Detection of Primary Hepatic Malignancy in Liver Transplant Patient: Comparison of CT, MR Imaging, Ultrasound and PET
Added on 2022-10-01
1 Pages2156 Words132 Views
Study Developing Detection of Primary Hepatic Malignancy in Liver Transplant
Patient: Prospective Comparison of CT, MR Imaging, Ultrasound and PET
Name of Student:
Name of the University:
Author’s Note:
Ayuso, C., Rimola, J., Vilana, R., Burrel, M., Darnell, A., García-Criado, Á., Bianchi, L., Belmonte, E., Caparroz,
C., Barrufet, M. and Bruix, J., 2018. Diagnosis and staging of hepatocellular carcinoma (HCC): current
guidelines. European journal of radiology, 101, pp.72-81.
Castilla-Lièvre, M.A., Franco, D., Gervais, P., Kuhnast, B., Agostini, H., Marthey, L., Désarnaud, S. and Helal,
B.O., 2016. Diagnostic value of combining 11 C-choline and 18 F-FDG PET/CT in hepatocellular
carcinoma. European journal of nuclear medicine and molecular imaging, 43(5), pp.852-859.
Chalaye, J., Costentin, C.E., Luciani, A., Amaddeo, G., Ganne-Carrié, N., Baranes, L., Allaire, M., Calderaro, J.,
Azoulay, D., Nahon, P. and Seror, O., 2018. Positron emission tomography/computed tomography with 18F-
fluorocholine improve tumor staging and treatment allocation in patients with hepatocellular carcinoma. Journal
of hepatology, 69(2), pp.336-344.
Chou, R., Cuevas, C., Fu, R., Devine, B., Wasson, N., Ginsburg, A., Zakher, B., Pappas, M., Graham, E. and
Sullivan, S., 2014. Imaging techniques for the diagnosis and staging of hepatocellular carcinoma.
Galle, P.R., Forner, A., Llovet, J.M., Mazzaferro, V., Piscaglia, F., Raoul, J.L., Schirmacher, P. and Vilgrain, V.,
2018. EASL clinical practice guidelines: management of hepatocellular carcinoma. Journal of hepatology, 69(1),
pp.182-236.
Geissler, E.K., Schnitzbauer, A.A., Zülke, C., Lamby, P.E., Proneth, A., Duvoux, C., Burra, P., Jauch, K.W.,
Rentsch, M., Ganten, T.M. and Schmidt, J., 2016. Sirolimus use in liver transplant recipients with hepatocellular
carcinoma: a randomized, multicenter, open-label phase 3 trial. Transplantation, 100(1), p.116.
Halazun, K.J., Najjar, M., Abdelmessih, R.M., Samstein, B., Griesemer, A.D., Guarrera, J.V., Kato, T., Verna,
E.C., Emond, J.C. and Brown, R.S., 2017. Recurrence after liver transplantation for hepatocellular
carcinoma. Annals of surgery, 265(3), pp.557-564.
Jiang, H.Y., Chen, J., Xia, C.C., Cao, L.K., Duan, T. and Song, B., 2018. Noninvasive imaging of hepatocellular
carcinoma: From diagnosis to prognosis. World journal of gastroenterology, 24(22), p.2348.
Johnson, P.J., Berhane, S., Kagebayashi, C., Satomura, S., Teng, M., Reeves, H.L., O'Beirne, J., Fox, R.,
Skowronska, A., Palmer, D. and Yeo, W., 2015. Assessment of liver function in patients with hepatocellular
carcinoma: a new evidence-based approach—the ALBI grade. Journal of Clinical Oncology, 33(6), p.550.
Kawai, T., Yasuchika, K., Seo, S., Higashi, T., Ishii, T., Miyauchi, Y., Kojima, H., Yamaoka, R., Katayama, H.,
Yoshitoshi, E.Y. and Ogiso, S., 2017. Identification of Keratin 19–Positive Cancer Stem Cells Associating Human
Hepatocellular Carcinoma Using 18F-Fluorodeoxyglucose Positron Emission Tomography. Clinical Cancer
Research, 23(6), pp.1450-1460.
Kojima, S., Watanabe, F., Ueki, H., Konno, Y. and Tsubota, Y., Hitachi Healthcare Manufacturing Ltd, 2016. X-
ray CT device. U.S. Patent 9,380,987.
Kurokawa, S. and Tsubota, Y., Hitachi Ltd, 2019. X-ray CT device and imaging method for X-ray CT images.
U.S. Patent Application 10/219,762.
Lee, Y.J., Lee, J.M., Lee, J.S., Lee, H.Y., Park, B.H., Kim, Y.H., Han, J.K. and Choi, B.I., 2015. Hepatocellular
carcinoma: diagnostic performance of multidetector CT and MR imaging—a systematic review and meta-
analysis. Radiology, 275(1), pp.97-109.
Makuuchi, M., Kokudo, N., Arii, S., Futagawa, S., Kaneko, S., Kawasaki, S., Matsuyama, Y., Okazaki, M.,
Okita, K., Omata, M. and Saida, Y., 2008. Development of evidence‐based clinical guidelines for the diagnosis
and treatment of hepatocellular carcinoma in Japan. Hepatology Research, 38(1), pp.37-51.
Mittal, S., El-Serag, H.B., Sada, Y.H., Kanwal, F., Duan, Z., Temple, S., May, S.B., Kramer, J.R., Richardson,
P.A. and Davila, J.A., 2016. Hepatocellular carcinoma in the absence of cirrhosis in United States veterans is
associated with nonalcoholic fatty liver disease. Clinical Gastroenterology and Hepatology, 14(1), pp.124-131.
Mittal, S., Sada, Y.H., El-Serag, H.B., Kanwal, F., Duan, Z., Temple, S., May, S.B., Kramer, J.R., Richardson,
P.A. and Davila, J.A., 2015. Temporal trends of nonalcoholic fatty liver disease–related hepatocellular carcinoma
in the veteran affairs population. Clinical Gastroenterology and Hepatology, 13(3), pp.594-601.
Mulazzani, L., Sansone, V., Giordano, L., Di Bonaventura, C., Giamperoli, A., Cimino, A. and Piscaglia, F.,
2019, April. Clinical validation of the role of contrast-enhanced ultrasound in the EASL guidelines for the
diagnosis of hepatocellular carcinoma. In JOURNAL OF HEPATOLOGY (Vol. 70, pp. E842-E843). PO BOX 211,
1000 AE AMSTERDAM, NETHERLANDS: ELSEVIER SCIENCE BV.
Piscaglia, F., Svegliati‐Baroni, G., Barchetti, A., Pecorelli, A., Marinelli, S., Tiribelli, C., Bellentani, S. and HCC‐
NAFLD Italian Study Group, 2016. Clinical patterns of hepatocellular carcinoma in nonalcoholic fatty liver
disease: A multicenter prospective study. Hepatology, 63(3), pp.827-838.
Potretzke, T.A., Tan, B.R., Doyle, M.B., Brunt, E.M., Heiken, J.P. and Fowler, K.J., 2016. Imaging features of
biphenotypic primary liver carcinoma (hepatocholangiocarcinoma) and the potential to mimic hepatocellular
carcinoma: LI-RADS analysis of CT and MRI features in 61 cases. American Journal of Roentgenology, 207(1),
pp.25-31.
Preshlock, S., Tredwell, M. and Gouverneur, V., 2016. 18F-Labeling of arenes and heteroarenes for applications
in positron emission tomography. Chemical reviews, 116(2), pp.719-766.
Roberts, L.R., Sirlin, C.B., Zaiem, F., Almasri, J., Prokop, L.J., Heimbach, J.K., Murad, M.H. and Mohammed,
K., 2018. Imaging for the diagnosis of hepatocellular carcinoma: A systematic review and meta‐
analysis. Hepatology, 67(1), pp.401-421.
.
Abstract
Introduction
Literature Review Methodology Conclusion
References
• Hepatocellular Carcinoma is the fifth most common type
of cancer prevalent worldwide (Chou et al., 2014).
• The advancement of the disease is called
hepatocarcinogenesis that is a complex multiple step
process at the histologic and the cellular levels. These
steps are exposed by the non-imaging modalities.
• To ensure effective curative therapy it is important to
execute the diagnosis effectively. Hence, imaging
techniques play a vital role in detection of the disease
(Jiang et al., 2018).
• This article reviews the screening modalities for HCC.
• This article deals with the non-invasive imaging
modalities which includes Computed Tomography,
Magnetic resonance imaging, Ultrasonography and also
Positron Emission Tomography.
• The aim of this paper is to identify and analyze the
detection strategies that play an important role in the
curative therapy for the detected disease (Jiang et al.,
2018).
• The objective of this study is to analyze as well as
compare the diagnostic performances of the imaging
techniques. It utilizes the effectiveness of the imaging
modalities in order to detect the hepatocellular carcinoma
in the individual who has opted for liver transplant
(Makuuchi et al., 2008).
Computed Tomography (CT)
• This technique produces cross sectional
images exploiting X ray.
• It is an imaging modality that is well
tolerated by the patient.
• An advancement in the technique is the
computed tomography arteriography. It
improves the accuracy of the imaging
but it is a invasive technique and it is
expensive (Chou et al., 2014).
Clinical presentation of Hepatocellular carcinoma
HCC is considered to grow silently without much evident
symptoms making the discovery of the disease challenging.
The detection of the tumors in the patients are majorly by
the routine surveillance.
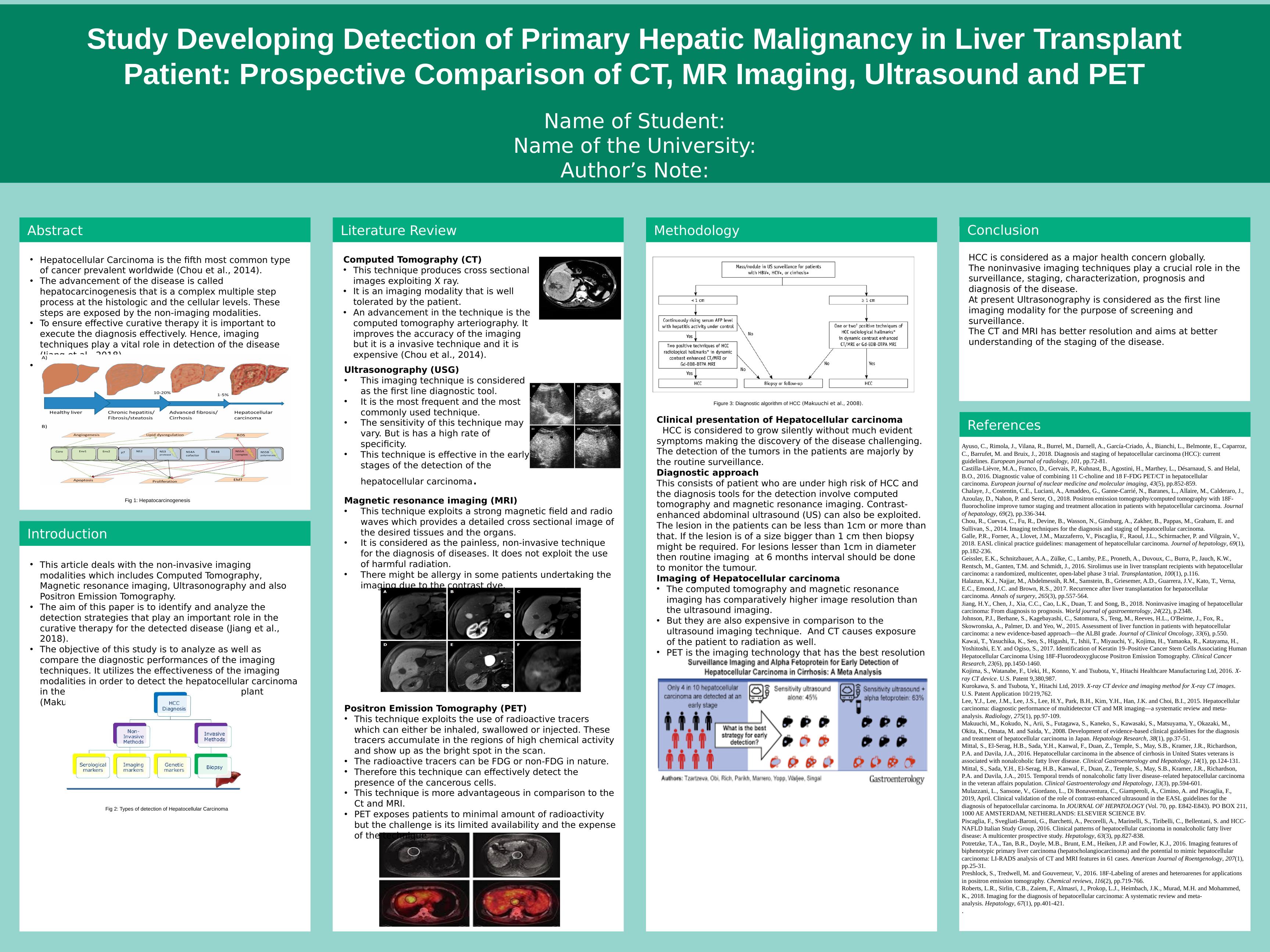
Diagnostic approach
This consists of patient who are under high risk of HCC and
the diagnosis tools for the detection involve computed
tomography and magnetic resonance imaging. Contrast-
enhanced abdominal ultrasound (US) can also be exploited.
The lesion in the patients can be less than 1cm or more than
that. If the lesion is of a size bigger than 1 cm then biopsy
might be required. For lesions lesser than 1cm in diameter
then routine imaging at 6 months interval should be done
to monitor the tumour.
Imaging of Hepatocellular carcinoma
• The computed tomography and magnetic resonance
imaging has comparatively higher image resolution than
the ultrasound imaging.
• But they are also expensive in comparison to the
ultrasound imaging technique. And CT causes exposure
of the patient to radiation as well.
• PET is the imaging technology that has the best resolution
but the challenge is its limited availability and the cost
incurred for the process (Makuuchi et al., 2008).
HCC is considered as a major health concern globally.
The noninvasive imaging techniques play a crucial role in the
surveillance, staging, characterization, prognosis and
diagnosis of the disease.
At present Ultrasonography is considered as the first line
imaging modality for the purpose of screening and
surveillance.
The CT and MRI has better resolution and aims at better
understanding of the staging of the disease.
Fig 1: Hepatocarcinogenesis
Fig 2: Types of detection of Hepatocellular Carcinoma
Ultrasonography (USG)
• This imaging technique is considered
as the first line diagnostic tool.
• It is the most frequent and the most
commonly used technique.
• The sensitivity of this technique may
vary. But is has a high rate of
specificity.
• This technique is effective in the early
stages of the detection of the
hepatocellular carcinoma.
Magnetic resonance imaging (MRI)
• This technique exploits a strong magnetic field and radio
waves which provides a detailed cross sectional image of
the desired tissues and the organs.
• It is considered as the painless, non-invasive technique
for the diagnosis of diseases. It does not exploit the use
of harmful radiation.
• There might be allergy in some patients undertaking the
imaging due to the contrast dye.
Positron Emission Tomography (PET)
• This technique exploits the use of radioactive tracers
which can either be inhaled, swallowed or injected. These
tracers accumulate in the regions of high chemical activity
and show up as the bright spot in the scan.
• The radioactive tracers can be FDG or non-FDG in nature.
• Therefore this technique can effectively detect the
presence of the cancerous cells.
• This technique is more advantageous in comparison to the
Ct and MRI.
• PET exposes patients to minimal amount of radioactivity
but the challenge is its limited availability and the expense
of the technique.
Figure 3: Diagnostic algorithm of HCC (Makuuchi et al., 2008).
Patient: Prospective Comparison of CT, MR Imaging, Ultrasound and PET
Name of Student:
Name of the University:
Author’s Note:
Ayuso, C., Rimola, J., Vilana, R., Burrel, M., Darnell, A., García-Criado, Á., Bianchi, L., Belmonte, E., Caparroz,
C., Barrufet, M. and Bruix, J., 2018. Diagnosis and staging of hepatocellular carcinoma (HCC): current
guidelines. European journal of radiology, 101, pp.72-81.
Castilla-Lièvre, M.A., Franco, D., Gervais, P., Kuhnast, B., Agostini, H., Marthey, L., Désarnaud, S. and Helal,
B.O., 2016. Diagnostic value of combining 11 C-choline and 18 F-FDG PET/CT in hepatocellular
carcinoma. European journal of nuclear medicine and molecular imaging, 43(5), pp.852-859.
Chalaye, J., Costentin, C.E., Luciani, A., Amaddeo, G., Ganne-Carrié, N., Baranes, L., Allaire, M., Calderaro, J.,
Azoulay, D., Nahon, P. and Seror, O., 2018. Positron emission tomography/computed tomography with 18F-
fluorocholine improve tumor staging and treatment allocation in patients with hepatocellular carcinoma. Journal
of hepatology, 69(2), pp.336-344.
Chou, R., Cuevas, C., Fu, R., Devine, B., Wasson, N., Ginsburg, A., Zakher, B., Pappas, M., Graham, E. and
Sullivan, S., 2014. Imaging techniques for the diagnosis and staging of hepatocellular carcinoma.
Galle, P.R., Forner, A., Llovet, J.M., Mazzaferro, V., Piscaglia, F., Raoul, J.L., Schirmacher, P. and Vilgrain, V.,
2018. EASL clinical practice guidelines: management of hepatocellular carcinoma. Journal of hepatology, 69(1),
pp.182-236.
Geissler, E.K., Schnitzbauer, A.A., Zülke, C., Lamby, P.E., Proneth, A., Duvoux, C., Burra, P., Jauch, K.W.,
Rentsch, M., Ganten, T.M. and Schmidt, J., 2016. Sirolimus use in liver transplant recipients with hepatocellular
carcinoma: a randomized, multicenter, open-label phase 3 trial. Transplantation, 100(1), p.116.
Halazun, K.J., Najjar, M., Abdelmessih, R.M., Samstein, B., Griesemer, A.D., Guarrera, J.V., Kato, T., Verna,
E.C., Emond, J.C. and Brown, R.S., 2017. Recurrence after liver transplantation for hepatocellular
carcinoma. Annals of surgery, 265(3), pp.557-564.
Jiang, H.Y., Chen, J., Xia, C.C., Cao, L.K., Duan, T. and Song, B., 2018. Noninvasive imaging of hepatocellular
carcinoma: From diagnosis to prognosis. World journal of gastroenterology, 24(22), p.2348.
Johnson, P.J., Berhane, S., Kagebayashi, C., Satomura, S., Teng, M., Reeves, H.L., O'Beirne, J., Fox, R.,
Skowronska, A., Palmer, D. and Yeo, W., 2015. Assessment of liver function in patients with hepatocellular
carcinoma: a new evidence-based approach—the ALBI grade. Journal of Clinical Oncology, 33(6), p.550.
Kawai, T., Yasuchika, K., Seo, S., Higashi, T., Ishii, T., Miyauchi, Y., Kojima, H., Yamaoka, R., Katayama, H.,
Yoshitoshi, E.Y. and Ogiso, S., 2017. Identification of Keratin 19–Positive Cancer Stem Cells Associating Human
Hepatocellular Carcinoma Using 18F-Fluorodeoxyglucose Positron Emission Tomography. Clinical Cancer
Research, 23(6), pp.1450-1460.
Kojima, S., Watanabe, F., Ueki, H., Konno, Y. and Tsubota, Y., Hitachi Healthcare Manufacturing Ltd, 2016. X-
ray CT device. U.S. Patent 9,380,987.
Kurokawa, S. and Tsubota, Y., Hitachi Ltd, 2019. X-ray CT device and imaging method for X-ray CT images.
U.S. Patent Application 10/219,762.
Lee, Y.J., Lee, J.M., Lee, J.S., Lee, H.Y., Park, B.H., Kim, Y.H., Han, J.K. and Choi, B.I., 2015. Hepatocellular
carcinoma: diagnostic performance of multidetector CT and MR imaging—a systematic review and meta-
analysis. Radiology, 275(1), pp.97-109.
Makuuchi, M., Kokudo, N., Arii, S., Futagawa, S., Kaneko, S., Kawasaki, S., Matsuyama, Y., Okazaki, M.,
Okita, K., Omata, M. and Saida, Y., 2008. Development of evidence‐based clinical guidelines for the diagnosis
and treatment of hepatocellular carcinoma in Japan. Hepatology Research, 38(1), pp.37-51.
Mittal, S., El-Serag, H.B., Sada, Y.H., Kanwal, F., Duan, Z., Temple, S., May, S.B., Kramer, J.R., Richardson,
P.A. and Davila, J.A., 2016. Hepatocellular carcinoma in the absence of cirrhosis in United States veterans is
associated with nonalcoholic fatty liver disease. Clinical Gastroenterology and Hepatology, 14(1), pp.124-131.
Mittal, S., Sada, Y.H., El-Serag, H.B., Kanwal, F., Duan, Z., Temple, S., May, S.B., Kramer, J.R., Richardson,
P.A. and Davila, J.A., 2015. Temporal trends of nonalcoholic fatty liver disease–related hepatocellular carcinoma
in the veteran affairs population. Clinical Gastroenterology and Hepatology, 13(3), pp.594-601.
Mulazzani, L., Sansone, V., Giordano, L., Di Bonaventura, C., Giamperoli, A., Cimino, A. and Piscaglia, F.,
2019, April. Clinical validation of the role of contrast-enhanced ultrasound in the EASL guidelines for the
diagnosis of hepatocellular carcinoma. In JOURNAL OF HEPATOLOGY (Vol. 70, pp. E842-E843). PO BOX 211,
1000 AE AMSTERDAM, NETHERLANDS: ELSEVIER SCIENCE BV.
Piscaglia, F., Svegliati‐Baroni, G., Barchetti, A., Pecorelli, A., Marinelli, S., Tiribelli, C., Bellentani, S. and HCC‐
NAFLD Italian Study Group, 2016. Clinical patterns of hepatocellular carcinoma in nonalcoholic fatty liver
disease: A multicenter prospective study. Hepatology, 63(3), pp.827-838.
Potretzke, T.A., Tan, B.R., Doyle, M.B., Brunt, E.M., Heiken, J.P. and Fowler, K.J., 2016. Imaging features of
biphenotypic primary liver carcinoma (hepatocholangiocarcinoma) and the potential to mimic hepatocellular
carcinoma: LI-RADS analysis of CT and MRI features in 61 cases. American Journal of Roentgenology, 207(1),
pp.25-31.
Preshlock, S., Tredwell, M. and Gouverneur, V., 2016. 18F-Labeling of arenes and heteroarenes for applications
in positron emission tomography. Chemical reviews, 116(2), pp.719-766.
Roberts, L.R., Sirlin, C.B., Zaiem, F., Almasri, J., Prokop, L.J., Heimbach, J.K., Murad, M.H. and Mohammed,
K., 2018. Imaging for the diagnosis of hepatocellular carcinoma: A systematic review and meta‐
analysis. Hepatology, 67(1), pp.401-421.
.
Abstract
Introduction
Literature Review Methodology Conclusion
References
• Hepatocellular Carcinoma is the fifth most common type
of cancer prevalent worldwide (Chou et al., 2014).
• The advancement of the disease is called
hepatocarcinogenesis that is a complex multiple step
process at the histologic and the cellular levels. These
steps are exposed by the non-imaging modalities.
• To ensure effective curative therapy it is important to
execute the diagnosis effectively. Hence, imaging
techniques play a vital role in detection of the disease
(Jiang et al., 2018).
• This article reviews the screening modalities for HCC.
• This article deals with the non-invasive imaging
modalities which includes Computed Tomography,
Magnetic resonance imaging, Ultrasonography and also
Positron Emission Tomography.
• The aim of this paper is to identify and analyze the
detection strategies that play an important role in the
curative therapy for the detected disease (Jiang et al.,
2018).
• The objective of this study is to analyze as well as
compare the diagnostic performances of the imaging
techniques. It utilizes the effectiveness of the imaging
modalities in order to detect the hepatocellular carcinoma
in the individual who has opted for liver transplant
(Makuuchi et al., 2008).
Computed Tomography (CT)
• This technique produces cross sectional
images exploiting X ray.
• It is an imaging modality that is well
tolerated by the patient.
• An advancement in the technique is the
computed tomography arteriography. It
improves the accuracy of the imaging
but it is a invasive technique and it is
expensive (Chou et al., 2014).
Clinical presentation of Hepatocellular carcinoma
HCC is considered to grow silently without much evident
symptoms making the discovery of the disease challenging.
The detection of the tumors in the patients are majorly by
the routine surveillance.
Diagnostic approach
This consists of patient who are under high risk of HCC and
the diagnosis tools for the detection involve computed
tomography and magnetic resonance imaging. Contrast-
enhanced abdominal ultrasound (US) can also be exploited.
The lesion in the patients can be less than 1cm or more than
that. If the lesion is of a size bigger than 1 cm then biopsy
might be required. For lesions lesser than 1cm in diameter
then routine imaging at 6 months interval should be done
to monitor the tumour.
Imaging of Hepatocellular carcinoma
• The computed tomography and magnetic resonance
imaging has comparatively higher image resolution than
the ultrasound imaging.
• But they are also expensive in comparison to the
ultrasound imaging technique. And CT causes exposure
of the patient to radiation as well.
• PET is the imaging technology that has the best resolution
but the challenge is its limited availability and the cost
incurred for the process (Makuuchi et al., 2008).
HCC is considered as a major health concern globally.
The noninvasive imaging techniques play a crucial role in the
surveillance, staging, characterization, prognosis and
diagnosis of the disease.
At present Ultrasonography is considered as the first line
imaging modality for the purpose of screening and
surveillance.
The CT and MRI has better resolution and aims at better
understanding of the staging of the disease.
Fig 1: Hepatocarcinogenesis
Fig 2: Types of detection of Hepatocellular Carcinoma
Ultrasonography (USG)
• This imaging technique is considered
as the first line diagnostic tool.
• It is the most frequent and the most
commonly used technique.
• The sensitivity of this technique may
vary. But is has a high rate of
specificity.
• This technique is effective in the early
stages of the detection of the
hepatocellular carcinoma.
Magnetic resonance imaging (MRI)
• This technique exploits a strong magnetic field and radio
waves which provides a detailed cross sectional image of
the desired tissues and the organs.
• It is considered as the painless, non-invasive technique
for the diagnosis of diseases. It does not exploit the use
of harmful radiation.
• There might be allergy in some patients undertaking the
imaging due to the contrast dye.
Positron Emission Tomography (PET)
• This technique exploits the use of radioactive tracers
which can either be inhaled, swallowed or injected. These
tracers accumulate in the regions of high chemical activity
and show up as the bright spot in the scan.
• The radioactive tracers can be FDG or non-FDG in nature.
• Therefore this technique can effectively detect the
presence of the cancerous cells.
• This technique is more advantageous in comparison to the
Ct and MRI.
• PET exposes patients to minimal amount of radioactivity
but the challenge is its limited availability and the expense
of the technique.
Figure 3: Diagnostic algorithm of HCC (Makuuchi et al., 2008).
End of preview
Want to access all the pages? Upload your documents or become a member.
Related Documents
Hepatocellular Carcinoma (HCC): Case History, Pathophysiology, Patient Care, Examination and Technique, Findings and Outcomelg...
|1
|1085
|72
Detection of Primary Hepatic Malignancylg...
|18
|3585
|375
Liver Fibrosis: Biomarkers and Diagnosislg...
|15
|1120
|322
Alpha-Fetoprotein Tumor Marker: Uses, Abnormal Levels, and Diagnosislg...
|4
|625
|233
Accuracy of Non Contrast Spiral Computerized Tomographylg...
|6
|2500
|367
(solved) Nursing Assignment - PDFlg...
|3
|368
|45
