David Game College: Unit 19 Reflective Essay and Action Plan, HNC/D
VerifiedAdded on 2022/11/19
|14
|3954
|494
Report
AI Summary
This report, submitted by a student, presents a reflective essay and action plan focused on person-centred care within a healthcare setting. The essay details a specific incident where a new staff member's actions led to a breach of patient dignity, prompting the author to reflect on their role as a senior carer and the importance of effective staff induction. The author explores the application of both medical and social models of care, analyzes relevant legislation such as the Health and Social Care Act 2008, and evaluates the challenges of implementing person-centred practice. The action plan outlines short, medium, and long-term goals for improving patient care, focusing on respect, patient autonomy, successful employee induction, and enhanced health outcomes, including strategies to increase patient satisfaction and ensure adherence to person-centred care principles. The report emphasizes the need for compassionate care, strong communication, and the recognition of each patient's unique needs and values to foster positive patient experiences and uphold their dignity.

Running head: TASK 2
Task 2: Reflective essay and individual action plan
Name of the Student
Name of the University
Author Note
Task 2: Reflective essay and individual action plan
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1TASK 2
Part 1- Reflective essay
Description- I have been working as a senior carer at the Nightingale hospital in
London for two years. As a senior carer, I was supposed to provide emotional and physical
support to the patients, besides exercising supervision on teams that comprised of care
assistants. While working at the hospital, I had been entitled with the duty of leading,
developing and coordinating a team that comprised of care workers, with the aim of
delivering excellent standards of care and respect. In addition, other roles and responsibilities
comprised of assisting the patients with their activities of daily living, providing necessary
documents and PPE to subordinate carers, ensuring delivery of service in accordance to
pertinent regulations and reporting issues to the management (McCormack, Manley and
Titchen 2013). During my practice, I encountered a situation where I had been assigned the
responsibility of inducting a new staff in my team, who was supposed to follow me.
However, the induction proved difficult since the staff was not able to gain a clear conception
about the job role and also demonstrated less involvement with the patients. On one such
instance, I found that despite shadowing me, the new staff violated the dignity of two patients
who had been admitted for treatment of psychiatric disorders. The staff interacted with them
rudely and also demonstrated discrimination and contempt towards the patients, owing to
their mental disorder, thus resulting in a breach of person-centred care. On being asked to
supervise the two patients, the new staff made jokes about people suffering from mental
disorder and also engaged in name-calling, thus enraging the patients, as well as their family
members. On knowing about the incident, I immediately reported it to an authority from the
hospital management.
Feelings- On knowing about the event, I became anxious and troubled since the
situation appeared challenging and new and my capacity to effectively communicate with the
patients was not facilitated by the fact that I was incapable to contemplate of novel way to
Part 1- Reflective essay
Description- I have been working as a senior carer at the Nightingale hospital in
London for two years. As a senior carer, I was supposed to provide emotional and physical
support to the patients, besides exercising supervision on teams that comprised of care
assistants. While working at the hospital, I had been entitled with the duty of leading,
developing and coordinating a team that comprised of care workers, with the aim of
delivering excellent standards of care and respect. In addition, other roles and responsibilities
comprised of assisting the patients with their activities of daily living, providing necessary
documents and PPE to subordinate carers, ensuring delivery of service in accordance to
pertinent regulations and reporting issues to the management (McCormack, Manley and
Titchen 2013). During my practice, I encountered a situation where I had been assigned the
responsibility of inducting a new staff in my team, who was supposed to follow me.
However, the induction proved difficult since the staff was not able to gain a clear conception
about the job role and also demonstrated less involvement with the patients. On one such
instance, I found that despite shadowing me, the new staff violated the dignity of two patients
who had been admitted for treatment of psychiatric disorders. The staff interacted with them
rudely and also demonstrated discrimination and contempt towards the patients, owing to
their mental disorder, thus resulting in a breach of person-centred care. On being asked to
supervise the two patients, the new staff made jokes about people suffering from mental
disorder and also engaged in name-calling, thus enraging the patients, as well as their family
members. On knowing about the incident, I immediately reported it to an authority from the
hospital management.
Feelings- On knowing about the event, I became anxious and troubled since the
situation appeared challenging and new and my capacity to effectively communicate with the
patients was not facilitated by the fact that I was incapable to contemplate of novel way to
2TASK 2
help the new staff understand the principles of person-centred care. In addition, on knowing
that the new staff had misbehaved with the two patients, their family members kept looking at
me for assurance that we will take all possible efforts for upholding patient dignity. I felt
extremely saddened at the turn of events and also realised my incompetence in conducting the
staff induction, which might have acted as a barrier in the delivery of person-centred care by
the staff. No previous encounter, in my experience till date had equipped me for such a
circumstance, where we as nursing professionals are expected to support the patient, while
maintaining a safe and secured care environment. It was then that I called the circumstance as
a confrontation. The family members of the two patients confronted the new staff, and I was
the silent witness to the incident. When the discussion proceeded I made supportive noise and
also tried to read the reactions of the patients, and their family members, in response to the
behaviour that had been manifested by the staff. I concluded that there was failure on my part
in conducting a successful induction of the staff and I must have played a role model, to help
the staff understand the core values of person-centred care.
Evaluation- I considered the incident to be extremely challenging since my feelings of
anxiety and apprehension were closely interrelated to my lack of proficiency in helping the
staff gain a sound understanding of how different social and medical models are applicable to
the delivery of person-centred practice. I regret that I did not act accordingly to challenge the
discriminatory attitude that had been meted out towards the patients. From this experience, I
was able to realise that while a new staff members begins working for a healthcare
organisation, it is extremely essential to help them become efficient and productive, as
rapidly as possible. Research evidences elaborate on the fact that providing new employees
with a comprehensive and clear introduction about the job role and duties result in
substantially enhanced long-term retention of staff (Matthews, Duck and Bartle 2017). The
conventional medical model that is related to the delivery of health services generally follows
help the new staff understand the principles of person-centred care. In addition, on knowing
that the new staff had misbehaved with the two patients, their family members kept looking at
me for assurance that we will take all possible efforts for upholding patient dignity. I felt
extremely saddened at the turn of events and also realised my incompetence in conducting the
staff induction, which might have acted as a barrier in the delivery of person-centred care by
the staff. No previous encounter, in my experience till date had equipped me for such a
circumstance, where we as nursing professionals are expected to support the patient, while
maintaining a safe and secured care environment. It was then that I called the circumstance as
a confrontation. The family members of the two patients confronted the new staff, and I was
the silent witness to the incident. When the discussion proceeded I made supportive noise and
also tried to read the reactions of the patients, and their family members, in response to the
behaviour that had been manifested by the staff. I concluded that there was failure on my part
in conducting a successful induction of the staff and I must have played a role model, to help
the staff understand the core values of person-centred care.
Evaluation- I considered the incident to be extremely challenging since my feelings of
anxiety and apprehension were closely interrelated to my lack of proficiency in helping the
staff gain a sound understanding of how different social and medical models are applicable to
the delivery of person-centred practice. I regret that I did not act accordingly to challenge the
discriminatory attitude that had been meted out towards the patients. From this experience, I
was able to realise that while a new staff members begins working for a healthcare
organisation, it is extremely essential to help them become efficient and productive, as
rapidly as possible. Research evidences elaborate on the fact that providing new employees
with a comprehensive and clear introduction about the job role and duties result in
substantially enhanced long-term retention of staff (Matthews, Duck and Bartle 2017). The
conventional medical model that is related to the delivery of health services generally follows
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3TASK 2
a paternalistic method where the patients are typically reassured of their health, which is
approved by their family members. Person-centred care generally places more emphasis on
the whole individual, and is not merely focused on the medical conditions (Haegele and
Hodge 2016). I was quick to realise that the staff demonstrated a failure in understanding the
significance and effect of mental, social, spiritual, and emotional needs of all patients, apart
from their medical needs and diagnosis. Person-centred care model holds particular relevance
to patients who suffer from disability or chronic conditions and it is imperative to recognise
each patient as a unique entity having distinct needs, goals and preferences (Britten et al.
2017). One of the most extensively quoted fundamentals of disrespect stated by patients is
merely failing to pay consideration to their requirements and desires, by leaving them ignored
or unattended. Therefore, recognising the significance of the personal values of the patients
and striving to deliver timely care, besides apologizing on demonstrating a failure to do so
(Sokol-Hessner et al. 2018).
The experience also helped me learn that in order to make the care model effective,
we as nursing professionals must have an integral vision of the care plan and must recognise
the singularity and value of the patients by looking at their skills, rather than disabilities,
besides supporting their self-determination. I also comprehended that the staff did not adhere
to the regulation 9 of the Health and Social Care Act 2008 that ensures that patients using
health service must be provided care that is custom-made explicitly for them. The act also
highlights the need of providers to work in partnership for making reasonable adjustment, and
supporting the patients while making informed health decisions (Care Quality Commission
2019).
Analysis- The fact that the new staff made discriminatory remarks against two patients
suffering from psychiatric disorder suggested that no efforts had been taken to protect the
patients, while attending to their dissimilar needs. Thus, during the induction, the staff was
a paternalistic method where the patients are typically reassured of their health, which is
approved by their family members. Person-centred care generally places more emphasis on
the whole individual, and is not merely focused on the medical conditions (Haegele and
Hodge 2016). I was quick to realise that the staff demonstrated a failure in understanding the
significance and effect of mental, social, spiritual, and emotional needs of all patients, apart
from their medical needs and diagnosis. Person-centred care model holds particular relevance
to patients who suffer from disability or chronic conditions and it is imperative to recognise
each patient as a unique entity having distinct needs, goals and preferences (Britten et al.
2017). One of the most extensively quoted fundamentals of disrespect stated by patients is
merely failing to pay consideration to their requirements and desires, by leaving them ignored
or unattended. Therefore, recognising the significance of the personal values of the patients
and striving to deliver timely care, besides apologizing on demonstrating a failure to do so
(Sokol-Hessner et al. 2018).
The experience also helped me learn that in order to make the care model effective,
we as nursing professionals must have an integral vision of the care plan and must recognise
the singularity and value of the patients by looking at their skills, rather than disabilities,
besides supporting their self-determination. I also comprehended that the staff did not adhere
to the regulation 9 of the Health and Social Care Act 2008 that ensures that patients using
health service must be provided care that is custom-made explicitly for them. The act also
highlights the need of providers to work in partnership for making reasonable adjustment, and
supporting the patients while making informed health decisions (Care Quality Commission
2019).
Analysis- The fact that the new staff made discriminatory remarks against two patients
suffering from psychiatric disorder suggested that no efforts had been taken to protect the
patients, while attending to their dissimilar needs. Thus, during the induction, the staff was
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4TASK 2
not able to identify my role as a senior carer and the activities that I undertake to support each
patient, for development of their capacities. The core principles of this framework are
namely, leadership, compassionate care, organisational culture, incident reporting, and safe
staffing levels, all of which are considered to improve patient outcomes (Mukwege and Berg
2016). Senior carers play an important role in developing a positive patient experience and
strong communication with patients helps in improving their satisfaction. Thus, initiating
conversation where the patient is asked about things that matter in the care process or
reassuring the patient will provide the perfect opportunity of building good rapport, within
the confines of roles and responsibilities (Ware 2017). The entire episode made me feel
uncomfortable since the four core values of understanding relationship, life experience,
environment and treating patients with respect and dignity had not been adequately followed.
Taking into consideration the fact that we must ensure that the patients are central to and
involved in their treatment, and are recognised as chief components of the care process, the
episode made me realise that being compassionate and respectful towards the patients are
imperative.
The social model of disability focuses on the fact that disability occurs by the way of
organisation of the society, rather than any difference or impairment in a person. This model
also looks at different strategies for effective removal of barriers that limit the life choices for
people who are disabled. This is in contrast to the medical model that elaborates on the fact
that impairment or differences between individuals are responsible for making them disabled
(Fatoye et al. 2019). In other words, the medical model attempts to explore what is wrong
with an individual, rather than what the individual needs. Thus, it leads to the development of
poor expectations and eventually makes the affected people lose their choice, independence
and control. However, use of the social model helps to explore the cognitive needs of the
affected person, in place of their physical needs (Haegele and Hodge 2016). Thus, from the
not able to identify my role as a senior carer and the activities that I undertake to support each
patient, for development of their capacities. The core principles of this framework are
namely, leadership, compassionate care, organisational culture, incident reporting, and safe
staffing levels, all of which are considered to improve patient outcomes (Mukwege and Berg
2016). Senior carers play an important role in developing a positive patient experience and
strong communication with patients helps in improving their satisfaction. Thus, initiating
conversation where the patient is asked about things that matter in the care process or
reassuring the patient will provide the perfect opportunity of building good rapport, within
the confines of roles and responsibilities (Ware 2017). The entire episode made me feel
uncomfortable since the four core values of understanding relationship, life experience,
environment and treating patients with respect and dignity had not been adequately followed.
Taking into consideration the fact that we must ensure that the patients are central to and
involved in their treatment, and are recognised as chief components of the care process, the
episode made me realise that being compassionate and respectful towards the patients are
imperative.
The social model of disability focuses on the fact that disability occurs by the way of
organisation of the society, rather than any difference or impairment in a person. This model
also looks at different strategies for effective removal of barriers that limit the life choices for
people who are disabled. This is in contrast to the medical model that elaborates on the fact
that impairment or differences between individuals are responsible for making them disabled
(Fatoye et al. 2019). In other words, the medical model attempts to explore what is wrong
with an individual, rather than what the individual needs. Thus, it leads to the development of
poor expectations and eventually makes the affected people lose their choice, independence
and control. However, use of the social model helps to explore the cognitive needs of the
affected person, in place of their physical needs (Haegele and Hodge 2016). Thus, from the
5TASK 2
incident, I realised that the staff must have concentrated on the remaining skills and abilities
of the two patients suffering from mental disorder, and must have taken efforts to stimulate
their mind. This would have developed a sense of belonging amid the patients, besides
providing them security and comfort, thus enhancing their quality of life.
Conclusion- In conclusion, owing to the failure in successfully conducting staff
induction, the new staff did not deliver person-centred care and gave rise to a confrontation.
It is evident that there was a necessity of building rapport with the patients and identifying
their needs, rather than focusing on pre-conceived notion about mental illness. Looking back
at the circumstance I can observe that I must have acted in a better way and ensured that none
of my patients were subjected to derogatory comments from the staff. I realise the importance
of acting as a role model to new staff and would also ensure that their actions do not threaten
the health and wellbeing of my patients.
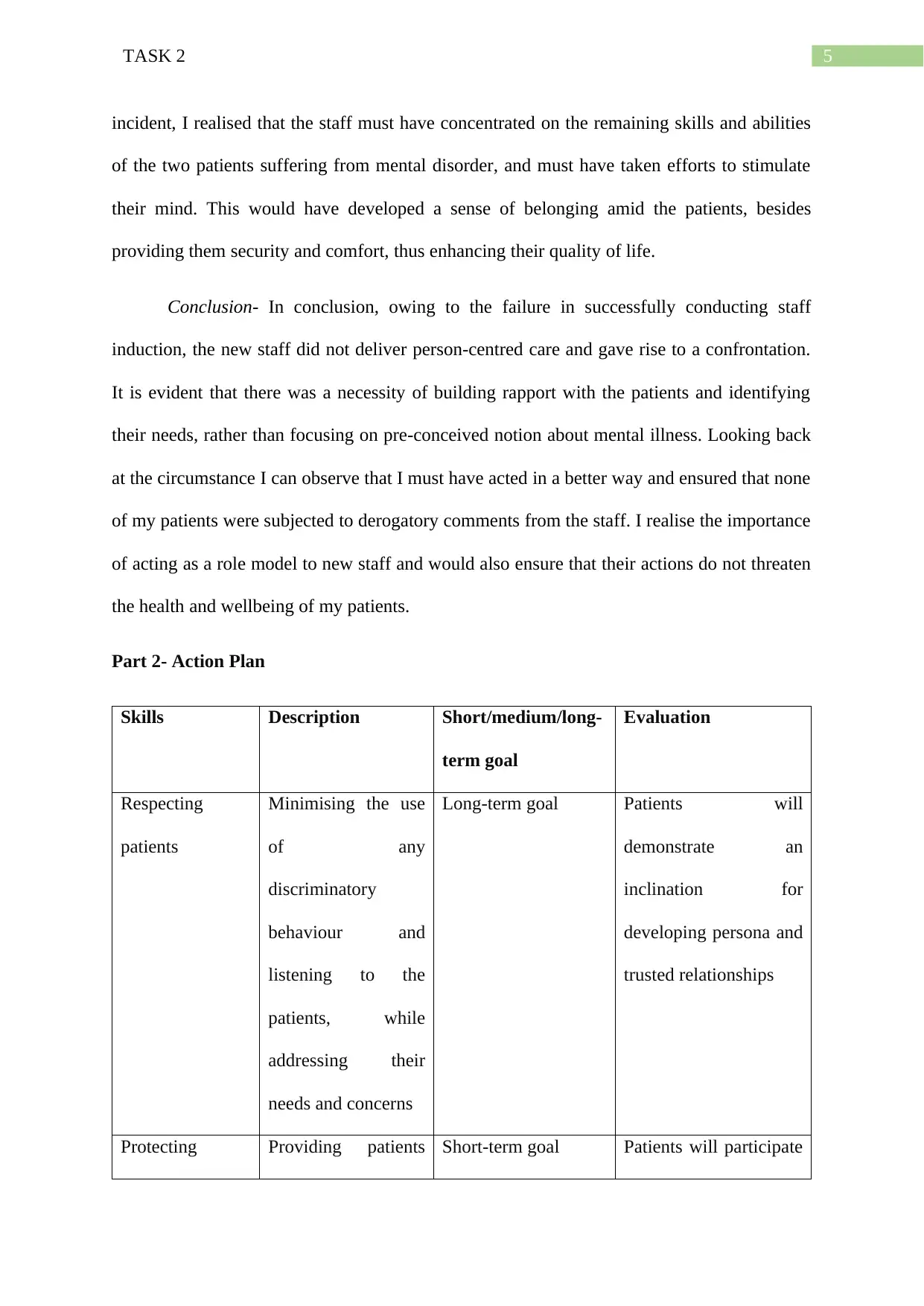
Part 2- Action Plan
Skills Description Short/medium/long-
term goal
Evaluation
Respecting
patients
Minimising the use
of any
discriminatory
behaviour and
listening to the
patients, while
addressing their
needs and concerns
Long-term goal Patients will
demonstrate an
inclination for
developing persona and
trusted relationships
Protecting Providing patients Short-term goal Patients will participate
incident, I realised that the staff must have concentrated on the remaining skills and abilities
of the two patients suffering from mental disorder, and must have taken efforts to stimulate
their mind. This would have developed a sense of belonging amid the patients, besides
providing them security and comfort, thus enhancing their quality of life.
Conclusion- In conclusion, owing to the failure in successfully conducting staff
induction, the new staff did not deliver person-centred care and gave rise to a confrontation.
It is evident that there was a necessity of building rapport with the patients and identifying
their needs, rather than focusing on pre-conceived notion about mental illness. Looking back
at the circumstance I can observe that I must have acted in a better way and ensured that none
of my patients were subjected to derogatory comments from the staff. I realise the importance
of acting as a role model to new staff and would also ensure that their actions do not threaten
the health and wellbeing of my patients.
Part 2- Action Plan
Skills Description Short/medium/long-
term goal
Evaluation
Respecting
patients
Minimising the use
of any
discriminatory
behaviour and
listening to the
patients, while
addressing their
needs and concerns
Long-term goal Patients will
demonstrate an
inclination for
developing persona and
trusted relationships
Protecting Providing patients Short-term goal Patients will participate
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
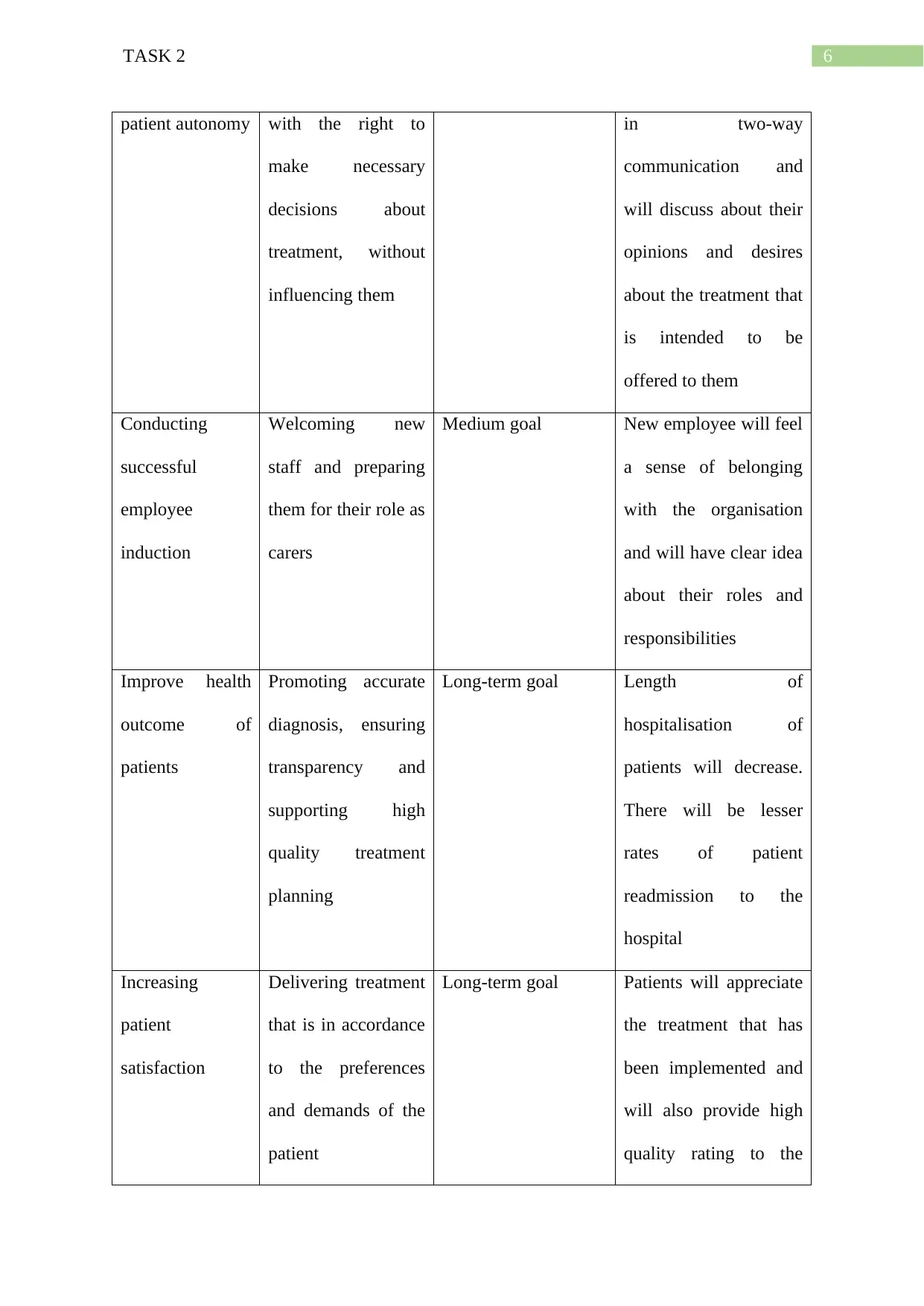
6TASK 2
patient autonomy with the right to
make necessary
decisions about
treatment, without
influencing them
in two-way
communication and
will discuss about their
opinions and desires
about the treatment that
is intended to be
offered to them
Conducting
successful
employee
induction
Welcoming new
staff and preparing
them for their role as
carers
Medium goal New employee will feel
a sense of belonging
with the organisation
and will have clear idea
about their roles and
responsibilities
Improve health
outcome of
patients
Promoting accurate
diagnosis, ensuring
transparency and
supporting high
quality treatment
planning
Long-term goal Length of
hospitalisation of
patients will decrease.
There will be lesser
rates of patient
readmission to the
hospital
Increasing
patient
satisfaction
Delivering treatment
that is in accordance
to the preferences
and demands of the
patient
Long-term goal Patients will appreciate
the treatment that has
been implemented and
will also provide high
quality rating to the
patient autonomy with the right to
make necessary
decisions about
treatment, without
influencing them
in two-way
communication and
will discuss about their
opinions and desires
about the treatment that
is intended to be
offered to them
Conducting
successful
employee
induction
Welcoming new
staff and preparing
them for their role as
carers
Medium goal New employee will feel
a sense of belonging
with the organisation
and will have clear idea
about their roles and
responsibilities
Improve health
outcome of
patients
Promoting accurate
diagnosis, ensuring
transparency and
supporting high
quality treatment
planning
Long-term goal Length of
hospitalisation of
patients will decrease.
There will be lesser
rates of patient
readmission to the
hospital
Increasing
patient
satisfaction
Delivering treatment
that is in accordance
to the preferences
and demands of the
patient
Long-term goal Patients will appreciate
the treatment that has
been implemented and
will also provide high
quality rating to the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
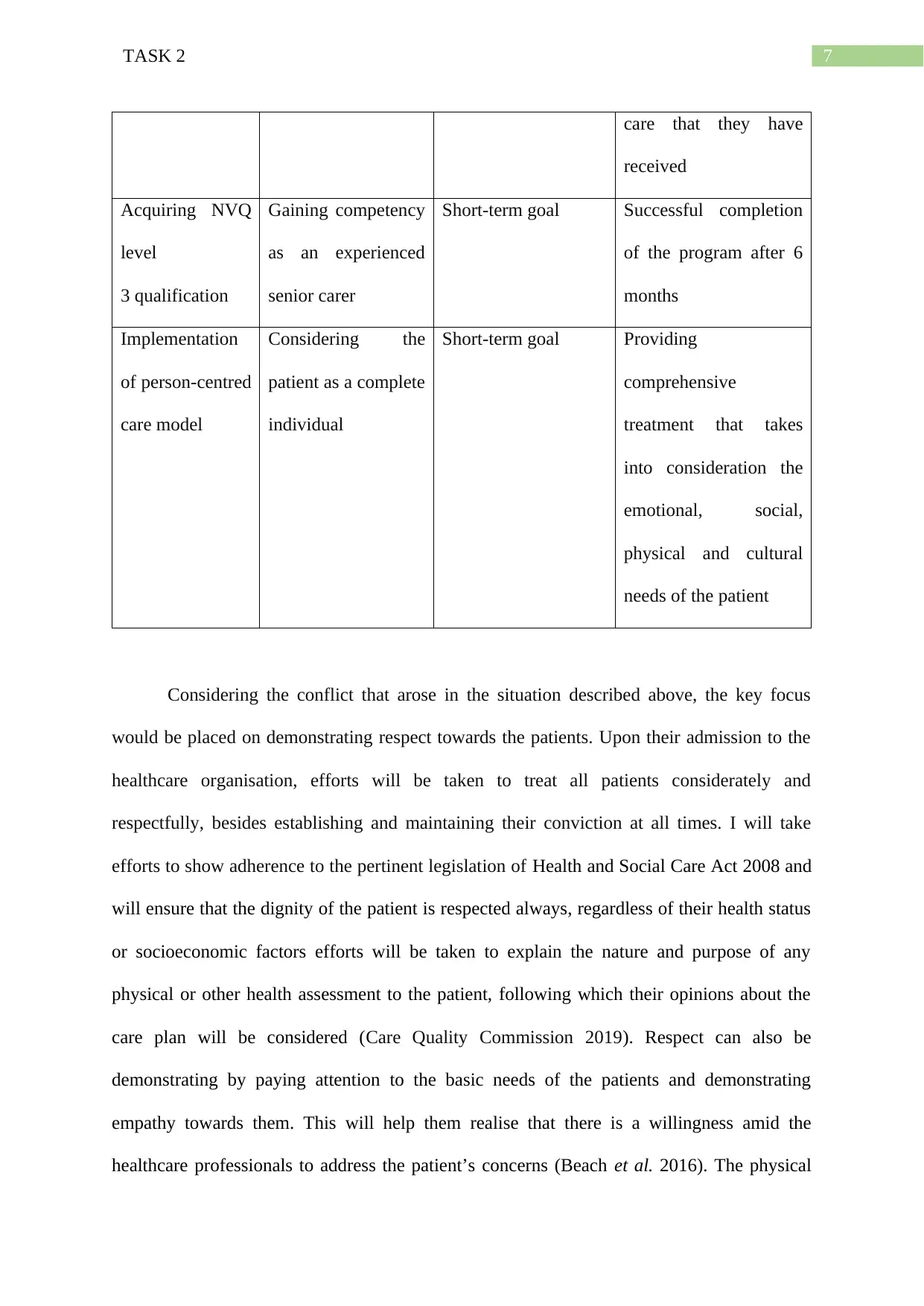
7TASK 2
care that they have
received
Acquiring NVQ
level
3 qualification
Gaining competency
as an experienced
senior carer
Short-term goal Successful completion
of the program after 6
months
Implementation
of person-centred
care model
Considering the
patient as a complete
individual
Short-term goal Providing
comprehensive
treatment that takes
into consideration the
emotional, social,
physical and cultural
needs of the patient
Considering the conflict that arose in the situation described above, the key focus
would be placed on demonstrating respect towards the patients. Upon their admission to the
healthcare organisation, efforts will be taken to treat all patients considerately and
respectfully, besides establishing and maintaining their conviction at all times. I will take
efforts to show adherence to the pertinent legislation of Health and Social Care Act 2008 and
will ensure that the dignity of the patient is respected always, regardless of their health status
or socioeconomic factors efforts will be taken to explain the nature and purpose of any
physical or other health assessment to the patient, following which their opinions about the
care plan will be considered (Care Quality Commission 2019). Respect can also be
demonstrating by paying attention to the basic needs of the patients and demonstrating
empathy towards them. This will help them realise that there is a willingness amid the
healthcare professionals to address the patient’s concerns (Beach et al. 2016). The physical
care that they have
received
Acquiring NVQ
level
3 qualification
Gaining competency
as an experienced
senior carer
Short-term goal Successful completion
of the program after 6
months
Implementation
of person-centred
care model
Considering the
patient as a complete
individual
Short-term goal Providing
comprehensive
treatment that takes
into consideration the
emotional, social,
physical and cultural
needs of the patient
Considering the conflict that arose in the situation described above, the key focus
would be placed on demonstrating respect towards the patients. Upon their admission to the
healthcare organisation, efforts will be taken to treat all patients considerately and
respectfully, besides establishing and maintaining their conviction at all times. I will take
efforts to show adherence to the pertinent legislation of Health and Social Care Act 2008 and
will ensure that the dignity of the patient is respected always, regardless of their health status
or socioeconomic factors efforts will be taken to explain the nature and purpose of any
physical or other health assessment to the patient, following which their opinions about the
care plan will be considered (Care Quality Commission 2019). Respect can also be
demonstrating by paying attention to the basic needs of the patients and demonstrating
empathy towards them. This will help them realise that there is a willingness amid the
healthcare professionals to address the patient’s concerns (Beach et al. 2016). The physical
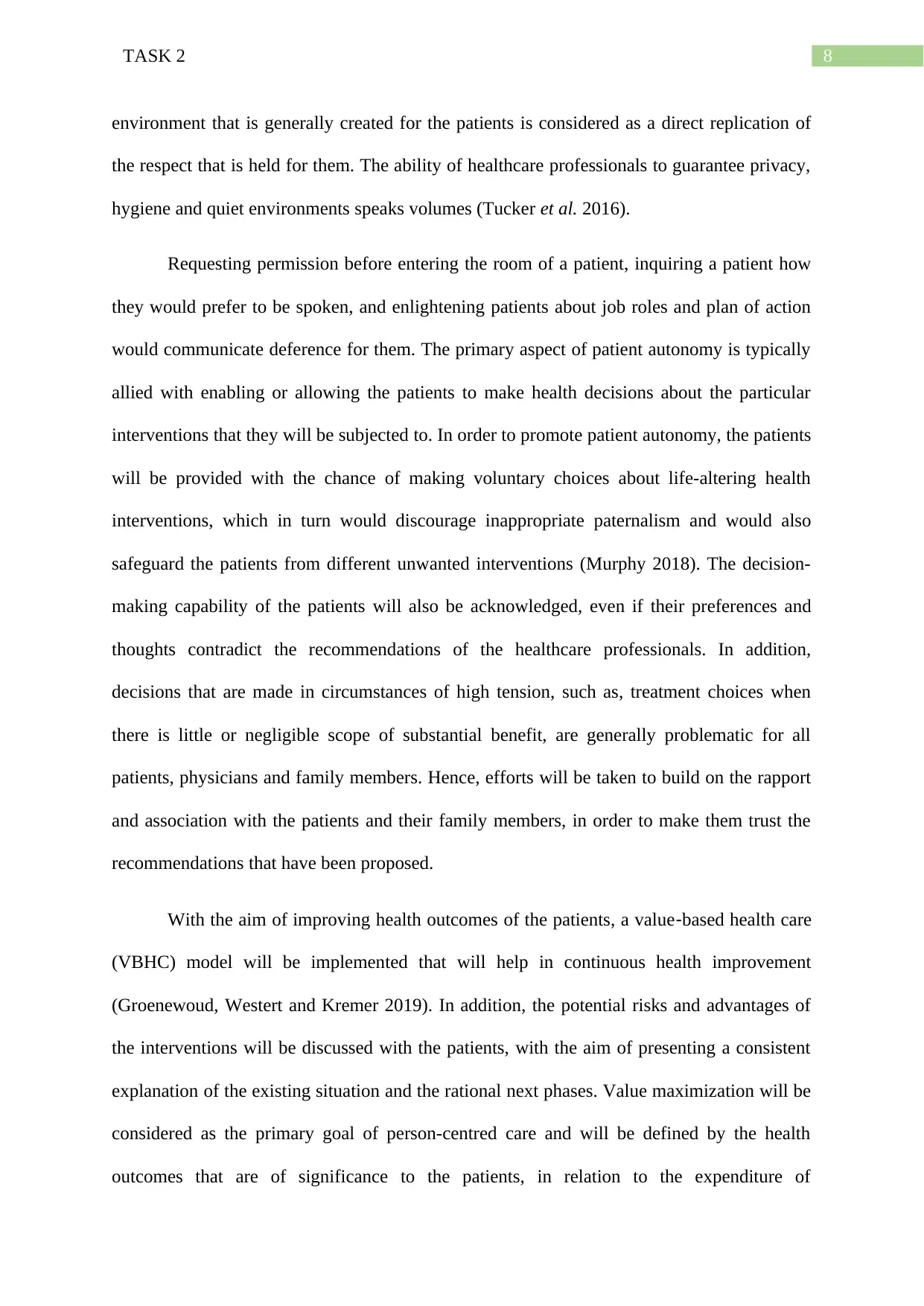
8TASK 2
environment that is generally created for the patients is considered as a direct replication of
the respect that is held for them. The ability of healthcare professionals to guarantee privacy,
hygiene and quiet environments speaks volumes (Tucker et al. 2016).
Requesting permission before entering the room of a patient, inquiring a patient how
they would prefer to be spoken, and enlightening patients about job roles and plan of action
would communicate deference for them. The primary aspect of patient autonomy is typically
allied with enabling or allowing the patients to make health decisions about the particular
interventions that they will be subjected to. In order to promote patient autonomy, the patients
will be provided with the chance of making voluntary choices about life-altering health
interventions, which in turn would discourage inappropriate paternalism and would also
safeguard the patients from different unwanted interventions (Murphy 2018). The decision-
making capability of the patients will also be acknowledged, even if their preferences and
thoughts contradict the recommendations of the healthcare professionals. In addition,
decisions that are made in circumstances of high tension, such as, treatment choices when
there is little or negligible scope of substantial benefit, are generally problematic for all
patients, physicians and family members. Hence, efforts will be taken to build on the rapport
and association with the patients and their family members, in order to make them trust the
recommendations that have been proposed.
With the aim of improving health outcomes of the patients, a value‐based health care
(VBHC) model will be implemented that will help in continuous health improvement
(Groenewoud, Westert and Kremer 2019). In addition, the potential risks and advantages of
the interventions will be discussed with the patients, with the aim of presenting a consistent
explanation of the existing situation and the rational next phases. Value maximization will be
considered as the primary goal of person-centred care and will be defined by the health
outcomes that are of significance to the patients, in relation to the expenditure of
environment that is generally created for the patients is considered as a direct replication of
the respect that is held for them. The ability of healthcare professionals to guarantee privacy,
hygiene and quiet environments speaks volumes (Tucker et al. 2016).
Requesting permission before entering the room of a patient, inquiring a patient how
they would prefer to be spoken, and enlightening patients about job roles and plan of action
would communicate deference for them. The primary aspect of patient autonomy is typically
allied with enabling or allowing the patients to make health decisions about the particular
interventions that they will be subjected to. In order to promote patient autonomy, the patients
will be provided with the chance of making voluntary choices about life-altering health
interventions, which in turn would discourage inappropriate paternalism and would also
safeguard the patients from different unwanted interventions (Murphy 2018). The decision-
making capability of the patients will also be acknowledged, even if their preferences and
thoughts contradict the recommendations of the healthcare professionals. In addition,
decisions that are made in circumstances of high tension, such as, treatment choices when
there is little or negligible scope of substantial benefit, are generally problematic for all
patients, physicians and family members. Hence, efforts will be taken to build on the rapport
and association with the patients and their family members, in order to make them trust the
recommendations that have been proposed.
With the aim of improving health outcomes of the patients, a value‐based health care
(VBHC) model will be implemented that will help in continuous health improvement
(Groenewoud, Westert and Kremer 2019). In addition, the potential risks and advantages of
the interventions will be discussed with the patients, with the aim of presenting a consistent
explanation of the existing situation and the rational next phases. Value maximization will be
considered as the primary goal of person-centred care and will be defined by the health
outcomes that are of significance to the patients, in relation to the expenditure of
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9TASK 2
accomplishing those outcomes. Hence, the goal would be to entail pertinent discussion,
awareness and engagement with the patients and family members on the evidences for
interventions and the decisions in play. Furthermore, in order to increase patient satisfaction,
care will be delivered in a manner that is in alignment with their cultural values and beliefs
(Comer et al. 2017). Furthermore, the patients will be provided more power about mentioning
the approach in which they want to be cared for.
During the delivery of person-centred care, the patient experience improvement
framework, formulated by the NHS will be followed. In addition, the perception of strong
care coordination and teamwork will also act as major markers for a positive patient
experience and will make the patients feel that they are being cared for. It has often been
found that patients who show compliance to the treatment are healthier, which in turn reduces
their healthcare related expenses (Ozsoy-Unubol et al. 2018). While working as a senior
carer, efforts will be taken to provide an outline for staff and management to share in
accountability, problem solving and power. This in turn will provide a voice in the method
the patients are cared for, and will eventually encourage liability and ownership of patient
health outcomes. Taking into consideration the fact that staff induction is the primary step
that prepares the employees for their roles, an organisational culture will be maintained where
the new staff feel valued and appreciated. Efforts will be taken to conduct good induction
programs that would ensure that the staff are able to follow the principles of person-centred
care, while contributing effectively to patient care (King, Roed and Wilson 2018). Moreover,
they will also be provided with adequate information about the objectives of the organisation
and the opportunities that must be utilised to deliver person-centred care.
The Hospital Consumer Assessment of Healthcare Providers and Systems Survey
(HCAHPS) will be conducted in order to determine patient satisfaction about the care
delivered. This 27-question survey will capture the opinions and perceptions of the patients
accomplishing those outcomes. Hence, the goal would be to entail pertinent discussion,
awareness and engagement with the patients and family members on the evidences for
interventions and the decisions in play. Furthermore, in order to increase patient satisfaction,
care will be delivered in a manner that is in alignment with their cultural values and beliefs
(Comer et al. 2017). Furthermore, the patients will be provided more power about mentioning
the approach in which they want to be cared for.
During the delivery of person-centred care, the patient experience improvement
framework, formulated by the NHS will be followed. In addition, the perception of strong
care coordination and teamwork will also act as major markers for a positive patient
experience and will make the patients feel that they are being cared for. It has often been
found that patients who show compliance to the treatment are healthier, which in turn reduces
their healthcare related expenses (Ozsoy-Unubol et al. 2018). While working as a senior
carer, efforts will be taken to provide an outline for staff and management to share in
accountability, problem solving and power. This in turn will provide a voice in the method
the patients are cared for, and will eventually encourage liability and ownership of patient
health outcomes. Taking into consideration the fact that staff induction is the primary step
that prepares the employees for their roles, an organisational culture will be maintained where
the new staff feel valued and appreciated. Efforts will be taken to conduct good induction
programs that would ensure that the staff are able to follow the principles of person-centred
care, while contributing effectively to patient care (King, Roed and Wilson 2018). Moreover,
they will also be provided with adequate information about the objectives of the organisation
and the opportunities that must be utilised to deliver person-centred care.
The Hospital Consumer Assessment of Healthcare Providers and Systems Survey
(HCAHPS) will be conducted in order to determine patient satisfaction about the care
delivered. This 27-question survey will capture the opinions and perceptions of the patients
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10TASK 2
and will also empower their decision making skills. This survey comprises of a domain that
focuses on patient dignity (Kahn et al. 2015). Thus, responses will also elucidate whether the
patients are treated with respect and courtesy. Healthcare costs and rates of hospital
readmission will be monitored by conducting a clinical audit. This audit will prove whether
the stated goals have been accomplished properly, which in turn would demonstrate
improvement in patient outcome and care. Furthermore, successful completion of the diploma
program after six months will also ensure that necessary skills and proficiency required for
the role of a senior carer have been acquired. In addition, successful employee induction will
be assessed by obtaining feedback from the employees about their workplace culture, rapport
with colleagues, and cooperation (Huang et al. 2015). It can be suggested that on
accomplishing the aforementioned goals, the specific needs and health outcomes of the
patients will be addressed. This will ensure that the patients are treated not merely from a
clinical perspective but also from mental, spiritual, financial, social and emotional
perspective. Realisation of the goals will help in delivery of care in a coordinated and
collaborative manner and will also enhance reputation of the providers, among the patients,
besides reducing expenses and improving resource allocation.
and will also empower their decision making skills. This survey comprises of a domain that
focuses on patient dignity (Kahn et al. 2015). Thus, responses will also elucidate whether the
patients are treated with respect and courtesy. Healthcare costs and rates of hospital
readmission will be monitored by conducting a clinical audit. This audit will prove whether
the stated goals have been accomplished properly, which in turn would demonstrate
improvement in patient outcome and care. Furthermore, successful completion of the diploma
program after six months will also ensure that necessary skills and proficiency required for
the role of a senior carer have been acquired. In addition, successful employee induction will
be assessed by obtaining feedback from the employees about their workplace culture, rapport
with colleagues, and cooperation (Huang et al. 2015). It can be suggested that on
accomplishing the aforementioned goals, the specific needs and health outcomes of the
patients will be addressed. This will ensure that the patients are treated not merely from a
clinical perspective but also from mental, spiritual, financial, social and emotional
perspective. Realisation of the goals will help in delivery of care in a coordinated and
collaborative manner and will also enhance reputation of the providers, among the patients,
besides reducing expenses and improving resource allocation.
11TASK 2
References
Beach, M.C., Saha, S., Branyon, E., Ehanire, I., Mathews, Z. and Cooper, L.A., 2016.
Communicating Respect for Patients as Persons: A Qualitative Study. International Journal
of Person Centered Medicine, 6(1), pp.42-49.
Britten, N., Moore, L., Lydahl, D., Naldemirci, O., Elam, M. and Wolf, A., 2017. Elaboration
of the Gothenburg model of person‐centred care. Health Expectations, 20(3), pp.407-418.
Care Quality Commission., 2019. Health and Social Care Act 2008 (Regulated Activities)
Regulations 2014: Regulation 9. [online] Available at: https://www.cqc.org.uk/guidance-
providers/regulations-enforcement/regulation-9-person-centred-care [Accessed 26 Feb. 2019]
Comer, D., Goldsack, J., Flaherty, J., Van Velzen, K., Caplan, R., Britt, K., Viohl, H., Heitz,
K. and Corbo, T., 2017. Impact of a discharge prescription program on hospital readmissions
and patient satisfaction. Journal of the American Pharmacists Association, 57(4), pp.498-
502.
Fatoye, C., Betts, A., Odeyemi, A., Fatoye, F. and Odeyemi, I., 2019. PNS149 THE
MEDICAL AND SOCIAL MODELS OF DISABILITY. Value in Health, 22, pp.S310-S311.
Groenewoud, A.S., Westert, G.P. and Kremer, J.A., 2019. Value based competition in health
care’s ethical drawbacks and the need for a values-driven approach. BMC health services
research, 19(1), p.256.
Haegele, J.A. and Hodge, S., 2016. Disability discourse: Overview and critiques of the
medical and social models. Quest, 68(2), pp.193-206.
Huang, M., Li, P., Meschke, F. and Guthrie, J.P., 2015. Family firms, employee satisfaction,
and corporate performance. Journal of Corporate Finance, 34, pp.108-127.
References
Beach, M.C., Saha, S., Branyon, E., Ehanire, I., Mathews, Z. and Cooper, L.A., 2016.
Communicating Respect for Patients as Persons: A Qualitative Study. International Journal
of Person Centered Medicine, 6(1), pp.42-49.
Britten, N., Moore, L., Lydahl, D., Naldemirci, O., Elam, M. and Wolf, A., 2017. Elaboration
of the Gothenburg model of person‐centred care. Health Expectations, 20(3), pp.407-418.
Care Quality Commission., 2019. Health and Social Care Act 2008 (Regulated Activities)
Regulations 2014: Regulation 9. [online] Available at: https://www.cqc.org.uk/guidance-
providers/regulations-enforcement/regulation-9-person-centred-care [Accessed 26 Feb. 2019]
Comer, D., Goldsack, J., Flaherty, J., Van Velzen, K., Caplan, R., Britt, K., Viohl, H., Heitz,
K. and Corbo, T., 2017. Impact of a discharge prescription program on hospital readmissions
and patient satisfaction. Journal of the American Pharmacists Association, 57(4), pp.498-
502.
Fatoye, C., Betts, A., Odeyemi, A., Fatoye, F. and Odeyemi, I., 2019. PNS149 THE
MEDICAL AND SOCIAL MODELS OF DISABILITY. Value in Health, 22, pp.S310-S311.
Groenewoud, A.S., Westert, G.P. and Kremer, J.A., 2019. Value based competition in health
care’s ethical drawbacks and the need for a values-driven approach. BMC health services
research, 19(1), p.256.
Haegele, J.A. and Hodge, S., 2016. Disability discourse: Overview and critiques of the
medical and social models. Quest, 68(2), pp.193-206.
Huang, M., Li, P., Meschke, F. and Guthrie, J.P., 2015. Family firms, employee satisfaction,
and corporate performance. Journal of Corporate Finance, 34, pp.108-127.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





