Nursing Priorities-Status Asthmaticus
Added on 2023-01-19
23 Pages3456 Words77 Views
NURSING PRIORITIES-STATUS ASTHMATICUS
Student’s Name
Institutional Affiliation
Course
Date
Instructor
Student’s Name
Institutional Affiliation
Course
Date
Instructor

Introduction
The nurse plays a fundamental role in the assessment, planning, implementation, and evaluation of care of a patient with status asthmatic.
The essay will focus on the case option 1 of Simon who is 14 years with Status asthmaticus. On ex amination at the emergency department,
Simon has audible wheeze and cannot communicate in full sentences. He has a respiratory rate of 32 breaths per minute, Oxygen Saturation of
88 percent, and a pulse of 132 beats per minute. The paper will identify and discuss two priority problems for Simon and discuss two major
interventions for each priority including independent and collaborative approaches.
Pathophysiology of Status Asthmaticus
Status asthmaticus refers to severe form of asthma whose exacerbation results in hypercarbia, hypoxemia, and respiratory failure since it
does not respond to the standard treatments such as corticosteroids and bronchodilators (Skaletzky & Totapally, 2013). Status asthmaticus is
stimulated by multiple triggers including respiratory infections, severe allergic reactions, severe stress, air pollution, smoking, cold weather,
smoking, and exposure to irritants and chemicals. There are pathophysiological mechanisms which result in changes of the airway through
airway limitation. These mechanisms include bronchoconstriction, hyperresponsiveness, airway edema, and remodeling of the airways (Hinkle
& Cheever, 2013).
In acute asthma attacks, bronchoconstriction causes the narrowing of the airways after exposure to irritants and allergens. Acute
bronchoconstriction following the exposure to allergens is attributed to the release of IgE-independent mediators from the mast cells which
directly result in the contraction of the smooth muscles of the airway (Hinkle & Cheever, 2013). Medications such as Non-steroidal anti-
inflammatory and aspirin contribute to the obstruction of the airway.
The nurse plays a fundamental role in the assessment, planning, implementation, and evaluation of care of a patient with status asthmatic.
The essay will focus on the case option 1 of Simon who is 14 years with Status asthmaticus. On ex amination at the emergency department,
Simon has audible wheeze and cannot communicate in full sentences. He has a respiratory rate of 32 breaths per minute, Oxygen Saturation of
88 percent, and a pulse of 132 beats per minute. The paper will identify and discuss two priority problems for Simon and discuss two major
interventions for each priority including independent and collaborative approaches.
Pathophysiology of Status Asthmaticus
Status asthmaticus refers to severe form of asthma whose exacerbation results in hypercarbia, hypoxemia, and respiratory failure since it
does not respond to the standard treatments such as corticosteroids and bronchodilators (Skaletzky & Totapally, 2013). Status asthmaticus is
stimulated by multiple triggers including respiratory infections, severe allergic reactions, severe stress, air pollution, smoking, cold weather,
smoking, and exposure to irritants and chemicals. There are pathophysiological mechanisms which result in changes of the airway through
airway limitation. These mechanisms include bronchoconstriction, hyperresponsiveness, airway edema, and remodeling of the airways (Hinkle
& Cheever, 2013).
In acute asthma attacks, bronchoconstriction causes the narrowing of the airways after exposure to irritants and allergens. Acute
bronchoconstriction following the exposure to allergens is attributed to the release of IgE-independent mediators from the mast cells which
directly result in the contraction of the smooth muscles of the airway (Hinkle & Cheever, 2013). Medications such as Non-steroidal anti-
inflammatory and aspirin contribute to the obstruction of the airway.
The persistence and progress of the inflammatory process in the airway results in further limit of airflow. The factors which contribute to
this include mucus hypersecretion, inflammation, airway edema, development of mucus plugs which are inspissated and airway hypertrophy and
hyperplasia. Airway hyperresponsiveness is an exaggerated response to the bronchoconstrictors. Some of the mechanisms that influence the
hyperresponsiveness of the airway include inflammation, and structural changes (Chang, 2012).
Airway remodeling results in the development and severity of asthmatic attacks in a patient. The process of remodeling involves the
activation of multiple structural cells which consequently result in permanent airway changes which result in increased obstruction of the airway
and responsiveness. This makes the patient to be less responsive to the prescribed medical therapy (Lewis, Dirksen, Heitkemper, Bucher, &
Camera, 2015). The structural changes associated with the remodeling of the airway include subepithelial fibrosis, thickening of sub-basement
membrane, proliferation and vasodilation of vessels, and hypersecretion by the mucus glands
The inflammatory process plays a central role in the underlying pathophysiology of severe asthmatic attacks. The inflammation of the
airway involves the interaction of multiple mediators and cell types with the airway thus resulting in characteristic pathophysiological
manifestations of the condition such as airway limitation and bronchial inflammation which leads to recurrent episodes of wheeze, cough, and
dyspnea (Lewis et al., 2015).
Priority Problems for Simon
Priority Problem Goal Assessment data Underlying pathophysiology
1. To maintain an On examination at the emergency Asthma is the chronic inflammation
this include mucus hypersecretion, inflammation, airway edema, development of mucus plugs which are inspissated and airway hypertrophy and
hyperplasia. Airway hyperresponsiveness is an exaggerated response to the bronchoconstrictors. Some of the mechanisms that influence the
hyperresponsiveness of the airway include inflammation, and structural changes (Chang, 2012).
Airway remodeling results in the development and severity of asthmatic attacks in a patient. The process of remodeling involves the
activation of multiple structural cells which consequently result in permanent airway changes which result in increased obstruction of the airway
and responsiveness. This makes the patient to be less responsive to the prescribed medical therapy (Lewis, Dirksen, Heitkemper, Bucher, &
Camera, 2015). The structural changes associated with the remodeling of the airway include subepithelial fibrosis, thickening of sub-basement
membrane, proliferation and vasodilation of vessels, and hypersecretion by the mucus glands
The inflammatory process plays a central role in the underlying pathophysiology of severe asthmatic attacks. The inflammation of the
airway involves the interaction of multiple mediators and cell types with the airway thus resulting in characteristic pathophysiological
manifestations of the condition such as airway limitation and bronchial inflammation which leads to recurrent episodes of wheeze, cough, and
dyspnea (Lewis et al., 2015).
Priority Problems for Simon
Priority Problem Goal Assessment data Underlying pathophysiology
1. To maintain an On examination at the emergency Asthma is the chronic inflammation
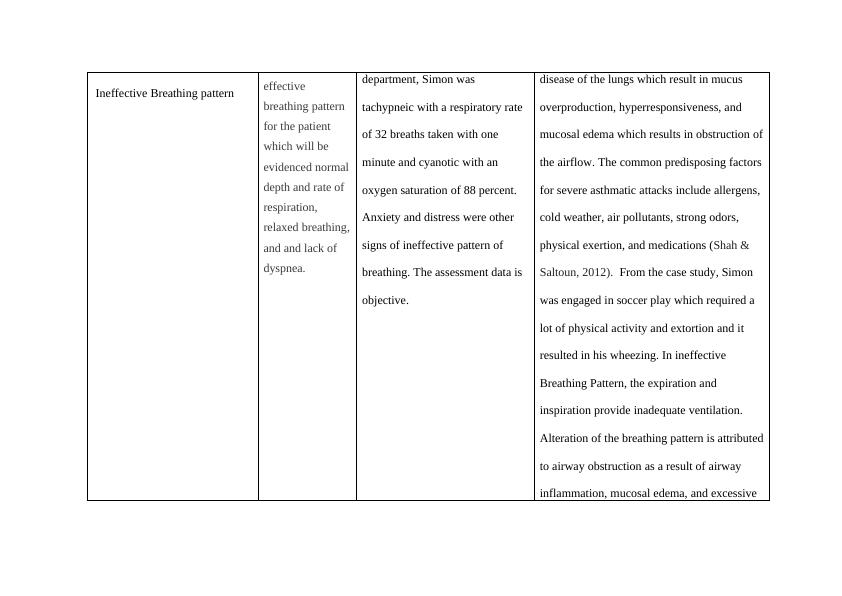
Ineffective Breathing pattern effective
breathing pattern
for the patient
which will be
evidenced normal
depth and rate of
respiration,
relaxed breathing,
and and lack of
dyspnea.
department, Simon was
tachypneic with a respiratory rate
of 32 breaths taken with one
minute and cyanotic with an
oxygen saturation of 88 percent.
Anxiety and distress were other
signs of ineffective pattern of
breathing. The assessment data is
objective.
disease of the lungs which result in mucus
overproduction, hyperresponsiveness, and
mucosal edema which results in obstruction of
the airflow. The common predisposing factors
for severe asthmatic attacks include allergens,
cold weather, air pollutants, strong odors,
physical exertion, and medications (Shah &
Saltoun, 2012). From the case study, Simon
was engaged in soccer play which required a
lot of physical activity and extortion and it
resulted in his wheezing. In ineffective
Breathing Pattern, the expiration and
inspiration provide inadequate ventilation.
Alteration of the breathing pattern is attributed
to airway obstruction as a result of airway
inflammation, mucosal edema, and excessive
breathing pattern
for the patient
which will be
evidenced normal
depth and rate of
respiration,
relaxed breathing,
and and lack of
dyspnea.
department, Simon was
tachypneic with a respiratory rate
of 32 breaths taken with one
minute and cyanotic with an
oxygen saturation of 88 percent.
Anxiety and distress were other
signs of ineffective pattern of
breathing. The assessment data is
objective.
disease of the lungs which result in mucus
overproduction, hyperresponsiveness, and
mucosal edema which results in obstruction of
the airflow. The common predisposing factors
for severe asthmatic attacks include allergens,
cold weather, air pollutants, strong odors,
physical exertion, and medications (Shah &
Saltoun, 2012). From the case study, Simon
was engaged in soccer play which required a
lot of physical activity and extortion and it
resulted in his wheezing. In ineffective
Breathing Pattern, the expiration and
inspiration provide inadequate ventilation.
Alteration of the breathing pattern is attributed
to airway obstruction as a result of airway
inflammation, mucosal edema, and excessive
production of secretions which results in
limited flow of air in the respiratory system
(Ackley et al., 2019).
Some of the indicators of an
ineffective breathing pattern include cyanosis,
cough, dyspnea, tachypnea, prolonged
expiration, changes in respiratory depth, and
loss of consciousness. (Doenges, Moorhouse,
& Murr, 2014).
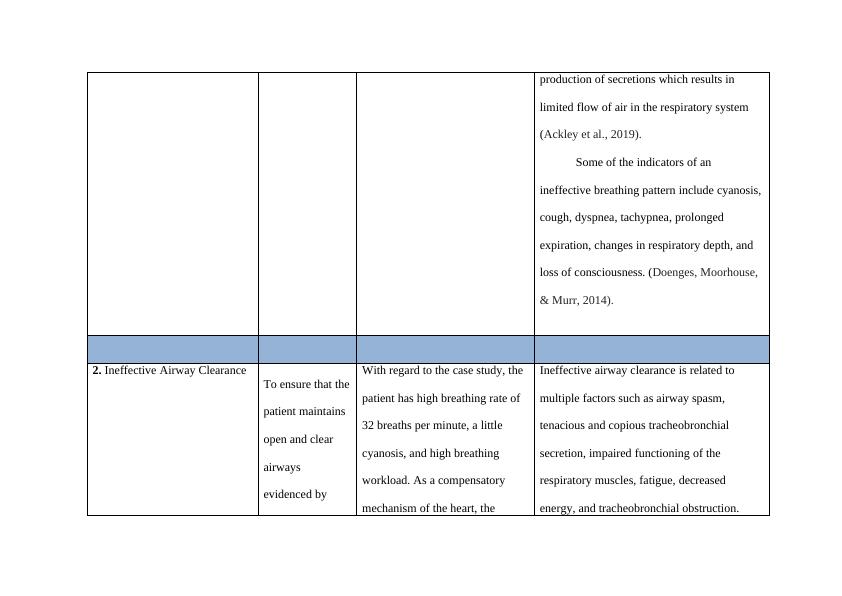
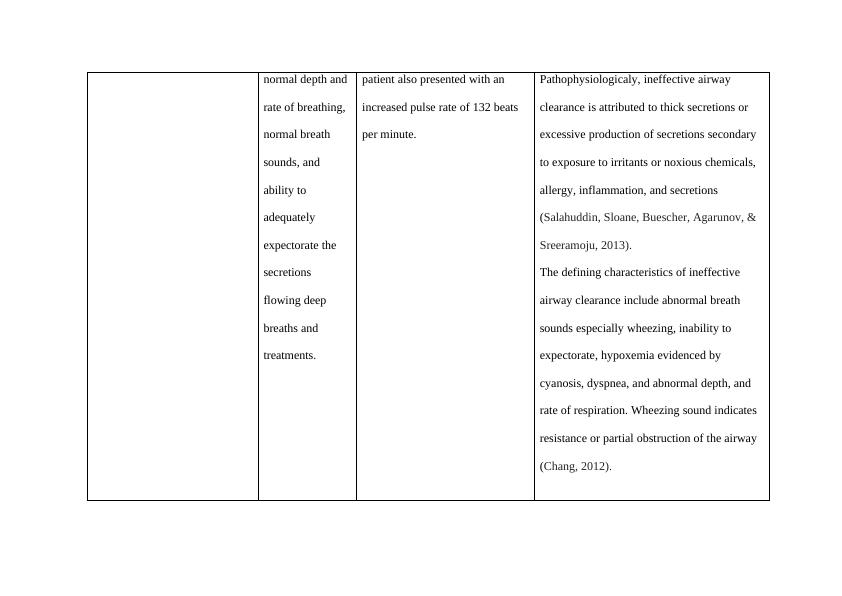
2. Ineffective Airway Clearance
To ensure that the
patient maintains
open and clear
airways
evidenced by
With regard to the case study, the
patient has high breathing rate of
32 breaths per minute, a little
cyanosis, and high breathing
workload. As a compensatory
mechanism of the heart, the
Ineffective airway clearance is related to
multiple factors such as airway spasm,
tenacious and copious tracheobronchial
secretion, impaired functioning of the
respiratory muscles, fatigue, decreased
energy, and tracheobronchial obstruction.
limited flow of air in the respiratory system
(Ackley et al., 2019).
Some of the indicators of an
ineffective breathing pattern include cyanosis,
cough, dyspnea, tachypnea, prolonged
expiration, changes in respiratory depth, and
loss of consciousness. (Doenges, Moorhouse,
& Murr, 2014).
2. Ineffective Airway Clearance
To ensure that the
patient maintains
open and clear
airways
evidenced by
With regard to the case study, the
patient has high breathing rate of
32 breaths per minute, a little
cyanosis, and high breathing
workload. As a compensatory
mechanism of the heart, the
Ineffective airway clearance is related to
multiple factors such as airway spasm,
tenacious and copious tracheobronchial
secretion, impaired functioning of the
respiratory muscles, fatigue, decreased
energy, and tracheobronchial obstruction.
normal depth and
rate of breathing,
normal breath
sounds, and
ability to
adequately
expectorate the
secretions
flowing deep
breaths and
treatments.
patient also presented with an
increased pulse rate of 132 beats
per minute.
Pathophysiologicaly, ineffective airway
clearance is attributed to thick secretions or
excessive production of secretions secondary
to exposure to irritants or noxious chemicals,
allergy, inflammation, and secretions
(Salahuddin, Sloane, Buescher, Agarunov, &
Sreeramoju, 2013).
The defining characteristics of ineffective
airway clearance include abnormal breath
sounds especially wheezing, inability to
expectorate, hypoxemia evidenced by
cyanosis, dyspnea, and abnormal depth, and
rate of respiration. Wheezing sound indicates
resistance or partial obstruction of the airway
(Chang, 2012).
rate of breathing,
normal breath
sounds, and
ability to
adequately
expectorate the
secretions
flowing deep
breaths and
treatments.
patient also presented with an
increased pulse rate of 132 beats
per minute.
Pathophysiologicaly, ineffective airway
clearance is attributed to thick secretions or
excessive production of secretions secondary
to exposure to irritants or noxious chemicals,
allergy, inflammation, and secretions
(Salahuddin, Sloane, Buescher, Agarunov, &
Sreeramoju, 2013).
The defining characteristics of ineffective
airway clearance include abnormal breath
sounds especially wheezing, inability to
expectorate, hypoxemia evidenced by
cyanosis, dyspnea, and abnormal depth, and
rate of respiration. Wheezing sound indicates
resistance or partial obstruction of the airway
(Chang, 2012).
End of preview
Want to access all the pages? Upload your documents or become a member.
Related Documents
Priority Problems in Asthma: Ineffective Airway Clearance and Impaired Gaseous Exchangelg...
|13
|3513
|23
Body Integrity Assignment PDFlg...
|5
|1450
|42
Pathogenesis of Severe Acute Asthma: Understanding the Mechanisms and Nursing Prioritieslg...
|8
|2078
|347
Pathophysiology of Asthma and Clinical Manifestations: A Case Studylg...
|8
|1938
|93
NURS 1400 - Chronic Asthma | Self Management of Chronic Asthma Assignmentlg...
|12
|2680
|44
Nurses Care Practice Case Study 2022lg...
|7
|1986
|20
