Effects of Age and Gender in the Development of Hypertension, Tachycardia and Congestive Heart Failure
VerifiedAdded on 2023/04/07
|1
|1871
|336
AI Summary
This study examines the effects of age and gender on the development of hypertension, tachycardia, and congestive heart failure. It explores the differences in blood pressure and heart rate among males and females, as well as individuals below 30 years and those aged 30 years and above. The study aims to evaluate the role of age and gender in the acquisition of heart failure risk factors and provides insights into the physiological parameters of heart rate and blood pressure. The findings suggest that males and individuals aged 30 and above have higher rates of blood pressure and heart rates, indicating an increased risk of future acquisition of congestive heart failure.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
Effects of Age and Gender in the Development of Hypertension, Tachycardia and
Congestive Heart FailureIntroduction
The physiological condition of congestive heart failure imply a gradual loss
of the heart’s circulatory ability to pump amount of blood required for
maintenance of adequate body functioning (Fisher et al. 2016). Some of the
major risk factors of heart failure include the presence of cardiovascular
symptoms like hypertension, abnormally high or fast heart rates
(tachycardia), vasoconstriction, atherosclerosis and anthropometric
abnormalities like obesity and body fat percentage. Additionally, ageing and
gender differences have been implicated as key intangible risk factors
underlying heart failure (Yu et al. 2015). Men, as compared to women, have
been documented to pose a greater susceptibility to hypertension and
tachycardia due to the androgenic and stimulatory effects of testosterone on
the rennin-angiotensin-aldosterone-system (RAAS) (Wannamethee et al.
2016). Women after menopause, may possess higher susceptibility to gain
heart failure risks such as hypertension and heart rate, due to the
vasodilation effects of estradiol (Joyner, Wallin and Charkoudian 2016).
Additionally, ageing increase one’s susceptibility to hypertension and
tachycardia due to the ageing effects of endothelial thickening and
hardening, valve stiffening, lipofuscin induced cardiac muscle degeneration
and reduced baroreceptor functioning (Nanayakkara, Marwick and Kaye
2018). Hence, taking insights from the above, the following study will aim
to assess the effects of ageing and gender in the acquisition of heart failure
risk factors such as hypertension and tachycardia.
Aims, Objectives and Hypothesis
The aim of the following study is to evaluate the differences in blood
pressure and heart rate among females and males, who are aged 30 years
and above. Hence, the objectives of the following study include:
1. To identify the differences in blood pressure and heart rate among
males and females.
2. To assess the difference in blood pressure and heart rate among
individuals aged above and below the age of 30 years.
3. To evaluate the role of age and gender in the acquisition of heart failure
susceptibility.
Hence, the hypothesis of the following study comprises of: Males as well as
individuals who belong to the age group of 30 years and above, are in
possession of a higher susceptibility to hypertension and tachycardia
resulting in increased risk of future acquisition of congestive heart failure.
Methods
The study was conducted by recruiting 238 individuals, which comprised of
80 males and 158 females, ranging from ages of 19 to 53 years. The
participants were measured in terms of their physiological parameters such
as heart rate, systolic and diastolic blood pressure. The systolic and diastolic
blood pressures of the participants were measured using a
sphygmomanometer which relies on assessment of evaluations in mercury
columns for reflecting the pressure of blood and is recorded in term of
mm/Hg (Zakrzewski and Anthony 2018). Heart rates of the individuals were
measured through the recording of heart sounds using a stethoscope and
measured in terms of beats/minute (Stacey and Stacey 2017). The data so
collected was recorded and tabulated using computer spreadsheet software
Microsoft Excel. The data was then grouped as per age and gender and the
systolic and diastolic blood pressures and heart rate were statistically
analyzed using mean values and figures like tables and graphs.
Discussion and Conclusion
Hence, gender as well as an individual’s age have key roles to play in physiological
parameters such as heart rate and hypertension. Heart rate implies the speed with
the heart induces blood circulation throughout the body (Beauchaine and Thayer
2015). Blood pressure implies the force with which blood travels through the blood
vessels to circulate throughout the entire body (Ettehad et al. 2016). A blood
pressure above 140/90 mm/Hg indicates hypertension as per the NHS (Canoy et al.
2016). Males are generally susceptible to high blood pressures since they possess
testosterone. Testosterone has been implicated to yield androgenic effects resulting
in the activation of RAAS – the system responsible for regulating the body’s blood
pressure. Females have protective mechanisms against hypertension due to
estradiol which regulates blood pressure through vasodilation (Di Giosa et al.
2018). Ageing results in thickening, stiffening and loss of elasticity of the blood
vessels possibly due to oxidative stress and cardiac muscle degeneration due to
deposition of ‘lipofuscin’ – a compound associated with ageing (Harvey,
Montezano and Touyz 2015).
Hence, the primary research objectives and hence the initial hypothesis has been
proven since it can be observed that males and individuals who are aged above 30
showed higher values of blood pressure and heart rates. High blood pressure and
heart rate have been implicated as key risk factors for congestive heart failure.
Hence, lack of healthcare interventions of the above healthcare parameters may
increase the susceptibility of males and people aged 30 and above, of acquiring
congestive heart failure in the future (Dokainish et al. 2017).
However, the study posed several limitations. It must noted that the sample groups
were unequally distributed as per genders and ages and may result in inconclusive
findings (Heale and Twycross 2015). Further, ages of 60 and above are generally
considered standards of ageing, and hence considering a population of 30 years and
above as ‘aged’ would seem inconclusive (Steptoe, Deaton and Stone 2015).
Further, despite age and gender differences in blood pressure and heart rate, none
of the groups presented abnormally high or low values as per NHS guidelines
(Canoy et al. 2016). Hence, to conclude, while the above study highlights the age
and gender effects on cardiovascular health, one needs to engage in further
research using greater age differences, equally distributed sample groups and
measurement of other risk factors of heart failure such as anthropometrics and
body fat (Alpert et al. 2017).
References
Alpert, C.M., Smith, M.A., Hummel, S.L. and Hummel, E.K., 2017. Symptom burden in heart failure: assessment, impact on
outcomes, and management. Heart failure reviews, 22(1), pp.25-39.
Beauchaine, T.P. and Thayer, J.F., 2015. Heart rate variability as a transdiagnostic biomarker of psychopathology. International
Journal of Psychophysiology, 98(2), pp.338-350.
Canoy, D., Cairns, B.J., Balkwill, A., Wright, F.L., Khalil, A., Beral, V., Green, J., Reeves, G. and Million Women Study Collaborators,
2016. Hypertension in pregnancy and risk of coronary heart disease and stroke: a prospective study in a large UK
cohort. International journal of cardiology, 222, pp.1012-1018.
Di Giosia, P., Giorgini, P., Stamerra, C.A., Petrarca, M., Ferri, C. and Sahebkar, A., 2018. Gender differences in epidemiology,
pathophysiology, and treatment of hypertension. Current atherosclerosis reports, 20(3), p.13.
Dokainish, H., Teo, K., Zhu, J., Roy, A., AlHabib, K.F., ElSayed, A., Palileo-Villaneuva, L., Lopez-Jaramillo, P., Karaye, K., Yusoff, K. and
Orlandini, A., 2017. Global mortality variations in patients with heart failure: results from the International Congestive Heart
Failure (INTER-CHF) prospective cohort study. The Lancet Global Health, 5(7), pp.e665-e672.
Ettehad, D., Emdin, C.A., Kiran, A., Anderson, S.G., Callender, T., Emberson, J., Chalmers, J., Rodgers, A. and Rahimi, K., 2016. Blood
pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. The
Lancet, 387(10022), pp.957-967.
Fisher, S.A., Doree, C., Mathur, A., Taggart, D.P. and Martin Rendon,‐ E., 2016. Stem cell therapy for chronic ischaemic heart
disease and congestive heart failure. Cochrane Database of Systematic Reviews, (12).
Harvey, A., Montezano, A.C. and Touyz, R.M., 2015. Vascular biology of ageing—Implications in hypertension. Journal of molecular
and cellular cardiology, 83, pp.112-121.
Heale, R. and Twycross, A., 2015. Validity and reliability in quantitative studies. Evidence-based nursing, 18(3), pp.66-67.
Joyner, M.J., Wallin, B.G. and Charkoudian, N., 2016. Sex differences and blood pressure regulation in humans. Experimental
physiology, 101(3), pp.349-355.
Lacey, B.C. and Lacey, J.I., 2017. Studies of heart rate and other bodily processes in sensorimotor behavior. In Cardiovascular
psychophysiology (pp. 538-564). Routledge.
Nanayakkara, S., Marwick, T.H. and Kaye, D.M., 2018. The ageing heart: the systemic and coronary circulation. Heart, 104(5),
pp.370-376.
Steptoe, A., Deaton, A. and Stone, A.A., 2015. Subjective wellbeing, health, and ageing. The Lancet, 385(9968), pp.640-648.
Wannamethee, S.G., Shaper, A.G., Papacosta, O., Lennon, L., Welsh, P. and Whincup, P.H., 2016. Lung function and airway
obstruction: associations with circulating markers of cardiac function and incident heart failure in older men—the British Regional
Heart Study. Thorax, 71(6), pp.526-534.
Yu, O.H.Y., Filion, K.B., Azoulay, L., Patenaude, V., Majdan, A. and Suissa, S., 2015. Incretin-based drugs and the risk of congestive
heart failure. Diabetes Care, 38(2), pp.277-284.
Zakrzewski, A.M. and Anthony, B.W., 2018. Noninvasive Blood Pressure Estimation Using Ultrasound and Simple Finite Element
Models. IEEE Transactions on Biomedical Engineering, 65(9), pp.2011-2022.
Results
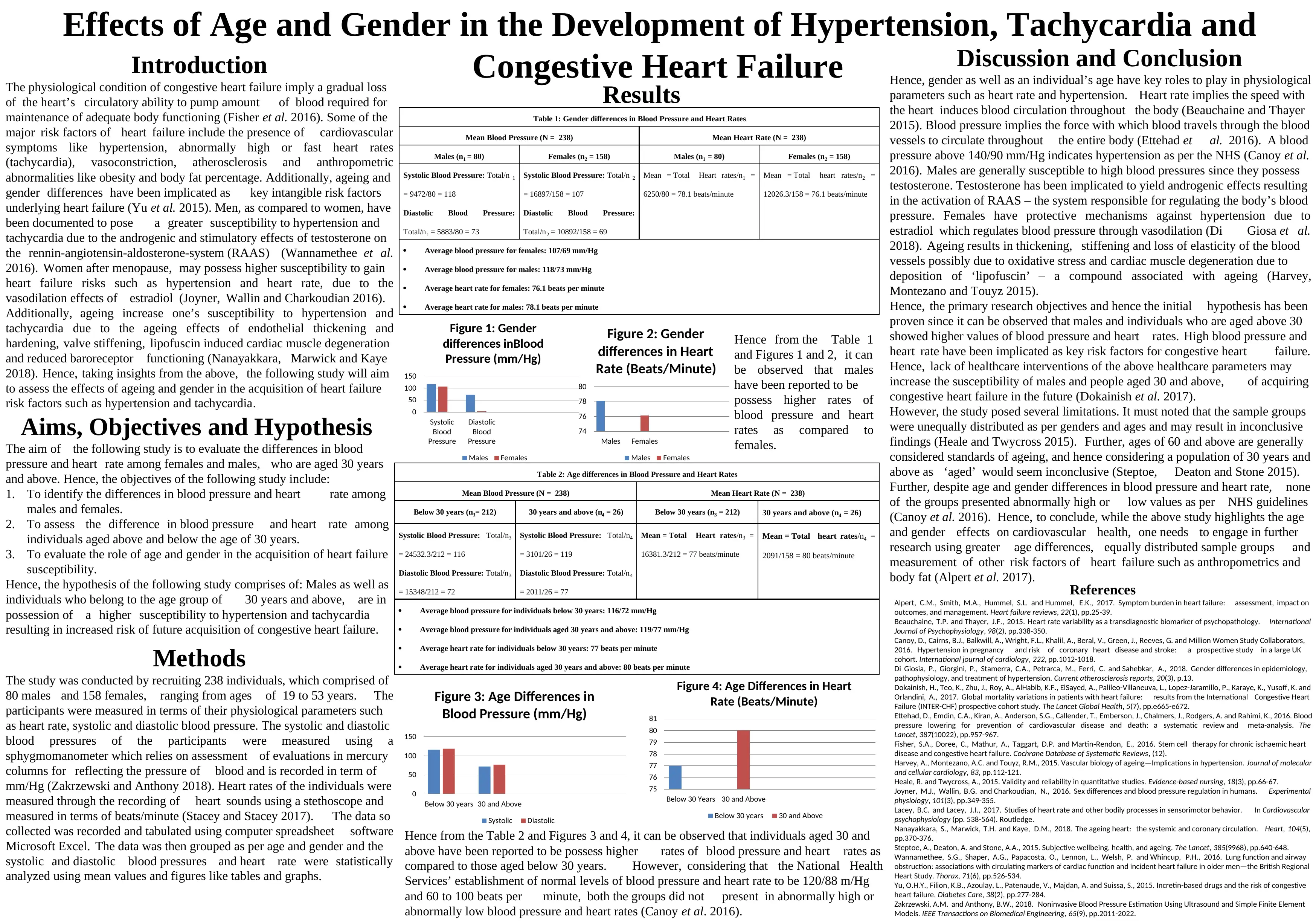
Table 2: Age differences in Blood Pressure and Heart Rates
Mean Blood Pressure (N = 238) Mean Heart Rate (N = 238)
Below 30 years (n3= 212) 30 years and above (n4 = 26) Below 30 years (n3 = 212) 30 years and above (n4 = 26)
Systolic Blood Pressure: Total/n3
= 24532.3/212 = 116
Diastolic Blood Pressure: Total/n3
= 15348/212 = 72
Systolic Blood Pressure: Total/n4
= 3101/26 = 119
Diastolic Blood Pressure: Total/n4
= 2011/26 = 77
Mean = Total Heart rates/n3 =
16381.3/212 = 77 beats/minute
Mean = Total heart rates/n4 =
2091/158 = 80 beats/minute
Average blood pressure for individuals below 30 years: 116/72 mm/Hg
Average blood pressure for individuals aged 30 years and above: 119/77 mm/Hg
Average heart rate for individuals below 30 years: 77 beats per minute
Average heart rate for individuals aged 30 years and above: 80 beats per minute
0
50
100
150
Below 30 years 30 and Above
Figure 3: Age Differences in
Blood Pressure (mm/Hg)
Systolic Diastolic
75
76
77
78
79
80
81
Below 30 Years 30 and Above
Figure 4: Age Differences in Heart
Rate (Beats/Minute)
Below 30 years 30 and Above
Hence from the Table 2 and Figures 3 and 4, it can be observed that individuals aged 30 and
above have been reported to be possess higher rates of blood pressure and heart rates as
compared to those aged below 30 years. However, considering that the National Health
Services’ establishment of normal levels of blood pressure and heart rate to be 120/88 m/Hg
and 60 to 100 beats per minute, both the groups did not present in abnormally high or
abnormally low blood pressure and heart rates (Canoy et al. 2016).
Table 1: Gender differences in Blood Pressure and Heart Rates
Mean Blood Pressure (N = 238) Mean Heart Rate (N = 238)
Males (n1 = 80) Females (n2 = 158) Males (n1 = 80) Females (n2 = 158)
Systolic Blood Pressure: Total/n 1
= 9472/80 = 118
Diastolic Blood Pressure:
Total/n1 = 5883/80 = 73
Systolic Blood Pressure: Total/n 2
= 16897/158 = 107
Diastolic Blood Pressure:
Total/n2 = 10892/158 = 69
Mean = Total Heart rates/n1 =
6250/80 = 78.1 beats/minute
Mean = Total heart rates/n2 =
12026.3/158 = 76.1 beats/minute
Average blood pressure for females: 107/69 mm/Hg
Average blood pressure for males: 118/73 mm/Hg
Average heart rate for females: 76.1 beats per minute
Average heart rate for males: 78.1 beats per minute
0
50
100
150
Systolic
Blood
Pressure
Diastolic
Blood
Pressure
Figure 1: Gender
differences inBlood
Pressure (mm/Hg)
Males Females
74
76
78
80
Males Females
Figure 2: Gender
differences in Heart
Rate (Beats/Minute)
Males Females
Hence from the Table 1
and Figures 1 and 2, it can
be observed that males
have been reported to be
possess higher rates of
blood pressure and heart
rates as compared to
females.
Congestive Heart FailureIntroduction
The physiological condition of congestive heart failure imply a gradual loss
of the heart’s circulatory ability to pump amount of blood required for
maintenance of adequate body functioning (Fisher et al. 2016). Some of the
major risk factors of heart failure include the presence of cardiovascular
symptoms like hypertension, abnormally high or fast heart rates
(tachycardia), vasoconstriction, atherosclerosis and anthropometric
abnormalities like obesity and body fat percentage. Additionally, ageing and
gender differences have been implicated as key intangible risk factors
underlying heart failure (Yu et al. 2015). Men, as compared to women, have
been documented to pose a greater susceptibility to hypertension and
tachycardia due to the androgenic and stimulatory effects of testosterone on
the rennin-angiotensin-aldosterone-system (RAAS) (Wannamethee et al.
2016). Women after menopause, may possess higher susceptibility to gain
heart failure risks such as hypertension and heart rate, due to the
vasodilation effects of estradiol (Joyner, Wallin and Charkoudian 2016).
Additionally, ageing increase one’s susceptibility to hypertension and
tachycardia due to the ageing effects of endothelial thickening and
hardening, valve stiffening, lipofuscin induced cardiac muscle degeneration
and reduced baroreceptor functioning (Nanayakkara, Marwick and Kaye
2018). Hence, taking insights from the above, the following study will aim
to assess the effects of ageing and gender in the acquisition of heart failure
risk factors such as hypertension and tachycardia.
Aims, Objectives and Hypothesis
The aim of the following study is to evaluate the differences in blood
pressure and heart rate among females and males, who are aged 30 years
and above. Hence, the objectives of the following study include:
1. To identify the differences in blood pressure and heart rate among
males and females.
2. To assess the difference in blood pressure and heart rate among
individuals aged above and below the age of 30 years.
3. To evaluate the role of age and gender in the acquisition of heart failure
susceptibility.
Hence, the hypothesis of the following study comprises of: Males as well as
individuals who belong to the age group of 30 years and above, are in
possession of a higher susceptibility to hypertension and tachycardia
resulting in increased risk of future acquisition of congestive heart failure.
Methods
The study was conducted by recruiting 238 individuals, which comprised of
80 males and 158 females, ranging from ages of 19 to 53 years. The
participants were measured in terms of their physiological parameters such
as heart rate, systolic and diastolic blood pressure. The systolic and diastolic
blood pressures of the participants were measured using a
sphygmomanometer which relies on assessment of evaluations in mercury
columns for reflecting the pressure of blood and is recorded in term of
mm/Hg (Zakrzewski and Anthony 2018). Heart rates of the individuals were
measured through the recording of heart sounds using a stethoscope and
measured in terms of beats/minute (Stacey and Stacey 2017). The data so
collected was recorded and tabulated using computer spreadsheet software
Microsoft Excel. The data was then grouped as per age and gender and the
systolic and diastolic blood pressures and heart rate were statistically
analyzed using mean values and figures like tables and graphs.
Discussion and Conclusion
Hence, gender as well as an individual’s age have key roles to play in physiological
parameters such as heart rate and hypertension. Heart rate implies the speed with
the heart induces blood circulation throughout the body (Beauchaine and Thayer
2015). Blood pressure implies the force with which blood travels through the blood
vessels to circulate throughout the entire body (Ettehad et al. 2016). A blood
pressure above 140/90 mm/Hg indicates hypertension as per the NHS (Canoy et al.
2016). Males are generally susceptible to high blood pressures since they possess
testosterone. Testosterone has been implicated to yield androgenic effects resulting
in the activation of RAAS – the system responsible for regulating the body’s blood
pressure. Females have protective mechanisms against hypertension due to
estradiol which regulates blood pressure through vasodilation (Di Giosa et al.
2018). Ageing results in thickening, stiffening and loss of elasticity of the blood
vessels possibly due to oxidative stress and cardiac muscle degeneration due to
deposition of ‘lipofuscin’ – a compound associated with ageing (Harvey,
Montezano and Touyz 2015).
Hence, the primary research objectives and hence the initial hypothesis has been
proven since it can be observed that males and individuals who are aged above 30
showed higher values of blood pressure and heart rates. High blood pressure and
heart rate have been implicated as key risk factors for congestive heart failure.
Hence, lack of healthcare interventions of the above healthcare parameters may
increase the susceptibility of males and people aged 30 and above, of acquiring
congestive heart failure in the future (Dokainish et al. 2017).
However, the study posed several limitations. It must noted that the sample groups
were unequally distributed as per genders and ages and may result in inconclusive
findings (Heale and Twycross 2015). Further, ages of 60 and above are generally
considered standards of ageing, and hence considering a population of 30 years and
above as ‘aged’ would seem inconclusive (Steptoe, Deaton and Stone 2015).
Further, despite age and gender differences in blood pressure and heart rate, none
of the groups presented abnormally high or low values as per NHS guidelines
(Canoy et al. 2016). Hence, to conclude, while the above study highlights the age
and gender effects on cardiovascular health, one needs to engage in further
research using greater age differences, equally distributed sample groups and
measurement of other risk factors of heart failure such as anthropometrics and
body fat (Alpert et al. 2017).
References
Alpert, C.M., Smith, M.A., Hummel, S.L. and Hummel, E.K., 2017. Symptom burden in heart failure: assessment, impact on
outcomes, and management. Heart failure reviews, 22(1), pp.25-39.
Beauchaine, T.P. and Thayer, J.F., 2015. Heart rate variability as a transdiagnostic biomarker of psychopathology. International
Journal of Psychophysiology, 98(2), pp.338-350.
Canoy, D., Cairns, B.J., Balkwill, A., Wright, F.L., Khalil, A., Beral, V., Green, J., Reeves, G. and Million Women Study Collaborators,
2016. Hypertension in pregnancy and risk of coronary heart disease and stroke: a prospective study in a large UK
cohort. International journal of cardiology, 222, pp.1012-1018.
Di Giosia, P., Giorgini, P., Stamerra, C.A., Petrarca, M., Ferri, C. and Sahebkar, A., 2018. Gender differences in epidemiology,
pathophysiology, and treatment of hypertension. Current atherosclerosis reports, 20(3), p.13.
Dokainish, H., Teo, K., Zhu, J., Roy, A., AlHabib, K.F., ElSayed, A., Palileo-Villaneuva, L., Lopez-Jaramillo, P., Karaye, K., Yusoff, K. and
Orlandini, A., 2017. Global mortality variations in patients with heart failure: results from the International Congestive Heart
Failure (INTER-CHF) prospective cohort study. The Lancet Global Health, 5(7), pp.e665-e672.
Ettehad, D., Emdin, C.A., Kiran, A., Anderson, S.G., Callender, T., Emberson, J., Chalmers, J., Rodgers, A. and Rahimi, K., 2016. Blood
pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. The
Lancet, 387(10022), pp.957-967.
Fisher, S.A., Doree, C., Mathur, A., Taggart, D.P. and Martin Rendon,‐ E., 2016. Stem cell therapy for chronic ischaemic heart
disease and congestive heart failure. Cochrane Database of Systematic Reviews, (12).
Harvey, A., Montezano, A.C. and Touyz, R.M., 2015. Vascular biology of ageing—Implications in hypertension. Journal of molecular
and cellular cardiology, 83, pp.112-121.
Heale, R. and Twycross, A., 2015. Validity and reliability in quantitative studies. Evidence-based nursing, 18(3), pp.66-67.
Joyner, M.J., Wallin, B.G. and Charkoudian, N., 2016. Sex differences and blood pressure regulation in humans. Experimental
physiology, 101(3), pp.349-355.
Lacey, B.C. and Lacey, J.I., 2017. Studies of heart rate and other bodily processes in sensorimotor behavior. In Cardiovascular
psychophysiology (pp. 538-564). Routledge.
Nanayakkara, S., Marwick, T.H. and Kaye, D.M., 2018. The ageing heart: the systemic and coronary circulation. Heart, 104(5),
pp.370-376.
Steptoe, A., Deaton, A. and Stone, A.A., 2015. Subjective wellbeing, health, and ageing. The Lancet, 385(9968), pp.640-648.
Wannamethee, S.G., Shaper, A.G., Papacosta, O., Lennon, L., Welsh, P. and Whincup, P.H., 2016. Lung function and airway
obstruction: associations with circulating markers of cardiac function and incident heart failure in older men—the British Regional
Heart Study. Thorax, 71(6), pp.526-534.
Yu, O.H.Y., Filion, K.B., Azoulay, L., Patenaude, V., Majdan, A. and Suissa, S., 2015. Incretin-based drugs and the risk of congestive
heart failure. Diabetes Care, 38(2), pp.277-284.
Zakrzewski, A.M. and Anthony, B.W., 2018. Noninvasive Blood Pressure Estimation Using Ultrasound and Simple Finite Element
Models. IEEE Transactions on Biomedical Engineering, 65(9), pp.2011-2022.
Results
Table 2: Age differences in Blood Pressure and Heart Rates
Mean Blood Pressure (N = 238) Mean Heart Rate (N = 238)
Below 30 years (n3= 212) 30 years and above (n4 = 26) Below 30 years (n3 = 212) 30 years and above (n4 = 26)
Systolic Blood Pressure: Total/n3
= 24532.3/212 = 116
Diastolic Blood Pressure: Total/n3
= 15348/212 = 72
Systolic Blood Pressure: Total/n4
= 3101/26 = 119
Diastolic Blood Pressure: Total/n4
= 2011/26 = 77
Mean = Total Heart rates/n3 =
16381.3/212 = 77 beats/minute
Mean = Total heart rates/n4 =
2091/158 = 80 beats/minute
Average blood pressure for individuals below 30 years: 116/72 mm/Hg
Average blood pressure for individuals aged 30 years and above: 119/77 mm/Hg
Average heart rate for individuals below 30 years: 77 beats per minute
Average heart rate for individuals aged 30 years and above: 80 beats per minute
0
50
100
150
Below 30 years 30 and Above
Figure 3: Age Differences in
Blood Pressure (mm/Hg)
Systolic Diastolic
75
76
77
78
79
80
81
Below 30 Years 30 and Above
Figure 4: Age Differences in Heart
Rate (Beats/Minute)
Below 30 years 30 and Above
Hence from the Table 2 and Figures 3 and 4, it can be observed that individuals aged 30 and
above have been reported to be possess higher rates of blood pressure and heart rates as
compared to those aged below 30 years. However, considering that the National Health
Services’ establishment of normal levels of blood pressure and heart rate to be 120/88 m/Hg
and 60 to 100 beats per minute, both the groups did not present in abnormally high or
abnormally low blood pressure and heart rates (Canoy et al. 2016).
Table 1: Gender differences in Blood Pressure and Heart Rates
Mean Blood Pressure (N = 238) Mean Heart Rate (N = 238)
Males (n1 = 80) Females (n2 = 158) Males (n1 = 80) Females (n2 = 158)
Systolic Blood Pressure: Total/n 1
= 9472/80 = 118
Diastolic Blood Pressure:
Total/n1 = 5883/80 = 73
Systolic Blood Pressure: Total/n 2
= 16897/158 = 107
Diastolic Blood Pressure:
Total/n2 = 10892/158 = 69
Mean = Total Heart rates/n1 =
6250/80 = 78.1 beats/minute
Mean = Total heart rates/n2 =
12026.3/158 = 76.1 beats/minute
Average blood pressure for females: 107/69 mm/Hg
Average blood pressure for males: 118/73 mm/Hg
Average heart rate for females: 76.1 beats per minute
Average heart rate for males: 78.1 beats per minute
0
50
100
150
Systolic
Blood
Pressure
Diastolic
Blood
Pressure
Figure 1: Gender
differences inBlood
Pressure (mm/Hg)
Males Females
74
76
78
80
Males Females
Figure 2: Gender
differences in Heart
Rate (Beats/Minute)
Males Females
Hence from the Table 1
and Figures 1 and 2, it can
be observed that males
have been reported to be
possess higher rates of
blood pressure and heart
rates as compared to
females.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1 out of 1
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





