Nursing Priorities-Status Asthmaticus
VerifiedAdded on 2023/01/19
|23
|3456
|77
AI Summary
This essay focuses on the nursing priorities and interventions for a patient with status asthmaticus. It discusses the pathophysiology of status asthmaticus and identifies two priority problems for the patient. The essay also provides independent and collaborative interventions for each priority problem.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

NURSING PRIORITIES-STATUS ASTHMATICUS
Student’s Name
Institutional Affiliation
Course
Date
Instructor
Student’s Name
Institutional Affiliation
Course
Date
Instructor
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Introduction
The nurse plays a fundamental role in the assessment, planning, implementation, and evaluation of care of a patient with status asthmatic.
The essay will focus on the case option 1 of Simon who is 14 years with Status asthmaticus. On ex amination at the emergency department,
Simon has audible wheeze and cannot communicate in full sentences. He has a respiratory rate of 32 breaths per minute, Oxygen Saturation of
88 percent, and a pulse of 132 beats per minute. The paper will identify and discuss two priority problems for Simon and discuss two major
interventions for each priority including independent and collaborative approaches.
Pathophysiology of Status Asthmaticus
Status asthmaticus refers to severe form of asthma whose exacerbation results in hypercarbia, hypoxemia, and respiratory failure since it
does not respond to the standard treatments such as corticosteroids and bronchodilators (Skaletzky & Totapally, 2013). Status asthmaticus is
stimulated by multiple triggers including respiratory infections, severe allergic reactions, severe stress, air pollution, smoking, cold weather,
smoking, and exposure to irritants and chemicals. There are pathophysiological mechanisms which result in changes of the airway through
airway limitation. These mechanisms include bronchoconstriction, hyperresponsiveness, airway edema, and remodeling of the airways (Hinkle
& Cheever, 2013).
In acute asthma attacks, bronchoconstriction causes the narrowing of the airways after exposure to irritants and allergens. Acute
bronchoconstriction following the exposure to allergens is attributed to the release of IgE-independent mediators from the mast cells which
directly result in the contraction of the smooth muscles of the airway (Hinkle & Cheever, 2013). Medications such as Non-steroidal anti-
inflammatory and aspirin contribute to the obstruction of the airway.
The nurse plays a fundamental role in the assessment, planning, implementation, and evaluation of care of a patient with status asthmatic.
The essay will focus on the case option 1 of Simon who is 14 years with Status asthmaticus. On ex amination at the emergency department,
Simon has audible wheeze and cannot communicate in full sentences. He has a respiratory rate of 32 breaths per minute, Oxygen Saturation of
88 percent, and a pulse of 132 beats per minute. The paper will identify and discuss two priority problems for Simon and discuss two major
interventions for each priority including independent and collaborative approaches.
Pathophysiology of Status Asthmaticus
Status asthmaticus refers to severe form of asthma whose exacerbation results in hypercarbia, hypoxemia, and respiratory failure since it
does not respond to the standard treatments such as corticosteroids and bronchodilators (Skaletzky & Totapally, 2013). Status asthmaticus is
stimulated by multiple triggers including respiratory infections, severe allergic reactions, severe stress, air pollution, smoking, cold weather,
smoking, and exposure to irritants and chemicals. There are pathophysiological mechanisms which result in changes of the airway through
airway limitation. These mechanisms include bronchoconstriction, hyperresponsiveness, airway edema, and remodeling of the airways (Hinkle
& Cheever, 2013).
In acute asthma attacks, bronchoconstriction causes the narrowing of the airways after exposure to irritants and allergens. Acute
bronchoconstriction following the exposure to allergens is attributed to the release of IgE-independent mediators from the mast cells which
directly result in the contraction of the smooth muscles of the airway (Hinkle & Cheever, 2013). Medications such as Non-steroidal anti-
inflammatory and aspirin contribute to the obstruction of the airway.
The persistence and progress of the inflammatory process in the airway results in further limit of airflow. The factors which contribute to
this include mucus hypersecretion, inflammation, airway edema, development of mucus plugs which are inspissated and airway hypertrophy and
hyperplasia. Airway hyperresponsiveness is an exaggerated response to the bronchoconstrictors. Some of the mechanisms that influence the
hyperresponsiveness of the airway include inflammation, and structural changes (Chang, 2012).
Airway remodeling results in the development and severity of asthmatic attacks in a patient. The process of remodeling involves the
activation of multiple structural cells which consequently result in permanent airway changes which result in increased obstruction of the airway
and responsiveness. This makes the patient to be less responsive to the prescribed medical therapy (Lewis, Dirksen, Heitkemper, Bucher, &
Camera, 2015). The structural changes associated with the remodeling of the airway include subepithelial fibrosis, thickening of sub-basement
membrane, proliferation and vasodilation of vessels, and hypersecretion by the mucus glands
The inflammatory process plays a central role in the underlying pathophysiology of severe asthmatic attacks. The inflammation of the
airway involves the interaction of multiple mediators and cell types with the airway thus resulting in characteristic pathophysiological
manifestations of the condition such as airway limitation and bronchial inflammation which leads to recurrent episodes of wheeze, cough, and
dyspnea (Lewis et al., 2015).
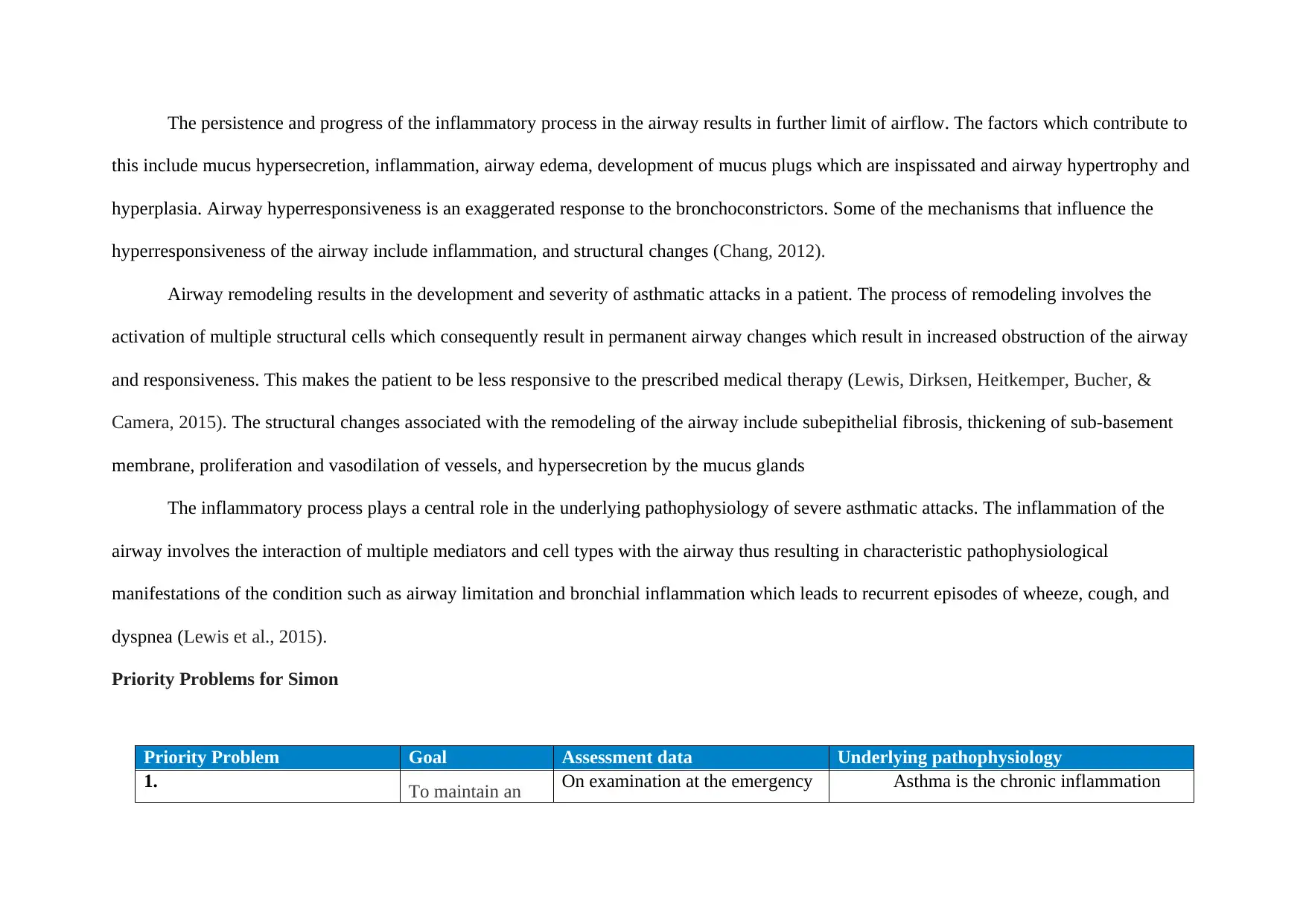
Priority Problems for Simon
Priority Problem Goal Assessment data Underlying pathophysiology
1. To maintain an On examination at the emergency Asthma is the chronic inflammation
this include mucus hypersecretion, inflammation, airway edema, development of mucus plugs which are inspissated and airway hypertrophy and
hyperplasia. Airway hyperresponsiveness is an exaggerated response to the bronchoconstrictors. Some of the mechanisms that influence the
hyperresponsiveness of the airway include inflammation, and structural changes (Chang, 2012).
Airway remodeling results in the development and severity of asthmatic attacks in a patient. The process of remodeling involves the
activation of multiple structural cells which consequently result in permanent airway changes which result in increased obstruction of the airway
and responsiveness. This makes the patient to be less responsive to the prescribed medical therapy (Lewis, Dirksen, Heitkemper, Bucher, &
Camera, 2015). The structural changes associated with the remodeling of the airway include subepithelial fibrosis, thickening of sub-basement
membrane, proliferation and vasodilation of vessels, and hypersecretion by the mucus glands
The inflammatory process plays a central role in the underlying pathophysiology of severe asthmatic attacks. The inflammation of the
airway involves the interaction of multiple mediators and cell types with the airway thus resulting in characteristic pathophysiological
manifestations of the condition such as airway limitation and bronchial inflammation which leads to recurrent episodes of wheeze, cough, and
dyspnea (Lewis et al., 2015).
Priority Problems for Simon
Priority Problem Goal Assessment data Underlying pathophysiology
1. To maintain an On examination at the emergency Asthma is the chronic inflammation
Ineffective Breathing pattern effective
breathing pattern
for the patient
which will be
evidenced normal
depth and rate of
respiration,
relaxed breathing,
and and lack of
dyspnea.
department, Simon was
tachypneic with a respiratory rate
of 32 breaths taken with one
minute and cyanotic with an
oxygen saturation of 88 percent.
Anxiety and distress were other
signs of ineffective pattern of
breathing. The assessment data is
objective.
disease of the lungs which result in mucus
overproduction, hyperresponsiveness, and
mucosal edema which results in obstruction of
the airflow. The common predisposing factors
for severe asthmatic attacks include allergens,
cold weather, air pollutants, strong odors,
physical exertion, and medications (Shah &
Saltoun, 2012). From the case study, Simon
was engaged in soccer play which required a
lot of physical activity and extortion and it
resulted in his wheezing. In ineffective
Breathing Pattern, the expiration and
inspiration provide inadequate ventilation.
Alteration of the breathing pattern is attributed
to airway obstruction as a result of airway
inflammation, mucosal edema, and excessive
breathing pattern
for the patient
which will be
evidenced normal
depth and rate of
respiration,
relaxed breathing,
and and lack of
dyspnea.
department, Simon was
tachypneic with a respiratory rate
of 32 breaths taken with one
minute and cyanotic with an
oxygen saturation of 88 percent.
Anxiety and distress were other
signs of ineffective pattern of
breathing. The assessment data is
objective.
disease of the lungs which result in mucus
overproduction, hyperresponsiveness, and
mucosal edema which results in obstruction of
the airflow. The common predisposing factors
for severe asthmatic attacks include allergens,
cold weather, air pollutants, strong odors,
physical exertion, and medications (Shah &
Saltoun, 2012). From the case study, Simon
was engaged in soccer play which required a
lot of physical activity and extortion and it
resulted in his wheezing. In ineffective
Breathing Pattern, the expiration and
inspiration provide inadequate ventilation.
Alteration of the breathing pattern is attributed
to airway obstruction as a result of airway
inflammation, mucosal edema, and excessive
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
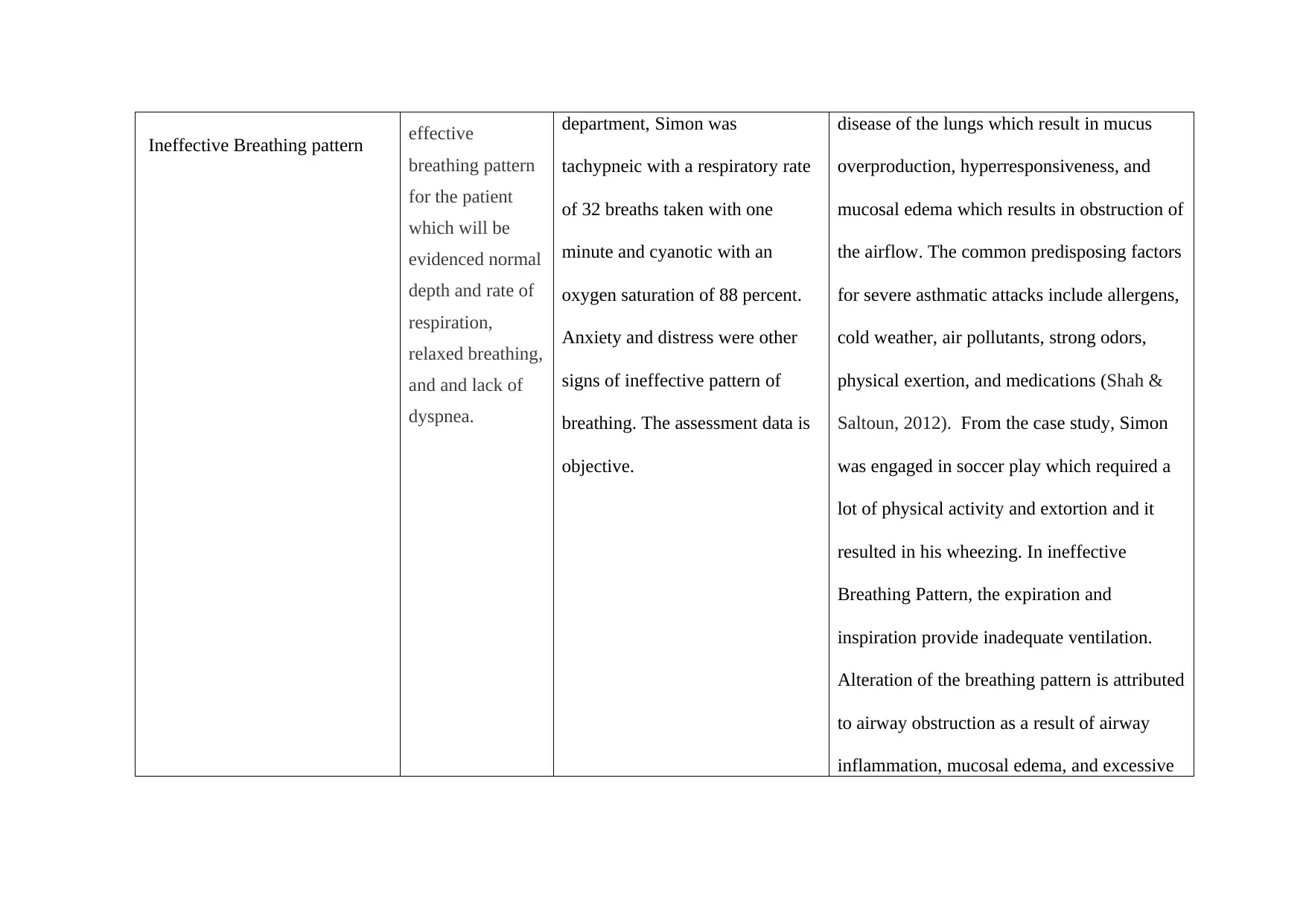
production of secretions which results in
limited flow of air in the respiratory system
(Ackley et al., 2019).
Some of the indicators of an
ineffective breathing pattern include cyanosis,
cough, dyspnea, tachypnea, prolonged
expiration, changes in respiratory depth, and
loss of consciousness. (Doenges, Moorhouse,
& Murr, 2014).
2. Ineffective Airway Clearance
To ensure that the
patient maintains
open and clear
airways
evidenced by
With regard to the case study, the
patient has high breathing rate of
32 breaths per minute, a little
cyanosis, and high breathing
workload. As a compensatory
mechanism of the heart, the
Ineffective airway clearance is related to
multiple factors such as airway spasm,
tenacious and copious tracheobronchial
secretion, impaired functioning of the
respiratory muscles, fatigue, decreased
energy, and tracheobronchial obstruction.
limited flow of air in the respiratory system
(Ackley et al., 2019).
Some of the indicators of an
ineffective breathing pattern include cyanosis,
cough, dyspnea, tachypnea, prolonged
expiration, changes in respiratory depth, and
loss of consciousness. (Doenges, Moorhouse,
& Murr, 2014).
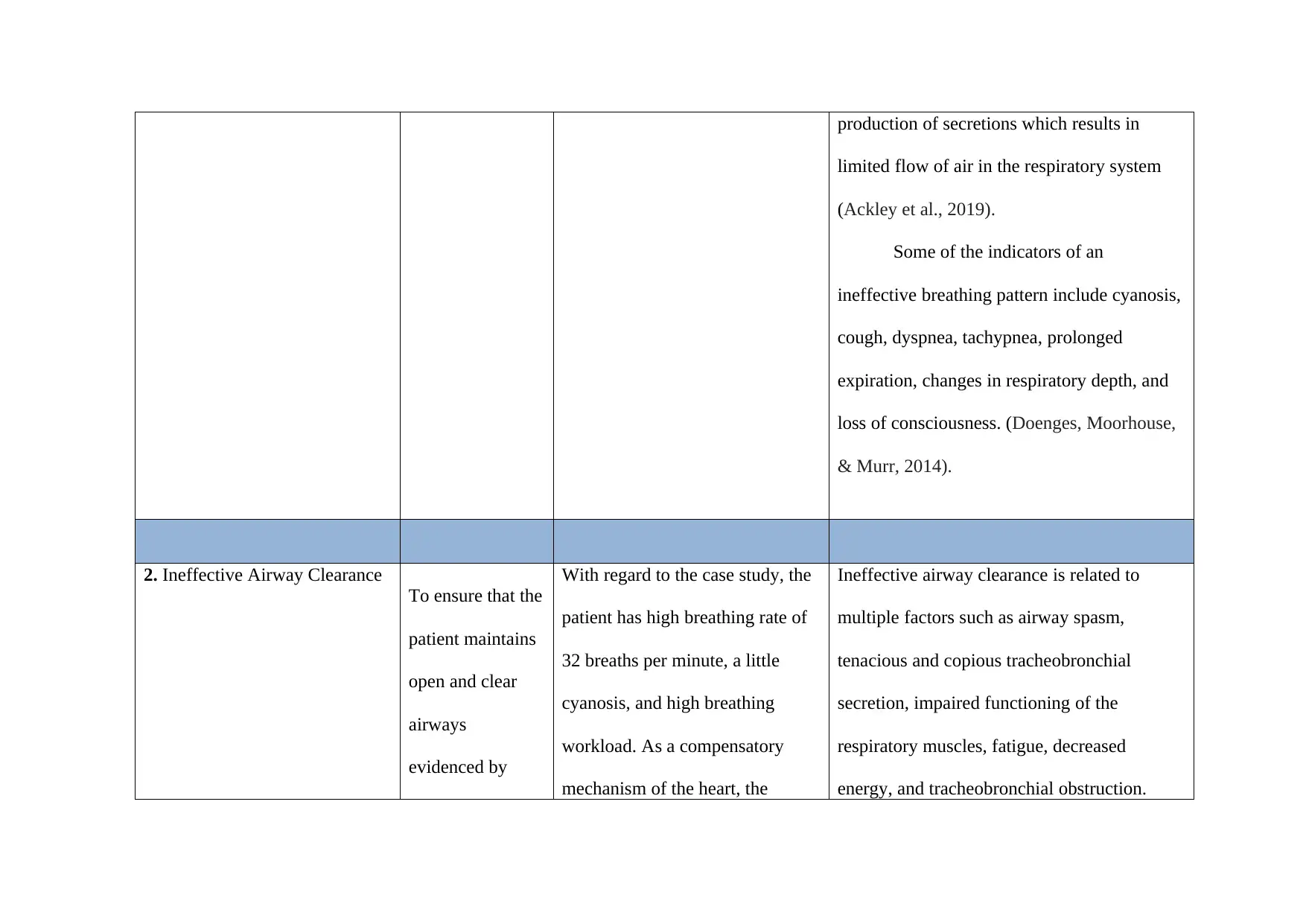
2. Ineffective Airway Clearance
To ensure that the
patient maintains
open and clear
airways
evidenced by
With regard to the case study, the
patient has high breathing rate of
32 breaths per minute, a little
cyanosis, and high breathing
workload. As a compensatory
mechanism of the heart, the
Ineffective airway clearance is related to
multiple factors such as airway spasm,
tenacious and copious tracheobronchial
secretion, impaired functioning of the
respiratory muscles, fatigue, decreased
energy, and tracheobronchial obstruction.
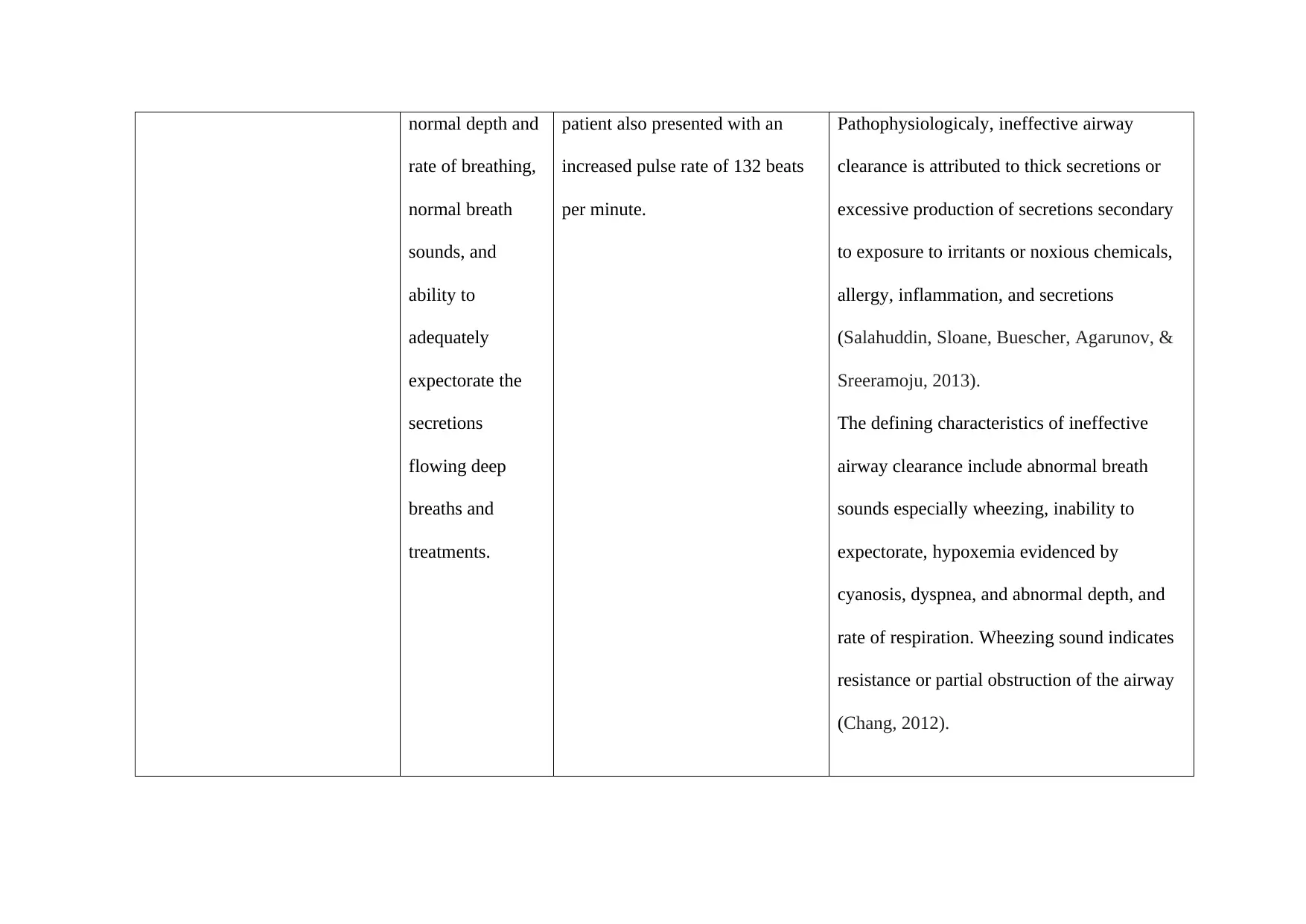
normal depth and
rate of breathing,
normal breath
sounds, and
ability to
adequately
expectorate the
secretions
flowing deep
breaths and
treatments.
patient also presented with an
increased pulse rate of 132 beats
per minute.
Pathophysiologicaly, ineffective airway
clearance is attributed to thick secretions or
excessive production of secretions secondary
to exposure to irritants or noxious chemicals,
allergy, inflammation, and secretions
(Salahuddin, Sloane, Buescher, Agarunov, &
Sreeramoju, 2013).
The defining characteristics of ineffective
airway clearance include abnormal breath
sounds especially wheezing, inability to
expectorate, hypoxemia evidenced by
cyanosis, dyspnea, and abnormal depth, and
rate of respiration. Wheezing sound indicates
resistance or partial obstruction of the airway
(Chang, 2012).
rate of breathing,
normal breath
sounds, and
ability to
adequately
expectorate the
secretions
flowing deep
breaths and
treatments.
patient also presented with an
increased pulse rate of 132 beats
per minute.
Pathophysiologicaly, ineffective airway
clearance is attributed to thick secretions or
excessive production of secretions secondary
to exposure to irritants or noxious chemicals,
allergy, inflammation, and secretions
(Salahuddin, Sloane, Buescher, Agarunov, &
Sreeramoju, 2013).
The defining characteristics of ineffective
airway clearance include abnormal breath
sounds especially wheezing, inability to
expectorate, hypoxemia evidenced by
cyanosis, dyspnea, and abnormal depth, and
rate of respiration. Wheezing sound indicates
resistance or partial obstruction of the airway
(Chang, 2012).
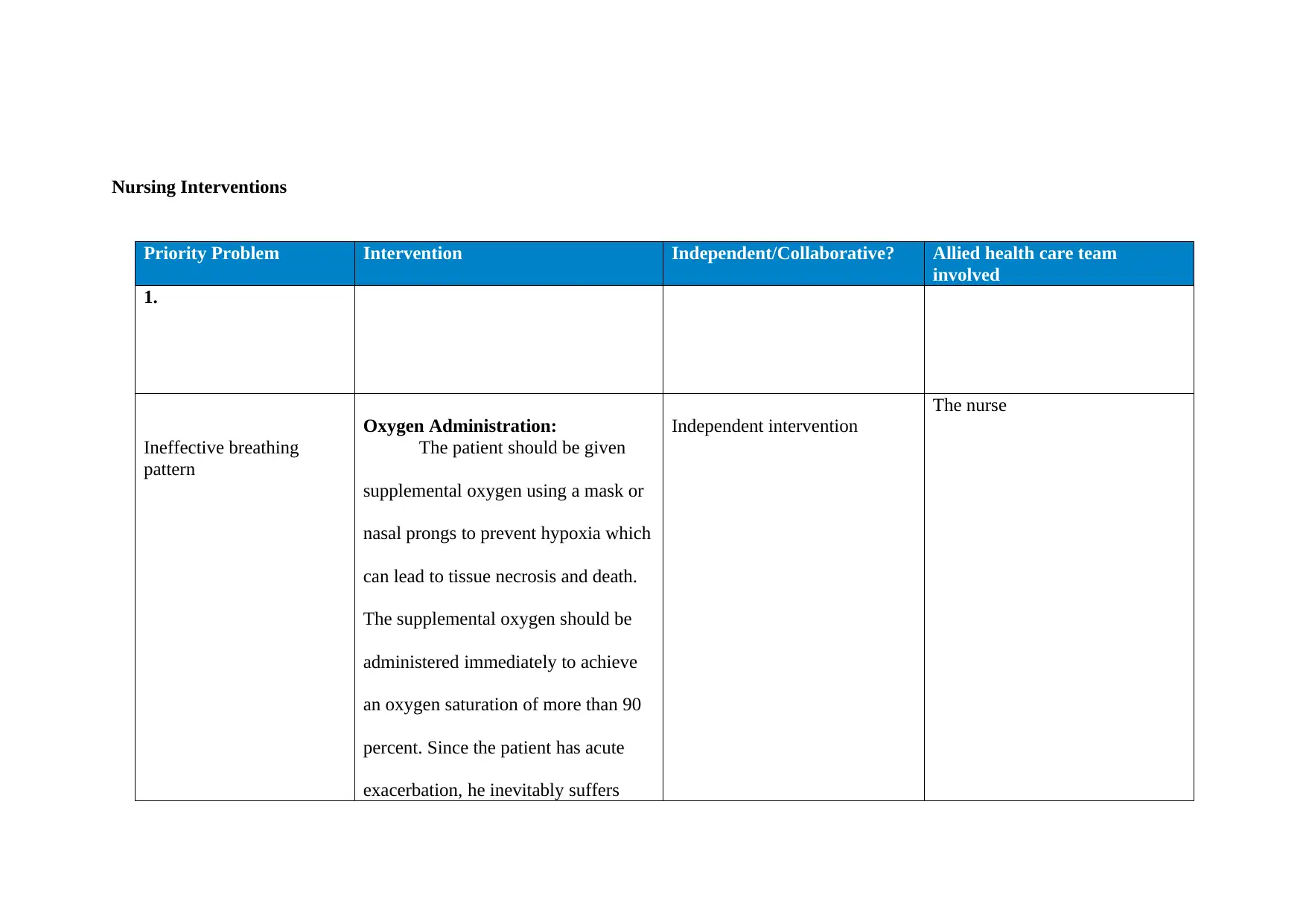
Nursing Interventions
Priority Problem Intervention Independent/Collaborative? Allied health care team
involved
1.
Ineffective breathing
pattern
Oxygen Administration:
The patient should be given
supplemental oxygen using a mask or
nasal prongs to prevent hypoxia which
can lead to tissue necrosis and death.
The supplemental oxygen should be
administered immediately to achieve
an oxygen saturation of more than 90
percent. Since the patient has acute
exacerbation, he inevitably suffers
Independent intervention
The nurse
Priority Problem Intervention Independent/Collaborative? Allied health care team
involved
1.
Ineffective breathing
pattern
Oxygen Administration:
The patient should be given
supplemental oxygen using a mask or
nasal prongs to prevent hypoxia which
can lead to tissue necrosis and death.
The supplemental oxygen should be
administered immediately to achieve
an oxygen saturation of more than 90
percent. Since the patient has acute
exacerbation, he inevitably suffers
Independent intervention
The nurse
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
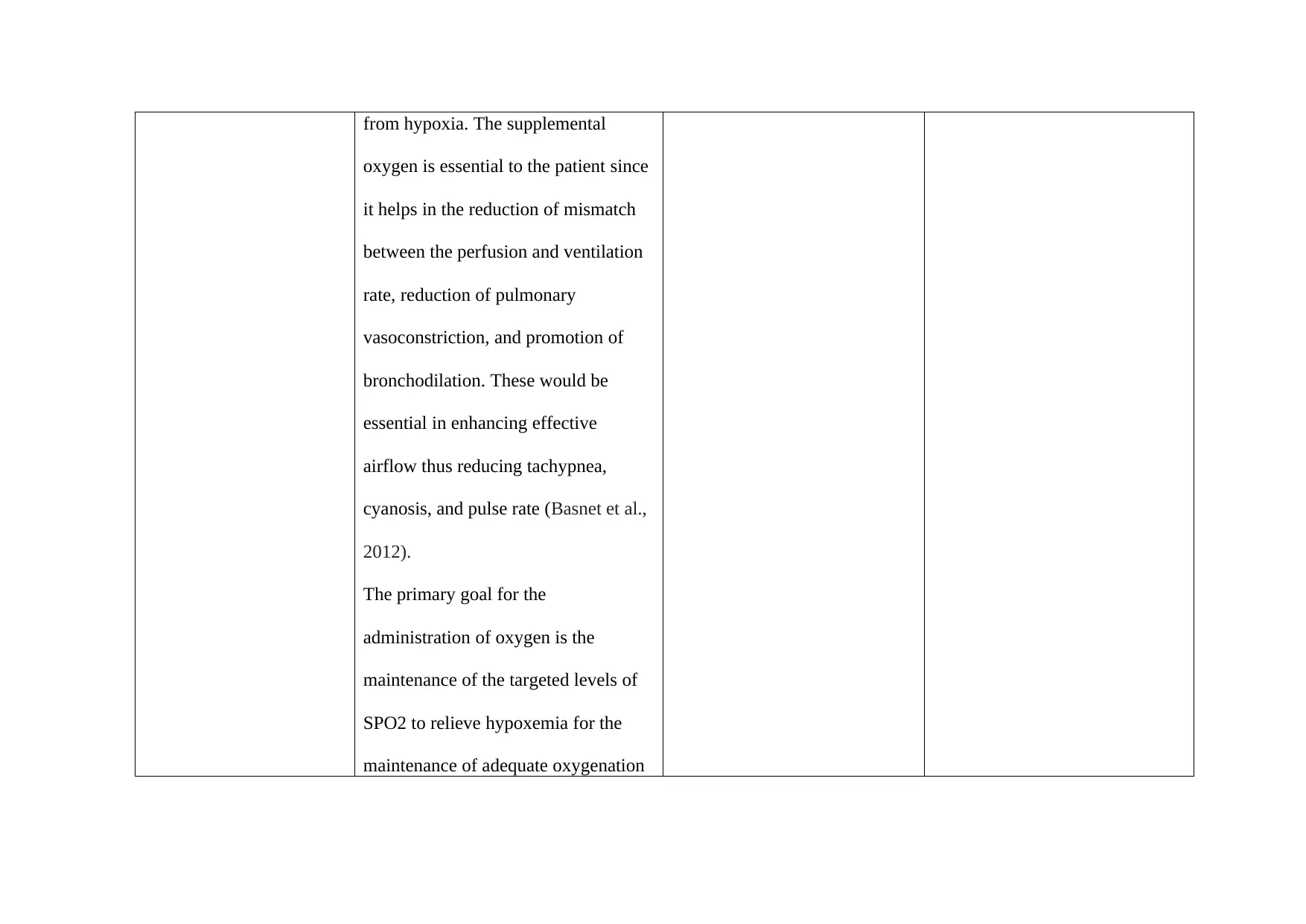
from hypoxia. The supplemental
oxygen is essential to the patient since
it helps in the reduction of mismatch
between the perfusion and ventilation
rate, reduction of pulmonary
vasoconstriction, and promotion of
bronchodilation. These would be
essential in enhancing effective
airflow thus reducing tachypnea,
cyanosis, and pulse rate (Basnet et al.,
2012).
The primary goal for the
administration of oxygen is the
maintenance of the targeted levels of
SPO2 to relieve hypoxemia for the
maintenance of adequate oxygenation
oxygen is essential to the patient since
it helps in the reduction of mismatch
between the perfusion and ventilation
rate, reduction of pulmonary
vasoconstriction, and promotion of
bronchodilation. These would be
essential in enhancing effective
airflow thus reducing tachypnea,
cyanosis, and pulse rate (Basnet et al.,
2012).
The primary goal for the
administration of oxygen is the
maintenance of the targeted levels of
SPO2 to relieve hypoxemia for the
maintenance of adequate oxygenation
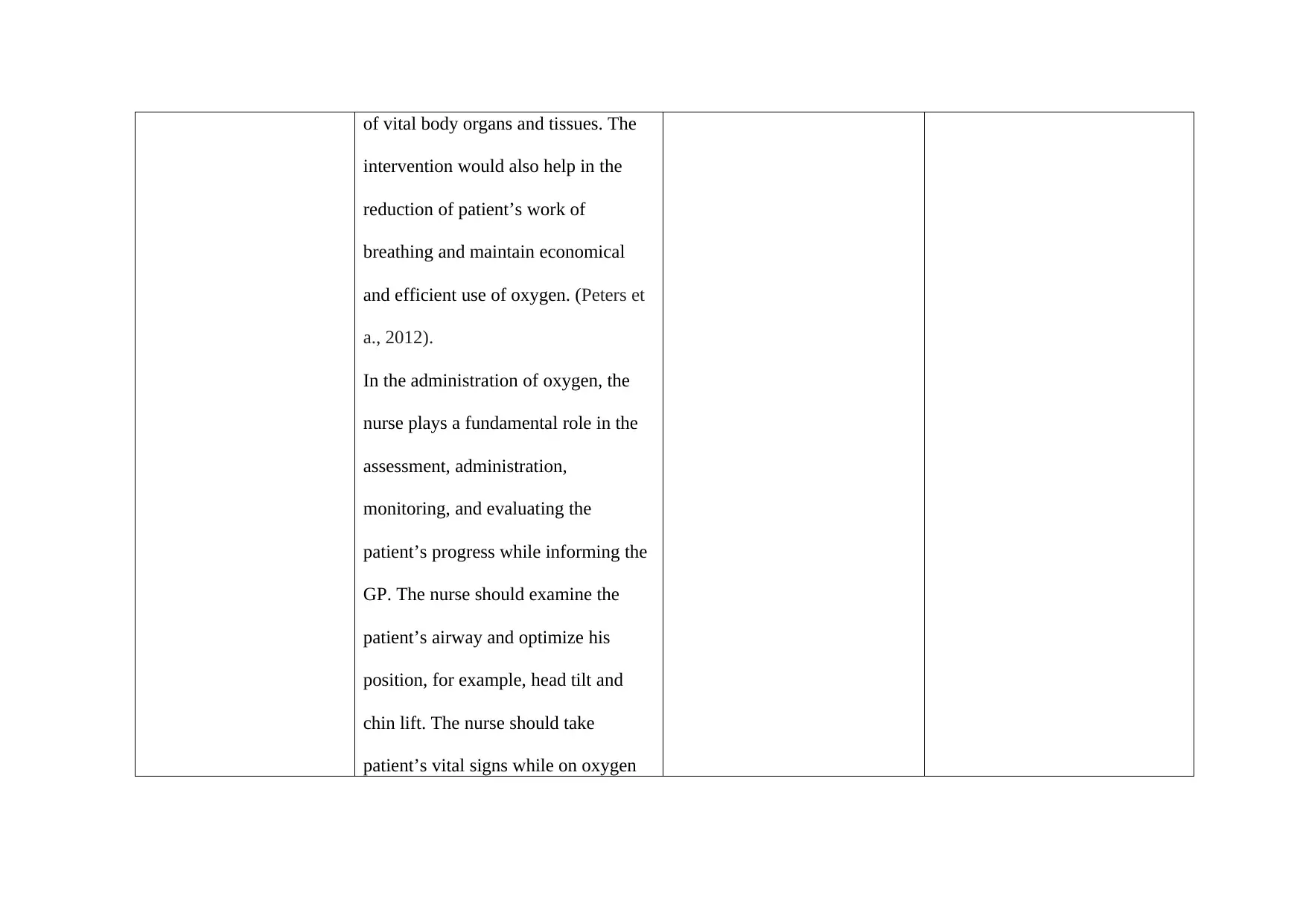
of vital body organs and tissues. The
intervention would also help in the
reduction of patient’s work of
breathing and maintain economical
and efficient use of oxygen. (Peters et
a., 2012).
In the administration of oxygen, the
nurse plays a fundamental role in the
assessment, administration,
monitoring, and evaluating the
patient’s progress while informing the
GP. The nurse should examine the
patient’s airway and optimize his
position, for example, head tilt and
chin lift. The nurse should take
patient’s vital signs while on oxygen
intervention would also help in the
reduction of patient’s work of
breathing and maintain economical
and efficient use of oxygen. (Peters et
a., 2012).
In the administration of oxygen, the
nurse plays a fundamental role in the
assessment, administration,
monitoring, and evaluating the
patient’s progress while informing the
GP. The nurse should examine the
patient’s airway and optimize his
position, for example, head tilt and
chin lift. The nurse should take
patient’s vital signs while on oxygen
to check for the progress by reduction
of the respiration rate and respiratory
rates which are common in severe
asthmatic attacks (Lewis et al., 2015).
Controlled Breathing Exercises
The breathing exercise would
be essential to the patient to aid in the
reduction of shortness of breath,
anxiety, distress, and encourage
adequate supply of oxygen in the
respiratory system to reduce the risk of
reoccurrence of the severe asthmatic
attack. The nurse should guide the
patient in taking short and shallow
breaths into his chest to reduce anxiety
and zap his energy. The nurse should
of the respiration rate and respiratory
rates which are common in severe
asthmatic attacks (Lewis et al., 2015).
Controlled Breathing Exercises
The breathing exercise would
be essential to the patient to aid in the
reduction of shortness of breath,
anxiety, distress, and encourage
adequate supply of oxygen in the
respiratory system to reduce the risk of
reoccurrence of the severe asthmatic
attack. The nurse should guide the
patient in taking short and shallow
breaths into his chest to reduce anxiety
and zap his energy. The nurse should
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
instruct the patient to get comfortable
whereby he can lie in the bed or the
floor with a pillow under his knees and
head. The patient can also sit in a chair
with his shoulders, neck, and head
supported on the back of the chair. The
nurse should instruct the patient to
breath in via his nose and let his belly
fill with air and breath out. Since in
asthmatic attacks, the air is trapped in
the lungs, the breathing exercises can
help the patient get more air out thus
making the breathing easier (Lewis et
al., 2015).
The nurse can also guide the
patient to do the diaphragmatic
whereby he can lie in the bed or the
floor with a pillow under his knees and
head. The patient can also sit in a chair
with his shoulders, neck, and head
supported on the back of the chair. The
nurse should instruct the patient to
breath in via his nose and let his belly
fill with air and breath out. Since in
asthmatic attacks, the air is trapped in
the lungs, the breathing exercises can
help the patient get more air out thus
making the breathing easier (Lewis et
al., 2015).
The nurse can also guide the
patient to do the diaphragmatic
breathing technique which maximizes
the distribution of air in the lungs.
Another technique is the Buteyko
breathing which would help James to
consciously reduce the breathing
volume or breathing rate. He can do
this by sitting upright and relaxing his
belly muscles and the chest while
breathing. The patient should then
breath shallow and slowly via the nose
while his mouth is closed. He should
then breath out slowly until no air is
left in the lungs. Additionally, James
can be instructed to hold his breath for
a certain period based on his ability
and return to his gentle breathing
the distribution of air in the lungs.
Another technique is the Buteyko
breathing which would help James to
consciously reduce the breathing
volume or breathing rate. He can do
this by sitting upright and relaxing his
belly muscles and the chest while
breathing. The patient should then
breath shallow and slowly via the nose
while his mouth is closed. He should
then breath out slowly until no air is
left in the lungs. Additionally, James
can be instructed to hold his breath for
a certain period based on his ability
and return to his gentle breathing
(Pinfield, Gaskin, Bentley, & Rouse,
2015).
2.
Ineffective airway
clearance
Patient positioning and education
The nurse should enlighten the
patient on the most effective ways of
breathing and coughing, that is, deep
breathing, holding breath for two
seconds, and coughing for more than
two times in succession. Coughing is
one of the most convenient ways of
Independent Intervention The nurse
2015).
2.
Ineffective airway
clearance
Patient positioning and education
The nurse should enlighten the
patient on the most effective ways of
breathing and coughing, that is, deep
breathing, holding breath for two
seconds, and coughing for more than
two times in succession. Coughing is
one of the most convenient ways of
Independent Intervention The nurse
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
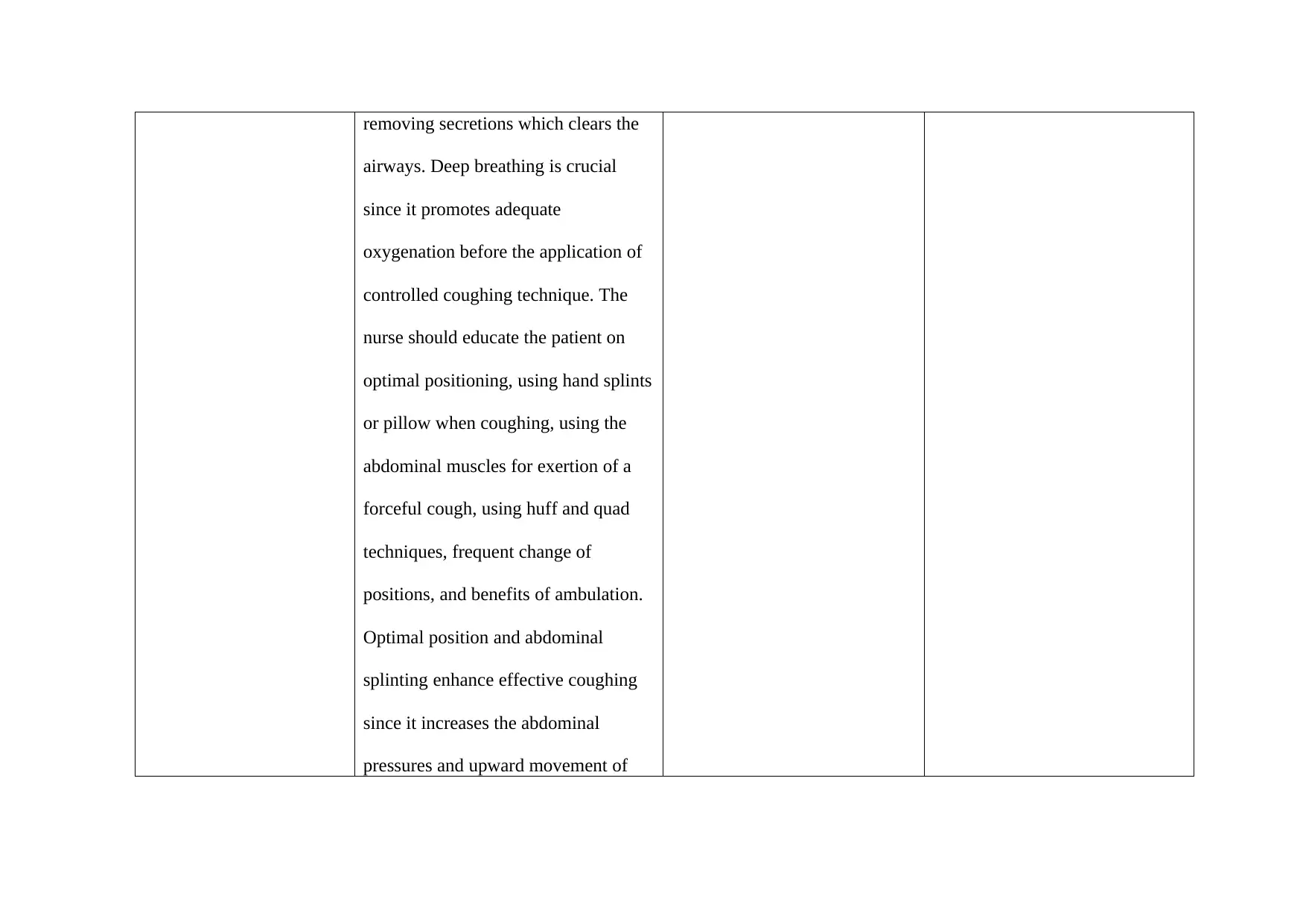
removing secretions which clears the
airways. Deep breathing is crucial
since it promotes adequate
oxygenation before the application of
controlled coughing technique. The
nurse should educate the patient on
optimal positioning, using hand splints
or pillow when coughing, using the
abdominal muscles for exertion of a
forceful cough, using huff and quad
techniques, frequent change of
positions, and benefits of ambulation.
Optimal position and abdominal
splinting enhance effective coughing
since it increases the abdominal
pressures and upward movement of
airways. Deep breathing is crucial
since it promotes adequate
oxygenation before the application of
controlled coughing technique. The
nurse should educate the patient on
optimal positioning, using hand splints
or pillow when coughing, using the
abdominal muscles for exertion of a
forceful cough, using huff and quad
techniques, frequent change of
positions, and benefits of ambulation.
Optimal position and abdominal
splinting enhance effective coughing
since it increases the abdominal
pressures and upward movement of
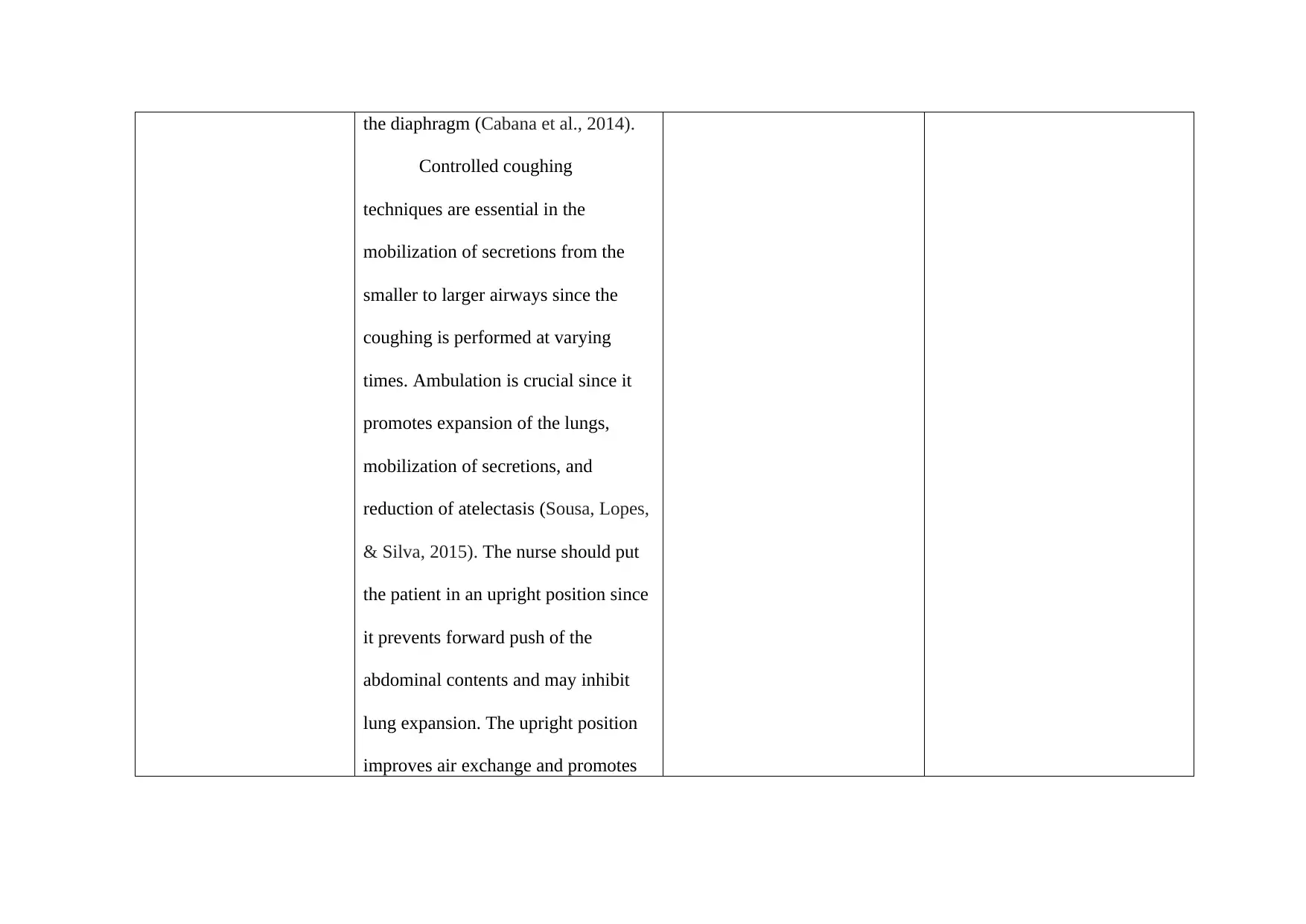
the diaphragm (Cabana et al., 2014).
Controlled coughing
techniques are essential in the
mobilization of secretions from the
smaller to larger airways since the
coughing is performed at varying
times. Ambulation is crucial since it
promotes expansion of the lungs,
mobilization of secretions, and
reduction of atelectasis (Sousa, Lopes,
& Silva, 2015). The nurse should put
the patient in an upright position since
it prevents forward push of the
abdominal contents and may inhibit
lung expansion. The upright position
improves air exchange and promotes
Controlled coughing
techniques are essential in the
mobilization of secretions from the
smaller to larger airways since the
coughing is performed at varying
times. Ambulation is crucial since it
promotes expansion of the lungs,
mobilization of secretions, and
reduction of atelectasis (Sousa, Lopes,
& Silva, 2015). The nurse should put
the patient in an upright position since
it prevents forward push of the
abdominal contents and may inhibit
lung expansion. The upright position
improves air exchange and promotes
lung expansion which increases the
lung volume for adequate gaseous
exchange. Lastly, the nurse should
enlighten the patient on the risk factors
and triggers of asthmatic attacks
especially the physical activities he
engages in while playing soccer. The
patient should engage in less strenuous
physical activities which does not
require more energy (Pinfield et al.,
2015).
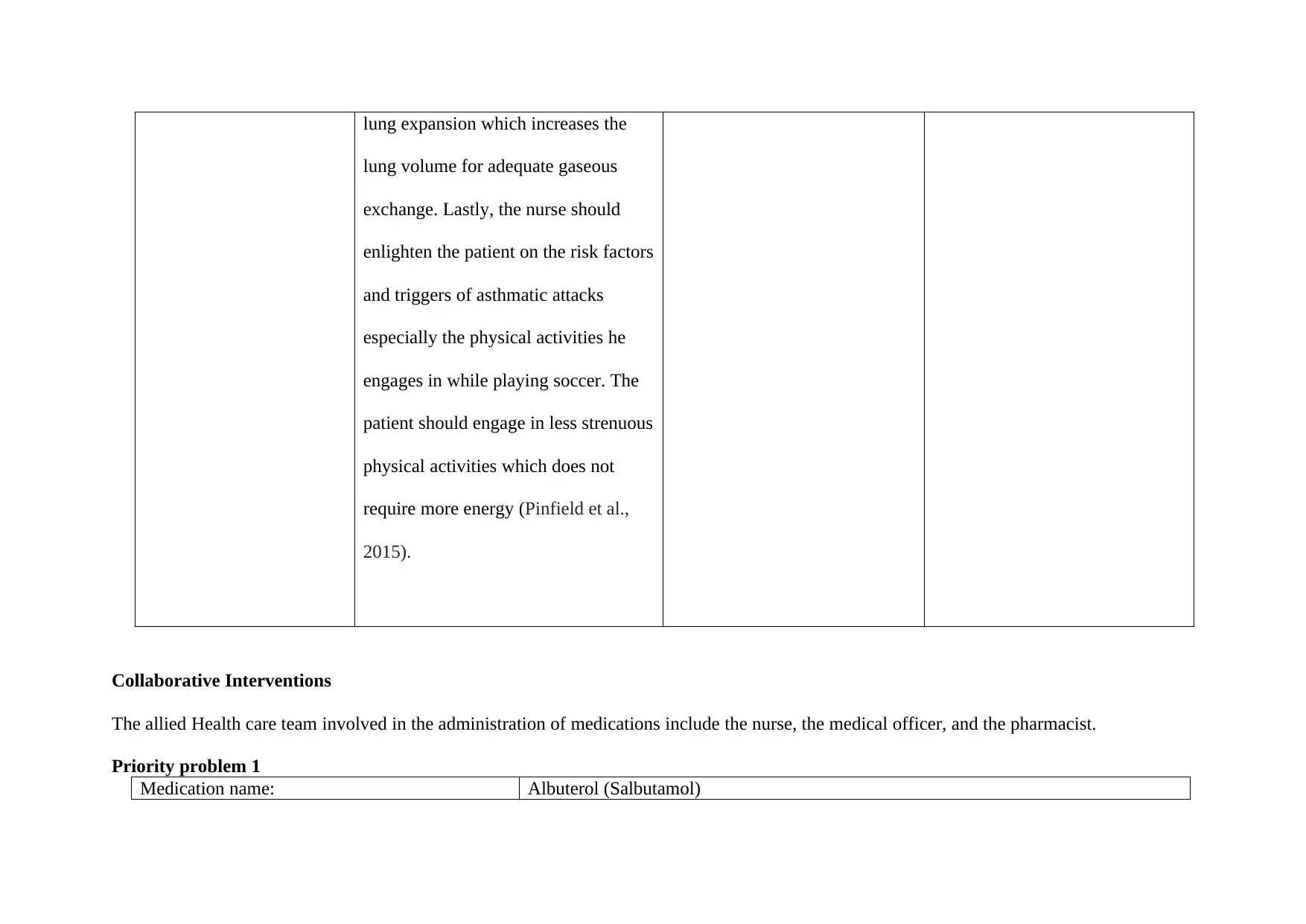
Collaborative Interventions
The allied Health care team involved in the administration of medications include the nurse, the medical officer, and the pharmacist.
Priority problem 1
Medication name: Albuterol (Salbutamol)
lung volume for adequate gaseous
exchange. Lastly, the nurse should
enlighten the patient on the risk factors
and triggers of asthmatic attacks
especially the physical activities he
engages in while playing soccer. The
patient should engage in less strenuous
physical activities which does not
require more energy (Pinfield et al.,
2015).
Collaborative Interventions
The allied Health care team involved in the administration of medications include the nurse, the medical officer, and the pharmacist.
Priority problem 1
Medication name: Albuterol (Salbutamol)
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Medication type: Beta- Agonist, Short-acting bronchodilator
Indications for medication: Symptomatic prevention and relief of bronchospasm secondary to reversible
obstructive airway disease, bronchial ssthma, Chronic Obstructive Pulmonary Disease
(COPD), and various chronic bronchopulmonary problems (Katzung, 2017).
Actions of medication: Promotes relaxation of the smooth muscles of the airways thus promoting
bronchodilation.
Usual dose and route: Inhaler PRN
Any special precautions needed: Enquiring about hypersensitivity reactions
Contraindications: Diabetes, hypertension, seizures, overactive thyroid gland, hypokalemia (Katzung,
2017).
Education required specific to drug including
common side effects:
Mode and time of use, the expected side effects such as headache, dizziness, increased
pulse rate, anxiety, and shakiness. The patient should also be enlightened on the
importance of the drug in relation to his health condition (Smeulers, Onderwater,
Zwieten, & Vermeulen, 2014).
Nursing responsibilities with administering
medication
Ensuring the right dose, route, time, patient, and the response.
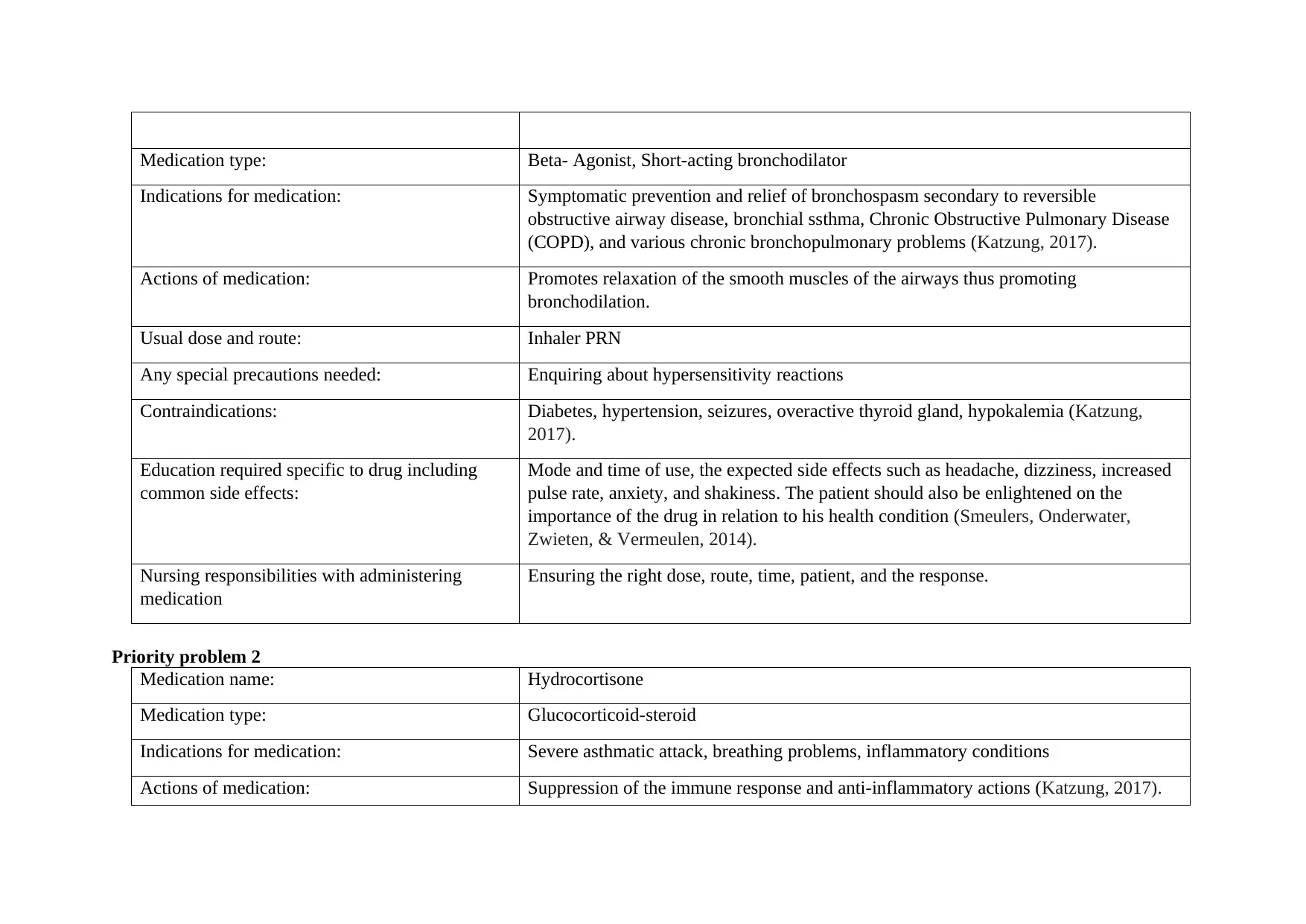
Priority problem 2
Medication name: Hydrocortisone
Medication type: Glucocorticoid-steroid
Indications for medication: Severe asthmatic attack, breathing problems, inflammatory conditions
Actions of medication: Suppression of the immune response and anti-inflammatory actions (Katzung, 2017).
Indications for medication: Symptomatic prevention and relief of bronchospasm secondary to reversible
obstructive airway disease, bronchial ssthma, Chronic Obstructive Pulmonary Disease
(COPD), and various chronic bronchopulmonary problems (Katzung, 2017).
Actions of medication: Promotes relaxation of the smooth muscles of the airways thus promoting
bronchodilation.
Usual dose and route: Inhaler PRN
Any special precautions needed: Enquiring about hypersensitivity reactions
Contraindications: Diabetes, hypertension, seizures, overactive thyroid gland, hypokalemia (Katzung,
2017).
Education required specific to drug including
common side effects:
Mode and time of use, the expected side effects such as headache, dizziness, increased
pulse rate, anxiety, and shakiness. The patient should also be enlightened on the
importance of the drug in relation to his health condition (Smeulers, Onderwater,
Zwieten, & Vermeulen, 2014).
Nursing responsibilities with administering
medication
Ensuring the right dose, route, time, patient, and the response.
Priority problem 2
Medication name: Hydrocortisone
Medication type: Glucocorticoid-steroid
Indications for medication: Severe asthmatic attack, breathing problems, inflammatory conditions
Actions of medication: Suppression of the immune response and anti-inflammatory actions (Katzung, 2017).
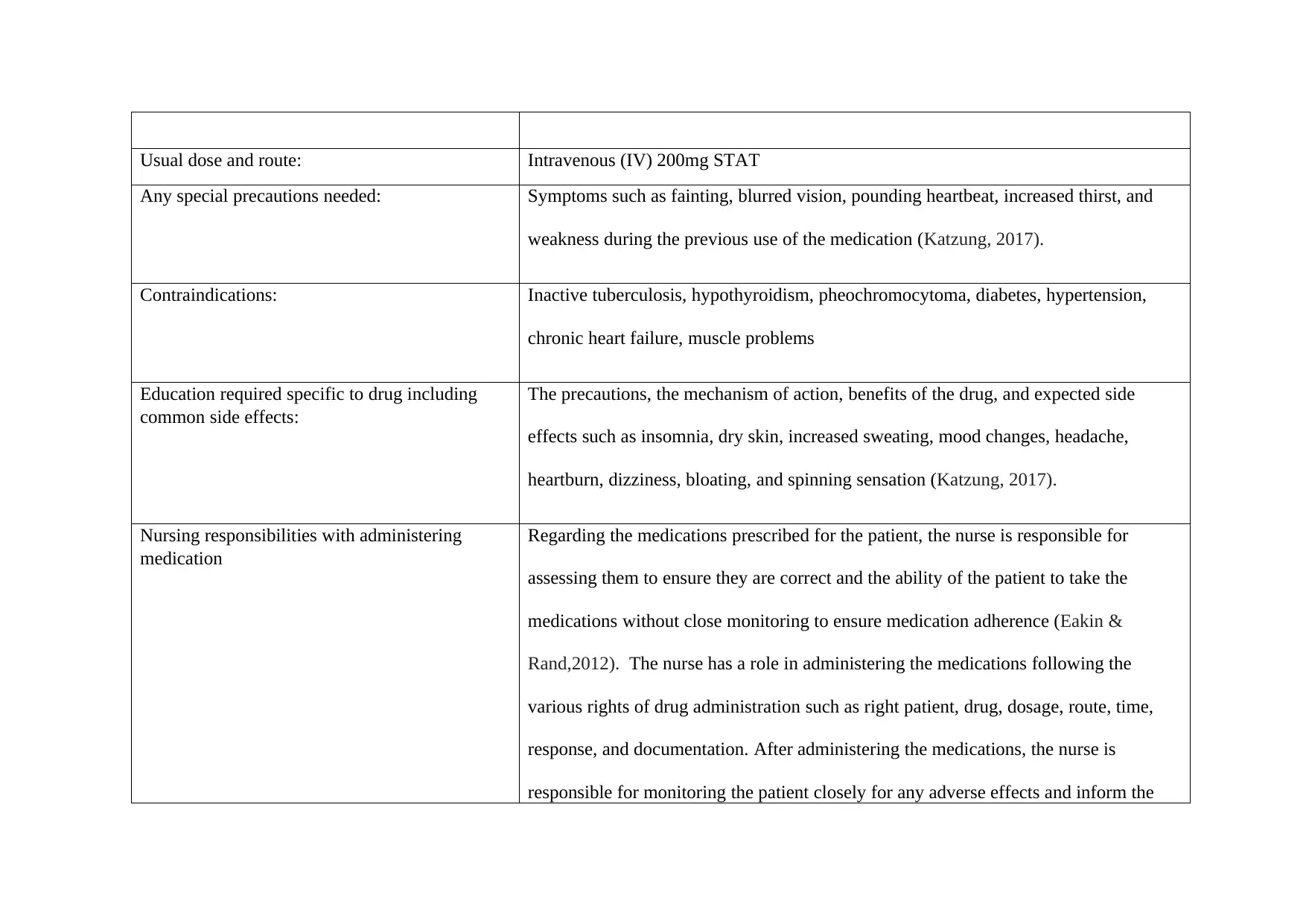
Usual dose and route: Intravenous (IV) 200mg STAT
Any special precautions needed: Symptoms such as fainting, blurred vision, pounding heartbeat, increased thirst, and
weakness during the previous use of the medication (Katzung, 2017).
Contraindications: Inactive tuberculosis, hypothyroidism, pheochromocytoma, diabetes, hypertension,
chronic heart failure, muscle problems
Education required specific to drug including
common side effects:
The precautions, the mechanism of action, benefits of the drug, and expected side
effects such as insomnia, dry skin, increased sweating, mood changes, headache,
heartburn, dizziness, bloating, and spinning sensation (Katzung, 2017).
Nursing responsibilities with administering
medication
Regarding the medications prescribed for the patient, the nurse is responsible for
assessing them to ensure they are correct and the ability of the patient to take the
medications without close monitoring to ensure medication adherence (Eakin &
Rand,2012). The nurse has a role in administering the medications following the
various rights of drug administration such as right patient, drug, dosage, route, time,
response, and documentation. After administering the medications, the nurse is
responsible for monitoring the patient closely for any adverse effects and inform the
Any special precautions needed: Symptoms such as fainting, blurred vision, pounding heartbeat, increased thirst, and
weakness during the previous use of the medication (Katzung, 2017).
Contraindications: Inactive tuberculosis, hypothyroidism, pheochromocytoma, diabetes, hypertension,
chronic heart failure, muscle problems
Education required specific to drug including
common side effects:
The precautions, the mechanism of action, benefits of the drug, and expected side
effects such as insomnia, dry skin, increased sweating, mood changes, headache,
heartburn, dizziness, bloating, and spinning sensation (Katzung, 2017).
Nursing responsibilities with administering
medication
Regarding the medications prescribed for the patient, the nurse is responsible for
assessing them to ensure they are correct and the ability of the patient to take the
medications without close monitoring to ensure medication adherence (Eakin &
Rand,2012). The nurse has a role in administering the medications following the
various rights of drug administration such as right patient, drug, dosage, route, time,
response, and documentation. After administering the medications, the nurse is
responsible for monitoring the patient closely for any adverse effects and inform the
medical officer in case of drug-induced side effects or adverse events (Doenges et al.,
2014).
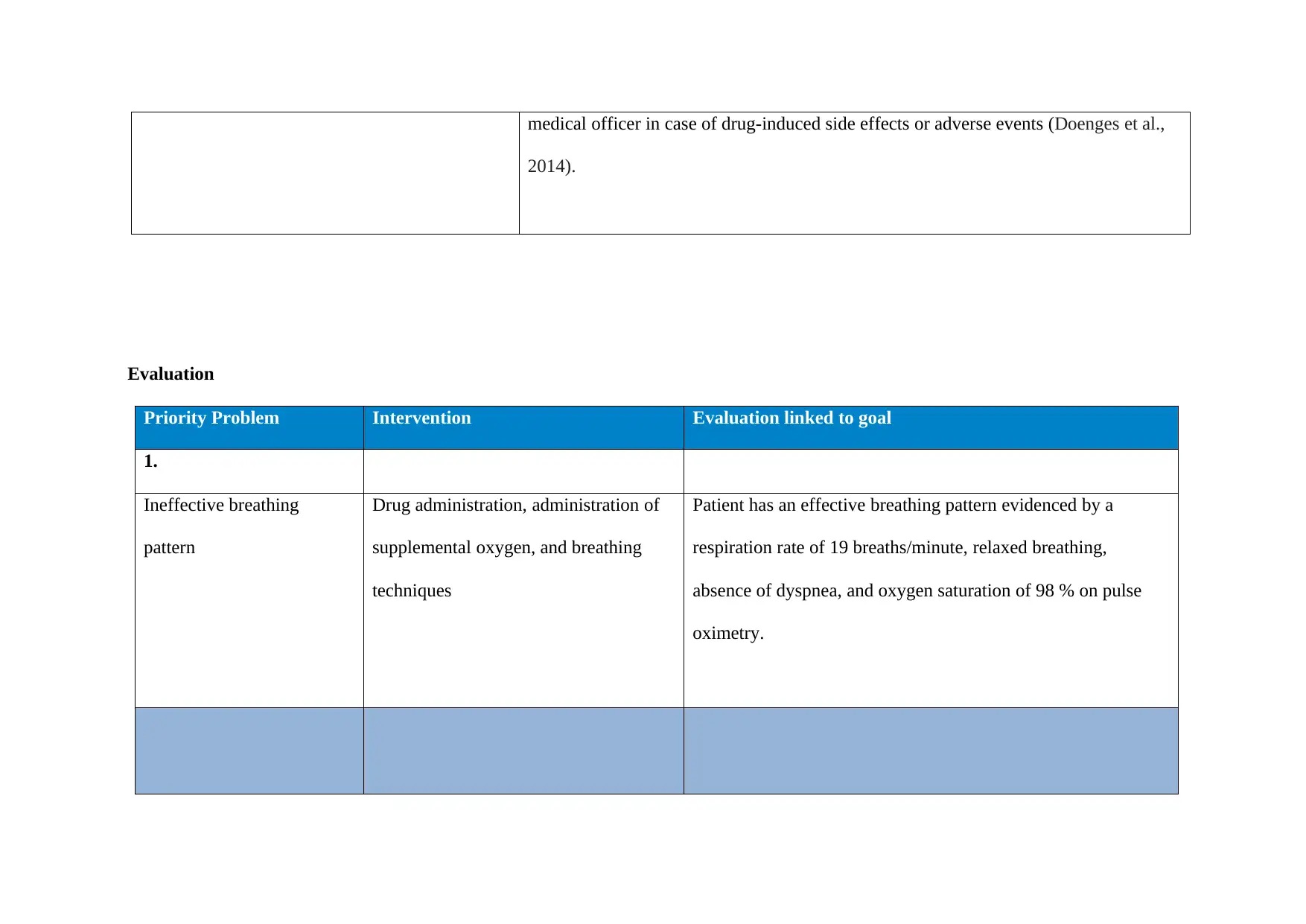
Evaluation
Priority Problem Intervention Evaluation linked to goal
1.
Ineffective breathing
pattern
Drug administration, administration of
supplemental oxygen, and breathing
techniques
Patient has an effective breathing pattern evidenced by a
respiration rate of 19 breaths/minute, relaxed breathing,
absence of dyspnea, and oxygen saturation of 98 % on pulse
oximetry.
2014).
Evaluation
Priority Problem Intervention Evaluation linked to goal
1.
Ineffective breathing
pattern
Drug administration, administration of
supplemental oxygen, and breathing
techniques
Patient has an effective breathing pattern evidenced by a
respiration rate of 19 breaths/minute, relaxed breathing,
absence of dyspnea, and oxygen saturation of 98 % on pulse
oximetry.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
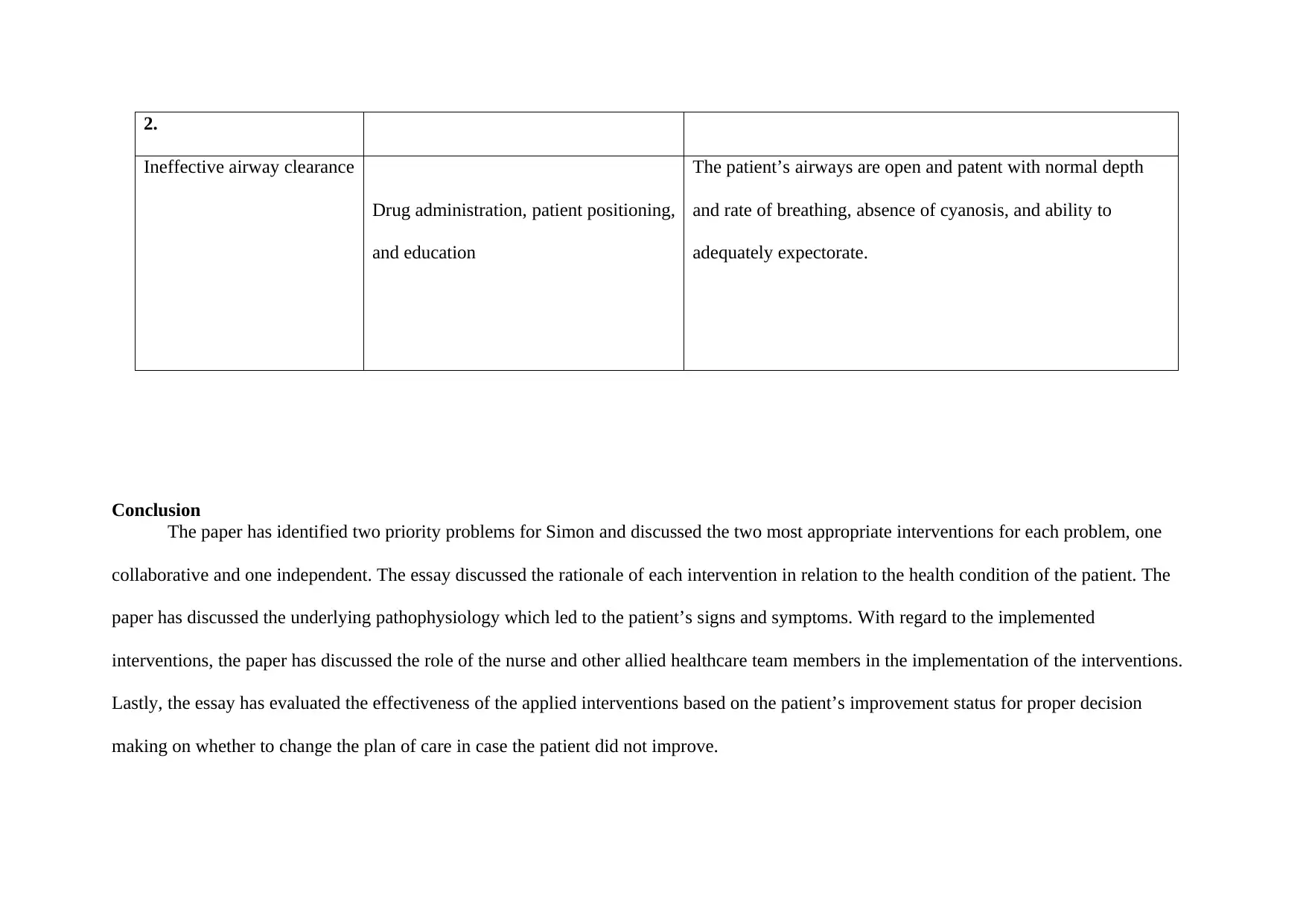
2.
Ineffective airway clearance
Drug administration, patient positioning,
and education
The patient’s airways are open and patent with normal depth
and rate of breathing, absence of cyanosis, and ability to
adequately expectorate.
Conclusion
The paper has identified two priority problems for Simon and discussed the two most appropriate interventions for each problem, one
collaborative and one independent. The essay discussed the rationale of each intervention in relation to the health condition of the patient. The
paper has discussed the underlying pathophysiology which led to the patient’s signs and symptoms. With regard to the implemented
interventions, the paper has discussed the role of the nurse and other allied healthcare team members in the implementation of the interventions.
Lastly, the essay has evaluated the effectiveness of the applied interventions based on the patient’s improvement status for proper decision
making on whether to change the plan of care in case the patient did not improve.
Ineffective airway clearance
Drug administration, patient positioning,
and education
The patient’s airways are open and patent with normal depth
and rate of breathing, absence of cyanosis, and ability to
adequately expectorate.
Conclusion
The paper has identified two priority problems for Simon and discussed the two most appropriate interventions for each problem, one
collaborative and one independent. The essay discussed the rationale of each intervention in relation to the health condition of the patient. The
paper has discussed the underlying pathophysiology which led to the patient’s signs and symptoms. With regard to the implemented
interventions, the paper has discussed the role of the nurse and other allied healthcare team members in the implementation of the interventions.
Lastly, the essay has evaluated the effectiveness of the applied interventions based on the patient’s improvement status for proper decision
making on whether to change the plan of care in case the patient did not improve.
References
Ackley, B. J., Ladwig, G. B., Msn, R. N., Makic, M. B. F., Martinez-Kratz, M., & Zanotti, M. (2019). Nursing Diagnosis Handbook E-Book: An
Evidence-Based Guide to Planning Care. Mosby.
Basnet, S., Mander, G., Andoh, J., Klaska, H., Verhulst, S., & Koirala, J. (2012). Safety, efficacy, and tolerability of early initiation of
noninvasive positive pressure ventilation in pediatric patients admitted with status asthmaticus: a pilot study. Pediatric Critical Care
Medicine, 13(4), 393-398.
Ackley, B. J., Ladwig, G. B., Msn, R. N., Makic, M. B. F., Martinez-Kratz, M., & Zanotti, M. (2019). Nursing Diagnosis Handbook E-Book: An
Evidence-Based Guide to Planning Care. Mosby.
Basnet, S., Mander, G., Andoh, J., Klaska, H., Verhulst, S., & Koirala, J. (2012). Safety, efficacy, and tolerability of early initiation of
noninvasive positive pressure ventilation in pediatric patients admitted with status asthmaticus: a pilot study. Pediatric Critical Care
Medicine, 13(4), 393-398.
Cabana, M. D., Slish, K. K., Evans, D., Mellins, R. B., Brown, R. W., Lin, X., ... & Clark, N. M. (2014). Impact of physician asthma care
education on patient outcomes. Health Education & Behavior, 41(5), 509-517.
Chang, C. (2012). Asthma in children and adolescents: a comprehensive approach to diagnosis and management. Clinical reviews in allergy &
immunology, 43(1-2), 98-137.
Doenges, M. E., Moorhouse, M. F., & Murr, A. C. (2014). Nursing care plans: Guidelines for individualizing client care across the life span. FA
Davis.
Eakin, M. N., & Rand, C. S. (2012). Improving patient adherence with asthma self-management practices: what works?. Annals of Allergy,
Asthma & Immunology, 109(2), 90-92.
Hinkle, J. L., & Cheever, K. H. (2013). Study Guide for Brunner & Suddarth's Textbook of Medical-surgical Nursing. Lippincott Williams &
Wilkins.
Lewis, S. L., Dirksen, S. R., Heitkemper, M. M., Bucher, L., & Camera, I. (2015). Medical-Surgical Nursing-E-Book: Assessment and
Management of Clinical Problems, Single Volume. Elsevier Health Sciences.
Peters, J. I., Stupka, J. E., Singh, H., Rossrucker, J., Angel, L. F., Melo, J., & Levine, S. M. (2012). Status asthmaticus in the medical intensive
care unit: a 30-year experience. Respiratory medicine, 106(3), 344-348.
education on patient outcomes. Health Education & Behavior, 41(5), 509-517.
Chang, C. (2012). Asthma in children and adolescents: a comprehensive approach to diagnosis and management. Clinical reviews in allergy &
immunology, 43(1-2), 98-137.
Doenges, M. E., Moorhouse, M. F., & Murr, A. C. (2014). Nursing care plans: Guidelines for individualizing client care across the life span. FA
Davis.
Eakin, M. N., & Rand, C. S. (2012). Improving patient adherence with asthma self-management practices: what works?. Annals of Allergy,
Asthma & Immunology, 109(2), 90-92.
Hinkle, J. L., & Cheever, K. H. (2013). Study Guide for Brunner & Suddarth's Textbook of Medical-surgical Nursing. Lippincott Williams &
Wilkins.
Lewis, S. L., Dirksen, S. R., Heitkemper, M. M., Bucher, L., & Camera, I. (2015). Medical-Surgical Nursing-E-Book: Assessment and
Management of Clinical Problems, Single Volume. Elsevier Health Sciences.
Peters, J. I., Stupka, J. E., Singh, H., Rossrucker, J., Angel, L. F., Melo, J., & Levine, S. M. (2012). Status asthmaticus in the medical intensive
care unit: a 30-year experience. Respiratory medicine, 106(3), 344-348.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Pinfield, J., Gaskin, K., Bentley, J., & Rouse, J. (2015). Recognition and management of asthma in children and young people. Nursing
Standard (2014+), 30(3), 50.
Salahuddin, F. F., Sloane, P., Buescher, P., Agarunov, L., & Sreeramoju, D. (2013). A case of apical ballooning syndrome in a male with status
asthmaticus; highlighting the role of B2 agonists in the pathophysiology of a reversible cardiomyopathy. Journal of community hospital
internal medicine perspectives, 3(2), 20530.
Shah, R., & Saltoun, C. A. (2012, May). Acute severe asthma (status asthmaticus). In Allergy and Asthma proceedings (Vol. 33, No. 3, p. 47).
OceanSide Publications.
Skaletzky, S., & Totapally, B. R. (2013). Common topics in adolescent critical care medicine. Adolescent medicine: state of the art
reviews, 24(1), 167-84.
Smeulers, M., Onderwater, A. T., Zwieten, M. C., & Vermeulen, H. (2014). Nurses' experiences and perspectives on medication safety practices:
an explorative qualitative study. Journal of Nursing Management, 22(3), 276-285.
Sousa, V. E. C., Lopes, M. V. D. O., & Silva, V. M. (2015). Systematic review and meta‐analysis of the accuracy of clinical indicators for
ineffective airway clearance. Journal of advanced nursing, 71(3), 498-513.
Katzung, B. G. (2017). Basic and clinical pharmacology. McGraw-Hill Education.
Standard (2014+), 30(3), 50.
Salahuddin, F. F., Sloane, P., Buescher, P., Agarunov, L., & Sreeramoju, D. (2013). A case of apical ballooning syndrome in a male with status
asthmaticus; highlighting the role of B2 agonists in the pathophysiology of a reversible cardiomyopathy. Journal of community hospital
internal medicine perspectives, 3(2), 20530.
Shah, R., & Saltoun, C. A. (2012, May). Acute severe asthma (status asthmaticus). In Allergy and Asthma proceedings (Vol. 33, No. 3, p. 47).
OceanSide Publications.
Skaletzky, S., & Totapally, B. R. (2013). Common topics in adolescent critical care medicine. Adolescent medicine: state of the art
reviews, 24(1), 167-84.
Smeulers, M., Onderwater, A. T., Zwieten, M. C., & Vermeulen, H. (2014). Nurses' experiences and perspectives on medication safety practices:
an explorative qualitative study. Journal of Nursing Management, 22(3), 276-285.
Sousa, V. E. C., Lopes, M. V. D. O., & Silva, V. M. (2015). Systematic review and meta‐analysis of the accuracy of clinical indicators for
ineffective airway clearance. Journal of advanced nursing, 71(3), 498-513.
Katzung, B. G. (2017). Basic and clinical pharmacology. McGraw-Hill Education.
1 out of 23
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





