan
To curb the prevalence of the condition, Bill will need an education plan which will be an
interlink between him and the desired physician. The essential part of the program will
involve self-management which will be triggered by a health physician so that behavioural
adherence may be ensured including medication. Bill’s condition requires rigorous self-
monitoring while reporting all observed complications to the respective desired physician
who will educate him on how to adhere to the plan (Rosenstock et al., 2014). In the case
professional knowledge is not sought, it may fail because of unfortunate problem-solving
skills, limited resources or because of exceeding cognitive ability required to elaborate (El-
Gayar, 2013). If adhered to, as mentioned earlier, the plan should ensure he is well aware of
all factors attributing to type 2 diabetes and should help him avoid it appropriately.
Note the four crucial times to evaluate, provide and adjust diabetes self-management
education and support (El-Gayar, 2013).
1. During diagnosis 2. During an annual
assessment of the
knowledge,
emotional needs, and
3. When new
complicating
elements come up to
influence self-
4. In the case, some
transitions occur.
Nutrition
Visit a registered
dietician for medical
nutrition therapy.
Education
Engage in diabetes
self-management
education and
support.
Emotional health
Ensure mental health is
maintained by seeing a
professional.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING ASSIGNMENT. 8
nutrition. management.
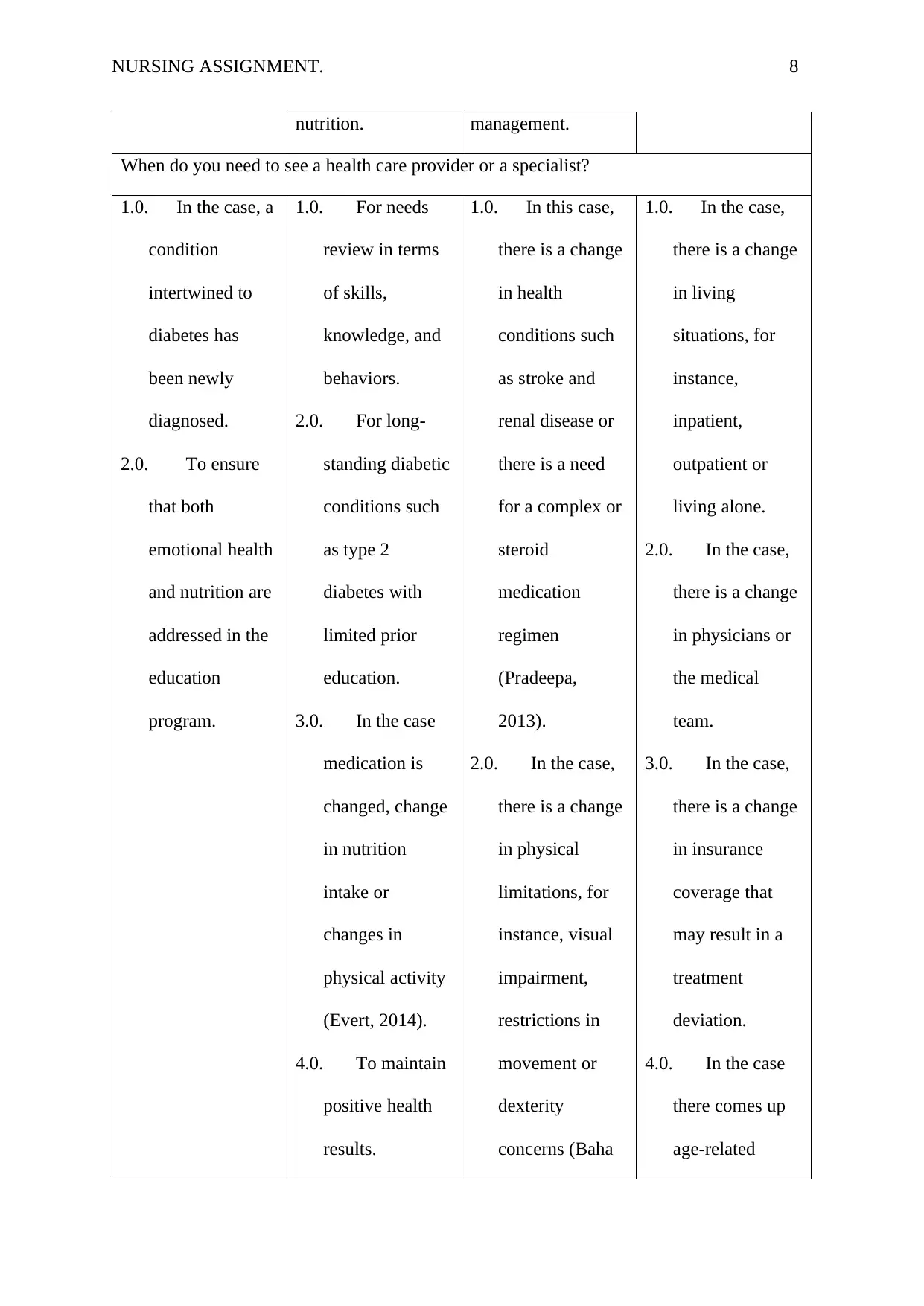
When do you need to see a health care provider or a specialist?
1.0. In the case, a
condition
intertwined to
diabetes has
been newly
diagnosed.
2.0. To ensure
that both
emotional health
and nutrition are
addressed in the
education
program.
1.0. For needs
review in terms
of skills,
knowledge, and
behaviors.
2.0. For long-
standing diabetic
conditions such
as type 2
diabetes with
limited prior
education.
3.0. In the case
medication is
changed, change
in nutrition
intake or
changes in
physical activity
(Evert, 2014).
4.0. To maintain
positive health
results.
1.0. In this case,
there is a change
in health
conditions such
as stroke and
renal disease or
there is a need
for a complex or
steroid
medication
regimen
(Pradeepa,
2013).
2.0. In the case,
there is a change
in physical
limitations, for
instance, visual
impairment,
restrictions in
movement or
dexterity
concerns (Baha
1.0. In the case,
there is a change
in living
situations, for
instance,
inpatient,
outpatient or
living alone.
2.0. In the case,
there is a change
in physicians or
the medical
team.
3.0. In the case,
there is a change
in insurance
coverage that
may result in a
treatment
deviation.
4.0. In the case
there comes up
age-related
nutrition. management.
When do you need to see a health care provider or a specialist?
1.0. In the case, a
condition
intertwined to
diabetes has
been newly
diagnosed.
2.0. To ensure
that both
emotional health
and nutrition are
addressed in the
education
program.
1.0. For needs
review in terms
of skills,
knowledge, and
behaviors.
2.0. For long-
standing diabetic
conditions such
as type 2
diabetes with
limited prior
education.
3.0. In the case
medication is
changed, change
in nutrition
intake or
changes in
physical activity
(Evert, 2014).
4.0. To maintain
positive health
results.
1.0. In this case,
there is a change
in health
conditions such
as stroke and
renal disease or
there is a need
for a complex or
steroid
medication
regimen
(Pradeepa,
2013).
2.0. In the case,
there is a change
in physical
limitations, for
instance, visual
impairment,
restrictions in
movement or
dexterity
concerns (Baha
1.0. In the case,
there is a change
in living
situations, for
instance,
inpatient,
outpatient or
living alone.
2.0. In the case,
there is a change
in physicians or
the medical
team.
3.0. In the case,
there is a change
in insurance
coverage that
may result in a
treatment
deviation.
4.0. In the case
there comes up
age-related
NURSING ASSIGNMENT. 9
5.0. In the case,
new life
situations or new
demands come
up.
6.0. In the case
weight concerns
as well as
nutrition
interests prevail
(Nolan, 2011).
7.0. In the case
of unexplained
hypoglycaemia
(Inzucchi, 2015).
8.0. For support
to attain and
sustain
behaviour
change.
9.0. In the case, a
new disease is
developed in the
body or a change
in the
Doran, 2013).
3.0. In the case,
there is a change
in the basic
living needs, for
instance, assess
to food or
recurring
financial
limitations.
4.0. In the case,
there is a change
in emotional
factors such as
clinical
depression or
anxiety.
changes that
affect self-care
and cognitive
abilities
(American
Diabetes
Association,
2013).
5.0. In the case,
new life
situations or new
demands come
up.
6.0. In the case
weight concerns
as well as
nutrition
interests prevail
(Nolan, 2011).
7.0. In the case
of unexplained
hypoglycaemia
(Inzucchi, 2015).
8.0. For support
to attain and
sustain
behaviour
change.
9.0. In the case, a
new disease is
developed in the
body or a change
in the
Doran, 2013).
3.0. In the case,
there is a change
in the basic
living needs, for
instance, assess
to food or
recurring
financial
limitations.
4.0. In the case,
there is a change
in emotional
factors such as
clinical
depression or
anxiety.
changes that
affect self-care
and cognitive
abilities
(American
Diabetes
Association,
2013).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NURSING ASSIGNMENT. 10
environment.
Figure 1.0. Education and support plan involving self-management for individuals with type
2 diabetes.
In summation, type 2 diabetes can be directly related to lifestyle because the key
factor as presented gets back to obesity. As mentioned when addressing impairment of
Impending insulin secretion as well as appreciating insulin resistance requires physical
activity engagement and sticking to the proper diet reducing intake of cholesterol and fats.
Additionally, the education plan also focuses more on diet and physical activity. Diabetes is
also amplified by stress which is explained by the plan focusing more on mental well-being
and lifestyle welfare to manage diabetes. Check-ups are also important for all individuals in
order to have the knowledge on what to eat in lesser quantities or what to consume in
significant quantities. A self-monitoring plan is all that individuals need to manage the
condition and prevent its prevalence.
environment.
Figure 1.0. Education and support plan involving self-management for individuals with type
2 diabetes.
In summation, type 2 diabetes can be directly related to lifestyle because the key
factor as presented gets back to obesity. As mentioned when addressing impairment of
Impending insulin secretion as well as appreciating insulin resistance requires physical
activity engagement and sticking to the proper diet reducing intake of cholesterol and fats.
Additionally, the education plan also focuses more on diet and physical activity. Diabetes is
also amplified by stress which is explained by the plan focusing more on mental well-being
and lifestyle welfare to manage diabetes. Check-ups are also important for all individuals in
order to have the knowledge on what to eat in lesser quantities or what to consume in
significant quantities. A self-monitoring plan is all that individuals need to manage the
condition and prevent its prevalence.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING ASSIGNMENT. 11
References
American Diabetes Association. (2013). Executive summary: Standards of medical care in
diabetes—2013. Diabetes care, 36(Supplement 1), S4-S10.
Baha Doran, Z., Mirmiran, P., & Azizi, F. (2013). Dietary polyphenols as potential
nutraceuticals in management of diabetes: a review. Journal of diabetes & metabolic
disorders, 12(1), 43.
Barnett, A. H., Mithal, A., Manassie, J., Jones, R., Rattunde, H., Woerle, H. J., ... & EMPA-REG
RENAL trial investigators. (2014). Efficacy and safety of empagliflozin added to existing antidiabetes
treatment in patients with type 2 diabetes and chronic kidney disease: a randomised, double-blind,
placebo-controlled trial. The lancet Diabetes & endocrinology, 2(5), 369-384.
Care, D. (2019). Standards of Medical Care in Diabetes 2019. Diabetes Care, 42, S81.
Dunbar, J. A., Jayawardena, A., Johnson, G., Roger, K., Timoshanko, A., Versace, V. L., ... & Best, J.
D. (2014). Scaling up diabetes prevention in Victoria, Australia: policy development, implementation,
and evaluation. Diabetes Care, 37(4), 934-942.
El-Gayar, O., Timsina, P., Nawar, N., & Eid, W. (2013). Mobile applications for diabetes
self-management: status and potential. Journal of diabetes science and technology, 7(1), 247-
262.
Evert, A. B., Boucher, J. L., Cypress, M., Dunbar, S. A., Franz, M. J., Mayer-Davis, E. J., ...
& Yancy, W. S. (2014). Nutrition therapy recommendations for the management of adults
with diabetes. Diabetes care, 37(Supplement 1), S120-S143.
Inzucchi, S. E., Bergenstal, R. M., Buse, J. B., Diamant, M., Ferrannini, E., Nauck, M., ... &
Matthews, D. R. (2015). Management of hyperglycemia in type 2 diabetes, 2015: a patient-
centered approach: update to a position statement of the American Diabetes Association and
the European Association for the Study of Diabetes. Diabetes care, 38(1), 140-149.
References
American Diabetes Association. (2013). Executive summary: Standards of medical care in
diabetes—2013. Diabetes care, 36(Supplement 1), S4-S10.
Baha Doran, Z., Mirmiran, P., & Azizi, F. (2013). Dietary polyphenols as potential
nutraceuticals in management of diabetes: a review. Journal of diabetes & metabolic
disorders, 12(1), 43.
Barnett, A. H., Mithal, A., Manassie, J., Jones, R., Rattunde, H., Woerle, H. J., ... & EMPA-REG
RENAL trial investigators. (2014). Efficacy and safety of empagliflozin added to existing antidiabetes
treatment in patients with type 2 diabetes and chronic kidney disease: a randomised, double-blind,
placebo-controlled trial. The lancet Diabetes & endocrinology, 2(5), 369-384.
Care, D. (2019). Standards of Medical Care in Diabetes 2019. Diabetes Care, 42, S81.
Dunbar, J. A., Jayawardena, A., Johnson, G., Roger, K., Timoshanko, A., Versace, V. L., ... & Best, J.
D. (2014). Scaling up diabetes prevention in Victoria, Australia: policy development, implementation,
and evaluation. Diabetes Care, 37(4), 934-942.
El-Gayar, O., Timsina, P., Nawar, N., & Eid, W. (2013). Mobile applications for diabetes
self-management: status and potential. Journal of diabetes science and technology, 7(1), 247-
262.
Evert, A. B., Boucher, J. L., Cypress, M., Dunbar, S. A., Franz, M. J., Mayer-Davis, E. J., ...
& Yancy, W. S. (2014). Nutrition therapy recommendations for the management of adults
with diabetes. Diabetes care, 37(Supplement 1), S120-S143.
Inzucchi, S. E., Bergenstal, R. M., Buse, J. B., Diamant, M., Ferrannini, E., Nauck, M., ... &
Matthews, D. R. (2015). Management of hyperglycemia in type 2 diabetes, 2015: a patient-
centered approach: update to a position statement of the American Diabetes Association and
the European Association for the Study of Diabetes. Diabetes care, 38(1), 140-149.
NURSING ASSIGNMENT. 12
Kahn, S. E., Cooper, M. E., & Del Prato, S. (2014). Pathophysiology and treatment of type 2
diabetes: perspectives on the past, present, and future. The Lancet, 383(9922), 1068-1083.
Morris, A. P., Voight, B. F., Teslovich, T. M., Ferreira, T., Segre, A. V., Steinthorsdottir,
V., ... & Prokopenko, I. (2012). Large-scale association analysis provides insights into the
genetic architecture and pathophysiology of type 2 diabetes. Nature genetics, 44(9), 981.
Nolan, C. J., Damm, P., & Prentki, M. (2011). Type 2 diabetes across generations: from
pathophysiology to prevention and management. The Lancet, 378(9786), 169-181.
Ozougwu, J. C., Obimba, K. C., Belonwu, C. D., & Unakalamba, C. B. (2013). The
pathogenesis and pathophysiology of type 1 and type 2 diabetes mellitus. Journal of
Physiology and Pathophysiology, 4(4), 46-57.
Paterson, M. A., Smart, C. E. M., Lopez, P. E., McElduff, P., Attia, J., Morbey, C., & King, B. R.
(2016). Influence of dietary protein on postprandial blood glucose levels in individuals with type 2
diabetes mellitus using intensive insulin therapy. Diabetic Medicine, 33(5), 592-598.
Pecoits‐Filho, R., Bucharles, S., & Barberato, S. H. (2012, January). Diastolic heart failure in
dialysis patients: mechanisms, diagnostic approach, and treatment. In Seminars in
dialysis (Vol. 25, No. 1, pp. 35-41). Oxford, UK: Blackwell Publishing Ltd.
Pradeepa, R. (2013). The rising burden of diabetes and hypertension in southeast asian and
african regions: need for effective strategies for prevention and control in primary health care
settings. International journal of hypertension, 2013.
Rosenstock, J., Jelaska, A., Frappin, G., Salsali, A., Kim, G., Woerle, H. J., & Broedl, U. C. (2014).
Improved glucose control with weight loss, lower insulin doses, and no increased hypoglycemia with
empagliflozin added to titrated multiple daily injections of insulin in obese inadequately controlled type
2 diabetes. Diabetes care, 37(7), 1815-1823.
Kahn, S. E., Cooper, M. E., & Del Prato, S. (2014). Pathophysiology and treatment of type 2
diabetes: perspectives on the past, present, and future. The Lancet, 383(9922), 1068-1083.
Morris, A. P., Voight, B. F., Teslovich, T. M., Ferreira, T., Segre, A. V., Steinthorsdottir,
V., ... & Prokopenko, I. (2012). Large-scale association analysis provides insights into the
genetic architecture and pathophysiology of type 2 diabetes. Nature genetics, 44(9), 981.
Nolan, C. J., Damm, P., & Prentki, M. (2011). Type 2 diabetes across generations: from
pathophysiology to prevention and management. The Lancet, 378(9786), 169-181.
Ozougwu, J. C., Obimba, K. C., Belonwu, C. D., & Unakalamba, C. B. (2013). The
pathogenesis and pathophysiology of type 1 and type 2 diabetes mellitus. Journal of
Physiology and Pathophysiology, 4(4), 46-57.
Paterson, M. A., Smart, C. E. M., Lopez, P. E., McElduff, P., Attia, J., Morbey, C., & King, B. R.
(2016). Influence of dietary protein on postprandial blood glucose levels in individuals with type 2
diabetes mellitus using intensive insulin therapy. Diabetic Medicine, 33(5), 592-598.
Pecoits‐Filho, R., Bucharles, S., & Barberato, S. H. (2012, January). Diastolic heart failure in
dialysis patients: mechanisms, diagnostic approach, and treatment. In Seminars in
dialysis (Vol. 25, No. 1, pp. 35-41). Oxford, UK: Blackwell Publishing Ltd.
Pradeepa, R. (2013). The rising burden of diabetes and hypertension in southeast asian and
african regions: need for effective strategies for prevention and control in primary health care
settings. International journal of hypertension, 2013.
Rosenstock, J., Jelaska, A., Frappin, G., Salsali, A., Kim, G., Woerle, H. J., & Broedl, U. C. (2014).
Improved glucose control with weight loss, lower insulin doses, and no increased hypoglycemia with
empagliflozin added to titrated multiple daily injections of insulin in obese inadequately controlled type
2 diabetes. Diabetes care, 37(7), 1815-1823.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





