HLTAAP003: Pneumonia Case Study Analysis, Treatment and Care Plan
VerifiedAdded on 2023/06/04
|8
|1716
|315
Case Study
AI Summary
This case study examines a patient diagnosed with pneumonia, focusing on the analysis of the patient's symptoms, vital signs, and medical history, including diabetes and bronchitis. The document delves into the pathophysiology of pneumonia, explaining how the infection affects the lungs and triggers an immune response. It analyzes the significance of the patient's elevated respiratory rate, fever, and low oxygen saturation, relating them to the disease process. The case study also explores the patient's history of diabetes and its impact on their susceptibility to infection. Furthermore, it outlines potential treatment options, including antibiotics and supportive care such as oxygen therapy and intravenous fluids, and proposes a comprehensive nursing care plan. The care plan details assessment, diagnosis, planning, intervention, rationale, and evaluation, providing a structured approach to managing the patient's condition and promoting improved ventilation and oxygenation.

Nursing
Student’s name:
Institutional:
Student’s name:
Institutional:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Pneumonia
Pneumonia is a disease which affects the lung and usually portrayed by the airspaces (alveoli) in
the lungs being inflamed, mostly as a result of infection. Causes of pneumonia include infections
caused by viruses, bacteria or fungi. It is a more serious disease especially when in infects young
children and infants or the elderly since there immune system is weak. Those with weakened
immunity for example, those suffering from HIV/AIDS also get affected much when they get
infected with pneumonia. Pneumonia can be classified as Hospital-acquired pneumonia,
community-acquired pneumonia and aspiration pneumonia. Hospital-acquired pneumonia
develops when a person is already in the hospital premises whereas community-acquired is
acquired outside the healthcare environment. Aspiration pneumonia on the other hand is as a
result of food, drink, vomit or saliva inhalation when the swallowing reflex is ineffective.
Pneumonia may also be classified according to the causative agent, for example bacterial
pneumonia or viral pneumonia. Most types of pneumonia are contagious and may easily spread
from one person to another through inhalation of droplets from sneeze or even cough (La Rosa,
Fratini, Libera, Iaconelli,. and Muscillo, 2013 pp. 124-132).
Pathophysiology of Pneumonia
When an organism such as bacteria, fungi or virus reaches the lungs they trigger an immune
response (Singh 2012, pp. 7-9). This makes the neutrophils to engulf the invading pathogen and
cytokines are released. This leads to inflammatory reactions. The lungs become hyperaemic.
Fluid shifts from the intravascular spaces into the alveoli and lung tissue since the capillaries
become highly permeable. This results to impairment of ventilation as the gaseous exchange
space become less. Congestion of the lungs therefore ensues due to the fluid shifting. The lungs
appear hard and red. This is shown by the large amount of confluent exudates by red blood cells,
Pneumonia is a disease which affects the lung and usually portrayed by the airspaces (alveoli) in
the lungs being inflamed, mostly as a result of infection. Causes of pneumonia include infections
caused by viruses, bacteria or fungi. It is a more serious disease especially when in infects young
children and infants or the elderly since there immune system is weak. Those with weakened
immunity for example, those suffering from HIV/AIDS also get affected much when they get
infected with pneumonia. Pneumonia can be classified as Hospital-acquired pneumonia,
community-acquired pneumonia and aspiration pneumonia. Hospital-acquired pneumonia
develops when a person is already in the hospital premises whereas community-acquired is
acquired outside the healthcare environment. Aspiration pneumonia on the other hand is as a
result of food, drink, vomit or saliva inhalation when the swallowing reflex is ineffective.
Pneumonia may also be classified according to the causative agent, for example bacterial
pneumonia or viral pneumonia. Most types of pneumonia are contagious and may easily spread
from one person to another through inhalation of droplets from sneeze or even cough (La Rosa,
Fratini, Libera, Iaconelli,. and Muscillo, 2013 pp. 124-132).
Pathophysiology of Pneumonia
When an organism such as bacteria, fungi or virus reaches the lungs they trigger an immune
response (Singh 2012, pp. 7-9). This makes the neutrophils to engulf the invading pathogen and
cytokines are released. This leads to inflammatory reactions. The lungs become hyperaemic.
Fluid shifts from the intravascular spaces into the alveoli and lung tissue since the capillaries
become highly permeable. This results to impairment of ventilation as the gaseous exchange
space become less. Congestion of the lungs therefore ensues due to the fluid shifting. The lungs
appear hard and red. This is shown by the large amount of confluent exudates by red blood cells,
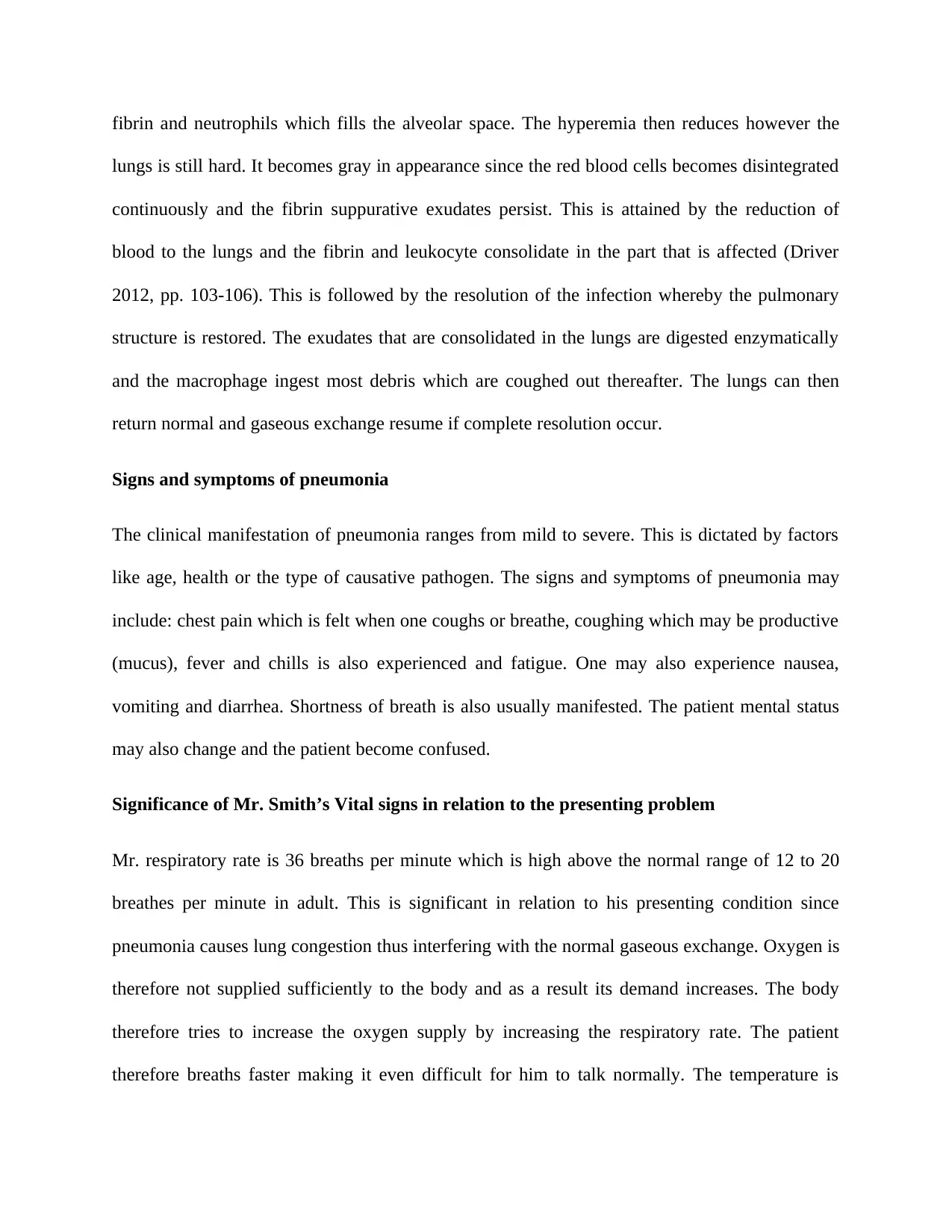
fibrin and neutrophils which fills the alveolar space. The hyperemia then reduces however the
lungs is still hard. It becomes gray in appearance since the red blood cells becomes disintegrated
continuously and the fibrin suppurative exudates persist. This is attained by the reduction of
blood to the lungs and the fibrin and leukocyte consolidate in the part that is affected (Driver
2012, pp. 103-106). This is followed by the resolution of the infection whereby the pulmonary
structure is restored. The exudates that are consolidated in the lungs are digested enzymatically
and the macrophage ingest most debris which are coughed out thereafter. The lungs can then
return normal and gaseous exchange resume if complete resolution occur.
Signs and symptoms of pneumonia
The clinical manifestation of pneumonia ranges from mild to severe. This is dictated by factors
like age, health or the type of causative pathogen. The signs and symptoms of pneumonia may
include: chest pain which is felt when one coughs or breathe, coughing which may be productive
(mucus), fever and chills is also experienced and fatigue. One may also experience nausea,
vomiting and diarrhea. Shortness of breath is also usually manifested. The patient mental status
may also change and the patient become confused.
Significance of Mr. Smith’s Vital signs in relation to the presenting problem
Mr. respiratory rate is 36 breaths per minute which is high above the normal range of 12 to 20
breathes per minute in adult. This is significant in relation to his presenting condition since
pneumonia causes lung congestion thus interfering with the normal gaseous exchange. Oxygen is
therefore not supplied sufficiently to the body and as a result its demand increases. The body
therefore tries to increase the oxygen supply by increasing the respiratory rate. The patient
therefore breaths faster making it even difficult for him to talk normally. The temperature is
lungs is still hard. It becomes gray in appearance since the red blood cells becomes disintegrated
continuously and the fibrin suppurative exudates persist. This is attained by the reduction of
blood to the lungs and the fibrin and leukocyte consolidate in the part that is affected (Driver
2012, pp. 103-106). This is followed by the resolution of the infection whereby the pulmonary
structure is restored. The exudates that are consolidated in the lungs are digested enzymatically
and the macrophage ingest most debris which are coughed out thereafter. The lungs can then
return normal and gaseous exchange resume if complete resolution occur.
Signs and symptoms of pneumonia
The clinical manifestation of pneumonia ranges from mild to severe. This is dictated by factors
like age, health or the type of causative pathogen. The signs and symptoms of pneumonia may
include: chest pain which is felt when one coughs or breathe, coughing which may be productive
(mucus), fever and chills is also experienced and fatigue. One may also experience nausea,
vomiting and diarrhea. Shortness of breath is also usually manifested. The patient mental status
may also change and the patient become confused.
Significance of Mr. Smith’s Vital signs in relation to the presenting problem
Mr. respiratory rate is 36 breaths per minute which is high above the normal range of 12 to 20
breathes per minute in adult. This is significant in relation to his presenting condition since
pneumonia causes lung congestion thus interfering with the normal gaseous exchange. Oxygen is
therefore not supplied sufficiently to the body and as a result its demand increases. The body
therefore tries to increase the oxygen supply by increasing the respiratory rate. The patient
therefore breaths faster making it even difficult for him to talk normally. The temperature is
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
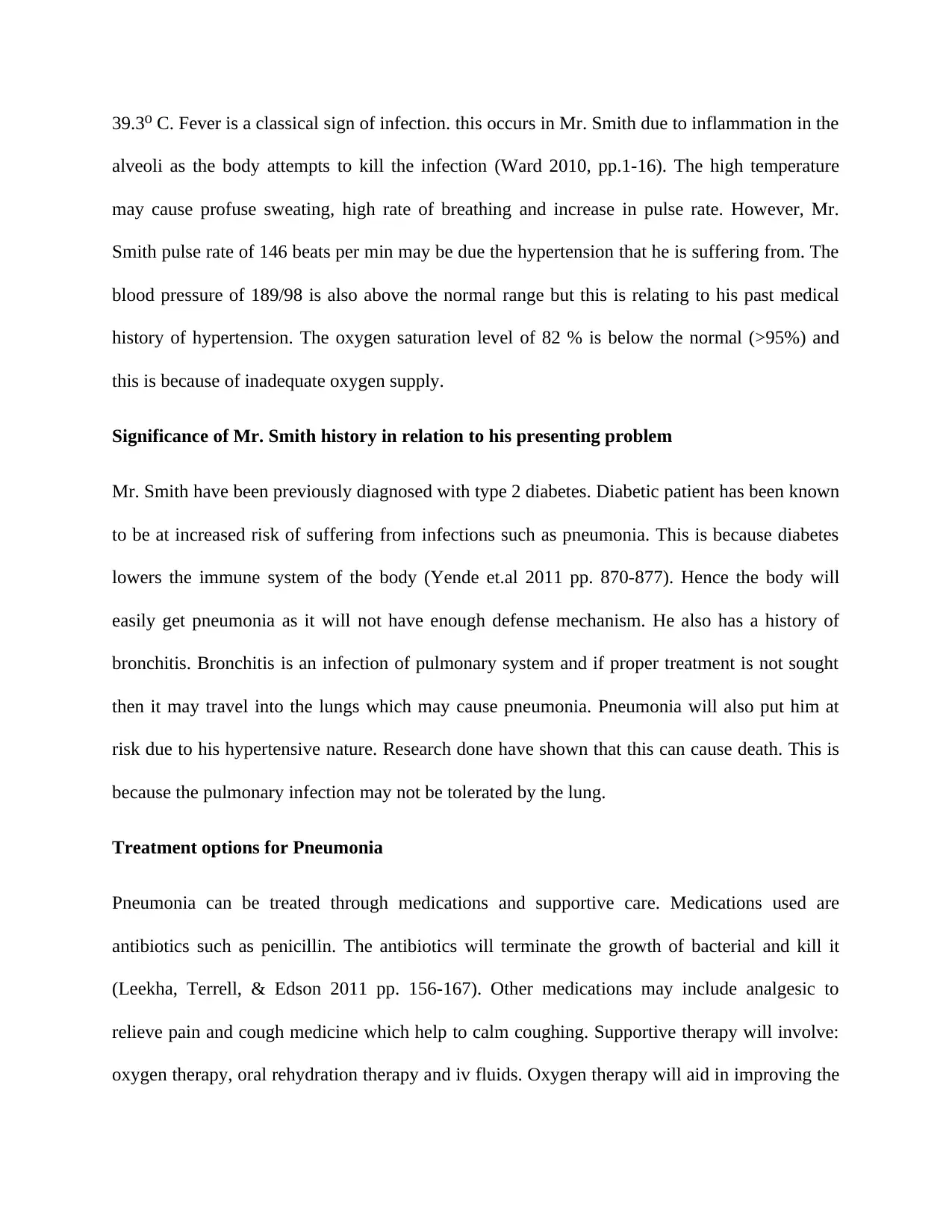
39.3 C. Fever is a classical sign of infection. this occurs in Mr. Smith due to inflammation in the⁰
alveoli as the body attempts to kill the infection (Ward 2010, pp.1-16). The high temperature
may cause profuse sweating, high rate of breathing and increase in pulse rate. However, Mr.
Smith pulse rate of 146 beats per min may be due the hypertension that he is suffering from. The
blood pressure of 189/98 is also above the normal range but this is relating to his past medical
history of hypertension. The oxygen saturation level of 82 % is below the normal (>95%) and
this is because of inadequate oxygen supply.
Significance of Mr. Smith history in relation to his presenting problem
Mr. Smith have been previously diagnosed with type 2 diabetes. Diabetic patient has been known
to be at increased risk of suffering from infections such as pneumonia. This is because diabetes
lowers the immune system of the body (Yende et.al 2011 pp. 870-877). Hence the body will
easily get pneumonia as it will not have enough defense mechanism. He also has a history of
bronchitis. Bronchitis is an infection of pulmonary system and if proper treatment is not sought
then it may travel into the lungs which may cause pneumonia. Pneumonia will also put him at
risk due to his hypertensive nature. Research done have shown that this can cause death. This is
because the pulmonary infection may not be tolerated by the lung.
Treatment options for Pneumonia
Pneumonia can be treated through medications and supportive care. Medications used are
antibiotics such as penicillin. The antibiotics will terminate the growth of bacterial and kill it
(Leekha, Terrell, & Edson 2011 pp. 156-167). Other medications may include analgesic to
relieve pain and cough medicine which help to calm coughing. Supportive therapy will involve:
oxygen therapy, oral rehydration therapy and iv fluids. Oxygen therapy will aid in improving the
alveoli as the body attempts to kill the infection (Ward 2010, pp.1-16). The high temperature
may cause profuse sweating, high rate of breathing and increase in pulse rate. However, Mr.
Smith pulse rate of 146 beats per min may be due the hypertension that he is suffering from. The
blood pressure of 189/98 is also above the normal range but this is relating to his past medical
history of hypertension. The oxygen saturation level of 82 % is below the normal (>95%) and
this is because of inadequate oxygen supply.
Significance of Mr. Smith history in relation to his presenting problem
Mr. Smith have been previously diagnosed with type 2 diabetes. Diabetic patient has been known
to be at increased risk of suffering from infections such as pneumonia. This is because diabetes
lowers the immune system of the body (Yende et.al 2011 pp. 870-877). Hence the body will
easily get pneumonia as it will not have enough defense mechanism. He also has a history of
bronchitis. Bronchitis is an infection of pulmonary system and if proper treatment is not sought
then it may travel into the lungs which may cause pneumonia. Pneumonia will also put him at
risk due to his hypertensive nature. Research done have shown that this can cause death. This is
because the pulmonary infection may not be tolerated by the lung.
Treatment options for Pneumonia
Pneumonia can be treated through medications and supportive care. Medications used are
antibiotics such as penicillin. The antibiotics will terminate the growth of bacterial and kill it
(Leekha, Terrell, & Edson 2011 pp. 156-167). Other medications may include analgesic to
relieve pain and cough medicine which help to calm coughing. Supportive therapy will involve:
oxygen therapy, oral rehydration therapy and iv fluids. Oxygen therapy will aid in improving the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
oxygen supply to the bloodstream while the oral rehydration therapy and iv fluids is given to
cover up for the lost fluid in case of vomiting and diarrhea.
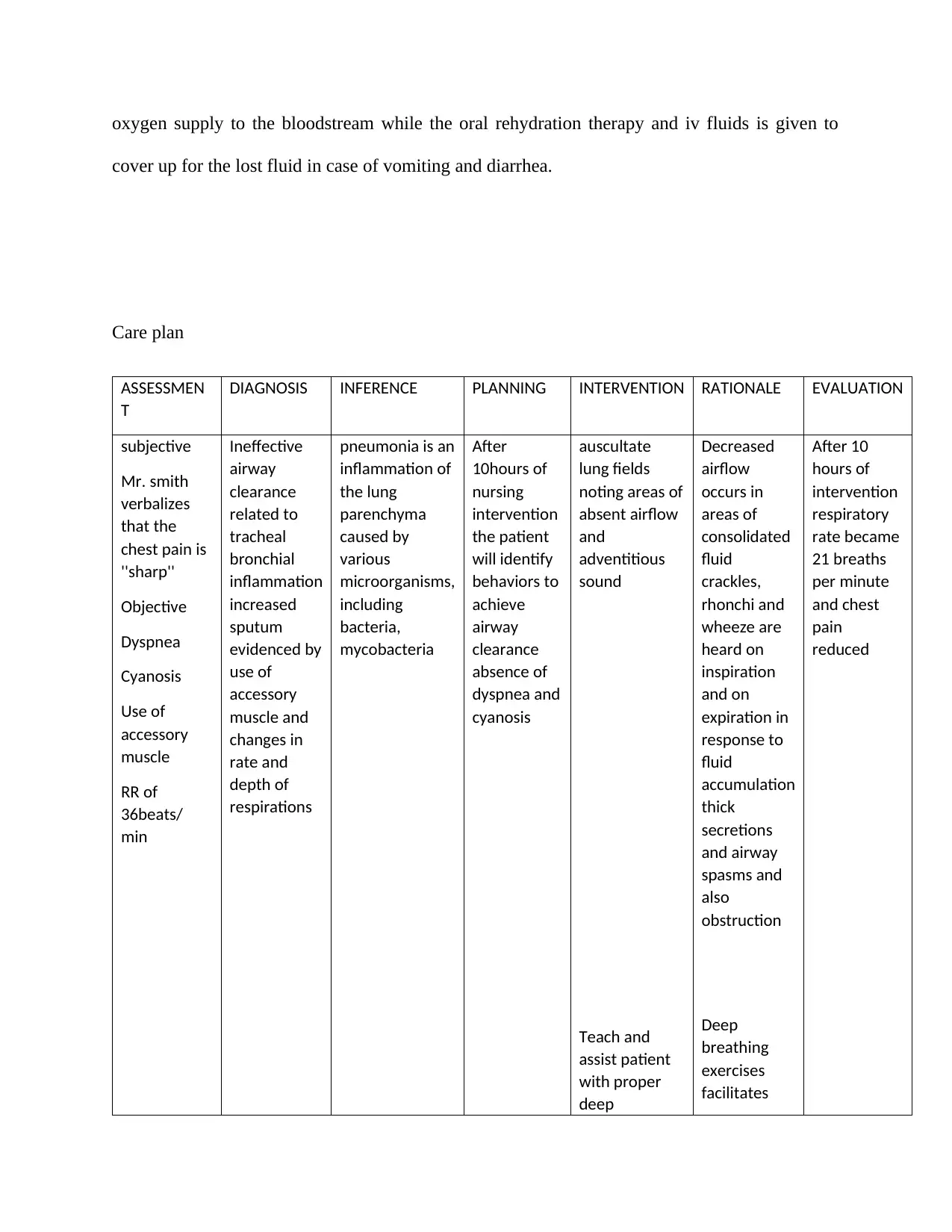
Care plan
ASSESSMEN
T
DIAGNOSIS INFERENCE PLANNING INTERVENTION RATIONALE EVALUATION
subjective
Mr. smith
verbalizes
that the
chest pain is
''sharp''
Objective
Dyspnea
Cyanosis
Use of
accessory
muscle
RR of
36beats/
min
Ineffective
airway
clearance
related to
tracheal
bronchial
inflammation
increased
sputum
evidenced by
use of
accessory
muscle and
changes in
rate and
depth of
respirations
pneumonia is an
inflammation of
the lung
parenchyma
caused by
various
microorganisms,
including
bacteria,
mycobacteria
After
10hours of
nursing
intervention
the patient
will identify
behaviors to
achieve
airway
clearance
absence of
dyspnea and
cyanosis
auscultate
lung fields
noting areas of
absent airflow
and
adventitious
sound
Teach and
assist patient
with proper
deep
Decreased
airflow
occurs in
areas of
consolidated
fluid
crackles,
rhonchi and
wheeze are
heard on
inspiration
and on
expiration in
response to
fluid
accumulation
thick
secretions
and airway
spasms and
also
obstruction
Deep
breathing
exercises
facilitates
After 10
hours of
intervention
respiratory
rate became
21 breaths
per minute
and chest
pain
reduced
cover up for the lost fluid in case of vomiting and diarrhea.
Care plan
ASSESSMEN
T
DIAGNOSIS INFERENCE PLANNING INTERVENTION RATIONALE EVALUATION
subjective
Mr. smith
verbalizes
that the
chest pain is
''sharp''
Objective
Dyspnea
Cyanosis
Use of
accessory
muscle
RR of
36beats/
min
Ineffective
airway
clearance
related to
tracheal
bronchial
inflammation
increased
sputum
evidenced by
use of
accessory
muscle and
changes in
rate and
depth of
respirations
pneumonia is an
inflammation of
the lung
parenchyma
caused by
various
microorganisms,
including
bacteria,
mycobacteria
After
10hours of
nursing
intervention
the patient
will identify
behaviors to
achieve
airway
clearance
absence of
dyspnea and
cyanosis
auscultate
lung fields
noting areas of
absent airflow
and
adventitious
sound
Teach and
assist patient
with proper
deep
Decreased
airflow
occurs in
areas of
consolidated
fluid
crackles,
rhonchi and
wheeze are
heard on
inspiration
and on
expiration in
response to
fluid
accumulation
thick
secretions
and airway
spasms and
also
obstruction
Deep
breathing
exercises
facilitates
After 10
hours of
intervention
respiratory
rate became
21 breaths
per minute
and chest
pain
reduced
breathing
exercises.
Demonstrate
proper
splinting of
chest and
effective
coughing to
him while in
upright
position .
maximum
expansion of
the lungs and
smaller
airway
coughing is a
reflex and a
natural self-
cleaning
mechanism
that assist
the cilia to
maintain
patent
airways,
splinting
reduces
chest
discomfort
and upright
position
favors
deeper and
more
forceful
effort
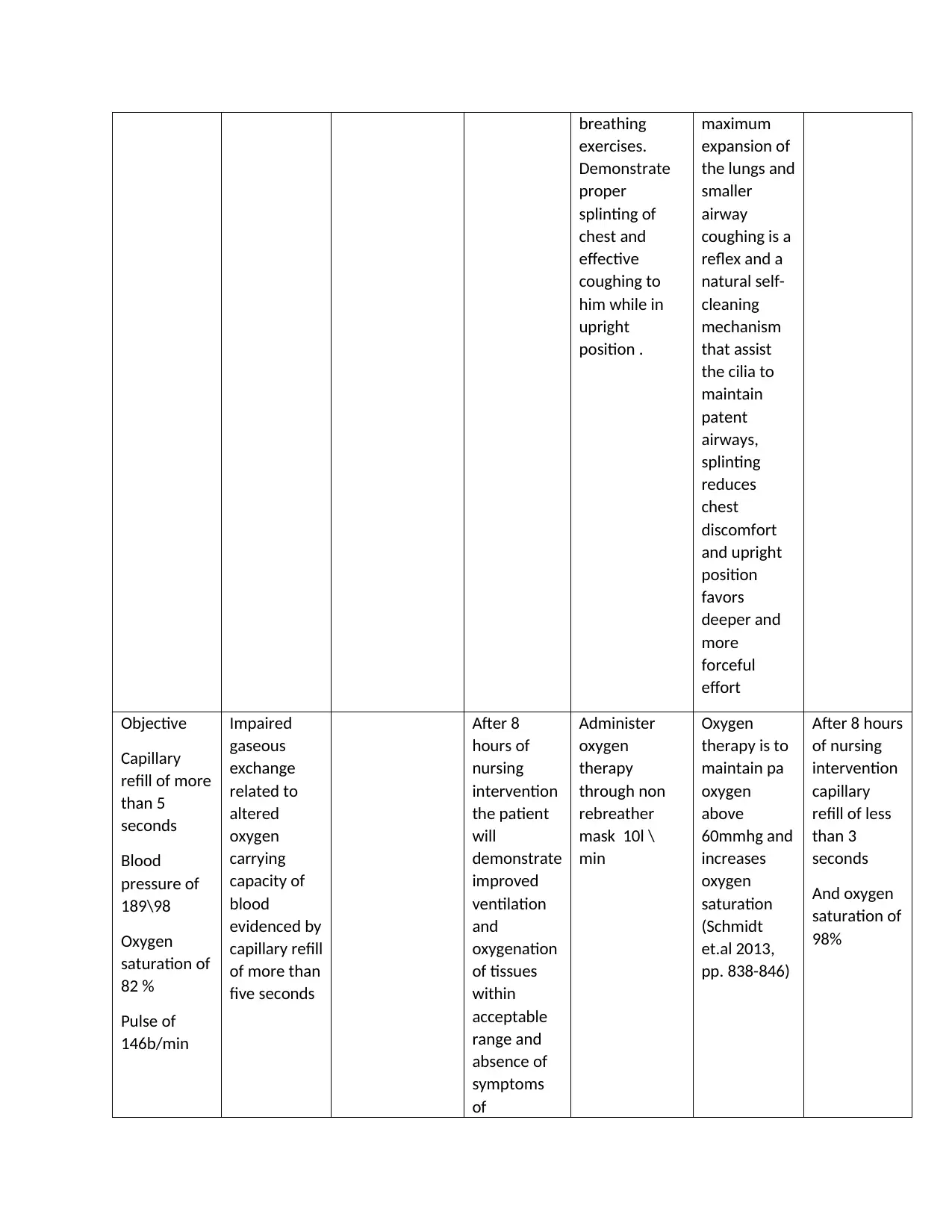
Objective
Capillary
refill of more
than 5
seconds
Blood
pressure of
189\98
Oxygen
saturation of
82 %
Pulse of
146b/min
Impaired
gaseous
exchange
related to
altered
oxygen
carrying
capacity of
blood
evidenced by
capillary refill
of more than
five seconds
After 8
hours of
nursing
intervention
the patient
will
demonstrate
improved
ventilation
and
oxygenation
of tissues
within
acceptable
range and
absence of
symptoms
of
Administer
oxygen
therapy
through non
rebreather
mask 10l \
min
Oxygen
therapy is to
maintain pa
oxygen
above
60mmhg and
increases
oxygen
saturation
(Schmidt
et.al 2013,
pp. 838-846)
After 8 hours
of nursing
intervention
capillary
refill of less
than 3
seconds
And oxygen
saturation of
98%
exercises.
Demonstrate
proper
splinting of
chest and
effective
coughing to
him while in
upright
position .
maximum
expansion of
the lungs and
smaller
airway
coughing is a
reflex and a
natural self-
cleaning
mechanism
that assist
the cilia to
maintain
patent
airways,
splinting
reduces
chest
discomfort
and upright
position
favors
deeper and
more
forceful
effort
Objective
Capillary
refill of more
than 5
seconds
Blood
pressure of
189\98
Oxygen
saturation of
82 %
Pulse of
146b/min
Impaired
gaseous
exchange
related to
altered
oxygen
carrying
capacity of
blood
evidenced by
capillary refill
of more than
five seconds
After 8
hours of
nursing
intervention
the patient
will
demonstrate
improved
ventilation
and
oxygenation
of tissues
within
acceptable
range and
absence of
symptoms
of
Administer
oxygen
therapy
through non
rebreather
mask 10l \
min
Oxygen
therapy is to
maintain pa
oxygen
above
60mmhg and
increases
oxygen
saturation
(Schmidt
et.al 2013,
pp. 838-846)
After 8 hours
of nursing
intervention
capillary
refill of less
than 3
seconds
And oxygen
saturation of
98%
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
respiratory
distress
distress
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
List of references
Driver, C. (2012). Pneumonia part 1: pathology, presentation and prevention. British Journal of
Nursing, 21(2), 103-106.
La Rosa, G., Fratini, M., Libera, S.D., Iaconelli, M. and Muscillo, M., 2013. Viral infections
acquired indoors through airborne, droplet or contact transmission. Annali dell'Istituto superiore
di sanita, 49, pp.124-132.
Leekha, S., Terrell, C. L., & Edson, R. S. (2011, February). General principles of antimicrobial
therapy. In Mayo Clinic Proceedings (Vol. 86, No. 2, pp. 156-167). Elsevier.
Schmidt, M., Tachon, G., Devilliers, C., Muller, G., Hekimian, G., Bréchot, N., Merceron, S.,
Luyt, C.E., Trouillet, J.L., Chastre, J. and Leprince, P., 2013. Blood oxygenation and
decarboxylation determinants during venovenous ECMO for respiratory failure in
adults. Intensive care medicine, 39(5), pp.838-846.
Singh, Y.D., 2012. Pathophysiology of community acquired pneumonia. Supplement to JAPI, 60,
pp.7-9.
Ward, P.A., 2010. Acute and chronic inflammation. Fundamentals of inflammation, pp.1-16.
Yende, S., van der Poll, T., Lee, M., Huang, D.T., Newman, A.B., Kong, L., Kellum, J.A.,
Harris, T.B., Bauer, D., Satterfield, S. and Angus, D.C., 2010. The influence of pre-existing
diabetes mellitus on the host immune response and outcome of pneumonia: analysis of two
multicentre cohort studies. Thorax, 65(10), pp.870-877.
Driver, C. (2012). Pneumonia part 1: pathology, presentation and prevention. British Journal of
Nursing, 21(2), 103-106.
La Rosa, G., Fratini, M., Libera, S.D., Iaconelli, M. and Muscillo, M., 2013. Viral infections
acquired indoors through airborne, droplet or contact transmission. Annali dell'Istituto superiore
di sanita, 49, pp.124-132.
Leekha, S., Terrell, C. L., & Edson, R. S. (2011, February). General principles of antimicrobial
therapy. In Mayo Clinic Proceedings (Vol. 86, No. 2, pp. 156-167). Elsevier.
Schmidt, M., Tachon, G., Devilliers, C., Muller, G., Hekimian, G., Bréchot, N., Merceron, S.,
Luyt, C.E., Trouillet, J.L., Chastre, J. and Leprince, P., 2013. Blood oxygenation and
decarboxylation determinants during venovenous ECMO for respiratory failure in
adults. Intensive care medicine, 39(5), pp.838-846.
Singh, Y.D., 2012. Pathophysiology of community acquired pneumonia. Supplement to JAPI, 60,
pp.7-9.
Ward, P.A., 2010. Acute and chronic inflammation. Fundamentals of inflammation, pp.1-16.
Yende, S., van der Poll, T., Lee, M., Huang, D.T., Newman, A.B., Kong, L., Kellum, J.A.,
Harris, T.B., Bauer, D., Satterfield, S. and Angus, D.C., 2010. The influence of pre-existing
diabetes mellitus on the host immune response and outcome of pneumonia: analysis of two
multicentre cohort studies. Thorax, 65(10), pp.870-877.
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




