Systematic Review: Smoking Cessation and Mental Health in UK
VerifiedAdded on 2022/08/21
|68
|16982
|22
Assignment
AI Summary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: DISSERTATION: SYSTEMATIC REVIEW
DISSERTATION: SYSTEMATIC REVIEW: THE EFFECT OF SMOKING CESSATION ON
MENTAL HEALTH OF ACUTELY ILL PATIENTS IN A MENTAL HEALTH SETTING IN
THE UNITED KINGDOM
Name of the Student:
Name of the University:
Author note:
DISSERTATION: SYSTEMATIC REVIEW: THE EFFECT OF SMOKING CESSATION ON
MENTAL HEALTH OF ACUTELY ILL PATIENTS IN A MENTAL HEALTH SETTING IN
THE UNITED KINGDOM
Name of the Student:
Name of the University:
Author note:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
Abstract
This thesis aims to critically review existing evidence based research exploring the impact of
smoking cessation on mental illness symptoms in patients with acute mental illnesses and
admitted across mental healthcare settings of the United Kingdom. Based on current literature
which were reviewed and analysed critically in this thesis, smoking cessation interventions were
found to facilitate the achievement of positive physiological and psychological outcomes across
patients with acute mental illnesses. The key psychological effects of smoking cessation were
found to be: reduced severity of depressive and anxiety symptoms and overall sympathetic
nervous system functioning, improvements in dopamine activity especially with regards to
schizophrenia and an overall enhancement of feelings of self-esteem. Additionally, smoking
cessation was also evidenced to result in beneficial metabolic and cardiovascular outcomes
which in turn, can significantly mitigate the risk of reduced life expectancy and high mortality
rates across patients with acute mental illness. Such findings demonstrate considerable
significance with regards to future nursing as well as mental health practice due to their ability to
inform and guide mental healthcare organizations on the factors, outcomes and facilitators to
look for when administering smoking cessation based interventions across mental health settings.
However, dearth of evidence based literature across the mental health settings of United
Kingdom raised significant difficulty in terms of applicability of these findings in practical,
mental healthcare scenarios. Additionally, the dearth of standardized mental health assessments
further made it difficult to analyze the association between findings and changes in mental health
outcomes, symptoms, wellbeing and quality of life across patients with acute mental illnesses in
the UK. It is recommended that nurses as well as healthcare organizations prioritize engagement
Abstract
This thesis aims to critically review existing evidence based research exploring the impact of
smoking cessation on mental illness symptoms in patients with acute mental illnesses and
admitted across mental healthcare settings of the United Kingdom. Based on current literature
which were reviewed and analysed critically in this thesis, smoking cessation interventions were
found to facilitate the achievement of positive physiological and psychological outcomes across
patients with acute mental illnesses. The key psychological effects of smoking cessation were
found to be: reduced severity of depressive and anxiety symptoms and overall sympathetic
nervous system functioning, improvements in dopamine activity especially with regards to
schizophrenia and an overall enhancement of feelings of self-esteem. Additionally, smoking
cessation was also evidenced to result in beneficial metabolic and cardiovascular outcomes
which in turn, can significantly mitigate the risk of reduced life expectancy and high mortality
rates across patients with acute mental illness. Such findings demonstrate considerable
significance with regards to future nursing as well as mental health practice due to their ability to
inform and guide mental healthcare organizations on the factors, outcomes and facilitators to
look for when administering smoking cessation based interventions across mental health settings.
However, dearth of evidence based literature across the mental health settings of United
Kingdom raised significant difficulty in terms of applicability of these findings in practical,
mental healthcare scenarios. Additionally, the dearth of standardized mental health assessments
further made it difficult to analyze the association between findings and changes in mental health
outcomes, symptoms, wellbeing and quality of life across patients with acute mental illnesses in
the UK. It is recommended that nurses as well as healthcare organizations prioritize engagement
2SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
in more comprehensive, robust and quantitative research specific to UK settings so as to acquired
clinical findings relevance to the management of acutely ill mental health patients.
in more comprehensive, robust and quantitative research specific to UK settings so as to acquired
clinical findings relevance to the management of acutely ill mental health patients.
3SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
Table of Contents
Chapter 1: Introduction........................................................................................................6
1.1. Introduction........................................................................................................6
1.1.2. Research Background........................................................................................6
1.2. Research Rationale...................................................................................................7
1.2.1. Nursing Implications.........................................................................................8
1.3. Aims and Objectives.................................................................................................8
1.3.1. Objectives..........................................................................................................8
1.3.2. Research Question.............................................................................................9
1.4. Research Structure....................................................................................................9
Chapter 2: Literature Review.........................................................................................11
2.1. Introduction...........................................................................................................11
2.2. Health Effects of Smoking and associated perceptions.....................................11
2.3. Prevalence and mental health outcomes of smoking in the United Kingdom.13
2.4. Health Effects of Smoking Cessation..................................................................16
2.5. Health Effects of Smoking Cessation in Mental Health Patients.....................19
2.6. Theoretical Framework...........................................................................................20
2.7. Research Limitations and Implications..............................................................21
Chapter 3: Methodology.................................................................................................23
3.1. Literature Review Findings.................................................................................23
Table of Contents
Chapter 1: Introduction........................................................................................................6
1.1. Introduction........................................................................................................6
1.1.2. Research Background........................................................................................6
1.2. Research Rationale...................................................................................................7
1.2.1. Nursing Implications.........................................................................................8
1.3. Aims and Objectives.................................................................................................8
1.3.1. Objectives..........................................................................................................8
1.3.2. Research Question.............................................................................................9
1.4. Research Structure....................................................................................................9
Chapter 2: Literature Review.........................................................................................11
2.1. Introduction...........................................................................................................11
2.2. Health Effects of Smoking and associated perceptions.....................................11
2.3. Prevalence and mental health outcomes of smoking in the United Kingdom.13
2.4. Health Effects of Smoking Cessation..................................................................16
2.5. Health Effects of Smoking Cessation in Mental Health Patients.....................19
2.6. Theoretical Framework...........................................................................................20
2.7. Research Limitations and Implications..............................................................21
Chapter 3: Methodology.................................................................................................23
3.1. Literature Review Findings.................................................................................23
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
3.2. Chosen Methodology: Systematic Review..........................................................23
3.3. PICOT Question...................................................................................................24
3.4. Search Strategy.....................................................................................................25
3.5. Inclusion and Exclusion Criteria.........................................................................25
3.5.1. Inclusion Criteria...........................................................................................25
3.5.2. Exclusion Criteria..........................................................................................26
3.6. PRISMA Flow Diagram.......................................................................................26
Figure A: PRISMA Flow Diagram............................................................................27
3.7. Critiquing the Articles..........................................................................................28
3.8. Research Validity..................................................................................................28
Chapter 4: Results...........................................................................................................29
4.1. Introduction...........................................................................................................29
4.2. Article 1: Royal College of Physicians (2013).....................................................29
4.3. Article 2: Knowles et al. (2016)............................................................................30
4.4. Article 3: Trainer and Leavey (2017)..................................................................31
4.5. Article 4: Osborn et al. (2018)..............................................................................32
4.6. Article 5: Richardson, McNeill and Brose (2019)..............................................33
4.7. Article 6: GillBody et al. (2019)...........................................................................34
4.8. Conclusion: Findings and Observations.............................................................35
Chapter 5: Discussion......................................................................................................37
3.2. Chosen Methodology: Systematic Review..........................................................23
3.3. PICOT Question...................................................................................................24
3.4. Search Strategy.....................................................................................................25
3.5. Inclusion and Exclusion Criteria.........................................................................25
3.5.1. Inclusion Criteria...........................................................................................25
3.5.2. Exclusion Criteria..........................................................................................26
3.6. PRISMA Flow Diagram.......................................................................................26
Figure A: PRISMA Flow Diagram............................................................................27
3.7. Critiquing the Articles..........................................................................................28
3.8. Research Validity..................................................................................................28
Chapter 4: Results...........................................................................................................29
4.1. Introduction...........................................................................................................29
4.2. Article 1: Royal College of Physicians (2013).....................................................29
4.3. Article 2: Knowles et al. (2016)............................................................................30
4.4. Article 3: Trainer and Leavey (2017)..................................................................31
4.5. Article 4: Osborn et al. (2018)..............................................................................32
4.6. Article 5: Richardson, McNeill and Brose (2019)..............................................33
4.7. Article 6: GillBody et al. (2019)...........................................................................34
4.8. Conclusion: Findings and Observations.............................................................35
Chapter 5: Discussion......................................................................................................37
5SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
5.1. Introduction and Brief Overview........................................................................37
5.2. Smoking Cessation effects on Mental Health.....................................................37
5.3. Smoking cessation effects on Cardiovascular Health........................................38
5.4. Smoking Cessation effects on Social and Emotional Outcomes.......................39
Chapter 6: Limitations....................................................................................................40
Chapter 7: Conclusion.....................................................................................................41
References..........................................................................................................................42
Appendices........................................................................................................................50
Appendix 1: PRISMA Table.........................................................................................50
Appendix 2: Inclusion and Exclusion Table..................................................................50
Appendix 3: CASP Tool for Cohort Studies (Richardson, McNeill and Brose 2019). .51
Appendix 4: CASP Tool for Qualitative Studies (Knowles et al. 2016).......................52
Appendix 5: CASP Tool for Systematic Reviews.........................................................53
Appendix 6: CASP Tools for Randomized Controlled Trials.......................................53
Appendix 7: Summary Table...........................................................................................0
Appendix 8: Gantt chart...................................................................................................4
Appendix 8: Search terms/results used for each Database..............................................5
5.1. Introduction and Brief Overview........................................................................37
5.2. Smoking Cessation effects on Mental Health.....................................................37
5.3. Smoking cessation effects on Cardiovascular Health........................................38
5.4. Smoking Cessation effects on Social and Emotional Outcomes.......................39
Chapter 6: Limitations....................................................................................................40
Chapter 7: Conclusion.....................................................................................................41
References..........................................................................................................................42
Appendices........................................................................................................................50
Appendix 1: PRISMA Table.........................................................................................50
Appendix 2: Inclusion and Exclusion Table..................................................................50
Appendix 3: CASP Tool for Cohort Studies (Richardson, McNeill and Brose 2019). .51
Appendix 4: CASP Tool for Qualitative Studies (Knowles et al. 2016).......................52
Appendix 5: CASP Tool for Systematic Reviews.........................................................53
Appendix 6: CASP Tools for Randomized Controlled Trials.......................................53
Appendix 7: Summary Table...........................................................................................0
Appendix 8: Gantt chart...................................................................................................4
Appendix 8: Search terms/results used for each Database..............................................5
6SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
Chapter 1: Introduction
1.1. Introduction
Understandably, smoking is a preventable and modifiable risky health behaviour which
can be addressed in patients with mental health conditions to improved health outcomes (Bailey
et al., 2017). There is, however, limited research and exploration of the ways in which the
compliance to smoking by patients with acute and acute mental disorders can be reduced and
resultant impact on their wellbeing and mental health, especially within the context of the United
Kingdom (UK). The author thus aims to review current evidence-based literature on the effect
and effect of smoking cessation upon the wellbeing and mental health in patients with acute
mental disorders, admitted across mental health unit across healthcare organizations in the UK.
1.1.2. Research Background
Patients admitted with an acute mental illness are also susceptible to have shorter spans
of life expectancy due to prevalent co-morbidities like cardiovascular conditions or respiratory
illness (Evins, Cather and Daumit, 2019). It has been evidenced in the data presented by Public
Health England that approximately 40.5% of adults, with an acute mental illness, engage in
smoking (Forman et al. 2017). Such debilitating lifestyle behaviours thus contribute to further
aggravation of the pre-existing physiological co-morbidities impacting this population. Such
high rates of smoking by an already-vulnerable population thus demonstrates the need for
developing comprehensive and efficient smoking cessation strategies (Gilbody et al. 2019).
The findings by Public Health England (2016) also report deaths due to smoking-
associated conditions across approximately 78, 200 individuals within the UK. It has further
been postulated that smoking is one of the strongest contributors to decreased rates of life
Chapter 1: Introduction
1.1. Introduction
Understandably, smoking is a preventable and modifiable risky health behaviour which
can be addressed in patients with mental health conditions to improved health outcomes (Bailey
et al., 2017). There is, however, limited research and exploration of the ways in which the
compliance to smoking by patients with acute and acute mental disorders can be reduced and
resultant impact on their wellbeing and mental health, especially within the context of the United
Kingdom (UK). The author thus aims to review current evidence-based literature on the effect
and effect of smoking cessation upon the wellbeing and mental health in patients with acute
mental disorders, admitted across mental health unit across healthcare organizations in the UK.
1.1.2. Research Background
Patients admitted with an acute mental illness are also susceptible to have shorter spans
of life expectancy due to prevalent co-morbidities like cardiovascular conditions or respiratory
illness (Evins, Cather and Daumit, 2019). It has been evidenced in the data presented by Public
Health England that approximately 40.5% of adults, with an acute mental illness, engage in
smoking (Forman et al. 2017). Such debilitating lifestyle behaviours thus contribute to further
aggravation of the pre-existing physiological co-morbidities impacting this population. Such
high rates of smoking by an already-vulnerable population thus demonstrates the need for
developing comprehensive and efficient smoking cessation strategies (Gilbody et al. 2019).
The findings by Public Health England (2016) also report deaths due to smoking-
associated conditions across approximately 78, 200 individuals within the UK. It has further
been postulated that smoking is one of the strongest contributors to decreased rates of life
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
expectancy across mental health patients with mental health issues like personality disorders (18
years for females and males), depression (11 years for males and 7 years for females
respectively), alcohol misuse (10.8 years for females and 17.1 years for males) and opioid
misuse associated disorders (9.0 years for males and 17.3 years for females). According to the
findings by the WHO (2019), approximately 8 million individuals across the globe are inflicted
as a result of prolonged contact with tobacco smoke or engagement in associated detrimental
lifestyle habits such as cigarette smoking.
1.2. Research Rationale
Smoking cessation causes withdrawal symptoms such as anxiety, irritability, depression
and emotional distress, which in turn, hinders an individual’s eagerness and enthusiasm to quit
the same. Such issues may be aggravated in acute mental health illness due to inability to engage
in self-regulation of depressive or anxiety symptoms (Roberts et al. 2016). The addictive effects
of smoking is largely associated with nicotine which in turn, has been evidenced to facilitate the
production of dopamine. Individuals with mental illnesses demonstrate low amounts of essential
neurotransmitters like dopamine, which thus results in smoking instilling feelings of relaxation
and wellbeing with a potency greater than that observed across the healthy population (Sharma et
al. 2018). Thus, it is unsurprising to find higher rates of prevalence and relapse in smoking
behaviours as well as physiological health issues across patients with acute mental illness, which
in turn, impacts their ability to achieve long term positive health outcomes. The high risk of
smoking and its associated consequences across patients with acute mental illness as well as lack
of sufficient research in the UK context thus form the rationale underlying the need to develop
comprehensive and efficient smoking cessation strategies and thus, the formulation of this
research topic (Jaén-Moreno et al. 2019).
expectancy across mental health patients with mental health issues like personality disorders (18
years for females and males), depression (11 years for males and 7 years for females
respectively), alcohol misuse (10.8 years for females and 17.1 years for males) and opioid
misuse associated disorders (9.0 years for males and 17.3 years for females). According to the
findings by the WHO (2019), approximately 8 million individuals across the globe are inflicted
as a result of prolonged contact with tobacco smoke or engagement in associated detrimental
lifestyle habits such as cigarette smoking.
1.2. Research Rationale
Smoking cessation causes withdrawal symptoms such as anxiety, irritability, depression
and emotional distress, which in turn, hinders an individual’s eagerness and enthusiasm to quit
the same. Such issues may be aggravated in acute mental health illness due to inability to engage
in self-regulation of depressive or anxiety symptoms (Roberts et al. 2016). The addictive effects
of smoking is largely associated with nicotine which in turn, has been evidenced to facilitate the
production of dopamine. Individuals with mental illnesses demonstrate low amounts of essential
neurotransmitters like dopamine, which thus results in smoking instilling feelings of relaxation
and wellbeing with a potency greater than that observed across the healthy population (Sharma et
al. 2018). Thus, it is unsurprising to find higher rates of prevalence and relapse in smoking
behaviours as well as physiological health issues across patients with acute mental illness, which
in turn, impacts their ability to achieve long term positive health outcomes. The high risk of
smoking and its associated consequences across patients with acute mental illness as well as lack
of sufficient research in the UK context thus form the rationale underlying the need to develop
comprehensive and efficient smoking cessation strategies and thus, the formulation of this
research topic (Jaén-Moreno et al. 2019).
8SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
1.2.1. Nursing Implications
Thus, from the above findings, it can be observed that smoking and interventions like
smoking cessation are not merely associated with a reduction of mental illness symptom
aggravation but a range of changes in cardiovascular and neurological disease outcomes.
Additionally, the impact of nicotine on the functional wellbeing of patients further demonstrate
the need to address social and emotional outcomes in patients with acute mental health illnesses
(Sharma et al. 2018). All of these highlight the importance of therapeutic communication as well
as multidisciplinary and collaborative approaches to treatment – which are in turn, are key
perquisites in nursing practice. Thus, this research has key implications for future nursing
practice in terms of guiding nurses on the need to therapeutically and empathetically
communicate as well as the key comorbidities required to be assessed and collaborated with
inter-disciplinary professions for optimum smoking cessation implementation and mental health
management across real life mental health settings (Sheals et al. 2016).
1.3. Aims and Objectives
Thus, the aim of this thesis is to systematically review the effect of smoking cessation
on mental health and wellbeing of patients with acute mental illness across mental health
settings in the United Kingdom.
1.3.1. Objectives
To critically review primary research articles on the association between smoking and
mental health and wellbeing with respect to with acute mental illness across mental health
settings in the United Kingdom.
1.2.1. Nursing Implications
Thus, from the above findings, it can be observed that smoking and interventions like
smoking cessation are not merely associated with a reduction of mental illness symptom
aggravation but a range of changes in cardiovascular and neurological disease outcomes.
Additionally, the impact of nicotine on the functional wellbeing of patients further demonstrate
the need to address social and emotional outcomes in patients with acute mental health illnesses
(Sharma et al. 2018). All of these highlight the importance of therapeutic communication as well
as multidisciplinary and collaborative approaches to treatment – which are in turn, are key
perquisites in nursing practice. Thus, this research has key implications for future nursing
practice in terms of guiding nurses on the need to therapeutically and empathetically
communicate as well as the key comorbidities required to be assessed and collaborated with
inter-disciplinary professions for optimum smoking cessation implementation and mental health
management across real life mental health settings (Sheals et al. 2016).
1.3. Aims and Objectives
Thus, the aim of this thesis is to systematically review the effect of smoking cessation
on mental health and wellbeing of patients with acute mental illness across mental health
settings in the United Kingdom.
1.3.1. Objectives
To critically review primary research articles on the association between smoking and
mental health and wellbeing with respect to with acute mental illness across mental health
settings in the United Kingdom.
9SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
To critically review primary research articles on the strategies to aid in smoking cessations
and overall improvement in mental health and wellbeing outcomes in patients with acute
mental illness across mental health settings in the United Kingdom.
To critically review primary research articles on the effect of smoking cessation on mental
health and wellbeing of patients with acute mental illness across mental health settings in
the United Kingdom.
1.3.2. Research Question
The PICOT components of this thesis are as follows: What is the effect of smoking
cessation on mental health symptoms and wellbeing of patients with acute mental illness
across mental health settings in the United Kingdom?
Population: (P): Adult patients with acute mental illnesses admitted in UK base mental
health settings.
Intervention (I): Interventions prioritized around cessation of smoking.
Comparison (C): Absence of smoking cessation
Outcomes (O): Reduced severity and frequency of mental health symptoms, improved
sense of quality of life and wellbeing.
Time (T): A minimum of 3 months or more.
1.4. Research Structure
For exploring the formulated research questions in a scientifically valid manner, the
author will proceed with the following structure.
To critically review primary research articles on the strategies to aid in smoking cessations
and overall improvement in mental health and wellbeing outcomes in patients with acute
mental illness across mental health settings in the United Kingdom.
To critically review primary research articles on the effect of smoking cessation on mental
health and wellbeing of patients with acute mental illness across mental health settings in
the United Kingdom.
1.3.2. Research Question
The PICOT components of this thesis are as follows: What is the effect of smoking
cessation on mental health symptoms and wellbeing of patients with acute mental illness
across mental health settings in the United Kingdom?
Population: (P): Adult patients with acute mental illnesses admitted in UK base mental
health settings.
Intervention (I): Interventions prioritized around cessation of smoking.
Comparison (C): Absence of smoking cessation
Outcomes (O): Reduced severity and frequency of mental health symptoms, improved
sense of quality of life and wellbeing.
Time (T): A minimum of 3 months or more.
1.4. Research Structure
For exploring the formulated research questions in a scientifically valid manner, the
author will proceed with the following structure.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
The ‘Introduction’ will briefly discuss on relevant background and limitations of research
which in turn, prompted the development of identified research aim, objectives and
questions pertaining to smoking cessation and mental health.
The ‘Literature Review’ chapter critically explores present literature and scientific studies
which have explored smoking cessation and mental health outcomes and in-depth evaluation
of their associated limitations.
The chapter on ‘Methodology’ will discuss on the strategies used to collect articles relevant
for answering the associated PICOT question on smoking cessation and mental health.
The ‘Results’ chapter will succinctly discuss on the evidence-based findings acquired from
the literature review and associated reflections on smoking cessation and mental health.
The chapter on ‘Limitations’ will briefly highlight the relevant gaps in literature and scope
of improvement for future research.
The ‘Conclusion’ chapter will summarize the overall findings of the systematic review as
well as future recommendations with regards to smoking cessation and mental health.
The ‘Introduction’ will briefly discuss on relevant background and limitations of research
which in turn, prompted the development of identified research aim, objectives and
questions pertaining to smoking cessation and mental health.
The ‘Literature Review’ chapter critically explores present literature and scientific studies
which have explored smoking cessation and mental health outcomes and in-depth evaluation
of their associated limitations.
The chapter on ‘Methodology’ will discuss on the strategies used to collect articles relevant
for answering the associated PICOT question on smoking cessation and mental health.
The ‘Results’ chapter will succinctly discuss on the evidence-based findings acquired from
the literature review and associated reflections on smoking cessation and mental health.
The chapter on ‘Limitations’ will briefly highlight the relevant gaps in literature and scope
of improvement for future research.
The ‘Conclusion’ chapter will summarize the overall findings of the systematic review as
well as future recommendations with regards to smoking cessation and mental health.
11SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
Chapter 2: Literature Review
2.1. Introduction
This chapter will hence elaborately and extensively review and review current clinical
and evidence-based research exploring the context of smoking behaviour, smoking cessation,
associated health consequences and mental health outcomes across the global context as well as
specifically within the UK population.
2.2. Health Effects of Smoking and associated perceptions
At present, as estimated by the World Health Organization, (WHO, 2019), one of the
most damaging and challenging issues impacting the world is the ‘tobacco epidemic’. According
to the findings by the WHO (2019), approximately 8 million individuals across the globe are
inflicted as a result of prolonged exposure to tobacco smoke or engagement in associated
detrimental lifestyle habits such as cigarette smoking. Of these, as denoted by the WHO (2019),
approximately 1.2 million and 7 million deaths have been reported as a result of passive or direct
cigarette smoking behaviours. Cigarette smoking has been related to long term adverse chronic
health conditions such as: cardiovascular disease, fatal pulmonary conditions such as lung cancer
and high susceptibility to give birth to low-birth weight infants by pregnant women. Second hand
smoking has also been associated with complications such as sudden infant death syndrome.
Additionally, the WHO (2019), also denotes the economical and familial impacts caused as a
result of long smoking habits. Not only do the chronically damaging adverse health
consequences of cigarette pave the way for extensive financial expenditures, the addictive nature
of the same also compels individuals to prioritize their monetary activity on cigarette acquisition
rather than the fulfilment of familial needs. Thus, the aforementioned global details by the WHO
Chapter 2: Literature Review
2.1. Introduction
This chapter will hence elaborately and extensively review and review current clinical
and evidence-based research exploring the context of smoking behaviour, smoking cessation,
associated health consequences and mental health outcomes across the global context as well as
specifically within the UK population.
2.2. Health Effects of Smoking and associated perceptions
At present, as estimated by the World Health Organization, (WHO, 2019), one of the
most damaging and challenging issues impacting the world is the ‘tobacco epidemic’. According
to the findings by the WHO (2019), approximately 8 million individuals across the globe are
inflicted as a result of prolonged exposure to tobacco smoke or engagement in associated
detrimental lifestyle habits such as cigarette smoking. Of these, as denoted by the WHO (2019),
approximately 1.2 million and 7 million deaths have been reported as a result of passive or direct
cigarette smoking behaviours. Cigarette smoking has been related to long term adverse chronic
health conditions such as: cardiovascular disease, fatal pulmonary conditions such as lung cancer
and high susceptibility to give birth to low-birth weight infants by pregnant women. Second hand
smoking has also been associated with complications such as sudden infant death syndrome.
Additionally, the WHO (2019), also denotes the economical and familial impacts caused as a
result of long smoking habits. Not only do the chronically damaging adverse health
consequences of cigarette pave the way for extensive financial expenditures, the addictive nature
of the same also compels individuals to prioritize their monetary activity on cigarette acquisition
rather than the fulfilment of familial needs. Thus, the aforementioned global details by the WHO
12SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
(2019), provide an interesting and comprehensive insights into the alarming global prevalence of
cigarette smoking, its related health consequences and the economic burdens inflicted by the
same. Such information thus demonstrates the immediate need to establish smoking cessation
policies and programs for the purpose of ensuring positive health outcomes across the global
population - a key area of intervention addressed by the chosen research question. However,
despite the global acceptance of evidence provided by international organizations like the WHO
(2019), the lack of inclusion of any clinical primary research followed by demonstrating an
insight into the global nature of issue, rather than specifying mental health consequences with
respect to the United Kingdom (UK) context, prompts the need to review additional evidence-
based information.
The cross sectional research by Lonergan et al. (2017), provides an interesting insight
into the prevalence of cigarette smoking behaviours, a detailed outlining of the chronic diseases
associated with the same as well as perceptions concerning these harms within the UK context.
According to Lonergan et al. (2017), cigarette smoking in addition to cardiovascular diseases, is
associated with fatal health complications such as cancers of the mouth, lung, renal, stomach,
haematological, pharyngeal, throat, breast and blood. Additionally, cigarette smoking was also
evidenced by Lonergan et al. (2017), to cause health issues such as asthma, emphysema,
hypertension, coronary artery disease, bronchitis, tuberculosis, and shrinkage of the mouth,
discoloration of gums and teeth as well as cardiovascular failure. Interestingly, the cross
sectional study by Lonergan et al. (2017), demonstrated the prevalence of cigarette smoking
across approximately two-third of UK children and adolescents at the age of 18 years or below.
While approximately 80% of children from two UK schools aged 11 to 17 years reported
knowledge and awareness on consequences of lung cancer due to cigarette smoking, the findings
(2019), provide an interesting and comprehensive insights into the alarming global prevalence of
cigarette smoking, its related health consequences and the economic burdens inflicted by the
same. Such information thus demonstrates the immediate need to establish smoking cessation
policies and programs for the purpose of ensuring positive health outcomes across the global
population - a key area of intervention addressed by the chosen research question. However,
despite the global acceptance of evidence provided by international organizations like the WHO
(2019), the lack of inclusion of any clinical primary research followed by demonstrating an
insight into the global nature of issue, rather than specifying mental health consequences with
respect to the United Kingdom (UK) context, prompts the need to review additional evidence-
based information.
The cross sectional research by Lonergan et al. (2017), provides an interesting insight
into the prevalence of cigarette smoking behaviours, a detailed outlining of the chronic diseases
associated with the same as well as perceptions concerning these harms within the UK context.
According to Lonergan et al. (2017), cigarette smoking in addition to cardiovascular diseases, is
associated with fatal health complications such as cancers of the mouth, lung, renal, stomach,
haematological, pharyngeal, throat, breast and blood. Additionally, cigarette smoking was also
evidenced by Lonergan et al. (2017), to cause health issues such as asthma, emphysema,
hypertension, coronary artery disease, bronchitis, tuberculosis, and shrinkage of the mouth,
discoloration of gums and teeth as well as cardiovascular failure. Interestingly, the cross
sectional study by Lonergan et al. (2017), demonstrated the prevalence of cigarette smoking
across approximately two-third of UK children and adolescents at the age of 18 years or below.
While approximately 80% of children from two UK schools aged 11 to 17 years reported
knowledge and awareness on consequences of lung cancer due to cigarette smoking, the findings
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
from the authors also highlighted inadequate levels of knowledge and awareness on additional
minor health consequences of cigarette smoking. The lack of any randomization within the
methodological strategies along with inclusion of cross-sectional data collection methods raises
concerns regarding the above study’s validity and significance (Mohajan 2017). Despite the
study’s advantageous inclusion of research within the UK context, the lack of prioritization of
mental health patients along with mental health issues associated with smoking and smoking
cessation thus demonstrates the need for further reviewing of relevant articles as mentioned in
the succeeding sections.
2.3. Prevalence and mental health outcomes of smoking in the United Kingdom
According to Public Health England (2016), detrimental lifestyle behaviours such as
cigarette smoking, is a preventable and harmful causative factors of healthcare disparities and
high rates of mortality and morbidity across the UK population as well as a significant
contributor of differences in the rates of life expectancy observed between economically
privileged and underprivileged communities in the nation. The findings by Public Health
England also demonstrate the prevalence of death due to smoking-associated conditions across
approximately 78, 200 individuals within the UK. It has further been postulated that smoking is
one of the strongest contributors to decreased rates of life expectancy across mental health
patients with mental health issues like personality disorders (18 years for females and males),
depression (7 years for females and 11 years for males respectively), alcohol misuse (10.8 years
for females and 17.1 years for males) and opioid misuse associated disorders (17.3 years for
females and 9.0 years for males). The key systematic reviews included in this public health
report by Public Health England (2016), further provide key research insights demonstrating the
positive association between negative mental health outcome and prolonged cigarette smoking
from the authors also highlighted inadequate levels of knowledge and awareness on additional
minor health consequences of cigarette smoking. The lack of any randomization within the
methodological strategies along with inclusion of cross-sectional data collection methods raises
concerns regarding the above study’s validity and significance (Mohajan 2017). Despite the
study’s advantageous inclusion of research within the UK context, the lack of prioritization of
mental health patients along with mental health issues associated with smoking and smoking
cessation thus demonstrates the need for further reviewing of relevant articles as mentioned in
the succeeding sections.
2.3. Prevalence and mental health outcomes of smoking in the United Kingdom
According to Public Health England (2016), detrimental lifestyle behaviours such as
cigarette smoking, is a preventable and harmful causative factors of healthcare disparities and
high rates of mortality and morbidity across the UK population as well as a significant
contributor of differences in the rates of life expectancy observed between economically
privileged and underprivileged communities in the nation. The findings by Public Health
England also demonstrate the prevalence of death due to smoking-associated conditions across
approximately 78, 200 individuals within the UK. It has further been postulated that smoking is
one of the strongest contributors to decreased rates of life expectancy across mental health
patients with mental health issues like personality disorders (18 years for females and males),
depression (7 years for females and 11 years for males respectively), alcohol misuse (10.8 years
for females and 17.1 years for males) and opioid misuse associated disorders (17.3 years for
females and 9.0 years for males). The key systematic reviews included in this public health
report by Public Health England (2016), further provide key research insights demonstrating the
positive association between negative mental health outcome and prolonged cigarette smoking
14SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
behaviors across the UK population. Indeed, smoking behaviors have been observed to facilitate
one’s acquisition of mental health issues with a positive relationship between the amount of
smoking and the frequency and severity of mental health symptoms of anxiety and depression
associated mental health conditions. The systematic reviews incorporated by Public Health
England (2016), also postulate that individuals with mental health conditions have a high risk of
physiological co-morbidities which in turn, increases their susceptibility of acquiring cigarette
smoking behaviours. Additionally, individuals in the UK, with both acute mental health issues as
well as cigarette smoking behaviours, have been evidenced to experience death a decade or two
decades earlier than those without such mental health conditions or cigarette smoking. Mental
health patients engaging in chronic smoking also demonstrate high rates of morbidity and
mortality due to their high risk of acquiring adverse physiological conditions such as respiratory
or cardiovascular ailments. Thus, as evidenced from the findings, the paper by Public Health
England (2016), served to be extensively useful in terms of providing specification information
on not only the mental health issues associated with mental health patients engaging in smoking
but also concerning the current state health issues across the UK population. However, the
inclusion of only a literature review as the primary methodology instead of primary research
demonstrates issues in validity and applicability in terms of publication bias. There is thus a need
to procure not only primary research but also data relevant to the UK population with respect to
the health impacts of smoking on individuals with any relevant health condition (Cypress 2017).
The national level observational study performed by Mangera et al. (2017), aimed to
identify the prevalence of smoking across hospital admissions in the UK. The research
comprised of an online survey formulated by the British Thoracic Society which was then used
by UK-based hospitals to record patient documentation information, case study notes, emergency
behaviors across the UK population. Indeed, smoking behaviors have been observed to facilitate
one’s acquisition of mental health issues with a positive relationship between the amount of
smoking and the frequency and severity of mental health symptoms of anxiety and depression
associated mental health conditions. The systematic reviews incorporated by Public Health
England (2016), also postulate that individuals with mental health conditions have a high risk of
physiological co-morbidities which in turn, increases their susceptibility of acquiring cigarette
smoking behaviours. Additionally, individuals in the UK, with both acute mental health issues as
well as cigarette smoking behaviours, have been evidenced to experience death a decade or two
decades earlier than those without such mental health conditions or cigarette smoking. Mental
health patients engaging in chronic smoking also demonstrate high rates of morbidity and
mortality due to their high risk of acquiring adverse physiological conditions such as respiratory
or cardiovascular ailments. Thus, as evidenced from the findings, the paper by Public Health
England (2016), served to be extensively useful in terms of providing specification information
on not only the mental health issues associated with mental health patients engaging in smoking
but also concerning the current state health issues across the UK population. However, the
inclusion of only a literature review as the primary methodology instead of primary research
demonstrates issues in validity and applicability in terms of publication bias. There is thus a need
to procure not only primary research but also data relevant to the UK population with respect to
the health impacts of smoking on individuals with any relevant health condition (Cypress 2017).
The national level observational study performed by Mangera et al. (2017), aimed to
identify the prevalence of smoking across hospital admissions in the UK. The research
comprised of an online survey formulated by the British Thoracic Society which was then used
by UK-based hospitals to record patient documentation information, case study notes, emergency
15SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
and elective based admissions selected randomly. Of the total 14, 750 records of patient details
submitted by a total of 146 participating healthcare institutions, the total prevalence rate of
smoking was estimated to be 73% while the prevalence rate of smoking across hospital
admissions were evidenced to be 23% in female patients and 28% in male patients – a finding
grossly higher than the mean national UK estimate of 19% (p < 0.0001). The highest reported
smoking prevalence was interestingly reported to be across patients aged 45 years or above
(42%). Higher rates of smoking prevalence was also observed in patients with respiratory
conditions (30%) as compared to alternative surgical and medical departments. Such findings
can be well related to the high risk of smoking and physiological morbidities like pulmonary and
cardiovascular diseases reported by both Public Health England (2016) and WHO (2019), and
thus further highlights the chronic consequences of smoking and the immediate need to assess
the impact of smoking cessation policies as per the identified clinical research question. While
these findings do not outline smoking behaviours in mental health patients, the reported
association between smoking and pulmonary conditions imply that the possibility of an
associated mental health issue cannot be fully overlooked.
Lastly, it was reported by Mangera et al. (2017), that out of the total reported 2716
smokers within the acquired survey data, 28% received medical interventions while 6% were
administered with institutional-based smoking cessation treatments. Thus, the findings of this
research prove to be a useful resource for the supplementing the given research question since it
demonstrates the high prevalence of smoking not just within the UK population but specifically
across patients admitted in healthcare institutions, which were largely missing in national public
health data. However, the lack of findings concerning the prevalence of smoking behaviors
specifically in the mental health ward of healthcare organizations further demonstrate how
and elective based admissions selected randomly. Of the total 14, 750 records of patient details
submitted by a total of 146 participating healthcare institutions, the total prevalence rate of
smoking was estimated to be 73% while the prevalence rate of smoking across hospital
admissions were evidenced to be 23% in female patients and 28% in male patients – a finding
grossly higher than the mean national UK estimate of 19% (p < 0.0001). The highest reported
smoking prevalence was interestingly reported to be across patients aged 45 years or above
(42%). Higher rates of smoking prevalence was also observed in patients with respiratory
conditions (30%) as compared to alternative surgical and medical departments. Such findings
can be well related to the high risk of smoking and physiological morbidities like pulmonary and
cardiovascular diseases reported by both Public Health England (2016) and WHO (2019), and
thus further highlights the chronic consequences of smoking and the immediate need to assess
the impact of smoking cessation policies as per the identified clinical research question. While
these findings do not outline smoking behaviours in mental health patients, the reported
association between smoking and pulmonary conditions imply that the possibility of an
associated mental health issue cannot be fully overlooked.
Lastly, it was reported by Mangera et al. (2017), that out of the total reported 2716
smokers within the acquired survey data, 28% received medical interventions while 6% were
administered with institutional-based smoking cessation treatments. Thus, the findings of this
research prove to be a useful resource for the supplementing the given research question since it
demonstrates the high prevalence of smoking not just within the UK population but specifically
across patients admitted in healthcare institutions, which were largely missing in national public
health data. However, the lack of findings concerning the prevalence of smoking behaviors
specifically in the mental health ward of healthcare organizations further demonstrate how
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
16SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
inadequately explored this field of research is, as per the clinical question. Additionally the
reliance of only survey and administrative data as the key research methodologies instead of
randomized primary data further raise the risk of bias and thus the need to conduct further studies
concerning the associated clinical research question (Nardi 2018).
With respect to the above however, the cross sectional research by Plurphanswat,
Kaestner and Rodu (2017), provides an interesting primary research based insight into the
relationship between smoking and mental health of individuals – which was largely overlooked
in the data by Public Health England (2016). The investigation comprised of evaluating the
mental health impact of smoking via evaluation of adults aged 18 years and above in the United
States via the usage of 2000-2010 Behavioural Risk Factor Surveillance System. The findings
reported that prolonged engagement in smoking caused an increment of approximately 2 weeks
of experiencing mental health associated symptoms within one month, especially in those
individuals with acute mental health issues. While the cross sectional study by Plurphanswat,
Kaestner and Rodu (2017) do not specify mental health outcomes of cigarette smoking across the
UK population, the identified relationship between mental health outcomes and smoking in
individuals with acute mental health issues formulates the rationale underlying the need to
explore the effect of smoking cessation policies, with respect to the identified research question.
2.4. Health Effects of Smoking Cessation
In addition to the evidenced association between smoking and health consequences, the
positive health outcomes of smoking cessation further necessitate the need to research on the
mental health effects of the same with respect to mental health patients which can then direct
future policy implications in the UK (Forman et al. 2017). With this respect, the review by
Harris, Zopey and Friedman (2016), aimed to expound upon the metabolic health impacts of
inadequately explored this field of research is, as per the clinical question. Additionally the
reliance of only survey and administrative data as the key research methodologies instead of
randomized primary data further raise the risk of bias and thus the need to conduct further studies
concerning the associated clinical research question (Nardi 2018).
With respect to the above however, the cross sectional research by Plurphanswat,
Kaestner and Rodu (2017), provides an interesting primary research based insight into the
relationship between smoking and mental health of individuals – which was largely overlooked
in the data by Public Health England (2016). The investigation comprised of evaluating the
mental health impact of smoking via evaluation of adults aged 18 years and above in the United
States via the usage of 2000-2010 Behavioural Risk Factor Surveillance System. The findings
reported that prolonged engagement in smoking caused an increment of approximately 2 weeks
of experiencing mental health associated symptoms within one month, especially in those
individuals with acute mental health issues. While the cross sectional study by Plurphanswat,
Kaestner and Rodu (2017) do not specify mental health outcomes of cigarette smoking across the
UK population, the identified relationship between mental health outcomes and smoking in
individuals with acute mental health issues formulates the rationale underlying the need to
explore the effect of smoking cessation policies, with respect to the identified research question.
2.4. Health Effects of Smoking Cessation
In addition to the evidenced association between smoking and health consequences, the
positive health outcomes of smoking cessation further necessitate the need to research on the
mental health effects of the same with respect to mental health patients which can then direct
future policy implications in the UK (Forman et al. 2017). With this respect, the review by
Harris, Zopey and Friedman (2016), aimed to expound upon the metabolic health impacts of
17SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
smoking cessation. An overall direct association between smoking cessation and anthropometric
measurements, that is, an increased Body Mass Index have been evidenced. Such mechanisms
has been postulated to be largely due to increments in insulin resistance as a result of smoking
cessation. It is prevalent to find post cessation reports of weight gain by smokers engaging in
corrective interventions which in turn, serves as a key reason for lack of motivation to participate
in similar treatment. Such metabolic issues are largely due to nicotine’s ability to suppress one’s
appetite which in turn, encourages increased rates of hunger, food intake and weight gain in
individuals engaging in smoking cessation. Nicotine demonstrates metabolic and biochemical
effects in the form of suppression of the activities of protein kinase as well as lipolysis which in
turn, restricts the delivery of free fatty acids to the muscular tissues. Thus, such mechanisms are
largely halted during smoking cessation which in turn causes insulin resistance and weight gain
across participants. While there remains no certified or standardized weight loss programs which
may be helpful in reducing post smoking cessation weight gain. However, the review by Harris,
Zopey and Friedman (2016), demonstrates the benefits of a long term, personalized weight loss
program with individualized motivational and weight loss goals in assisting individuals to
regulate weight gain and experience positive mental health outcomes of empowerment in
individuals experiencing post smoking cessation weight gain. While these findings do not bear
direct resemblance to the identified clinical research question assessing smoking cessation and
mental health outcomes in patients with mental health issues, the review by Harris, Zopey and
Friedman (2016), provides a comprehensive insight into the biochemical and physiological
impacts of smoking cessation and their indirect impacts on motivation which in turn, can be used
to understand the outcomes of the same on patients with mental health conditions.
smoking cessation. An overall direct association between smoking cessation and anthropometric
measurements, that is, an increased Body Mass Index have been evidenced. Such mechanisms
has been postulated to be largely due to increments in insulin resistance as a result of smoking
cessation. It is prevalent to find post cessation reports of weight gain by smokers engaging in
corrective interventions which in turn, serves as a key reason for lack of motivation to participate
in similar treatment. Such metabolic issues are largely due to nicotine’s ability to suppress one’s
appetite which in turn, encourages increased rates of hunger, food intake and weight gain in
individuals engaging in smoking cessation. Nicotine demonstrates metabolic and biochemical
effects in the form of suppression of the activities of protein kinase as well as lipolysis which in
turn, restricts the delivery of free fatty acids to the muscular tissues. Thus, such mechanisms are
largely halted during smoking cessation which in turn causes insulin resistance and weight gain
across participants. While there remains no certified or standardized weight loss programs which
may be helpful in reducing post smoking cessation weight gain. However, the review by Harris,
Zopey and Friedman (2016), demonstrates the benefits of a long term, personalized weight loss
program with individualized motivational and weight loss goals in assisting individuals to
regulate weight gain and experience positive mental health outcomes of empowerment in
individuals experiencing post smoking cessation weight gain. While these findings do not bear
direct resemblance to the identified clinical research question assessing smoking cessation and
mental health outcomes in patients with mental health issues, the review by Harris, Zopey and
Friedman (2016), provides a comprehensive insight into the biochemical and physiological
impacts of smoking cessation and their indirect impacts on motivation which in turn, can be used
to understand the outcomes of the same on patients with mental health conditions.
18SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
Smoking cessation and its related metabolic impacts have been largely associated with
regulation of inflammatory markers, associated oxidative stress and cardiovascular risks. With
this respect, the longitudinal cohort study by King et al. (2017) aimed to investigate the effects of
smoking cessation on the key inflammatory outcomes associated with the risk of cardiovascular
disease. Out of a total participant group of 1652 smokers, the study evaluated the independent
associations between the number of cigarette packets per year as well as amount of exhaled
carbon monoxide and inflammatory outcomes such as white blood cell count, C-reactive protein,
D-dimer fibrinogen, myeloperoxidase and ratio of F2 isoprostane: creatinine. Of these, 888
smokers participating in a supervised cessation intervention were also evaluated after one year
regarding the above inflammatory markers. The findings reported significant reductions in
inflammatory indicators such as white blood cell count, myeloperoxidase and ratio of
F2 isoprostane: creatinine after one year of smoking cessation (p < 0.001). While approximately
344 participants reported increases in insulin resistance (p < 0.02) and weight gain (p < 0.001)
after one year of cessation as compared to smokers, there were still decrements observed with
respect to white blood cell count, myeloperoxidase and ratio of F2 isoprostane: creatinine (p <
0.001). Such reductions in inflammatory outcomes are particularly useful since high levels of
oxidative stress and inflammation are largely associated with arterial stiffness, endothelial
damage and high risk of atherosclerotic damage. Despite the comprehensiveness of the results
with respect to the impact of smoking cessation the lack of randomization coupled with absence
of mental health impacts due to smoking cessation are key research limitations as per the
research question. However, considering the evidenced association between smoking,
physiological comorbidities and poor mental health outcomes thus render the findings by King et
al. (2017) useful with respect to the range of cardiovascular issues which may be reduced in
Smoking cessation and its related metabolic impacts have been largely associated with
regulation of inflammatory markers, associated oxidative stress and cardiovascular risks. With
this respect, the longitudinal cohort study by King et al. (2017) aimed to investigate the effects of
smoking cessation on the key inflammatory outcomes associated with the risk of cardiovascular
disease. Out of a total participant group of 1652 smokers, the study evaluated the independent
associations between the number of cigarette packets per year as well as amount of exhaled
carbon monoxide and inflammatory outcomes such as white blood cell count, C-reactive protein,
D-dimer fibrinogen, myeloperoxidase and ratio of F2 isoprostane: creatinine. Of these, 888
smokers participating in a supervised cessation intervention were also evaluated after one year
regarding the above inflammatory markers. The findings reported significant reductions in
inflammatory indicators such as white blood cell count, myeloperoxidase and ratio of
F2 isoprostane: creatinine after one year of smoking cessation (p < 0.001). While approximately
344 participants reported increases in insulin resistance (p < 0.02) and weight gain (p < 0.001)
after one year of cessation as compared to smokers, there were still decrements observed with
respect to white blood cell count, myeloperoxidase and ratio of F2 isoprostane: creatinine (p <
0.001). Such reductions in inflammatory outcomes are particularly useful since high levels of
oxidative stress and inflammation are largely associated with arterial stiffness, endothelial
damage and high risk of atherosclerotic damage. Despite the comprehensiveness of the results
with respect to the impact of smoking cessation the lack of randomization coupled with absence
of mental health impacts due to smoking cessation are key research limitations as per the
research question. However, considering the evidenced association between smoking,
physiological comorbidities and poor mental health outcomes thus render the findings by King et
al. (2017) useful with respect to the range of cardiovascular issues which may be reduced in
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
19SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
mental health patients due to smoking cessation which in turn can pave the way for improved
health and wellbeing.
In addition to the metabolic effects highlighted above, smoking cessation interventions
have also been evidenced to yield benefits in the form of improved rates of health literacy,
awareness and health associated knowledge in the participating smokers, especially when
delivered as a part of public health and community campaigns (Chang et al. 2017). Likewse, the
follow up study by Li et al. (2019), reported that a specialist smoking cessation intervention
specific for patients with acute mental health illness demonstrate greater cost effective outcomes
and no additional co-morbidity associated health expenditures as compared to standard smoking
cessation interventions across 526 acutely ill mental health patients in England, thus
demonstrating the economic benefits of this intervention.
2.5. Health Effects of Smoking Cessation in Mental Health Patients
According to Public Health England (2016), smoking cessations paves the way for a
range of beneficial health, social and economic effects in the individual these include:
improvements in life expectancy rates, physiological health outcomes, economical savings,
reduce reliance on medications, improve regulation of anxiety and depression symptoms,
increased motivation to participate in beneficial lifestyle interventions such as exercise and
decrements in terms of alcohol and substance abuse associated behaviors. Considering the
limited evidence on mental health based outcomes, this report however needs to be supplemented
with additional evidence based research.
With respect to the same, the experiment by Rademacher et al. (2016) aimed to examine
the impact of smoking cessation on the function of presynaptic dopamine across males with
addictive smoking behaviors. The authors obtained baseline 6-[18F]fluoro-L-DOPA (FDOPA)-
mental health patients due to smoking cessation which in turn can pave the way for improved
health and wellbeing.
In addition to the metabolic effects highlighted above, smoking cessation interventions
have also been evidenced to yield benefits in the form of improved rates of health literacy,
awareness and health associated knowledge in the participating smokers, especially when
delivered as a part of public health and community campaigns (Chang et al. 2017). Likewse, the
follow up study by Li et al. (2019), reported that a specialist smoking cessation intervention
specific for patients with acute mental health illness demonstrate greater cost effective outcomes
and no additional co-morbidity associated health expenditures as compared to standard smoking
cessation interventions across 526 acutely ill mental health patients in England, thus
demonstrating the economic benefits of this intervention.
2.5. Health Effects of Smoking Cessation in Mental Health Patients
According to Public Health England (2016), smoking cessations paves the way for a
range of beneficial health, social and economic effects in the individual these include:
improvements in life expectancy rates, physiological health outcomes, economical savings,
reduce reliance on medications, improve regulation of anxiety and depression symptoms,
increased motivation to participate in beneficial lifestyle interventions such as exercise and
decrements in terms of alcohol and substance abuse associated behaviors. Considering the
limited evidence on mental health based outcomes, this report however needs to be supplemented
with additional evidence based research.
With respect to the same, the experiment by Rademacher et al. (2016) aimed to examine
the impact of smoking cessation on the function of presynaptic dopamine across males with
addictive smoking behaviors. The authors obtained baseline 6-[18F]fluoro-L-DOPA (FDOPA)-
20SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
PET results across 30 nicotine dependent smokers and 15 smokers engaging in regular habits
after which, 15 participants who had undergone complete cessation for three months were
estimated in terms of levels of synthesis capacity of dopamine and brain turnover of traces of
dopamine. The findings reported a reduction of 15 to 20% of dopamine synthesis across smokers
in comparison to those who had successfully underwent smoking cessation. Such findings
demonstrate the low levels of dopamine neurotransmitter across smokers, the levels of which
improve as a result of cessation. Considering the evidenced association between dopamine
imbalances and mental health issues like depression, such findings demonstrate useful insights
into the usefulness of smoking cessation in ensuring positive mental outcomes in mental health
patients (Sharma et al. 2018). There is however, no mention of the effects of smoking cessation
with respect to any specific mental health issue or disorder – which can thus be considered as a
limitation.
The cohort study by Miyauchi et al. (2017) investigates the impact of smoking cessation
across patients hospitalized with acute mental health issues like schizophrenia. Baseline results
of 32 non-smokers and 38 smokers were acquired in terms of activity of the autonomic nervous
system, level of plasma cholesterol, drug therapy, body mass and scores of Global Assessment
were collected as well as after three years of smoking cessation. The findings reported high
levels of nervous system function and usage of anti-Parkinson drugs in smokers in comparison to
non-smokers. Further, three years of cessation in smoking also resulted in reduced rates of drug
consumption and activity of the sympathetic nervous system. Such findings demonstrate high
relevance to the given research question due to its ability to outline smoking cessation-associated
mental health impacts upon patients with acute mental health issues. The lack of inclusion of a
PET results across 30 nicotine dependent smokers and 15 smokers engaging in regular habits
after which, 15 participants who had undergone complete cessation for three months were
estimated in terms of levels of synthesis capacity of dopamine and brain turnover of traces of
dopamine. The findings reported a reduction of 15 to 20% of dopamine synthesis across smokers
in comparison to those who had successfully underwent smoking cessation. Such findings
demonstrate the low levels of dopamine neurotransmitter across smokers, the levels of which
improve as a result of cessation. Considering the evidenced association between dopamine
imbalances and mental health issues like depression, such findings demonstrate useful insights
into the usefulness of smoking cessation in ensuring positive mental outcomes in mental health
patients (Sharma et al. 2018). There is however, no mention of the effects of smoking cessation
with respect to any specific mental health issue or disorder – which can thus be considered as a
limitation.
The cohort study by Miyauchi et al. (2017) investigates the impact of smoking cessation
across patients hospitalized with acute mental health issues like schizophrenia. Baseline results
of 32 non-smokers and 38 smokers were acquired in terms of activity of the autonomic nervous
system, level of plasma cholesterol, drug therapy, body mass and scores of Global Assessment
were collected as well as after three years of smoking cessation. The findings reported high
levels of nervous system function and usage of anti-Parkinson drugs in smokers in comparison to
non-smokers. Further, three years of cessation in smoking also resulted in reduced rates of drug
consumption and activity of the sympathetic nervous system. Such findings demonstrate high
relevance to the given research question due to its ability to outline smoking cessation-associated
mental health impacts upon patients with acute mental health issues. The lack of inclusion of a
21SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
UK based cohort demonstrate the significant research limitation and thus forms the rationale of
the identified research question of this thesis.
2.6. Theoretical Framework
As a part of the Five Year Forward View (NHS 2014) a number of care models have
been established and implemented for the purpose of assisting acutely ill patients admitted across
the mental health setting of the United Kingdom. The ‘acute care collaborations’ model signify
the importance of establishing collaboration across all local healthcare organizations for the
purpose of improvement of clinical and financial efficiency in patient management. The
‘multispecialty community providers’ model is relevant for patients with mental illnesses as well
as a range of physiological co-morbidities and thus comprises of integration of specialist care
services with community health organizations for improved quality of life. The ‘integrated
primary and acute are systems’ model aims to provide comprehensive mental healthcare to the
acutely ill patient via integration of general practitioner, mental health services, community care
services and primary care services such as hospitals or healthcare organizations. Additionally,
authors Sharma, Khubchandani and Nahar (2017) postulate the usage of a multi-theory model
(MTM) as the key health behaviour change model for the purpose of providing assistance to
mental health patients in successful smoking cessation. According to the MTM, the first step in
successful smoking cessation is to implement ‘participatory dialogue’ – a form of two way
communication in which the healthcare volunteer delivering the intervention educates and
attempts to make the client understand the benefits of smoking cessation as being worth the
harms and costs of adverse effects of withdrawal. The second step in smoking cessation as per
the MTM is to enhance the client’s ‘behavioural confidence’ by establishing simple, gradual
goals of quitting such as: abstaining from smoking for a week or praising the client for being
UK based cohort demonstrate the significant research limitation and thus forms the rationale of
the identified research question of this thesis.
2.6. Theoretical Framework
As a part of the Five Year Forward View (NHS 2014) a number of care models have
been established and implemented for the purpose of assisting acutely ill patients admitted across
the mental health setting of the United Kingdom. The ‘acute care collaborations’ model signify
the importance of establishing collaboration across all local healthcare organizations for the
purpose of improvement of clinical and financial efficiency in patient management. The
‘multispecialty community providers’ model is relevant for patients with mental illnesses as well
as a range of physiological co-morbidities and thus comprises of integration of specialist care
services with community health organizations for improved quality of life. The ‘integrated
primary and acute are systems’ model aims to provide comprehensive mental healthcare to the
acutely ill patient via integration of general practitioner, mental health services, community care
services and primary care services such as hospitals or healthcare organizations. Additionally,
authors Sharma, Khubchandani and Nahar (2017) postulate the usage of a multi-theory model
(MTM) as the key health behaviour change model for the purpose of providing assistance to
mental health patients in successful smoking cessation. According to the MTM, the first step in
successful smoking cessation is to implement ‘participatory dialogue’ – a form of two way
communication in which the healthcare volunteer delivering the intervention educates and
attempts to make the client understand the benefits of smoking cessation as being worth the
harms and costs of adverse effects of withdrawal. The second step in smoking cessation as per
the MTM is to enhance the client’s ‘behavioural confidence’ by establishing simple, gradual
goals of quitting such as: abstaining from smoking for a week or praising the client for being
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
22SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
able to engage in all daily life activities without feeling distressed or the need to smoke. The
third construct useful to bring about a behaviour change of smoking cessation is associated with
‘physical environment’ comprising of: replacing smoking breaks with other activities, removing
cigarettes from one’s home or educating families and friends on the importance of keeping the
client motivated.
2.7. Research Limitations and Implications
The above review thus successfully integrates current evidence based research and
clinical studies demonstrating relevant data, concepts and insights into the identified research
question, that is, an exploration of the mental health outcomes observed due to smoking
cessation across mental health patients admitted across UK mental health settings. A range of
public health reports as well as academic, scholarly and per reviewed literature were acquired
and discussed in this chapter. While both national as well as global level public health reports
along with academic insights (Public Health England 2016; WHO 2019), demonstrate useful
insights into the prevalence and impacts of smoking upon the international as well as UK context
– there is a lack of specific evidence-based information with respect to mental health patients
with acute illnesses across the UK. Thus, this forms a key rationale underlying the formulation
and implementation of systematic methodologies pertaining to the identified research question.
Considering the high rates of smoking and associated mental health complications across
the UK, the findings of this research will serve to be useful sources of information which both
public and private health organizations can use prior to and during implementation of smoking
cessation interventions across patients with mental health outcomes (Sheals et al. 2016).
Additionally, the widespread, nationwide prevalence of the issue of smoking and associated
able to engage in all daily life activities without feeling distressed or the need to smoke. The
third construct useful to bring about a behaviour change of smoking cessation is associated with
‘physical environment’ comprising of: replacing smoking breaks with other activities, removing
cigarettes from one’s home or educating families and friends on the importance of keeping the
client motivated.
2.7. Research Limitations and Implications
The above review thus successfully integrates current evidence based research and
clinical studies demonstrating relevant data, concepts and insights into the identified research
question, that is, an exploration of the mental health outcomes observed due to smoking
cessation across mental health patients admitted across UK mental health settings. A range of
public health reports as well as academic, scholarly and per reviewed literature were acquired
and discussed in this chapter. While both national as well as global level public health reports
along with academic insights (Public Health England 2016; WHO 2019), demonstrate useful
insights into the prevalence and impacts of smoking upon the international as well as UK context
– there is a lack of specific evidence-based information with respect to mental health patients
with acute illnesses across the UK. Thus, this forms a key rationale underlying the formulation
and implementation of systematic methodologies pertaining to the identified research question.
Considering the high rates of smoking and associated mental health complications across
the UK, the findings of this research will serve to be useful sources of information which both
public and private health organizations can use prior to and during implementation of smoking
cessation interventions across patients with mental health outcomes (Sheals et al. 2016).
Additionally, the widespread, nationwide prevalence of the issue of smoking and associated

23SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
mental and physical health outcomes necessitate the formulation of comprehensive and robust
public health policies and programs. Thus, the findings of this research will also prove to be
useful resources for governmental bodies on development of relevant smoking cessation and
community mental health protocols (Garey et al. 2020).
mental and physical health outcomes necessitate the formulation of comprehensive and robust
public health policies and programs. Thus, the findings of this research will also prove to be
useful resources for governmental bodies on development of relevant smoking cessation and
community mental health protocols (Garey et al. 2020).
24SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
Chapter 3: Methodology
3.1. Literature Review Findings
A prevalent observation was the absence of primary data suited specifically to the mental
health settings of the United Kingdom and across patients with acute mental health illnesses.
Additionally, some of the key limitations which were observed included: possibilities of bias and
social desirability and lack of implementation of studies across UK mental health settings as well
as inclusion of participants with acute mental health illnesses. Thus the lack of sufficient studies
specific to the mental health settings of UK and acute mental health illnesses formed the
rationale behind formulation of the above identified research aim and the relevant clinical
question to be answered. This chapter aims to outline the key methodological components which
were followed for the purpose of collecting evidence based articles relevant to the identified
research aim, that is: to critically review the effect of smoking cessation on mental health and
wellbeing of patients with acute mental illness across mental health settings in the United
Kingdom.
3.2. Chosen Methodology: Systematic Review
A systematic review is a form of qualitative research methodology which is characterized
by the systematic collection of either quantitative or qualitative studies followed critical and in-
depth appraisal of relevant findings in lieu of the research question (Yardley 2017). A systematic
review has been evidenced to be more efficacious as compared to a literature review due to the
former’s inclusion of valid academic, peer reviewed and scholarly research as findings in
comparison to the possibility of including unpublished, grey literature in the latter (Cook et al.
2016). Additionally, in comparison to quantitative methodologies, systematic reviews pave the
Chapter 3: Methodology
3.1. Literature Review Findings
A prevalent observation was the absence of primary data suited specifically to the mental
health settings of the United Kingdom and across patients with acute mental health illnesses.
Additionally, some of the key limitations which were observed included: possibilities of bias and
social desirability and lack of implementation of studies across UK mental health settings as well
as inclusion of participants with acute mental health illnesses. Thus the lack of sufficient studies
specific to the mental health settings of UK and acute mental health illnesses formed the
rationale behind formulation of the above identified research aim and the relevant clinical
question to be answered. This chapter aims to outline the key methodological components which
were followed for the purpose of collecting evidence based articles relevant to the identified
research aim, that is: to critically review the effect of smoking cessation on mental health and
wellbeing of patients with acute mental illness across mental health settings in the United
Kingdom.
3.2. Chosen Methodology: Systematic Review
A systematic review is a form of qualitative research methodology which is characterized
by the systematic collection of either quantitative or qualitative studies followed critical and in-
depth appraisal of relevant findings in lieu of the research question (Yardley 2017). A systematic
review has been evidenced to be more efficacious as compared to a literature review due to the
former’s inclusion of valid academic, peer reviewed and scholarly research as findings in
comparison to the possibility of including unpublished, grey literature in the latter (Cook et al.
2016). Additionally, in comparison to quantitative methodologies, systematic reviews pave the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
25SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
way for inclusion of a large amount of relevant data using more cost effective frameworks
(Bengtsson 2016). Indeed, considering the possibility of the huge financial and ethical
complications associated with implementing a quantitative study on smoking cessation impacts
across real life mental health settings, incorporation of qualitative research methodologies like
systematic reviews pose greater relevance.
However, systematic reviews are not devoid of certain limitations. One of the major
limitations include publication bias which comprises of author’s tendency to include only those
studies which demonstrate findings positive to the proposed hypothesis. Additionally, the
inclusion of studies of poor result and methodological quality within systematic reviews are a
key limitation which may impact findings (Cypress 2017).
3.3. PICOT Question
The relevant search strategy key words and data collection frameworks for the systematic
review were generated by the given PICOT question: What is the effect of smoking cessation
on mental health symptoms and wellbeing of patients with acute mental illness across
mental health settings in the United Kingdom?
Population: (P): Adult patients with acute mental illnesses admitted in UK base mental
health settings.
Intervention (I): Interventions prioritized around cessation of smoking.
Comparison (C): Absence of smoking cessation
Outcomes (O): Reduced severity and frequency of mental health symptoms, improved
sense of quality of life and wellbeing.
Time (T): A minimum of 3 months or more.
way for inclusion of a large amount of relevant data using more cost effective frameworks
(Bengtsson 2016). Indeed, considering the possibility of the huge financial and ethical
complications associated with implementing a quantitative study on smoking cessation impacts
across real life mental health settings, incorporation of qualitative research methodologies like
systematic reviews pose greater relevance.
However, systematic reviews are not devoid of certain limitations. One of the major
limitations include publication bias which comprises of author’s tendency to include only those
studies which demonstrate findings positive to the proposed hypothesis. Additionally, the
inclusion of studies of poor result and methodological quality within systematic reviews are a
key limitation which may impact findings (Cypress 2017).
3.3. PICOT Question
The relevant search strategy key words and data collection frameworks for the systematic
review were generated by the given PICOT question: What is the effect of smoking cessation
on mental health symptoms and wellbeing of patients with acute mental illness across
mental health settings in the United Kingdom?
Population: (P): Adult patients with acute mental illnesses admitted in UK base mental
health settings.
Intervention (I): Interventions prioritized around cessation of smoking.
Comparison (C): Absence of smoking cessation
Outcomes (O): Reduced severity and frequency of mental health symptoms, improved
sense of quality of life and wellbeing.
Time (T): A minimum of 3 months or more.
26SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
3.4. Search Strategy
For the purpose of data collection, an electronic search strategy was implemented across
databases such as PubMed, CINAHL, Cochrane and Medline due to their extensive repertoire of
research pertaining to healthcare, biology, medicine and nursing (Gough and Richardson 2018).
The key search terms which were used along with relevant Boolean operators, truncation and
wildcards include: ‘effects’, ‘smoking cessation’, ‘acute mental illnesses’, ‘United Kingdom’ and
‘mental health units’. Limiters of ‘English’ and ‘peer reviewed’ were place to ensure
procurement of valid, peer reviewed articles written in English language (McGowan et al.
2016).Full text articles with relevance to the key words and inclusion/exclusion criteria,
highlighted below, were selected for further screening as per the PRISMA flow chart and table
(Figure A, Appendix) (Grewal, Kataria and Dhawan 2016). A detailed insight on the key search
terms and results have been outlined in a PRISMA table as well as attached search histories
(Appendix).
3.5. Inclusion and Exclusion Criteria
3.5.1. Inclusion Criteria
Study participants comprising of adult patients with acute mental illnesses admitted in
mental health settings of UK based healthcare organizations
Studies with interventions prioritizing smoking cessation.
Studied with methodologies like systematic reviews, qualitative studies, randomized
controlled trials, cross sectional or observational studies.
Studies with interventions implemented for a duration of 3 months or more
Studies published since the last 7 years (2013 to 2020).
3.4. Search Strategy
For the purpose of data collection, an electronic search strategy was implemented across
databases such as PubMed, CINAHL, Cochrane and Medline due to their extensive repertoire of
research pertaining to healthcare, biology, medicine and nursing (Gough and Richardson 2018).
The key search terms which were used along with relevant Boolean operators, truncation and
wildcards include: ‘effects’, ‘smoking cessation’, ‘acute mental illnesses’, ‘United Kingdom’ and
‘mental health units’. Limiters of ‘English’ and ‘peer reviewed’ were place to ensure
procurement of valid, peer reviewed articles written in English language (McGowan et al.
2016).Full text articles with relevance to the key words and inclusion/exclusion criteria,
highlighted below, were selected for further screening as per the PRISMA flow chart and table
(Figure A, Appendix) (Grewal, Kataria and Dhawan 2016). A detailed insight on the key search
terms and results have been outlined in a PRISMA table as well as attached search histories
(Appendix).
3.5. Inclusion and Exclusion Criteria
3.5.1. Inclusion Criteria
Study participants comprising of adult patients with acute mental illnesses admitted in
mental health settings of UK based healthcare organizations
Studies with interventions prioritizing smoking cessation.
Studied with methodologies like systematic reviews, qualitative studies, randomized
controlled trials, cross sectional or observational studies.
Studies with interventions implemented for a duration of 3 months or more
Studies published since the last 7 years (2013 to 2020).
27SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
3.5.2. Exclusion Criteria
Study participants comprising of paediatric and geriatric patients or adult patients without
acute mental illnesses or admitted in non-UK based mental healthcare settings.
Studies with interventions not associated with smoking cessation.
Newspaper reports, editorials, protocols or opinion articles.
Studies with interventions implemented less than 3 months.
Studies older than the last 7 years (2013 to 2020) (Appendix).
3.6. PRISMA Flow Diagram
The following PRISMA Flow chart (Figure A) demonstrate the key steps and search
results underlying the selection of 6 relevant evidence-based studies. These studies were selected
based on their relevance to the research question, the PICOT question and the associated key
words. A detailed insight of the search results in tabular form have also been outlined in a
PRISMA table (Appendix) (Tricco et al. 2016). As per the PRISMA Flow Chart (Figure A) and
Table (Appendix), the total number of article results after the initial search was 100 for Medline,
143 for PubMed, 160 for CINAHL and 183 for Cochrane. After removal of duplicates, a total of
450 articles were screened and evaluated for systematic review selection. A detailed insight on
the key search terms and results have been outlined in a PRISMA table as well as attached search
histories (Appendix).
3.5.2. Exclusion Criteria
Study participants comprising of paediatric and geriatric patients or adult patients without
acute mental illnesses or admitted in non-UK based mental healthcare settings.
Studies with interventions not associated with smoking cessation.
Newspaper reports, editorials, protocols or opinion articles.
Studies with interventions implemented less than 3 months.
Studies older than the last 7 years (2013 to 2020) (Appendix).
3.6. PRISMA Flow Diagram
The following PRISMA Flow chart (Figure A) demonstrate the key steps and search
results underlying the selection of 6 relevant evidence-based studies. These studies were selected
based on their relevance to the research question, the PICOT question and the associated key
words. A detailed insight of the search results in tabular form have also been outlined in a
PRISMA table (Appendix) (Tricco et al. 2016). As per the PRISMA Flow Chart (Figure A) and
Table (Appendix), the total number of article results after the initial search was 100 for Medline,
143 for PubMed, 160 for CINAHL and 183 for Cochrane. After removal of duplicates, a total of
450 articles were screened and evaluated for systematic review selection. A detailed insight on
the key search terms and results have been outlined in a PRISMA table as well as attached search
histories (Appendix).
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
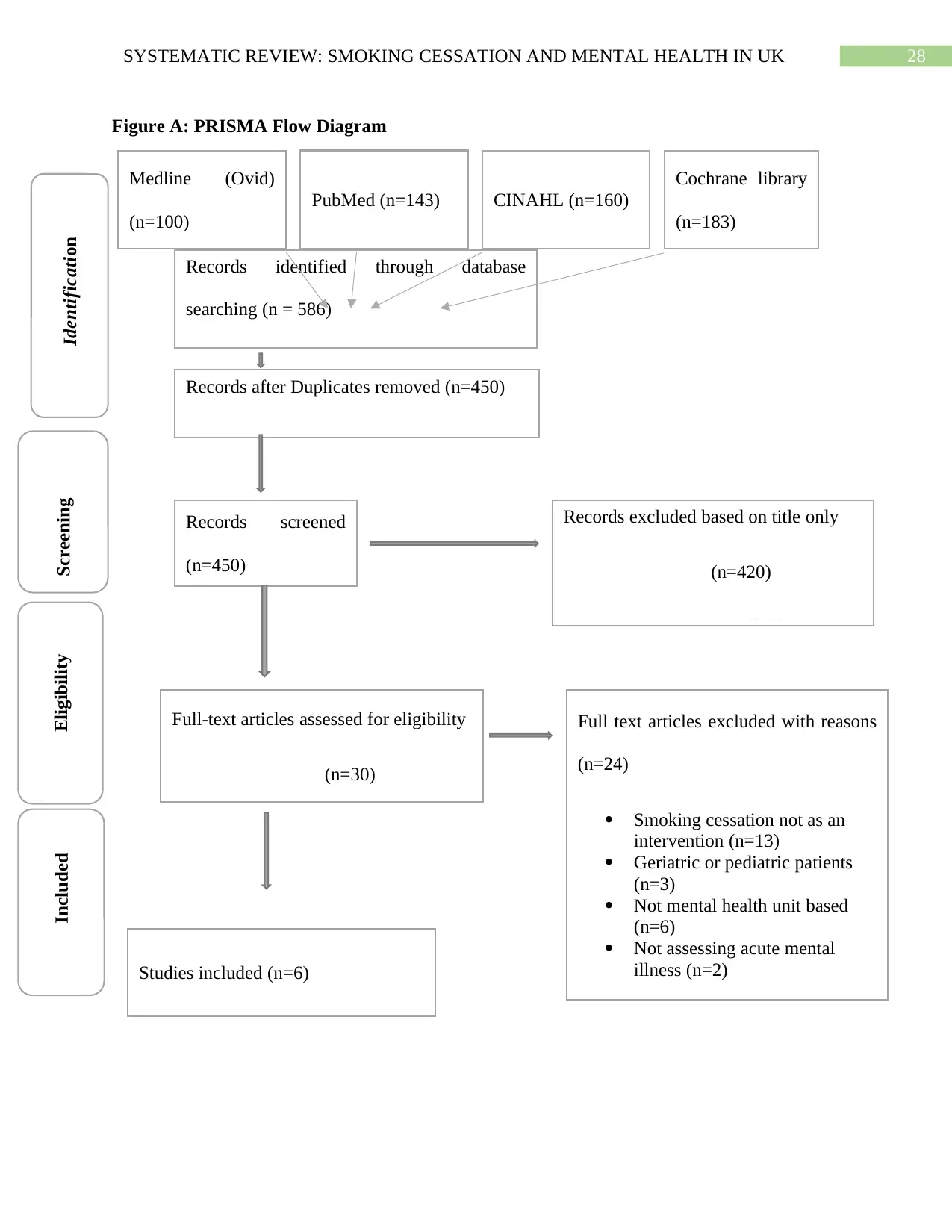
28SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
Figure A: PRISMA Flow Diagram
Records identified through database
searching (n = 586)
Studies included (n=6)
Records after Duplicates removed (n=450)
(n=453)
Records screened
(n=450)
Full text articles excluded with reasons
(n=24)
Smoking cessation not as an
intervention (n=13)
Geriatric or pediatric patients
(n=3)
Not mental health unit based
(n=6)
Not assessing acute mental
illness (n=2)
Full-text articles assessed for eligibility
(n=30)
Records excluded based on title only
(n=420)
Records excluded based on
IdentificationScreeningEligibilityIncluded
Medline (Ovid)
(n=100)
PubMed (n=143) CINAHL (n=160)
Cochrane library
(n=183)
Figure A: PRISMA Flow Diagram
Records identified through database
searching (n = 586)
Studies included (n=6)
Records after Duplicates removed (n=450)
(n=453)
Records screened
(n=450)
Full text articles excluded with reasons
(n=24)
Smoking cessation not as an
intervention (n=13)
Geriatric or pediatric patients
(n=3)
Not mental health unit based
(n=6)
Not assessing acute mental
illness (n=2)
Full-text articles assessed for eligibility
(n=30)
Records excluded based on title only
(n=420)
Records excluded based on
IdentificationScreeningEligibilityIncluded
Medline (Ovid)
(n=100)
PubMed (n=143) CINAHL (n=160)
Cochrane library
(n=183)
29SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
3.7. Critiquing the Articles
Each study was reviewed critically using relevant tools of critical appraisal and in
chronological order, from researches published at the earliest to those which have been published
in the most recent year. These have then been expounded upon in the succeeding chapters of
Results and Discussion in this thesis (Braun et al. 2019) (Appendix).
3.8. Research Validity
Academic, scholarly and peer reviewed articles were selected, and unpublished studies,
protocols and opinion articles were avoided due to the prevalence of higher validity,
significance, trustworthiness and rigor in the former (Morey et al. 2016). Additionally, each of
the selected studies were appraised critically using a relevant critical appraisal tool. The critical
appraisal tools developed by the Critical Appraisal Skills Program (CASP) proved to be useful in
this respect due to their renowned usage nationally as well as international usage along with
ability to appraisal a range of research methodologies and types (Quigley et al. 2019). Based on
the appraised results, all peer reviewed, academic and scholarly articles which were found to be
of moderate to high result and methodological quality as per the CASP tools were included
(Williams, Boylan and Nunan 2020).
3.7. Critiquing the Articles
Each study was reviewed critically using relevant tools of critical appraisal and in
chronological order, from researches published at the earliest to those which have been published
in the most recent year. These have then been expounded upon in the succeeding chapters of
Results and Discussion in this thesis (Braun et al. 2019) (Appendix).
3.8. Research Validity
Academic, scholarly and peer reviewed articles were selected, and unpublished studies,
protocols and opinion articles were avoided due to the prevalence of higher validity,
significance, trustworthiness and rigor in the former (Morey et al. 2016). Additionally, each of
the selected studies were appraised critically using a relevant critical appraisal tool. The critical
appraisal tools developed by the Critical Appraisal Skills Program (CASP) proved to be useful in
this respect due to their renowned usage nationally as well as international usage along with
ability to appraisal a range of research methodologies and types (Quigley et al. 2019). Based on
the appraised results, all peer reviewed, academic and scholarly articles which were found to be
of moderate to high result and methodological quality as per the CASP tools were included
(Williams, Boylan and Nunan 2020).
30SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
Chapter 4: Results
4.1. Introduction
This chapter expounds upon the key findings and observations appraised critically from
the selected research studies, using relevant methodological and appraisal frameworks.
4.2. Article 1: Dickens, Staniford and Long (2014)
The case control, survey research by Dickens, Staniford and Long (2014), assessed the
prevalence and outcomes of nicotine craving, nicotine dependence, previous attempts of
cessation, motivating factors for smoking as well as underlying quitting of smoking and the self-
efficiency of abstaining from smoking across mental health patients who were smokers and
admitted across a UK based mental healthcare setting. This experimental sample was compared
with a control sample comprising of staff working in the chosen mental health care settings who
identified themselves as smokers. Thus, a total of 100 participants, 50 belonging to each of the
experimental and control groups were assessed with respect to the above outcomes using
questionnaires like: the 10-point Contemplation Ladder, the 10 item Smoker Clinic
Questionnaire, single item valid questions of self-efficacy and nicotine cravings and 4 item
questions for nicotine dependence. Based on statistical methods of t-test using a significance
value of α = < 0.01, the results indicated greater levels of nicotine dependence and cravings
across the experimental group. Additionally, the results revealed that while health concerns were
the key motivators of smoking cessation across staff, patients demonstrated a greater likelihood
to smoke during times of stress and as a reliever of boredom, for the purpose of gaining pleasure
or enjoyment. These social, emotional and motivational outcomes in turn, also served as the key
Chapter 4: Results
4.1. Introduction
This chapter expounds upon the key findings and observations appraised critically from
the selected research studies, using relevant methodological and appraisal frameworks.
4.2. Article 1: Dickens, Staniford and Long (2014)
The case control, survey research by Dickens, Staniford and Long (2014), assessed the
prevalence and outcomes of nicotine craving, nicotine dependence, previous attempts of
cessation, motivating factors for smoking as well as underlying quitting of smoking and the self-
efficiency of abstaining from smoking across mental health patients who were smokers and
admitted across a UK based mental healthcare setting. This experimental sample was compared
with a control sample comprising of staff working in the chosen mental health care settings who
identified themselves as smokers. Thus, a total of 100 participants, 50 belonging to each of the
experimental and control groups were assessed with respect to the above outcomes using
questionnaires like: the 10-point Contemplation Ladder, the 10 item Smoker Clinic
Questionnaire, single item valid questions of self-efficacy and nicotine cravings and 4 item
questions for nicotine dependence. Based on statistical methods of t-test using a significance
value of α = < 0.01, the results indicated greater levels of nicotine dependence and cravings
across the experimental group. Additionally, the results revealed that while health concerns were
the key motivators of smoking cessation across staff, patients demonstrated a greater likelihood
to smoke during times of stress and as a reliever of boredom, for the purpose of gaining pleasure
or enjoyment. These social, emotional and motivational outcomes in turn, also served as the key
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
31SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
barriers underlying successful smoking cessation for mental illness patients who were smokers
which is why, the results indicated lower likelihood of quitting across this group.
While such results are not specific the mental health outcomes of smoking cessation, the
study by Dickens, Staniford and Long (2014) are of considerable relevance to future nursing
practice due to its ability to inform nurses of the role of boredom or the importance of motivation
in hindering or facilitating smoking cessation. Additionally, another strength of this study is its
ability to inform healthcare professionals on the need to not just focus on the mental health
symptoms but also the experiences which may facilitate or deter a smoker’s motivation to quit,
especially across those with mental health illness. However, it must be noted that the data
collection tools chosen by the authors of this study were largely associated with survey which
increases the risk of bias, social desirability and thus, raises doubts on the validity and quality of
results (Heale and Twycross 2015). One of the most concerning limitations of this study
however, is the lack of similarity between the baseline characteristics of experimental and
control controls – since it is likely that staff will have greater levels of health literacy and
awareness as compared to patients. Additionally, the authors make no mention of the type of
mental health disorders included within the participant group, thus raising doubts on the
transferability and validity of results across future mental health settings with acutely ill patients
(Cypress 2017).
4.3. Article 2: Knowles et al. (2016)
The qualitative study by Knowles et al. (2016), aimed to assess the subjective
experiences of individuals with acute mental health disorders while availing smoking cessation
interventions delivered by mental health practitioners in the United Kingdom. With the help of
semi-structured interviews, 3 mental healthcare professionals entrusted with deliverance of
barriers underlying successful smoking cessation for mental illness patients who were smokers
which is why, the results indicated lower likelihood of quitting across this group.
While such results are not specific the mental health outcomes of smoking cessation, the
study by Dickens, Staniford and Long (2014) are of considerable relevance to future nursing
practice due to its ability to inform nurses of the role of boredom or the importance of motivation
in hindering or facilitating smoking cessation. Additionally, another strength of this study is its
ability to inform healthcare professionals on the need to not just focus on the mental health
symptoms but also the experiences which may facilitate or deter a smoker’s motivation to quit,
especially across those with mental health illness. However, it must be noted that the data
collection tools chosen by the authors of this study were largely associated with survey which
increases the risk of bias, social desirability and thus, raises doubts on the validity and quality of
results (Heale and Twycross 2015). One of the most concerning limitations of this study
however, is the lack of similarity between the baseline characteristics of experimental and
control controls – since it is likely that staff will have greater levels of health literacy and
awareness as compared to patients. Additionally, the authors make no mention of the type of
mental health disorders included within the participant group, thus raising doubts on the
transferability and validity of results across future mental health settings with acutely ill patients
(Cypress 2017).
4.3. Article 2: Knowles et al. (2016)
The qualitative study by Knowles et al. (2016), aimed to assess the subjective
experiences of individuals with acute mental health disorders while availing smoking cessation
interventions delivered by mental health practitioners in the United Kingdom. With the help of
semi-structured interviews, 3 mental healthcare professionals entrusted with deliverance of
32SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
smoking cessation while 13 participants of the same, with acute mental illnesses were
interviewed concerning their perceptions and acceptance concerning these interventions. One of
the major themes which emerged were the lack of motivation and prevalence of discouragement
across patients due to absence of any form of empathy, patience or motivation by service
providers. The second theme which emerged across service providers and patients included an
increased level of acceptance and effectiveness towards bespoke smoking cessation interventions
instead of traditional, routine care interventions due to the former’s ability to be customized as
per the mental health needs of the patients.
Thus, the above findings by Knowles et al. (2016) provide an interesting and
comprehensive insight into the perceptions of both practitioners as well as participants with
mental health illnesses concerning the nature and type of smoking cessation interventions which
are associated with higher levels of acceptance and motivation for quitting. Further, the author’s
inclusion of interview based methodologies demonstrate congruence with the research question
to the effectiveness of such data collection methods in acquiring subjective data. However, in
criticism, the interviews are also associated with higher rates bias and social desirability, which
in turn, raises doubts concerning the validity of the results in this research (Nardi 2018). The
author’s usage of blinding however can be considered a key strength in terms of mitigation of
any bias. However, the absence of any standardized psychological or physiological assessments
for outcome and effectiveness measurement hinders the applicability of the results of this
research across real life mental health inpatient settings (Brown et al. 2017).
4.4. Article 4: Osborn et al. (2018)
The cluster randomized controlled trials by Osborn et al. (2018), aimed to assess the
physiological as well as financial effectiveness of a set of clinical interventions on reducing the
smoking cessation while 13 participants of the same, with acute mental illnesses were
interviewed concerning their perceptions and acceptance concerning these interventions. One of
the major themes which emerged were the lack of motivation and prevalence of discouragement
across patients due to absence of any form of empathy, patience or motivation by service
providers. The second theme which emerged across service providers and patients included an
increased level of acceptance and effectiveness towards bespoke smoking cessation interventions
instead of traditional, routine care interventions due to the former’s ability to be customized as
per the mental health needs of the patients.
Thus, the above findings by Knowles et al. (2016) provide an interesting and
comprehensive insight into the perceptions of both practitioners as well as participants with
mental health illnesses concerning the nature and type of smoking cessation interventions which
are associated with higher levels of acceptance and motivation for quitting. Further, the author’s
inclusion of interview based methodologies demonstrate congruence with the research question
to the effectiveness of such data collection methods in acquiring subjective data. However, in
criticism, the interviews are also associated with higher rates bias and social desirability, which
in turn, raises doubts concerning the validity of the results in this research (Nardi 2018). The
author’s usage of blinding however can be considered a key strength in terms of mitigation of
any bias. However, the absence of any standardized psychological or physiological assessments
for outcome and effectiveness measurement hinders the applicability of the results of this
research across real life mental health inpatient settings (Brown et al. 2017).
4.4. Article 4: Osborn et al. (2018)
The cluster randomized controlled trials by Osborn et al. (2018), aimed to assess the
physiological as well as financial effectiveness of a set of clinical interventions on reducing the
33SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
risk of hypercholesterolemia and cardiovascular diseases across patients with acute mental
illnesses like psychosis, bipolar disorder and schizophrenia, across general practitioner services
in England. The interventions were a part of the Primrose intervention and comprised of dietary
changes, exercise, and adherence to statins, alcohol reduction and smoking cessation. A total of
40 participants were randomized to either usual treatment control groups or the Primrose
intervention group for 12 months and were assessed based on outcomes such as costs incurred in
health care and levels of total cholesterol. The results demonstrated however, a lack of
significant differences in the mean values of total cholesterol between the control and Primrose
group (0.03, 95% CI 0.22 to 0.29; p=0.788) at 12 months. However, a decrease in the levels of
cholesterol were observed after 12 months in the Primrose group as compared to the control
group (a decrease of 0.22 mmol/L vs. a decrease of 0.36 mmol/liter). Additionally, patients in the
Primrose intervention group incurred savings of £895 in healthcare costs as compared to the
control group patients receiving usual treatment.
Such findings provide useful insights into the key benefits of smoking cessation in terms
of reduction of cardiovascular disease risk and cholesterol levels which in turn can be considered
to reduce morbidity and mortality and improve long term metabolic outcomes across patients
with acute mental illnesses. Additionally, the usage of randomization and blinding are major
strengths of this research in terms of high research validity and mitigation of bias. However,
small sample size and the fact that smoking cessation interventions were administered in a
cluster and not individually thus raising the possibility of results being affected by confounders
(Edmonds and Kennedy 2016).
risk of hypercholesterolemia and cardiovascular diseases across patients with acute mental
illnesses like psychosis, bipolar disorder and schizophrenia, across general practitioner services
in England. The interventions were a part of the Primrose intervention and comprised of dietary
changes, exercise, and adherence to statins, alcohol reduction and smoking cessation. A total of
40 participants were randomized to either usual treatment control groups or the Primrose
intervention group for 12 months and were assessed based on outcomes such as costs incurred in
health care and levels of total cholesterol. The results demonstrated however, a lack of
significant differences in the mean values of total cholesterol between the control and Primrose
group (0.03, 95% CI 0.22 to 0.29; p=0.788) at 12 months. However, a decrease in the levels of
cholesterol were observed after 12 months in the Primrose group as compared to the control
group (a decrease of 0.22 mmol/L vs. a decrease of 0.36 mmol/liter). Additionally, patients in the
Primrose intervention group incurred savings of £895 in healthcare costs as compared to the
control group patients receiving usual treatment.
Such findings provide useful insights into the key benefits of smoking cessation in terms
of reduction of cardiovascular disease risk and cholesterol levels which in turn can be considered
to reduce morbidity and mortality and improve long term metabolic outcomes across patients
with acute mental illnesses. Additionally, the usage of randomization and blinding are major
strengths of this research in terms of high research validity and mitigation of bias. However,
small sample size and the fact that smoking cessation interventions were administered in a
cluster and not individually thus raising the possibility of results being affected by confounders
(Edmonds and Kennedy 2016).
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
34SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
4.5. Article 5: Richardson, McNeill and Brose (2019)
The cohort study by Richardson, McNeill and Brose (2019), aimed to examine the nature
of smoking cessation and abstinence behaviours which were observed in individuals with mental
health conditions in the United Kingdom, between the years 1193 and 2014. The authors
engaged in evaluation of the Adult Psychiatric Morbidity Survey for the purpose of evaluating
smoking prevalence trends as well as the association between various mental health conditions
and smoking cessation behaviours. The findings demonstrated a positive association between
individuals with mental health conditions like generalized and mixed anxiety, phobias,
depression and personality related disorders who engage in smoking cessation interventions and
higher rates of heavy smoking behaviours, difficult to abstain from smoking, a perception that
smoking cessation is difficult and a strong desire to quit. Interestingly, despite the prevalence of
strong sense of eagerness to quit, the prevalence of smoking behaviours across individuals with
mental health conditions were in fact 50% greater than those observed across individuals without
mental health conditions.
Such findings are useful in terms of the effects of high desire to quit and perceptions of
difficulties across individuals with acute mental health conditions. However, the lack of any
standardized mental health assessment frameworks as well as the lack of specifying whether
participants were from mental healthcare settings can be considered as a key issue in terms of
applicability and transferability of these results across real life, UK based mental healthcare
settings. Further, the lack of inclusion of any confidence intervals as well as the absence of
consideration of bias across survey responses not only hinder the validity but also the readers’
understanding of the precision of these findings (Nardi 2018).
4.5. Article 5: Richardson, McNeill and Brose (2019)
The cohort study by Richardson, McNeill and Brose (2019), aimed to examine the nature
of smoking cessation and abstinence behaviours which were observed in individuals with mental
health conditions in the United Kingdom, between the years 1193 and 2014. The authors
engaged in evaluation of the Adult Psychiatric Morbidity Survey for the purpose of evaluating
smoking prevalence trends as well as the association between various mental health conditions
and smoking cessation behaviours. The findings demonstrated a positive association between
individuals with mental health conditions like generalized and mixed anxiety, phobias,
depression and personality related disorders who engage in smoking cessation interventions and
higher rates of heavy smoking behaviours, difficult to abstain from smoking, a perception that
smoking cessation is difficult and a strong desire to quit. Interestingly, despite the prevalence of
strong sense of eagerness to quit, the prevalence of smoking behaviours across individuals with
mental health conditions were in fact 50% greater than those observed across individuals without
mental health conditions.
Such findings are useful in terms of the effects of high desire to quit and perceptions of
difficulties across individuals with acute mental health conditions. However, the lack of any
standardized mental health assessment frameworks as well as the lack of specifying whether
participants were from mental healthcare settings can be considered as a key issue in terms of
applicability and transferability of these results across real life, UK based mental healthcare
settings. Further, the lack of inclusion of any confidence intervals as well as the absence of
consideration of bias across survey responses not only hinder the validity but also the readers’
understanding of the precision of these findings (Nardi 2018).
35SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
4.6. Article 6: GillBody et al. (2019)
The pragmatic randomized controlled trial by Gillbody et al. (2019), known popularly as
the ‘Smoking Cessation Intervention for Acute Mental Illness’ (SCIMITAR) Trial, investigated
the effectiveness of behavioural and pharmacological based smoking cessation interventions
across patients with acute mental illnesses admitted across community and primary care settings
in the UK. A total of 526 patients with schizophrenia and bipolar disorders were randomized
between control group interventions of usual care and the bespoke smoking cessation
intervention group and evaluated after 12 months, in terms of the Generalised Anxiety Disorder-
7 (GAD-7) questionnaire, Fagerström Test for Nicotine Dependence (FTND), Patient Health
Questionnaire-9 (PHQ-9) and Motivation to Quit (MTQ) questionnaire. Higher rates of smoking
abstinence were observed in the intervention group at 6 months as compared to the control group
(32 [14%] of 226 vs. 14 [6%] of 217). However, there were no significant differences observed
in quitting between the two groups at 12 months. Similarly, there were no statistically significant
differences observed between both the groups at 6 as well as 12 months, in terms of scores of
motivation to quit, generalized anxiety disorder, patient health outcomes and nicotine
dependence.
Such findings generate insights considering the inverse association between duration of
smoking cessation interventions and the potency of these interventions as evidenced by Gillbody
et al. (2019), where a lack of significant differences in mental health symptoms were reported at
12 months, despite demonstrating dramatic reductions in depression and anxiety symptoms as
well as nicotine dependence. However, it is worthwhile to mention that there is no mention of
participants being blinded to the research objectives. Lastly, despite inclusion of standardized
4.6. Article 6: GillBody et al. (2019)
The pragmatic randomized controlled trial by Gillbody et al. (2019), known popularly as
the ‘Smoking Cessation Intervention for Acute Mental Illness’ (SCIMITAR) Trial, investigated
the effectiveness of behavioural and pharmacological based smoking cessation interventions
across patients with acute mental illnesses admitted across community and primary care settings
in the UK. A total of 526 patients with schizophrenia and bipolar disorders were randomized
between control group interventions of usual care and the bespoke smoking cessation
intervention group and evaluated after 12 months, in terms of the Generalised Anxiety Disorder-
7 (GAD-7) questionnaire, Fagerström Test for Nicotine Dependence (FTND), Patient Health
Questionnaire-9 (PHQ-9) and Motivation to Quit (MTQ) questionnaire. Higher rates of smoking
abstinence were observed in the intervention group at 6 months as compared to the control group
(32 [14%] of 226 vs. 14 [6%] of 217). However, there were no significant differences observed
in quitting between the two groups at 12 months. Similarly, there were no statistically significant
differences observed between both the groups at 6 as well as 12 months, in terms of scores of
motivation to quit, generalized anxiety disorder, patient health outcomes and nicotine
dependence.
Such findings generate insights considering the inverse association between duration of
smoking cessation interventions and the potency of these interventions as evidenced by Gillbody
et al. (2019), where a lack of significant differences in mental health symptoms were reported at
12 months, despite demonstrating dramatic reductions in depression and anxiety symptoms as
well as nicotine dependence. However, it is worthwhile to mention that there is no mention of
participants being blinded to the research objectives. Lastly, despite inclusion of standardized
36SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
and valid assessment methods, the prevalence of self-reported tools such as questionnaire raise
the possibility of bias and thus invalidity across findings (Cor 2016).
4.7. Article 7: Gemma et al. (2020)
The prospective cohort study by Taylor et al. (2020), aimed to investigate the efficacies
and prevalence of acquiring positive outcomes with respect to safety in mental health associated
with the administration of pharmacological based interventions of smoking cessation. The
authors examined the effectiveness of smoking cessation interventions based on their
administration on a total of 654 general healthcare practicing organizations across England from
the year 2006. Patients with mental health illnesses such as depression, bipolar disorder,
schizophrenia or under anxiolytic or antidepressant prescriptions were administered with either
varenicline (n = 19117) or nicotine replacement therapy (NRT) (n = 59340) belonging to a
cohort of 1st of September 2006 to 31st of December, 2015, based upon periodic follow up
evaluations approximately: 3 months, 6th months, 9 months, 1 year, 2 years and 4 years
respectively. The results acquired from the study by Taylor et al. (2020), indicated a positive
association between varenicline administration and decreased incidences of mental health
symptom deterioration as compared to patients provided with NRT, both in the presence as well
as the absence of severe mental illnesses. In comparison to smokers who were devoid of any
mental health conditions, the results indicated an increased odds of 19% with respect to quitting
smoking behaviors across patients under varenicline prescription at the 2nd years relative to those
patients receiving NRT. (95% CI: 15% to 24%).
Such findings impart significant usefulness with respect to implications in future nursing
practice with respect to the effectiveness of varenicline administration as a key facilitator of
smoking cessation – a medication which is largely avoided or administered with caution across
and valid assessment methods, the prevalence of self-reported tools such as questionnaire raise
the possibility of bias and thus invalidity across findings (Cor 2016).
4.7. Article 7: Gemma et al. (2020)
The prospective cohort study by Taylor et al. (2020), aimed to investigate the efficacies
and prevalence of acquiring positive outcomes with respect to safety in mental health associated
with the administration of pharmacological based interventions of smoking cessation. The
authors examined the effectiveness of smoking cessation interventions based on their
administration on a total of 654 general healthcare practicing organizations across England from
the year 2006. Patients with mental health illnesses such as depression, bipolar disorder,
schizophrenia or under anxiolytic or antidepressant prescriptions were administered with either
varenicline (n = 19117) or nicotine replacement therapy (NRT) (n = 59340) belonging to a
cohort of 1st of September 2006 to 31st of December, 2015, based upon periodic follow up
evaluations approximately: 3 months, 6th months, 9 months, 1 year, 2 years and 4 years
respectively. The results acquired from the study by Taylor et al. (2020), indicated a positive
association between varenicline administration and decreased incidences of mental health
symptom deterioration as compared to patients provided with NRT, both in the presence as well
as the absence of severe mental illnesses. In comparison to smokers who were devoid of any
mental health conditions, the results indicated an increased odds of 19% with respect to quitting
smoking behaviors across patients under varenicline prescription at the 2nd years relative to those
patients receiving NRT. (95% CI: 15% to 24%).
Such findings impart significant usefulness with respect to implications in future nursing
practice with respect to the effectiveness of varenicline administration as a key facilitator of
smoking cessation – a medication which is largely avoided or administered with caution across
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
37SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
primary care mental health settings due to prevalent adverse health effects like insomnia and
nausea (Taylor et al. 2020). Such findings thus inform the effectiveness of primary care settings
and most notably nursing responsibilities of specific medication administration in ensuring
achievement of positive impacts like reduced mental health symptoms across smokers who are
patients of acute illnesses and severe mental health disorders (Taylor et al. 2020). Additionally,
the usage of a relative large sample size coupled with periodic follow ups, blinding, inclusion of
a range of mental health and substance abuse disorders, statistical measurement of confidence
intervals and a significantly extensive study period were major strengths of this study with
respect to high precision, methodological and result quality (Cook et al. 2016). Additionally, the
inclusion of an UK exclusive participant data coupled with measurement of outcomes specific to
mental health symptoms were also major strengths of this study, with respect to future
applicability and transferability across UK specific mental healthcare settings (Burke 2016).
However, the study largely overlooked the prevalence of nicotine dependence as confounding
factors as well as did not consider the measurement of the impact of smoking cessation
interventions on quality of life components like social or emotional wellbeing. The results are
also largely specific to primary or acute care settings. Such limitations thus hinder applicability,
internal validity and transferability of research methodological and result quality with respect to
community care settings or the social and emotional outcomes of pharmacological smoking
cessation interventions (Edmonds and Kennedy 2016).
4.8. Conclusion: Findings and Observations
Based on the above the results, it can be observed that implementation and effectiveness
of smoking cessation interventions are associated with a range of positive mental, metabolic and
social outcomes like: reduced mental health symptoms, enhanced or degraded motivation to quit
primary care mental health settings due to prevalent adverse health effects like insomnia and
nausea (Taylor et al. 2020). Such findings thus inform the effectiveness of primary care settings
and most notably nursing responsibilities of specific medication administration in ensuring
achievement of positive impacts like reduced mental health symptoms across smokers who are
patients of acute illnesses and severe mental health disorders (Taylor et al. 2020). Additionally,
the usage of a relative large sample size coupled with periodic follow ups, blinding, inclusion of
a range of mental health and substance abuse disorders, statistical measurement of confidence
intervals and a significantly extensive study period were major strengths of this study with
respect to high precision, methodological and result quality (Cook et al. 2016). Additionally, the
inclusion of an UK exclusive participant data coupled with measurement of outcomes specific to
mental health symptoms were also major strengths of this study, with respect to future
applicability and transferability across UK specific mental healthcare settings (Burke 2016).
However, the study largely overlooked the prevalence of nicotine dependence as confounding
factors as well as did not consider the measurement of the impact of smoking cessation
interventions on quality of life components like social or emotional wellbeing. The results are
also largely specific to primary or acute care settings. Such limitations thus hinder applicability,
internal validity and transferability of research methodological and result quality with respect to
community care settings or the social and emotional outcomes of pharmacological smoking
cessation interventions (Edmonds and Kennedy 2016).
4.8. Conclusion: Findings and Observations
Based on the above the results, it can be observed that implementation and effectiveness
of smoking cessation interventions are associated with a range of positive mental, metabolic and
social outcomes like: reduced mental health symptoms, enhanced or degraded motivation to quit

38SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
due to prevalence or lack of boredom and pleasure, improved cardiovascular health parameters
as well as the role of emotional outcomes such as a strong willingness to quit despite the
possibility of relapse. Additionally, this review briefly sheds light on the expectations held by
both patients as well as practitioners and healthcare staff with regards to smoking cessation
interventions. Thus, along with answering the initial research question of effectiveness of
smoking cessation in mental health, this review also paved the way for various themes like social
and emotional outcomes and expectations held by patients during the process of abstinence. Such
findings have the potential to guide nurses on the required mental health assessments as well as
compliance and communication strategies to consider during future simultaneous management of
acute mental illness and preventable smoking behaviours.
due to prevalence or lack of boredom and pleasure, improved cardiovascular health parameters
as well as the role of emotional outcomes such as a strong willingness to quit despite the
possibility of relapse. Additionally, this review briefly sheds light on the expectations held by
both patients as well as practitioners and healthcare staff with regards to smoking cessation
interventions. Thus, along with answering the initial research question of effectiveness of
smoking cessation in mental health, this review also paved the way for various themes like social
and emotional outcomes and expectations held by patients during the process of abstinence. Such
findings have the potential to guide nurses on the required mental health assessments as well as
compliance and communication strategies to consider during future simultaneous management of
acute mental illness and preventable smoking behaviours.
39SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
Chapter 5: Discussion
5.1. Introduction and Brief Overview
As per the previous chapter, it was observed that current evidence demonstrates not just
an association between disease outcomes and smoking cessation but also the emergence of
themes associated with the emotional and social wellbeing of smokers. Using evidence based on
the literature review findings, the results of the studies reviewed systematically have been
critiqued and further explored, as mention in the following sections.
5.2. Smoking Cessation effects on Mental Health
The positive association between smoking cessation and reduction or improvement in
mental health outcomes and likelihood of quitting coupled with decreased susceptibility to
mental health adversities were reported extensively in the cohort study by Taylor et al. (2020) as
well as the bespoke SCIMITAR study by Gillbody et al. (2019). This reason for such effects are
likely to be a result of the neurotransmitter and neurological effects of smoking. Such
associations can indeed be strengthened by the experiment implemented by Rademacher et al.
(2016), which demonstrated higher levels of dopamine synthesis – whose deficiency paves the
way for depression – across individuals abstaining from smoking in comparison to smokers.
Additionally, the association between metal health improvement and smoking cessation can be
further postulated in the cohort study by Miyauchi et al. (2017), where smoking cessation
resulted in significant reduction in the excitatory functions of the sympathetic nervous system as
well as the intake of anti-Parkinson drugs. Such findings demonstrate positive implications in
terms of nursing practice components such as patient education and neurological assessments. In
criticism however, as per Taylor and Shiers (2016), such neurological effects of smoking
Chapter 5: Discussion
5.1. Introduction and Brief Overview
As per the previous chapter, it was observed that current evidence demonstrates not just
an association between disease outcomes and smoking cessation but also the emergence of
themes associated with the emotional and social wellbeing of smokers. Using evidence based on
the literature review findings, the results of the studies reviewed systematically have been
critiqued and further explored, as mention in the following sections.
5.2. Smoking Cessation effects on Mental Health
The positive association between smoking cessation and reduction or improvement in
mental health outcomes and likelihood of quitting coupled with decreased susceptibility to
mental health adversities were reported extensively in the cohort study by Taylor et al. (2020) as
well as the bespoke SCIMITAR study by Gillbody et al. (2019). This reason for such effects are
likely to be a result of the neurotransmitter and neurological effects of smoking. Such
associations can indeed be strengthened by the experiment implemented by Rademacher et al.
(2016), which demonstrated higher levels of dopamine synthesis – whose deficiency paves the
way for depression – across individuals abstaining from smoking in comparison to smokers.
Additionally, the association between metal health improvement and smoking cessation can be
further postulated in the cohort study by Miyauchi et al. (2017), where smoking cessation
resulted in significant reduction in the excitatory functions of the sympathetic nervous system as
well as the intake of anti-Parkinson drugs. Such findings demonstrate positive implications in
terms of nursing practice components such as patient education and neurological assessments. In
criticism however, as per Taylor and Shiers (2016), such neurological effects of smoking
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
40SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
cessation are likely to facilitate blood levels of neurotransmitters - enhanced by antipsychotic
and anxiolytic medications, in patients with acute mental illness, which in turn increase the risk
of side effects like aggression, euphoria, agitation, sweating, pupil dilation, trembling and
gastrointestinal discomfort. Thus, mental health nurses and practitioners are advised to reduce
the dosage of such medications during administration of smoking cessation interventions.
5.3. Smoking cessation effects on Cardiovascular Health
High mortality and morbidity as are result of cardiovascular and pulmonary deficits have
been evidenced previously by Public Health England (2016), especially in case of simultaneous
presence of both acute mental illnesses and chronic smoking. Thus, with this respect, the
findings of inverse association between smoking cessation and cardiovascular disease markers
like cholesterol by Osborn et al. (2019) in the Primrose study, serve as a useful nursing
implication with respect nursing collaboration with multidisciplinary team for future smoking
cessation administration across mental health settings. These findings can further be
supplemented as per the study by King et al. (2017), where smoking cessation was found to
reduce inflammatory markers of cardiovascular diseases like and thus demonstrates the effects of
smoking cessation in preventing oxidative stress and cardiovascular disease induced mortality
and morbidity across patients with acute mental illnesses.
However, alternatively, the impact of smoking cessation on weight gain evidenced by
Haris, Zopey and Friedman (2016) cannot be overlooked since such metabolic effects serve as
key barriers for smoking cessation compliance. The metabolic impacts of smoking cessation
have indeed been evidenced in the systematic review by Haris, Zopey and Friedman (2016)
which denoted an increase in insulin sensitivity and hunger and as a result, weight gain across
smokers attempting to abstain from smoking. Such impacts, as evidenced by Taylor and Shiers
cessation are likely to facilitate blood levels of neurotransmitters - enhanced by antipsychotic
and anxiolytic medications, in patients with acute mental illness, which in turn increase the risk
of side effects like aggression, euphoria, agitation, sweating, pupil dilation, trembling and
gastrointestinal discomfort. Thus, mental health nurses and practitioners are advised to reduce
the dosage of such medications during administration of smoking cessation interventions.
5.3. Smoking cessation effects on Cardiovascular Health
High mortality and morbidity as are result of cardiovascular and pulmonary deficits have
been evidenced previously by Public Health England (2016), especially in case of simultaneous
presence of both acute mental illnesses and chronic smoking. Thus, with this respect, the
findings of inverse association between smoking cessation and cardiovascular disease markers
like cholesterol by Osborn et al. (2019) in the Primrose study, serve as a useful nursing
implication with respect nursing collaboration with multidisciplinary team for future smoking
cessation administration across mental health settings. These findings can further be
supplemented as per the study by King et al. (2017), where smoking cessation was found to
reduce inflammatory markers of cardiovascular diseases like and thus demonstrates the effects of
smoking cessation in preventing oxidative stress and cardiovascular disease induced mortality
and morbidity across patients with acute mental illnesses.
However, alternatively, the impact of smoking cessation on weight gain evidenced by
Haris, Zopey and Friedman (2016) cannot be overlooked since such metabolic effects serve as
key barriers for smoking cessation compliance. The metabolic impacts of smoking cessation
have indeed been evidenced in the systematic review by Haris, Zopey and Friedman (2016)
which denoted an increase in insulin sensitivity and hunger and as a result, weight gain across
smokers attempting to abstain from smoking. Such impacts, as evidenced by Taylor and Shiers
41SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
(2016), can further be aggravated in patients who, along with acute mental illnesses, are also
diabetic and being administered with antipsychotic. Such findings thus guide nursing practice in
terms of the importance of patient education, administration of early lifestyle interventions like
diet and exercise and collaboration with multidisciplinary teams for simultaneous management
of mental illness and metabolic deficits during future smoking cessation intervention
implementation which in turn can enhance patient compliance and motivation towards the same.
5.4. Smoking Cessation effects on Social and Emotional Outcomes
The cohort study by Dickens, Staniford and Long (2014), provided interesting insights
into the key factors which motivated and discouraged smokers to engage in smoking cessation,
some of which include, the prevalence of boredom, pleasure and enjoyment benefits associated
with smoking behaviours, which in turn, hindered their ability to quit. In criticism however, the
studies by Chang et al. (2017) and Li et al. (2019), demonstrated greater levels of readiness to
quit across smokers with mental health conditions due to factors like reduced health care costs
and increased levels of participant health literacy levels which in turn, facilitated greater
motivation and compliance. However, the study by Knowles et al. (2016) as well as Dickens,
Staniford and Long (2020) expounded upon the role of social and practitioner support as well as
the prevalence of motivational interventions in facilitating smokers to engage in smoking
cessation and thus tackling lack of appreciation, motivation and prevalence of boredom and
stigma across healthcare organizations are common reasons for relapse. Such findings are of
utmost importance to nursing practice due to their demonstration of the importance of nursing
therapeutic relationships and family centred or peer supported practice in encouraging smokers
to feel motivated to abstain from smoking. This is because, emotion coping strategies such as
support from family or friends as well as empathy from practitioners have been evidenced to
(2016), can further be aggravated in patients who, along with acute mental illnesses, are also
diabetic and being administered with antipsychotic. Such findings thus guide nursing practice in
terms of the importance of patient education, administration of early lifestyle interventions like
diet and exercise and collaboration with multidisciplinary teams for simultaneous management
of mental illness and metabolic deficits during future smoking cessation intervention
implementation which in turn can enhance patient compliance and motivation towards the same.
5.4. Smoking Cessation effects on Social and Emotional Outcomes
The cohort study by Dickens, Staniford and Long (2014), provided interesting insights
into the key factors which motivated and discouraged smokers to engage in smoking cessation,
some of which include, the prevalence of boredom, pleasure and enjoyment benefits associated
with smoking behaviours, which in turn, hindered their ability to quit. In criticism however, the
studies by Chang et al. (2017) and Li et al. (2019), demonstrated greater levels of readiness to
quit across smokers with mental health conditions due to factors like reduced health care costs
and increased levels of participant health literacy levels which in turn, facilitated greater
motivation and compliance. However, the study by Knowles et al. (2016) as well as Dickens,
Staniford and Long (2020) expounded upon the role of social and practitioner support as well as
the prevalence of motivational interventions in facilitating smokers to engage in smoking
cessation and thus tackling lack of appreciation, motivation and prevalence of boredom and
stigma across healthcare organizations are common reasons for relapse. Such findings are of
utmost importance to nursing practice due to their demonstration of the importance of nursing
therapeutic relationships and family centred or peer supported practice in encouraging smokers
to feel motivated to abstain from smoking. This is because, emotion coping strategies such as
support from family or friends as well as empathy from practitioners have been evidenced to
42SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
enhance feelings of self-esteem, control and security across patients. Such findings hold greater
importance for smokers especially, due to their long term reliance on smoking as a coping
strategy (Hubbard et al. 2016).
Chapter 6: Limitations
One of the major limitations which were prevalent in this research, is the prevalence of
inadequacies in methodological quality of studies such as bias, social desirability and
confounders. Such issues raise doubts on the internal validity of this systematic review which
could have been prevented possibly, via the inclusion of quantitative research methodologies
(Cook et al. 2016).
The lack of research assessing mental health, wellbeing, physiological and quality of life
outcomes after smoking cessation made it further difficult to acquire articles devoid of
confounders and of relevance to the research question (Heale and Twycross 2015). Thus, the
absence of any standardized screening or mental health assessment outcomes make it difficult to
completely apply or transfer the same across real life mental health clinical settings. Such
limitations were particularly noticeable during critical appraisal which in turn demonstrated the
importance of critical thinking nursing skills and influenced the discussion section in succeeding
chapters and conclusions concerning future implications in nursing (Edmonds and Kennedy
2016).
Thus, there is still a need to engage in a more robust, valid and comprehensive evidence
based research prior to translating such findings into practice. The inclusion of randomized,
quantitative methodologies specifically targeting UK mental healthcare settings as well as
inclusion of participants with acute mental illnesses, will prove to be useful in terms of
enhance feelings of self-esteem, control and security across patients. Such findings hold greater
importance for smokers especially, due to their long term reliance on smoking as a coping
strategy (Hubbard et al. 2016).
Chapter 6: Limitations
One of the major limitations which were prevalent in this research, is the prevalence of
inadequacies in methodological quality of studies such as bias, social desirability and
confounders. Such issues raise doubts on the internal validity of this systematic review which
could have been prevented possibly, via the inclusion of quantitative research methodologies
(Cook et al. 2016).
The lack of research assessing mental health, wellbeing, physiological and quality of life
outcomes after smoking cessation made it further difficult to acquire articles devoid of
confounders and of relevance to the research question (Heale and Twycross 2015). Thus, the
absence of any standardized screening or mental health assessment outcomes make it difficult to
completely apply or transfer the same across real life mental health clinical settings. Such
limitations were particularly noticeable during critical appraisal which in turn demonstrated the
importance of critical thinking nursing skills and influenced the discussion section in succeeding
chapters and conclusions concerning future implications in nursing (Edmonds and Kennedy
2016).
Thus, there is still a need to engage in a more robust, valid and comprehensive evidence
based research prior to translating such findings into practice. The inclusion of randomized,
quantitative methodologies specifically targeting UK mental healthcare settings as well as
inclusion of participants with acute mental illnesses, will prove to be useful in terms of
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
43SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
generating findings which are valid, applicable, trustworthy and transferable to national
healthcare scenarios. Additionally, there is also a need to consider socioeconomic demographics
of participants so as to ensure that findings of future research can be implemented across mental
health patients belonging to economically underprivileged or culturally diverse groups in the UK
(Burke 2016).
generating findings which are valid, applicable, trustworthy and transferable to national
healthcare scenarios. Additionally, there is also a need to consider socioeconomic demographics
of participants so as to ensure that findings of future research can be implemented across mental
health patients belonging to economically underprivileged or culturally diverse groups in the UK
(Burke 2016).
44SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
Chapter 7: Conclusion
The key psychological effects of smoking cessation include: reduced severity of
depressive and anxiety symptoms and overall sympathetic nervous system functioning,
improvements in dopamine activity especially with regards to schizophrenia and an overall
enhancement of feelings of self-esteem. Additionally, smoking cessation was improved
metabolic and cardiovascular outcomes which in turn, can significantly mitigate the risk of
reduced life expectancy and high mortality rates across patients with acute mental illness. Such
findings demonstrate considerable significance with regards to future nursing as well as mental
health practice due to their ability to inform and guide mental healthcare organizations on the
factors, outcomes and facilitators to look for when administering smoking cessation-based
interventions across mental health settings.
To conclude, smoking cessation indeed yields beneficial metabolic, cardiovascular and
mental health outcomes across mental illnesses which in turn, can inform further nursing practice
and patient education during nursing management of patients with mental illnesses. However, it
is recommended that nurses as well as healthcare organizations prioritize engagement in more
comprehensive, robust and quantitative research specific to UK settings so as to acquire clinical
findings relevance to the management of acutely ill mental health patients.
Chapter 7: Conclusion
The key psychological effects of smoking cessation include: reduced severity of
depressive and anxiety symptoms and overall sympathetic nervous system functioning,
improvements in dopamine activity especially with regards to schizophrenia and an overall
enhancement of feelings of self-esteem. Additionally, smoking cessation was improved
metabolic and cardiovascular outcomes which in turn, can significantly mitigate the risk of
reduced life expectancy and high mortality rates across patients with acute mental illness. Such
findings demonstrate considerable significance with regards to future nursing as well as mental
health practice due to their ability to inform and guide mental healthcare organizations on the
factors, outcomes and facilitators to look for when administering smoking cessation-based
interventions across mental health settings.
To conclude, smoking cessation indeed yields beneficial metabolic, cardiovascular and
mental health outcomes across mental illnesses which in turn, can inform further nursing practice
and patient education during nursing management of patients with mental illnesses. However, it
is recommended that nurses as well as healthcare organizations prioritize engagement in more
comprehensive, robust and quantitative research specific to UK settings so as to acquire clinical
findings relevance to the management of acutely ill mental health patients.
45SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
References
Bailey, J.M., Wye, P.M., Stockings, E.A., Bartlem, K.M., Metse, A.P., Wiggers, J.H. and
Bowman, J.A., 2017. Smoking cessation care for people with a mental illness: family carer
expectations of health and community services. Journal of Smoking Cessation, 12(4), pp.221-
230.
Bengtsson, M., 2016. How to plan and perform a qualitative study using content analysis.
NursingPlus Open, 2, pp.8-14.
Braun, V., Clarke, V., Hayfield, N. and Terry, G., 2019. Thematic analysis. Handbook of
research methods in health social sciences, pp.843-860.
Brown, G., Strickland-Munro, J., Kobryn, H. and Moore, S.A., 2017. Mixed methods
participatory GIS: An evaluation of the validity of qualitative and quantitative mapping
methods. Applied geography, 79, pp.153-166.
Burke, S., 2016. Rethinking ‘validity’and ‘trustworthiness’ in qualitative inquiry: How might we
judge the quality of qualitative research in sport and exercise sciences?. In Routledge handbook
of qualitative research in sport and exercise (pp. 352-362). Routledge.
Chang, F.C., Sung, H.Y., Zhu, S.H., Feng, T.Y. and Chiou, S.T., 2017. Effects of smoking
cessation media and community campaigns in Taiwan. American Journal of Health
Promotion, 31(1), pp.43-51.
Cook, D.A., Kuper, A., Hatala, R. and Ginsburg, S., 2016. When assessment data are words:
validity evidence for qualitative educational assessments. Academic Medicine, 91(10), pp.1359-
1369.
References
Bailey, J.M., Wye, P.M., Stockings, E.A., Bartlem, K.M., Metse, A.P., Wiggers, J.H. and
Bowman, J.A., 2017. Smoking cessation care for people with a mental illness: family carer
expectations of health and community services. Journal of Smoking Cessation, 12(4), pp.221-
230.
Bengtsson, M., 2016. How to plan and perform a qualitative study using content analysis.
NursingPlus Open, 2, pp.8-14.
Braun, V., Clarke, V., Hayfield, N. and Terry, G., 2019. Thematic analysis. Handbook of
research methods in health social sciences, pp.843-860.
Brown, G., Strickland-Munro, J., Kobryn, H. and Moore, S.A., 2017. Mixed methods
participatory GIS: An evaluation of the validity of qualitative and quantitative mapping
methods. Applied geography, 79, pp.153-166.
Burke, S., 2016. Rethinking ‘validity’and ‘trustworthiness’ in qualitative inquiry: How might we
judge the quality of qualitative research in sport and exercise sciences?. In Routledge handbook
of qualitative research in sport and exercise (pp. 352-362). Routledge.
Chang, F.C., Sung, H.Y., Zhu, S.H., Feng, T.Y. and Chiou, S.T., 2017. Effects of smoking
cessation media and community campaigns in Taiwan. American Journal of Health
Promotion, 31(1), pp.43-51.
Cook, D.A., Kuper, A., Hatala, R. and Ginsburg, S., 2016. When assessment data are words:
validity evidence for qualitative educational assessments. Academic Medicine, 91(10), pp.1359-
1369.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
46SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
Cook, D.A., Kuper, A., Hatala, R. and Ginsburg, S., 2016. When assessment data are words:
validity evidence for qualitative educational assessments. Academic Medicine, 91(10), pp.1359-
1369.
Cor, M.K., 2016. Trust me, it is valid: Research validity in pharmacy education
research. Currents in Pharmacy Teaching and Learning, 8(3), pp.391-400.
Cypress, B.S., 2017. Rigor or reliability and validity in qualitative research: Perspectives,
strategies, reconceptualization, and recommendations. Dimensions of Critical Care Nursing,
36(4), pp.253-263.
Dickens, G.L., Staniford, J. and Long, C.G., 2014. Smoking behaviour, motives, motivation to
quit and self‐efficacy among patients in a secure mental health service: comparison with staff
controls. Journal of psychiatric and mental health nursing, 21(6), pp.483-490.
Evins, A.E., Cather, C. and Daumit, G.L., 2019. Smoking cessation in people with serious
mental illness. The Lancet Psychiatry, 6(7), pp.563-564.
Forman, J., Harris, J.M., Lorencatto, F., McEwen, A. and Duaso, M.J., 2017. National survey of
smoking and smoking cessation education within UK midwifery school curricula. Nicotine &
Tobacco Research, 19(5), pp.591-596.
Forman, J., Harris, J.M., Lorencatto, F., McEwen, A. and Duaso, M.J., 2017. National survey of
smoking and smoking cessation education within UK midwifery school curricula. Nicotine &
Tobacco Research, 19(5), pp.591-596.
Garey, L., Rogers, A.H., Manning, K., Smit, T., Derrick, J.L., Viana, A.G., Schmidt, N.B. and
Zvolensky, M.J., 2020. Effects of smoking cessation treatment attendance on abstinence: The
Cook, D.A., Kuper, A., Hatala, R. and Ginsburg, S., 2016. When assessment data are words:
validity evidence for qualitative educational assessments. Academic Medicine, 91(10), pp.1359-
1369.
Cor, M.K., 2016. Trust me, it is valid: Research validity in pharmacy education
research. Currents in Pharmacy Teaching and Learning, 8(3), pp.391-400.
Cypress, B.S., 2017. Rigor or reliability and validity in qualitative research: Perspectives,
strategies, reconceptualization, and recommendations. Dimensions of Critical Care Nursing,
36(4), pp.253-263.
Dickens, G.L., Staniford, J. and Long, C.G., 2014. Smoking behaviour, motives, motivation to
quit and self‐efficacy among patients in a secure mental health service: comparison with staff
controls. Journal of psychiatric and mental health nursing, 21(6), pp.483-490.
Evins, A.E., Cather, C. and Daumit, G.L., 2019. Smoking cessation in people with serious
mental illness. The Lancet Psychiatry, 6(7), pp.563-564.
Forman, J., Harris, J.M., Lorencatto, F., McEwen, A. and Duaso, M.J., 2017. National survey of
smoking and smoking cessation education within UK midwifery school curricula. Nicotine &
Tobacco Research, 19(5), pp.591-596.
Forman, J., Harris, J.M., Lorencatto, F., McEwen, A. and Duaso, M.J., 2017. National survey of
smoking and smoking cessation education within UK midwifery school curricula. Nicotine &
Tobacco Research, 19(5), pp.591-596.
Garey, L., Rogers, A.H., Manning, K., Smit, T., Derrick, J.L., Viana, A.G., Schmidt, N.B. and
Zvolensky, M.J., 2020. Effects of smoking cessation treatment attendance on abstinence: The
47SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
moderating role of psychologically based behavioral health conditions. Journal of Substance
Abuse Treatment, 109, pp.1-7.
Gilbody, S., Peckham, E., Bailey, D., Arundel, C., Heron, P., Crosland, S., Fairhurst, C., Hewitt,
C., Li, J., Parrott, S. and Bradshaw, T., 2019. Smoking cessation for people with acute mental
illness (SCIMITAR+): a pragmatic randomised controlled trial. The Lancet Psychiatry, 6(5),
pp.379-390.
Gilbody, S., Peckham, E., Bailey, D., Arundel, C., Heron, P., Crosland, S., Fairhurst, C., Hewitt,
C., Li, J., Parrott, S. and Bradshaw, T., 2019. Smoking cessation for people with acute mental
illness (SCIMITAR+): a pragmatic randomised controlled trial. The Lancet Psychiatry, 6(5),
pp.379-390.
Gough, D. and Richardson, M., 2018. Systematic reviews. In Advanced Research Methods for
Applied Psychology (pp. 75-87). Routledge.
Grewal, A., Kataria, H. and Dhawan, I., 2016. Literature search for research planning and
identification of research problem. Indian journal of anaesthesia, 60(9), p.635.
Harris, K.K., Zopey, M. and Friedman, T.C., 2016. Metabolic effects of smoking
cessation. Nature Reviews Endocrinology, 12(5), p.299.
Heale, R. and Twycross, A., 2015. Validity and reliability in quantitative studies. Evidence-
based nursing, 18(3), pp.66-67.
Hubbard, G., Gorely, T., Ozakinci, G., Polson, R. and Forbat, L., 2016. A systematic review and
narrative summary of family-based smoking cessation interventions to help adults quit
smoking. BMC family practice, 17(1), p.73.
moderating role of psychologically based behavioral health conditions. Journal of Substance
Abuse Treatment, 109, pp.1-7.
Gilbody, S., Peckham, E., Bailey, D., Arundel, C., Heron, P., Crosland, S., Fairhurst, C., Hewitt,
C., Li, J., Parrott, S. and Bradshaw, T., 2019. Smoking cessation for people with acute mental
illness (SCIMITAR+): a pragmatic randomised controlled trial. The Lancet Psychiatry, 6(5),
pp.379-390.
Gilbody, S., Peckham, E., Bailey, D., Arundel, C., Heron, P., Crosland, S., Fairhurst, C., Hewitt,
C., Li, J., Parrott, S. and Bradshaw, T., 2019. Smoking cessation for people with acute mental
illness (SCIMITAR+): a pragmatic randomised controlled trial. The Lancet Psychiatry, 6(5),
pp.379-390.
Gough, D. and Richardson, M., 2018. Systematic reviews. In Advanced Research Methods for
Applied Psychology (pp. 75-87). Routledge.
Grewal, A., Kataria, H. and Dhawan, I., 2016. Literature search for research planning and
identification of research problem. Indian journal of anaesthesia, 60(9), p.635.
Harris, K.K., Zopey, M. and Friedman, T.C., 2016. Metabolic effects of smoking
cessation. Nature Reviews Endocrinology, 12(5), p.299.
Heale, R. and Twycross, A., 2015. Validity and reliability in quantitative studies. Evidence-
based nursing, 18(3), pp.66-67.
Hubbard, G., Gorely, T., Ozakinci, G., Polson, R. and Forbat, L., 2016. A systematic review and
narrative summary of family-based smoking cessation interventions to help adults quit
smoking. BMC family practice, 17(1), p.73.
48SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
Jaén-Moreno, M.J., Feu, N., Redondo-Écija, J., Montiel, F.J., Gómez, C., Del Pozo, G.I., Alcalá,
J.Á., Gutiérrez-Rojas, L., Balanzá-Martinez, V., Chauca, G.M. and Carrión, L., 2019. Smoking
cessation opportunities in acute mental illness (tobacco intensive motivational and estimate risk
—TIMER—): study protocol for a randomized controlled trial. Trials, 20(1), pp.1-11.
King, C.C., Piper, M.E., Gepner, A.D., Fiore, M.C., Baker, T.B. and Stein, J.H., 2017.
Longitudinal impact of smoking and smoking cessation on inflammatory markers of
cardiovascular disease risk. Arteriosclerosis, thrombosis, and vascular biology, 37(2), pp.374-
379.
Knowles, S., Planner, C., Bradshaw, T., Peckham, E., Man, M.S. and Gilbody, S., 2016. Making
the journey with me: a qualitative study of experiences of a bespoke mental health smoking
cessation intervention for service users with serious mental illness. BMC psychiatry, 16(1),
p.193.
Li, J., Fairhurst, C., Peckham, E., Bailey, D., Arundel, C., Hewitt, C., Heron, P., Crosland, S. and
Collaborative, S., 2019. Cost-Effectiveness of a Specialist Smoking Cessation Package
Compared with Standard Smoking Cessation Service for People with Acute Mental Illness in
England: A Trial-Based Economic Evaluation From the SCIMITAR+ Study. Available at SSRN
3393728.
Lonergan, B., Harding, V., Cohen, H., Wylleman, E., Cohen, R. and Stebbing, J., 2019. Harms
of cigarette smoking: call to increase knowledge among children. European Journal of Cancer
Prevention, 28(1), pp.54-57.
Mangera, Z., Lewis, A., Hutchinson, J., Searle, L. and Agrawal, S., 2017. Smoking prevalence in
UK hospital admissions from a national observational study.
Jaén-Moreno, M.J., Feu, N., Redondo-Écija, J., Montiel, F.J., Gómez, C., Del Pozo, G.I., Alcalá,
J.Á., Gutiérrez-Rojas, L., Balanzá-Martinez, V., Chauca, G.M. and Carrión, L., 2019. Smoking
cessation opportunities in acute mental illness (tobacco intensive motivational and estimate risk
—TIMER—): study protocol for a randomized controlled trial. Trials, 20(1), pp.1-11.
King, C.C., Piper, M.E., Gepner, A.D., Fiore, M.C., Baker, T.B. and Stein, J.H., 2017.
Longitudinal impact of smoking and smoking cessation on inflammatory markers of
cardiovascular disease risk. Arteriosclerosis, thrombosis, and vascular biology, 37(2), pp.374-
379.
Knowles, S., Planner, C., Bradshaw, T., Peckham, E., Man, M.S. and Gilbody, S., 2016. Making
the journey with me: a qualitative study of experiences of a bespoke mental health smoking
cessation intervention for service users with serious mental illness. BMC psychiatry, 16(1),
p.193.
Li, J., Fairhurst, C., Peckham, E., Bailey, D., Arundel, C., Hewitt, C., Heron, P., Crosland, S. and
Collaborative, S., 2019. Cost-Effectiveness of a Specialist Smoking Cessation Package
Compared with Standard Smoking Cessation Service for People with Acute Mental Illness in
England: A Trial-Based Economic Evaluation From the SCIMITAR+ Study. Available at SSRN
3393728.
Lonergan, B., Harding, V., Cohen, H., Wylleman, E., Cohen, R. and Stebbing, J., 2019. Harms
of cigarette smoking: call to increase knowledge among children. European Journal of Cancer
Prevention, 28(1), pp.54-57.
Mangera, Z., Lewis, A., Hutchinson, J., Searle, L. and Agrawal, S., 2017. Smoking prevalence in
UK hospital admissions from a national observational study.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
49SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
McGowan, J., Sampson, M., Salzwedel, D.M., Cogo, E., Foerster, V. and Lefebvre, C., 2016.
PRESS peer review of electronic search strategies: 2015 guideline statement. Journal of clinical
epidemiology, 75, pp.40-46.
Miyauchi, M., Kishida, I., Suda, A., Shiraishi, Y., Fujibayashi, M., Taguri, M., Ishii, C., Ishii, N.,
Moritani, T. and Hirayasu, Y., 2017. Long term effects of smoking cessation in hospitalized
schizophrenia patients. BMC psychiatry, 17(1), p.87.
Mohajan, H.K., 2017. Two criteria for good measurements in research: Validity and
reliability. Annals of Spiru Haret University. Economic Series, 17(4), pp.59-82.
Morey, R.D., Chambers, C.D., Etchells, P.J., Harris, C.R., Hoekstra, R., Lakens, D.,
Lewandowsky, S., Morey, C.C., Newman, D.P., Schönbrodt, F.D. and Vanpaemel, W., 2016.
The Peer Reviewers' Openness Initiative: incentivizing open research practices through peer
review. Royal Society Open Science, 3(1), p.150547.
Nardi, P.M., 2018. Doing survey research: A guide to quantitative methods. Routledge.
Nardi, P.M., 2018. Doing survey research: A guide to quantitative methods. Routledge.
NHS, 2014. NHS England » Models of care. [online] England.nhs.uk. Available at:
https://www.england.nhs.uk/new-care-models/about/ [Accessed 25 Feb. 2020].
Osborn, D., Burton, A., Hunter, R., Marston, L., Atkins, L., Barnes, T., Blackburn, R., Craig, T.,
Gilbert, H., Heinkel, S. and Holt, R., 2018. Clinical and cost-effectiveness of an intervention for
reducing cholesterol and cardiovascular risk for people with acute mental illness in English
primary care: a cluster randomised controlled trial. The Lancet Psychiatry, 5(2), pp.145-154.
McGowan, J., Sampson, M., Salzwedel, D.M., Cogo, E., Foerster, V. and Lefebvre, C., 2016.
PRESS peer review of electronic search strategies: 2015 guideline statement. Journal of clinical
epidemiology, 75, pp.40-46.
Miyauchi, M., Kishida, I., Suda, A., Shiraishi, Y., Fujibayashi, M., Taguri, M., Ishii, C., Ishii, N.,
Moritani, T. and Hirayasu, Y., 2017. Long term effects of smoking cessation in hospitalized
schizophrenia patients. BMC psychiatry, 17(1), p.87.
Mohajan, H.K., 2017. Two criteria for good measurements in research: Validity and
reliability. Annals of Spiru Haret University. Economic Series, 17(4), pp.59-82.
Morey, R.D., Chambers, C.D., Etchells, P.J., Harris, C.R., Hoekstra, R., Lakens, D.,
Lewandowsky, S., Morey, C.C., Newman, D.P., Schönbrodt, F.D. and Vanpaemel, W., 2016.
The Peer Reviewers' Openness Initiative: incentivizing open research practices through peer
review. Royal Society Open Science, 3(1), p.150547.
Nardi, P.M., 2018. Doing survey research: A guide to quantitative methods. Routledge.
Nardi, P.M., 2018. Doing survey research: A guide to quantitative methods. Routledge.
NHS, 2014. NHS England » Models of care. [online] England.nhs.uk. Available at:
https://www.england.nhs.uk/new-care-models/about/ [Accessed 25 Feb. 2020].
Osborn, D., Burton, A., Hunter, R., Marston, L., Atkins, L., Barnes, T., Blackburn, R., Craig, T.,
Gilbert, H., Heinkel, S. and Holt, R., 2018. Clinical and cost-effectiveness of an intervention for
reducing cholesterol and cardiovascular risk for people with acute mental illness in English
primary care: a cluster randomised controlled trial. The Lancet Psychiatry, 5(2), pp.145-154.
50SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
Plurphanswat, N., Kaestner, R. and Rodu, B., 2017. The effect of smoking on mental
health. American journal of health behavior, 41(4), pp.471-483.
Public Health England, 2016. Smokefree mental health services in England Implementation
document for providers of mental health services. [online] Assets.publishing.service.gov.uk.
Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/
attachment_data/file/779497/SF_MH_services_in_England__Guidance_for_Providers.pdf
[Accessed 12 Feb. 2020].
Quigley, J.M., Thompson, J.C., Halfpenny, N.J. and Scott, D.A., 2019. Critical appraisal of
nonrandomized studies—A review of recommended and commonly used tools. Journal of
evaluation in clinical practice, 25(1), pp.44-52.
Rademacher, L., Prinz, S., Winz, O., Henkel, K., Dietrich, C.A., Schmaljohann, J., Shali, S.M.,
Schabram, I., Stoppe, C., Cumming, P. and Hilgers, R.D., 2016. Effects of smoking cessation on
presynaptic dopamine function of addicted male smokers. Biological psychiatry, 80(3), pp.198-
206.
Richardson, S., McNeill, A. and Brose, L.S., 2019. Smoking and quitting behaviours by mental
health conditions in Great Britain (1993–2014). Addictive behaviors, 90, pp.14-19.
Roberts, E., Eden Evins, A., McNeill, A. and Robson, D., 2016. Efficacy and tolerability of
pharmacotherapy for smoking cessation in adults with serious mental illness: a systematic review
and network meta‐analysis. Addiction, 111(4), pp.599-612.
Sharma, M., Khubchandani, J. and Nahar, V.K., 2017. Applying a new theory to smoking
cessation: case of multi-theory model (MTM) for health behavior change. Health promotion
perspectives, 7(2), p.102.
Plurphanswat, N., Kaestner, R. and Rodu, B., 2017. The effect of smoking on mental
health. American journal of health behavior, 41(4), pp.471-483.
Public Health England, 2016. Smokefree mental health services in England Implementation
document for providers of mental health services. [online] Assets.publishing.service.gov.uk.
Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/
attachment_data/file/779497/SF_MH_services_in_England__Guidance_for_Providers.pdf
[Accessed 12 Feb. 2020].
Quigley, J.M., Thompson, J.C., Halfpenny, N.J. and Scott, D.A., 2019. Critical appraisal of
nonrandomized studies—A review of recommended and commonly used tools. Journal of
evaluation in clinical practice, 25(1), pp.44-52.
Rademacher, L., Prinz, S., Winz, O., Henkel, K., Dietrich, C.A., Schmaljohann, J., Shali, S.M.,
Schabram, I., Stoppe, C., Cumming, P. and Hilgers, R.D., 2016. Effects of smoking cessation on
presynaptic dopamine function of addicted male smokers. Biological psychiatry, 80(3), pp.198-
206.
Richardson, S., McNeill, A. and Brose, L.S., 2019. Smoking and quitting behaviours by mental
health conditions in Great Britain (1993–2014). Addictive behaviors, 90, pp.14-19.
Roberts, E., Eden Evins, A., McNeill, A. and Robson, D., 2016. Efficacy and tolerability of
pharmacotherapy for smoking cessation in adults with serious mental illness: a systematic review
and network meta‐analysis. Addiction, 111(4), pp.599-612.
Sharma, M., Khubchandani, J. and Nahar, V.K., 2017. Applying a new theory to smoking
cessation: case of multi-theory model (MTM) for health behavior change. Health promotion
perspectives, 7(2), p.102.
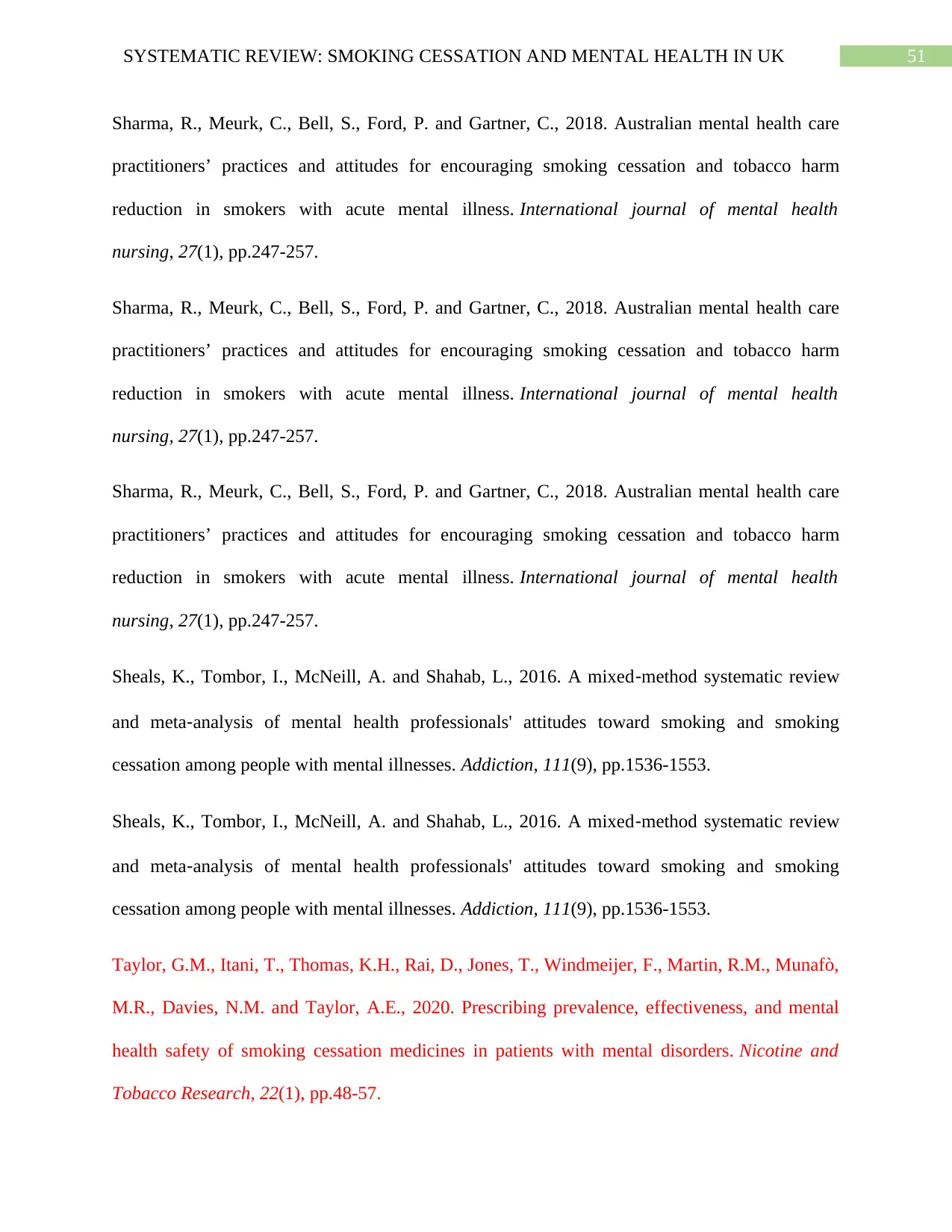
51SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
Sharma, R., Meurk, C., Bell, S., Ford, P. and Gartner, C., 2018. Australian mental health care
practitioners’ practices and attitudes for encouraging smoking cessation and tobacco harm
reduction in smokers with acute mental illness. International journal of mental health
nursing, 27(1), pp.247-257.
Sharma, R., Meurk, C., Bell, S., Ford, P. and Gartner, C., 2018. Australian mental health care
practitioners’ practices and attitudes for encouraging smoking cessation and tobacco harm
reduction in smokers with acute mental illness. International journal of mental health
nursing, 27(1), pp.247-257.
Sharma, R., Meurk, C., Bell, S., Ford, P. and Gartner, C., 2018. Australian mental health care
practitioners’ practices and attitudes for encouraging smoking cessation and tobacco harm
reduction in smokers with acute mental illness. International journal of mental health
nursing, 27(1), pp.247-257.
Sheals, K., Tombor, I., McNeill, A. and Shahab, L., 2016. A mixed‐method systematic review
and meta‐analysis of mental health professionals' attitudes toward smoking and smoking
cessation among people with mental illnesses. Addiction, 111(9), pp.1536-1553.
Sheals, K., Tombor, I., McNeill, A. and Shahab, L., 2016. A mixed‐method systematic review
and meta‐analysis of mental health professionals' attitudes toward smoking and smoking
cessation among people with mental illnesses. Addiction, 111(9), pp.1536-1553.
Taylor, G.M., Itani, T., Thomas, K.H., Rai, D., Jones, T., Windmeijer, F., Martin, R.M., Munafò,
M.R., Davies, N.M. and Taylor, A.E., 2020. Prescribing prevalence, effectiveness, and mental
health safety of smoking cessation medicines in patients with mental disorders. Nicotine and
Tobacco Research, 22(1), pp.48-57.
Sharma, R., Meurk, C., Bell, S., Ford, P. and Gartner, C., 2018. Australian mental health care
practitioners’ practices and attitudes for encouraging smoking cessation and tobacco harm
reduction in smokers with acute mental illness. International journal of mental health
nursing, 27(1), pp.247-257.
Sharma, R., Meurk, C., Bell, S., Ford, P. and Gartner, C., 2018. Australian mental health care
practitioners’ practices and attitudes for encouraging smoking cessation and tobacco harm
reduction in smokers with acute mental illness. International journal of mental health
nursing, 27(1), pp.247-257.
Sharma, R., Meurk, C., Bell, S., Ford, P. and Gartner, C., 2018. Australian mental health care
practitioners’ practices and attitudes for encouraging smoking cessation and tobacco harm
reduction in smokers with acute mental illness. International journal of mental health
nursing, 27(1), pp.247-257.
Sheals, K., Tombor, I., McNeill, A. and Shahab, L., 2016. A mixed‐method systematic review
and meta‐analysis of mental health professionals' attitudes toward smoking and smoking
cessation among people with mental illnesses. Addiction, 111(9), pp.1536-1553.
Sheals, K., Tombor, I., McNeill, A. and Shahab, L., 2016. A mixed‐method systematic review
and meta‐analysis of mental health professionals' attitudes toward smoking and smoking
cessation among people with mental illnesses. Addiction, 111(9), pp.1536-1553.
Taylor, G.M., Itani, T., Thomas, K.H., Rai, D., Jones, T., Windmeijer, F., Martin, R.M., Munafò,
M.R., Davies, N.M. and Taylor, A.E., 2020. Prescribing prevalence, effectiveness, and mental
health safety of smoking cessation medicines in patients with mental disorders. Nicotine and
Tobacco Research, 22(1), pp.48-57.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
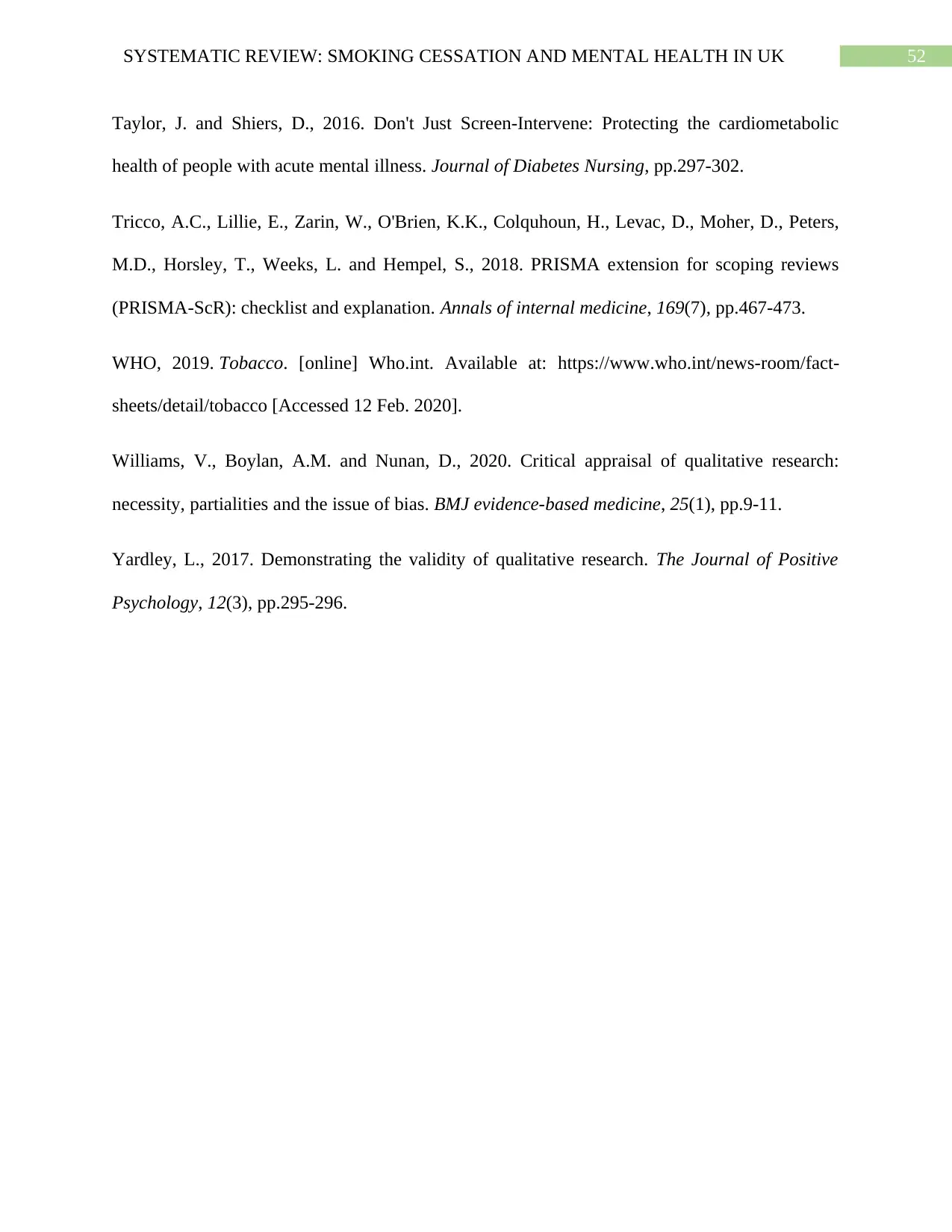
52SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
Taylor, J. and Shiers, D., 2016. Don't Just Screen-Intervene: Protecting the cardiometabolic
health of people with acute mental illness. Journal of Diabetes Nursing, pp.297-302.
Tricco, A.C., Lillie, E., Zarin, W., O'Brien, K.K., Colquhoun, H., Levac, D., Moher, D., Peters,
M.D., Horsley, T., Weeks, L. and Hempel, S., 2018. PRISMA extension for scoping reviews
(PRISMA-ScR): checklist and explanation. Annals of internal medicine, 169(7), pp.467-473.
WHO, 2019. Tobacco. [online] Who.int. Available at: https://www.who.int/news-room/fact-
sheets/detail/tobacco [Accessed 12 Feb. 2020].
Williams, V., Boylan, A.M. and Nunan, D., 2020. Critical appraisal of qualitative research:
necessity, partialities and the issue of bias. BMJ evidence-based medicine, 25(1), pp.9-11.
Yardley, L., 2017. Demonstrating the validity of qualitative research. The Journal of Positive
Psychology, 12(3), pp.295-296.
Taylor, J. and Shiers, D., 2016. Don't Just Screen-Intervene: Protecting the cardiometabolic
health of people with acute mental illness. Journal of Diabetes Nursing, pp.297-302.
Tricco, A.C., Lillie, E., Zarin, W., O'Brien, K.K., Colquhoun, H., Levac, D., Moher, D., Peters,
M.D., Horsley, T., Weeks, L. and Hempel, S., 2018. PRISMA extension for scoping reviews
(PRISMA-ScR): checklist and explanation. Annals of internal medicine, 169(7), pp.467-473.
WHO, 2019. Tobacco. [online] Who.int. Available at: https://www.who.int/news-room/fact-
sheets/detail/tobacco [Accessed 12 Feb. 2020].
Williams, V., Boylan, A.M. and Nunan, D., 2020. Critical appraisal of qualitative research:
necessity, partialities and the issue of bias. BMJ evidence-based medicine, 25(1), pp.9-11.
Yardley, L., 2017. Demonstrating the validity of qualitative research. The Journal of Positive
Psychology, 12(3), pp.295-296.
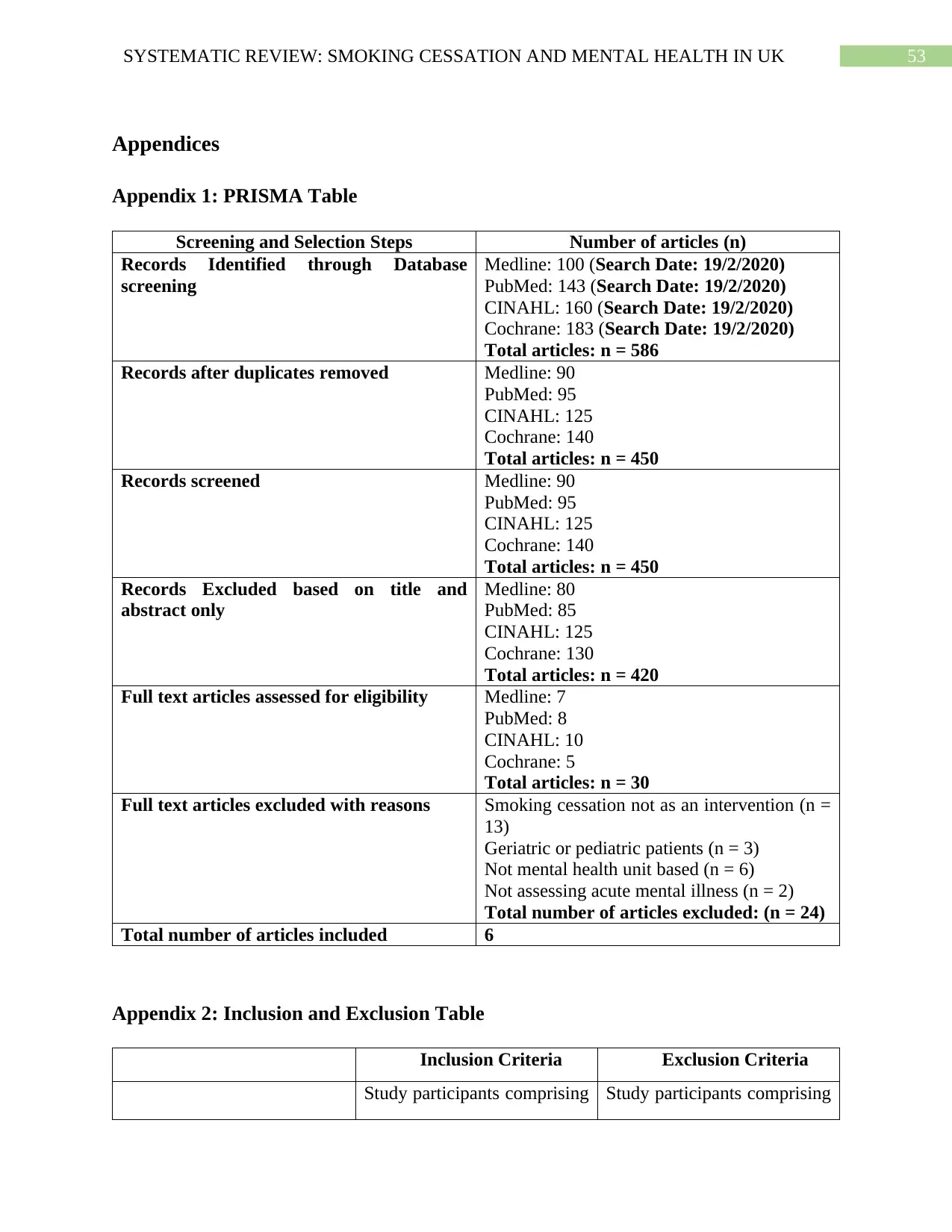
53SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
Appendices
Appendix 1: PRISMA Table
Screening and Selection Steps Number of articles (n)
Records Identified through Database
screening
Medline: 100 (Search Date: 19/2/2020)
PubMed: 143 (Search Date: 19/2/2020)
CINAHL: 160 (Search Date: 19/2/2020)
Cochrane: 183 (Search Date: 19/2/2020)
Total articles: n = 586
Records after duplicates removed Medline: 90
PubMed: 95
CINAHL: 125
Cochrane: 140
Total articles: n = 450
Records screened Medline: 90
PubMed: 95
CINAHL: 125
Cochrane: 140
Total articles: n = 450
Records Excluded based on title and
abstract only
Medline: 80
PubMed: 85
CINAHL: 125
Cochrane: 130
Total articles: n = 420
Full text articles assessed for eligibility Medline: 7
PubMed: 8
CINAHL: 10
Cochrane: 5
Total articles: n = 30
Full text articles excluded with reasons Smoking cessation not as an intervention (n =
13)
Geriatric or pediatric patients (n = 3)
Not mental health unit based (n = 6)
Not assessing acute mental illness (n = 2)
Total number of articles excluded: (n = 24)
Total number of articles included 6
Appendix 2: Inclusion and Exclusion Table
Inclusion Criteria Exclusion Criteria
Study participants comprising Study participants comprising
Appendices
Appendix 1: PRISMA Table
Screening and Selection Steps Number of articles (n)
Records Identified through Database
screening
Medline: 100 (Search Date: 19/2/2020)
PubMed: 143 (Search Date: 19/2/2020)
CINAHL: 160 (Search Date: 19/2/2020)
Cochrane: 183 (Search Date: 19/2/2020)
Total articles: n = 586
Records after duplicates removed Medline: 90
PubMed: 95
CINAHL: 125
Cochrane: 140
Total articles: n = 450
Records screened Medline: 90
PubMed: 95
CINAHL: 125
Cochrane: 140
Total articles: n = 450
Records Excluded based on title and
abstract only
Medline: 80
PubMed: 85
CINAHL: 125
Cochrane: 130
Total articles: n = 420
Full text articles assessed for eligibility Medline: 7
PubMed: 8
CINAHL: 10
Cochrane: 5
Total articles: n = 30
Full text articles excluded with reasons Smoking cessation not as an intervention (n =
13)
Geriatric or pediatric patients (n = 3)
Not mental health unit based (n = 6)
Not assessing acute mental illness (n = 2)
Total number of articles excluded: (n = 24)
Total number of articles included 6
Appendix 2: Inclusion and Exclusion Table
Inclusion Criteria Exclusion Criteria
Study participants comprising Study participants comprising
54SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
POPULATION of adult patients (age 21 to 55
years) with acute mental
illnesses admitted in mental
health settings of UK based
healthcare organizations
of paediatric and geriatric
patients or adult patients
without acute mental illnesses
or admitted in non-UK based
mental healthcare settings.
INTERVENTION
Interventions prioritizing
smoking cessation
Studies with interventions not
associated with smoking
cessation.
COMPARATIVE GROUPS
Absence of smoking
cessation
Absence of smoking
cessation
OUTCOME
Reduced severity and
frequency of mental health
symptoms, improved sense of
quality of life and wellbeing.
Cost analysis between mental
health interventions and
reduction of only health
outcomes other than those
associated with mental health.
TYPE OF STUDY
Methodologies like
systematic reviews,
qualitative studies,
randomized controlled trials,
cross sectional or
observational studies, with
interventions implemented
for a duration of 3 months or
more and published since the
last 7 years (2013 to 2020).
Newspaper reports, editorials,
protocols or opinion articles,
studies with interventions
implemented less than 3
months and older than the last
7 years (2013 to 2020).
Appendix 3: CASP Tool for Cohort Studies (Richardson, McNeill and Brose 2019;
Taylor et al. 2020)
SCREENING QUESTIONS Answers
Richardson,
McNeill and
Brose (2019)
Taylor et al. (2020)
Did the study address a clearly focused issue? Yes Yes
Did the authors use an appropriate method to
answer their question?
Yes Yes
Was the cohort recruited in an acceptable
way?
Yes Yes
Was the exposure accurately measured to
minimize bias?
Yes Yes
POPULATION of adult patients (age 21 to 55
years) with acute mental
illnesses admitted in mental
health settings of UK based
healthcare organizations
of paediatric and geriatric
patients or adult patients
without acute mental illnesses
or admitted in non-UK based
mental healthcare settings.
INTERVENTION
Interventions prioritizing
smoking cessation
Studies with interventions not
associated with smoking
cessation.
COMPARATIVE GROUPS
Absence of smoking
cessation
Absence of smoking
cessation
OUTCOME
Reduced severity and
frequency of mental health
symptoms, improved sense of
quality of life and wellbeing.
Cost analysis between mental
health interventions and
reduction of only health
outcomes other than those
associated with mental health.
TYPE OF STUDY
Methodologies like
systematic reviews,
qualitative studies,
randomized controlled trials,
cross sectional or
observational studies, with
interventions implemented
for a duration of 3 months or
more and published since the
last 7 years (2013 to 2020).
Newspaper reports, editorials,
protocols or opinion articles,
studies with interventions
implemented less than 3
months and older than the last
7 years (2013 to 2020).
Appendix 3: CASP Tool for Cohort Studies (Richardson, McNeill and Brose 2019;
Taylor et al. 2020)
SCREENING QUESTIONS Answers
Richardson,
McNeill and
Brose (2019)
Taylor et al. (2020)
Did the study address a clearly focused issue? Yes Yes
Did the authors use an appropriate method to
answer their question?
Yes Yes
Was the cohort recruited in an acceptable
way?
Yes Yes
Was the exposure accurately measured to
minimize bias?
Yes Yes
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
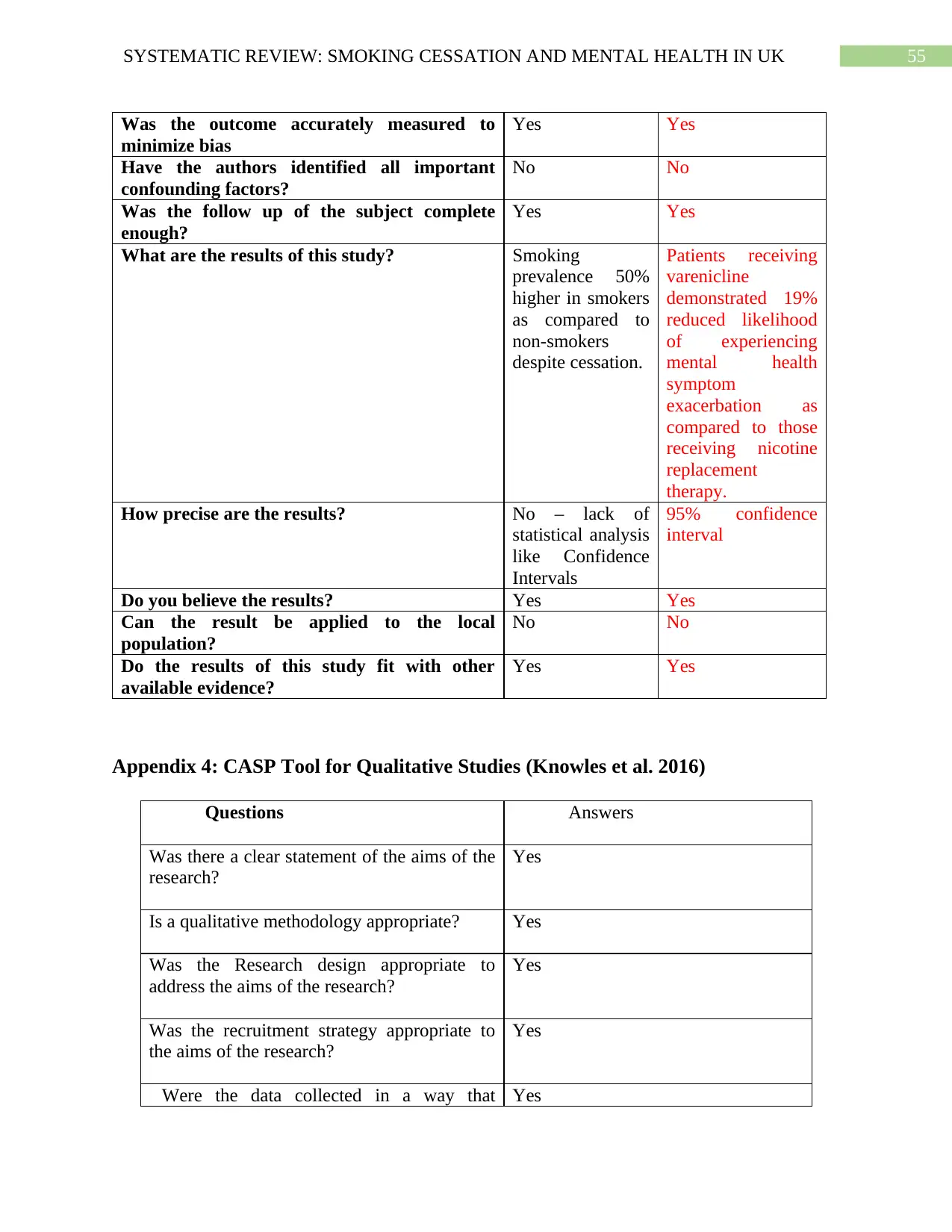
55SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
Was the outcome accurately measured to
minimize bias
Yes Yes
Have the authors identified all important
confounding factors?
No No
Was the follow up of the subject complete
enough?
Yes Yes
What are the results of this study? Smoking
prevalence 50%
higher in smokers
as compared to
non-smokers
despite cessation.
Patients receiving
varenicline
demonstrated 19%
reduced likelihood
of experiencing
mental health
symptom
exacerbation as
compared to those
receiving nicotine
replacement
therapy.
How precise are the results? No – lack of
statistical analysis
like Confidence
Intervals
95% confidence
interval
Do you believe the results? Yes Yes
Can the result be applied to the local
population?
No No
Do the results of this study fit with other
available evidence?
Yes Yes
Appendix 4: CASP Tool for Qualitative Studies (Knowles et al. 2016)
Questions Answers
Was there a clear statement of the aims of the
research?
Yes
Is a qualitative methodology appropriate? Yes
Was the Research design appropriate to
address the aims of the research?
Yes
Was the recruitment strategy appropriate to
the aims of the research?
Yes
Were the data collected in a way that Yes
Was the outcome accurately measured to
minimize bias
Yes Yes
Have the authors identified all important
confounding factors?
No No
Was the follow up of the subject complete
enough?
Yes Yes
What are the results of this study? Smoking
prevalence 50%
higher in smokers
as compared to
non-smokers
despite cessation.
Patients receiving
varenicline
demonstrated 19%
reduced likelihood
of experiencing
mental health
symptom
exacerbation as
compared to those
receiving nicotine
replacement
therapy.
How precise are the results? No – lack of
statistical analysis
like Confidence
Intervals
95% confidence
interval
Do you believe the results? Yes Yes
Can the result be applied to the local
population?
No No
Do the results of this study fit with other
available evidence?
Yes Yes
Appendix 4: CASP Tool for Qualitative Studies (Knowles et al. 2016)
Questions Answers
Was there a clear statement of the aims of the
research?
Yes
Is a qualitative methodology appropriate? Yes
Was the Research design appropriate to
address the aims of the research?
Yes
Was the recruitment strategy appropriate to
the aims of the research?
Yes
Were the data collected in a way that Yes
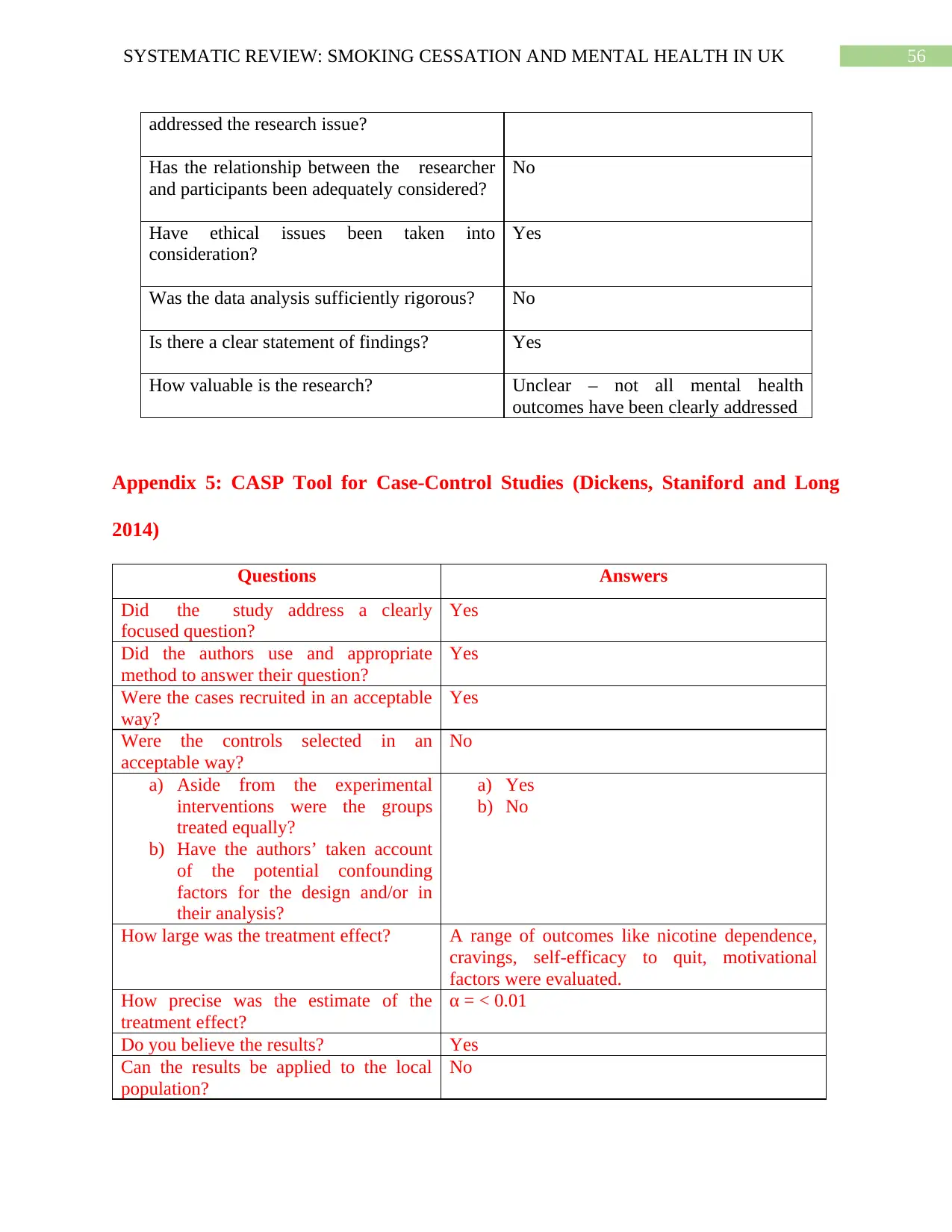
56SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
addressed the research issue?
Has the relationship between the researcher
and participants been adequately considered?
No
Have ethical issues been taken into
consideration?
Yes
Was the data analysis sufficiently rigorous? No
Is there a clear statement of findings? Yes
How valuable is the research? Unclear – not all mental health
outcomes have been clearly addressed
Appendix 5: CASP Tool for Case-Control Studies (Dickens, Staniford and Long
2014)
Questions Answers
Did the study address a clearly
focused question?
Yes
Did the authors use and appropriate
method to answer their question?
Yes
Were the cases recruited in an acceptable
way?
Yes
Were the controls selected in an
acceptable way?
No
a) Aside from the experimental
interventions were the groups
treated equally?
b) Have the authors’ taken account
of the potential confounding
factors for the design and/or in
their analysis?
a) Yes
b) No
How large was the treatment effect? A range of outcomes like nicotine dependence,
cravings, self-efficacy to quit, motivational
factors were evaluated.
How precise was the estimate of the
treatment effect?
α = < 0.01
Do you believe the results? Yes
Can the results be applied to the local
population?
No
addressed the research issue?
Has the relationship between the researcher
and participants been adequately considered?
No
Have ethical issues been taken into
consideration?
Yes
Was the data analysis sufficiently rigorous? No
Is there a clear statement of findings? Yes
How valuable is the research? Unclear – not all mental health
outcomes have been clearly addressed
Appendix 5: CASP Tool for Case-Control Studies (Dickens, Staniford and Long
2014)
Questions Answers
Did the study address a clearly
focused question?
Yes
Did the authors use and appropriate
method to answer their question?
Yes
Were the cases recruited in an acceptable
way?
Yes
Were the controls selected in an
acceptable way?
No
a) Aside from the experimental
interventions were the groups
treated equally?
b) Have the authors’ taken account
of the potential confounding
factors for the design and/or in
their analysis?
a) Yes
b) No
How large was the treatment effect? A range of outcomes like nicotine dependence,
cravings, self-efficacy to quit, motivational
factors were evaluated.
How precise was the estimate of the
treatment effect?
α = < 0.01
Do you believe the results? Yes
Can the results be applied to the local
population?
No
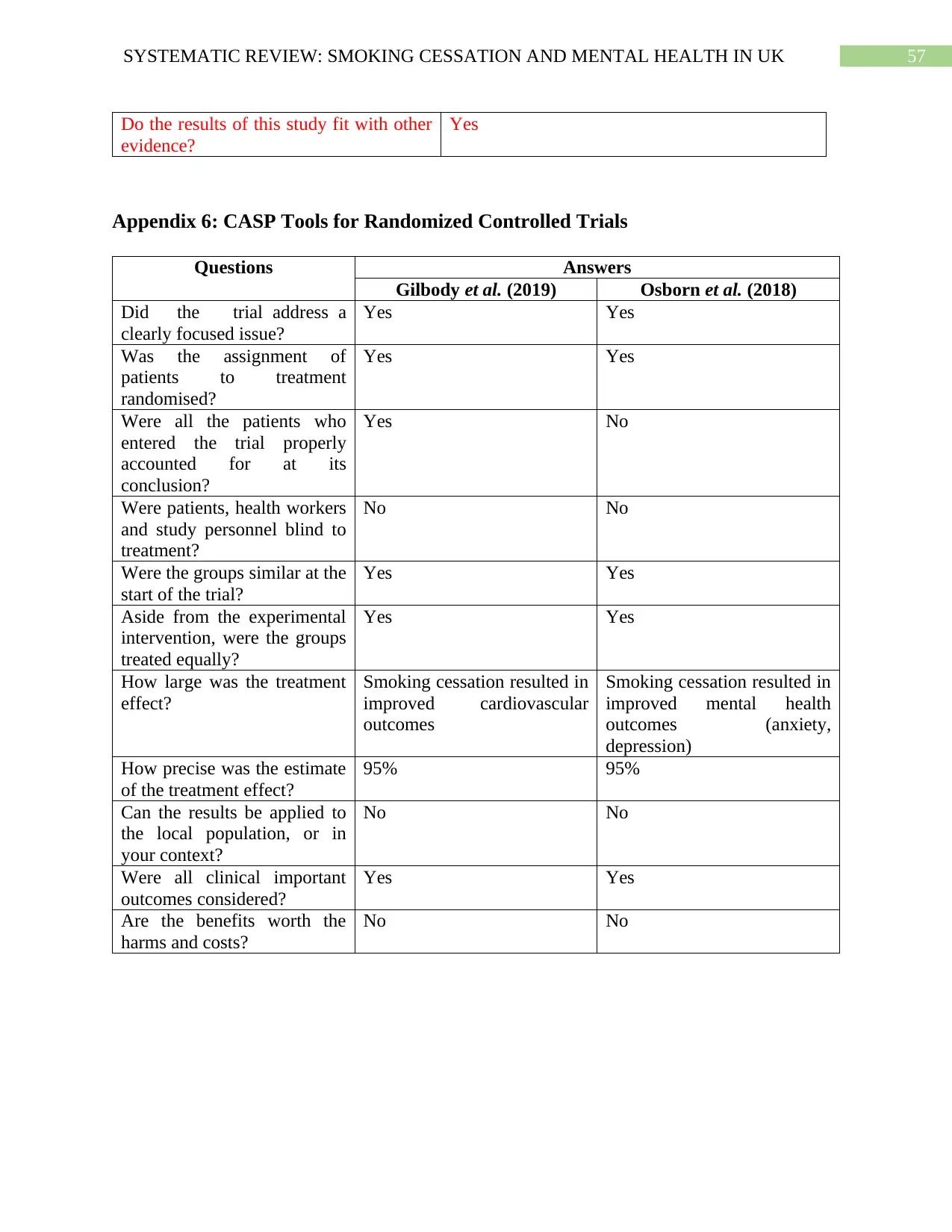
57SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
Do the results of this study fit with other
evidence?
Yes
Appendix 6: CASP Tools for Randomized Controlled Trials
Questions Answers
Gilbody et al. (2019) Osborn et al. (2018)
Did the trial address a
clearly focused issue?
Yes Yes
Was the assignment of
patients to treatment
randomised?
Yes Yes
Were all the patients who
entered the trial properly
accounted for at its
conclusion?
Yes No
Were patients, health workers
and study personnel blind to
treatment?
No No
Were the groups similar at the
start of the trial?
Yes Yes
Aside from the experimental
intervention, were the groups
treated equally?
Yes Yes
How large was the treatment
effect?
Smoking cessation resulted in
improved cardiovascular
outcomes
Smoking cessation resulted in
improved mental health
outcomes (anxiety,
depression)
How precise was the estimate
of the treatment effect?
95% 95%
Can the results be applied to
the local population, or in
your context?
No No
Were all clinical important
outcomes considered?
Yes Yes
Are the benefits worth the
harms and costs?
No No
Do the results of this study fit with other
evidence?
Yes
Appendix 6: CASP Tools for Randomized Controlled Trials
Questions Answers
Gilbody et al. (2019) Osborn et al. (2018)
Did the trial address a
clearly focused issue?
Yes Yes
Was the assignment of
patients to treatment
randomised?
Yes Yes
Were all the patients who
entered the trial properly
accounted for at its
conclusion?
Yes No
Were patients, health workers
and study personnel blind to
treatment?
No No
Were the groups similar at the
start of the trial?
Yes Yes
Aside from the experimental
intervention, were the groups
treated equally?
Yes Yes
How large was the treatment
effect?
Smoking cessation resulted in
improved cardiovascular
outcomes
Smoking cessation resulted in
improved mental health
outcomes (anxiety,
depression)
How precise was the estimate
of the treatment effect?
95% 95%
Can the results be applied to
the local population, or in
your context?
No No
Were all clinical important
outcomes considered?
Yes Yes
Are the benefits worth the
harms and costs?
No No
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
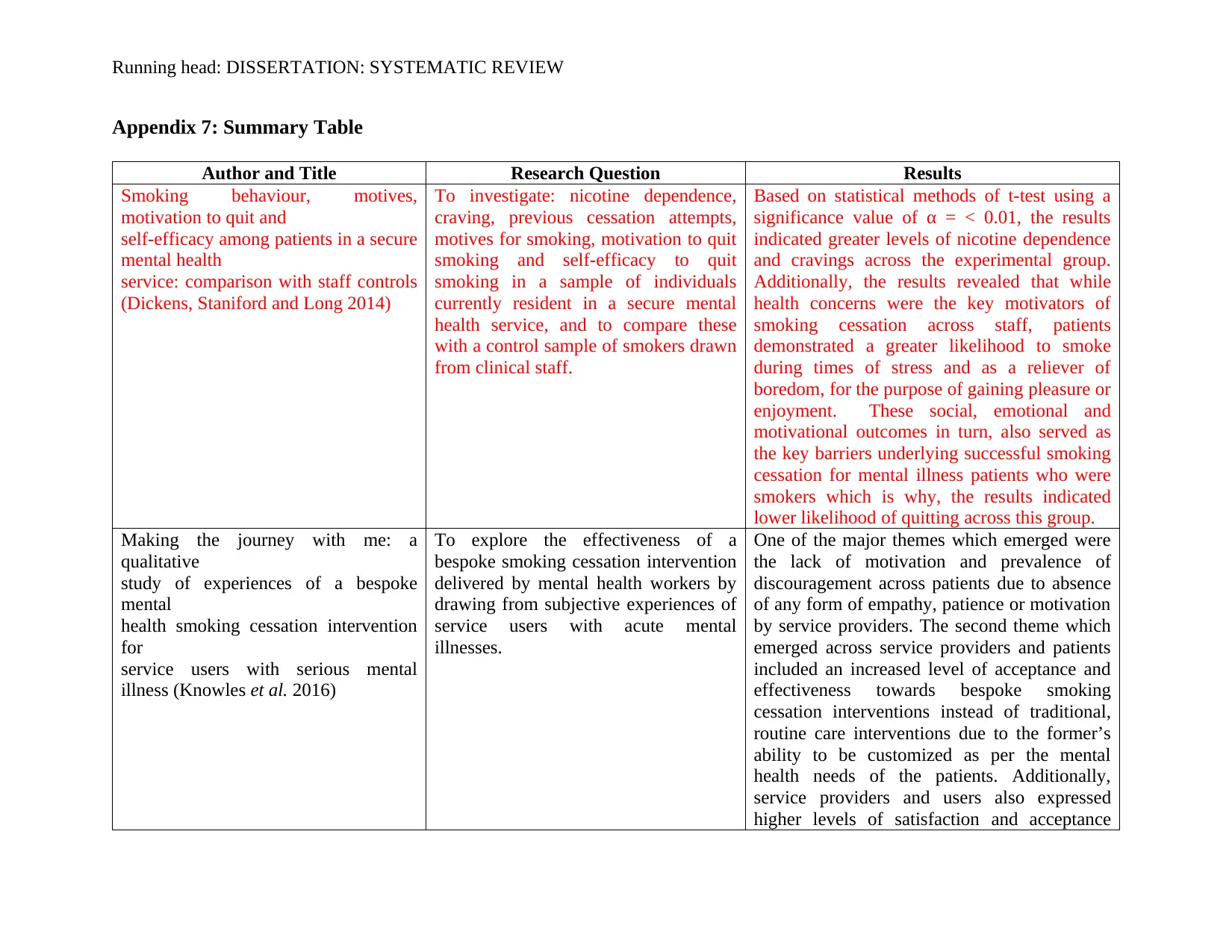
Running head: DISSERTATION: SYSTEMATIC REVIEW
Appendix 7: Summary Table
Author and Title Research Question Results
Smoking behaviour, motives,
motivation to quit and
self-efficacy among patients in a secure
mental health
service: comparison with staff controls
(Dickens, Staniford and Long 2014)
To investigate: nicotine dependence,
craving, previous cessation attempts,
motives for smoking, motivation to quit
smoking and self-efficacy to quit
smoking in a sample of individuals
currently resident in a secure mental
health service, and to compare these
with a control sample of smokers drawn
from clinical staff.
Based on statistical methods of t-test using a
significance value of α = < 0.01, the results
indicated greater levels of nicotine dependence
and cravings across the experimental group.
Additionally, the results revealed that while
health concerns were the key motivators of
smoking cessation across staff, patients
demonstrated a greater likelihood to smoke
during times of stress and as a reliever of
boredom, for the purpose of gaining pleasure or
enjoyment. These social, emotional and
motivational outcomes in turn, also served as
the key barriers underlying successful smoking
cessation for mental illness patients who were
smokers which is why, the results indicated
lower likelihood of quitting across this group.
Making the journey with me: a
qualitative
study of experiences of a bespoke
mental
health smoking cessation intervention
for
service users with serious mental
illness (Knowles et al. 2016)
To explore the effectiveness of a
bespoke smoking cessation intervention
delivered by mental health workers by
drawing from subjective experiences of
service users with acute mental
illnesses.
One of the major themes which emerged were
the lack of motivation and prevalence of
discouragement across patients due to absence
of any form of empathy, patience or motivation
by service providers. The second theme which
emerged across service providers and patients
included an increased level of acceptance and
effectiveness towards bespoke smoking
cessation interventions instead of traditional,
routine care interventions due to the former’s
ability to be customized as per the mental
health needs of the patients. Additionally,
service providers and users also expressed
higher levels of satisfaction and acceptance
Appendix 7: Summary Table
Author and Title Research Question Results
Smoking behaviour, motives,
motivation to quit and
self-efficacy among patients in a secure
mental health
service: comparison with staff controls
(Dickens, Staniford and Long 2014)
To investigate: nicotine dependence,
craving, previous cessation attempts,
motives for smoking, motivation to quit
smoking and self-efficacy to quit
smoking in a sample of individuals
currently resident in a secure mental
health service, and to compare these
with a control sample of smokers drawn
from clinical staff.
Based on statistical methods of t-test using a
significance value of α = < 0.01, the results
indicated greater levels of nicotine dependence
and cravings across the experimental group.
Additionally, the results revealed that while
health concerns were the key motivators of
smoking cessation across staff, patients
demonstrated a greater likelihood to smoke
during times of stress and as a reliever of
boredom, for the purpose of gaining pleasure or
enjoyment. These social, emotional and
motivational outcomes in turn, also served as
the key barriers underlying successful smoking
cessation for mental illness patients who were
smokers which is why, the results indicated
lower likelihood of quitting across this group.
Making the journey with me: a
qualitative
study of experiences of a bespoke
mental
health smoking cessation intervention
for
service users with serious mental
illness (Knowles et al. 2016)
To explore the effectiveness of a
bespoke smoking cessation intervention
delivered by mental health workers by
drawing from subjective experiences of
service users with acute mental
illnesses.
One of the major themes which emerged were
the lack of motivation and prevalence of
discouragement across patients due to absence
of any form of empathy, patience or motivation
by service providers. The second theme which
emerged across service providers and patients
included an increased level of acceptance and
effectiveness towards bespoke smoking
cessation interventions instead of traditional,
routine care interventions due to the former’s
ability to be customized as per the mental
health needs of the patients. Additionally,
service providers and users also expressed
higher levels of satisfaction and acceptance
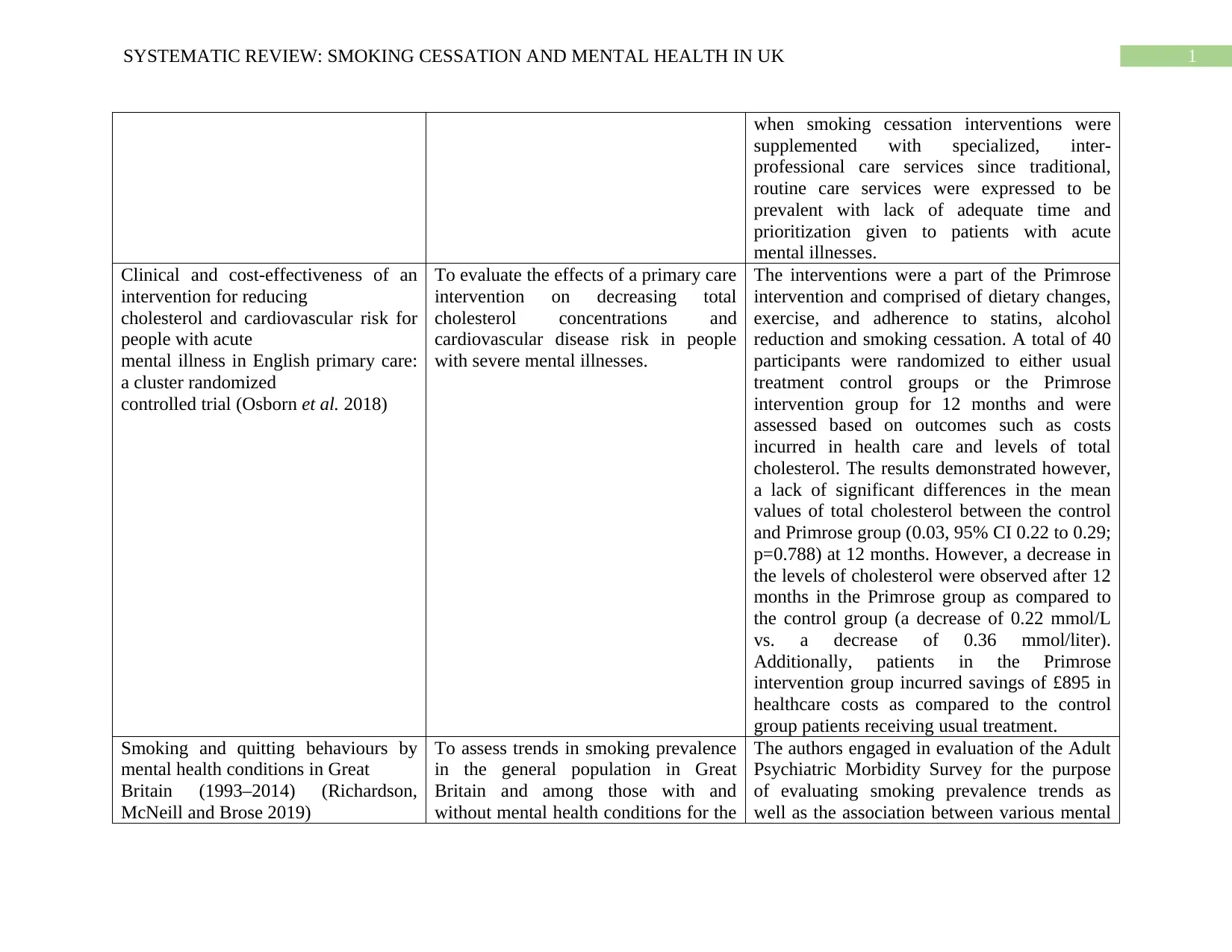
1SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
when smoking cessation interventions were
supplemented with specialized, inter-
professional care services since traditional,
routine care services were expressed to be
prevalent with lack of adequate time and
prioritization given to patients with acute
mental illnesses.
Clinical and cost-effectiveness of an
intervention for reducing
cholesterol and cardiovascular risk for
people with acute
mental illness in English primary care:
a cluster randomized
controlled trial (Osborn et al. 2018)
To evaluate the effects of a primary care
intervention on decreasing total
cholesterol concentrations and
cardiovascular disease risk in people
with severe mental illnesses.
The interventions were a part of the Primrose
intervention and comprised of dietary changes,
exercise, and adherence to statins, alcohol
reduction and smoking cessation. A total of 40
participants were randomized to either usual
treatment control groups or the Primrose
intervention group for 12 months and were
assessed based on outcomes such as costs
incurred in health care and levels of total
cholesterol. The results demonstrated however,
a lack of significant differences in the mean
values of total cholesterol between the control
and Primrose group (0.03, 95% CI 0.22 to 0.29;
p=0.788) at 12 months. However, a decrease in
the levels of cholesterol were observed after 12
months in the Primrose group as compared to
the control group (a decrease of 0.22 mmol/L
vs. a decrease of 0.36 mmol/liter).
Additionally, patients in the Primrose
intervention group incurred savings of £895 in
healthcare costs as compared to the control
group patients receiving usual treatment.
Smoking and quitting behaviours by
mental health conditions in Great
Britain (1993–2014) (Richardson,
McNeill and Brose 2019)
To assess trends in smoking prevalence
in the general population in Great
Britain and among those with and
without mental health conditions for the
The authors engaged in evaluation of the Adult
Psychiatric Morbidity Survey for the purpose
of evaluating smoking prevalence trends as
well as the association between various mental
when smoking cessation interventions were
supplemented with specialized, inter-
professional care services since traditional,
routine care services were expressed to be
prevalent with lack of adequate time and
prioritization given to patients with acute
mental illnesses.
Clinical and cost-effectiveness of an
intervention for reducing
cholesterol and cardiovascular risk for
people with acute
mental illness in English primary care:
a cluster randomized
controlled trial (Osborn et al. 2018)
To evaluate the effects of a primary care
intervention on decreasing total
cholesterol concentrations and
cardiovascular disease risk in people
with severe mental illnesses.
The interventions were a part of the Primrose
intervention and comprised of dietary changes,
exercise, and adherence to statins, alcohol
reduction and smoking cessation. A total of 40
participants were randomized to either usual
treatment control groups or the Primrose
intervention group for 12 months and were
assessed based on outcomes such as costs
incurred in health care and levels of total
cholesterol. The results demonstrated however,
a lack of significant differences in the mean
values of total cholesterol between the control
and Primrose group (0.03, 95% CI 0.22 to 0.29;
p=0.788) at 12 months. However, a decrease in
the levels of cholesterol were observed after 12
months in the Primrose group as compared to
the control group (a decrease of 0.22 mmol/L
vs. a decrease of 0.36 mmol/liter).
Additionally, patients in the Primrose
intervention group incurred savings of £895 in
healthcare costs as compared to the control
group patients receiving usual treatment.
Smoking and quitting behaviours by
mental health conditions in Great
Britain (1993–2014) (Richardson,
McNeill and Brose 2019)
To assess trends in smoking prevalence
in the general population in Great
Britain and among those with and
without mental health conditions for the
The authors engaged in evaluation of the Adult
Psychiatric Morbidity Survey for the purpose
of evaluating smoking prevalence trends as
well as the association between various mental
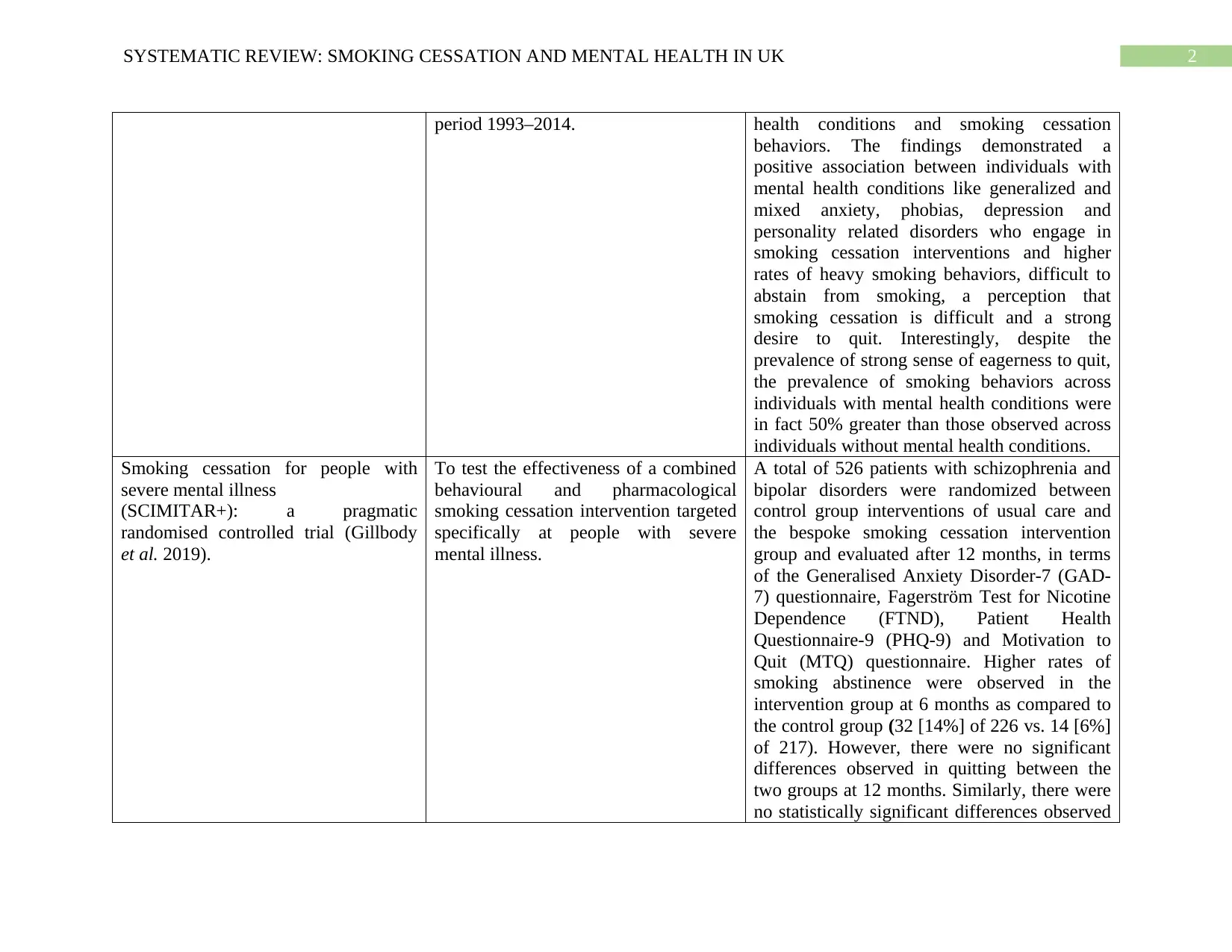
2SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
period 1993–2014. health conditions and smoking cessation
behaviors. The findings demonstrated a
positive association between individuals with
mental health conditions like generalized and
mixed anxiety, phobias, depression and
personality related disorders who engage in
smoking cessation interventions and higher
rates of heavy smoking behaviors, difficult to
abstain from smoking, a perception that
smoking cessation is difficult and a strong
desire to quit. Interestingly, despite the
prevalence of strong sense of eagerness to quit,
the prevalence of smoking behaviors across
individuals with mental health conditions were
in fact 50% greater than those observed across
individuals without mental health conditions.
Smoking cessation for people with
severe mental illness
(SCIMITAR+): a pragmatic
randomised controlled trial (Gillbody
et al. 2019).
To test the effectiveness of a combined
behavioural and pharmacological
smoking cessation intervention targeted
specifically at people with severe
mental illness.
A total of 526 patients with schizophrenia and
bipolar disorders were randomized between
control group interventions of usual care and
the bespoke smoking cessation intervention
group and evaluated after 12 months, in terms
of the Generalised Anxiety Disorder-7 (GAD-
7) questionnaire, Fagerström Test for Nicotine
Dependence (FTND), Patient Health
Questionnaire-9 (PHQ-9) and Motivation to
Quit (MTQ) questionnaire. Higher rates of
smoking abstinence were observed in the
intervention group at 6 months as compared to
the control group (32 [14%] of 226 vs. 14 [6%]
of 217). However, there were no significant
differences observed in quitting between the
two groups at 12 months. Similarly, there were
no statistically significant differences observed
period 1993–2014. health conditions and smoking cessation
behaviors. The findings demonstrated a
positive association between individuals with
mental health conditions like generalized and
mixed anxiety, phobias, depression and
personality related disorders who engage in
smoking cessation interventions and higher
rates of heavy smoking behaviors, difficult to
abstain from smoking, a perception that
smoking cessation is difficult and a strong
desire to quit. Interestingly, despite the
prevalence of strong sense of eagerness to quit,
the prevalence of smoking behaviors across
individuals with mental health conditions were
in fact 50% greater than those observed across
individuals without mental health conditions.
Smoking cessation for people with
severe mental illness
(SCIMITAR+): a pragmatic
randomised controlled trial (Gillbody
et al. 2019).
To test the effectiveness of a combined
behavioural and pharmacological
smoking cessation intervention targeted
specifically at people with severe
mental illness.
A total of 526 patients with schizophrenia and
bipolar disorders were randomized between
control group interventions of usual care and
the bespoke smoking cessation intervention
group and evaluated after 12 months, in terms
of the Generalised Anxiety Disorder-7 (GAD-
7) questionnaire, Fagerström Test for Nicotine
Dependence (FTND), Patient Health
Questionnaire-9 (PHQ-9) and Motivation to
Quit (MTQ) questionnaire. Higher rates of
smoking abstinence were observed in the
intervention group at 6 months as compared to
the control group (32 [14%] of 226 vs. 14 [6%]
of 217). However, there were no significant
differences observed in quitting between the
two groups at 12 months. Similarly, there were
no statistically significant differences observed
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
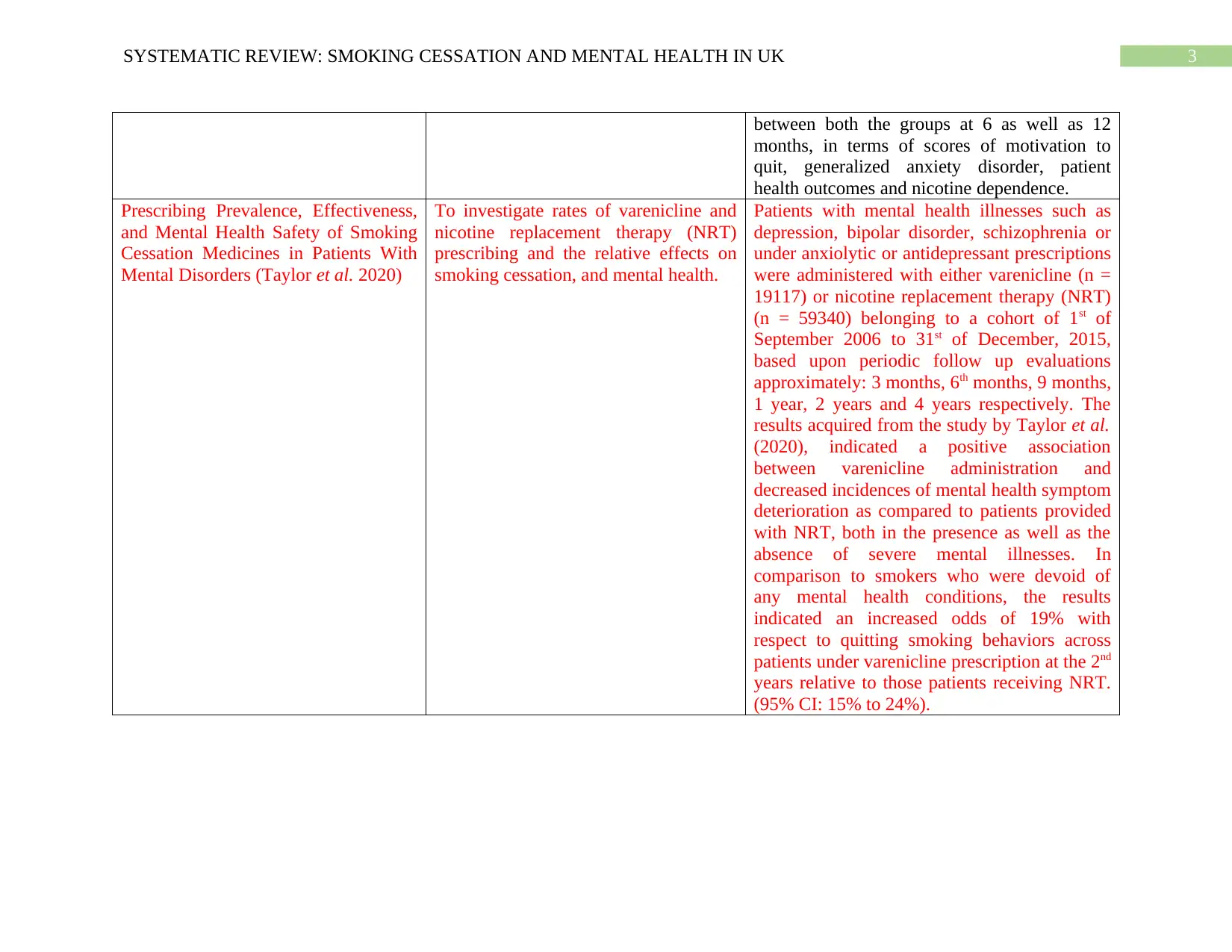
3SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
between both the groups at 6 as well as 12
months, in terms of scores of motivation to
quit, generalized anxiety disorder, patient
health outcomes and nicotine dependence.
Prescribing Prevalence, Effectiveness,
and Mental Health Safety of Smoking
Cessation Medicines in Patients With
Mental Disorders (Taylor et al. 2020)
To investigate rates of varenicline and
nicotine replacement therapy (NRT)
prescribing and the relative effects on
smoking cessation, and mental health.
Patients with mental health illnesses such as
depression, bipolar disorder, schizophrenia or
under anxiolytic or antidepressant prescriptions
were administered with either varenicline (n =
19117) or nicotine replacement therapy (NRT)
(n = 59340) belonging to a cohort of 1st of
September 2006 to 31st of December, 2015,
based upon periodic follow up evaluations
approximately: 3 months, 6th months, 9 months,
1 year, 2 years and 4 years respectively. The
results acquired from the study by Taylor et al.
(2020), indicated a positive association
between varenicline administration and
decreased incidences of mental health symptom
deterioration as compared to patients provided
with NRT, both in the presence as well as the
absence of severe mental illnesses. In
comparison to smokers who were devoid of
any mental health conditions, the results
indicated an increased odds of 19% with
respect to quitting smoking behaviors across
patients under varenicline prescription at the 2nd
years relative to those patients receiving NRT.
(95% CI: 15% to 24%).
between both the groups at 6 as well as 12
months, in terms of scores of motivation to
quit, generalized anxiety disorder, patient
health outcomes and nicotine dependence.
Prescribing Prevalence, Effectiveness,
and Mental Health Safety of Smoking
Cessation Medicines in Patients With
Mental Disorders (Taylor et al. 2020)
To investigate rates of varenicline and
nicotine replacement therapy (NRT)
prescribing and the relative effects on
smoking cessation, and mental health.
Patients with mental health illnesses such as
depression, bipolar disorder, schizophrenia or
under anxiolytic or antidepressant prescriptions
were administered with either varenicline (n =
19117) or nicotine replacement therapy (NRT)
(n = 59340) belonging to a cohort of 1st of
September 2006 to 31st of December, 2015,
based upon periodic follow up evaluations
approximately: 3 months, 6th months, 9 months,
1 year, 2 years and 4 years respectively. The
results acquired from the study by Taylor et al.
(2020), indicated a positive association
between varenicline administration and
decreased incidences of mental health symptom
deterioration as compared to patients provided
with NRT, both in the presence as well as the
absence of severe mental illnesses. In
comparison to smokers who were devoid of
any mental health conditions, the results
indicated an increased odds of 19% with
respect to quitting smoking behaviors across
patients under varenicline prescription at the 2nd
years relative to those patients receiving NRT.
(95% CI: 15% to 24%).
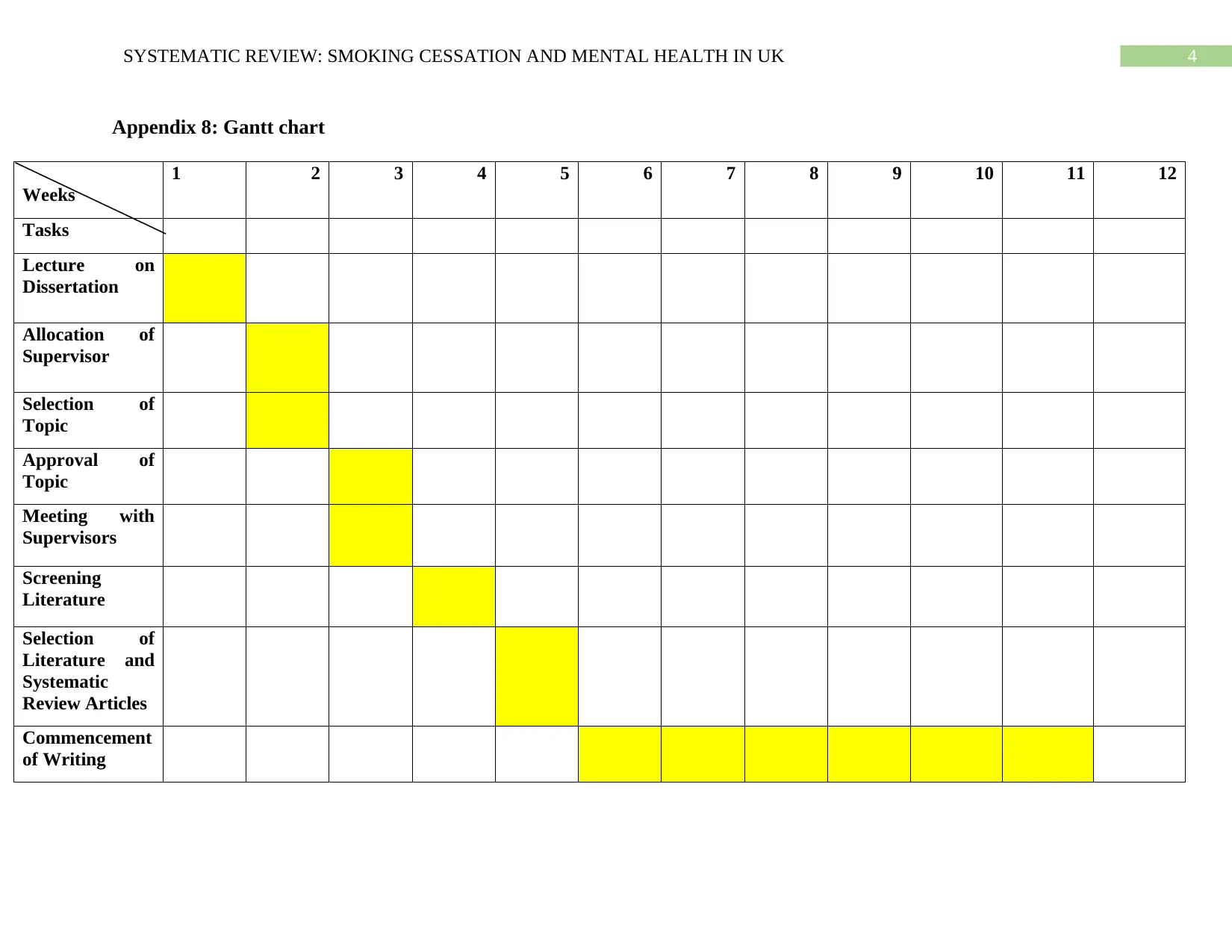
4SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
Appendix 8: Gantt chart
Weeks
1 2 3 4 5 6 7 8 9 10 11 12
Tasks
Lecture on
Dissertation
Allocation of
Supervisor
Selection of
Topic
Approval of
Topic
Meeting with
Supervisors
Screening
Literature
Selection of
Literature and
Systematic
Review Articles
Commencement
of Writing
Appendix 8: Gantt chart
Weeks
1 2 3 4 5 6 7 8 9 10 11 12
Tasks
Lecture on
Dissertation
Allocation of
Supervisor
Selection of
Topic
Approval of
Topic
Meeting with
Supervisors
Screening
Literature
Selection of
Literature and
Systematic
Review Articles
Commencement
of Writing
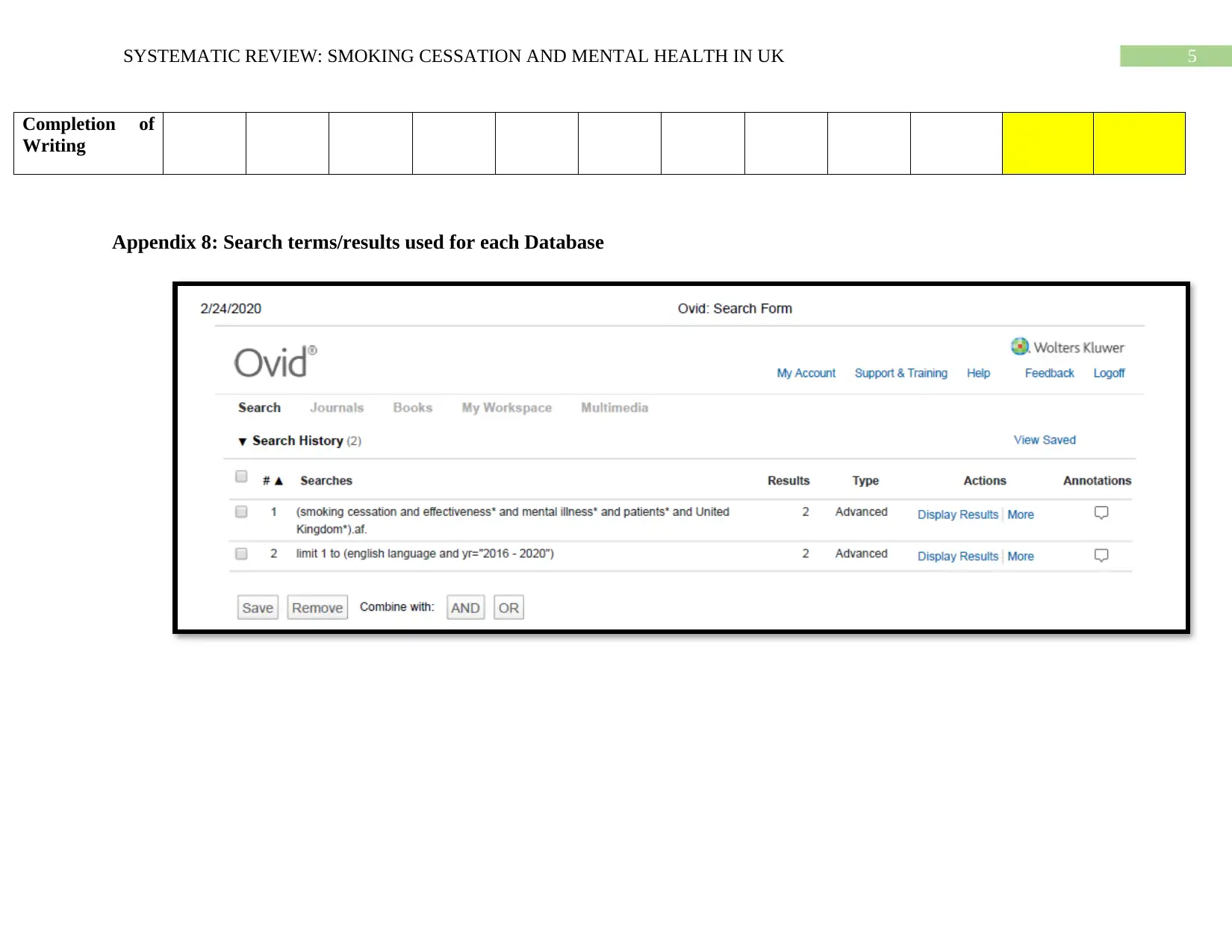
5SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
Completion of
Writing
Appendix 8: Search terms/results used for each Database
Completion of
Writing
Appendix 8: Search terms/results used for each Database
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
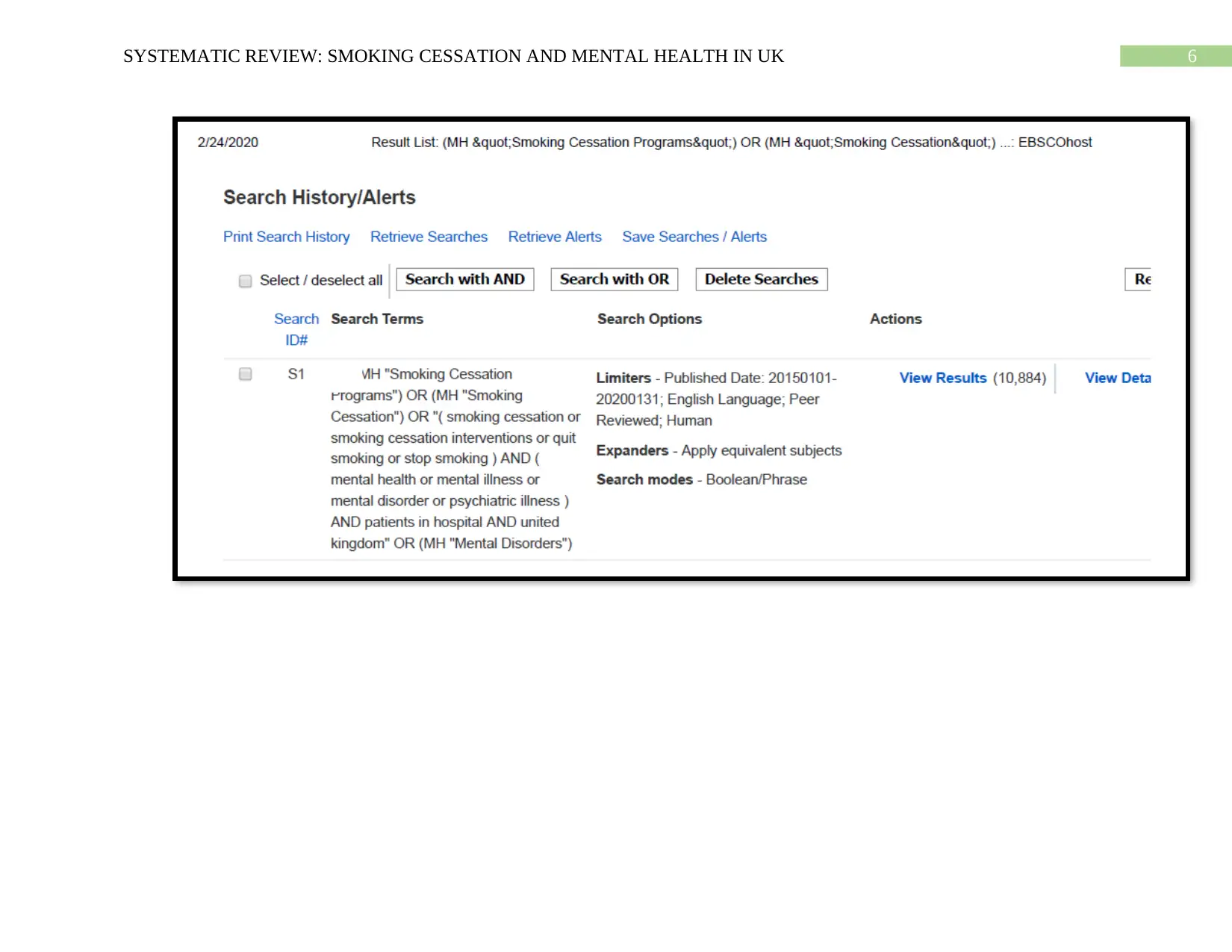
6SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
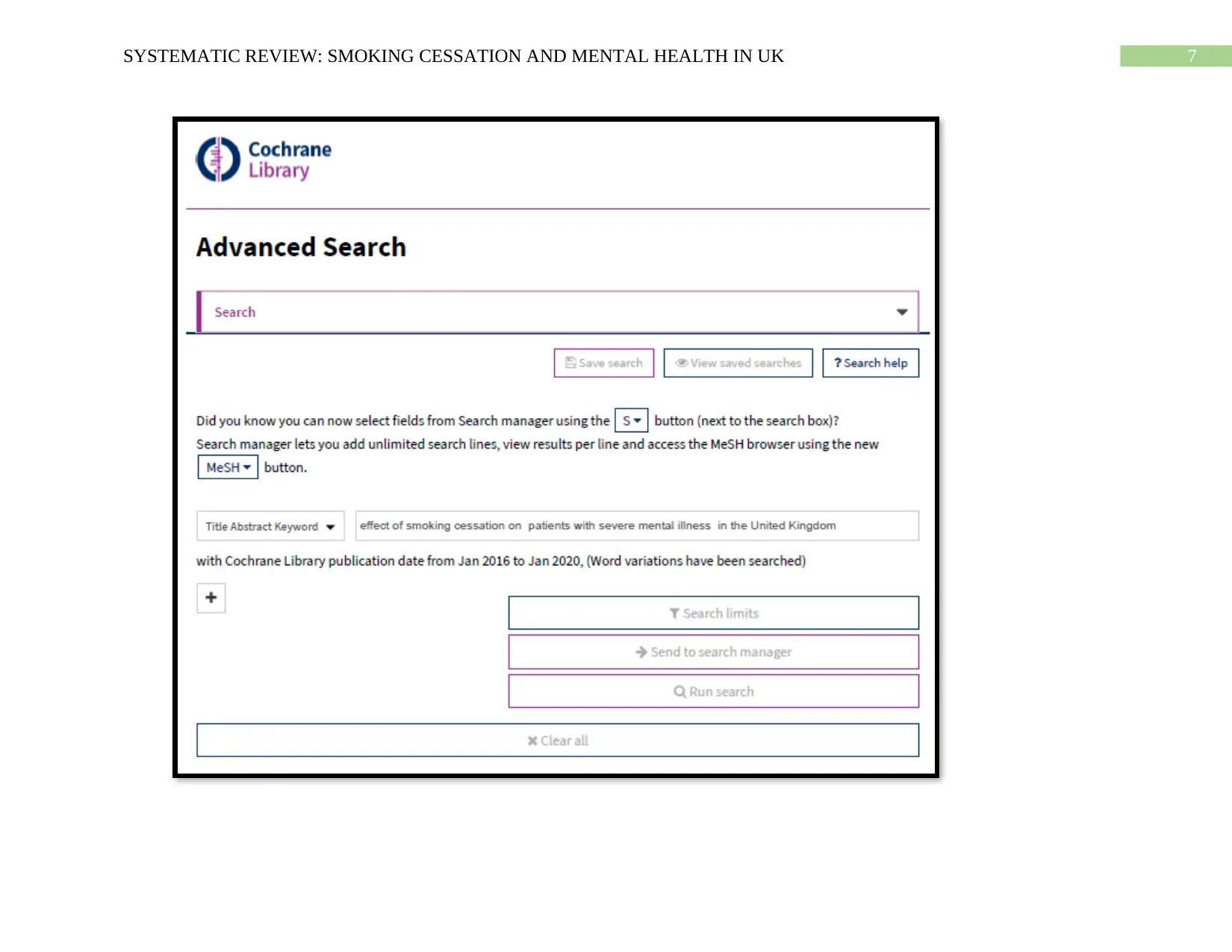
7SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
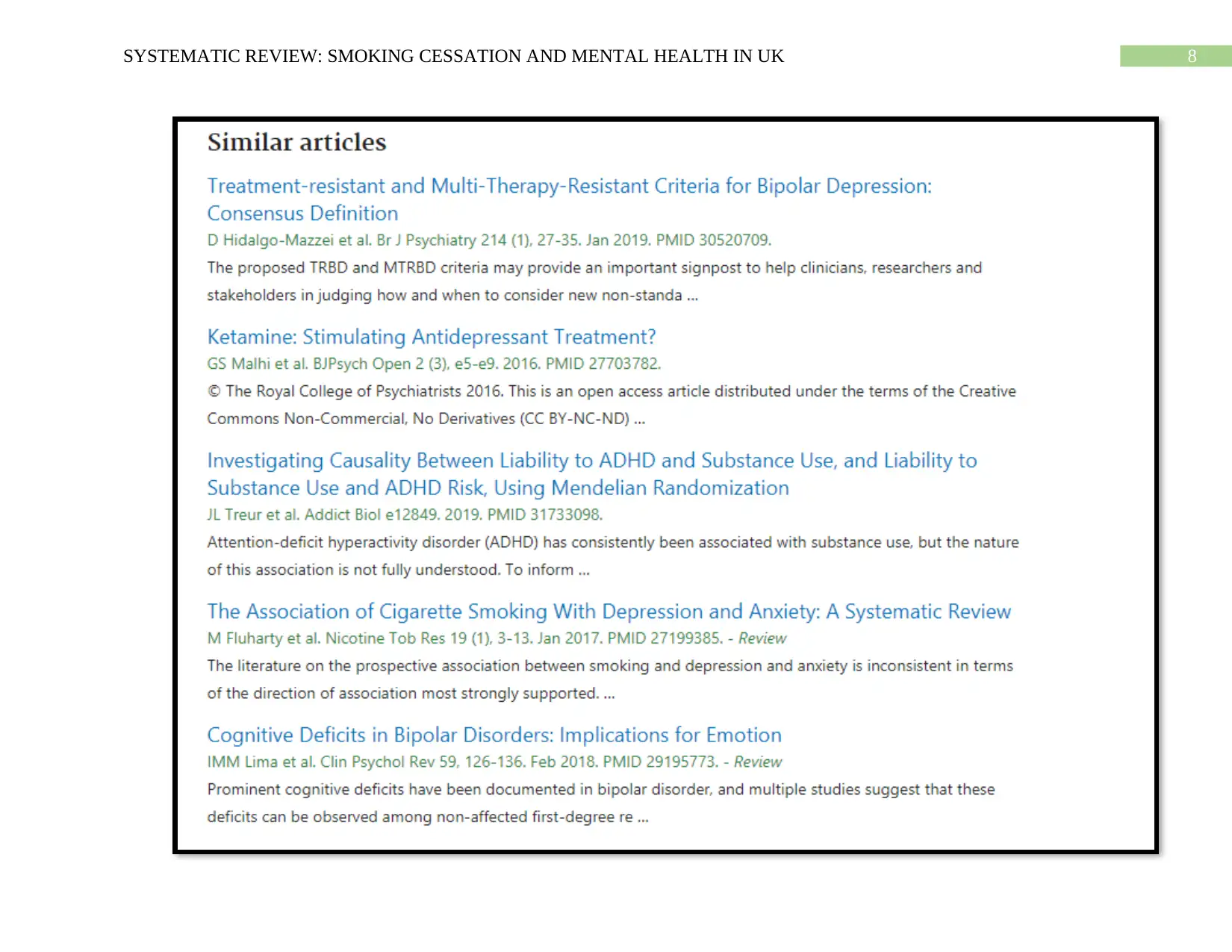
8SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
9SYSTEMATIC REVIEW: SMOKING CESSATION AND MENTAL HEALTH IN UK
1 out of 68
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





