Nursing and Critical Care Case Study 2022
VerifiedAdded on 2022/09/26
|8
|2282
|18
AI Summary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
Running Head: CRITICAL CARE
CRITICAL CARE
Name of the Student
Name of the University
Author Note
CRITICAL CARE
Name of the Student
Name of the University
Author Note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1NURSING CARE
Introduction
Paul has been admitted to the hospital and was provided with 24 hours of ventilation
support. Thus, he needs the oxygenation and the nurse should be able to critically analyse,
interpret and manage the oxygenation levels (Jorgensen, 2013). Health care provider
administering oxygen is accountable for tracking patient reaction and maintaining target
range oxygen saturation concentrations. Critically ill patients present a great deal of challenge
for the entire healthcare sector because they require invasive diagnostic testing, sophisticated
processes and intensive nursing care (Malek & Nematbakhsh, 2015; Watson et al., 2013).
In the early phases of the renal disease, the patients might have disabilities of the
urine volume or the composition that is the presence of the red blood cells or protein in the
blood. Later, the pathophysiology might observe the systemic signs and symptoms of the lost
renal function that can be marked by fluid overload, edema, anemia and electrolyte
abnormalities (Watson et al., 2013). The progress of the function of the kidney might be
progressed depending on the type of the renal disease. This may display a variety of chronic
complications that results from the inadequate functioning of renal (Gaudry et al., 2016).
Introduction
Paul has been admitted to the hospital and was provided with 24 hours of ventilation
support. Thus, he needs the oxygenation and the nurse should be able to critically analyse,
interpret and manage the oxygenation levels (Jorgensen, 2013). Health care provider
administering oxygen is accountable for tracking patient reaction and maintaining target
range oxygen saturation concentrations. Critically ill patients present a great deal of challenge
for the entire healthcare sector because they require invasive diagnostic testing, sophisticated
processes and intensive nursing care (Malek & Nematbakhsh, 2015; Watson et al., 2013).
In the early phases of the renal disease, the patients might have disabilities of the
urine volume or the composition that is the presence of the red blood cells or protein in the
blood. Later, the pathophysiology might observe the systemic signs and symptoms of the lost
renal function that can be marked by fluid overload, edema, anemia and electrolyte
abnormalities (Watson et al., 2013). The progress of the function of the kidney might be
progressed depending on the type of the renal disease. This may display a variety of chronic
complications that results from the inadequate functioning of renal (Gaudry et al., 2016).
2NURSING CARE
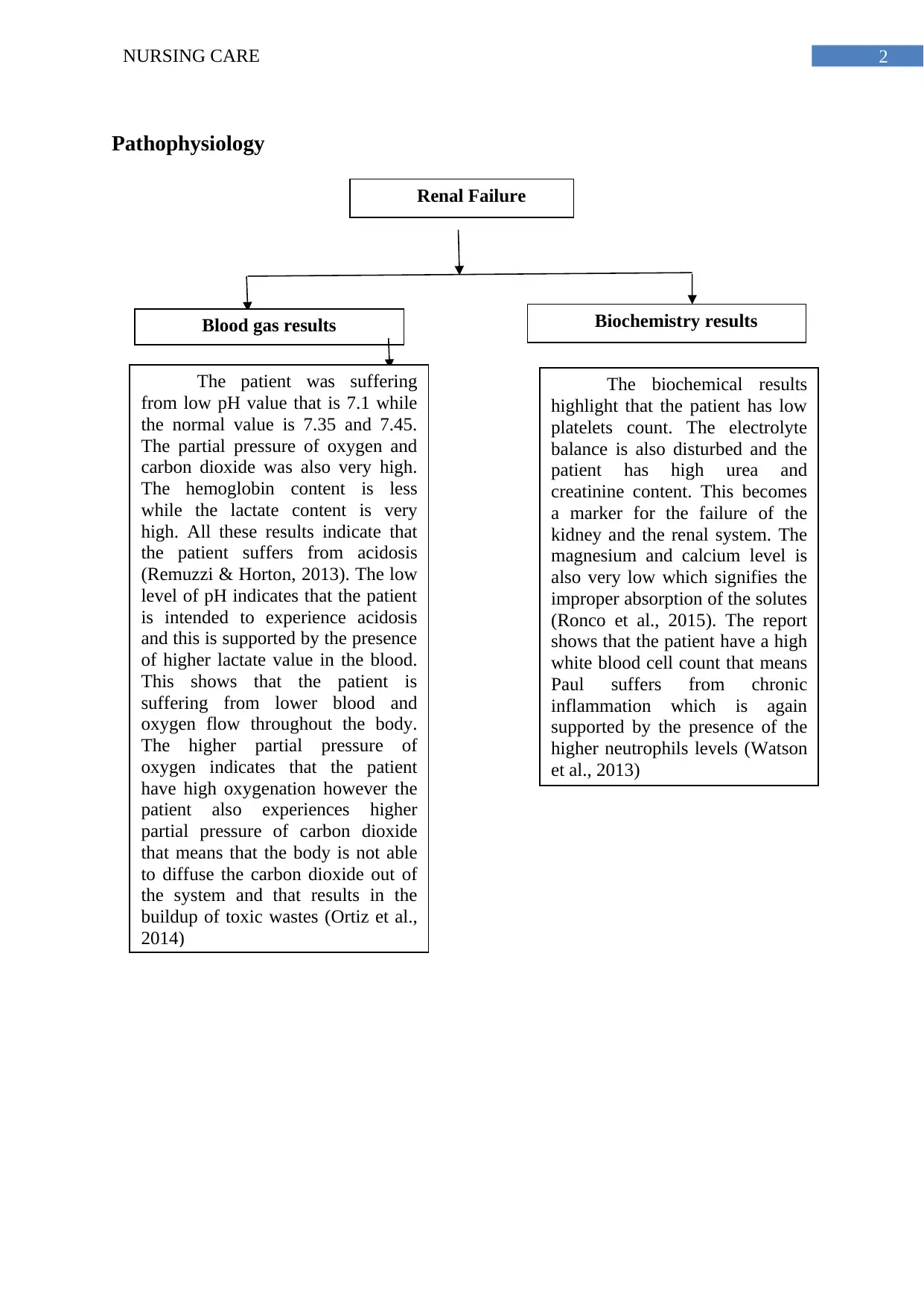
Pathophysiology
Renal Failure
Blood gas results Biochemistry results
The patient was suffering
from low pH value that is 7.1 while
the normal value is 7.35 and 7.45.
The partial pressure of oxygen and
carbon dioxide was also very high.
The hemoglobin content is less
while the lactate content is very
high. All these results indicate that
the patient suffers from acidosis
(Remuzzi & Horton, 2013). The low
level of pH indicates that the patient
is intended to experience acidosis
and this is supported by the presence
of higher lactate value in the blood.
This shows that the patient is
suffering from lower blood and
oxygen flow throughout the body.
The higher partial pressure of
oxygen indicates that the patient
have high oxygenation however the
patient also experiences higher
partial pressure of carbon dioxide
that means that the body is not able
to diffuse the carbon dioxide out of
the system and that results in the
buildup of toxic wastes (Ortiz et al.,
2014)
The biochemical results
highlight that the patient has low
platelets count. The electrolyte
balance is also disturbed and the
patient has high urea and
creatinine content. This becomes
a marker for the failure of the
kidney and the renal system. The
magnesium and calcium level is
also very low which signifies the
improper absorption of the solutes
(Ronco et al., 2015). The report
shows that the patient have a high
white blood cell count that means
Paul suffers from chronic
inflammation which is again
supported by the presence of the
higher neutrophils levels (Watson
et al., 2013)
Pathophysiology
Renal Failure
Blood gas results Biochemistry results
The patient was suffering
from low pH value that is 7.1 while
the normal value is 7.35 and 7.45.
The partial pressure of oxygen and
carbon dioxide was also very high.
The hemoglobin content is less
while the lactate content is very
high. All these results indicate that
the patient suffers from acidosis
(Remuzzi & Horton, 2013). The low
level of pH indicates that the patient
is intended to experience acidosis
and this is supported by the presence
of higher lactate value in the blood.
This shows that the patient is
suffering from lower blood and
oxygen flow throughout the body.
The higher partial pressure of
oxygen indicates that the patient
have high oxygenation however the
patient also experiences higher
partial pressure of carbon dioxide
that means that the body is not able
to diffuse the carbon dioxide out of
the system and that results in the
buildup of toxic wastes (Ortiz et al.,
2014)
The biochemical results
highlight that the patient has low
platelets count. The electrolyte
balance is also disturbed and the
patient has high urea and
creatinine content. This becomes
a marker for the failure of the
kidney and the renal system. The
magnesium and calcium level is
also very low which signifies the
improper absorption of the solutes
(Ronco et al., 2015). The report
shows that the patient have a high
white blood cell count that means
Paul suffers from chronic
inflammation which is again
supported by the presence of the
higher neutrophils levels (Watson
et al., 2013)
3NURSING CARE
Management
The management of Paul who is being admitted to the critical care unit should be
done properly by the nurses as he had become oliguic with a urine output of 5-10 ml/hr as the
normal output of urine for an adult should be 400 ml. Thus, he was diagnosed with acute
renal failure. Along with this the GCS or the Glasgow Coma Score for Paul was also
deteriorating at a fast rate which means that Paul was losing consciousness at a fast rate. For
the management of this situation the clinicians decide to perform Renal Replacement
Therapy. It is required when there is
acute decrease in the rate of glomerular filtration and has developed or is at risk of developin
g clinically significant solvent imbalance or toxicity or volume overload (Gaudry et al.,
2016).
The patient was sedated with Fentayl and Propofol which are needed to suppress the
responses for the perioperative stimuli of tracheal intubation, laryngoscopy, and skin
incision. During the increase in blood pressure at the time of the renal surgery of Paul then
these medicines had to be administered (Iwagami et al., 2015; Ortiz et al., 2014).
Recommendation
It is recommended that the patient with renal failure should opt for Renal replacement
therapy (RRT) that replaces the non-endocrine function of the kidney. The techniques for
the RRT include continuous hemofiltration, intermittent hemodialysis, and peritoneal
dialysis. All these techniques exchange the solute and remove the fluid from the blood,
using the process of filtration and dialysis across the permeable membranes ( Dahlerus et al.,
2016; Schefold et al., 2014).
The patients should be monitored for the amount of urine that is being passed before
and after the surgery as it is a marker for the functioning of the kidney. The other thing that
Management
The management of Paul who is being admitted to the critical care unit should be
done properly by the nurses as he had become oliguic with a urine output of 5-10 ml/hr as the
normal output of urine for an adult should be 400 ml. Thus, he was diagnosed with acute
renal failure. Along with this the GCS or the Glasgow Coma Score for Paul was also
deteriorating at a fast rate which means that Paul was losing consciousness at a fast rate. For
the management of this situation the clinicians decide to perform Renal Replacement
Therapy. It is required when there is
acute decrease in the rate of glomerular filtration and has developed or is at risk of developin
g clinically significant solvent imbalance or toxicity or volume overload (Gaudry et al.,
2016).
The patient was sedated with Fentayl and Propofol which are needed to suppress the
responses for the perioperative stimuli of tracheal intubation, laryngoscopy, and skin
incision. During the increase in blood pressure at the time of the renal surgery of Paul then
these medicines had to be administered (Iwagami et al., 2015; Ortiz et al., 2014).
Recommendation
It is recommended that the patient with renal failure should opt for Renal replacement
therapy (RRT) that replaces the non-endocrine function of the kidney. The techniques for
the RRT include continuous hemofiltration, intermittent hemodialysis, and peritoneal
dialysis. All these techniques exchange the solute and remove the fluid from the blood,
using the process of filtration and dialysis across the permeable membranes ( Dahlerus et al.,
2016; Schefold et al., 2014).
The patients should be monitored for the amount of urine that is being passed before
and after the surgery as it is a marker for the functioning of the kidney. The other thing that
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4NURSING CARE
can be used by the patients to stay healthy and fit includes the reduction of sodium in the
diet and to include fresh fruits and vegetables. The patients should reduce the intake of food
high in cholesterol. The patient should also be involved with physical activity that offers a
number of health benefits that includes increase in the muscle strength, decreasing the blood
pressure, lowering the blood fat levels, improving sleep and to control body weight (Fealy et
al., 2017; Singhal et al., 2014).
Question 3
The peripheral veins can be used in order to get the allowance into the central venous
system. However, this needs the placement of a long catheter through the superficial veins
that might be difficult to identify in case of an emergency. The Renal Replacement Therapy
or RRT via the Right Femoral Vascath is better than the other available CRRT modes
because of the reduction in the cardiopulmonary recirculation. It also influences the adequacy
of the dialysis process (Beard, Roper & Hodges, 2016). It is advantageous to use the femoral
site in patients who are very ill because it is free of devices that are used for monitoring and
access of airway. It also allows free movement of the arms and neck in the patients who are
critically ill (Bos-Touwen et al., 2015; Schneider et al., 2013). This technology is used more
than the other available methods due to the increased monitoring of the invasive and the
aggressive hemodynamic protocols. Thus, the capability to gain the accurate and the rapid
vascular access is a necessary skill in order to maintain the imperative and emergency care
for the physicians who are involved with renal replacement therapy.
can be used by the patients to stay healthy and fit includes the reduction of sodium in the
diet and to include fresh fruits and vegetables. The patients should reduce the intake of food
high in cholesterol. The patient should also be involved with physical activity that offers a
number of health benefits that includes increase in the muscle strength, decreasing the blood
pressure, lowering the blood fat levels, improving sleep and to control body weight (Fealy et
al., 2017; Singhal et al., 2014).
Question 3
The peripheral veins can be used in order to get the allowance into the central venous
system. However, this needs the placement of a long catheter through the superficial veins
that might be difficult to identify in case of an emergency. The Renal Replacement Therapy
or RRT via the Right Femoral Vascath is better than the other available CRRT modes
because of the reduction in the cardiopulmonary recirculation. It also influences the adequacy
of the dialysis process (Beard, Roper & Hodges, 2016). It is advantageous to use the femoral
site in patients who are very ill because it is free of devices that are used for monitoring and
access of airway. It also allows free movement of the arms and neck in the patients who are
critically ill (Bos-Touwen et al., 2015; Schneider et al., 2013). This technology is used more
than the other available methods due to the increased monitoring of the invasive and the
aggressive hemodynamic protocols. Thus, the capability to gain the accurate and the rapid
vascular access is a necessary skill in order to maintain the imperative and emergency care
for the physicians who are involved with renal replacement therapy.
5NURSING CARE
References
Beard, L., Roper, M., & Hodges, M. (2016). Life threatening complication following Vascath
insertion in a patient with immune thrombocytopenic purpura (ITP). Anaesthesia
Cases, 4(1), 50-54.
Bos-Touwen, I., Schuurmans, M., Monninkhof, E. M., Korpershoek, Y., Spruit-Bentvelzen,
L., Ertugrul-van der Graaf, I., ... & Trappenburg, J. (2015). Patient and disease
characteristics associated with activation for self-management in patients with
diabetes, chronic obstructive pulmonary disease, chronic heart failure and chronic
renal disease: a cross-sectional survey study. PloS one, 10(5), e0126400.
Dahlerus, C., Quinn, M., Messersmith, E., Lachance, L., Subramanian, L., Perry, E., ... &
Paulson, L. (2016). Patient perspectives on the choice of dialysis modality: results
from the Empowering Patients on Choices for Renal Replacement Therapy (EPOCH-
RRT) Study. American Journal of Kidney Diseases, 68(6), 901-910.
Fealy, N., Aitken, L., du Toit, E., Lo, S., & Baldwin, I. (2017). Faster blood flow rate does
not improve circuit life in continuous renal replacement therapy: a randomized
controlled trial. Critical care medicine, 45(10), e1018-e1025.
Gaudry, S., Hajage, D., Schortgen, F., Martin-Lefevre, L., Pons, B., Boulet, E., ... & De
Prost, N. (2016). Initiation strategies for renal-replacement therapy in the intensive
care unit. New England Journal of Medicine, 375(2), 122-133.
Iwagami, M., Yasunaga, H., Noiri, E., Horiguchi, H., Fushimi, K., Matsubara, T., ... & Doi,
K. (2015). Choice of renal replacement therapy modality in intensive care units: data
from a Japanese Nationwide Administrative Claim Database. Journal of critical
care, 30(2), 381-385.
References
Beard, L., Roper, M., & Hodges, M. (2016). Life threatening complication following Vascath
insertion in a patient with immune thrombocytopenic purpura (ITP). Anaesthesia
Cases, 4(1), 50-54.
Bos-Touwen, I., Schuurmans, M., Monninkhof, E. M., Korpershoek, Y., Spruit-Bentvelzen,
L., Ertugrul-van der Graaf, I., ... & Trappenburg, J. (2015). Patient and disease
characteristics associated with activation for self-management in patients with
diabetes, chronic obstructive pulmonary disease, chronic heart failure and chronic
renal disease: a cross-sectional survey study. PloS one, 10(5), e0126400.
Dahlerus, C., Quinn, M., Messersmith, E., Lachance, L., Subramanian, L., Perry, E., ... &
Paulson, L. (2016). Patient perspectives on the choice of dialysis modality: results
from the Empowering Patients on Choices for Renal Replacement Therapy (EPOCH-
RRT) Study. American Journal of Kidney Diseases, 68(6), 901-910.
Fealy, N., Aitken, L., du Toit, E., Lo, S., & Baldwin, I. (2017). Faster blood flow rate does
not improve circuit life in continuous renal replacement therapy: a randomized
controlled trial. Critical care medicine, 45(10), e1018-e1025.
Gaudry, S., Hajage, D., Schortgen, F., Martin-Lefevre, L., Pons, B., Boulet, E., ... & De
Prost, N. (2016). Initiation strategies for renal-replacement therapy in the intensive
care unit. New England Journal of Medicine, 375(2), 122-133.
Iwagami, M., Yasunaga, H., Noiri, E., Horiguchi, H., Fushimi, K., Matsubara, T., ... & Doi,
K. (2015). Choice of renal replacement therapy modality in intensive care units: data
from a Japanese Nationwide Administrative Claim Database. Journal of critical
care, 30(2), 381-385.
6NURSING CARE
Jorgensen, A. L. (2013). Contrast-induced nephropathy: pathophysiology and preventive
strategies. Critical care nurse, 33(1), 37-46.
Malek, M., & Nematbakhsh, M. (2015). Renal ischemia/reperfusion injury; from
pathophysiology to treatment. Journal of renal injury prevention, 4(2), 20.
Ortiz, A., Covic, A., Fliser, D., Fouque, D., Goldsmith, D., Kanbay, M., ... & Wiecek, A.
(2014). Epidemiology, contributors to, and clinical trials of mortality risk in chronic
kidney failure. The lancet, 383(9931), 1831-1843.
Remuzzi, G., & Horton, R. (2013). Acute renal failure: an unacceptable death sentence
globally. The Lancet, 382(9910), 2041-2042.
Ronco, C., Ricci, Z., De Backer, D., Kellum, J. A., Taccone, F. S., Joannidis, M., ... &
Bellomo, R. (2015). Renal replacement therapy in acute kidney injury: controversy
and consensus. Critical Care, 19(1), 146.
Schefold, J. C., Von Haehling, S., Pschowski, R., Bender, T. O., Berkmann, C., Briegel, S., ...
& Jörres, A. (2014). The effect of continuous versus intermittent renal replacement
therapy on the outcome of critically ill patients with acute renal failure (CONVINT):
a prospective randomized controlled trial. Critical care, 18(1), R11.
Schneider, A. G., Bellomo, R., Bagshaw, S. M., Glassford, N. J., Lo, S., Jun, M., ... &
Gallagher, M. (2013). Choice of renal replacement therapy modality and dialysis
dependence after acute kidney injury: a systematic review and meta-
analysis. Intensive care medicine, 39(6), 987-997.
Singhal, R., Hux, J. E., Alibhai, S. M., & Oliver, M. J. (2014). Inadequate predialysis care
and mortality after initiation of renal replacement therapy. Kidney
international, 86(2), 399-406.
Jorgensen, A. L. (2013). Contrast-induced nephropathy: pathophysiology and preventive
strategies. Critical care nurse, 33(1), 37-46.
Malek, M., & Nematbakhsh, M. (2015). Renal ischemia/reperfusion injury; from
pathophysiology to treatment. Journal of renal injury prevention, 4(2), 20.
Ortiz, A., Covic, A., Fliser, D., Fouque, D., Goldsmith, D., Kanbay, M., ... & Wiecek, A.
(2014). Epidemiology, contributors to, and clinical trials of mortality risk in chronic
kidney failure. The lancet, 383(9931), 1831-1843.
Remuzzi, G., & Horton, R. (2013). Acute renal failure: an unacceptable death sentence
globally. The Lancet, 382(9910), 2041-2042.
Ronco, C., Ricci, Z., De Backer, D., Kellum, J. A., Taccone, F. S., Joannidis, M., ... &
Bellomo, R. (2015). Renal replacement therapy in acute kidney injury: controversy
and consensus. Critical Care, 19(1), 146.
Schefold, J. C., Von Haehling, S., Pschowski, R., Bender, T. O., Berkmann, C., Briegel, S., ...
& Jörres, A. (2014). The effect of continuous versus intermittent renal replacement
therapy on the outcome of critically ill patients with acute renal failure (CONVINT):
a prospective randomized controlled trial. Critical care, 18(1), R11.
Schneider, A. G., Bellomo, R., Bagshaw, S. M., Glassford, N. J., Lo, S., Jun, M., ... &
Gallagher, M. (2013). Choice of renal replacement therapy modality and dialysis
dependence after acute kidney injury: a systematic review and meta-
analysis. Intensive care medicine, 39(6), 987-997.
Singhal, R., Hux, J. E., Alibhai, S. M., & Oliver, M. J. (2014). Inadequate predialysis care
and mortality after initiation of renal replacement therapy. Kidney
international, 86(2), 399-406.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

7NURSING CARE
Watson, A. R., Hayes, W. N., Vondrak, K., Ariceta, G., Schmitt, C. P., Ekim, M., ... &
Zurowska, A. (2013). Factors influencing choice of renal replacement therapy in
European paediatric nephrology units. Pediatric nephrology, 28(12), 2361-2368.
Watson, A. R., Hayes, W. N., Vondrak, K., Ariceta, G., Schmitt, C. P., Ekim, M., ... &
Zurowska, A. (2013). Factors influencing choice of renal replacement therapy in
European paediatric nephrology units. Pediatric nephrology, 28(12), 2361-2368.
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





