Grand Canyon University: Diabetes Education for Diverse Populations
VerifiedAdded on 2022/08/24
|27
|2268
|37
Presentation
AI Summary
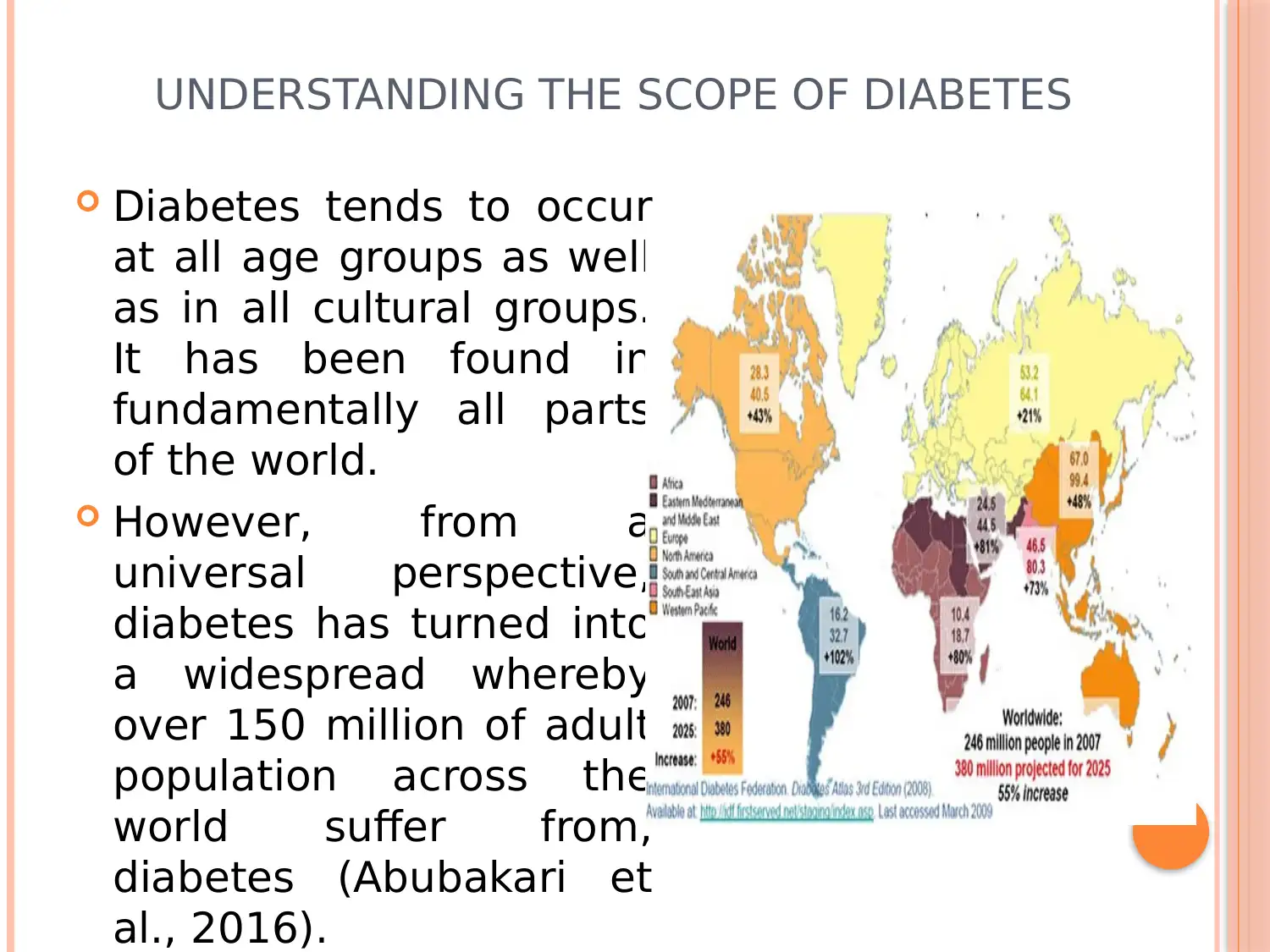
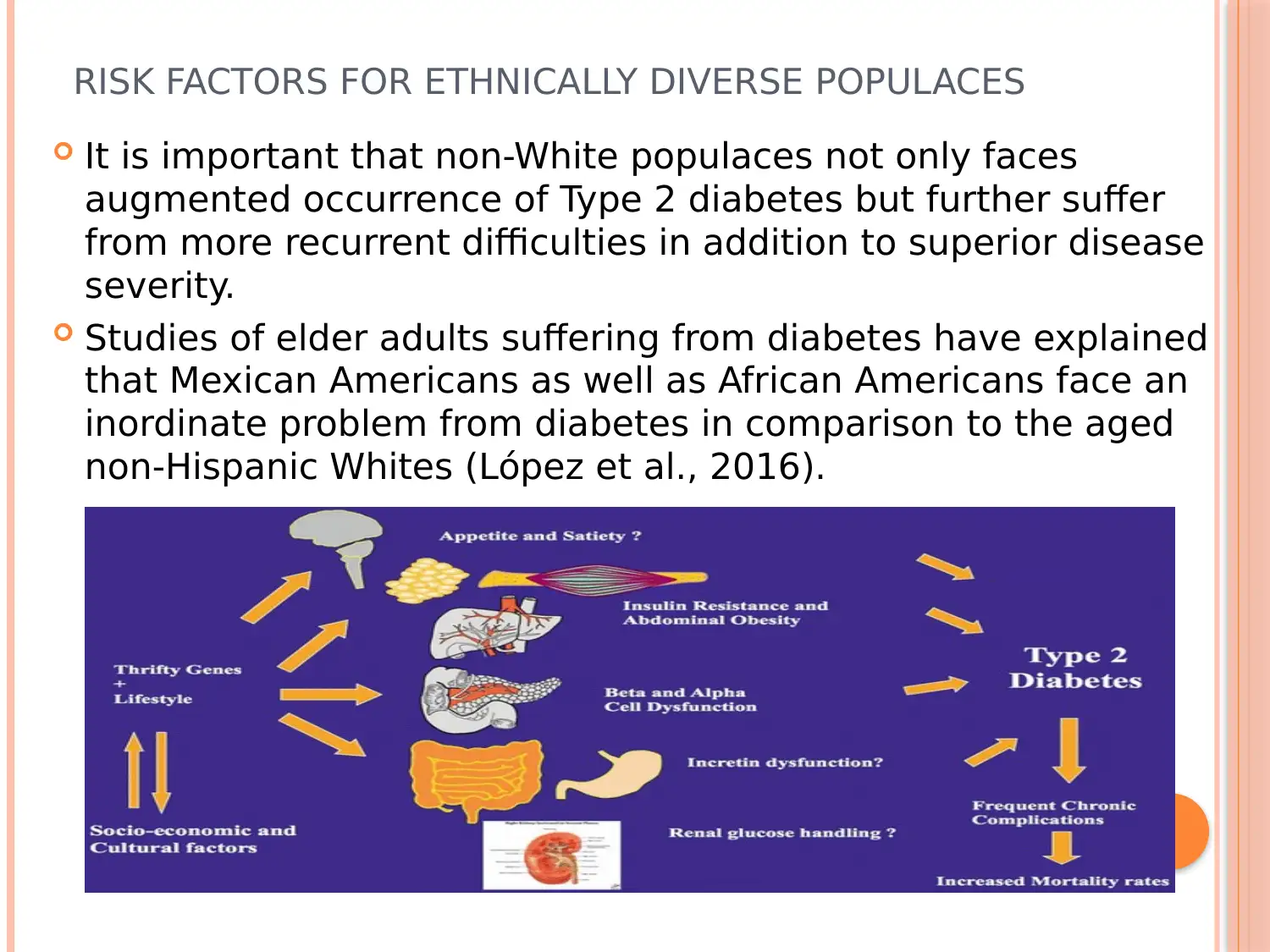
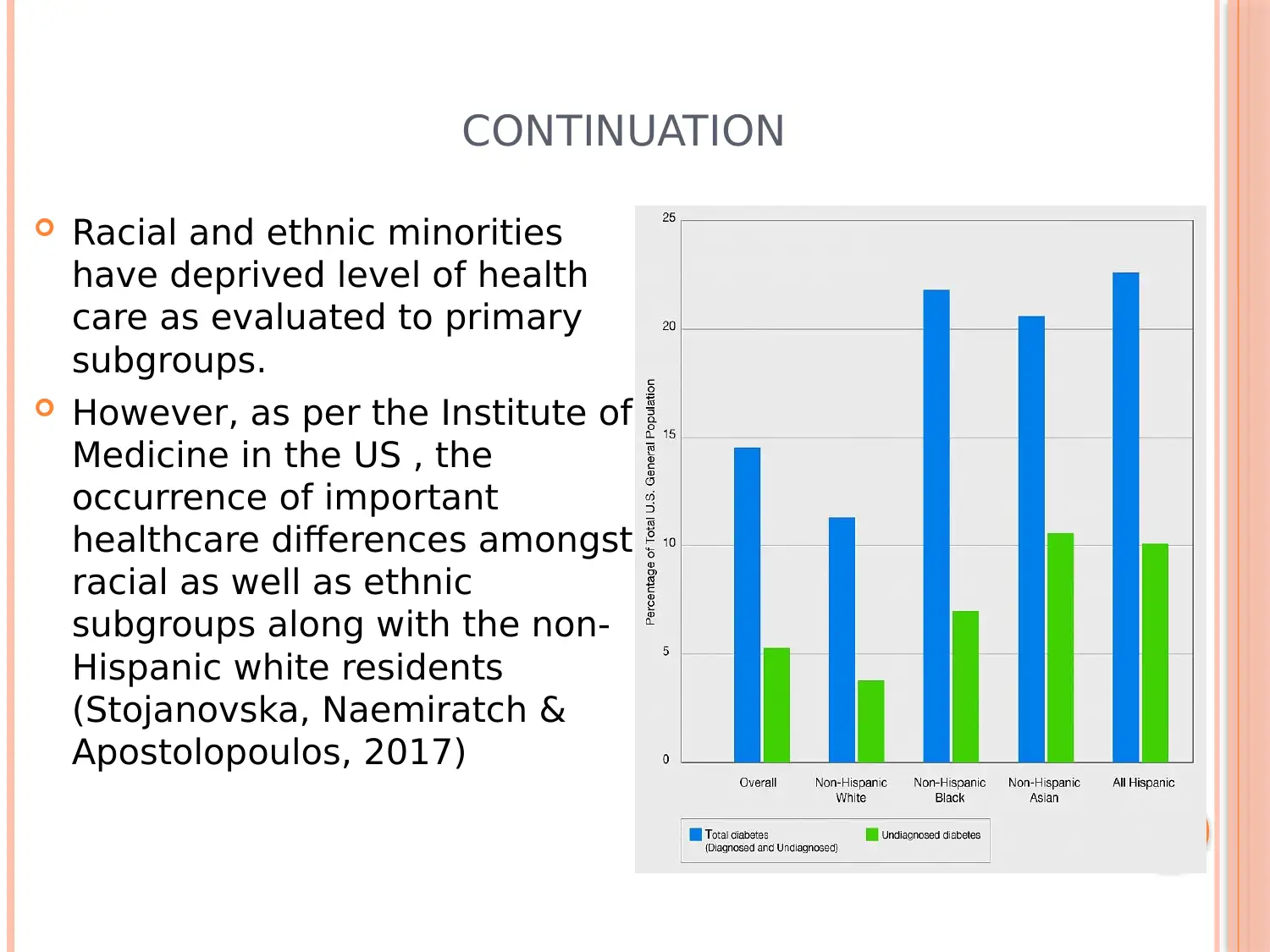
This presentation addresses the critical need for culturally sensitive diabetes education, particularly focusing on the disproportionate impact of Type 2 diabetes on racial and ethnic minorities. It emphasizes the importance of understanding cultural factors, beliefs, and practices in providing effective diabetes self-management education. The presentation covers the scope of diabetes, risk factors for diverse populations, community education strategies, and the biology of Type 2 diabetes. It also addresses cultural barriers to insulin use, fears related to diabetes, and the importance of group engagement and nutritional preferences. The conclusion highlights the challenges healthcare providers face in delivering care to diverse patient populations and underscores the significance of considering patients' perspectives, values, and language barriers to achieve optimal health outcomes. The presentation is based on research from various sources and is designed to inform healthcare professionals on best practices for diabetes education in diverse communities.
1 out of 27






![[object Object]](/_next/static/media/star-bottom.7253800d.svg)